Abstract
BACKGROUND
Inflammatory bowel diseases (IBD) is a heterogenous, lifelong disease, with an unpredictable and potentially progressive course, that may impose negative psychosocial impact on patients. While informed patients with chronic illness have improved adherence and outcomes, previous research showed that the majority of IBD patients receive insufficient information regarding their disease. The large heterogeneity of IBD and the wide range of information topics makes a one-size fits all knowledge resource overwhelming and cumbersome. We hypothesized that different patient profiles may have different and specific information needs, the identification of which will allow building personalized computer-based information resources in the future.
AIM
To evaluate the scope of disease-related knowledge among IBD patients and determine whether different patient profiles drive unique information needs.
METHODS
We conducted a nationwide survey addressing hospital-based IBD clinics. A Total of 571 patients completed a 28-item questionnaire, rating the amount of information received at time of diagnosis and the importance of information, as perceived by participants, for a newly diagnosed patient, and for the participants themselves, at current time. We performed an exploratory factor analysis of the crude responses aiming to create a number of representative knowledge domains (factors), and analyzed the responses of a set of 15 real-life patient profiles generated by the study team.
RESULTS
Participants gave low ratings for the amount of information received at disease onset (averaging 0.9/5) and high ratings for importance, both for the newly diagnosed patients (mean 4.2/5) and for the participants themselves at current time (mean 3.5/5). Factor analysis grouped responses into six information-domains. The responses of selected profiles, compared with the rest of the participants, yielded significant associations (defined as a difference in rating of > 0.5 points with a P < 0.05). Patients with active disease showed a higher interest in work-disability, stress-coping, and therapy-complications. Patients newly diagnosed at age > 50, and patients with long-standing disease (> 10 years) showed less interest in work-disability. Patients in remission with mesalamine or no therapy showed less interest in all domains except for nutrition and long-term complications.
CONCLUSION
We demonstrate unmet patient information needs. Analysis of various patient profiles revealed associations with specific information topics, paving the way for building patient-tailored information resources.
Keywords: Inflammatory bowel diseases, Information needs, Patient education, Knowledge resources, Patient profiles
Core tip: A majority of inflammatory bowel diseases (IBD) patients have inadequate information regarding their disease. Self-knowledge in chronic diseases improves long-term outcomes. We performed a nationwide survey of 571 IBD patients utilizing a 28 items questionnaire to measure the adequacy of patients' knowledge and define unmet needs, and examined whether different patient profiles drive unique needs. We found a universal lack of information among the participants regarding IBD. Different patient profiles, as derived from demographic and clinical parameters, had clinically relevant associations with unique information needs. We aim for future adoption of a personalized education approach by building a patient tailored information resource website.
INTRODUCTION
Inflammatory bowel diseases (IBD) comprising Crohn’s disease (CD) and ulcerative colitis (UC) are characterized by chronic, immune mediated inflammation within the gastrointestinal tract. As exacerbations are unpredictable, and the course is potentially progressive, IBD have an important psychosocial impact[1,2]. Patients’ well-being, mental state, employment, family planning and nutrition, among others, are all negatively affected[3-5]. Furthermore, chronic dependence on medications and need for surgery impose further burdens on patients. To help with coping, patients benefit from consistent education, a recommendation made in consensus guidelines[1,2].
Previous studies have explored both the needs and the support systems available for and used by IBD patients. While patients with active disease were often concerned about symptoms, patients in remission still had disease-related concerns[3]. Both newly diagnosed and those with long standing IBD believed it was highly important to receive information on a wide range of topics close to the time of diagnosis, while in fact, a majority indicated they received little or no information in many areas that they judged to be very important[6-9].
Most IBD patients rely on their gastroenterologist and the Internet for obtaining disease-related information. In two recent studies, medical specialists were rated as the most desired vehicle for information transfer, but the Internet was considered to be very acceptable source by more than 60% of patients[6,8]. Moreover, up to 75% of patients felt that obtaining more information would be useful, and audits of IBD internet support sites showed that continued enhancement was possible[8-10]. Finally, understanding patient needs will also assist in patient activation and shared decision making, and, as such, may improve outcomes[11,12]. According to the International Patient Decision Aids Standards Collaboration, a key process in the area of developing information decision aids is to find out what information patients need and want[13]. In previous studies of information needs, no attempt was made to explore whether different IBD patient characteristics drive specific information needs.
The aims of our study were to conduct a national survey of IBD patients' information needs, to identify gaps in the information received, and to relate unique patient characteristics to specific information needs. This would enable construction of a Web-based information resource capable of tailoring information delivery for patients’ specific characteristics.
MATERIALS AND METHODS
Study population
This study was approved by the Hadassah-Hebrew university hospital Ethics Boards. All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment. IBD patients from the Israeli Crohn’s and Colitis Foundation database were contacted via email or phone. Alternatively, IBD patients were approached during their follow-up visits in five hospital-based IBD clinics in Israel and asked to participate in the survey. Participants completed the questionnaire via the web from home or through dedicated computers at the hospital clinics. Analysis of computer IP addresses showed that there was a participation level of over 90% for patients recruited during the clinic visit.
In all, 1320 subjects were contacted and 1221 agreed to participate, of these 571 completed the survey to a point that allowed inclusion into the study (43%). The participants included 382 (66.9%) with CD, 179 (31.3%) with UC and 10 (1.8%) with IBD-undefined. According to a recent epidemiological study, there are an estimated 38291 IBD patients in Israel, 20,196 with CD (53%) and 17810 with UC (47%) (Unpublished data by the Israeli IBD Research Nucleus IIRN). There were no significant differences regarding disease type, gender, country of birth, current age, age at diagnosis, level of education, and occupational status between patients who did not complete the survey and those who were included in the analysis (data not shown).
Measures
We collected demographic information including sex, age, marital status, employment and education. Clinical questions included disease type (CD, UC, IBD-undefined), age at diagnosis, age at presentation, history of flare ups, previous hospitalization, previous surgery, and current medical treatment (mesalamine, corticosteroids, thiopurines, methotrexate and biologic agents). Additionally, respondents were asked which health care professional informed them of their diagnosis. To assess recent disease activity, subjects completed the Manitoba IBD Index (MIBDI), a single-item rating scale validated to address symptom activity over the previous 6 months, that correlates highly with other highly used symptom measures. Respondents with active disease as determined by the MIBDI rated their disease as constantly active (A), often active(B), sometimes active(C), or occasionally active (1-2 d/mo) (D). Those with inactive disease rated symptoms as occurring rarely to never over the previous 6 mo (E and F respectively)[14].
Patient information needs
The questions in this study have been used in previous research, thus allowing comparison of the findings[6,7]. First, the participants were asked to rate the amount of information they received from different sources (medical staff, family, friends, patient support groups and foundations and the internet etc.) within two months from the initial diagnosis. We utilized a list of 28 questions or items covering information regarding the disease, medical treatment, and self-management of IBD. Participants utilized a 6-point Likert scale to rate the amount of information received: none, a little, moderate amount, the right amount, too much, far too much. Additionally, there was an option for "do not recall". In order to evaluate the importance of information items for a newly diagnosed patient, participants were requested to answer the following question: ‘‘If you had a close family member or friend who just found out that they had IBD, how important do you think it would be for them to receive information in the following areas in the first 2 mo after they had received their diagnosis.’’ A Likert scale from 0 to 8 was utilized, with the anchors 0, not at all important; 4, moderately important; and 8, very important. In the final section, participants were asked to rate, on the same 0 to 8 Likert scale, the importance of the same information items to them, currently.
Factor analysis of the questionnaire responses
We employed exploratory factor analysis of the questionnaire responses, to cluster interrelated items to a small number of common factors or domains, that were primarily responsible for co variation in the data, and reflect "areas of interest" to the patients[15]. We analyzed the data concerning both current helpfulness of information (current needs), and the importance of the information at disease onset (needs at disease onset). This resulted in 6 and 4 domains, respectively. We calculated the average rating for each domain based on the rating of its comprising items.
Patient profiles
Lastly, we explored the grading of importance (at diagnosis) and helpfulness (currently) for information items as well as domains, as given by a hypothetical, predetermined set of 15 patient profiles. We generated simple patient profiles (based on one patient characteristic, e.g., time from diagnosis) as well as compound profiles (based on multiple demographic and/or clinical characteristics) thought to represent a significant portion of our real-life patients. The profiles were intended to have minimal overlap, but some patients could fall into more than one profile. We sought to examine whether specific profiles yielded positive or negative associations with single information items or with domains, and whether these profiles were statistically separate from the rest of study participants, regarding information needs.
Statistical analysis
For comparing demographic and disease characteristics between CD and UC, we utilized Fisher's exact test (categorical variables) and T-test (quantitative variables). A proportion test with Bonferroni adjustment was used to evaluate possible significant differences pertaining to different sub-variables comprising a categorical variable (e.g., all possible occupational statuses comprising the variable "occupational status").
Univariate analysis of each of the items or the domains was done for association with single demographics and clinical characteristics. As items ratings were ordinal, we utilized Spearman’s correlation for continuous demographic variables, and ANOVA with post hoc analysis for categorical demographic variables. We also performed multivariate analysis based on a general linear model (linearity assumed for items and factors distribution). Finally, we used t-test to evaluate possible differences in the ratings of items and domains for single profiles in comparison to the rest of participants. Statistical analysis was performed with the software by SPSS Inc., version 23, Chicago, IL, United States.
RESULTS
A total of 571 patients completed the questionnaire, of which nearly 30% were in symptomatic remission, as defined by MIBDI (Table 1). When comparing UC with CD patients, there were no significant differences regarding sociodemographic variables. Nevertheless, CD patients had higher mean disability rate. Most patients were informed about their disease by a gastroenterologist, though more CD patients were informed by their family physician or a surgeon (P = 0.02). Consistent with previous research, respondents with CD had higher rates of past hospitalizations and surgeries (P < 0.001)[16].
Table 1.
Characteristics of the study participants
| Crohn's Disease | Ulcerative colitis | Total | P value | ||
| Diagnosis, n (%) | 392 (69) | 179 (31) | 571(100) | NS | |
| Gender, M/F, n | 190/162 | 75/78 | 505 | NS | |
| Age, yr, mean ± SD | |||||
| Current | 33.8 ± 12.5 | 35.1 ± 15.1 | 34.2 ± 13.3 | NS | |
| At diagnosis | 24.1 ± 10.8 | 26.8 ± 12.5 | 25.0 ± 11.4 | NS | |
| Active symptoms (MIBDI A-D) | 269 (69) | 127 (71) | 396 (69) | NS | |
| Marital status, n (%) | NS | ||||
| Single | 192 (49) | 88 (49) | 280 (49) | ||
| Married | 176 (45) | 80 (45) | 265 (45) | ||
| Divorced | 19 (5) | 9 (5) | 28 (5) | ||
| Widow | 3 (< 1) | 2 (1) | 5 (< 1) | ||
| Separated | 2 (< 1) | 0 (0) | 2 (< 1) | ||
| Total | 392 (100) | 179 (100) | 571 (100) | ||
| Occupational status, n (%) | NS | ||||
| Full time work | 163 (47) | 64 (40) | 227 (44) | ||
| Part time work | 46 (13) | 23 (14) | 69 (14) | ||
| Homemaker | 9 (3) | 5 (3) | 14 (3) | ||
| Student full time | 47 (13) | 25 (16) | 72 (14) | ||
| Student part time | 38 (11) | 28 (17) | 66 (13) | ||
| Retired | 9 (3) | 9 (6) | 18 (4) | ||
| Unemployed | 15 (4) | 4 (3) | 19 (4) | ||
| Disability | 23 (7) | 3 (2) | 26 (5) | ||
| Total | 350 (100) | 161 (100) | 511 (100) | ||
| Level of education, n (%) | NS | ||||
| High school completion | 155 (50) | 68 (50) | 223 (50) | ||
| Bachelor’s degree | 105 (34) | 41 (30) | 146 (33) | ||
| Master’s degree | 43 (14) | 25 (18) | 68 (15) | ||
| Doctorate | 10 (3) | 2 (2) | 12 (3) | ||
| Total | 313 (100) | 136 (100) | 449 (100) | ||
| Diagnosis informed by, n (%) | 0.02 | ||||
| Family doctor | 25 (6) | 5 (3) | 30 (5) | ||
| Gastroenterologist | 306 (78) | 155 (87) | 461 (81) | ||
| Nurse | 1 (< 1) | 2 (1) | 3 (< 1) | ||
| Surgeon | 28 (7) | 3 (2) | 31 (5) | ||
| Parent | 12 (3) | 6 (3) | 18 (3) | ||
| Someone else | 20 (5) | 8 (5) | 28 (5) | ||
| Total | 392 (100) | 179 (100) | 571 (100) | ||
| Country of birth, n (%) | NS | ||||
| Israel | 343 (88) | 149 (83) | 492 (86) | ||
| Former Soviet Union | 18 (5) | 11 (6) | 29 (5) | ||
| Western Europe | 12 (3) | 6 (3) | 18 (3) | ||
| USA/Canada | 8 (2) | 9 (5) | 17 (3) | ||
| Middle East (Exc. Israel) | 7 (2) | 3 (2) | 10 (2) | ||
| Latin America | 3 (< 1) | 1 (0.6) | 4 (< 1) | ||
| Total | 391 (100) | 179 (100) | 570 (100) | ||
| Religion, n (%) | NS | ||||
| Jewish | 384 (98) | 173 (97) | 557 (98) | ||
| Muslim | 3 (< 1) | 2 (1) | 5 (1) | ||
| Druze | 2 (< 1) | 3 (2) | 5 (1) | ||
| Christian | 3 (< 1) | 1 (< 1) | 4 (< 1) | ||
| Total | 392 (100) | 179 (100) | 571 (100) | ||
| Family history of IBD, n (%) | NS | ||||
| 1st degree relative | 57 (15) | 16 (9) | 73 (13) | ||
| 2nd degree relative | 76 (19) | 40 (22) | 116 (20) | ||
| Total | 133 (34) | 56 (31) | 189 (33) | ||
| Prior hospitalization for IBD, n (%) | |||||
| Ever | 276 (70) | 86 (48) | 362 (63) | < 0.001 | |
| Last year | 120 (31) | 43 (24) | 163 (29) | NS | |
| Prior surgery for IBD, n (%) | |||||
| Ever | 130 (33) | 9 (5) | 139 (24) | < 0.001 | |
| Last year | 36 (17) | 3 (4) | 39 (14) | 0.005 |
NS: Non-significant; MIBDI: Manitoba Inflammatory Bowel Diseases Index; IBD: Inflammatory bowel diseases.
Table 2 shows the mean ratings (adjusted to a scale from 1-5) of the information items as derived from the study questionnaires. There was a clear deficit in the information received at disease onset, spanning all questions within the survey, with an average rating of 0.9 out of 5. There were higher ratings (approaching 1.5/5) given for information regarding medications, side effects, changes to diet, complications of disease and contacting the treating physician. There was a large gap between perceived importance of the information topics, and the actual amount delivered at disease onset. In addition, the rating of current information needs was also universally high, with few exceptions. Interestingly, some of the highest-ranking items at disease onset still ranked high currently, implying continued relevance.
Table 2.
Mean rating (adjusted to a scale from 1-5) of the 28 questionnaire items
|
(A) Importance at time of diagnosis |
(B) Actual amount received |
(C) Helpfulness currently |
|||||
| Item | mean | ± CI | mean | ± CI | mean | ± CI | |
| 1 | Common symptoms of IBD | 4.4 | 0.1 | 1.7 | 0.1 | 3.1 | 0.2 |
| 2 | Complications that may arise from IBD | 4.1 | 0.1 | 1.5 | 0.1 | 3.6 | 0.1 |
| 3 | What is known (or not known) about the causes of IBD | 3.9 | 0.1 | 1.3 | 0.1 | 3.5 | 0.2 |
| 4 | Medication treatments for IBD | 4.5 | 0.1 | 1.7 | 0.1 | 4.1 | 0.1 |
| 5 | Possible side effects of medications | 4.4 | 0.1 | 1.3 | 0.1 | 4.1 | 0.1 |
| 6 | Surgical treatments that may be required for IBD | 3.7 | 0.1 | 1.1 | 0.1 | 3.3 | 0.2 |
| 7 | How to manage pain related to IBD | 4.4 | 0.1 | 0.7 | 0.1 | 3.9 | 0.1 |
| 8 | How to manage symptoms other than pain of IBD | 4.3 | 0.1 | 0.8 | 0.1 | 3.9 | 0.1 |
| 9 | How to adjust medications when symptoms cause more problems | 4.5 | 0.1 | 0.9 | 0.1 | 4.0 | 0.1 |
| 10 | When to contact your doctor | 4.6 | 0.1 | 1.5 | 0.1 | 3.4 | 0.2 |
| 11 | How IBD or the medications may affect their fertility | 4.2 | 0.1 | 0.4 | 0.1 | 3.6 | 0.2 |
| 12 | How to manage time away from work or school related to IBD | 4.3 | 0.1 | 0.4 | 0.1 | 3.6 | 0.2 |
| 13 | Insurance coverage if they run out of sick days at their work place | 4.5 | 0.1 | 0.3 | 0.1 | 4.0 | 0.1 |
| 14 | Changes to diet that may be helpful when the disease is active | 4.6 | 0.1 | 1.5 | 0.1 | 3.9 | 0.1 |
| 15 | Changes to diet that may be helpful when the disease is inactive | 4.5 | 0.1 | 1.2 | 0.1 | 3.9 | 0.1 |
| 16 | What foods offer the best nutritional value | 4.3 | 0.1 | 0.9 | 0.1 | 3.8 | 0.1 |
| 17 | What nutritional deficiencies you may be at risk for | 4.4 | 0.0 | 1.0 | 0.0 | 3.8 | 0.0 |
| 18 | When to use nutritional supplements | 4.1 | 0.1 | 0.8 | 0.1 | 3.5 | 0.2 |
| 19 | Patient's children risk of developing IBD at some point in their life | 3.9 | 0.1 | 0.5 | 0.1 | 3.5 | 0.2 |
| 20 | Informing family members about IBD | 3.7 | 0.1 | 0.3 | 0. | 2.3 | 0.2 |
| 21 | Sources of support in coping with IBD | 4.3 | 0.1 | 0.6 | 0.1 | 3.5 | 0.2 |
| 22 | Long-term prognosis/outcome of IBD | 4.3 | 0.1 | 0.7 | 0.1 | 3.9 | 0.1 |
| 23 | Risk of developing cancer | 4.1 | 0.1 | 0.7 | 0.1 | 3.8 | 0.1 |
| 24 | Alternative medicine treatments for IBD | 4.1 | 0.1 | 0.5 | 0.1 | 3.8 | 0.1 |
| 25 | How to deal psychologically with the diagnosis of IBD | 4.4 | 0.1 | 0.5 | 0.1 | 3.8 | 0.2 |
| 26 | Tools for dealing with stress affecting or resulting from the disease | 4.2 | 0.1 | 0.4 | 0.1 | 3.8 | 0.1 |
| 27 | How IBD may affect military service | 3.9 | 0.1 | 0.8 | 0.1 | 1.8 | 0.2 |
| 28 | Religious topics that may be related to IBD | 2.9 | 0.2 | 0.2 | 0.1 | 1.9 | 0.2 |
A: Rating of the importance of information for a friend or family member with new onset inflammatory bowel diseases; B: Rating of actual amount of information received within 2 mo following diagnosis; C: Rating of helpfulness of information currently. IBD: Inflammatory bowel diseases.
We performed factor analysis of the participants responses (see Tables S1 and S2, Supplementary Data, which present the full results of factor analysis). Analysis of items regarding current needs yielded 6 domains and regarding needs at disease onset yielded 4 domains (Table 3, and Supplementary Table S3). Interestingly, most information domains were homogenous and included clinically related information items, implying that participants tended to give similar ratings to associated items. Nevertheless, some items didn't intuitively fit into the domain theme (e.g., fertility was clustered within the domain work-disability). The domains were named according to the dominant theme of the clustered items.
Table 3.
Ratings of information domains
|
Rating of importance of information domains at disease onset1 |
||||
| Information domain as per factor analysis | Not important, n (%) | Moderately/very important, n (%) | Mean rating 0-8 (± CIa) | |
| Domain 1 | Managing symptoms and therapy | 15 (3) | 503 (97) | 7.1 ± 0.1 |
| Domain 2 | Stress-coping | 41 (8) | 475 (92) | 6.9 ± 0.1 |
| Domain 3 | Complications | 52 (10) | 465 (90) | 6.4 ± 0.1 |
| Domain 4 | Nutrition | 18 (4) | 499 (96) | 7 ± 0.1 |
| Rating of helpfulness of information domains at current time2 | ||||
| Information domain as per factor analysis | Not helpful, n (%) | Moderately/very helpful, n (%) | Mean rating 0-8 (± CIa) | |
| Domain 1 | Managing symptoms, therapy and complications | 60 (12) | 420 (88) | 5.9 ± 0.2 |
| Domain 2 | Nutrition | 59 (12) | 423 (88) | 6.1 ± 0.2 |
| Domain 3 | Stress-coping | 64 (13) | 317 (87) | 6.1 ± 0.2 |
| Domain 4 | Family, society, and religion | 247 (51) | 235 (49) | 3.2 ± 0.3 |
| Domain 5 | Work-disability | 70 (15) | 412 (85) | 6.1 ± 0.2 |
| Domain 6 | Long term complications | 68 (14) | 413 (86) | 5.9 ± 0.2 |
Participants rated how important the information to be given to family member or friend during the two-month period following diagnosis with inflammatory bowel diseases on a 9-point scale with the following anchors: 0-2 (not important); 3-5 (moderately important); 6-8 (very important);
Participants rated current helpfulness of information on a 9-point rating scale with the anchors: 0-2 (not helpful); 3-5 (moderately helpful); 6-8 (very helpful).
95% confidence interval.
Table 3 shows the rating of importance of information domains at disease onset (3A), and rating of helpfulness of information domains at the current time (3B), respectively, as derived from factor analysis. As for disease onset, all domains were rated as "very important". Regarding current needs, all domains were rated "very helpful" (6/8), except for domain 4 (family, society and religion) which was rated as "moderately helpful" (3.2/8).
Univariate analysis of the items or the domains did not yield clinically significant associations with the demographic or clinical characteristics. After considering typical patients attending our IBD clinics, 15 different patient profiles were constructed, some simple and some compound (Table 4). Apart from an overlap of 35% between profiles 5 and 13, the maximal overlap between profiles was 25%.
Table 4.
Number of responders matching each predetermined patient profile
| Profiles | n | |
| Compound | ||
| 1 | Patients with active disease (MIBDI A/B/C) and a history of hospitalization during the preceding 12 mo | 94 |
| 2 | Patients with significantly active disease (MIBDI A/B/C) treated with immunomodulators and biologic agents | 52 |
| 3 | Patients in remission while treated with immunomodulators and/or biologic agents | 26 |
| 4 | Patients in remission treated only with mesalamine or receiving no treatment | 90 |
| 5 | Patients aged 21-65 yr with any active disease (MIBDI A/B/C/D) | 341 |
| 6 | Patients with any active disease (MIBDI A/B/C/D) and a previous surgery for IBD | 92 |
| 7 | Patients older than age 50 yr, diagnosed during the preceding 12 mo | 8 |
| 8 | Patient younger than age 21 yr, diagnosed during the preceding 12 mo | 21 |
| Simple | ||
| 9 | Patients diagnosed during the preceding 12 mo | 92 |
| 10 | Patients hospitalized during the preceding 12 mo | 163 |
| 11 | Patients diagnosed more than 10 yr ago | 212 |
| 12 | Patients who had surgery during the preceding 12 mo | 39 |
| 13 | Patients with highly disease activity (MIBDI A/B) | 246 |
| 14 | Patients diagnosed at age > 50 yr | 72 |
| 15 | Patients who were unemployed or received disability pension during the preceding 12 mo | 45 |
MIBDI: Manitoba Inflammatory Bowel Diseases Index; IBD: Inflammatory bowel diseases. MIBDI A/B: Highly active disease; A/B/C: Significantly active disease (at least weekly symptoms); A/B/C/D: Refers to any active disease.
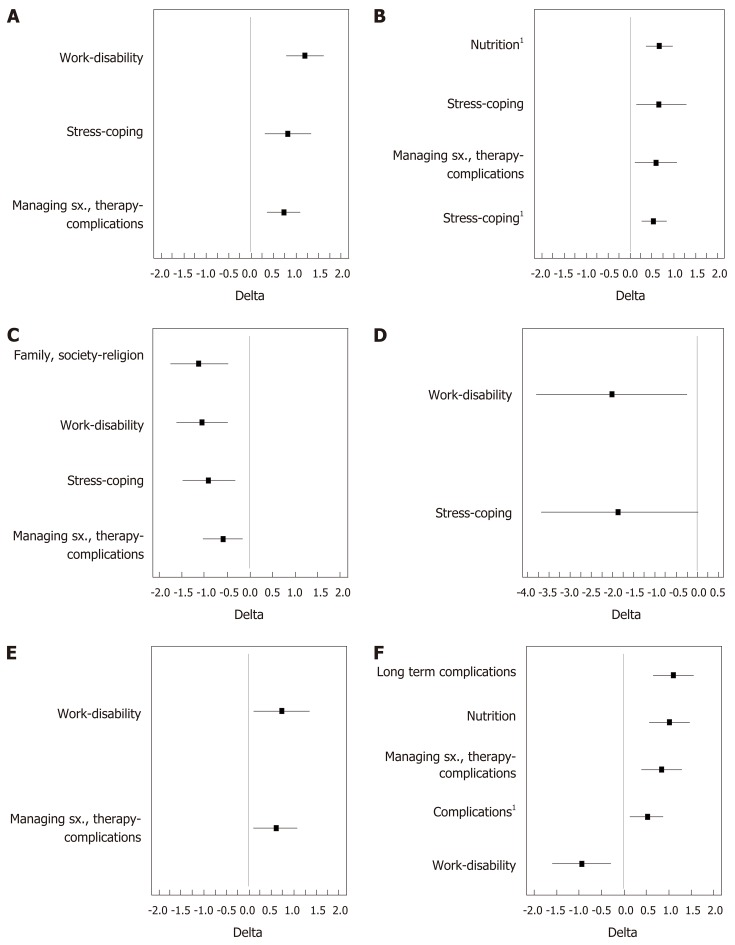
Profiles were analyzed for positive or negative association with domains and with items, regarding both current needs, and needs at disease onset. The difference between the average rating given by the profile and that given by the rest of the participants was considered to be clinically significant if it was greater than 1 point regarding domains, and greater than 0.5 points regarding single items. Table 5 lists all the significant disparities in rating of domains between patient profiles (compound and simple) and the rest of the participants. Significant disparities in ratings of items are presented in Tables S4 and S5 (Supplementary Data). Importantly, within a given profile, the highest-ranking items didn’t necessarily belong to the highest-ranking domain. A graphical presentation of the differences between selected profiles vs. other participants is shown in Figure 1.
Table 5.
Clinically significant disparities in rating of domains1
| mean ± CI2 profile vs others | Deltaa | |||
| P1: Patients with active disease (MIBDI A/B/C) and a history of hospitalization during the preceding 12 mo | ||||
| Domains | DC5 | Work-disability | 7.1 ± 0.3 vs 5.9 ± 0.2 | 1.2 |
| DC3 | Stress-coping | 6.7 ± 0.4 vs 5.9 ± 0.2 | 0.8 | |
| DC1 | managing symptoms, therapy-complications | 6.5 ± 0.3 vs 5.8 ± 0.2 | 0.7 | |
| P2: Patients with significantly active disease (MIBDI A/B/C) treated with immunomodulators and biologics | ||||
| Domains | DD4 | Nutrition | 7.6 ± 0.3 vs 6.9 ± 0.1 | 0.7 |
| DC3 | Stress-coping | 6.7 ± 0.6 vs 6 ± 0.2 | 0.7 | |
| DC1 | managing symptoms, therapy-complications | 6.4 ± 0.4 vs 5.8 ± 0.2 | 0.6 | |
| DD2 | Stress-coping | 7.4 ± 0.3 vs 6.8 ± 0.1 | 0.6 | |
| P3: Patients in remission while treated with immunomodulators and/or biologics | ||||
| Domains | DD3 | Complications | 5.5 ± 0.8 vs 6.5 ± 0.1 | -1 |
| DD1 | managing symptoms, therapy | 6.6 ± 0.7 vs 7.2 ± 0.1 | -0.6 | |
| P4: Patients in remission while treated with mesalamine or receiving no treatment | ||||
| Domains | DC4 | Family, Society & Religion | 2.3 ± 0.6 vs 3.4 ± 0.3 | -1.1 |
| DC5 | Work-disability | 5.3 ± 0.6 vs 6.3 ± 0.2 | -1 | |
| DC3 | Stress-coping | 5.3 ± 0.6 vs 6.2 ± 0.4 | -0.9 | |
| DC1 | managing symptoms, therapy-complications | 5.4 ± 0.5 vs 6 ± 0.2 | -0.6 | |
| P5: Patients aged 21-65 yr with any disease activity (MIBDI A/B/C/D) | ||||
| Domains | DC5 | Work-disability | 6.5 ± 0.2 vs 5.6 ± 0.4 | 0.9 |
| DC1 | managing symptoms, therapy-complications | 6.1 ± 0.2 vs 5.5 ± 0.3 | 0.6 | |
| DC3 | Stress-coping | 6.3 ± 0.3 vs 5.7 ± 0.4 | 0.6 | |
| P7: Patients older than age 50 yr, diagnosed during the preceding 12 mo | ||||
| Domains | DC5 | Work-disability | 4.1 ± 2 vs 6.2 ± 0.2 | -2.1 |
| DC3 | Stress-coping | 4.2 ± 1.9 vs 6.1 ± 0.2 | -1.9 | |
| P8: Patients younger than age 21 yr, diagnosed during the preceding 12 mo | ||||
| Domains | DC1 | managing symptoms, therapy-complications | 4.6 ± 1.5 vs 5.9 ± 0.1 | -1.3 |
| DD1 | managing symptoms, therapy | 6 ± 1.1 vs 7.2 ± 0.1 | -1.2 | |
| DD4 | Nutrition | 5.9 ± 1.3 vs 7 ± 0.1 | -1.1 | |
| DD3 | Complications | 5.6 ± 1.1 vs 6.5 ± 0.1 | -0.9 | |
| P10: patients hospitalized during the preceding 12 mo | ||||
| Domains | DC5 | Work-disability | 6.7 ± 0.3 vs 5.9 ± 0.3 | 0.8 |
| DC1 | managing symptoms, therapy-complications | 6.3 ± 0.3 vs 5.7 ± 0.2 | 0.6 | |
| P11: Patients diagnosed more than 10 yr ago | ||||
| Domains | DC5 | Work-disability | 5.5 ± 0.4 vs 6.5 ± 0.2 | -1 |
| P12: Patients who had surgery during the preceding 12 mo | ||||
| Domains | DC5 | Work-disability | 6.8 ± 0.6 vs 6.1 ± 0.2 | 0.7 |
| DC1 | managing symptoms, therapy-complications | 6.4 ± 0.4 vs 5.8 ± 0.2 | 0.6 | |
| P13: Patients with high disease activity (MIBDI A/B) | ||||
| Domains | DC4 | Family social and religion | 3.6 ± 0.4 vs 2.9 ± 0.3 | 0.7 |
| DC1 | managing symptoms, therapy-complications | 6.2 ± 0.2 vs 5.7 ± 0.2 | 0.5 | |
| P14: Patients diagnosed at age > 50 yr | ||||
| Domains | DC6 | Long term complications | 6.9 ± 0.4 vs 5.8 ± 0.2 | 1.1 |
| DC2 | Nutrition | 6.9 ± 0.4 vs 5.9 ± 0.2 | 1 | |
| DC1 | managing symptoms, therapy-complications | 6.6 ± 0.4 vs 5.8 ± 0.2 | 0.8 | |
| DD3 | Complications | 6.9 ± 0.3 vs 6.4 ± 0.2 | 0.5 | |
| DC5 | Work-disability | 5.3 ± 0.7 vs 6.2 ± 0.2 | -0.9 | |
| P15: Patients who were unemployed (or received disability pension) during the preceding 12 mo | ||||
| Domains | DC4 | Family social and religion | 4.2 ± 0.9 vs 3.1 ± 0.2 | 1.1 |
Profile 6 and 9 not included due to lack of clinically significant differences;
95% confidence intervals;
P < 0.05. P: Profile; DD: Domains concerning needs at disease onset; DC: Domains concerning current needs.
Figure 1.
Forest plots showing the magnitude of difference ("Delta") between the rating of information domains given by profiles vs other participants. A, B, C, D, E and F stands for profiles 1, 2, 4, 7, 12 and 14, respectively. A: Patients with active disease [Manitona Inflammatory Bowel Diseases Index (MIBDI) A/B/C] and a history of hospitalization during the preceding 12 mo (n = 94); B: Patients with significantly active disease (MIBDI A/B/C) treated with immunomodulators and biologics (n = 52); C: Patients in remission while treated with mesalamine or receiving no treatment (n = 90); D: Patients older than age 50 years, diagnosed during the preceding 12 mo (n = 8); E: Patients who had surgery during the preceding 12 mo (n = 39); F: Patients diagnosed at age > 50 years (n = 72). Positive values indicate increased interest in the information domain, negative value indicates decreased interest. 1In which case data pertains to information needs at time of disease onset, presented data pertains to current information needs. MIBDI: Manitona Inflammatory Bowel Diseases Index.
Compared with the rest of the participants, patients with significantly active disease (MIBDI A/B/C) and a history of hospitalization in the preceding year, ranked higher scores for the domains work-disability, stress-coping and therapy-complications, all pertaining to current needs. Within work-disability the most important items were: How to manage time away from work or school and how IBD or the medications may affect fertility. Patients who had surgery during preceding year ranked higher scores for work-disability and managing symptoms, therapy-complications, both pertaining to current needs. Within the latter, the most important item was surgical treatments that may be required for IBD. Patients with significantly active disease (MIBDI A/B/C) treated with immunomodulators and biologics gave higher rating for nutrition and stress-coping concerning disease onset, and for stress-coping and managing symptoms, therapy-complications concerning current needs. Patients in remission while treated with mesalamine or receiving no treatments showed less interest in the domains family, society and religion, work-disability, stress-coping and managing symptoms, therapy-complications, all pertaining to current needs. At the item level, the most prominent negative associations were with sources of support in coping with IBD and how to manage pain related to IBD. Patients diagnosed at an age older than 50 ranked higher scores for long term complications, nutrition, managing symptoms, therapy-complications pertaining to current needs, and for complications pertaining to disease onset. On the other hand, they showed less interest, currently, in work-disability. Patients aged > 50 but with a recent diagnosis of IBD ranked lower scores for work-disability and stress-coping. On the other hand, at the item level, the most prominent associations were increased interest in risk of developing cancer and complications that may arise from IBD. As for all patients with a recent diagnosis, positive associations didn’t reach a level of significance, but they did show a statistically significant negative association with stress-coping. Patients who were unemployed over the last year showed more interest in familial, social and religious issues.
DISCUSSION
Our study demonstrates a large information deficit among IBD patients. In responding to questions about the information received at disease onset, a majority indicated they received little or no information on a wide variety of topics that they judged to be very important.
The medical literature concerning patients' information about IBD has been inconsistent. In studies performed up to the early 1990s, most patients viewed their information as inadequate. Multiple European studies reported that 70%-80% of participants viewed their information to be less than adequate and desired more information[8,17-19]. Studies published since 2000 present a different view. For instance, only 10% of Irish IBD patients and 15% of Spanish IBD patients, many of whom had longstanding disease, felt they had inadequate information[20,21]. The average disease duration in our study was 9.7 years for CD and 8.3 years for UC. Ninety-two participants (16%) were diagnosed over the prior 12 mo, while 212 (37%) were diagnosed more than 10 years ago.
In a British study from 2001 (n = 168), 64% reported being well informed[22]. Bernstein et al[7] studied information needs and preferences of recently diagnosed patients with IBD. Among 74 participants, 24%, 31% and 45% reported being dissatisfied, moderately satisfied and very satisfied with the information about their disease, respectively. The same group studied the information needs of 272 persons with longstanding IBD. Recalling the information they were given at the time of diagnosis, 80% rated as very important information regarding symptoms, complications, and medical treatment, while only 10%-36% believed they received the right amount of information about these issues. The majority of information items were rated as very helpful at the current time by more than 50% of participants[6]. A Swiss study from 2016 explored patient needs at different stages of disease and found that 27% of 728 IBD patients were dissatisfied with information received at the time of diagnosis. The activity of disease affected patients’ responses. Forty-three percent of patients with flare were concerned about drugs and therapies, while 57% of patients in remission had concerns on research and developments, and 27% of them searched for information linked to daily disease management. Activity of disease was positively correlated with Information-seeking[9].
Differences in study populations may have had influenced the results. The shorter the disease duration, the more likely that patients reported that they didn’t accrue enough information. In addition, it is reasonable that wider access to the internet increased over the years and enabled patients to get more information regarding their disease. Furthermore, English speakers probably have more information available compared to other groups.
Prior to establishing educational and coping aids for patients, it is important to understand their unique needs. Apart from disease duration and activity, previous studies have not explored whether different patient characteristics drive specific information needs. After analyzing 15 patient profiles, we demonstrated differences in information needs, reflected by positive or negative associations with domains and items. Some associations were expected, while others were surprising and non-intuitive. Patients with active disease showed more interest in the domains work-disability and stress-coping, ranking them higher than medical therapy, the latter generally considered by caregivers to be the most significant topic in the patient-physician interaction. A potential explanation might be the fact that a larger body of information regarding medications and complications was relayed to patients upon diagnoses, as Table 2 suggests. These results emphasize the importance of a multi-disciplinary team caring for patients with IBD to inform patients on a wide range of medical and social topics. Fertility was also a high-ranking topic in patient profiles with active disease. Work-disability was the highest-ranking domain in patients following surgery. Studies from recent years have shown work-disability rates approaching 30% in patients with IBD, mostly being partial rather than complete disability[23,24].
Nutrition was the leading domain for patients with active disease while receiving maximal medical therapy. This may reflect the fact that lack of remission with medical therapy may lead IBD patients to look for other treatment options. Stress-coping followed nutrition in ranking. As expected, patients in remission while receiving mesalamine or no therapy showed less interest in most domains.
A surprising finding was that participants older than 50 showed more interest in long term complications, possibly reflecting more awareness of the natural history of IBD among this population. On the other hand, patients below age 21 were less interested in a wide range of domains and items, possibly a reflection of a wide lack of awareness of the complexity and consequences of IBD and a higher reliance on parents for decisions regarding the diseases. Alternatively, older, more mature patients may have a greater curiosity as to the impact of the a newly diagnosed disease in many domains, whereas young adults may be more focused on issues that have an immediate impact. An interesting finding was that patients with a recent diagnosis, both below (not shown in Table) and above age 50, showed less interest in stress-coping. Our data suggest that the activity of disease, rather than a recent diagnosis, is the drive for stress and the determinant for seeking of coping tools and aids.
The strength of our work lies in its large sample size, asking about information needs at diagnosis and currently and implementing new approaches for analyzing information needs. A limitation, however, is that surveys may be biased by who completes and does not complete them. The high response rate in the clinic sample increases our confidence that the findings are well representative of the IBD population. The findings are also limited by the questions asked. Persons with IBD may have other information needs that were not addressed here.
Our study demonstrates large information gaps among IBD patients. While it is imperative to ask individuals what information they want in order to supply their specific information needs accordingly, there are many patients, especially at disease onset that are not fully aware what to ask regarding their disease. Our study demonstrates that different patient characteristics drive specific information needs. With the use of machine learning and advanced bioinformatics we plan to utilize the data that were acquired to develop a web-based resource for IBD patients. By analyzing simple clinical and demographic parameters that are introduced by the patients, this platform would be able to suggest specific items that were shown in this study to be of high interest in a large cohort of patients, and thus provide per-sonalized information.
ARTICLE HIGHLIGHTS
Research background
Inflammatory bowel diseases (IBD) are heterogenous, lifelong diseases, with an unpredictable and potentially progressive course. Being an IBD patient means, in most cases, chronic use of medications, some with significant adverse effects, and, not infrequently, need for repeated surgeries. As affected patients are mostly young in their second or third decade of life, IBD imposes negative psychosocial impact on many aspects of their lives. Research on other chronic illnesses suggests that patients who are well informed about their disease probably have improved adherence and outcomes. Research among IBD patients showed that a majority of them received insufficient information regarding their disease. Patients usually rely on the internet or their gastroenterologist to receive information regarding their disease. The fact that IBD is a complex, heterogenous disease that encompasses a wide range of information topics, probably makes a one-size fits all computerized knowledge resource overwhelming and cumbersome, and make relevant and adequate patient education in the everyday visit in the gastroenterology clinic impractical and ineffective. Yet, in previous research, no attempt was made to explore personalized patient needs. We hypothesized that different patient profiles may have different information needs, and as such may allow building versatile, personalized computer-based information resources in the future.
Research motivation
The main topics that drove our interest in performing this research were: evaluating the self-knowledge among a large group of real-life patients, defining unmet needs in current practice, and, most importantly, exploring whether information needs differ in relation to patients’ clinical and demographic characteristics. The central problem to be solved is how to communicate personalized information to specific patients in a practical and effective way. The findings of our research are to serve as a platform for large scale future research and for applying the gained knowledge in the process of building new platforms for patient educations.
Research objectives
We aimed at and were actually able to evaluate the scope of patient self-knowledge in a large nationwide survey of IBD patients, to identify gaps of knowledge and define unmet needs, and explore whether different patient profiles correlate with different information needs. Our findings will serve future comparable research in other countries, and assist in planning newer platforms for patient education and assess their impact on compliance and outcomes.
Research methods
We performed a nationwide survey of 571 IBD patients (both ulcerative colitis and Crohn’s disease) utilizing a 28 items questionnaire to measure the adequacy of patients' knowledge and define unmet needs. The novelty of our research lies in two major methodological areas. Following the analysis of the participants' responses we utilized the technique of factor analysis in order to cluster the responses into a few, strongly representative clusters or “knowledge domains”, that were used in further analysis of the data. Another innovation was the utilization of a predefined set of real-world patient profiles for analyses of the data, replacing the conventional statistical methods of uni- and multivariate analyses. By doing so we looked for significant associations between specific patient profiles and unique information needs, both in terms of domains and in terms of specific items.
Research results
In the initial analyses we found a universal deficit in patient self-knowledge, spanning most of the items in the questionnaire. Participants gave low ratings for the amount of information received at disease onset (averaging 0.9/5). As for the importance of the same information items, participants gave high ratings, both as perceived for the newly diagnosed patient (mean 4.2/5) and for the participants themselves at current time (mean 3.5/5). These findings emphasize the need to delineate associations between patient- profiles and knowledge-needs, in a way that can prioritize the supply of knowledge according to a patient's values and needs. Factor analysis grouped participants’ responses into six information-domains. The responses of selected patients’ profiles, compared with the rest of the participants, yielded significant, clinically relevant, associations. Patients with active disease showed a higher interest in the domains work-disability, stress-coping, and therapy-complications. Patients newly diagnosed at age > 50, and patients with long-standing disease (> 10 years) showed less interest in work-disability. Patients in remission with mesalamine or no therapy showed less interest in all domains except for nutrition and long-term complications. Larger, populations-based studies, incorporating a wide range of IBD patient are needed to further delineate the links between patient characteristics and information needs, in a way that computerized algorithms can, in a stepwise process, navigate the patient through all knowledge domains that may be relevant to him.
Research conclusions
Our major findings are that IBD patients are mostly lacking self-knowledge regarding their disease and that patients differ in their information needs. We made a clear demonstration of the link between patient “profiles” (encompassing demographic, clinical and psychosocial variables) and their information needs. Not all patients need the same information in a given disease state and a given time in their life. Similar to drug therapy in the era of personalized medicine, education and information delivery should not be generic to the whole range of patient population. Rather, it should be personalized as much as possible, hoping to increase relevance and effectiveness. Personalized education resources may improve patient compliance and outcomes. The centrality of IBD in gastroenterological practice worldwide necessitates efforts to improve the education of our patients so they can feel in control, and engage in shared decision making that may in turn improve their compliance and outcomes. Our study paves the way to building a patient tailored information resource.
Research perspectives
Patients with chronic, complex disease may lack adequate knowledge regarding their disease state, and as such it may be not surprising that many of them do not comply with therapy and experience negative psychosocial impact on their daily lives. Physicians may not be aware of the importance of patient education, and the everyday clinical encounter in the clinic is far from being a suitable platform for relaying adequate information to our patients. In addition, different patients are probably interested in different information topics at different disease states and time, so our digital platforms should be updated to handle such heterogeneity. Large scale cross sectional surveys can serve to fine-tune the process of patient education while prospective cohorts can examine the impact of such education programs on disease control, patient well being and long term outcomes.
ACKNOWLEDGEMENTS
The authors are indebted to the Israeli Crohn and Colitis Foundation for aiding in patient recruitment. The authors would like to thank all patients who have chosen to participate in this study.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Israel
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: The study was reviewed and approved by the local ethical committee at Hadassah Medical center number 0327-14-HMO.
Informed consent statement: All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment.
Conflict-of-interest statement: The authors declare no conflict of interest regarding this manuscript.
Data sharing statement: Statistical code and dataset available from the corresponding author at [Saleh@Hadassah.org.il]. Consent was not obtained for data sharing but the presented data are anonymized and risk of identification is low.
STROBE statement: The authors have read the STORBE Checklist, and the manuscript was prepared and revised according to it.
Peer-review started: March 19, 2019
First decision: April 30, 2019
Article in press: June 23, 2019
P-Reviewer: Matsui T, Romano M, Tarnawski AS, Yang MS S-Editor: Yan JP L-Editor: A E-Editor: Zhang YL
Contributor Information
Saleh Daher, Institute of Gastroenterology and Liver Diseases, Hadassah-Hebrew University Medical Center, Jerusalem 91120, Israel. saleh@hadassah.org.il.
Tawfik Khoury, Institute of Gastroenterology and Liver Diseases, Hadassah-Hebrew University Medical Center, Jerusalem 91120, Israel; Department of Gastroenterology, Galilee Medical Center, Faculty of Medicine in the Galilee, Bar-Ilan University, Nahariya 22100, Israel.
Ariel Benson, Institute of Gastroenterology and Liver Diseases, Hadassah-Hebrew University Medical Center, Jerusalem 91120, Israel.
John R Walker, IBD Clinical and Research Centre, University of Manitoba, Winnipeg, MB R3E3P4, Canada.
Oded Hammerman, Institute of Gastroenterology and Liver Diseases, Hadassah-Hebrew University Medical Center, Jerusalem 91120, Israel.
Ron Kedem, Research Branch, IDF Medical Corps, Tel-Hashomer, Ramat Gan 52630, Israel.
Timna Naftali, Institute of Gastroenterology, Meir Medical Center, Kfar-saba 4428164, Israel; Sackler School of Medicine, Tel-Aviv University, Tel-Aviv 6997801, Israel.
Rami Eliakim, Sackler School of Medicine, Tel-Aviv University, Tel-Aviv 6997801, Israel; Institute of Gastroenterology, Sheba Medical Center, Ramat-Gan 52630, Israel.
Ofer Ben-Bassat, Institute of Gastroenterology, Rabin Medical Center, Petach-Tikva 49100, Israel.
Charles N Bernstein, IBD Clinical and Research Centre, University of Manitoba, Winnipeg, MB R3E3P4, Canada.
Eran Israeli, Institute of Gastroenterology and Liver Diseases, Hadassah-Hebrew University Medical Center, Jerusalem 91120, Israel.
References
- 1.Van Assche G, Dignass A, Bokemeyer B, Danese S, Gionchetti P, Moser G, Beaugerie L, Gomollón F, Häuser W, Herrlinger K, Oldenburg B, Panes J, Portela F, Rogler G, Stein J, Tilg H, Travis S, Lindsay JO European Crohn's and Colitis Organisation. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: Special situations. J Crohns Colitis. 2013;7:1–33. doi: 10.1016/j.crohns.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Van Assche G, Dignass A, Reinisch W, van der Woude CJ, Sturm A, De Vos M, Guslandi M, Oldenburg B, Dotan I, Marteau P, Ardizzone A, Baumgart DC, D'Haens G, Gionchetti P, Portela F, Vucelic B, Söderholm J, Escher J, Koletzko S, Kolho KL, Lukas M, Mottet C, Tilg H, Vermeire S, Carbonnel F, Cole A, Novacek G, Reinshagen M, Tsianos E, Herrlinger K, Oldenburg B, Bouhnik Y, Kiesslich R, Stange E, Travis S, Lindsay J European Crohn's and Colitis Organisation (ECCO) The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Special situations. J Crohns Colitis. 2010;4:63–101. doi: 10.1016/j.crohns.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Keeton RL, Mikocka-Walus A, Andrews JM. Concerns and worries in people living with inflammatory bowel disease (IBD): A mixed methods study. J Psychosom Res. 2015;78:573–578. doi: 10.1016/j.jpsychores.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Becker HM, Grigat D, Ghosh S, Kaplan GG, Dieleman L, Wine E, Fedorak RN, Fernandes A, Panaccione R, Barkema HW. Living with inflammatory bowel disease: A Crohn's and Colitis Canada survey. Can J Gastroenterol Hepatol. 2015;29:77–84. doi: 10.1155/2015/815820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burkhalter H, Stucki-Thür P, David B, Lorenz S, Biotti B, Rogler G, Pittet V. Assessment of inflammatory bowel disease patient's needs and problems from a nursing perspective. Digestion. 2015;91:128–141. doi: 10.1159/000371654. [DOI] [PubMed] [Google Scholar]
- 6.Wong S, Walker JR, Carr R, Graff LA, Clara I, Promislow S, Rogala L, Miller N, Rawsthorne P, Bernstein CN. The information needs and preferences of persons with longstanding inflammatory bowel disease. Can J Gastroenterol. 2012;26:525–531. doi: 10.1155/2012/735386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernstein KI, Promislow S, Carr R, Rawsthorne P, Walker JR, Bernstein CN. Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:590–598. doi: 10.1002/ibd.21363. [DOI] [PubMed] [Google Scholar]
- 8.Catalán-Serra I, Huguet-Malavés JM, Mínguez M, Torrella E, Paredes JM, Vázquez N, Ramírez JJ, Calvo F, Nos P, Gutiérrez A, Palau A, Cortés J, Ramón-Monllor P, Hinojosa J. Information resources used by patients with inflammatory bowel disease: Satisfaction, expectations and information gaps. Gastroenterol Hepatol. 2015;38:355–363. doi: 10.1016/j.gastrohep.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Pittet V, Vaucher C, Maillard MH, Girardin M, de Saussure P, Burnand B, Rogler G, Michetti P. Information Needs and Concerns of Patients with Inflammatory Bowel Disease: What Can We Learn from Participants in a Bilingual Clinical Cohort? PLoS One. 2016;11:e0150620. doi: 10.1371/journal.pone.0150620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Promislow S, Walker JR, Taheri M, Bernstein CN. How well does the Internet answer patients' questions about inflammatory bowel disease? Can J Gastroenterol. 2010;24:671–677. doi: 10.1155/2010/957264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah SL, Siegel CA. Increasing Patient Activation Could Improve Outcomes for Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:2975–2978. doi: 10.1097/MIB.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 12.Siegel CA. Shared decision making in inflammatory bowel disease: helping patients understand the tradeoffs between treatment options. Gut. 2012;61:459–465. doi: 10.1136/gutjnl-2011-300988. [DOI] [PubMed] [Google Scholar]
- 13.Holmes-Rovner M. International Patient Decision Aid Standards (IPDAS): Beyond decision aids to usual design of patient education materials. Health Expect. 2007;10:103–107. doi: 10.1111/j.1369-7625.2007.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clara I, Lix LM, Walker JR, Graff LA, Miller N, Rogala L, Rawsthorne P, Bernstein CN. The Manitoba IBD Index: Evidence for a new and simple indicator of IBD activity. Am J Gastroenterol. 2009;104:1754–1763. doi: 10.1038/ajg.2009.197. [DOI] [PubMed] [Google Scholar]
- 15.Kim JO, Mueller CW. Introduction to Factor Analysis: What It Is and How to Do It. Los Angeles: SAGE Publications Inc, 1979. [Google Scholar]
- 16.Hwang JM, Varma MG. Surgery for inflammatory bowel disease. World J Gastroenterol. 2008;14:2678–2690. doi: 10.3748/wjg.14.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin A, Leone L, Castagliuolo I, Di Mario F, Naccarato R. What do patients want to know about their inflammatory bowel disease? Ital J Gastroenterol. 1992;24:477–480. [PubMed] [Google Scholar]
- 18.Schölmerich J, Sedlak P, Hoppe-Seyler P, Gerok W. The information needs and fears of patients with inflammatory bowel disease. Hepatogastroenterology. 1987;34:182–185. [PubMed] [Google Scholar]
- 19.Probert CS, Mayberry JF. Inflammatory bowel disease: Patients' expectations in the 1990s. J R Soc Med. 1991;84:131–132. doi: 10.1177/014107689108400305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Sullivan MA, Mahmud N, Kelleher DP, Lovett E, O'Morain CA. Patient knowledge and educational needs in irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2000;12:39–43. doi: 10.1097/00042737-200012010-00008. [DOI] [PubMed] [Google Scholar]
- 21.Casellas F, Fontanet G, Borruel N, Malagelada JR. The opinion of patients with inflammatory bowel disease on healthcare received. Rev Esp Enferm Dig. 2004;96:174–184. doi: 10.4321/s1130-01082004000300003. [DOI] [PubMed] [Google Scholar]
- 22.Verma S, Tsai HH, Giaffer MH. Does better disease-related education improve quality of life? A survey of IBD patients. Dig Dis Sci. 2001;46:865–869. doi: 10.1023/a:1010725106411. [DOI] [PubMed] [Google Scholar]
- 23.Boonen A, Dagnelie PC, Feleus A, Hesselink MA, Muris JW, Stockbrügger RW, Russel MG. The impact of inflammatory bowel disease on labor force participation: Results of a population sampled case-control study. Inflamm Bowel Dis. 2002;8:382–389. doi: 10.1097/00054725-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Mandel MD, Bálint A, Lovász BD, Gulácsi L, Strbák B, Golovics PA, Farkas K, Kürti Z, Szilágyi BK, Mohás A, Molnár T, Lakatos PL. Work disability and productivity loss in patients with inflammatory bowel diseases in Hungary in the era of biologics. Eur J Health Econ. 2014;15 Suppl 1:S121–S128. doi: 10.1007/s10198-014-0603-7. [DOI] [PubMed] [Google Scholar]