Abstract
Objective
To evaluate the effectiveness of a brief mindfulness intervention on hand hygiene performance and mindful attention for inpatient physician teams.
Design
A pilot, pretest-posttest randomized controlled mixed methods trial.
Setting
One academic medical center in the U.S.
Participants
Four internal medicine physician teams consisting of one attending, one resident, two to three interns, and up to four medical students.
Intervention
A facilitated, group-based educational discussion on how mindfulness, as practiced through mindful hand hygiene, may improve clinical care and practices in the hospital setting.
Main Outcomes and Measures
The primary outcome was hand hygiene adherence (percentage) for each patient encounter. Other outcomes were observable mindful moments and mindful attention, measured using the Mindfulness Attention Awareness Scale, from baseline to post-intervention, and qualitative evaluation of the intervention.
Results
For attending physicians, hand hygiene adherence increased 14.1% in the intervention group compared to a decrease of 5.7% in the controls (p = 0.035). For residents, the comparable figures were 24.7% (intervention) versus 0.2% (control) (p = 0.064). For interns, adherence increased 10.0% with the intervention versus 4.2% in the controls (p = 0.007). For medical students, adherence improved more in the control group (4.7% intervention vs. 7.7% controls; p = 0.003). An increase in mindfulness behaviors was observed for the intervention group (3.7%) versus controls (0.9%) (p = 0.021). Self-reported mindful attention did not change (p = 0.865).
Conclusions
A brief, education-based mindfulness intervention improved hand hygiene in attending physicians and residents, but not in medical students. The intervention was well-received, increased mindfulness practice, and appears to be a feasible way to introduce mindfulness in the clinical setting. Future work instructing clinicians in mindfulness to improve hand hygiene may prove valuable.
Introduction
Hand hygiene is broadly accepted as an integral component for preventing infection in hospitalized patients.1 Unfortunately, healthcare provider adherence to hand hygiene practices are relatively low, even when education programs for hand hygiene are well-resourced and well-coordinated.2–4 Of note, hand hygiene adherence is known to be lower among physicians than nurses,5–7 and before patient encounters relative to after.2,7 Although myriad strategies including education, feedback, and incentives have been implemented to encourage hand hygiene, most have had only transient or modest impact.8 Therefore, innovative strategies are needed to improve hand hygiene among healthcare providers.9
The practice of mindfulness is described as paying attention in the present moment, in a purposeful and non-judgmental way.10 Mindfulness is meant to help move a person from a state where thoughts are unobserved and actions are on automatic pilot, to a state where situations are observed, acknowledged, and accepted. A recent systematic review found that brief mindfulness interventions aimed at healthcare providers improve myriad clinical outcomes.11 Teaching healthcare providers informal practices, such as mindful hand hygiene, could similarly bring mindfulness into clinical practice. Further, the role modeling of mindful hand hygiene within a clinical setting may have a cascading effect on others. This group effect could lead to collective mindfulness,12 where the behavior of peers affects others to improve hand hygiene rates of others.7,9 Adoption of mindful practice, in turn, may have other benefits including enhanced attention,13 situational awareness,14 provider well-being,10 and reduction of diagnostic medical errors by addressing cognitive biases.15
We sought to assess if mindful hand hygiene would promote hand hygiene adherence and mindful attention among physicians and medical students in a hospital setting. We selected physicians in particular for hand hygiene compliance among physicians lags behind that of most other professional groups.6 Using a pilot, randomized controlled mixed methods trial, we examined the effectiveness of a brief, mindfulness educational session on hand hygiene adherence and mindful attention for inpatient physician teams. This proof of concept intervention sought to understand whether physicians were receptive to mindfulness as a means to improve hand hygiene. We hypothesized that participants exposed to mindfulness would exhibit increased hand hygiene and mindfulness behaviors compared to those randomized to the control group.
METHODS
Study Design, Setting, and Participants
We designed a pretest-posttest randomized controlled mixed methods trial at a tertiary care health system. Participants were attending physicians, residents, interns and medical students, who were recruited and enrolled by a research coordinator from inpatient, internal medicine teaching teams in February and March 2016. Morning rounds on the medical wards were selected as they are a key part of daily clinical care where most medical decisions are made. Rounds are also a time when senior physicians role model group norms, set expectations, and outline best practices to physicians in training.16 All team members provided written informed consent to be part of the two-week study.
Baseline Measures
Baseline rates of hand hygiene before and after patient room entry for each member of the team on the medicine wards were collected using a standardized, secret shopper auditing approach.17 Five observers with previous experience observing hand hygiene adherence (3 research specialists, two students) received training regarding the established recommendations for hand hygiene auditing (i.e., type of hand hygiene performed, upon entry and exit of patient room, and when to document “unknown”) (Online Supplement 1).18 Additional training was provided regarding the observation of mindfulness behaviors, which were identified in two ways: first, if a person paused from walking, talking, or engaging with their environment and appeared to focus on the process of rubbing soap/gel into hands and, second, when a person was noted to take multiple, slow, deliberate breaths while performing hand hygiene.10 Observers were instructed to document “unknown” if they were unable to observe or unsure that they witnessed mindful behavior. Baseline observations occurred for five weekdays, during morning rounds (2–4 hours), on acute care medicine units. No new hand hygiene programs were being introduced in the organization during this timeframe.
To measure self-reported mindfulness before and after the intervention, all participants completed the Mindfulness Attention Awareness Scale (MAAS) at baseline. The MAAS13 is a validated 15-item scale that focuses on the self-regulation of attention aspect of mindfulness. The MAAS was selected over other mindfulness measures19 due to the brevity of the scale13 and prior use with healthcare providers.20–23 The MAAS survey items ask respondents to indicate the frequency with which they experience various behaviors related to mindfulness, ranging from one (almost always) to six (almost never). Higher scores reflect higher levels of mindful attention.
Randomization
Following baseline evaluation, an independent statistician allocated teaching teams to either the intervention or control group in a concealed fashion using an allocation ratio of 1:1 derived from SAS™. Each team contained eight participants (i.e., one attending, one resident, two to three interns, three to four medical students). Hand hygiene observers were blinded to allocation. Following randomization, the teams were observed for hand hygiene adherence and mindfulness behaviors for another five weekdays during morning rounds (2–4 hours each day). At the completion of the second period of observations, both teams were invited to re-take the MAAS survey and provide feedback on the intervention through individual interviews and focus groups.
Intervention
The intervention consisted of two components: first, a brief 10-minute informational video entitled, “All it Takes is 10 Mindful Minutes” by mindfulness expert, Andy Puddicombe was shown.24 Following the video presentation, the primary investigator (retracted) led a 60-minute guided discussion on how he uses principles of mindfulness to generate reflective pauses while providing clinical care. The primary investigator shared personal anecdotes and clinical examples of instances where stopping to be aware of his physical and emotional state influenced decision-making, patient care and outcomes. Because it is difficult to find moments to practice mindfulness during busy clinical days, hand hygiene was offered as a prompt to pause, take a few deep breaths and attend to the flow of thoughts in one’s mind before entering a patient’s room. During this pause, a moment to reflect, crystallize thoughts, and visualize what may happen in the encounter while acknowledging and accepting internal emotions or feelings was suggested. Participants were given a guide for a moment of mindfulness during hand hygiene (Online Supplement 2).9 The discussion then turned to the group who shared their experiences and asked question about integrating this into their clinical practice. The control group did not receive the brief mindfulness education session and continued with usual care.
Main Outcomes
The primary study outcome was hand hygiene adherence (yes/no) as blindly observed from an independent observer for each encounter with a patient. Other outcomes of interest were observable mindful moments as recorded by the independent observer for each patient encounter and MAAS scores from baseline to post-intervention.
Statistical Analysis
Differences in baseline hand hygiene adherence, mindfulness behaviors, and MAAS scores between intervention and control groups were assessed using Fisher’s exact and t-tests, as appropriate. Risk differences in adherence to hand hygiene from baseline to post-intervention were calculated for both intervention and control groups. Similarly, risk differences from baseline to post-intervention were computed for mindfulness behavior, stratified by intervention/control group. Because the primary outcome (i.e., hand hygiene) occurred frequently, we utilized generalized linear models to evaluate pre-post changes in hand hygiene adherence for the intervention versus control group, with the Poisson distribution (log link) and robust error variance, incorporating clustering by teaching team.25 Statistical significance was calculated for the interaction term for time (pre-post) and intervention (intervention versus control), stratified by physician type. A similar approach was used to assess mindfulness behavior. For MAAS scores, a generalized linear model was used with a normal distribution and an identity link, with an interaction term to assess time*intervention, clustered by teaching team. All statistical tests were two-sided, with p < 0.05 considered statistically significant. All analyses were conducted using Stata v14 (StataCorp, College Station, TX).
Qualitative Evaluation of the Intervention
To enhance our understanding of mindfulness, hand hygiene practices and the MAAS survey results,26 we conducted focus groups and interviews with those randomized to the intervention in accordance with published recommendations.27,28 Focus groups were performed using a semi-structured guide (Online Supplement 3) that aimed to understand how residents, interns, and medical students perceived the intervention and their lived experience of practicing mindfulness during hand hygiene. Similarly, we conducted separate, in-person, one-on-one interviews with attending physicians to understand their experiences and perceptions. Focus groups and interviews were recorded and transcribed. Two qualitative researchers (retracted) independently reviewed the transcripts and conducted a descriptive content analysis. Researchers used a list of preliminary deductive codes to identify and develop additional inductive codes that further explained the data. Differences in coding were resolved through discussion and key themes and quotes from the focus groups and interviews were synthesized to explicate findings.
RESULTS
Study Population
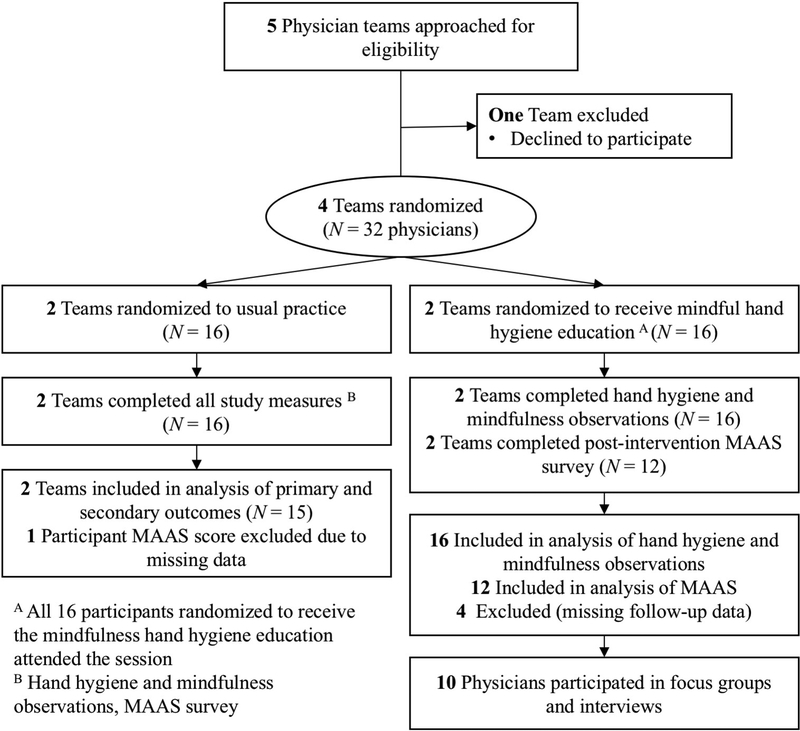
Participant flow in the study is presented in Figure 1. Five physician teams were approached; one team declined to participate owing to high patient volumes. The remaining four physician teams were randomized to two groups (intervention and control). Each team included eight participants. All participants were observed for hand hygiene and mindful behaviors during patient encounters, yielding a total of 1,299 unique hand hygiene observations. For the secondary outcome using the MAAS instrument, four participants randomized to the intervention group did not attend morning rounds when post-intervention surveys were completed, and one participant in the control group did not complete all questions on the MAAS, yielding a final sample of 27 participants for this outcome. A total of six physicians and four medical students participated in the focus groups and interviews following the intervention. Due to the pilot nature of this study, demographic data for the teams (e.g., gender, age) was not collected.
Figure 1.
Study flow diagram. MAAS, Mindfulness Attention Awareness Scale.
At the end of the first week of baseline observations, hand hygiene adherence rates for the intervention and control groups were 72% and 85% (p < 0.001), respectively. At baseline, mindfulness behavior during hand hygiene was observed once (<1% of all observations) for the intervention group and once (<1%) for the control group (p = 0.89). No significant difference in baseline mean MAAS scores between the intervention and control group were observed (4.21 (standard deviation [SD] = 0.70 vs. 3.86 [SD = 0.64], respectively) (p = 0.18). Both groups reported moderately high MAAS scores, similar to results for healthy community dwelling adults (4.20).13
Primary Outcome: Hand Hygiene Adherence
Hand hygiene adherence increased 14.1% from baseline to post-intervention for attending physicians who received the intervention, but decreased by 5.7% in the control group (p =0.035). Similarly, interns who received the intervention increased hand hygiene adherence by 10.0% from baseline to post-intervention compared to a 4.2% increase for interns in the control group, a statistically significant difference (p = 0.007). Residents who received the intervention demonstrated the greatest absolute improvement in hand hygiene practice with a 24.7% increase, while residents in the control group saw no improvement in adherence (0.2%) (p = 0.064). Medical students in both the intervention and control groups increased hand hygiene adherence (4.7% vs. 7.7%, respectively). However, the increase was greater among the controls (p = 0.003) (Table 1).
Table 1.
Hand hygiene and mindfulness moments by intervention group
| Observations | Intervention | Control | P-value | ||||
|---|---|---|---|---|---|---|---|
| N1 | N2 | Change from Baseline % (95% CI) |
N1 | N2 | Change from Baseline % (95% CT) |
||
| Hand Hygiene | |||||||
| Physician type | |||||||
| Attending | 2 | 132 | 14.1 (−1.1, 29.5) | 2 | 113 | −5.7 (−15.9, 4.5) | 0.035 |
| Senior | 2 | 90 | 24.7 (5.4, 44.0) | 2 | 81 | 0.2 (−15.5, 15.9) | 0.064 |
| Resident | |||||||
| Intern | 5 | 136 | 10.0 (−2.6, 22.6) | 5 | 215 | 4.2 (−6.4, 14.9) | 0.007 |
| Medical | 7 | 267 | 4.7 (−4.4, 14.0) | 7 | 265 | 7.7 (0.2, 15.1) | 0.003 |
| Student | |||||||
| Mindful | |||||||
| Moments | |||||||
| Overall | 16 | 621 | 3.7 (1.3, 6.0) | 16 | 662 | 0.9 (−0.4, 2.3) | 0.021 |
Key: N1 = providers; N2 = handwashing events; CI = confidence interval; p = < 0.05
Observed Mindfulness Behaviors and MAAS Results
A 3.7% increase in observed mindfulness behaviors during hand hygiene was recorded for members of the intervention group and a 0.9% increase was observed for members of the control group (p = 0.021) (Table 1). Despite the significant increase in observed mindfulness behaviors with the intervention, no significant changes in MAAS mean scores from baseline to post-intervention were noted for intervention (−0.15; CI = −0.46, 0.76) or control groups (−0.14; CI = −0.40, 0.68; p = 0.865).
Focus Groups and Interviews
A total of two focus groups comprising members of two different teaching teams (N = 8 residents, interns, and medical students) and two interviews (N = 2 attending physicians) were conducted. Key themes related to physician perceptions of mindfulness, how physicians linked hand hygiene to mindfulness, and recommendations for future implementation were identified. No harms or unintended effects were reported by participants.
Physician Perceptions of Mindfulness
In general, all participants were favorable to the idea of the practice of mindfulness in clinical settings. The overwhelming sense was that practicing mindfulness could result in improved physician well-being and consequently, improved doctor-patient relationships.
“…Anything that allows a healthcare provider to just be more present, I don’t know how to say it without sounding hyper corny, but like more emotionally available and open, I think contributes to a much better provider-patient relationship.” (Attending)
“When you survey physicians…the stress levels are just so high. So, to me, mindfulness is a way to help people be happy with what they’re doing…and then you hope that filters into their interactions with patients.” (Attending)
Feedback on Mindfulness Educational Session
Overall, participants reported positive feedback for the content and length of the educational session.
“I thought it was great. I thought some of the positives were that it was relatively brief, which I think is good because unfortunately logistics are always something we have to think about in the clinical day and I thought it was great to be able to get the entire team there to sort of have it at the same time and experience the same thing and it allowed some people to share thoughts on the topic.”(Attending)
“I thought the length of it was appropriate. It didn’t seem too long to incorporate on a busy day. I liked the mix of trying to include personal interaction and then the video. I think if we had just watched the video, it would have felt kind of flat but…the personal remarks added a lot.” (Resident)
Experiences Linking Hand Hygiene and Mindfulness during the Intervention
When asked, seven of the 10 participants said they began to practice mindfulness during hand hygiene following the intervention, indicating feasibility of the practice. Although a moment of hand hygiene for mindfulness was appreciated, maintaining consistency in the practice proved challenging.
“I liked the hand hygiene thing. I thought it was just interesting. I never thought about that as an opportunity to be mindful so it was…one moment that we all experience multiple times a day that we just take a second to think.” (Student)
“I mean it crossed my mind the first couple of days after the session but usually there were three other people behind me and I thought it would be a little strange to just sit there pausing and thinking while everybody waited to go in the patient room.” (Intern)
“I think the challenge is to remember to do it…with all the other things going on, that’s just something that’s easily forgotten and takes a backseat to a lot of the other things that you end up doing.” (Intern)
Recommendations for Increasing Mindfulness during Hand Hygiene
Several participants offered suggestions to improve mindfulness and hand hygiene during clinical practice.
“Attendings are kind of responsible for setting the pace of rounds and so if the attending stands outside the room and finishes washing his or her hands with the sanitizer, the rest of the team may actually pause there with him or her to do that.” (Resident)
“I think before rounds is a better time, like when the whole team is there, either on the floor or in the team room, would be a good time to have a moment of mindfulness.” (Intern)
DISCUSSION
In this pilot randomized controlled study, we found that a brief, education-based mindfulness intervention using hand hygiene was feasible to instruct physicians and medical students on mindfulness in the clinical setting. The intervention appeared to improve hand hygiene rates in physicians, particularly among attendings and interns. Hygiene rates for medical students increased in both intervention and control groups. There was a significant increase in observed and self-reported mindfulness behaviors during hand hygiene in the intervention group, but no significant difference was in the MAAS scale. Qualitative feedback from participants suggested that while they attempted to improve mindfulness behaviors, integrating the practice into clinical rounds was challenging. However, because the physicians and medical students embraced mindfulness within a hand hygiene-based intervention, future work linking mindfulness to hand hygiene practice may prove valuable.
Our study adds to an existing body of literature investigating how mindfulness practice can be a resource for healthcare providers. Two recent publications have proposed mindfulness practice for clinicians as a strategy to increase metacognition and reduce the effects of biases that are associated with diagnostic and other medical errors.15,29 In a review of empirical studies of traditional, 8-week mindfulness-based stress reduction (MBSR) programs for healthcare providers, the evidence suggested that participation in MBSR yields physical and mental health benefits for providers.30 In a systematic review, brief mindfulness interventions modified to fit the schedules of providers positively influenced levels of stress, anxiety, mindfulness, resiliency, and burnout symptoms in hospital-based nurses and physicians.11 Collectively, these studies suggest that mindfulness practice can impact a variety of attributes that could influence patient safety. However, few studies have focused on identifying key factors such as the dose of mindfulness practice required to provide long-term benefits for provider and patients.11,30
Why use hand hygiene as a moment to integrate mindfulness into clinical practice? First, hand hygiene is an activity performed multiple times throughout a day and thus provides defined moments for pause and practice. The data gleaned from participant interviews suggests that physicians are looking for an oasis in time to concentrate and reflect in the midst of patient care. Second, because hand hygiene occurs immediately before and after patient interaction, it was embraced by physicians and medical students in our study as an opportune time to become present and practice self-care. Additionally, collective mindfulness, such that the behavior of attendings influenced others, was also viewed as a benefit of this approach during morning rounds. However, providers also noted that it was challenging to perform mindful hand hygiene at this time due to competing demands. Similarly, concerns about social stigma when practicing mindfulness is a reality that will require leadership and role-modeling by attendings and residents to offset. The suggestion to briefly practice as a group prior to rounds has been previously studied with inpatient nurses21 and resident physicians.31 The approach was reported to be relatively easy to implement and well-received by participants, however the influence on provider and patient outcomes requires further study.
We found no significant change in MAAS scores despite improvement in observed and self-reported mindfulness behaviors. Absence of such findings may relate to the small sample size of this study, compounded by missing data from several participants who did not complete the post-intervention survey assessment. Alternatively, the brief nature of mindful hand hygiene practice introduced in this study may not have been a large enough dose to alter MAAS scores, especially in participants with an inherent predisposition to mindfulness.11 Lastly, relative insensitivity of the scale to small changes in mindful attention may also explain lack of improvement in mindful attention.
Limitations and Strengths
Our study has several limitations. First, ours was a proof of concept study conducted at a single center with a brief observation period and limited follow-up. Multi-center studies that are larger in scale and address the sustainability of the intervention are needed. Second, our study targeted physicians and medical students; whether mindfulness would be effective with nurses and other health professionals is unknown. However, nursing theory32 describes hand hygiene as a self-care practice, suggesting that nurses may be an ideal group to shape organizational and cultural norms and propagate mindful hand hygiene. Third, our study only focused on the effect of mindful practice on hand hygiene during rounds. The impact on hand hygiene moments during other times of the day (or night) are not known. However, team rounds are an integral aspect of clinical care and often include nurses, pharmacists, and patients; thus, making it an ideal time to role model mindful practice.
Our study was also performed in an academic setting where baseline hand hygiene adherence was high. Whether similar findings will be generalizable to other healthcare settings involving different patient and provider populations is unclear. Further, hand hygiene adherence was measured using covert observations. Though an industry standard, hand hygiene practice is reported to increase when clinicians are aware of auditor activity.17 Relatedly, the external observation of a mindful moment is subjective and may have unblinded the intervention group to auditors. Validation of a mindful moment through objective measurement (e.g. devices that measure breathing rate) may prove interesting for future research.
The intervention was 60-minutes in length and included open discussion among peers, perhaps limiting generalizability and scalability to other settings. Finally, although the exact mechanism for the increase in hand hygiene is unclear, the evaluative feedback from physicians exposed to the intervention was encouraging. The reported influence of seeing a senior physician practice mindful hand hygiene suggests the group effect may be an underlying mechanism, as previously suggested in the literature.7,33,34 Though this may not translate to times when individual physicians see patients outside of rounds or in non-academic settings, mindfulness practice through hand hygiene appears feasible and acceptable to attendings, residents, interns and medical students.
Our study also has strengths. First, this was a methodologically rigorous study that used a randomized design with concealed allocation in a real-world setting. Outcomes were recorded by trained observers who were blinded to assignment. Additionally, we used qualitative and observational evaluative techniques to supplement the quantitative data. Due to the known challenges of measuring and observing the construct of mindfulness,26 the use of a mixed methods approach provides insight into how participants viewed the intervention and may have used it in practice. Future studies that focus on the enhancement of well-being,26 the impact on patient safety,15 and the positive effect on others26 of mindful hand hygiene thus appear possible. Third, we found that healthcare providers uniformly appreciated the opportunity to pause and reflect before engaging in patient care. Given rising concerns about provider burnout and well-being, our study suggests that mindfulness may be an option in building physician resilience.
CONCLUSION
A brief mindfulness-based intervention introduced mindfulness in the clinical setting and improved physician hand hygiene rates. Though the exact mechanism for the improvement in hand hygiene is unclear, the intervention was well received by participating medical teams and resulted in self-reported and observed increases in mindfulness practice. Larger trials that test the intervention in diverse settings are needed to determine whether mindful hand hygiene can increase clinician mindfulness, improve hand hygiene practice, influence provider well-being, and ultimately enhance patient safety.
Supplementary Material
Acknowledgements:
The authors wish to thank the physicians who participated in the educational sessions.
Competing Interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work. All authors, external and internal, had full access to all the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Disclaimer Removed to maintain anonymity
Provenance and peer review Not commissioned; externally peer reviewed
Ethical approval Removed to maintain anonymity
Provenance and peer review: Not commissioned; externally peer reviewed.
Trial Registration: ClinicalTrials.gov ID:
Full Trial Protocol: Available upon request from corresponding author
Contributor Information
Heather Gilmartin, Denver/Seattle Center of Innovation for Veteran-Centered and Value Driven Care Denver, CO 80220.
Sanjay Saint, VA Ann Arbor & University of Michigan Health System, Ann Arbor, MI, USA.
Mary Rogers, University of Michigan Health System & VA Ann Arbor, Ann Arbor, MI, USA.
Suzanne Winter, University of Michigan Health System & VA Ann Arbor, Ann Arbor, MI, USA.
Ashley Snyder, University of Michigan Health System & VA Ann Arbor, Ann Arbor, MI, USA.
Martha Quinn, University of Michigan Health System & VA Ann Arbor, Ann Arbor, MI, USA.
Vineet Chopra, University of Michigan Health System & VA Ann Arbor, Ann Arbor, MI, USA.
References
- 1.Ellingson K, Haas JP, Aiello AE, et al. Strategies to prevent healthcare-associated infections through hand hygiene. Infection Control & Hospital Epidemiology 2014;35(S2):S155–S78. doi: 10.1017/S0899823X00193900 [DOI] [PubMed] [Google Scholar]
- 2.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infection Control & Hospital Epidemiology 2010;31(03):283–94. doi: 10.1086/650451 [DOI] [PubMed] [Google Scholar]
- 3.Fuller C, Michie S, Savage J, et al. The Feedback Intervention Trial (FIT) - improving hand-hygiene compliance in UK healthcare workers: A stepped wedge cluster randomised controlled trial. PLoS ONE 2012;7(10):e41617. doi: 10.1371/journal.pone.0041617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayer J, Mooney B, Gundlapalli A, et al. Dissemination and sustainability of a hospital-wide hand hygiene program emphasizing positive reinforcement. Infection Control & Hospital Epidemiology 2011;32(01):59–66. doi: 10.1086/657666 [DOI] [PubMed] [Google Scholar]
- 5.Pittet D, Simon A, Hugonnet S, et al. Hand hygiene among physicians: performance, beliefs, and perceptions. Annals of internal medicine 2004;141(1):1–8. [DOI] [PubMed] [Google Scholar]
- 6.Squires JE, Suh KN, Linklater S, et al. Improving physician hand hygiene compliance using behavioural theories: a study protocol. Implement Sci 2013;8(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kovacs - Litman A, Wong K, Shojania KG, et al. Do physicians clean their hands? Insights from a covert observational study. Journal of hospital medicine 2016;11(12):862–64. [DOI] [PubMed] [Google Scholar]
- 8.Boyce JM, Chartier Y,MC, et al. WHO guidelines on hand hygiene in health care: First global patient safety challenge - Clean care is safer care: World Health Organization 2009:1–270. [PubMed] [Google Scholar]
- 9.Gilmartin HM. Use hand cleaning to prompt mindfulness in clinic. BMJ 2016;352:i13. doi: 10.1136/bmj.i13 [DOI] [PubMed] [Google Scholar]
- 10.Kabat-Zinn J Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Bantam Books; 2013. [Google Scholar]
- 11.Gilmartin H, Goyal A, Hamati M, et al. Brief mindfulness practices for healthcare providers: A systematic literature review. Am J Med 2017; 130(10): 1219e1–19e17. doi: 10.1016/j.amjmed.2017.05.041 [DOI] [PubMed] [Google Scholar]
- 12.Weick KE, Sutcliffe KM, Obstfeld D. Organizing for high reliability: Processes of collective mindfulness In: Boin A, ed. Crisis Management. Los Angeles: Sage; 2008:31–66. [Google Scholar]
- 13.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology 2003;84(4):822. doi: 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- 14.Kiyoshi-Teo H, Krein S, Saint S. Applying mindful evidence-based practice at the bedside: Using catheter-associated urinary tract infection as a model. Infection Control and Hopsital Epidemiology 2013;34(10):1099–101. doi: 10.1086/673147 [DOI] [PubMed] [Google Scholar]
- 15.Sibinga EMS, Wu AW. Clinician mindfulness and patient safety. JAMA 2010;304(22):2532–33. doi: 10.1001/jama.2010.1817 [DOI] [PubMed] [Google Scholar]
- 16.Houchens N, Harrod M, Fowler KE, et al. How Exemplary Inpatient Teaching Physicians Foster Clinical Reasoning. The American Journal of Medicine 2017 [DOI] [PubMed] [Google Scholar]
- 17.Srigley JA, Furness CD, Baker GR, et al. Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study. BMJ Qual Saf 2014;23(12):974–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. American Journal of Infection Control 2002;30(8):S1–S46. [DOI] [PubMed] [Google Scholar]
- 19.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302(12):1284–93. [DOI] [PubMed] [Google Scholar]
- 20.Chesak SS, Bhagra A, Schroeder DR, et al. Enhancing resilience among new nurses: Feasibility and efficacy of a pilot intervention. The Ochsner Journal 2015;15(1):38–44. [PMC free article] [PubMed] [Google Scholar]
- 21.Gauthier T, Meyer RM, Grefe D, et al. An on-the-job mindfulness-based intervention for pediatric ICU nurses: A pilot. J Pediatr Nurs 2015;30(2):402–09. [DOI] [PubMed] [Google Scholar]
- 22.Kemper KJ, Khirallah M. Acute effects of online mind-body skills training on resilience, mindfulness, and empathy. Journal of Evidence-based Complementary & Alternative Medicine 2015;20(4):247–53. [DOI] [PubMed] [Google Scholar]
- 23.Taylor M, Hageman JR, Brown M. A mindfulness intervention for residents: Relevance for pediatricians. Pediatric Annals 2016;45(10):e373–e76. [DOI] [PubMed] [Google Scholar]
- 24.Puddicombe A All it Takes is 10 Mindful Minutes. In: Puddicombe A, ed. TED Talks; New York, 2012. [Google Scholar]
- 25.Chen W, Shi J, Qian L, et al. Comparison of robustness to outliers between robust poisson models and log-binomial models when estimating relative risks for common binary outcomes: A simulation study. BMC Medical Research Methodology 2014;14(1):82. doi: 10.1186/1471-2288-14-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grossman P On measuring mindfulness in psychosomatic and psychological research. Journal of psychosomatic research 2008;64(4):405–08. [DOI] [PubMed] [Google Scholar]
- 27.Green J, Britten N. Qualitative research and evidence based medicine. BMJ 1998;316(7139):1230. doi: 10.1136/bmj.316.7139.1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murtagh M, Thomson R, May C, et al. Qualitative methods in a randomised controlled trial: The role of an integrated qualitative process evaluation in providing evidence to discontinue the intervention in one arm of a trial of a decision support tool. Quality and Safety in Health Care 2007;16(3):224–29. doi: 10.1136/qshc.2006.018499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Groopman JE, Prichard M. How Doctors Think. Boston, MA: Houghton Mifflin; 2007. [Google Scholar]
- 30.Irving JA, Dobkin PL, Park J. Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction. Complementary Therapies in Clinical Practice 2009;15:61–66. doi: 10.1016/j.ctcp.2009.01.002 [DOI] [PubMed] [Google Scholar]
- 31.Brennan J, McGrady A. Designing and implementing a resiliency program for family medicine residents. The International Journal of Psychiatry in Medicine 2015;50(1):104–14. doi: 10.1177/0091217415592369 [DOI] [PubMed] [Google Scholar]
- 32.Watson J Nursing: Human science and human care: A theory of nursing. Boston: Jones & Bartlett Learning; 1999. [Google Scholar]
- 33.Squires JE, Linklater S, Grimshaw JM, et al. Understanding practice: Factors that influence physician hand hygiene compliance. Infection Control & Hospital Epidemiology 2014;35(12): 1511–20. [DOI] [PubMed] [Google Scholar]
- 34.Schneider J, Moromisato D, Zemetra B, et al. Hand hygiene adherence is influenced by the behavior of role models. Pediatric Critical Care Medicine 2009;10(3):360–63. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.