Abstract
Background:
Many chronic conditions, including heart disease, cancer, and rheumatoid arthritis, are associated with underlying chronic inflammatory processes. Literature reviews have analyzed a variety of integrative therapies and their relationships with chronic inflammation. This systematic review is unique in reporting solely on yoga’s relationship with inflammation. Its purpose was to synthesize current literature examining the impact of yoga interventions on inflammatory biomarkers in adults with chronic inflammatory–related disorders.
Method:
Searches of several electronic databases were conducted. Inclusion criteria were (a) English language, (b) sample age >18 years old, (c) yoga interventions involving postures with or without yoga breathing and/or meditation, and (d) measured inflammatory biomarkers.
Results:
The final review included 15 primary studies. Of these, seven were rated as excellent and eight as average or fair. There was considerable variability in yoga types, components, frequency, session length, intervention duration, and intensity. The most common biomarkers measured were interleukin-6 (n = 11), C-reactive protein (n = 10), and tumor necrosis factor (n = 8). Most studies reported positive effects on inflammatory biomarkers (n = 11) from baseline to post yoga intervention. Analysis of the dose showed higher total dose (>1,000 min) resulted in greater improvements in inflammation.
Conclusion:
This review suggests that yoga can be a viable intervention to reduce inflammation across a multitude of chronic conditions. Future studies with detailed descriptions of yoga interventions, measurement of new and well-established inflammatory biomarkers, and larger sample sizes are warranted to advance the science and corroborate results.
Keywords: yoga, inflammation, biomarkers, review, chronic conditions
Many chronic conditions including heart disease (Kaptoge et al., 2013; Libby, Ridker, & Maseri, 2002), cancer (Ben-Neriah & Karin, 2011; Trinchieri, 2012), and rheumatoid arthritis (Choy, 2012; McInnes & Schett, 2011) are characterized by underlying chronic inflammation, known as “inflammaging.” Chronic stress is also associated with inflammaging, which is linked to increased morbidity and mortality in the aging population (Franceschi & Campisi, 2014; Michaud et al., 2013).
Biomarkers often measured to estimate chronic inflammation include interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and C-reactive protein (CRP;Liu et al., 2017). IL-6 is a pleiotropic cytokine that supports maintenance of inflammation (Hunter & Jones, 2015) and, together with TNF-α and IL-1, stimulates the hepatic production of inflammatory acute-phase proteins such as CRP (Gabay & Kushner, 1999; Jenny & Cushman, 2014). Despite the growth and proliferation of pharmaceutical research, the projected medical costs associated with chronic inflammatory conditions keep mounting. Interventions aimed at reducing chronic inflammation can help attenuate chronic conditions and improve patients’ well-being (Pawelec, Goldeck, & Derhovanessian, 2014). Emerging evidence suggests that mind–body interventions (i.e., mindfulness-based stress reduction [MBSR], meditation, tai chi, qigong, yoga, and relaxation) have the potential to reduce circulating pro-inflammatory cytokines, but results have been mixed (Bower & Irwin, 2016; Morgan, Irwin, Chung, & Wang, 2014).
Yoga is the most commonly practiced mind–body therapy in the United States, comprising about 80% of the total practice among three of the major categories of mind–body therapies: yoga, tai chi, and qigong (Clarke, Black, Stussman, Barnes, & Nahin, 2015). The practice of yoga began thousands of years ago in India and consists of eight components (limbs): yamas (ethical disciplines), niyamas (rules of conduct), asana (postures), pranayama (breathing), pratyahara (control of the senses), dharana (concentration of the mind), dyhana (meditation), and samadhi (merging one with eternity;Iyengar, 1994). Reviews of yoga intervention studies have found it to be as effective or better than exercise at improving health-related outcome measures (Ross & Thomas, 2010) and to have benefits similar to those of traditional aerobic physical activity in reducing cardiovascular risk factors (Chu, Gotink, Yeh, Goldie, & Hunink, 2016). Although prior literature reviews have investigated the potential impact of mind–body therapies on inflammatory biomarkers, a review solely focused on yoga’s propensity to lower chronic inflammation apart from other therapies is needed to synthesize the current knowledge and to identify a role for yoga in clinical practice.
Accordingly, we conducted a systematic review of literature to examine the efficacy of yoga interventions on reducing levels of inflammatory biomarkers in individuals with chronic inflammatory conditions including chronic stress. The objectives were to (1) evaluate the quality of existing evidence; (2) describe types, components, frequency, length, duration, and intensity of yoga used; (3) identify inflammatory biomarkers measured and the impact of yoga on inflammation; and (4) discern the relationship between the yoga dose and inflammatory biomarkers, if one exists.
Method
Eligibility Criteria
We conducted this systematic review using the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines (Moher, Liberati, Tetzlaff, Altman, & PRISMA Group, 2009). The following were the inclusion criteria for the studies: (a) English language, (b) sample age > 18 years, (c) yoga interventions involving postures with or without yoga breathing and/or meditation, and (d) measured inflammatory biomarkers. We excluded studies that included healthy participants with no known chronic conditions or chronic stress. In addition, we excluded studies if yoga was part of multimodal intervention such as MBSR, the yoga intervention lacked the component of postures, or the study measured cortisol as a mood-state biomarker and lacked any discussion of its relationship with inflammation.
Literature Search Strategy
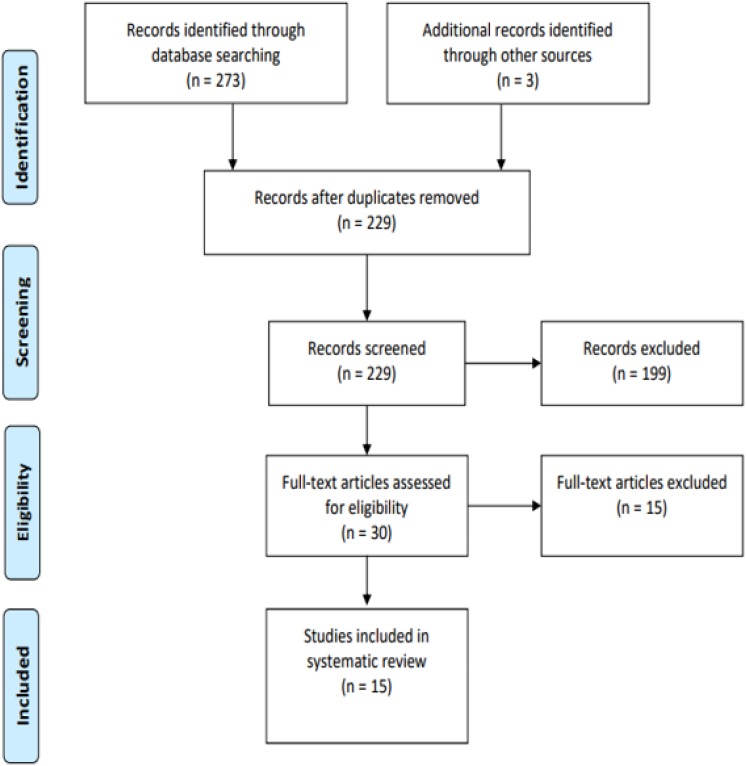
With the help of a medical librarian, we conducted electronic database searches of PubMed, PsycINFO, Embase, and Cochrane (Figure 1) for articles published from the date of inception of each database to August 31, 2017. The search terms included “yoga,” “inflammation,” and “inflammatory biomarkers.” We also used individualized MESH terms for each database. For example, the complete search that we used for PubMed was (“Yoga”[Mesh] OR yoga* OR “Astanga Yoga” OR “Bikram Yoga” OR “Iyengar Yoga” OR “Vinyasa Yoga” OR “Tantric Buddhism Yoga”) AND (“Inflammation” [Mesh] OR inflammat*). The first author (D. M. D) screened titles and abstracts after the removal of all the duplicates. Full-text articles were assessed for final inclusion upon discussion with the second author (P. S.).
Figure 1.
Preferred reporting items for systematic reviews and meta-analysis flow diagram of literature review.
Quality of Evidence
We assessed quality of the evidence in each study using the Quality Rating Scale, which was originally developed to rate the quality of randomized controlled trials in psychology (Yates, Morley, Eccleston, & Williams, 2005). The scale consists of two subscales: Treatment Quality (scores 0–9) and Quality of Study Designs and Methods (scores 0–26). The first subscale evaluates the treatment content and duration, manualization of the protocol, therapist training, and patient engagement. The second subscale includes sample description, randomization, allocation, validity and reliability of outcomes, and statistical analysis. The validation study for the Quality Rating Scale listed mean (SD) total quality scores for a study to earn a rating of excellent as 22.7 (1.95), of average as 18.71 (2.25), and of poor as 12.10 (3.17; Yates et al., 2005).
We assessed the two studies with one-group designs using the National Heart, Lung, and Blood Institute quality-assessment tool for pre–post studies with no control group (NIH: National Heart, Lung, and Blood Institute, 2018). The tool consists of 12 items, and scoring options are yes, no, cannot determine, not applicable, and not reported. Reviewers assessed the overall bias of each study by examining the individual items that were rated as no to assign a quality rating of good, fair, or poor. Two independent raters (D. D. and P. S.) evaluated the quality of the evidence, discussed incongruencies in the scores, and reached concordance through a careful examination of the selected tools’ criteria.
Calculation of the Total Dose of Yoga Practice
For each study, we calculated the total dose in minutes of yoga practice to discern the effect of dose on the outcome of inflammation. Although seven of the studies (Kiecolt-Glaser et al., 2014; Parma et al., 2015; Pullen et al., 2008; Pullen et al., 2010; Rao et al., 2017; Sohl et al., 2016; Wolff, Memon, Chalmers, Sundquist, & Midlov, 2015) reported giving instructions to practice yoga at home, we used only supervised yoga minutes to calculate the dose due to lack of overall minutes reported for yoga at home. We multiplied session length in minutes by frequency per week by duration in weeks to calculate the total dose in minutes of yoga practice per study. This review was not limited to a specific population; thus, we discuss our findings based on each inflammatory condition and the inflammation-related outcomes post yoga intervention.
Results
Study Selection
The PRISMA flow diagram depicts the number of included articles and the number of articles excluded at each stage of the literature search (Figure 1). In total, we retrieved 273 articles using the search criteria and an additional three articles through screening the reference lists of the retrieved reviews. After removing 47 duplicates, we screened 229 titles and abstracts. Of these, we excluded 199 articles because they did not meet inclusion criteria. We assessed the full text of the remaining 30 articles for eligibility and ultimately included 15 articles in the present review. Of the excluded articles, 91 were not full-text peer-reviewed articles, 49 did not include yoga interventions, 56 did not measure inflammatory biomarkers in response to yoga, 11 included yoga as part of a multimodal intervention or the intervention lacked the component of postures, 2 included participants younger than 18 years of age, and 5 had healthy participants with no known chronic conditions or chronic stress. Harkess, Ryan, Delfabbro, and Cohen-Woods (2016) cited a separate publication for the details of their yoga intervention. Upon our search of the databases, we located a dissertation report that included details of the intervention. Thus, we will cite both the original article and the dissertation report when we discuss the yoga intervention.
Study Characteristics
Detailed information about selected studies appears in Table 1. The review included three studies with quasi-experimental designs (Cho, Moon, & Kim, 2015; Parma et al., 2015; Wolff et al., 2015) and two single-group pre–post studies (Sarvottam, Magan, Yadav, Mehta, & Mahapatra, 2013; Yadav, Magan, Mehta, Sharma, & Mahapatra, 2012), with the remaining 10 studies being randomized controlled trials. A total of five studies had waitlist control groups (Harkess, Ryan, Delfabbro, & Cohen-Woods, 2016; Kiecolt-Glaser et al., 2014; Rajbhoj, Shete, Verma, & Bhogal, 2015; Shete, Verma, Kulkarni, & Bhogal, 2017; Singh, Bhandari, & Rana, 2011) and four used usual-care or no-treatment groups (Cho et al., 2015; Pullen et al., 2008; Pullen et al., 2010; Wolff et al., 2015). Neither the waitlist control nor the usual-care groups were matched in general structure to the treatment groups in any of the relevant studies, which can threaten internal validity and impact the study outcomes (Mohr et al., 2009). Two studies provided education as a control condition (Bower et al., 2014; Rao et al., 2017), and one used equal time and attention (Sohl et al., 2016). Finally, two of the studies used three-arm intervention trials comparing yoga against two control groups (Parma et al., 2015; Wolff et al., 2015).
Table 1.
Description of the Studies.
| First Author (Year) | Location; Design | Quality Ratinga | Diagnosis (Total Sample); Group n; Mean Age (SD) | Yoga Type; Components | Control Group | Frequency × Session Length × Intervention Duration = Total Dose in Minutes | Inflammatory Biomarkers | Outcomes on Inflammatory Biomarkers From Baseline to Post Yoga Intervention |
|---|---|---|---|---|---|---|---|---|
| Bower et al. (2014) | USA; RCT | Excellent | Breast cancer Stages 0–II (N = 31); YG (n = 16), CG (n = 15); x̅ age = 54 (5.4) | HY/IY; postures, breathing | HE | 2/week × 90 min × 12 weeks = 2,160 min | NF-κB, GR, sTNF-RII, IL-1, IL-6, CRP, CREB, and salivary cortisol | No changes in CRP, IL-1, IL-6 or diurnal cortisol. Reduced NF-κB, increased activity of the CREB (all p < .05). sTNF-RII plasma levels remained stable in the yoga group compared to the control group (p = .028) after 12 weeks of yoga |
| Cho et al. (2015) | Republic of Korea; non-RCT | Excellent | Premenopausal women with CLBP (N = 25); YG (n = 14), CG (n = 11); x¯ age = 43.3 (7.5) | HY; postures, breathing, meditation | UC | 3/week × 60 min × 12 weeks = 2,160 min | CRP, TNF-α, and cortisol | TNF-α maintained in the yoga group, whereas TNF-α significantly increased in the control group (p < .01). Serum cortisol level significantly decreased in the yoga group (p < .05) after 12 weeks of yoga |
| Harkess et al. (2016) | Australia; subsample of large RCT | Average | Chronically stressed women (N = 26); YG (n = 11), CG (n = 15); x¯ age = 41 (4.3) | HY/Ashtanga; postures, breathing, meditation | WL | 1/weekb × 60 min × 8 weeks = 480 min | Il-6, TNF, CRP, and LINE-1 methylation | No significant findings after 8 weeks of yoga. However, methylation of the TNF region in the yoga group was reduced relative to the waitlist control group, but the change was not statistically significant |
| Kiecolt-Glaser et al. (2014) | USA; RCT | Excellent | Breast cancer Stages 0–III (N = 200); YG (n = 100), CG (n = 100); x¯ age = 51.6 (9.2) | HY; postures, breathing | WL | 2/week × 90 min × 12 weeks = 2,160 min | IL-6, TNF-α, and IL-1B | IL-6 (p = .027), TNF-α (p = .027), and IL-1B (p = .037) were lower for yoga participants compared with the CG at 3 months’ follow-up, but not after 12 weeks of yoga |
| Parma et al. (2015) | USA; non-RCT | Excellent | Breast cancer survivors Stages I–II (N = 94); YG (n = 31), CE (n = 31), C (n = 32); x¯ age = 56.2 (7.9) | HY; not described, postures mentioned in the text | CE (second arm) and any exercise (third arm) | 3/week × 60 min × 24 weeks = 4,320 min | IL-6, IL-8, TNF-α, and CRP | No significant differences among groups after 24 weeks of yoga. Note. YG had attrition of 11 participants |
| Pullen et al. (2008) | USA; RCT | Average | HF (N = 19); YG (n = 9), CG (n = 10); YG x¯ age = 52.1 (3.3), CG x¯ age = 50.5 (12.8) | HY; postures, breathing, meditation | UC | 2/week × 70 min × 8 weeks = 1,120 min | IL-6, hs-CRP, and EC-SOD | Statistically significant reductions in serum levels of IL-6 and hs-CRP and an increase in EC-SOD in the YG group (p < .005) after 8 weeks of yoga |
| Pullen et al. (2010) | USA; RCT | Average | HF (N = 40); YG (n = 21), CG (n =19); YG x¯ age = 55.8 (7.6), CG x¯ age = 52.5 (12.7) | HY; postures, breathing, meditation | UC | 2/week × 60 min × 8 weeks = 1,080 min | IL-6, CRP, and EC-SOD | IL-6 (p = .004) and CRP (p = .016) were reduced, and EC-SOD (p = .012) was increased after 8 weeks of yoga |
| Rajbhoj et al. (2015) | India; RCT | Average | Industrial workers w/chronic stress (N = 48); YG (n = 24), CG (n = 24); YG x¯ age = 40.7 (6.8), CG x¯ age = 40.2 (6.3) | Not identified; postures, breathing, “om” chanting | WL | 6/week × 45 min × 12 weeks = 3,240 min | IL-10 and IL-1B | YG showed a significant decrease in IL-1 β and a significant increase in IL-10 (p < .05 for both) after 12 weeks of yoga |
| Rao et al. (2017) | India; RCT | Excellent | Metastatic breast cancer, Stage IV (N = 91); YG (n = 45), CG (n = 46); YG x¯ age = 48.9 (9.1), CG x¯ age = 50.2 (9.2) | Not identified; postures, breathing, meditation, relaxation w/imagery, philosophical concepts of yoga | Ed and STS | 2/week × 60 min × 12 weeks = 1,440 min | Salivary cortisol, and NK cells | Significant decrease in morning waking cortisol (p < .05) and improvement in NK cell % (p = .03) in YG compared to CG after 12 weeks of yoga |
| Sarvottam et al. (2013) | India; one-group pre–post | Fair | Overweight or obese men (N = 51); x¯ age = 39 (12.2) | Not identified; postures, breathing, nutrition counseling, yoga theory | N/A | 1/day × 120 min × 10 days = 1,200 min | IL-6, adiponectin, and ET-1 | Plasma levels of IL-6 decreased significantly (p = .012) and adiponectin increased significantly (p = .014) following 10 days of yoga compared with baseline. There was no significant change in the levels of plasma ET-1 |
| Shete et al. (2017) | India; RCT | Excellent | Industrial workers with prolonged stress (N = 48); YG (n = 24), CG (n = 24); x¯ age 41.5 (5.2) | Classical yoga; postures, breathing | WL | 6/week × 60 min × 12 weeks = 4,320 min | IL-6, TNF-α, and hs-CRP | Hs-CRP (p < .01), IL-6 (p < .001), and TNF-α (p < .001) significantly reduced in the YG after 12 weeks of yoga |
| Singh et al. (2011) | India; RCT | Average | Rheumatoid arthritis (N = 80); YG (n = 40), CG (n = 40); YG x¯ age = 35.1 (7.3), CG x¯ age = 34.7 (7.3) | Not identified; postures, cleansing practices, healthy yoga diet, breathing, meditation | WL | 6/week × 90 min × 7 weeks = 4,410 min | Lymphocyte count, CRP, and uric acid | CRP, uric acid levels, and lymphocyte count all significantly reduced (p < .01 for all three) in the YG after 7 weeks of yoga |
| Sohl et al. (2016) | USA; RCT-pilot | Excellent | Colorectal cancer Stages 0–IV (N = 15); YG (n = 6), CG (n = 5); median age = 61 | Not identified; movement, breathing, awareness meditation, and relaxation | AC | 3 every 2 weeks × 15 min × 8 weeks = 180 min | IL-6, IL-1, soluble TNF receptor 1, TNF-α, and CRP | No significant differences after 8 weeks of yoga due to underpowered sample |
| Wolff et al. (2015) | Sweden; three-group matched participants design | Average | Adults with diagnosed HTN (N = 83); YG1 (n = 28) YG2 (n = 28), CG (n = 27); YG1 x¯ age = 66.2 (7.7), YG2 x¯ age = 65 (10.3), CG x¯ age = 60.8 (11) | Kundalini; postures, breathing, meditation | Yoga at home (2nd arm) and UC (3rd arm) | 1/week × 60 min × 12 weeks = 720 min | hs-CRP and IL-6 | No significant group differences after 12 weeks of yoga |
| Yadav et al. (2012) | India; one-group, pre–post | Fair | Patients with chronic inflammatory diseases (N = 86); x¯ age = 40.1 (13.9) | Not identified; postures, breathing, nutrition counseling, yoga theory | N/A | 1/day × 120 min × 10 days = 1,200 min | IL-6, TNF-α, cortisol, and β-endorphins | Mean cortisol (p = .001), IL-6 (p = .036) and TNF-α (p = .002) levels decreased and mean β-endorphin levels increased (p = .024) from baseline to after 10 days of yoga |
Note. AC = attention control; C = comparison exercise; CE = comprehensive exercise; CG = control group; CLBP = chronic lower back pain; CREB = cAMP response element-binding protein; CRP = C-reactive protein; EC-SOD = extracellular superoxide dismutase; Ed = education; ET-1 = endothelin-1; GR = glucocorticoid receptor; HE = health education; HF = heart failure; hs-CRP = high-sensitivity C-reactive protein; HTN = hypertension; HY = hatha yoga; IL = interleukin; IY = Iyengar yoga; LINE-1 = long interspersed nuclear element 1; N/A= not applicable; NF-κB = transcription factor nuclear factor kappa B; NK = natural killer; RCT = randomized controlled trial; STS = supportive therapy sessions; sTNF-RII = soluble tumor necrosis factor receptor Type II; TNF-α = tumor necrosis factor-α; UC = usual care; WL = waitlist control; YG = yoga group.
a Yates, Morley, Eccleston, and Williams (2005) and NIH: National Heart, Lung, and Blood Institute (2018).
b Yoga intervention was offered 2 times per week, but only 1 time per week was counted as completion.
Participants
The 15 studies we reviewed included a total of 937 participants. Sample sizes ranged from 15 patients (Sohl et al., 2016) to 200 participants (Kiecolt-Glaser et al., 2014). The mean age of the participants ranged from 35 to 66 years, with a weighted mean age of 48.54 years. The combined samples consisted of 706 females (75%) and 231 males (25%). Many studies (n = 9) did not report the racial and ethnic backgrounds of the participants. Of the six studies that did report race (Kiecolt-Glaser et al., 2014; Parma et al., 2015; Pullen et al., 2008; Pullen et al., 2010; Shete et al., 2017; Sohl et al., 2016), 264 (64%) participants were White, 80 (19%) Black, 48 (12%) Indian, and 5% were described as Asian or “Other.”
The chronic conditions participants in these studies had were breast cancer (Bower et al., 2014; Kiecolt-Glaser et al., 2014; Parma et al., 2015; Rao et al., 2017), colorectal cancer (Sohl et al., 2016), heart failure (Pullen et al., 2008; Pullen et al., 2010), high blood pressure (Wolff et al., 2015) and cardiometabolic risk factors (Sarvottam et al., 2013), chronic stress (Cho et al., 2015; Harkess et al., 2016) including prolonged exposure to occupational hazards/pollutants (Rajbhoj et al., 2015; Shete et al., 2017), and rheumatoid arthritis (Singh et al., 2011). One study involved a heterogeneous sample of participants diagnosed with a variety of chronic inflammatory conditions: mental stress, diabetes, hypertension, musculoskeletal pain, bronchial asthma, constipation, and a subsample of overweight and obese individuals (Yadav et al., 2012).
Objective 1: Quality of Evidence
Seven of the selected articles were excellent, with scores on the quality scale above 22.7, six were average, and two single-group studies were fair, with a lowest score of 19 (Table 1). Only four of the articles described adequate steps for minimizing biases via rigorous randomization methods, such as blinding to group assignment, and provided information regarding allocation and data collection (Bower et al., 2014; Kiecolt-Glaser et al., 2014; Rao et al., 2017; Sohl et al., 2016). Other methodological gaps included lack of reporting on the power analysis calculation and insufficient sample sizes based on the power analysis. Specifically, eight studies did not include a power analysis (Harkess et al., 2016; Parma et al., 2015; Pullen et al., 2008; Pullen et al., 2010; Rajbhoj et al., 2015; Shete et al., 2017; Singh et al., 2011; Sohl et al., 2016), and two others included the power analysis but did not reach sufficient sample size based on those calculations (Bower et al., 2014; Wolff et al., 2015). None of the studies included a long enough follow-up time (6 months) to adequately identify a sustained change in outcome variables (Yates et al., 2005). Only Kiecolt et al. (2014) and Bower et al. (2014) followed the participants for as long as 3 months postintervention.
We evaluated the two studies with single-group designs using National Heart, Lung, and Blood Institute criteria (NIH: National Heart, Lung, and Blood Institute, 2018) and rated both fair due to the presence of several potential risks of bias. First, power analysis was lacking for sample size calculations. Both studies used convenience sampling, which limits the generalizability of their findings and introduces bias in the conclusions. Additionally, Sarvottam, Magan, Yadav, Mehta, and Mahapatra (2013) used only male participants; thus, the sample was not representative of clinical populations. Both single-group studies provided additional nutritional counseling and encouraged support from partners in the group, which may have biased the results and potentially impacted adherence and inflammatory outcomes.
Objective 2: Yoga Interventions
Yoga types
Hatha yoga was the most common style named across the studies, with five of the selected articles describing interventions using this type of yoga (Cho et al., 2015; Kiecolt-Glaser et al., 2014; Parma et al., 2015; Pullen et al., 2008; Pullen et al., 2010) and two reporting using a type of hatha yoga, Iyengar (Bower et al., 2014), and Ashtanga (Harkess, 2016; Harkess et al., 2016). Another six studies did not identify the type of yoga used (Rajbhoj et al., 2015; Rao et al., 2017; Sarvottam et al., 2013; Singh et al., 2011; Sohl et al., 2016; Yadav et al., 2012), while one used medical kundalini yoga (Wolff et al., 2015), and another described the style as a “classical yoga” grounded in the principles of the Kaivalyadhama Yoga Institute (Shete et al., 2017).
Components
Although the primary component of the interventions was postures, the number of components in each study varied from two to five. Postures were combined with breathing techniques in three studies (Bower et al., 2014; Kiecolt-Glaser et al., 2014; Shete et al., 2017) and with breathing and meditation in six studies (Cho et al., 2015; Harkess et al., 2016; Pullen et al., 2008; Pullen et al., 2010; Sohl et al., 2016; Wolff et al., 2015). Other studies that had postures and breathing with or without meditation included additional yoga practices such as “om” chanting (Rajbhoj et al., 2015) and yoga theory and/or philosophy teachings together with nutrition counseling (Rao et al., 2017; Sarvottam et al., 2013; Singh et al., 2011; Yadav et al., 2012).
Duration and frequency
Authors reported intervention duration in weeks or months, ranging from three 15-min sessions every 2 weeks over 8 weeks (Sohl et al., 2016) to three 1-hr sessions weekly over 6 months (Parma et al., 2015). The frequency of the sessions ranged from once per week (Wolff et al., 2015) to every day of the week (Sarvottam et al., 2013; Yadav et al., 2012), with session length ranging from 60 to 120 min, respectively. The most common frequency offered (n = 6) was twice a week (Bower et al., 2014; Harkess et al., 2016; Kiecolt-Glaser et al., 2014; Pullen et al., 2008; Pullen et al., 2010; Rao et al., 2017) with session lengths ranging from 60 to 90 min.
Intensity
Authors generally did not describe the intensity of the interventions. In fact, only one researcher described the yoga intervention as moderate intensity (Harkess, 2016; Harkess et al., 2016). In studies that included participants with cancer, researchers described the interventions as restorative (Kiecolt-Glaser et al., 2014) or using easy (Rao et al., 2017) or supported postures (Bower et al., 2014). In studies that included participants with heart failure or cancer, researchers often included variations in the yoga interventions with the use of props such as blocks, chairs, and a wall (Pullen et al., 2008; Pullen et al., 2010; Sohl et al., 2016), suggesting lower intensity. Wolff, Memon, Chalmers, Sundquist, and Midlov (2015) described kundalini yoga as accessible and easy to perform and adapted for individuals with high blood pressure.
Of the remaining six studies, five were conducted in India. All five used a high-frequency yoga class, ranging from daily 120-min sessions for a total of 10 days (Sarvottam et al., 2013; Yadav et al., 2012) to 45–90 min 6 days a week (Rajbhoj et al., 2015; Shete et al., 2017; Singh et al., 2011) for 7–12 weeks. All five studies included a progression toward advanced postures (e.g., advanced backbends). The remaining study, conducted in the Republic of Korea, also included advanced postures such as half-moon and wheel (Cho et al., 2015). The frequency and advanced nature of the postures in these six studies led us to conclude the intensity was moderate to vigorous. Overall, the interventions varied from easier supported postures to moderate and more advanced yoga postures. Notably, in one study, researchers reported that the intervention included yogic postures but lacked a detailed description of the intervention or the intensity (Parma et al., 2015). We found considerable variability across studies in yoga types, components, frequency, length, duration and intensity, with 40% (n = 6) of the studies lacking a description of the type of yoga used.
Objective 3: Inflammatory Biomarkers and the Impact of Yoga on Inflammation
Despite the heterogeneity in study designs and populations, 11 of the 15 studies reported favorable outcomes on inflammation following yoga intervention. The most common biomarkers measured were IL-6 (n = 11), CRP (n = 10), and TNF-α (n = 8). Chronic conditions addressed included cancer, cardiovascular disease, chronic stress, and other inflammatory conditions.
Cancer
Of the 15 studies, 5 explored yoga’s effects on patients with cancer, 4 of which were in breast cancer at varying stages of disease and treatment periods (Bower et al., 2014; Kiecolt-Glaser et al., 2014; Parma et al., 2015; Rao et al., 2017) and 1 that included patients with colorectal cancer during their chemotherapy treatment (Sohl et al., 2016). Of the studies involving patients with breast cancer, three found favorable outcomes on inflammation after the yoga intervention (Bower et al., 2014; Kiecolt-Glaser et al., 2014; Rao et al., 2017). The favorable outcomes on inflammation were not associated with any particular cancer stage.
Effects on biomarkers varied among similar diagnoses. Kiecolt-Glaser et al. (2014) did not find reductions in the levels of IL-6, IL-1B, or TNF-α immediately post intervention, but levels were significantly reduced 3 months later (p < .05). Rao et al. (2017) found significant reductions in natural killer cells (p = .03) and morning waking cortisol (p < .05). Bower et al. (2014), who measured inflammatory gene expression, made a unique discovery: postintervention, there were no significant changes in circulating IL-1, CRP, or IL-6, but researchers did find lower levels of transcription factor nuclear factor-κB, a pro-inflammatory factor, and increased levels of glucocorticoid receptor, an anti-inflammatory factor (p < .05). Additionally, a marker of TNF, soluble TNF receptor Type II, remained stable in the yoga group, whereas in the control group, it continued to increase, reflecting increasing inflammation (p = .028).
Two studies found no changes in inflammatory markers (Parma et al., 2015; Sohl et al., 2016). After 6 months of three sessions of yoga practice per week, levels of IL-6, IL-8, TNF-α, and CRP did not differ significantly among three exercise groups (Parma et al. 2015). The authors suggested their findings were hindered by the relatively small sample size (n = 20) and high attrition rate (n = 11) in the yoga group. Similarly, Sohl et al. (2016) also did not find significant changes in inflammatory biomarkers in response to the yoga intervention in patients with colorectal cancer due to the submarginal number of participants (n = 6) in the intervention group.
Cardiovascular disease
Studies that focused on inflammatory biomarkers association with cardiovascular factors reported varying severity of conditions studied, including cardiometabolic risk factors (Sarvottam et al., 2013), Stage I hypertension (Wolff et al., 2015), and New York Heart Failure Association class I–III heart failure (Pullen et al., 2008; Pullen et al., 2010). Both of the pilot studies exploring effects of yoga in heart failure (Pullen et al., 2008; Pullen et al., 2010) found significant reductions in pro-inflammatory cytokines, IL-6 and high-sensitivity CRP (hs-CRP), and increased levels of extracellular superoxide dismutase, an antioxidant enzyme thought to have a protective effect on the cardiovascular system (Nozik-Grayck, Suliman, & Piantadosi, 2005).
In their study on participants with Stage I hypertension, Wolff et al. (2015) measured IL-6 and hs-CRP and found no significant differences among the supervised-yoga, the yoga-at-home, and usual-care groups. The researchers attributed their lack of significant findings to the small sample and the use of antihypertensive medications by the participants, as these drugs are known to attenuate levels of IL-6. In contrast, Sarvottam et al. (2013) found decreased levels of plasma IL-6, increased levels of adiponectin, an anti-inflammatory protein, and an unchanged level of endothelin-1, a potent contributor to progression of atherosclerosis among metabolically at-risk individuals, after a 10-day yoga intervention.
Chronic stress
Also included in this review were four studies that included participants with prolonged stress conditions (Cho et al., 2015; Harkess et al., 2016; Rajbhoj et al., 2015; Shete et al., 2017). Of these, two included industrial workers from a factory in India exposed to occupational hazards and various pollutants as by-products of paint and steel (Rajbhoj et al., 2015; Shete et al., 2017). Although the two studies were conducted among workers of the same region, researchers reported on different inflammatory biomarkers. Shete, Verma, Kulkarni, and Bhogal (2017) reported significant reduction in IL-6, TNF-α, and hs-CRP (p < .01) in the yoga compared to the control group, while Rajbhoj et al. (2015) showed a decrease in IL-1β and an increase in the anti-inflammatory cytokine, IL-10 (p < .05). In two other studies, investigators reported on yoga’s impact on inflammation among chronically stressed premenopausal women with chronic lower back pain (Cho et al., 2015) and women with self-reported psychological stress (Harkess et al., 2016). The study by Harkess et al. (2016) was unique in evaluating markers of DNA methylation, with findings that, though not statistically significant, suggested that yoga practice may alter DNA methylation. Cho, Moon, and Kim (2015) reported that the yoga intervention group had reduced serum cortisol (p < .05) and stable serum TNF-α levels, while the control group’s TNF-α increased significantly (p < .01).
Other inflammatory conditions
Only one study focused on inflammatory biomarkers of patients with rheumatoid arthritis. After six weekly 90-min yoga sessions, participants had a significant reduction in levels of circulating CRP and lymphocyte counts and had fewer self-reported inflamed joints (Singh et al., 2011). Yadav, Magan, Mehta, Sharma, and Mahapatra (2012) had a mixed sample of participants who had various multiple chronic conditions: mental stress, diabetes, hypertension, musculoskeletal pain, bronchial asthma, constipation, and a subsample of overweight and obese individuals. The authors reported decreased IL-6, TNF-α, and plasma cortisol levels and increased β-endorphin levels in all the participants in response to the yoga intervention but did not provide a breakdown in inflammatory outcomes by individual chronic condition. Overall, the types of biomarkers measured varied greatly across all 15 studies and also varied within similar cohorts of chronic diagnoses.
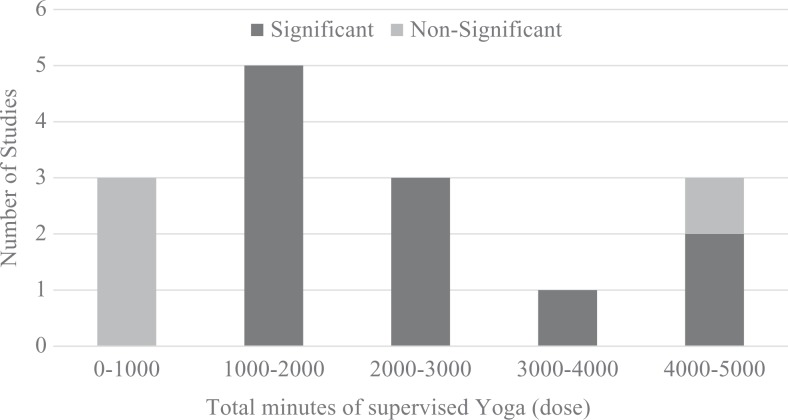
Objective 4: Relationship Between the Total Dose of Yoga and Inflammatory Biomarkers
The last objective of this review was to discern the relationship between total dose of yoga in minutes and inflammatory biomarkers (Figure 2). For this analysis, we classified the effect of yoga on inflammation as either significant or nonsignificant as reported in the individual study findings. Higher dose (Intervention Duration × Session Length × Frequency) produced significant reductions in inflammation. The three studies (Harkess et al., 2016; Sohl et al., 2016; Wolff et al., 2015) that had a dose of less than 1,000 min of supervised-yoga practice did not report significant findings regarding inflammation. Studies that included a dose of 1,000–4,500 min of supervised-yoga practice (n = 11) all showed improvements in inflammatory profiles with the exception of one study whose authors reported a high attrition rate in the yoga group (Parma et al., 2015). These results indicate that a higher dose may be more efficacious than a lower dose on post intervention inflammatory biomarkers.
Figure 2.
Number of studies reporting significant versus nonsignificant effects of yoga on inflammation based on the total dose.
Discussion
The major finding from this review is that most of the selected studies suggest that yoga interventions with postures as a component may have a beneficial impact on inflammatory biomarkers. This conclusion is congruent with results from a prior review on mind–body therapies (Morgan et al., 2014). The present review was unique because it examined yoga apart from other mind–body therapies. Yoga interventions reduced inflammation in three of the five studies involving cancer (Bower et al., 2014; Kiecolt-Glaser et al., 2014; Rao et al., 2017), three of the four studies involving cardiovascular disease (Pullen et al., 2008; Pullen et al., 2010; Sarvottam et al., 2013), three of the four studies involving chronic stress conditions (Cho et al., 2015; Rajbhoj et al., 2015; Shete et al., 2017), one study involving rheumatoid arthritis (Singh et al., 2011), and one with a mixed sample of individuals with chronic conditions (Yadav et al., 2012).
Our careful examination of the effect of dose on outcome is unique among existing reviews on mind–body therapies and inflammation. We found that five of the studies with higher doses of yoga practice and advanced postures (Rajbhoj et al., 2015; Sarvottam et al., 2013; Shete et al., 2017; Singh et al., 2011; Yadav et al., 2012) reported significant improvements in inflammatory biomarkers. While intensity was not part of the calculated dose, the extant literature suggests that higher intensity physical activity favorably impacts the inflammatory cytokine responses in participants who are healthy and in those with chronic inflammatory conditions (Hawkins et al., 2012; Nimmo, Leggate, Viana, & King, 2013). For example, 5 years of daily 1-hr sessions of moderate- to high-intensity yoga practice lowered basal pro-inflammatory cytokines (IL-6 and TNF-α) among healthy yoga practitioners in India (Vijayaraghava, Doreswamy, Narasipur, Kunnavil, & Srinivasamurthy, 2015). Our results also showed that the yoga interventions designed in India and the Republic of Korea (n = 6) included more advanced postures and higher frequency and intensity compared to those designed in the United States. Yoga may be a more culturally accepted exercise in India and the Republic of Korea; thus, higher frequency and advanced postures were feasible among participants in these countries. However, participants in the United States, particularly those with chronic conditions, may find lower frequency and modified yoga postures more acceptable. This finding is an important detail, and future investigators need to consider cultural variations in designing replication studies.
Another potential mechanism by which yoga interventions may influence inflammation is through their effects on the sympathetic and parasympathetic nervous systems. Accordingly, eight of the selected studies used a slower paced yoga and props. Most of the studies we analyzed included some type of slow-breathing technique. Prior studies that used slow-breathing techniques have demonstrated that yoga interventions positively affect parasympathetic nervous system and decrease sympathetic activity (Lakkireddy et al., 2013; Mourya, Mahajan, Singh, & Jain, 2009; Patil, Aithala, & Das, 2015). Prior reviews of yoga interventions also found evidence to support yoga’s efficacy in improving heart rate, heart rate variability (Ross & Thomas, 2010), and blood pressure, the markers of sympathetic activity (Chu et al., 2016). These findings suggest that certain yoga-based breathing techniques and slow movements may aid the relaxation of the autonomic nervous system. Thus, yoga may be particularly effective in reducing inflammation because, unlike exercise or stress reduction alone, yoga has components of both relaxation techniques and exercise.
Another important finding of our review is that the studies used a variety of inflammatory biomarkers as outcome measures. The most commonly measured cytokines in the studies were IL-6, CRP, and TNF-α. The conflicting findings regarding the common biomarkers among the different studies suggest a need for investigators to use a consistent and yet wider range of inflammatory biomarkers to gain a better understanding of the mechanisms of inflammation. Specifically, the novel findings of decreased pro-inflammatory gene expression (Bower et al., 2014) and changes in DNA methylation (Harkess et al., 2016) suggest that the genetic pathway is one mechanism by which yoga influences inflammation. Yoga’s effects on the genetic expression of inflammatory markers were not, however, supported by the findings regarding pro-inflammatory cytokines, suggesting that changes to the genetic pathways may precede changes to the expression of circulating cytokines (Bower et al., 2014). Bower and Irwin (2016)) drew a similar conclusion in a review in which they examined seven studies using mind–body therapy interventions (tai chi [n = 3], meditation [n = 3], and yoga [n = 1]) and found a favorable impact on genetic markers of inflammation. Further investigation is required to determine the mechanisms by which yoga may impact the genetic inflammatory process.
The reviewed studies illustrate the current state of the science of yoga research. There was considerable variability in the types, components, frequency, length, duration, and intensity of the yoga interventions. Most studies only included two to five yoga components, which limit the comparisons of the interventions. For example, yogic diet as an additional component may mediate the inflammatory pathways. The philosophical teachings (Rao et al., 2017) and the nutrition counseling (Sarvottam et al., 2013; Singh et al., 2011; Yadav et al., 2012) described in four studies may have had confounding effects. In the study by Singh, Bhandari, and Rana (2011), authors listed yogic diet as a component but did not describe it, whereas Sarvottam et al. (2013) and Yadav et al. (2012) included nutritional counseling without meals, encouraged support from partners, and included unstructured discussions in the group. Thus, education about healthy eating and support from others in the group may have led some participants to engage in a more comprehensive lifestyle change, which may have increased the beneficial impact on inflammation in these patients. However, we did not discover any studies that directly compared the effects of controlled yoga with and without the additional lifestyle changes, so the impact of additive non-yoga components on inflammation cannot be quantified. New investigations comparing the individual and combined effects of multiple components of yoga are needed to support the use of more than four common components: postures, breathing, relaxation, and meditation.
Limitations
The review has several limitations, and readers are advised to consider the conclusions regarding each chronic condition with caution. We found only a few studies examining the efficacy of yoga interventions on biomarkers of inflammation in each chronic condition, thus limiting the generalizability of the findings. Many of the included studies had small sample sizes, which hindered researchers’ ability to detect statistically significant changes. The total dose of yoga practice varied across studies and only included supervised minutes due to the lack of description of the total minutes of home practice. Intensity of yoga is another important variable affecting the efficacy of the exercise. However, due to the diverse set of chronic conditions with numerous confounders combined with a lack of description of the intensity, we could not quantify this variable. Nevertheless, our analysis of total dose showed an impact on inflammation based on number of supervised minutes, alone.
Conclusion
Our findings support the premise that yoga may positively impact inflammatory pathways and the symptoms of existing inflammatory disease. Yoga is a viable mind–body therapy available to nursing clinicians and researchers for use across patients with a variety of chronic conditions. The National Institute of Nursing Research’s symptom science model supports the integration of biomarkers into clinical applications such as intervention-based research (Cashion & Grady, 2015; Grady, 2017). Nurses have a long history of focusing on health promotion, understanding the underlying mechanisms of diseases, and designing nonpharmacological interventions. The present review suggests that yoga using adaptive postures and props is a promising option for individuals with chronic inflammatory conditions. The combination of postures, slow-breathing techniques, and higher doses of yoga practice may be particularly advantageous in reducing inflammation in chronic conditions.
Acknowledgments
The authors gratefully acknowledge Alissa Fial, MA, MLIS, Education and Research Services Librarian, Supervisor, Circulation Services, McGoogan Library of Medicine, University of Nebraska Medical Center, Omaha, Nebraska, for her professional literature search guidance and assistance with this manuscript.
Footnotes
Author Contributions: Dilorom M. Djalilova contributed to conception and design, acquisition, analysis, and interpretation; drafted the manuscript; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Paula S. Schulz contributed to conception and design, analysis and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Ann M. Berger contributed to analysis and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Adam J. Case contributed to analysis and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Kevin A. Kupzyk contributed to analysis and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Alyson C. Ross contributed to analysis and interpretation; critically revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by the Intramural Research Program of the NIH Clinical Center.
References
- Ben-Neriah Y., Karin M. (2011). Inflammation meets cancer, with NF-κB as the matchmaker. Nature Immunology, 12, 715–723. doi:10.1038/ni.2060 [DOI] [PubMed] [Google Scholar]
- Bower J., Greendale G., Crosswell A., Garet D., Sternlieb B., Ganz P.…Cole S. (2014). Yoga reduces inflammatory signaling in fatigued breast cancer survivors: A randomized controlled trial. Psychoneuroendocrinology, 43, 20–29. doi:10.1016/j.psyneuen.2014.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower J., Irwin M. (2016). Mind–Body therapies and control of inflammatory biology: A descriptive review. Brain, Behavior, and Immunity, 51, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashion A. K., Grady P. A. (2015). The National Institutes of Health/National Institutes of Nursing Research intramural research program and the development of the National Institutes of Health symptom science model. Nursing Outlook, 63, 484–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H. K., Moon W., Kim J. (2015). Effects of yoga on stress and inflammatory factors in patients with chronic low back pain: A non-randomized controlled study. European Journal of Integrative Medicine, 7, 118–123. doi:10.1016/j.eujim.2014.10.008 [Google Scholar]
- Choy E. (2012). Understanding the dynamics: Pathways involved in the pathogenesis of rheumatoid arthritis. Rheumatology, 51, v3–v11. [DOI] [PubMed] [Google Scholar]
- Chu P., Gotink R. A., Yeh G. Y., Goldie S. J., Hunink M. M. (2016). The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. European Journal of Preventive Cardiology, 23, 291–307. [DOI] [PubMed] [Google Scholar]
- Clarke T. C., Black L. I., Stussman B. J., Barnes P. M., Nahin R. L. (2015). Trends in the use of complementary health approaches among adults: United States, 2002-2012. National Health Statistics Reports, 79, 1–16. [PMC free article] [PubMed] [Google Scholar]
- Franceschi C., Campisi J. (2014). Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 69, S4–S9. [DOI] [PubMed] [Google Scholar]
- Gabay C., Kushner I. (1999). Acute-phase proteins and other systemic responses to inflammation. New England Journal of Medicine, 340, 448–454. [DOI] [PubMed] [Google Scholar]
- Grady P. A. (2017). Advancing science, improving lives: NINR’s new strategic plan and the future of nursing science. Journal of Nursing Scholarship, 49, 247–248. [DOI] [PubMed] [Google Scholar]
- Harkess K. N. (2016). The effect of a hatha yoga practice on factors related to chronic stress [Combined Doctor of philosophy/master of psychology dissertation]. doi:10.4225/55/58ae1dfe11248 [Google Scholar]
- Harkess K. N., Ryan J., Delfabbro P. H., Cohen-Woods S. (2016). Preliminary indications of the effect of a brief yoga intervention on markers of inflammation and DNA methylation in chronically stressed women. Translational Psychiatry, 6, e965 doi:10.1038/tp.2016.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins M., Belalcazar L. M., Schelbert K. B., Richardson C., Ballantyne C. M., Kriska A. (2012). The effect of various intensities of physical activity and chronic inflammation in men and women by diabetes status in a national sample. Diabetes Research and Clinical Practice, 97, e6–e8. doi:10.1016/j.diabres.2012.03.019 [DOI] [PubMed] [Google Scholar]
- Hunter C. A., Jones S. A. (2015). IL-6 as a keystone cytokine in health and disease. Nature Immunology, 16, 448–457. [DOI] [PubMed] [Google Scholar]
- Iyengar B. K. S. (1994). Light on yoga. New York, NY: Schocken Books. [Google Scholar]
- Jenny N. S., Cushman M. (2014). C-reactive protein: Initiator or product of inflammation? Circulation Research, 114, 596–597. doi:10.1161/CIRCRESAHA.114.303216 [DOI] [PubMed] [Google Scholar]
- Kaptoge S., Seshasai S. R. K., Gao P., Freitag D. F., Butterworth A. S., Borglykke A.…Lowe G. D. (2013). Inflammatory cytokines and risk of coronary heart disease: New prospective study and updated meta-analysis. European Heart Journal, 35, 578–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J. K., Bennett J. M., Andridge R., Peng J., Shapiro C. L., Malarkey W. B.…Glaser R. (2014). Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: A randomized controlled trial. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 32, 1040–1049. doi:10.1200/JCO.2013.51.8860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakkireddy D., Atkins D., Pillarisetti J., Ryschon K., Bommana S., Drisko J.…Dawn B. (2013). Effect of yoga on arrhythmia burden, anxiety, depression, and quality of life in paroxysmal atrial fibrillation: The YOGA my heart study. Journal of the American College of Cardiology, 61, 1177–1182. [DOI] [PubMed] [Google Scholar]
- Libby P., Ridker P. M., Maseri A. (2002). Inflammation and atherosclerosis. Circulation, 105, 1135–1143. [DOI] [PubMed] [Google Scholar]
- Liu C. H., Abrams N. D., Carrick D. M., Chander P., Dwyer J., Hamlet M. R. J.…Vedamony M. M. (2017). Biomarkers of chronic inflammation in disease development and prevention: Challenges and opportunities. Nature Immunology, 18, 1175–1180. doi:10.1038/ni.3828 [DOI] [PubMed] [Google Scholar]
- McInnes I. B., Schett G. (2011). The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365, 2205–2219. [DOI] [PubMed] [Google Scholar]
- Michaud M., Balardy L., Moulis G., Gaudin C., Peyrot C., Vellas B.…Nourhashemi F. (2013). Proinflammatory cytokines, aging, and age-related diseases. Journal of the American Medical Directors Association, 14, 877–882. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G., & Preferred Reporting Items for Systematic Reviews and Meta-Analysis Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D. C., Spring B., Freedland K. E., Beckner V., Arean P., Hollon S. D.…Kaplan R. (2009). The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychotherapy and Psychosomatics, 78, 275–284. doi:10.1159/000228248 [DOI] [PubMed] [Google Scholar]
- Morgan N., Irwin M. R., Chung M., Wang C. (2014). The effects of mind-body therapies on the immune system: Meta-analysis. PLoS One, 9, e100903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mourya M., Mahajan A. S., Singh N. P., Jain A. K. (2009). Effect of slow- and fast-breathing exercises on autonomic functions in patients with essential hypertension. Journal of Alternative and Complementary Medicine, 15, 711–717. [DOI] [PubMed] [Google Scholar]
- NIH: National Heart, Lung, and Blood Institute. (2018). Quality assessment tool for before-after (pre-post) studies with no control group. Retrieved from https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/before-after
- Nimmo M., Leggate M., Viana J., King J. (2013). The effect of physical activity on mediators of inflammation. Diabetes, Obesity and Metabolism, 15, 51–60. [DOI] [PubMed] [Google Scholar]
- Nozik-Grayck E., Suliman H. B., Piantadosi C. A. (2005). Extracellular superoxide dismutase. International Journal of Biochemistry & Cell Biology, 37, 2466–2471. [DOI] [PubMed] [Google Scholar]
- Parma D. L., Hughes D. C., Ghosh S., Li R., Treviño-Whitaker R. A., Ogden S. M., Ramirez A. G. (2015). Effects of six months of yoga on inflammatory serum markers prognostic of recurrence risk in breast cancer survivors. SpringerPlus, 4, 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil S. G., Aithala M. R., Das K. K. (2015). Effect of yoga on arterial stiffness in elderly subjects with increased pulse pressure: A randomized controlled study. Complementary Therapies in Medicine, 23, 562–569. [DOI] [PubMed] [Google Scholar]
- Pawelec G., Goldeck D., Derhovanessian E. (2014). Inflammation, ageing and chronic disease. Current Opinion in Immunology, 29, 23–28. [DOI] [PubMed] [Google Scholar]
- Pullen P. R., Nagamia S. H., Mehta P. K., Thompson W. R., Benardot D., Hammoud R.…Khan B. V. (2008). Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. Journal of Cardiac Failure, 14, 407–413. doi:10.1016/j.cardfail.2007.12.007 [DOI] [PubMed] [Google Scholar]
- Pullen P. R., Thompson W. R., Benardot D., Brandon L. J., Mehta P. K., Rifai L.…Khan B. V. (2010). Benefits of yoga for African American heart failure patients. Medicine and Science in Sports and Exercise, 42, 651–657. doi:10.1249/MSS.0b013e3181bf24c4 [DOI] [PubMed] [Google Scholar]
- Rajbhoj P. H., Shete S. U., Verma A., Bhogal R. S. (2015). Effect of yoga module on pro-inflammatory and anti-inflammatory cytokines in industrial workers of Lonavla: A randomized controlled trial. Journal of Clinical and Diagnostic Research, 9, CC01–CC05. doi:10.7860/JCDR/2015/11426.5551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao R. M., Vadiraja H., Nagaratna R., Gopinath K., Patil S., Diwakar R. B.…Nagendra H. (2017). Effect of yoga on sleep quality and neuroendocrine immune response in metastatic breast cancer patients. Indian Journal of Palliative Care, 23, 253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross A., Thomas S. (2010). The health benefits of yoga and exercise: A review of comparison studies. Journal of Alternative and Complementary Medicine, 16, 3–12. [DOI] [PubMed] [Google Scholar]
- Sarvottam K., Magan D., Yadav R. K., Mehta N., Mahapatra S. C. (2013). Adiponectin, interleukin-6, and cardiovascular disease risk factors are modified by a short-term yoga-based lifestyle intervention in overweight and obese men. Journal of Alternative and Complementary Medicine, 19, 397–402. doi:10.1089/acm.2012.0086 [DOI] [PubMed] [Google Scholar]
- Shete S. U., Verma A., Kulkarni D. D., Bhogal R. S. (2017). Effect of yoga training on inflammatory cytokines and C-reactive protein in employees of small-scale industries. Journal of Education and Health Promotion, 6, 76 doi:10.4103/jehp.jehp_65_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh V. K., Bhandari R. B., Rana B. B. (2011). Effect of yogic package on rheumatoid arthritis. Indian Journal of Physiology and Pharmacology, 55, 329–335. [PubMed] [Google Scholar]
- Sohl S. J., Danhauer S. C., Birdee G. S., Nicklas B. J., Yacoub G., Aklilu M., Avis N. E. (2016). A brief yoga intervention implemented during chemotherapy: A randomized controlled pilot study. Complementary Therapies in Medicine, 25, 139–142. doi:10.1016/j.ctim.2016.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinchieri G. (2012). Cancer and inflammation: An old intuition with rapidly evolving new concepts. Annual Review of Immunology, 30, 677–706. [DOI] [PubMed] [Google Scholar]
- Vijayaraghava A., Doreswamy V., Narasipur O. S., Kunnavil R., Srinivasamurthy N. (2015). Effect of yoga practice on levels of inflammatory markers after moderate and strenuous exercise. Journal of Clinical and Diagnostic Research, 9, CC08–CC12. doi:10.7860/JCDR/2015/12851.6021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff M., Memon A. A., Chalmers J. P., Sundquist K., Midlov P. (2015). Yoga’s effect on inflammatory biomarkers and metabolic risk factors in a high risk population—A controlled trial in primary care. BMC Cardiovascular Disorders, 15, 91 doi:10.1186/s12872-015-0086-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav R. K., Magan D., Mehta N., Sharma R., Mahapatra S. C. (2012). Efficacy of a short-term yoga-based lifestyle intervention in reducing stress and inflammation: Preliminary results. Journal of Alternative and Complementary Medicine, 18, 662–667. doi:10.1089/acm.2011.0265 [DOI] [PubMed] [Google Scholar]
- Yates S., Morley S., Eccleston C., Williams A. (2005). A scale for rating the quality of psychological trials for pain. Pain, 117, 314–325. [DOI] [PubMed] [Google Scholar]