To the Editor:
Hospitalizations for acute exacerbation of chronic obstructive pulmonary disease (COPD) result in significant respiratory morbidity and account for two-thirds of the healthcare costs associated with the disease (1). After hospitalization, the 30-day readmission rate is approximately 20% (2). In 2014, the Centers for Medicare and Medicaid Services initiated penalties of up to 3% of Medicare reimbursement for 30-day readmission rates that are over the historic rate. In response to this, a number of hospitals have initiated multidisciplinary interventions targeted at reducing hospital readmissions, with minimal to modest success (2–4). These interventions have included varying combinations of discharge planning, frequent phone calls, close follow-up, smoking cessation, inhaler training, and social support. In this regard, pulmonary rehabilitation (PR) is associated with a 56% reduction in hospital readmission over a median duration of 9 months after discharge (5), but access to PR remains poor (6, 7). We hypothesized that early application of a video telehealth PR intervention would reduce 30-day all-cause readmission rates after hospitalization for a COPD exacerbation. Some of the results of this study have been previously reported in the form of an abstract (8).
Methods
Study design
We enrolled patients who had been hospitalized for an acute exacerbation of COPD in a video telehealth PR intervention at a single quaternary care academic hospital from March 2015 onward. Potential participants were identified by means of a daily hospital census, and patients were approached for enrollment irrespective of disease severity, except for those with unstable arrhythmias, congestive heart failure with a left ventricular ejection fraction of <25%, receiving mechanical ventilation, oxygen requirement of >5 L/min at rest, or other comorbidities that precluded participation in exercise, including orthopedic conditions and severe dementia. Written informed consent was obtained from all telehealth participants. Participants exposed to telehealth PR were retrospectively matched 1:2 by readmission risk with contemporaneous subjects who had been hospitalized for a COPD exacerbation but did not receive the telehealth PR intervention. Readmission risk was calculated using the LACE (length of stay, acuity of admission, comorbidities, and emergency room visits in the previous 6 months) index for predicting early mortality or unplanned readmission after discharge from the hospital (9). All participants received a comprehensive bundled care for readmission reduction during hospitalization and after discharge that was comprised of a uniform duration of 5 days of systemic steroids and antibiotics, disease management education, follow-up in the COPD clinic within 10 ± 2 days, smoking cessation counseling when applicable, home health or palliative care when suitable, and referrals to traditional PR (2). All participants received phone calls within 2 days of discharge via an automated telephone system (Emmi Solutions, LLC) to inquire about symptoms, use of inhalers, physical activity, diet and nutrition, vaccines, disease management, and smoking cessation. Any deterioration in a patient’s symptoms was relayed to the healthcare providers for appropriate action (2).
Telehealth PR intervention
Participants were enrolled at index hospitalization, and on return to the COPD clinic within 10 ± 2 days were provided a data-enabled smartphone with video capabilities to facilitate two-way live videoconferencing using a Health Insurance Portability and Accountability Act–compliant application. The intervention consisted of a standardized regimen of 36 exercise sessions over 12 weeks per traditional PR guidelines (10). Exercise was prescribed by an exercise physiologist after an initial outpatient exercise assessment and tailored according to the subject’s baseline functional level as well as impairment before the exacerbation (11). The exercise regimen included a combination of initial stretching and breathing exercises, followed by 20 minutes of aerobic exercises using a portable foot pedaler provided as part of the study to achieve heart rates between 60% and 80% of the maximum recorded on the baseline 6-minute-walk test. Other types of equipment, such as treadmills and exercise bikes, were used when available. Resistance training was done with the use of a resistance band. In addition, breathing exercises such as pursed-lips breathing, paced breathing, diaphragmatic muscle strength training, and basic yoga exercises were administered. Educational sessions were also included in the videoconference calls regarding smoking cessation, appropriate inhaler techniques, disease education, monitoring and reporting exacerbations, and self-efficacy. Safety was monitored by providing automatic sphygmomanometers to measure blood pressure before and after exercise, and a pulse oximeter was used to assess heart rate and oxygen saturation. Long-term recommendations for exercise were made at the time of graduation from PR. Subjects who participated in at least 20 sessions were considered completers (10, 12).
Outcomes
The primary outcome was the 30-day all-cause readmission rate, and secondary outcomes included 30-day readmissions due to acute exacerbation of COPD, and time to first readmission due to any cause.
Statistical analyses
Proportions of readmission within 30 days were compared between the exposed and unexposed groups using the chi-square test. The time to first readmission was compared between groups using Kaplan-Meier and Cox proportional hazards analyses. All analyses were performed using SPSS v22.0 (SPSS Inc.), and a two-tailed α of 0.05 was deemed statistically significant.
Results
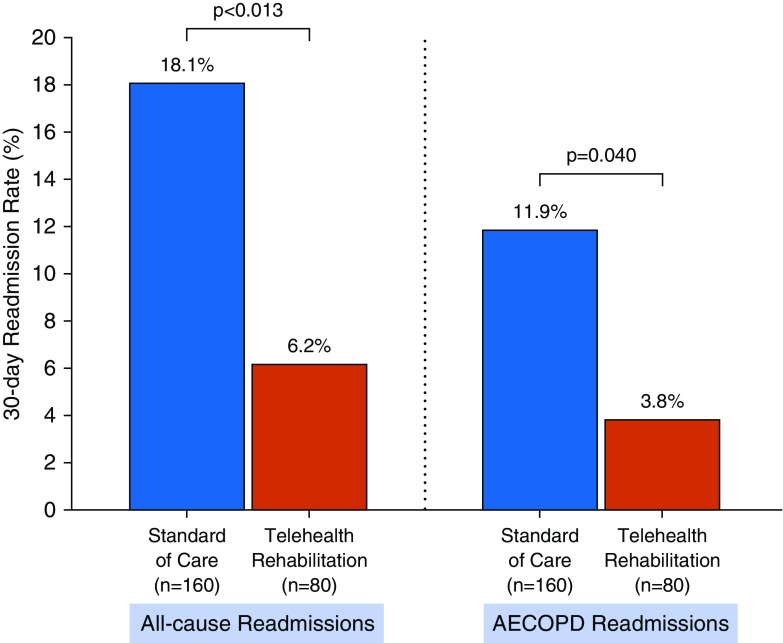
Eighty participants were enrolled in telehealth PR and matched with 160 unexposed subjects (Table 1). The two groups had similar demographics and comorbidities, but a greater proportion of telehealth patients were on domiciliary oxygen. The 30-day all-cause readmission rate was significantly lower in the telehealth PR group than in the unexposed group (6.2% vs. 18.1%; P = 0.013) (Figure 1). Thirty-day readmissions due to acute exacerbation of COPD were also lower in the telehealth PR group (3.8%) than in the unexposed group (11.9%, P = 0.040). The time to first readmission was longer in individuals who received telehealth PR than in those who did not (265 d [95% confidence interval (CI), 235–295 d] vs. 211 d [95% CI, 187–233 d]; unadjusted hazards ratio, 0.60; 95% CI, 0.40–0.90; P = 0.012). No adverse events were reported with telehealth PR, and 66 subjects (82.5%) completed at least 20 sessions of telehealth PR, resulting in an attrition rate of 17.5%. Forty-two of the 160 unexposed subjects (26%) were referred to traditional PR after discharge. Ten subjects (6%) enrolled in traditional PR within 3 months of discharge, and two of these subjects were already participating in PR at the time of admission. Of these, only eight (5%) enrolled in traditional PR within a month of discharge, and three completed at least 20 sessions.
Table 1.
Baseline Characteristics of Patients in the Video Telehealth Pulmonary Rehabilitation and Unexposed Arms
| Telehealth PR (n = 80) | Unexposed (n = 160) | |
|---|---|---|
| Age, yr | 64.5 (10.1) | 63.4 (11.8) |
| Sex, F | 49 (61.3%) | 92 (57.5%) |
| Race, African American | 26 (32.5%) | 57 (35.6%) |
| Body mass index, kg/m2 | 29.0 (10.2) | 28.2 (8.2) |
| Current smoker | 21 (26.3%) | 60 (37.5%) |
| FEV1% predicted* | 45.4 (18.1) | 48.6 (21.1) |
| FEV1/FVC* | 0.52 (0.15) | 0.57 (0.15) |
| Domiciliary oxygen use | 43 (53.8%) | 44 (27.5%) |
| Coronary artery disease | 16 (20.0%) | 31 (19.4%) |
| Atrial fibrillation | 8 (10.0%) | 13 (8.1%) |
| Congestive heart failure | 10 (12.5%) | 24 (15.0%) |
| Hypertension | 55 (68.8%) | 111 (69.4%) |
| Diabetes mellitus | 22 (27.5%) | 46 (28.8%) |
| Depression | 16 (20.0%) | 40 (25.0%) |
| Anxiety | 15 (18.8%) | 32 (20.0%) |
| Hospitalizations in prior 12 mo | 0.9 (1.4) | 0.9 (1.7) |
| ER visits in prior 6 mo | 1.0 (1.5) | 0.7 (1.4) |
| Length of stay, d† | 4 (2) | 4 (3) |
| LACE index | 10.7 (2.8) | 10.6 (3.0) |
Definition of abbreviations: ER = emergency room; LACE = length of stay, acuity of admission, comorbidities, and ER visits in the previous 6 months; PR = pulmonary rehabilitation.
All data are expressed as mean (SD) or n (%) unless otherwise stated.
Spirometry data were available for 77 intervention and 94 control subjects.
Median (interquartile range).
Figure 1.
Comparison of 30-day readmission rates for all causes and for acute exacerbation of chronic obstructive pulmonary disease (AECOPD) after an index admission for AECOPD.
Discussion
We demonstrate that a video telehealth PR intervention administered early after hospitalization for an acute exacerbation of COPD is feasible and safe and is associated with significantly lower 30-day all-cause readmission rates.
To our knowledge, this is the first active telehealth intervention to be associated with a significant reduction in 30-day all-cause readmission rates in COPD. Previous multidisciplinary interventions targeting 30-day readmissions have either failed or shown modest success. Jennings and colleagues randomized hospitalized patients with COPD to usual care or a predischarge bundle and found no difference in 30-day readmission rates (3). However, they assessed only readmissions due to acute exacerbations of COPD, and not all-cause readmissions, which is the target for the Centers for Medicare and Medicaid Services Hospital Readmissions Reduction Program. A retrospective study of a comprehensive care plan comprised of smoking cessation and inhaler education; pulmonary consultation; comorbidity assessment; palliative care assessment; mucus clearance device and inhaler selection based on clinical assessment of patient dexterity, competence, and peak inspiratory flow; and close outpatient follow-up showed a 16% reduction in all-cause readmissions (4). However, a similar multidisciplinary bundle of interventions developed by our group did not result in a reduction in all-cause readmission rates (6). These data suggest that interventions based on monitoring patients’ symptoms or physiologic signs, and triggering alerts that result in using existing medications to treat exacerbations early are not sufficient to reduce readmissions. The mechanisms by which early telehealth PR reduced readmissions requires more research, but PR increases patients’ physical, psychological, and social resilience as a result of improved exercise capacity, reduced sensitivity to dyspnea, improved mood, and greater self-efficacy, and a combination of these effects likely increases the symptomatic threshold for an exacerbation (13).
Our study has some limitations. Although we matched individuals by readmission risk, the participants were not randomized, and this can introduce bias. The LACE index has moderate discrimination for readmission risk in COPD but is commonly used for all-cause readmission risk assessments (14). Although the subjects were matched by readmission risk, the possibility of residual confounding cannot be excluded. We recorded all readmissions in the intervention group, but it is possible we missed readmissions at other hospitals in the control arm. This would, however, only bias the results in favor of the intervention. These results require confirmation with a randomized controlled trial.
Supplementary Material
Footnotes
Supported by grants from the University of Alabama at Birmingham Health Services Foundation Grant and the National Institute of Child Health and Human Development (1P2CHD086851). S.P.B. is supported by NIH grant K23HL133438.
Author Contributions: S.P.B. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: S.P.B. and M.T.D. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: S.P.B. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: S.P.B. Study supervision: all authors.
Originally Published in Press as DOI: 10.1164/rccm.201902-0314LE on April 12, 2019
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Elixhauser A, Au DH, Podulka J. Healthcare Cost and Utilization Project (HCUP) statistical briefs. Rockville, MD: Agency for Healthcare Research and Quality (US); 2011 Sep. Readmissions for chronic obstructive pulmonary disease, 2008: statistical brief #121. [accessed 2019 Feb 10]. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb121.pdf. [PubMed] [Google Scholar]
- 2.Bhatt SP, Wells JM, Iyer AS, Kirkpatrick DP, Parekh TM, Leach LT, et al. Results of a medicare bundled payments for care improvement initiative for chronic obstructive pulmonary disease readmissions. Ann Am Thorac Soc. 2017;14:643–648. doi: 10.1513/AnnalsATS.201610-775BC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jennings JH, Thavarajah K, Mendez MP, Eichenhorn M, Kvale P, Yessayan L. Predischarge bundle for patients with acute exacerbations of COPD to reduce readmissions and ED visits: a randomized controlled trial. Chest. 2015;147:1227–1234. doi: 10.1378/chest.14-1123. [DOI] [PubMed] [Google Scholar]
- 4.Ohar JA, Loh CH, Lenoir KM, Wells BJ, Peters SP. A comprehensive care plan that reduces readmissions after acute exacerbations of COPD. Respir Med. 2018;141:20–25. doi: 10.1016/j.rmed.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005305. doi: 10.1002/14651858.CD005305.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatt SP. It’s time to rehabilitate pulmonary rehabilitation. Ann Am Thorac Soc. 2019;16:55–57. doi: 10.1513/AnnalsATS.201809-641ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spitzer KA, Stefan MS, Priya A, Pack QR, Pekow PS, Lagu T, et al. Participation in pulmonary rehabilitation after hospitalization for COPD among Medicare beneficiaries. Ann Am Thorac Soc. 2019;16:99–106. doi: 10.1513/AnnalsATS.201805-332OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhatt SP, Sanders JG, Anderson EM, Baugh D, Schumann CD, Wells JM, et al. Telehealth exercise intervention reduces COPD readmissions [abstract] Am J Respir Crit Care Med. 2018;197:A4545. [Google Scholar]
- 9.van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. ATS/ERS Pulmonary Rehabilitation Writing Committee. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–1413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 11.Madden RH, Dune T, Lukersmith S, Hartley S, Kuipers P, Gargett A, et al. The relevance of the International Classification of Functioning, Disability and Health (ICF) in monitoring and evaluating community-based rehabilitation (CBR) Disabil Rehabil. 2014;36:826–837. doi: 10.3109/09638288.2013.821182. [DOI] [PubMed] [Google Scholar]
- 12.Brown AT, Hitchcock J, Schumann C, Wells JM, Dransfield MT, Bhatt SP. Determinants of successful completion of pulmonary rehabilitation in COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:391–397. doi: 10.2147/COPD.S100254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spruit MA, Franssen FM, Rutten EP, Wopereis S, Wouters EF, Vanfleteren LE. A new perspective on COPD exacerbations: monitoring impact by measuring physical, psychological and social resilience. Eur Respir J. 2016;47:1024–1027. doi: 10.1183/13993003.01645-2015. [DOI] [PubMed] [Google Scholar]
- 14.Hakim MA, Garden FL, Jennings MD, Dobler CC. Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin Epidemiol. 2017;10:51–59. doi: 10.2147/CLEP.S149574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.