Abstract
Background:
Understanding the policy context and how policy is implemented at the local and clinical level is an important precursor to developing preventive strategies focusing on dementia risk reduction in primary healthcare settings.
Objective:
Using England as a case study, we review policies and strategies relevant to dementia prevention from the national to local level and how these are translated into primary healthcare services.
Methods:
We conducted a scoping review covering: 1) identification of national, regional, and local policies and strategies that include dementia prevention; 2) identification of national guidelines for implementing dementia prevention at the clinical level; and 3) evaluation of the implementation of these at the clinical level.
Results:
Dementia prevention is addressed in national policy, and this filters through to regional and local levels. Focus on dementia prevention is limited and variable. Reference to modifiable risk factors is associated with other non-communicable diseases, placing less emphasis on factors more dementia specific. Evidence of implementation of dementia prevention policies at the clinical level is limited and inconsistent. Available evidence suggests messages about dementia prevention may best be delivered through primary healthcare services such as the National Health Service (NHS) Health Check.
Conclusion:
The limitations identified in this review could be addressed through development of a national policy focused specifically on dementia prevention. This could provide a platform for increasing knowledge and understanding among the general population and healthcare professionals. It would be important for such a policy to cover the full range of modifiable risk factors relevant to dementia.
Keywords: Commissioner, government, modifiable risk, primary healthcare, policymaker
INTRODUCTION
National health policies are fundamental for improving the health of a population. Evaluation of such policies is essential for understanding the impact of policy outcomes on populations, communities, and individuals particularly with respect to behavior changes [1–4]. Analysis of health policies, therefore, is core to developing public health reforms, for understanding policy failures, identifying gaps, and developing future policy [5–7]. Translation of national policies into practice, however, can be variable with barriers and challenges leading to variable provision at the clinical level [8–10]. Although there is an array of evidence on evaluating specific policy intervention programs such as those on smoking cessation and increasing physical activity [1], analysis of overall national policy implementation and outcomes is more limited [11]. Such knowledge and understanding is essential to help determine whether future practice-based interventions, particularly those focused on lifestyle modification, have the potential to be effective [3].
Numerous health policy analysis frameworks and theories [12] are available but more critical application is required as not all frameworks are necessarily transferable between high, middle, and low economic countries [5, 7]. Similarly, there are numerous methodological approaches that can be employed [2, 5, 7]. One such method is the use of case studies, a valid and common method for policy analysis applicable for researching policies from countries with any type of economies [1, 5, 13]. Case studies are useful for generating information for policy creation and restructuring, as seen in the reform of the health system in Pakistan [14]. They provide a tool for exploratory enquiry to gain understanding of a current policy, for example reviewing national policy in Kenya to identify gaps in HIV policy and practice [15]. They can help in determining policy outcomes, as in the comparison of support for USA Affordable Care Act (ACA) across four different states [16]. Case studies are particularly useful for analyzing policies in a real life setting [17, 18] and have been applied to investigate national public health initiatives and prevention of non-communicable diseases, for example secondary prevention of coronary heart disease in Ireland [11].
An area which is gaining increasing attention is the prevention of dementia. Dementia presents one of the biggest current social health care challenges [19]. The 2015 World Alzheimer Report estimated there are 47 million people worldwide aged 60 years and over with dementia, and this is predicted to rise to 131.5 million by 2050 [20]. Dementia not only has huge impact on the individuals affected but also on their relatives who often act as primary carers, on the health care system, on society, and on the national economy. Within the United Kingdom (UK), for example, the economic impact of dementia is estimated to be £26.3 billion per year including the associated costs of unpaid care, health, and social care costs. With increasing prevalence, it has been projected estimated costs will rise to £59.4 billion per year by 2050 [21]. As a cure for dementia is unlikely to be achieved by 2025, dementia prevention has become a high priority for many governments and national policymakers around the world [22].
Interventions focusing on modifying individual behavior and lifestyle may represent a promising area in dementia prevention. It is estimated that more than a third of dementia cases might be preventable through modifying health-related behaviors and other factors including years spent in education [23, 24]. For example, increasing physical activity, maintaining a healthy weight, and cessation of smoking have been associated with lower risk of dementia [23–25]. Similarly, increasing levels of complex cognitive activity and social and cultural engagement have been associated with better cognitive health [26, 27]. Interventions delivered via primary care offer an opportunity for targeting and supporting those at particularly high risk.
However, to ensure that interventions or programs specifically targeting dementia prevention are optimally beneficial, it is important to understand current national policy relevant to dementia risk-reduction, the extent to which the policy is translated into guidance and how it is being implemented in health care settings. It is also important to identify any potential gaps and barriers preventing successful implementation [28].
Here we use England as a case study to review the development of national policy on dementia risk-reduction and its local implementation. We have selected England as our focus for two reasons. First, England was one of the first countries to put dementia onto the political global map [29]. Second, it is a good example of a country with an increasingly aging population, where dementia prevalence is predicted to rise substantially with associated issues and challenges. The qualitative nature of the materials involved supports a narrative review approach [13].
We aimed to review the policy context, evaluate whether policies and strategies are available that can effectively support dementia prevention in England, and consider the wider implications, using scoping review methods. This review had four specific aims:
-
1)
To review evidence on the policies relevant to dementia risk reduction that are available in England from the national to local level, and on how these are translated into action in primary health care services.
-
2)
To identify the extent to which guidance on implementing dementia prevention at the clinical level is available.
-
3)
To evaluate the implementation of dementia prevention policies and strategies at local and clinical level.
-
4)
To consider, based on the evidence identified, what recommendations can be made about the use of primary health care services for the delivery of brief interventions focusing on lifestyle modification and dementia risk reduction.
MATERIALS AND METHODS
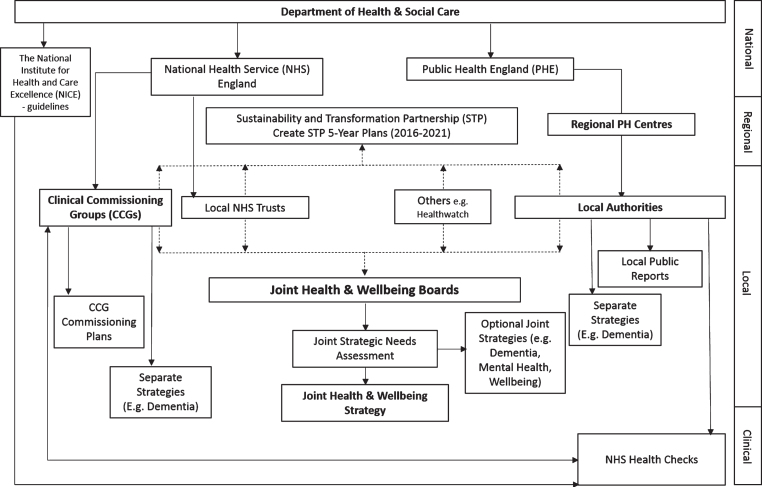
In order to evaluate policies, it is important to determine and understand the systems and actors involved in policy delivery [1, 2]. We therefore undertook an initial study to determine the structure of national policies and their delivery via regional and local systems (Fig. 1).
Fig. 1.
Structure of the England’s Department of Health & Social Care, health care commissioning bodies, and flow of policies from national to clinical level.
As the main value of case study work arises through full reporting on the data collection and analysis methods [18], we conducted this scoping review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement, following the guidelines outlined by Arksey and O’Malley (2005) [30] and a pre-defined protocol (available from the authors). A scoping review was considered more suitable than a systematic review given the aims of the review and the type of material to be reviewed, which was a combination of policy documents and primary research articles. This work did not involve human participants or animals and so no ethical approval was required.
Search strategy
As a first step we mapped current health care structures in England (Fig. 1). This structure then informed the search strategies shown in Supplementary Table 1A. We undertook a broad literature search to identify both primary research and grey literature on dementia prevention policies and strategies, their implementation at the clinical level, and guidance information.
For the purposes of this study the following terminology was used:
-
•
Policy – a specific set of principles agreed by an organization, such as the national government.
-
•
Strategy - long-term action plan, usually covering three to five years and focused on a particular goal.
-
•
Plan – sometimes used as an alternative to ‘strategy’, although possibly covering a shorter time frame (e.g., one to two years).
-
•
Action Plan - specific action points provided as a means to achieve goals laid out in policies or strategies.
-
•
Guideline - document laying out government recommended practices in order to achieve specific aims.
Any of these types of documents could be intended to exert influence at one of several levels:
-
•
National level - policies and guidance set by central government departments (i.e., England).
-
•
Regional level – focused on broad geographical regions of the country covering several local authority areas (A structured local government organization).
-
•
Local level – focused on smaller districts (e.g., a county, city, or large town) run by a single local authority.
-
•
Clinical level – focused on primary health care provision.
We identified policies and strategies by searching websites using a pre-defined strategy (see Supplementary Table 1B). To identify guidelines and evidence of implementation of policies and strategies, we have searched 22 resources including electronic databases, e.g., MEDLINE, EMBASE, Social Policy and Practice (Ovid), and online resources, e.g., NHS Evidence, NIHR Dissemination Centre (see Supplementary Table 1B for full list) for peer-reviewed primary studies, guidance documents, and evaluation reports, again using a pre-defined strategy (see Supplementary Table 1B). We chose 2009 as the start date for the searches as the first UK dementia policy document was published in that year. Where several versions of the same document existed, the most recent version was used for data extraction.
Inclusion criteria
We included policies or strategies if 1) they covered England as a whole or regions or local areas within England; 2) they included mention of dementia risk reduction or dementia prevention (regardless of significance), and 3) and in the case of regional and local policies they were initiated by national government, Sustainability and Transformation Partnerships, Joint Health and Wellbeing Boards (JHWBs), local authorities or Clinical Commissioning Groups (CCGs) (see Fig. 1 for an overview of the health care structure in England).
As dementia prevention can be considered under various categories, including general health, public health, and mental health as well as dementia or neurodegenerative disease, we included policies covering general public and mental health as long they referred to dementia prevention. National guidelines on clinical practice were also identified and included if they referred to dementia risk reduction or dementia prevention. We excluded policies not relating to England (including policies from other UK nations: Scotland, Wales, or Northern Ireland), and policies or strategies where the focus on health behavior change related to other non-communicable diseases rather than dementia. Additionally, policies were excluded if they focused on dementia screening and the ethics of screening, dementia diagnosis, support services, medication, or palliative care, or if the risk factors discussed were non-modifiable (e.g., learning difficulties, Down syndrome, Parkinson’s disease). Policies or strategies from non-government organizations, associations or charities were also excluded. Documents containing guidelines, recommended practices, and evaluation of policy implementation at the clinical level were only included if they were specific to England or English regions or local areas, and reported dementia risk or prevention policies and/or strategies at the clinical level.
We included information published in peer-reviewed journals, conference proceedings, theses or on-line platforms. For primary research articles, all types of research design were included, whether qualitative, quantitative or mixed methods. Editorials, commentaries, letters, and opinion-based papers were excluded. NHS Trust reports were excluded as these cover service provision for people with existing health conditions, rather than prevention.
Selection procedure
One researcher (RC) identified the relevant documents containing policies, strategies, and guidance. Next, we screened these documents for references to dementia prevention using key words (Dementia, Alzheimer’s, Vascular (Non-dementia policies/strategies) plus Prevent(ion), Risk, Factors, Cause, Link, Health check, Healthcheck, Polic*, Strategy, Government, National). Ten percent of all the national policies, regional, and local strategies were randomly selected using an online random number generator (https://www.random.org/lists/) for review by a second researcher (BS) to determine whether the inclusion and exclusion criteria had been met. Any disagreements regarding eligibility were discussed between the two reviewers and disagreements resolved by a third member of the review team (LC).
Data extraction
Data were extracted by one researcher (RC) using a standardized format in an Excel spreadsheet. Data from web-based resources and grey literature were presented in line with published guidelines [31]. A second researcher (BS) independently extracted data for 10% of all the national policies, regional and local strategies and any disagreements regarding extracted data were discussed between the two reviewers and disagreements resolved.
Collating, summarizing, and reporting the results
We grouped our results into three categories:
-
•
National policies, regional and local strategies.
-
•
Guidelines and recommendations for implementation of policies and strategies at clinical level.
-
•
Evaluation of implementation at local and clinical level.
Where possible we conducted narrative synthesis using thematic analysis and mapping to summaries information within the policies and strategies following Popay’s framework [32]. Based on these findings, recommendations for policymakers, commissioners, and other stakeholders were identified.
RESULTS
Structure of the healthcare system in England
We began by mapping the structure of the national healthcare system in England (Fig. 1). For simplicity, only those structures relevant to this current review have been included. The healthcare system is governed centrally via the Department of Health and Social Care. Two main organizations directed by the department are National Health Service (NHS) England and Public Health England (PHE). NHS England is responsible for clinical care, and PHE is responsible for public health programs. Local NHS services are directed by Clinical Commissioning Groups (CCGs) (n = 195) which identify the services that should be available and commission these from provider organizations such as NHS Trusts, the main organizations responsible for providing hospital and community physical and mental health care and ambulance services, or private companies. Public health is under the control of local authorities (n = 353) which are the organizations directly responsible for public services and facilities. Local authorities and CCGs, along with NHS trusts and other stakeholders combine to create regional statutory Sustainability and Transformation Partnerships (n = 44) in order to identify health issues and develop health plans specific to the region [33]. In addition, smaller statutory partnerships, the JHWBs (n = 159), are formed at the local level [34]. The purpose of the JHWBs is to formally manage partnerships between NHS, public health and local government and identify the health needs of the local population [34].
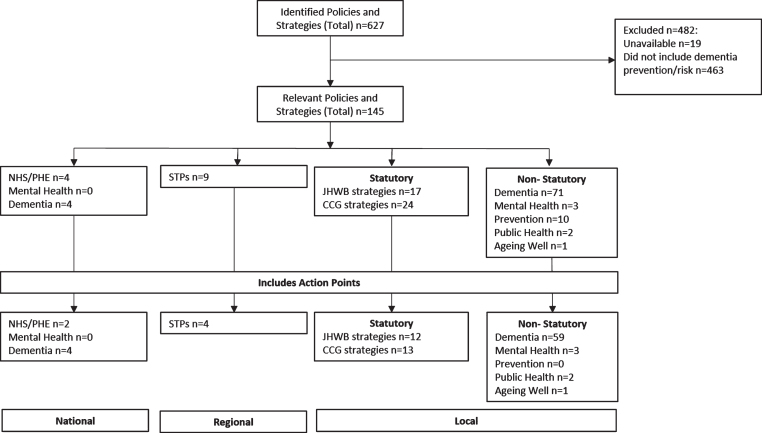
Identification of policies and strategies
A range of policies and strategies were identified at national, regional, and local levels that referred to dementia prevention (see modified PRISMA diagram in Fig. 2). A smaller proportion of these included at least one action point directly aimed at dementia prevention and risk reduction.
Fig. 2.
Modified PRISMA flow diagram showing the policies and strategies including primary dementia prevention CCG, Clinical Commissioning Group; JHWB, Joint Health and Wellbeing Board; NHS, National Health Service; PHE, Public Health England; STP, Sustainability and Transformation Plan.
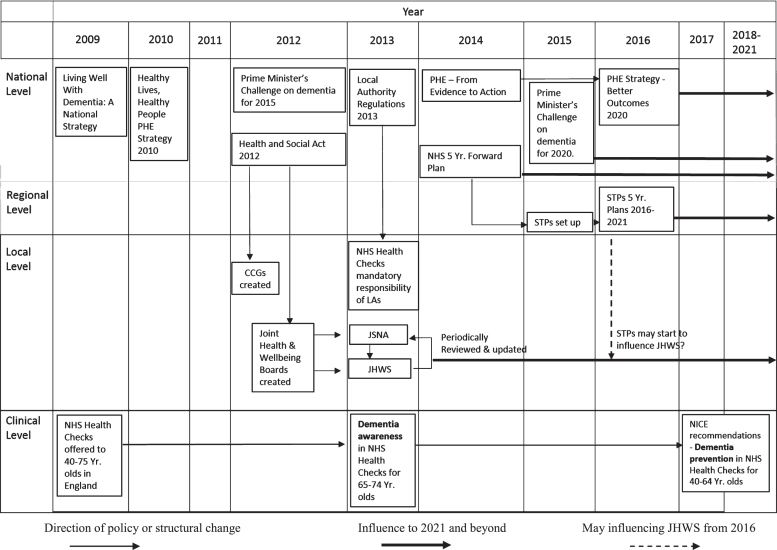
Reference to dementia prevention in national policies
Current English national dementia-specific, general, and public health policies include a focus on modifiable risk factors for dementia (Supplementary Table 2). In the case of dementia-specific policies, improving public and professional awareness and further research are described as necessary for effective dementia prevention. Among mental health policies (not presented in Supplementary Table 2; see Fig. 2), although dementia is mentioned, there is no reference to dementia prevention. Public health policies provide the most specific focus on dementia prevention and identify targeted outcomes (Supplementary Table 2). For example, dementia prevention is mentioned in ‘Healthy Lives, Healthy People: Our strategy for public health in England’ [35], later becoming a key priority in ‘Public Health England - From evidence into action: opportunities to protect and improve the nation’s health’ [36]. Specific implementation strategies proposed include the development of a personalized risk assessment calculator. The key priorities and action points drove the development of the strategic plan ‘Public Health England Strategy - Better outcomes 2020’ [37]. Concurrently the NHS 5 Year Forward View [38] highlighted the need for a comprehensive approach to prevention. These national policies which include dementia prevention have influenced strategy development at the regional and local levels (Fig. 3).
Fig. 3.
Summary of legislation, policies and strategies influencing the delivery of dementia prevention in England Direction of policy or structural change Influence to 2021 and beyond May influencing JHWS from 2016 CCG, Clinical Commissioning Group; JHWS, Joint Health and Wellbeing Strategy; JSNA, Joint Strategic Needs Assessment; LA, Local Authority; NHS, National Health Service; NICE, The National Institute for Health and Care Excellence; PHE, Public Health England; STP, Sustainability and Transformation Plan.
The inconsistency as to whether dementia prevention is considered a part of public health or combined with a specific focus dementia at national level is reflected in the strategies and plans that emerge at regional and local levels. We will consider the consequences of this divided focus below.
Implementation of government policy at the regional level
National policies filter to the regional level through the Sustainability and Transformation Partnerships producing a Sustainability and Transformation Plan (STP) (Fig. 1). The plan focuses on priorities including non-communicable disease prevention, general health and wellbeing improvement, social care, and a plan to join up health and social services (NHS 2015 Delivering the Forward View [39]). Within the STPs, the focus on dementia prevention varies greatly. Dementia prevention is sometimes not mentioned at all, sometimes presented as a brief example, and sometimes emphasized as a high priority (Supplementary Table 3; note that policies which do not refer to dementia prevention are not included). Where dementia prevention is given some prominence, the number of action points also varies; in some cases, prevention is briefly mentioned in general terms while other documents include well-constructed actions with explicit outcomes, timeframes, and responsibilities (Fig. 2; Supplementary Table 3). Only nine out of England’s 44 STPs cover dementia prevention, and four of these provide action points. Such limited information on dementia prevention within the STPs may have consequences for future priority setting, leading to a focus on improving overall health and well-being with less emphasis being given to dementia prevention (Fig. 3).
Implementation of government policies at local level
At the local level, the JHWBs produce statutory Joint Strategic Needs Assessments (JSNAs) identifying priority areas for health and well-being improvement at the local population level (Fig. 1). The JSNAs, along with national policies, STPs, and CCG plans are used to create a statutory Joint Health and Wellbeing Strategy (JHWS) targeting the whole local population. The JHWB may also produce a non-statutory strategy, targeting high-need groups or programs highlighted through the JSNA. As with the STPs, the degree of focus on dementia prevention and resulting action points at the local level is very variable. Non-statutory strategies place more emphasis on this area than statutory ones.
Statutory local strategies and plans
Statutory strategies cover both general improvement of health and well-being, e.g., increasing physical activity levels, and dementia care, often as a priority due to an aging population. There is a focus on increasing rates of early diagnosis of dementia. Dementia prevention, however, is less evident and is rarely considered a priority. Strategies including dementia prevention are shown in Supplementary Table 4. Across the 159 JHWBs, we identified 149 separate strategies; some JHWBs collaborate to produce a joint strategy (Fig. 2). Three strategies were not available. Of the 146 strategies reviewed, only 17 included reference to dementia prevention or modifiable risks, and 11 included clear prevention action points (Fig. 2). For completeness CCG plans were also checked. Dementia prevention was identified in a further 24 CCG plans, of which 13 included specific action points (Fig. 2).
The limited and variable coverage of dementia prevention within statutory strategies and plans creates a risk of a sporadic and inconsistent focus throughout the country. This could potentially mean that dementia prevention programs are delivered in certain areas only, with large swathes of the country being neglected.
Non-statutory local strategies and plans addressing specific needs
We examined whether the 353 local authorities, via the 159 JHWBs, had produced specific dementia, mental health, prevention, wellbeing, public health, or aging strategies (Supplementary Table 4). Encouragingly we identified 96 (60%) dementia-specific strategies which highlights the growing importance and focus given to dementia. Out of the 96, 70 referred to dementia prevention, with a high proportion providing details of specific action plans to reduce the risk and prevalence of dementia (Fig. 2). This is positive as it highlights that local authorities are becoming aware of dementia prevention and shows there is an appetite for reducing dementia risk. However, as these plans are non-statutory this also emphasizes the lack of accountability and variability at the local level. In addition, 35 mental health strategies were identified. Although many included mention of dementia, only three referred to prevention, mainly citing vascular factors, although North Tyneside [40] included loneliness as a risk factor (Supplementary Table 4). A further 11 strategies, 8 covering general prevention, 2 covering public health, and 1 covering aging, included mention of dementia prevention (Supplementary Table 4).
This emphasizes the variability in the type of strategies in which dementia prevention may be included, and the potential risk of fragmentation in services and focus.
Emerging key themes throughout the policies and strategies
We carried out a preliminary synthesis by identifying and coding reoccurring concepts identified across action points and statements about knowledge gaps found in the included policies and strategies. The documents were re-checked once the codes had been determined to ensure systematic thoroughness. The coded extracts were then synthesized into five emerging themes. The themes identified were 1) need to identify specific risk factors; 2) awareness and understanding among the general population; 3) awareness and understanding among healthcare practitioners and primary healthcare staff; 4) the role of NHS Health Checks; and 5) initiatives for improving health and well-being. These themes were then used to structure the analysis of the ways in which dementia prevention is implemented in practice.
Identification of risk factors
There was a strong focus on factors associated with cardiovascular (CVD) risk or risk of other non-communicable disease, e.g., physical inactivity, obesity, and smoking. Limited information or emphasis was given to dementia-specific factors including depression, sleep, cognitive stimulation, and social isolation. At the national level policies reflect the links between diet, the broad term “lifestyle” and the risk of dementia. In ‘Living Well with Dementia: A National Dementia Strategy’ (2009) it is suggested the message “What is good for your heart is good for your brain” should be embedded as part of the NHS Health Check program, which is a national program of structured clinical assessment and management for adults without pre-existing diabetes or CVD aged 40–74 years [41]. At the regional level, no STPs mentioned risks beyond those associated with cardiovascular risk. Other factors were mentioned, although infrequently, in some of the local statutory and non-statutory strategies (Fig. 2, Supplementary Table 4): social isolation or loneliness (14), general mental health or well-being (4), depression (6), education (5), cognitive or mental stimulation (2), head injury (2), and sleep (2).
Awareness and understanding in the general population
The national dementia strategies included a general objective to increase awareness and understanding of dementia with the potential to reduce prevalence, but no indication was given about how this would be achieved. One STP and one JHWB strategy mentioned the need to improve public understanding of the potential modifiable risks and the need to raise awareness about reducing the risk of dementia onset, including education about the benefits of healthy lifestyle choices in childhood. This aim was emphasized more within the dementia specific strategies, with examples of using methods such as public campaigns and integrating dementia into key health messages.
Awareness and understanding among healthcare practitioners and primary health care staff
As with the general population, national policies have highlighted the need to increase knowledge among health care professionals but, again, this is a vague objective, even though it is considered a key aspect for dementia prevention [42]. This was highlighted in subsequent dementia and public health policies [36, 43], which included the ambition to improve health care professionals’ understanding of modifiable risk factors through the delivery of education and training programs. None of the STPs included this action and at the local level, it was included only in dementia-specific strategies, with 12 of these mentioning the need for education and training, particularly for frontline staff and those delivering NHS Health Checks.
The role of primary healthcare services and NHS Health Checks
Primary healthcare services offer an important pathway for non-communicable disease prevention through modifying individual behavior and lifestyle [41]. In England, one example is the NHS Health Checks program. The program could be a potential platform for including a personalized dementia risk assessment and the potential for this has been identified in both dementia-related and public health policies [36, 37, 42, 43]. PHE (2014) [36] also included action points aimed at providing support for people to improve their lifestyles, including marketing campaigns aimed at 40 to 60-year-olds and developing a personalized risk assessment calculator. The possible role of NHS Health Checks with respect to dementia prevention is highlighted by only one STP, but it was the most frequent action referred to in both statutory and non-statutory local strategies.
Initiatives for improving health and wellbeing
Improving health and well-being and encouraging healthy lifestyle behaviors through both personal responsibility and community-based initiatives are common themes across all policies, plans and strategies at all levels of governance. This could be achieved, as stated above, through the NHS Health Check, or through the provision of care and support to those with predisposing conditions such as depression [36]. Alternatively, several action points state that dementia prevention can be supported by embedding dementia risk into programs that already aim to improve the general health of the population such as those aimed at maintaining healthy weight or improving level of physical activity (Supplementary Table 4). Interestingly, strategies aimed at reducing smoking levels did not refer to smoking as a risk factor for dementia (Supplementary Table 4; data available from corresponding author). Only one strategy was not focused on cardiovascular risks [44], and this targeted social isolation and loneliness, noting that social participation and increasing social networks could act as protective factors against cognitive decline or dementia for those over the age of 65.
Evidence of national guidelines and recommendations
Evidence of reference to national guidelines and recommendations regarding dementia prevention at the local and clinical level is limited and the available evidence is disparate. Three guidance and recommendation documents were identified: The National Institute for Health and Care Excellence (NICE) recommendations ‘Dementia, disability and frailty in later life – mid-life approaches to prevention’ [45]; ‘NHS Health Check - Best Practice Guidance’ [46]; and ‘Dementia: The NICE-SCIE Guideline on Supporting People with Dementia and their Carers’ [47, 48]. Again, the information provided in the guidelines is limited to the modifiable risk factors associated with CVD and there is encouragement to embed the messages within other health modifying advice.
Implementation of dementia prevention at local and clinical level
Three documents were identified that addressed policy and strategy implementation: a pilot study for embedding dementia prevention into NHS Health Checks [49]; an evaluation of the ‘Living Well with Dementia: A National Dementia Strategy’ [42] titled ‘Improving Dementia Services in England – an Interim Report’ [50]; and the report of this evaluation from the House of Commons Committee of Public Accounts, the body responsible for scrutinizing UK government expenditure [51].
Further information on implementation was identified via progress reports on strategies, but these were sporadic and varying in detail. Information was obtained from CCG, annual Public Health or HWB reports, HWB meeting minutes, council (elected governors of the local area, town, or city) health scrutiny reports or Healthwatch reports. Many strategies are currently in mid-term, e.g., STPs operate in a 5-year time frame that ends in 2021, and often the stated action points are long-term and difficult to measure. Only information regarding methods of raising public awareness was reported, e.g., Dementia Action Week (e.g., Northampton Borough Council 2016 [52]), local leaflets [53], public awareness events [54], and the use of social media, such as using the Twitter feed #DementiaDo … the Basics [55]. Links between wider national health campaigns such as Change4Life and community activities, particularly those aiming to improve physical activity as part of reducing the risk of dementia, were highlighted as examples of successful programs [56, 57]. Limited information was available regarding improving healthcare professionals’ knowledge, and only brief, non-specific statements about the training being provided to staff were included [58].
Information about the possible use of NHS Health Checks to present information regarding dementia risk to the local population was vague and non-specific. There was one indication that NHS Health Checks had been undertaken and that dementia awareness was a mandatory part of the health check provision (e.g., Nottinghamshire Health & Wellbeing Board 2017 [59]) but no further details were provided. Data regarding NHS Health Check invitation and uptake rates for each local authority were available from PHE which publishes figures on ‘Preventing well’, using key indicators of risk factors linked to dementia such as smoking rates with data being available for all local authorities, CCGs and STPs [60]. Information regarding whether dementia awareness was included or the quality of messaging is not recorded.
DISCUSSION
Summary
To the best of our knowledge, this is the first case study to examine the extent to which dementia prevention is considered within current national policy. Using a scoping review methodology, we examined the inclusion of dementia prevention in health policies and how this is implemented at the regional and local level. England was the focus of the study as it was one of the first nations to produce a national dementia policy and is often considered an example of good practice [29]. This review is also particularly timely due to the recent release of the World Health Organization (WHO) guide for creating dementia policies which states the need for enhancing dementia prevention [61].
Our review indicates that dementia prevention receives more attention in the public health policy domain than in relation to mental health, even though dementia itself is often covered in mental health policies. There is evidence that national dementia policies are successfully filtering to regional and local level with dementia becoming a key priority, especially in areas with a high proportion of older people, but there is considerable variation in the attention given to dementia prevention. This variation is partly accounted for by the complexity and fluidity of the healthcare structure. Across all governance levels, dementia prevention focuses primarily on risk factors related to other non-communicable diseases, such as physical activity and obesity. Limited emphasis is given to other significant factors such as social isolation, mental health, and cognitive stimulation, but this may be due to the slow and complex process of research translation into policy. There is evidence of national guidelines and recommendations being in place, such as NICE guidelines [45, 47, 48] and the recommendation to include dementia prevention in the NHS Health Checks for those aged 40–65 [46]. The guidelines and recommendations focus mainly on modifiable risks relating to CVD. The NICE guidelines (2015) [45] do state, however, interventions and programs to reduce dementia risk should include reducing loneliness and being mentally active. Evidence of implementation of dementia prevention at the local and clinical level is both limited and inconsistent.
Considering the wider context
Although this case study focuses on England, many of the concepts, issues, barriers, and recommendations are relevant internationally. However, caution is required as even when a national policy is considered successful, transferring the policy internationally does not guarantee a positive outcome due to wide variations and differences in governmental and political, social, healthcare, and economic structures [1, 10, 62], especially where policies are not backed up by specific legislation [63].
As stated, although many of the concepts, issues, and barriers identified in policies and strategies have the potential to be transferable internationally, similar caution should also be exercised when comparing the policies of different countries. As an example, one country that might be expected to be comparable with England is Australia, given similar levels of development, close cultural and social links, and complex health care systems. However, making comparisons is challenging as the health care systems have different governance structures. Overall, however, there seem to be three key differences between dementia prevention policies in the two countries: greater emphasis is given to unique factors associated with risk of dementia in Australian national and state dementia policies, suggesting a clearer distinction for dementia prevention; the Australian policies place greater emphasis on a collaborative approach to awareness raising and risk reduction, undertaken in parallel with their other relevant health priorities, including mental health; and less focus is placed on healthcare staff in the Australian policies compared to those of England. There are similarities, however, including the need to inform local communities, to target social inequalities using specific, culturally appropriate messaging, and to develop programs especially for those considered at high risk [64–68].
Key barriers to primary prevention of dementia that emerged from this study were lack of knowledge among stakeholders at all levels and limited resources. Similar barriers have been identified in other studies, for example a recent report commissioned by PHE [28]. However, as the authors stated, the review was not systematic and it was commissioned by PHE, potentially introducing bias. Some of its findings have been confirmed by the current study, such as the need for effective healthcare structures to ensure successful implementation of dementia prevention strategies. Similar conclusions were drawn from an analysis of policies on prevention and control of CVD and diabetes in Turkey which suggested the structure of the healthcare system limited the potential for implementation into practice [69]. Policies can be useful to highlight intent regarding population health but do not necessarily result in the impact intended [11].
Lack of knowledge and understanding of dementia is apparent in the terminology used in the policies. Although there are many forms of dementia, with Alzheimer’s disease being the most common, the general term “dementia” or the phrase “different types of dementia” is used in the majority of policies and strategies. General health policies and strategies (e.g., Public Health England, JHWS) refer to “dementia” risk reduction. More differentiation of risk factors relating to specific dementia types, especially vascular dementia, Alzheimer’s disease, or alcohol-related dementia/ Korsakoff’s syndrome, occurred more frequently in non-statutory strategies. There was also evidence of some confusion where Alzheimer’s disease and dementia were referred to as separate disorders.
As shown by our review, national guidelines need to be comprehensive and include accurate information [28]. However, guidelines do not necessarily guarantee successful implementation of policy, as highlighted in studies of the translation of policies on secondary prevention of coronary heart disease into practice in Ireland and Northern Ireland [11] and management of chronic diseases at the primary care level in Europe [70]. Interventions aimed at implementing policy guidance need to be conducted by well-informed and knowledgeable healthcare staff if they are to be successful [11, 28] and there is a need for increased knowledge and understanding of dementia prevention among healthcare professionals.
Implementation of policies is more likely when there is political and social focus around the launch of a policy, such as the launch of the National Dementia Strategy of Malta [71]. Initial indicators showed increases in measurable outcomes such as improved diagnosis rates [71], which is consistent with our findings in there was greater emphasis on measurable outcomes, such as diagnostic rates, in the local strategies. Establishing the long-term effectiveness and cost-effectiveness of primary prevention strategies particularly with respect to dementia proves challenging partly because of the long delay between mid-life interventions and the age at which dementia may occur [72].
This review has shown that dementia risk factors covered in policies and strategies are generally embedded within advice relating to other non-communicable diseases. It may be more beneficial to provide a specific focus on dementia prevention. Although recent systematic reviews [23, 24], along with some clinical trials such as FINGER [73], preDIVA [74], and MAPT [75], have advanced current knowledge and understanding of modifiable risk factors, continued research is needed [76] especially given the time lag involved in the translation of research into policy [77]. It is also noteworthy that mild cognitive impairment (MCI) was not addressed in any of the documents we looked at. As MCI does not necessarily progress to dementia, and some people with MCI revert to normal cognitive functioning, it could be beneficial to target this group to promote long term maintenance of cognitive health.
National campaigns specifically aimed at dementia risk reduction, similar to those in Australia, Finland, and the USA, could be beneficial for conveying relevant messages [20, 29]. Primary healthcare may be the appropriate platform for providing prevention for delivering risk messages [78]. One such example is the NHS Health Check program in England. A recent pilot study was undertaken to determine the feasibility of extending the NHS Health Checks for 40–64-year-olds with the aim of raising awareness of dementia risk reduction [49]. The pilot showed inclusion of dementia risk was feasible but highlighted the need for dementia-specific information and advice, rather than just adding dementia to the existing focus on modifying vascular risk. This is inconsistent, however, with findings from a recent qualitative study showing that members of the public preferred advice to focus on improving overall health and wellbeing rather than focusing specifically on dementia and giving them “another disease” to think about [79]. Which messages are most relevant and effective to support dementia prevention remains to be determined, and may differ for different groups in society.
Implications for research and practice
In order to effectively implement national policies at the level of local populations and individuals, there is a need for a transparent, stable, and well-structured healthcare system allowing for identification and sharing of good practice both nationally and internationally.
A separate, specific national dementia prevention policy may provide consistency in delivery throughout the country as this would separate prevention from other dementia-related issues such as diagnosis. This could provide a coherent governance structure within the public health domain, similar to the way in which prevention of other non-communicable diseases is handled [20, 29, 80]. Policies and strategies need to focus on the full range of dementia-specific factors including social isolation and lack of cognitive stimulation. Specific messages would be preferable to broad and vague statements about “improving lifestyle” or “changing behavior”. Messages about maintaining brain health and cognition could potentially be embedded in public health promotion campaigns (e.g., those focusing on weight maintenance, improving physical activity) [20, 45]. Some evidence from this review has shown that dementia prevention is sometimes included in general health strategies of this kind. However, as argued above, this only partially addresses the range of relevant factors, and carries the risk that dementia-specific messages can potentially be lost [49].
To be effective, messages should be designed for and targeted to specific audiences, including under-represented groups [81–83]. Examples of different types of messaging include the use of social media (e.g., Twitter feed #DementiaDo … the Basics) [55] and the “brainy app” [84]. Efforts to engage younger generations are important in order to embed dementia prevention into social consciousness, as in the Finnish National Plan for brain health promotion ‘TARGET 2020 - Life is Cool with Fit Brains’ project [29].
With the introduction of NHS England best practice guidelines suggesting the inclusion of dementia risk messaging for 40–74-year-olds attending NHS Health Checks [46], it is likely that frontline healthcare staff will need increased training to improve knowledge and understanding of dementia prevention and modifiable risk factors [29, 49]. It will be important to determine whether information relevant to dementia prevention is being delivered effectively at the clinical level. There is an urgent need for research of this kind as the process of implementing research into policy and policy into practice is complex and lengthy [5, 11, 77].
Strengths and limitations
The main strengths of this scoping review are the breadth and depth of the searches undertaken. We have been as systematic and thorough as possible in obtaining details of all the relevant policies and strategies at national, regional and local levels. We have strengthened this case study by using well-publicized methodological frameworks for data collection and data analysis. There were, however, several limitations to the current study. Firstly, there was inconsistency in terminology used in the various documents, with the words ‘policy’, ‘strategy’, and ‘plan’ often used interchangeably, which created challenges for identification, and it is possible that some policies or strategies may have been missed. However, the systematic approach taken in the searches limited this risk. Secondly, the health care system is subject to fluid structural changes, such as the development of Integrated Care Systems (ICSs) alongside STPs [85], the merger and dissolution of CCGs [86], and the devolution of financial control to some regional administrations, e.g., Greater Manchester [87]. This made it a complex task to determine the exact nature of current governance structures and to ensure that all strategies were correctly identified. This was compounded by the variability in partnerships formed in local areas, for example between local authorities, CCGs and other related partners. Again, however, the systematic approach to searching limited this risk.
Conclusion
The evaluation of national policies is essential for understanding the impact of policy outcomes on populations, communities, and individuals, particularly with respect to behavior change. Such evaluation also allows identification of gaps and potential reasons for failure, and supports development of future policy [5]. However, evaluation of national policy focusing on dementia prevention may be challenging and before any such evaluation is conducted it is important to define the expected outcomes of such policy (e.g., improvement in behaviors, decrease in dementia risk score, fewer dementia cases).
This is the first case study to examine how dementia prevention is addressed in national policy. The themes and implications emerging from this review show that dementia prevention appears to be more appropriately embedded in public health policies rather than as part of mental health policy, and that primary care is an appropriate platform for delivering dementia prevention. Local variation is largely due to the complexity of healthcare structures; successful policy implementation benefits from a stable and consistent healthcare structure and a validated framework for implementing policies at the clinical level, more emphasis on dementia-specific risk factors, rather than just on those that are shared with other non-communicable diseases, is needed. A separate national dementia prevention policy would aid in the delivery of brain health messages to both the general population and healthcare professionals. In order for policies to be enacted effectively in practice, consideration must be given to the social, professional, and structural context as this can lead to the success or failure of policy implementation [8]. Identifying challenges and opportunities due to policy failure or success is essential to help determine whether future practice-based interventions have the potential to deliver the desired outcomes. The findings of this review suggest that any dementia prevention interventions delivered in primary care may require added input with respect to governance and infrastructure in order to be effective.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the following grant: Centre for Research Excellence in Promoting Cognitive Health and Preventing Cognitive Decline with Chief Investigator Professor Kaarin Anstey. Funder’s number: APP 1100579.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/18-0608r1).
SUPPLEMENTARY MATERIAL
The supplementary material is available in the electronic version of this article: http://dx.doi.org/10.3233/JAD-180608.
REFERENCES
- [1]. Dodson EA, Brownson RC, Weiss SW (2012) Policy dissemination research. In Dissemination and implementation research in health: Translating science to practice, Brownson R, Colditz G, Proctor EK, Oxford University Press, Oxford, UK. [Google Scholar]
- [2]. Collins T (2005) Health policy analysis: A simple tool for policy makers. Publ Health 119, 192–196. [DOI] [PubMed] [Google Scholar]
- [3]. Bowman S, Unwin N, Critchley J, Capewell S, Husseini A, Maziak W, Zaman S, Romdhane HB, Fouad F, Phillimore P, Unal B (2012) Use of evidence to support healthy public policy: A policy effectiveness-feasibility loop. Bull World Health Org 90, 847–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Brownson RC, Chriqui JF, Stamatakis KA (2009) Understanding evidence-based public health policy. Am J Publ Health 99, 1576–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L (2008) 'Doing'health policy analysis: Methodological and conceptual reflections and challenges. Health Pol Plann 23,308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Walt G, Gilson L (1994) Reforming the health sector in developing countries: The central role of policy analysis. Health Pol Plann 9, 353–370. [DOI] [PubMed] [Google Scholar]
- [7]. Coveney J (2010) Analyzing public health policy: Three approaches. Health Promot Pract 11, 515–521. [DOI] [PubMed] [Google Scholar]
- [8]. Watt S, Sword W, Krueger P (2005) Implementation of a health care policy: An analysis of barriers and facilitators to practice change. BMC Health Serv Res 5, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Seddon D, Krayer A, Robinson C, Woods B, Tommis Y (2013) Care coordination: Translating policy into practice for older people. Qual Ageing 14, 81–92. [Google Scholar]
- [10]. McRobie E, Wringe A, Nakiyingi-Miiro J, Kiweewa F, Lutalo T, Nakigozi G, Todd J, Eaton JW, Zaba B, Church K (2017) HIV policy implementation in two health and demographic surveillance sites in Uganda: findings from a national policy review, health facility surveys and key informant interviews. Implement Sci 12, 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Prior L, Wilson J, Donnelly M, Murphy AW, Smith SM, Byrne M, Byrne M, Cupples ME (2014) Translating policy into practice: A case study in the secondary prevention of coronary heart disease. Health Expect 17, 291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Sabatier PA, (ed.) (2007) Theories of the policy process, Westview Press, Colorado, USA. [Google Scholar]
- [13]. Exworthy M, Peckham S, Powell M (2012) Shaping health policy: Case study methods and analysis, Policy Press, Bristol, UK. [Google Scholar]
- [14]. Shaikh I (2018) "Competency for public health policy analysis": A case study of Pakistan. J Glob Health Rep 2, e2018011. [Google Scholar]
- [15]. Cawley C, McRobie E, Oti S, Njamwea B, Nyaguara A, Odhiambo F, Otieno F, Njage M, Shoham T, Church K, Mee P (2017) Identifying gaps in HIV policy and practice along the HIV care continuum: Evidence from a national policy review and health facility surveys in urban and rural Kenya. Health Pol Plann 32, 1316–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Mayer M, Kenter RC, Morris JC, Lucero L (2018) State Implementation of the Affordable Care Act: Four Case Studies. Polit Pol 46, 295–319. [Google Scholar]
- [17]. Yin RK (2009) Case study research: Design and methods, Sage Publications, California, USA. [Google Scholar]
- [18]. Gilson L, Organization WH (2013) Health policy and system research: A methodology reader, World Health Organization, Geneva, Switzerland. [Google Scholar]
- [19]. Wu YT, Beiser AS, Breteler MM, Fratiglioni L, Helmer C, Hendrie HC, Honda H, Ikram MA, Langa KM, Lobo A, Matthews FE (2017) The changing prevalence and incidence of dementia over time-current evidence. Nat Rev Neurol 13, 327–339. [DOI] [PubMed] [Google Scholar]
- [20]. Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M (2016) World Alzheimer report 2016: Improving healthcare for people living with dementia: Coverage, quality and costs now and in the future, Alzheimer’s Disease International, London, UK. [Google Scholar]
- [21]. Lewis F, Karlsberg Schaffer S, Sussex J, O'Neill P, Cockcroft L (2014) The Trajectory of Dementia in the UK - Making a Difference, Office of Health Economics, London, UK. [Google Scholar]
- [22]. Lincoln P, Fenton K, Alessi C, Prince M, Brayne C, Wortmann M, Patel K, Deanfield J, Mwatsama M (2014) The Blackfriars Consensus on brain health and dementia. Lancet 383, 1805–1806. [DOI] [PubMed] [Google Scholar]
- [23]. Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, Ballard C, Banerjee S, Burns A, Cohen-Mansfield J, Cooper C (2017) Dementia prevention, intervention, and care. Lancet 390 2673–2734. [DOI] [PubMed] [Google Scholar]
- [24]. Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C (2014) Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol 13, 788–794. [DOI] [PubMed] [Google Scholar]
- [25]. Lafortune L, Martin S, Kelly S, Kuhn I, Remes O, Cowan A, Brayne C (2016) Behavioural risk factors in mid-life associated with successful ageing, disability, dementia and frailty in later life: A rapid systematic review PLoS One 11, e0144405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Valenzuela M, Sachdev PS (2009) Harnessing brain and cognitive reserve for the prevention of dementia. Indian J Psychiatr 51, S16–S21. [PMC free article] [PubMed] [Google Scholar]
- [27]. Read S, Wittenberg R, Karagiannidou M, Anderson R, Knapp M, Personal Social Services Research Unit L (2017) The effect of midlife risk factors on dementia in older age, Public Health England, London, UK. [Google Scholar]
- [28]. Wittenberg R, Karagiannidou M, Knapp M, Personal Social Services Research Unit, LSE (2017) Primary prevention of dementia: Barriers and facilitators, Public Health England, London, UK. [Google Scholar]
- [29]. Splaine M, Wortmann M, Seitzer M, Gordon K, Kerr S, Lynch C (2017) National Dementia Action Plans - Examples For Inspiration. Alzheimer’s Disease International, London, UK. [Google Scholar]
- [30]. Arksey H, O'Malley L (2005) Scoping studies: Towards a methodological framework. Int J Soc Res Meth 8, 19–32. [Google Scholar]
- [31]. Briscoe S (2017) A review of the reporting of web searching to identify studies for Cochrane systematic reviews. Res Synth Methods 9, 89–99. [DOI] [PubMed] [Google Scholar]
- [32]. Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S (2006) Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version, 1, b92. [Google Scholar]
- [33].The King’s Fund, Sustainability and transformation plans (STPs) explained https://www.kingsfund.org.uk/topics/integrated-care/sustainability-transformation-plans-explained, 21 February 2017, Accessed 10 June 2018.
- [34].The King’s Fund, Health and wellbeing boards (HWBs) explained https://www.kingsfund.org.uk/publications/health-wellbeing-boards-explained, 22 June 2016, Accessed 10 June 2018.
- [35].HM Government (2010) Healthy Lives, Healthy People: Our strategy for public health in England, The Stationary Office, London, UK.
- [36].Public Health England (2014) From evidence into action: Opportunities to protect and improve the nation’s health, PHE Publications, London, UK.
- [37].Public Health England (2016) Strategic plan for the next four years: Better outcomes by 2020, PHE Publications, London, UK.
- [38].NHS England, Five Year Forward View, HMSO, https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf, October 2014, Accessed 15 May 2018.
- [39].NHS England, NHS Improvement (Monitor and the NHS Trust Development Authority), Care Quality Commission (CQC), Health Education England (HEE), National Institute of Health and Care Excellence (NICE), Public Health England (PHE) (2015) Delivering the Forward View: NHS planning guidance 2016/17 - 2020/21, NHS England, London, UK.
- [40].North Tyneside Clinical Commissioning Group, North Tyneside Council, Mental Wellbeing in Later Life North Tyneside Joint Strategy 2017-2022, https://my.northtyneside.gov.uk/sites/default/files/consultation/related-documents/OPMH%20Strategy%20%20FINAL%20DRAFT%20for%20comment.pdf, 2017, Accessed 25 May 2018.
- [41]. Usher-Smith JA, Silarova B, Ward A, Youell J, Muir KR, Campbell J, Warcaba J (2017) Incorporating cancer risk information into general practice: A qualitative study using focus groups with health professionals. Br J Gen Pract 67, e218–e226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Department of Health (2009) Living well with dementia: A National Dementia Strategy, Department of Health, London, UK.
- [43].Department of Health (2015) Prime Minister’s challenge on dementia 2020, Department of Health, London, UK.
- [44].Hammersmith and Fulham Board for Social Inclusion, Tackling Social Isolation and Loneliness - A Strategy for Hammersmith and Fulham, http://democracy.lbhf.gov.uk/documents/s85537/Addressing%20Social%20Isolation%20and%20Loneliness%20In%20Hammersmith%20and%20Fulham%20-%20Appendix%201%20Tackling%20social%20i.pdf, Accessed 20 June 2018.
- [45].National Institute of Health and Care Excellence, Dementia, disability and frailty in later life: Mid-life approaches to delay or prevent onset overview, https://pathways.nice.org.uk/pathways/dementia-disability-and-frailty-in-later-life-mid-life-approaches-to-delay-or-prevent-onset, October 2015,Accessed 28 May 2018.
- [46].Public Health England (2017) NHS Health Check: Best practice guidance, Public Health England, London, UK.
- [47].National Institute for Health and Clinical Excellence (2007) in National Clinical Practice Guideline Number 42, National Collaborating Centre for Mental Health,The British Psychological Society and Gaskell, London, UK.
- [48].National Institute for Health and Clinical Excellence (2016) in National Clinical Practice Guideline Number 42 (Update), National Collaborating Centre for Mental Health, The British Psychological Society and Gaskell, London, UK.
- [49].Solutions Research (2017) NHS Health Check 40-64 Dementia Pilot Research Findings Summary Research Report, Solutions Research, London, UK.
- [50].National Audit Office, Improving Dementia Services in England - an Interim Report, https://www.nao.org.uk/wp-content/uploads/2010/01/091082.pdf, 14 January 2010, Accessed 3 June 2018.
- [51].House of Commons Committee of Public Accounts (2010) Improving Dementia Services in England— an Interim Report. Nineteenth Report of Session 2009- 10 The Stationery Office, London, UK.
- [52].Northampton Borough Council 2016 Health and Well-being Board, Director of Public Health Annual Report 2016/2017 - A report by the Director of Public Health and Wellbeing, Northamptonshire, 2016/17, http://www3.northamptonshire.gov.uk/councilservices/health/health-and-wellbeing-board/Documents/NCC%20DPH%20Report%20Aug%202017.pdf, Accessed 25 May 2018.
- [53].Doncaster Dementia Strategic Partnership, The Don-caster Dementia Strategy: Progress Report 2015/16, http://www.doncasterccg.nhs.uk/wp-content/uploads/2016/05/Dementia-Report.pdf, May 2016.
- [54].The Royal Borough of Kingston-Upon-Thames, Update on the progress of Annual Public Health Report 2014 recommendations, https://www.kingston.gov.uk/downloads/file/1518/update_on_the_progress_of_annual_public_health_report_2014_recommendations, Accessed 25 May 2018.
- [55].Cheshire West and Chester Council, Improving public health outcomes: 2016 Public Health Annual Report, https://cheshirewestandchester.gov.uk/documents/social-care-and-health/health-and-wellbeing/public-health/public-health-annual-report-2016.pdf, Accessed 25 May 2018.
- [56].London Borough of Richmond-Upon-Thames, Annual Report of the Director of Public Health 2016. Prevention: Redressing the balance in a time of austerity https://www.richmond.gov.uk/media/10923/annual_public_health_report_2016.pdf, 13 January 2016, Accessed 25 May 2018.
- [57].Brighton and Hove City Council, Living Well in A Health City. Annual Report of the Director of Public Health 2016/2017, https://www.brighton-hove.gov.uk/sites/brighton-hove.gov.uk/files/Director%20of%20Public%20Health%20AR%202017%20%28PDF%209MB%29.pdf, Accessed 25 May 2018.
- [58].Healthwatch Shropshire 2018, Albrighton Medical Practice Enter & View Visit Report http://www.healthwatchshropshire.co.uk/sites/default/files/uploads/Healthwatch_Shropshire_Enter_and_View.Report.Albrighton_Medical.Centre.2018.pdf, 16 May 2018, Accessed 25 May 2018.
- [59].Nottinghamshire County Council, Director of Public Health’s Annual Report 2016 - Update on Progress, http://www.nottinghamshire.gov.uk/media/129277/dph-annual-report-2016-update-final.pdf, November 2017, Accessed 25 May 2018.
- [60].Public Health England, Dementia Profile, https://fingertips.phe.org.uk/profile-group/mental-health/profile/dementia, March 2018, Accessed 20 May 2018.
- [61].World Health Organization (2018) Towards a dementia plan: A WHO guide, World Health Organization, Geneva, Switzerland.
- [62]. Stone D (2017) Understanding the transfer of policy failure: Bricolage, experimentalism and translation. Pol Polit 45, 55–70. [Google Scholar]
- [63]. McKenzie A, Sokpo E, Ager A (2014) Bridging the policy-implementation gap in federal health systems: Lessons from the Nigerian experience. J Publ Health Af 5, 82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Department of Health (2009) National Framework for Action on Dementia 2015 - 2019, Australian Government, Canberra, Australia.
- [65].NSW Department of Health (2011) Dementia Services Framework 2010-2015, State of New South Wales, North Sydney, Australia.
- [66].Department of Health (2014) Supporting people with dementia and their families and carers: Victorian dementia action plan 2014- 18, State of Victoria, Melbourne.
- [67].Office for the Ageing, Department for Families and Communities (2009) South Australia’s Dementia Action Plan 2009-2012: Facing the Challenges Together, State of South Australia, Adelaide, Australia.
- [68].Queensland Health (2010) Queensland Health Dementia Framework 2010-2014, The State of Queensland, Brisbane, Australia.
- [69]. Kilic B, Kalaca S, Unal B, Phillimore P, Zaman S (2015) Health policy analysis for prevention and control of cardiovascular diseases and diabetes mellitus in Turkey. Int J Publ Health 60, 47–53. [DOI] [PubMed] [Google Scholar]
- [70]. Brusamento S, Legido-Quigley H, Panteli D, Turk E, Knai C, Saliba V, Car J, McKee M, Busse R (2012) Assessing the effectiveness of strategies to implement clinical guidelines for the management of chronic diseases at primary care level in EU Member States: A systematic review. Health Pol 107, 168–183. [DOI] [PubMed] [Google Scholar]
- [71]. Formosa M (2018) National policies for healthy aging in Malta: Achievements and limitations Healthy Aging Res 7, e17. [Google Scholar]
- [72]. Wittenberg Rl, Anderson R, Read S, Knapp M, Personal Social Services Research Unit, LSE (2017) Why no reliable estimate can be producedfor the rate of return on investment in primary prevention of dementia, Public Health England, London, UK. [Google Scholar]
- [73]. Ngandu T, Lehtisalo J, Solomon A, Levalahti E, Ahtiluoto S, Antikainen R, Backman L, ffinninen T, Jula A, Laatikainen T, Lindström J (2015) A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 385, 2255–2263. [DOI] [PubMed] [Google Scholar]
- [74]. van Charante EPM, Richard E, Eurelings LS, van Dalen JW, Ligthart SA, Van Bussel EF, Hoevenaar-Blom MP, Vermeulen M, van Gool WA (2016) Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): A cluster-randomised controlled trial. Lancet 388, 797–805. [DOI] [PubMed] [Google Scholar]
- [75]. Vellas B, Carrie I, Gillette-Guyonnet S, Touchon J, Dantoine T, Dartigues JF, Cuffi MN, Bordes S, Gasnier Y, Robert P, Bories L (2014) MAPT study: A multidomain approach for preventing Alzheimer’s disease: Design and baseline data. J Prev Alzheimers Dis 1, 13–22. [PMC free article] [PubMed] [Google Scholar]
- [76]. Pickett J, Bird C, Ballard C, Banerjee S, Brayne C, Cowan K, Clare L, Comas-Herrera A, Corner L, Daley S, Knapp M (2018) A roadmap to advance dementia research in prevention, diagnosis, intervention, and care by 2025. Int J Geriatr Psychiatr 33, 900–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77]. Howlett M, McConnell A, Perl A (2017) Moving policy theory forward: Connecting multiple stream and advocacy coalition frameworks to policy cycle models of analysis. Aust J Publ Admin 76, 65–79. [Google Scholar]
- [78]. Demaio AR, Nielsen KK, Tersbøl BP, Kallestrup P, Meyrowitsch DW (2014) Primary Health Care: A strategic framework for the prevention and control of chronic non-communicable disease. Glob Health Action 7, 24504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79]. Robinson L, Dickinson C, Magklara E, Newton L, Prato L, Bamford C (2018) Proactive approaches to identifying dementia and dementia risk; a qualitative study of public attitudes and preferences BMJ Open 8, e018677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80]. Farrow M, Towards a Dementia Prevention Policy for Australia: Implications of the Current Evidence, Alzheimer’s Australia, https://yourbrainmatters.org.au/sites/default/files/Towards%20Dementia%20Prevention%20Policy.pdf, March 2010, Accessed 10 June 2018.
- [81]. Kelly MP, Barker M (2016) Why is changing health-related behaviour so difficult? Publ Health 136, 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Center for Disease Control and Prevention, Alzheimer’s Association (2013) The Healthy Brain Initiative: The Public Health Road Map for State and National Partnerships, 2013—2018, Alzheimer’s Association.
- [83].Center for Disease Control and Prevention (2015) The Healthy Brain Initiative:The Public Health Road Map for State and National Partnerships, 2013-2018. Interim Progress Report, Center for Disease Control and Prevention.
- [84].Dementia Australia, Your brain matters: The power of prevention, https://yourbrainmatters.org.au/, Accessed 25 May 2018.
- [85].NHS England, Integrated care - Local partnerships to improve health and care, https://www.england.nhs.uk/integratedcare/, June 2018, Accessed 28 May 2018.
- [86].NHS England, Clinical commissioning group details, https://www.england.nhs.uk/ccg-details/, 01 April 2018, Accessed 17 May 2018.
- [87].Greater Manchester Health and Social Care Partnership, Let’s take charge of our health together, http://www.gmhsc.org.uk/, Accessed 15 May 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.