Short abstract
Background
Qatar is located on the north-eastern coast of the Arabian Peninsula. Qatari natives account for less than 15% of the population while the largest migrant group comprising 60% derives from South Asia. Despite projections that stroke burden in Qatar will increase with population ageing, epidemiological studies focusing on stroke in Qatar are relatively scarce.
Method
We reviewed the available epidemiological publications relating to Qatar. In addition, we have added to this knowledge by incorporating Qatari data from the on-going Bio-Repository of DNA in Stroke, an independent multinational database of stroke patients.
Results
Qatar has low reported incidence and mortality rates of 58 and 9.17 per 100,000 per year, respectively, which may be explained by its middle-aged migrant worker majority population. Correspondingly, South Asian migrants in Qatar suffered younger strokes than Qatari natives (48.7 vs 63.4 years, P < 0.001). Among the most common risk factors identified in stroke patients were hypertension (77.9%), diabetes (43.8%) and hypercholesterolemia (28.5%). Ischaemic stroke was the most frequent subtype amongst migrant South Asians (71.1%). The majority of stroke cases had computed tomography and/or magnetic resonance imaging scans, but only 11.1% of ischaemic strokes were thrombolysed. Qataris on one-year follow up were more often found to have died (6.5% vs 0.3%) and had further stroke/transient ischaemic attack events (17.4% vs 6.4%, P = 0.009) compared to South Asians.
Conclusion
The burden of stroke is increasing in Qatar, and considerable disparities are observed between the native and migrant populations which likely will require different approaches to management by its healthcare system.
Keywords: Cardiology, cardiology, epidemiology, etiology, Qatar, review, stroke
Introduction
Stroke remains the second leading cause of mortality and a major cause of disability across the globe, with 6.7 million deaths in 2012 being attributed to stroke alongside 33 million stroke survivors, many of whom are left with long-term disability.1 Furthermore, in the midst of an ageing world population coupled to rapid socioeconomic development, particularly in low- to middle-income countries, global stroke burden is projected to increase for decades to come.2–5 Stroke deaths in low- and middle-income countries accounted for as much as 87% of total stroke mortality of all ages in 2005.6 Despite this, 90% of the population-attributable risk for worldwide stroke is accounted for by 10 conventional risk factors which consist of hypertension, obesity, smoking, alcohol consumption, diabetes, dyslipidaemia, cardiac causes, physical inactivity, poor diet and psychosocial factors,7 implying that stroke is likely preventable in the majority of cases.
The burden of stroke and other non-communicable diseases is projected to rise in Qatar.8 Qatar’s economy is driven heavily by carbon-based resources, namely petroleum and natural gas which, combined with its relatively small population, generates a substantial gross domestic product per capita. The appeal of Qatar’s growing economy and job prospects have attracted a large influx of migrant workers, increasing Qatar’s migrant population by at least 6% annually between 2000 and 2017.9 These migrants have come primarily from the Indian subcontinent, such that expatriate workers now make up the majority of Qatar’s population, heavily outnumbering native Qatari citizens.10 Although no official government data have been published, it has been estimated that Qatari nationals make up less than 15% of its total population.11 Consequently, Qatar’s population is relatively young and predominantly male. Despite Qatar’s assignment by the UN as a high-income country, it is still recognised as a developing country due to its majority migrant population, and the fact that most of its wealth is concentrated with the minority Qataris.12 As such, it may well be that Qatar’s native residents are experiencing the latter stages of socioeconomic development, whilst its expatriate population, coming from low- and middle-income countries into a high-income country, receives environmental exposure akin to inhabitants of countries at earlier stages of the wealth transition.
Being one of the wealthiest nations in the world, Qatar has undergone a considerable shift in socioeconomic status over recent decades with increased urbanization, accompanied by lifestyle changes such as lack of physical activity and the adoption of western calorie- and fat-rich diets.8,13,14 In addition to a rapidly ageing population, these conditions have promoted the spread of cardiovascular disease burden, including stroke amongst Qataris. Notwithstanding this increase, there has been a paucity of data with few studies reporting on stroke incidence and prevalence in Qatar. Qatar has one main hospital, Hamad General Hospital (HGH), which is the only tertiary referral government hospital that admits patients with acute stroke cases which are eligible for thrombosis. Out of 899 stroke admissions in Qatar in 2014, 81.5% were admitted in HGH.11
In order to tackle the growing problem of stroke in developing countries, a better understanding of its existence is required. In this paper, we will review stroke in Qatar making reference to published epidemiological data regarding the dynamics of Qatar’s stroke burden. We will include native Qatari and migrant South Asian data (1188 cases, age range 16–89 years) from the ongoing, multinational Bio-Repository of DNA in Stroke (BRAINS)15,16 where relevant, in order to give an up-to-date representation of stroke in Qatar.
For this review, all publications on stroke in Qatar were identified and included in any language. Key search terms were kept as broad as possible: ‘stroke’ with and without ‘ischaemic’, ‘haemorrhagic’ along with AND as a Boolean operator for the term ‘Qatar’. We also reviewed publications on stroke which covered the Middle East but excluded those which did not provide any information on Qatar.
Incidence
Despite the increasing burden of stroke in Qatar, a number of studies have demonstrated a particularly low incidence of stroke in the region. One such study was a retrospective analysis of first-ever stroke cases admitted in 1997 by Hamad et al.,17 which was based at HGH. A total of 217 stroke patients were identified, generating a crude annual incidence rate for first-ever stroke of 41 per 100,000 per year (95% CI: 30.2–52.4) which rose to 58 per 100,000 per year (95% CI: 43.1–73.8) after standardization to the world population. In the Global Burden of Diseases, Injuries and Risk Factors 2010 (GBD 2010) study, a similarly low age-standardized incidence rate for ischaemic stroke in Qatar was estimated at 51.88 per 100,000 person-years in 2010, having risen from 46.52 per 100,000 person-years in 1990.11,18,19
Bener et al.20 performed a cohort study over a five-year period between 1999 and 2003, in which stroke patients were recruited at HGH. The average annual incidence calculated from this study was found to be even less at 11.7 per 100,000 of the population. From the handful of studies reporting data, incidence rates of stroke in Middle Eastern countries appear to be relatively low, generally ranging between 11.7 and 63 per 100,000,21,22 which is likely reflective of the relatively young age of the populations within this region. This becomes more apparent with subjects over the age of 45 years in Qatar, in whom Hamad et al.17 found incidence rates of first-ever stroke to be 238 per 100,000.17 Likewise, the crude annual incidence of 41 per 100,000 per year reported by Hamad et al.17 rose to 123.7 (95% CI: 100.6–127.7) upon age standardization, making it the highest in the Middle East and North Africa region.21 These are closer to the range of reported incidence rates in Western countries which tend to be considerably higher, e.g. in Europe incidence rates range from 210 to 600 per 100,000 per year.23
Mortality
Qatar appears to have similarly low rates of mortality from stroke. The GBD 2010 study reported falling age-standardized mortality rates for ischaemic stroke from 31.27 per 100,000 person-years in 1990 to 9.17 in 2010, which, just as for reported incidence rates, was the lowest in the observed range.11,18,19 Hamad et al.17 found the rate of stroke mortality up to 30 days after admission to be 16% at HGH in 1997, with a greater contribution from intracerebral haemorrhage to mortality (31%) than ischaemic stroke (12%). Khan et al.24 reported in their later prospective observational study, recruiting first-ever stroke patients at the same hospital between 2004 and 2005, that total case fatality was reduced at a rate of 9.3%, again with a larger contribution risk from haemorrhagic mortality than ischaemic (30.2% vs 4.1%). In-hospital mortality from stroke in neighbouring Saudi Arabia has been reported to be similar at 10.0%25 with reports of a 30-day stroke case fatality range of 10–17.3% in other Arab nations.22 Low mortality rates have also been attributed to a young Qatar population together with improvements in stroke management and care.26 Although the findings of low incidence and mortality of stroke in Qatar suggest a low burden in the country, it is expected that as the population ages stroke will become a more prominent issue.
Demographics
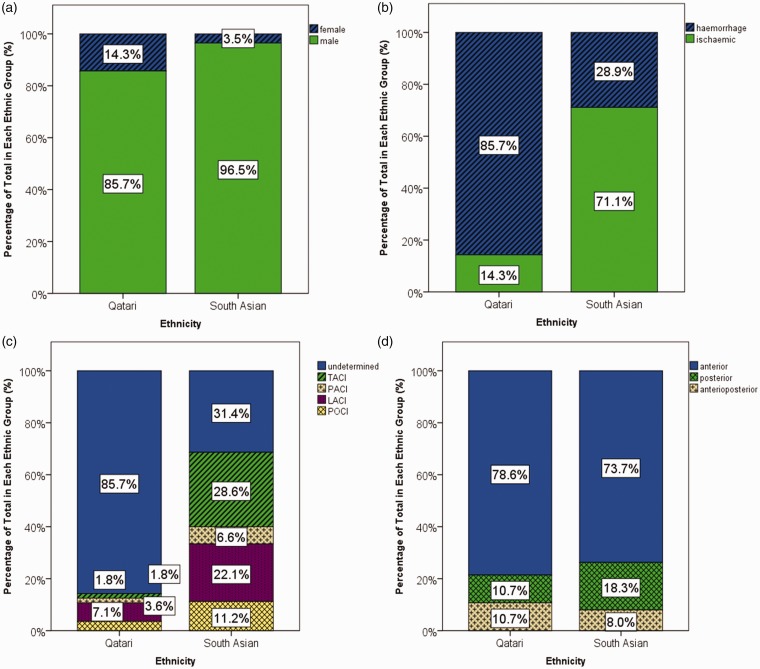
Observing total stroke in Qatari natives and South Asian migrants in BRAINS (a prospective international stroke repository), we immediately notice the predominantly male distribution (96% males vs 4% females) that has been reported, albeit to a lesser degree in previous studies. Khan et al.24 reported that 73% of stroke patients in their cohort were males and 27% were females. Qataris (85.7% males vs 14.3 females) and South Asians living in Qatar (96.5% males vs 3.5% females) both had a preponderance of male strokes in BRAINS (Figure 1(a)), although South Asians had a significantly higher proportion of male cases (χ2(1) = 15.91, P < 0.001). Likewise, the majority of the BRAINS study population consisted of South Asian migrants (95% South Asians vs 5% Qataris) which presumably accounts for the male bias, whilst Ibrahim et al.11 noted that 81% of stroke patients in their registry were non-Qatari. Hamad et al.17 found their patient cohort to have a mean age of stroke onset of 57 years for males and 60 years in females. We found a relatively young average age of onset of stroke (49.4 ± 11.0 years) with South Asian stroke cases (48.7 ± 10.4 years) having significantly younger strokes than Qatari nationals (63.4 ± 13.1 years, t (58.51) = 8.31, P < 0.001). Deleu et al.27 reported a similar finding in a retrospective review of non-cardioembolic stroke patients admitted to HGH (67.3 vs 55.5 years, P = 0.0001). Performing a time-trend analysis using ANOVA and Hochberg GT2 post hoc tests, we found a significantly lower average age of stroke onset in those cases occurring in 2016 than those in 2013, 2014, 2015 and 2017 (F[7, 1175] = 3.688, P = 0.001). This may be due to lower than expected recruitment of patients in 2016.
Figure 1.
Percentage proportions of total Qatari and South Asian strokes with stacks representing (a) gender groups, (b) ischaemic and haemorrhagic stroke, (c) OCSP ischaemic subtypes and (d) anatomical positioning of stroke event.
The particularly young age of onset of stroke corresponds to the young South Asian expatriate population who make up the majority of Qatar’s population. This unique population of migrants has been subject to a myriad of exposures relating to the migration from their country of origin to the Middle East. It is probable that in transition, a combination of socioeconomic, cultural and genetic factors influence the early presentation of stroke in this population. Additionally, a lack of awareness of stroke may also contribute to non-compliance with preventive measures for stroke, increasing the prevalence of risk factors that go untreated. A cross-sectional community survey of primary health care centres in the Gulf Cooperation Council countries found that a majority of patients were unfamiliar with the term ‘stroke’, and that those with the least knowledge of stroke were those at the highest risk of having a stroke.28,29 Pathophysiological mechanisms relating to pro-inflammatory mediators and endothelial dysfunction have also been implicated in the pathogenesis of early onset stroke in Qatar via their association with cardiovascular risk factors.30–32
Conventional risk factors
The prevalence of stroke risk factors has an important role to play in the observed burden of stroke in Qatar. Hamad et al.17 identified hypertension as being the most common risk factor among stroke patients (63%), which was significantly more prevalent among expatriate than native Qatari men (77% vs 48%, P = 0.02). Diabetes (42%) was the next most prevalent risk factor among patients and was significantly more common in native Qatari women than their expatriate counterparts (52% vs 18%, P = 0.02). Ischaemic heart disease and atrial fibrillation followed with prevalence of 17% and 4.5%, respectively. Khan et al.24 similarly found the three most prevalent risk factors to be hypertension (74%), diabetes (67%) and dyslipidaemia (53%). Risk factor profiles were largely comparable between natives and expatriates except for hypercholesterolemia which was more common in native Qatari patients. In Khan’s33 observational study focusing on prevalent risk factors involved in young stroke between the ages of 15 and 45 years in Qatar, the top five risk factors included hypertension (40%), diabetes mellitus (32.5%), hypercholesterolemia (27.5%), smoking (27.5%) and alcohol consumption (22.5%). Deleu et al.27 found that hypertension (69%) was again the most common risk factor among stroke patients, followed by dyslipidemia (57%), diabetes (51%), obesity (30%), a previous history of stroke (24%) and coronary artery disease (23%). The combination of hypertension, diabetes and dyslipidemia was most common in the third of patients with three concomitant risk factors. Diabetes was significantly more prevalent among women than men (76% vs 51%, P = 0.0001) and in native Qatari patients than expatriates (67% vs 49%, P = 0.003), whilst hypertension, smoking and alcohol consumption were found to be more prevalent in males with ischaemic stroke than in females in Khan’s34 post hoc analysis.
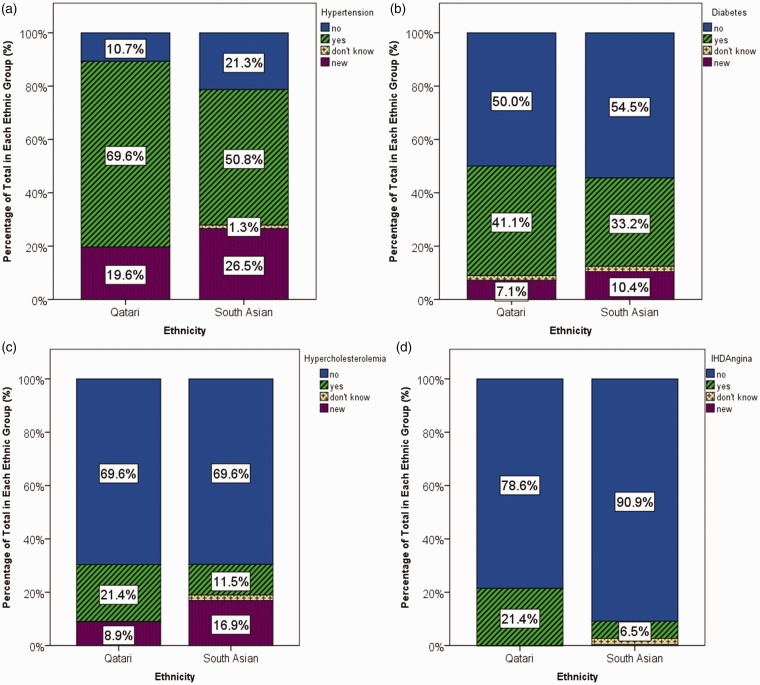
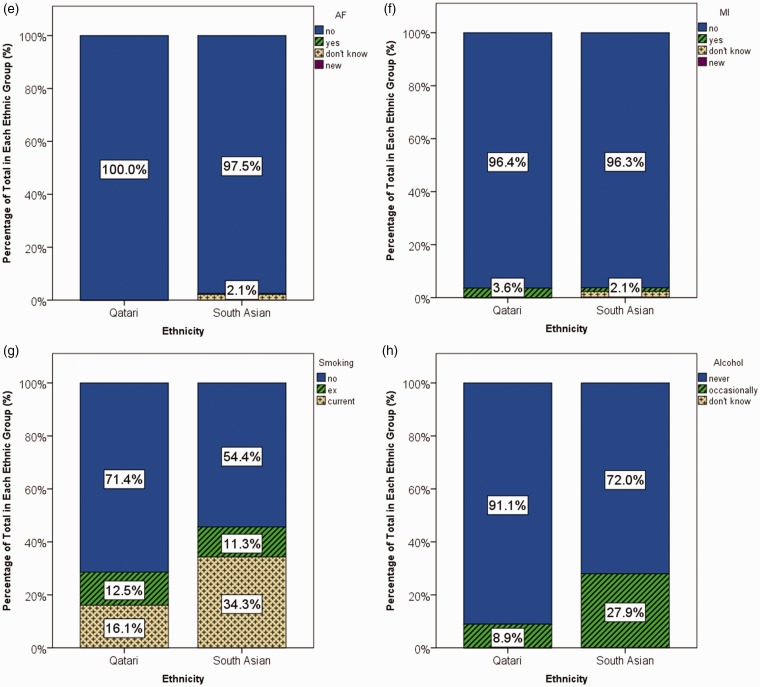
The aforementioned study findings are largely in concordance with the major stroke risk factors identified in BRAINS (Figure 2(a) to (h)). Hypertension was confirmed in 51.7% of stroke cases overall with a further 26.2% receiving a new diagnosis on admission. More Qataris than South Asians were confirmed to have hypertension from previous diagnosis (69.6% vs 50.8%), whilst South Asians had more new diagnoses (26.5% vs 19.6%, χ2(3) = 8.23, P = 0.041). A total of 43.8% of cases were identified with diabetes, and 23.5% of these being new diagnoses. Although more comparable with that of South Asians, Qataris also had higher proportions of cases with previously diagnosed diabetes (41.1% vs 33.2%) and fewer cases with newly diagnosed diabetes (7.1% vs 10.4%, χ2(3) = 1.76, P = 0.62). About 12.0% of patients overall were confirmed to have hypercholesterolemia with an additional 16.5% being newly diagnosed. Likewise, there was a tendency towards a higher prevalence of previously diagnosed hypercholesterolemia among Qatari cases (21.4% vs 11.5%) and fewer new diagnoses (8.9% vs 16.9%)), although this difference was not significant (χ2(3) = 7.59, P = 0.55). The average body mass index (BMI) among combined stroke cases was 26.6 ± 4.0 kg/m2. Among the cases, Qatari stroke patients were found to be significantly heavier than South Asian patients on average (28.6 ± 5.4 vs 26.5 ± 3.9 kg/m2, Mann–Whitney U = 23764.50, P = 0.003). Current and ex-smokers constituted 33.4 and 11.4% of total stroke patients, respectively, whilst 27% of stroke cases reported occasional drinking. Significantly, more South Asians than native Qataris were current smokers (34.3% vs 16.1%, χ2(2) = 8.18, P = 0.017) and reported occasional drinking (27.9% vs 8.9%, χ2(2) = 9.80, P = 0.007). Ischaemic heart disease/angina and myocardial infarction had prevalence among combined cases of 7.5% and 1.7%, respectively, although ischaemic heart disease/angina was more prevalent among Qatari cases (21.4% vs 6.5%, χ2(3) = 19.09, P < 0.001) whilst the prevalence of myocardial infarction did not differ significantly between South Asians and Qataris (1.4% vs 3.6%, χ2(3) = 2.92, P = 0.40). Atrial fibrillation was present in 0.3% of total cases but only in South Asians.
Figure 2.
Percentage proportions of total Qatari and South Asian strokes with stacks representing negative (no), positive (yes), undetermined (don’t know) and newly diagnosed (new) patient status of (a) hypertension, (b) diabetes, (c) hypercholesterolemia, (d) ischaemic heart disease/angina, (e) atrial fibrillation, (f) myocardial infarction, (g) smoking and (h) alcohol consumption.
As expected, hypertension was the most prevalent stroke risk factor.7,35,36 Evidently, Qatar’s stroke population also has a particularly high prevalence of diabetes and obesity, especially among the natives of Middle Eastern countries, which has been associated with the occurrence of hypertension in a cross-sectional study of native Qataris.37–39 Furthermore, case–control studies in Qatar have found that histories of diabetes, hypertension and high cholesterol increased risks of stroke (ischaemic or haemorrhagic infarct) relative to controls.40,41 In multivariate analyses adjusting for age, gender and smoking, these three major risk factors generated odds ratios (95% confidence intervals) of 5.12 (3.11–8.60), 3.59 (2.29–5.66) and 2.45 (1.27–4.83), respectively.
The prevalence of major stroke risk factors in Qatar, although comparable with other Middle Eastern and North African countries, is generally higher than that among high- and middle income countries with reported prevalences of 42.7 and 44.3% for hypertension, 7.9 and 7.5% for diabetes, 13.5 and 21.3% for current smoking and 25.6 and 18.7% for obesity, respectively.7,42,43 Prevalence of hypercholesterolemia and current alcohol use appears to be higher in high-income countries, whilst those rates in middle-income countries are comparable to those in Qatar.
Environmental factors
Alongside the conventional vascular risk factors are environmental factors that are likely contributing to stroke in Qatar.23,44 The westernization and urbanization that has been taking place in Qatar, accompanied by an increase in socioeconomic status, may explain the rising prevalence of sedentary lifestyles and poor nutrition, particularly among young native Qataris.45,46 The increasing level of air pollution in Qatar is another factor which relates to the economic growth of the country, yet bears close association with the rising burden of cardiovascular disease including stroke, possibly through interaction with hemostatic factors.47–53 Communicable diseases, although declining, are still notable issues in the countries of origin of many Qatari expatriates, and thus, the large migrant influx is thought to contribute in part to the increase in prevalence of infectious diseases in Qatar.18,54,55 There is evidence that infectious disease may be associated with the incidence of stroke through chronic inflammation and its potential interaction with atherosclerosis, albeit inconclusive.56–58 Consanguineous marriage, which remains relatively common amongst native Qataris as is widespread in other Arab countries, has also been associated with the prevalence of major risk factors for stroke such as hypertension and diabetes.59–62
Ethnic disparities
In one case–control study in Qatar, the strongest risk factor identified for diabetes was Qatari nationality, yielding an odds ratio (95% confidence intervals) of 5.5 (3.5–8.6) after adjustment for all other measured factors.62 Among the findings reported by Deleu et al.27 was that Arab stroke patients tended to be older than South Asian patients (65 years vs 53 years, P = 0.0001) despite having a higher average BMI (33 vs 28 kg/m2, P = 0.002), more often presenting with diabetes (64% vs 46%, P = 0.004) and a greater number of concomitant risk factors (3.0 vs 2.6, P = 0.005).27 This is corroborated by our observation of stroke of later onset even with a greater prevalence of most major risk factors among native Qataris than South Asians within BRAINS, as has similarly been reported by Akhtar et al.39 Ventricular wall motion abnormalities and carotid artery stenotic lesions were also significantly more prevalent among Arab patients. Despite Khan’s et al.24,33 report of largely similar risk factor profiles between ethnic groups, they noted significantly more posterior circulation stroke in Qataris and young (15–45 years) patients when compared with non-Qataris and older (>45 years) patients, respectively.24,33
Some ethnic disparities, particularly age and gender distributions, may be explained simply by the demographic profile in Qatar (predominantly male migrant work force and consequent variation in socioeconomic status). However, disparities that pertain more directly to the pathophysiology of stroke, such as the prevalence of risk factors and physiological and anatomical abnormalities, may have deeper origins. Findings from Deleu et al.,27 which suggest that South Asians may be suffering from stroke at earlier ages than would be expected from observance of their risk factor profiles relative to Qatari natives and expatriates from other Arab nations combined, are in concordance with other studies demonstrating a similar South Asian predisposition for stroke63,64 and may have a number of possible explanations.
Psychosocial factors
The lower socioeconomic status among migrant populations may be more conducive to psychosocial factors such as stress and depression, which have also been identified by O’Donnell et al.7 as being one of 10 risk factors with major contributions to global stroke. Regularly facing extreme hardships relating to harsh working conditions, potential exploitation and abuse in addition to the needs of family members in their home country, South Asians are often vulnerable to mental health illness,65 which can then lead to subsequent stroke events. As such, psychosocial elements may conceivably have a detrimental impact on South Asian stroke in Qatar.
Genetic and physiological factors
Inherent genetic factors may also have a role to play in any South Asian predisposition to stroke,66 potentially influencing the aetiology and age of stroke onset, impact of conventional risk factors and distribution of stroke subtypes and outcomes.67–71 Numerous genetic polymorphisms have been implicated in South Asian ischaemic stroke, ranging from those involved in the renin–angiotensin–aldosterone system and the metabolism of lipids to those central to inflammation, coagulation and endothelial dysfunction.66,72 Contrastingly, we identified no published studies investigating genetic associations with ischaemic stroke in Qatari populations.
One physical manifestation of the South Asian predisposition towards stroke is the finding of increased arterial stiffness in comparison to white Europeans.73 This is reflective of mean arterial pressure having a more detrimental impact on the South Asian vascular system, which may also explain the more adverse associations found between various blood pressure parameters and incident stroke in South Asians compared to Europeans.69 The inflammatory marker, C-reactive protein (CRP), has also been reported to associate strongly with measures of central obesity in South Asians, which persisted after adjustment for BMI or fat percentage.74 Thus, CRP, which was also found to associate positively with insulin and triglyceride and inversely with HDL-cholesterol, could be a key mediator in the excess risk of stroke conferred by obesity in South Asians.
Fetal origins
One theory which has accrued support since first proposed provides a possible explanation for increased susceptibility to cardiovascular disease in South Asian migrant populations such as those residing in Qatar. Barker75,76 in his ‘fetal origins’ hypothesis suggests that prenatal undernutrition during critical periods of fetal development predispose towards increased cardiovascular disease risk in later life. A combination of low birth weight from poor nutrition in utero, followed by rapid weight gain in childhood from relative overnutrition, subsequently leads to a pronounced excess in adult cardiovascular risk.77 Even though South Asian expatriates in Qatar may not experience relative overnutrition until they migrate in adulthood, an exposure to undernutrition in early life may predispose South Asian migrants towards stroke in adulthood.
Stroke subtypes
Hamad et al.17 found most stroke cases to be of ischaemic origin (80%), with the remaining haemorrhagic cases consisting of intracerebral (19%) and subarachnoid (1%) haemorrhage, which has been similarly reported by Khan et al.24 Proportions of ischaemic stroke were largely comparable to those reported in other developed, high-income countries (73–90% between 2000 and 2008), although haemorrhagic stroke proportions were more akin to those found in low to middle income countries.78 Khan et al.24 also found no major variations in proportions of the Oxfordshire Community Stroke Project (OCSP) ischaemic subtypes, although lacunar infarcts (LACI, 30.4%) were most commonly followed by total anterior circulation infarcts (TACI, 26.7%), partial anterior circulation infarcts (PACI, 24.4%) and posterior circulation infarcts (POCI, 18.4%).24,79 Among Deleu et al.’s27 recruitment of non-cardioembolic ischaemic strokes, 78% of patients had strokes localised to anterior circulation, 17% involved posterior circulation and 5% had anterioposterior stroke. Moreover, 68% of cases were identified as lacunar infarction, whilst 10% of patients had large vessel events. However, in a later study involving several Arabian gulf countries, large-artery atherosclerosis (38.1%) was identified to be the most common form of ischaemic stroke, followed closely by lacunar stroke (34.7%), with much less observed cardioembolic stroke (13.5%).80 The large proportion of lacunar strokes was considerably higher in comparison to those observed in European population-based studies (approximately 7–21%)81 and has been attributed to probable diabetes-related arteriopathy. Conversely, in a study in which only posterior circulation strokes were recruited, large artery disease (47%) was the most common of the ischaemic subtypes, with only 17% of strokes being due to small vessel disease,82 whilst in a later study, Akhtar et al.39 found the majority of strokes to be borne from small vessel disease both in Middle Eastern (63.8%) and South East Asian patients (67.3%) in Qatar. As for the sites of intracerebral haemorrhage, Khan et al.24 reported that lobar haemorrhages were most frequent (38.3%) whilst cerebellar haemorrhages were least frequent (8.6%). Intracerebral haemorrhage was more frequent among older patients whereas subarachnoid haemorrhage had increased prevalence among young patients.
Of the major stroke-type distribution in BRAINS, 68.4% of combined strokes were identified as being of ischaemic origin whilst 31.6% were haemorrhagic. Qatari cases were predominantly haemorrhagic but likely because of the small numbers, whereas South Asian cases consisted mostly of ischaemic strokes (71.1%, χ2(1) = 79.77, P < 0.001; Figure 1(b)). The major stroke event occurred anteriorly in 74%, posteriorly in 18% and was of anterioposterior origin in 8% of total cases, and these did not differ significantly between native Qataris and South Asian migrants (χ2(2) = 2.39, P = 0.30; Figure 1(d)). Among the overall distribution of OCSP ischaemic subtypes, 27.4% were TACI, 6.4% were PACI, 21.4% were LACI and 10.9% were POCI, with the remaining 34% being undetermined. South Asians had greater proportions of all four OCSP ischaemic subtypes and less undetermined stroke than native Qataris (Figure 1(c); χ2(4) = 70.86, P < 0.001). The sites of bleeding in combined cases of haemorrhage were identified as the basal ganglia (10.9%), cortex (15.7%), cerebellum (1.4%), brainstem (0.4%), internal capsule (0.3%) and thalamus (2.5%). Proportions of basal ganglia, cortical, cerebellar and thalamic haemorrhage were all greater among Qatari cases, although no brainstem or internal capsule strokes were identified in this group (χ2(6) = 95.25, P < 0.001). About 0.2% of strokes was identified as subarachnoid haemorrhages and was exclusive to South Asian patients.
Stroke care and outcome
BRAINS data demonstrate that brain imaging on admission is routinely performed in stroke cases with almost all patients receiving a CT scan (99.2%) and nearly three-quarters of patients having an MRI (72.5%). All Qataris and the vast majority of South Asian patients (100.0% and 99.2%, respectively) received a CT scan, whereas more South Asians had an MRI than native Qataris (73.7% vs 50.0%, χ2(1) = 14.98, P < 0.001). However, Khan et al.24 reported that although 81.6% of stroke patients in their cohort had a CT scan within 24 h of admission, only 12% had a confirmed diagnosis of stroke. Despite increased efforts to improve rates of thrombolysis, BRAINS data also revealed that only 8.1% of incident ischaemic stroke cases received thrombolysis and despite the existence of a trend towards higher rates among South Asians, the difference was not significant (8.4% vs 1.8%, χ2(1) = 3.14, P = 0.08). Between 2000 and 2008, reported rates of thrombolysis of ischaemic stroke were generally low and variable across North America (1.3–5.1%) and Europe (2.9–16%), although rates among hyperacute ischaemic stroke cases (admitted to hospital within three hours of stroke onset) reached as high as 58%.83,84 Correspondingly, Khan et al.24 reported that only 18% of patients were admitted to hospital within three hours of stroke onset, which they attributed to lack of awareness and late recognition of developing stroke symptoms, although much of this may relate to a specialised stroke unit only recently being established in Qatar. Reducing ‘door-to-needle time’ may lead to considerable benefits including higher rates of thrombolysis, fewer complications, shorter length of stay in hospitals and improved prognosis for patients.26
On discharge, 68.2% of patients went home and 28.5% were referred to rehabilitation. Mortality rate was 3.1%. Contrastingly, Khan et al.24,33 have reported up to 77.7% of patients being discharged with neurological deficit, with the majority being referred to stroke rehabilitation services. We identified statistically significant differences in discharge status between ethnic groups with more South Asians discharged to home (68.7% vs 57.1%) and a lower mortality rate amongst patients of this ethnicity in comparison to native Qataris (2.7% vs 10.7%, χ2(3) = 12.29, P = 0.006). Risk factors such as diabetes and atrial fibrillation have also been associated with heightened disability, mortality and recurrence with worse outcomes than those strokes in which these risk factors were absent.85,86 At one-year follow-up, 5.7% were reported to have had a secondary stroke/transient ischaemic attack (TIA), 0.3% suffered from myocardial infarction, 1.8% died and 74.7% had no further events. Of those who were followed up, more Qataris had a further event (17.4% vs 6.4%) and died (6.5% vs 0.3%, χ2(4) = 13.51, P = 0.009) than South Asians.
About 44.4% of total hypertensive cases were taking antihypertensives prior to their stroke event, with Qatari hypertensives more often receiving treatment than their South Asians counterparts (61.5% vs 43.2%, χ2(1) = 4.973, P = 0.03). Of the 40.1% of total patients with hypercholesterolemia taking statins before their stroke event, more Qatari patients with hypercholesterolemia were taking statins than South Asians (50.0% vs 39.2%, χ2(1) = 0.530, P = 0.47). These results along with the finding of consistently higher proportions of newly diagnosed risk factors on admission among South Asian strokes in BRAINS suggest that a lack of awareness, treatment prescription and compliance may be crucial determinants of the excess burden of stroke in this subpopulation.
Lack of prescription, medication compliance and adequate control of risk factors have been reported in Khan et al.’s24 prospective study, where, despite hypertension being the main risk factor for both ischaemic and haemorrhagic stroke, only 38.2 and 41.5% of hypertensives from each stroke type had received antihypertensive medication, respectively. About 61.8% of patients were identified who did not take their prescribed medication which is comparable to estimates of non-compliance to antihypertensive medication in the US of 62%.87 However, compliance rates are known to vary considerably, with non-compliance to diabetic medication ranging from 52 to 93% in the US, and similar variations reported in persistence with lipid-lowering treatment after two years, ranging between 48 and 91% in Europe.88–90 Of those in Qatar receiving treatment for diabetes and hypercholesterolemia, these major risk factors remained uncontrolled in 52.3 and 68.5%, respectively.24 This is comparable to the 66.7 and 66.6% of patients treated with antihypertensive and lipid-lowering medication, respectively, whose risk factors remained uncontrolled in European centres.91 Rates of hypertension control in the US have been reported to be similar, although this has been increasing with time, likely owing to increased administration of combined drug therapy alongside raised awareness and better patient compliance to treatment.92–94
Clinical basis to ethnic disparities
The excess burden in South Asians residing in Qatar does not seem to be explained by differences in the aforementioned stroke management and outcome measures from the BRAINS database, as has been demonstrated in multi-ethnic populations in the UK and US.95,96 Rather, these measures would largely point towards a more favourable stroke profile in South Asians, with the exception of risk factor management before stroke. Although healthcare is easily accessible for native Qataris and expatriates alike, some migrants may refuse to take local medication, preferring to use means of treatment akin to their native culture and may even decide to travel back to their home countries to receive treatment, especially in the case of serious illness.99 Other factors that may contribute to ethnic disparities in stroke burden in Qatar include the existence of language barriers, which may result in delays to treatment due to inability of clinicians to accurately establish symptoms and medical histories.97,98 Additionally, the treatments that are applicable to the native Qataris may not be appropriate for South Asian migrants, given their increased propensity for stroke and other cardiovascular diseases. As such, they may require a more intensive and aggressive treatment regimen than is typically required for native Qataris.
Limitations
The relative understudying of the population of Qatar with regards to stroke is reflected in the paucity of published epidemiological data. As such, our review gives an insight into the dynamics of stroke in Qatar but more and larger population-based studies will be required in order to fully uncover the burden of stroke in the region. Furthermore, given that the study population consists largely of migrant South Asian males, it is important to note that the findings of this review will not be readily applicable to females, the South Asian population as a whole, particularly in comparison to South Asians residing in their country of origin, or other multi-ethnic populations. The results may however be applicable to similar neighbouring countries in the Middle East and other migrant male South Asian populations, especially those who have migrated to other high-income countries under similar circumstances and exposures.
Conclusion
Very little stroke data exist from the Middle East despite this region accounting for around 5% of the entire world’s population.100,101 Qatar is a small but important part of this area and most of the stroke information from the Middle East arise from this Gulf state. In this review, we have incorporated data collected from Qatar from our ongoing international prospective repository, BRAINS and show that there are differences in stroke characteristics in Qataris compared to other populations. The fact that Qatar has a large migrant (mainly South Asian) population enabled us to undertake a unique ethnic comparison and we show significant differences between these two groups. We present, to the best of our knowledge, one of the most comprehensive reviews of stroke in Qatar.
Acknowledgements
We thank the patients and relatives without whom this work could not have been possible.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the Qatar National Research Fund (NPRP 6-068-3-015).
Ethical approval
Not applicable.
Guarantor
Not applicable.
Contributorship
EJ wrote the first draft and undertook the analysis. PS conceived the idea. FY led the recruitment of patients. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
References
- 1.Mendis S, Davis S, Norrving B. Organizational update: the World Health Organization Global Status Report on noncommunicable diseases 2014; one more landmark step in the combat against stroke and vascular disease. Stroke 2015; 46: e121–e122. [DOI] [PubMed] [Google Scholar]
- 2.Beard JR, Officer A, de Carvalho IA, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet 2016; 387: 2145–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Truelsen T, Bonita R. The worldwide burden of stroke: current status and future projections [Chapter 16]. Handb Clin Neurol 2008; 92: 327–336. [DOI] [PubMed] [Google Scholar]
- 4.Feigin VL. Stroke in developing countries: can the epidemic be stopped and outcomes improved? Lancet Neurol 2007; 6: 94–97. [DOI] [PubMed] [Google Scholar]
- 5.Mukherjee D, Patil CG. Epidemiology and the global burden of stroke. World Neurosurg 2011; 76: S85–S90. [DOI] [PubMed] [Google Scholar]
- 6.Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol 2007; 6: 182–187. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016; 388: 761–775. [DOI] [PubMed] [Google Scholar]
- 8.Akala FA, El-Saharty S. Public-health challenges in the Middle East and North Africa. Lancet 2006; 367: 961–964. [DOI] [PubMed] [Google Scholar]
- 9.International Organization for Migration. World migration report 2018. International Organization for Migration, 2017. [Google Scholar]
- 10.Kapiszewski A. United Nations expert group meeting on international migration and development in the Arab region population division Arab versus Asian migrant workers in the GCC countries, 2006. United Nations Secretariat: Department of Economic and Social Affairs.
- 11.Ibrahim F, Deleu D, Akhtar N, et al. Burden of stroke in Qatar. J Stroke Cerebrovasc Dis 2015; 24: 2875–2879. [DOI] [PubMed] [Google Scholar]
- 12.United Nations – Department of Economic U, Affairs – Development Policy S, Division A. World economic situation and prospects, 2018.
- 13.Aje TO, Miller M. Cardiovascular disease: a global problem extending into the developing world. WJC 2009; 1: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reddy KS. Cardiovascular diseases in the developing countries: dimensions, determinants, dynamics and directions for public health action. Public Health Nutr 2002; 5: 231–237. [DOI] [PubMed] [Google Scholar]
- 15.Yadav S, Schanz R, Maheshwari A, et al. Bio-repository of DNA in stroke (BRAINS): a study protocol. BMC Med Genet 2011; 12: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cotlarciuc I, Khan MS, Maheshwari A, et al. Bio-repository of DNA in stroke: a study protocol of three ancestral populations. JRSM Cardiovasc Dis 2012; 1: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamad A, Hamad A, Sokrab TEO, et al. Stroke in Qatar: a one-year, hospital-based study. J Stroke Cerebrovasc Dis 2001; 10: 236–241. [DOI] [PubMed] [Google Scholar]
- 18.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2095–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bennett DA, Krishnamurthi RV, Barker-Collo S, et al. The global burden of ischemic stroke: findings of the GBD 2010 study. Glob Heart 2014; 9: 107–112. [DOI] [PubMed] [Google Scholar]
- 20.Bener A, Kamran S, Elouzi EB, et al. Association between stroke and acute myocardial infarction and its related risk factors: hypertension and diabetes. Anadolu Kardiyol Derg 2006; 6: 24–27. [PubMed] [Google Scholar]
- 21.Tran J, Mirzaei M, Anderson L, et al. The epidemiology of stroke in the Middle East and North Africa. J Neurol Sci 2010; 295: 38–40. [DOI] [PubMed] [Google Scholar]
- 22.Benamer HT, Grosset D. Stroke in Arab countries: a systematic literature review. J Neurol Sci 2009; 284: 18–23. [DOI] [PubMed] [Google Scholar]
- 23.Bejot Y, Benatru I, Rouaud O, et al. Epidemiology of stroke in Europe: geographic and environmental differences. J Neurol Sci 2007; 262: 85–88. [DOI] [PubMed] [Google Scholar]
- 24.Khan FY, Yasin M, Abu-Khattab M, et al. Stroke in Qatar: a first prospective hospital-based study of acute stroke. J Stroke Cerebrovasc Dis 2008; 17: 69–78. [DOI] [PubMed] [Google Scholar]
- 25.El Sayed MM, Adeuja AO, El-Nahrawy E, et al. Characteristics of stroke in Hofuf, Saudi Arabia. Ann Saudi Med 1999; 19: 27–31. [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim F, Akhtar N, Salam A, et al. Stroke thrombolysis protocol shortens “door-to-needle time” and improves outcomes–experience at a tertiary care center in Qatar. J Stroke Cerebrovasc Dis 2016; 25: 2043–2046. [DOI] [PubMed] [Google Scholar]
- 27.Deleu D, Hamad AA, Kamram S, et al. Ethnic variations in risk factor profile, pattern and recurrence of non-cardioembolic ischemic stroke. Arch Med Res 2006; 37: 655–662. [DOI] [PubMed] [Google Scholar]
- 28.Kamran S, Bener AB, Deleu D, et al. The level of awareness of stroke risk factors and symptoms in the Gulf Cooperation Council Countries: Gulf Cooperation Council Stroke Awareness Study. Neuroepidemiology 2007; 29: 235–242. [DOI] [PubMed] [Google Scholar]
- 29.Diab MI, Johnson BJ, Hudson S. Adherence to clinical guidelines in management of diabetes and prevention of cardiovascular disease in Qatar. Int J Clin Pharm 2013; 35: 101–112. [DOI] [PubMed] [Google Scholar]
- 30.Agouni A, Parray AS, Akhtar N, et al. There is selective increase in pro-thrombotic circulating extracellular vesicles in acute ischemic stroke and transient ischemic attack: a study of patients from the Middle East and Southeast Asia. Front Neurol 2019; 10: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cahill PA, Redmond EM. Vascular endothelium – gatekeeper of vessel health. Atherosclerosis 2016; 248: 97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Gamal H, Parray AS, Mir FA, et al. Circulating microparticles as biomarkers of stroke: a focus on the value of endothelial- and platelet-derived microparticles. J Cell Physiol 2019; 234(10): 16739–16754. [DOI] [PubMed] [Google Scholar]
- 33.Khan FY. Risk factors of young ischemic stroke in Qatar. Clin Neurol Neurosurg 2007; 109: 770–773. [DOI] [PubMed] [Google Scholar]
- 34.Khan F, Ibrahim A. Gender differences in risk factors, clinical presentation, and outcome of stroke: a secondary analysis of previous hospital-based study in Qatar. Libyan J Med Sci 2018; 2: 51. [Google Scholar]
- 35.Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol 2016; 15: 913–924. [DOI] [PubMed] [Google Scholar]
- 36.Lawes CM, Hoorn S, Vander and Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371: 1513–1518. [DOI] [PubMed] [Google Scholar]
- 37.Bener A, Al-Suwaidi J, Al-Jaber K, et al. Epidemiology of hypertension and its associated risk factors in the Qatari population. J Hum Hypertens 2004; 18: 529–530. [DOI] [PubMed] [Google Scholar]
- 38.Butler J, Bourke PJ. Diabetes and stroke in Qatar: results of a prospective stroke register. Int Diabetes Nurs 2015; 12: 63–68. [Google Scholar]
- 39.Akhtar N, Salam A, Kamran S, et al. Ethnic variation in acute cerebrovascular disease: analysis from the Qatar stroke registry. Eur Stroke J 2016; 1: 231–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mushlin AI, Christos PJ, Abu-Raddad L, et al. The importance of diabetes mellitus in the global epidemic of cardiovascular disease: the case of the state of Qatar. Trans Am Clin Climatol Assoc 2012; 123: 193–207; discussion 207–208. [PMC free article] [PubMed] [Google Scholar]
- 41.Christos PJ, Chemaitelly H, Abu-Raddad LJ, et al. Prevention during the epidemiologic shift to chronic illness: a case control study of risk factors associated with cardiovascular disease in Qatar. J Local Glob Heal Perspect Epub ahead of print 4 February 2013. DOI: 10.5339/jlghp.2013.4.
- 42.Yusuf S, Rangarajan S, Teo K, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 2014; 371: 818–827. [DOI] [PubMed] [Google Scholar]
- 43.Rukn S, Al Mazya MV, Hentati F, et al. Stroke in the Middle-East and North Africa: a 2-year prospective observational study of stroke characteristics in the region – results from the safe implementation of treatments in stroke (SITS) – Middle-East and North African (MENA). Int J Stroke Epub ahead of print March 2019. DOI: 10.1177/174749301983033. [DOI] [PubMed]
- 44.Bernal-Pacheco O. Environmental vascular risk factors: new perspectives for stroke prevention. J Neurol Sci 2007; 262: 60–70. [DOI] [PubMed] [Google Scholar]
- 45.Mandeya J, Kridli S-O. Childhood overweight and obesity in Qatar: a literature review. Avicenna Epub ahead of print 15 December 2014. DOI: 10.5339/avi.2014.2.
- 46.Al-Nakeeb Y, Lyons M, Dodd L, et al. An investigation into the lifestyle, health habits and risk factors of young adults. Int J Environ Res Public Health 2015; 12: 4380–4394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Charfeddine L, Yousef Al-Malk A, Al Korbi K. Is it possible to improve environmental quality without reducing economic growth: evidence from the Qatar economy. Renew Sustain Energy Rev 2018; 82: 25–39. [Google Scholar]
- 48.Shah AV, Lee KK, McAllister DA, et al. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ 2015; 350: h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017; 389: 1907–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Farahat A. Air pollution in the Arabian Peninsula (Saudi Arabia, the United Arab Emirates, Kuwait, Qatar, Bahrain, and Oman): causes, effects, and aerosol categorization. Arab J Geosci 2016; 9: 196. [Google Scholar]
- 51.Tsai S-S, Goggins WB, Chiu H-F, et al. Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke 2003; 34: 2612–2616. [DOI] [PubMed] [Google Scholar]
- 52.Hong Y-C, Lee J-T, Kim H, et al. Air pollution. Stroke 2002; 33: 2165–2169. [DOI] [PubMed] [Google Scholar]
- 53.McCracken JP, Wellenius GA, Bloomfield GS, et al. Household air pollution from solid fuel use. Glob Heart 2012; 7: 223–234. [DOI] [PubMed] [Google Scholar]
- 54.Taj-Aldeen SJ, Chandra P, Denning DW. Burden of fungal infections in Qatar. Mycoses 2015; 58: 51–57. [DOI] [PubMed] [Google Scholar]
- 55.Khattab MA, Khan FY, Maslamani M, Al, et al. Pulmonary and extra pulmonary tuberculosis in Qatar: a first retrospective population-based study. Aid 2015; 5: 148–153. [Google Scholar]
- 56.Ieven MM, Hoymans VY. Involvement of Chlamydia pneumoniae in atherosclerosis: more evidence for lack of evidence. J Clin Microbiol 2005; 43: 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Elkind MSV, Tondella MLC, Feikin DR, et al. Seropositivity to Chlamydia pneumoniae is associated with risk of first ischemic stroke. Stroke 2006; 37: 790–795. [DOI] [PubMed] [Google Scholar]
- 58.Rosenfeld M, Ann Campbell L. Pathogens and atherosclerosis: update on the potential contribution of multiple infectious organisms to the pathogenesis of atherosclerosis. Thromb Haemost 2011; 106: 858–867. [DOI] [PubMed] [Google Scholar]
- 59.Bener A, Alali KA. Consanguineous marriage in a newly developed country: the Qatari population. J Biosoc Sci 2006; 38: 239–246. [DOI] [PubMed] [Google Scholar]
- 60.Bener A, Hussain R, Teebi AS. Consanguineous marriages and their effects on common adult diseases: studies from an endogamous population. Med Princ Pract 2007; 16: 262–267. [DOI] [PubMed] [Google Scholar]
- 61.Bener A, Darwish S, Al-Hamaq AO, et al. Association of PPARγ2 gene variant Pro12Ala polymorphism with hypertension and obesity in the aboriginal Qatari population known for being consanguineous. Appl Clin Genet 2013; 6: 103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Christos PJ, Chemaitelly H, Abu-Raddad LJ, et al. Prevention of type II diabetes mellitus in Qatar: who is at risk? Qatar Med J 2014; 13: 70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gezmu T, Schneider D, Demissie K, et al. Risk factors for acute stroke among South Asians compared to other racial/ethnic groups. PLoS One 2014; 9: e108901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gunarathne A, Patel JV, Potluri R, et al. Secular trends in the cardiovascular risk profile and mortality of stroke admissions in an inner city, multiethnic population in the United Kingdom (1997-2005). J Hum Hypertens 2008; 22: 18–23. [DOI] [PubMed] [Google Scholar]
- 65.Kronfol Z, Saleh M, Al-Ghafry M. Mental health issues among migrant workers in Gulf Cooperation Council countries: literature review and case illustrations. Asian J Psychiatr 2014; 10: 109–113. [DOI] [PubMed] [Google Scholar]
- 66.Yadav S, Hasan N, Marjot T, et al. Detailed analysis of gene polymorphisms associated with ischemic stroke in South Asians. PLoS One 2013; 8: e57305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cappuccio F. Ethnicity and cardiovascular risk: variations in people of African ancestry and South Asian origin. J Hum Hypertens 1997; 11: 571–576. [DOI] [PubMed] [Google Scholar]
- 68.Majumdar V, Nagaraja D, Karthik N, et al. Association of endothelial nitric oxide synthase gene polymor-phisms with early-onset ischemic stroke in South Indians. J Atheroscler Thromb 2010; 17: 45–53. [DOI] [PubMed] [Google Scholar]
- 69.Eastwood SV, Tillin T, Chaturvedi N, et al. Ethnic differences in associations between blood pressure and stroke in South Asian and European men. Hypertension 2015; 66: 481–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tillin T, Hughes AD, Mayet J, et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians, and African Caribbeans. J Am Coll Cardiol 2013; 61: 1777–1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gunarathne A, Patel JV, Kausar S, et al. Glycemic status underlies increased arterial stiffness and impaired endothelial function in migrant South Asian stroke survivors compared to European Caucasians. Stroke 2009; 40: 2298–2306. [DOI] [PubMed] [Google Scholar]
- 72.Kaul S, Munshi A. Genetics of ischemic stroke: Indian perspective. Neurol India 2012; 60: 498. [DOI] [PubMed] [Google Scholar]
- 73.Gunarathne A, Patel JV, Gammon B, et al. Impact of mean arterial blood pressure on higher arterial stiffness indices in South Asians compared to white Europeans. J Hypertens 2008; 26: 1420–1426. [DOI] [PubMed] [Google Scholar]
- 74.Forouhi N, Sattar N, McKeigue P. Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord 2001; 25: 1327–1331. [DOI] [PubMed] [Google Scholar]
- 75.Barker DJ. Fetal origins of coronary heart disease. BMJ 1995; 311: 171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yajnik CS. The insulin resistance epidemic in India: fetal origins, later lifestyle, or both? Nutr Rev 2001; 59: 1–9. [DOI] [PubMed] [Google Scholar]
- 77.Bavdekar A, Yajnik CS, Fall CH, et al. Insulin resistance syndrome in 8-year-old Indian children: small at birth, big at 8 years, or both? Diabetes 1999; 48: 2422–2429. [DOI] [PubMed] [Google Scholar]
- 78.Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009; 8: 355–369. [DOI] [PubMed] [Google Scholar]
- 79.Bamford J, Sandercock P, Dennis M, et al. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991; 337: 1521–1526. [DOI] [PubMed] [Google Scholar]
- 80.Deleu D, Inshasi J, Akhtar N, et al. Risk factors, management and outcome of subtypes of ischemic stroke: a stroke registry from the Arabian Gulf. J Neurol Sci 2011; 300: 142–147. [DOI] [PubMed] [Google Scholar]
- 81.Béjot Y, Bailly H, Durier J, et al. Epidemiology of stroke in Europe and trends for the 21st century. Presse Med 2016; 45(12, Pt 2): e391–e398. [DOI] [PubMed] [Google Scholar]
- 82.Akhtar N, Kamran SI, Deleu D, et al. Ischaemic posterior circulation stroke in State of Qatar. Eur J Neurol. 2009; 16: 1004–1009. [DOI] [PubMed] [Google Scholar]
- 83.Dalloz MA, Bottin L, Muresan IP, et al. Thrombolysis rate and impact of a stroke code: a French hospital experience and a systematic review. J Neurol Sci 2012; 314: 120–125. [DOI] [PubMed] [Google Scholar]
- 84.Gladstone DJ, Rodan LH, Sahlas DJ, et al. a citywide prehospital protocol increases access to stroke thrombolysis in Toronto. Stroke 2009; 40: 3841–3844. [DOI] [PubMed] [Google Scholar]
- 85.Imam YZ, Kamran S, Akhtar N, et al. Incidence, clinical features and outcomes of atrial fibrillation and stroke in Qatar. Int J Stroke Epub ahead of print 21 February 2019. DOI: 10.174749301983057. [DOI] [PubMed]
- 86.Akhtar N, Kamran S, Singh R, et al. The impact of diabetes on outcomes after acute ischemic stroke: a prospective observational study. J Stroke Cerebrovasc Dis 2019; 28: 619–626. [DOI] [PubMed] [Google Scholar]
- 87.Koçkaya G, Wertheimer A. Can we reduce the cost of illness with more compliant patients? An estimation of the effect of 100% compliance with hypertension treatment. J Pharm Pract 2011; 24: 345–350. [DOI] [PubMed] [Google Scholar]
- 88.Kockaya G, Wertheimer AI. An estimation of the effect of 100% compliance with diabetes treatment: can we reduce cost of illness with higher compliance rates? Innov Pharm January 2011. Epub ahead of print 1 January 2011. DOI: 10.24926/iip.v2i2.228.
- 89.Larsen J, Vaccheri A, Andersen M, et al. Lack of adherence to lipid-lowering drug treatment. A comparison of utilization patterns in defined populations in Funen, Denmark and Bologna, Italy. Br J Clin Pharmacol 2002; 49: 463–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cramer JA, Benedict Á, Muszbek N, et al. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract 2007; 62: 76–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Heuschmann PU, Kircher J, Nowe T, et al. Control of main risk factors after ischaemic stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur J Prev Cardiol 2015; 22: 1354–1362. [DOI] [PubMed] [Google Scholar]
- 92.Knight EL, Bohn RL, Wang PS, et al. Predictors of uncontrolled hypertension in ambulatory patients. Hypertension 2001; 38: 809–814. [DOI] [PubMed] [Google Scholar]
- 93.Taylor AA. Combination drug treatment of hypertension: have we come full circle? Curr Cardiol Rep 2004; 6: 421–426. [DOI] [PubMed] [Google Scholar]
- 94.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA 2010; 303: 2043. [DOI] [PubMed] [Google Scholar]
- 95.Bourke J, Sylvester R, Sharma P. Ethnic variations in the management of patients with acute stroke. Postgrad Med J 2006; 82: 13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stansbury JP, Jia H, Williams LS, et al. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke 2005; 36: 374–386. [DOI] [PubMed] [Google Scholar]
- 97.Gunarathne A, Patel JV, Gammon B, et al. Ischemic stroke in South Asians. Stroke Epub ahead of print 1 June 2009. DOI: 10.1161/STROKEAHA.108.535724. [DOI] [PubMed]
- 98.Jones D, Gill P. Breaking down language barriers. The NHS needs to provide accessible interpreting services for all. BMJ 1998; 316(7143): 1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Goodman A. The development of the Qatar Healthcare System: a review of the literature. IJCM 2015; 6: 177–185. [Google Scholar]
- 100.United Nations, Department of Economic and Social Affairs PD. World population prospects: the 2017 revision, key findings and advance tables, 2017.
- 101.El-Hajj M, Salameh P, Rachidi S, et al. The epidemiology of stroke in the Middle East. Eur Stroke J 2016; 1: 180–198. [DOI] [PMC free article] [PubMed] [Google Scholar]