Abstract
Purpose
Children with sonographic grade IV hip dysplasia according to Graf and with failed conservative treatment usually need surgical reduction afterwards. Surgical reduction of the hip can lead to severe complications, the occurrence of residual acetabular dysplasia, osteonecrosis, redislocation and other postoperative complications. This paper investigates whether arthroscopic reduction is a promising alternative to open reduction.
Methods
We retrospectively examined 66 patients (78 hips) who were not older than two years at the first time of surgery. Arthroscopic reduction was performed on 17 children (19 hips) and open reduction on 49 children (59 hips). Patient records were used to determine redislocation, postoperative complication and residual dysplasia. Radiographs were used to determine Tönnis classification for osteonecrosis and pathological acetabular (AC) angle for residual dysplasia. We considered data up to a two-year follow-up. Statistical evaluation was performed with binary logistic regression.
Results
After arthroscopic reduction, 6% showed osteonecrosis, compared with 20% with open reduction (p = 0.334). Redislocation was not observed after arthroscopic reduction but for 29% after open reduction (p = 0.005). An improvement of femoral head coverage was achieved with residual dysplasia of 23.5% after arthroscopic reduction, compared with 62% after open reduction (p = 0.002).
Conclusion
The arthroscopic procedure represents a meaningful alternative to the open procedure due to a lower complication rate, a safe setting, a lower rate of residual dysplasia, no observed redislocation and occurrence of osteonecrosis only once in the arthroscopic group of developmental dysplasia of the hip. The arthroscopic procedure should be tested in further studies and in other clinics in order to broaden the empirical base.
Level of Evidence:
Level III (retrospective cohort study)
Keywords: developmental dysplasia of the hip, open reduction of the developmental diclocated hip, arthroscopic reduction, avascular necrosis
Introduction
Patients with dislocation of the hip (sonographic grade IV hip dysplasia according to Graf) show the most severe form of hip dysplasia.1-4 Successful conservative treatment is impossible due to pronounced anatomical changes in the form of obstacles to reduction such as hypertrophic ligamentum teres and transverse ligament, capsular constriction or hypertrophic pulvinar.1-3,5-7 In 1.3% to 4.4% of the cases, no closed reduction can be achieved with comprehensive hip screening. In these cases, early open reduction must be sought.7 Surgical reduction of the hip can lead to severe complications such as osteonecrosis and dislocated hips with multiple operations.5,8,9
In addition to the standardized open reduction of the dislocated hip, arthroscopic reductions are increasingly discussed.10-12 The literature describes the process of various new arthroscopic procedures with a comparison of their advantages and disadvantages. It is widely agreed that an arthroscopic reduction, in comparison with the established open reduction, does not represent any restrictions for the removal of intra-articular obstacles to reduction.10-12 Compared with the open procedure, the arthroscopic procedure offers the advantage of improved clarity of anatomical structures and allows a good view of the entire acetabulum through the use of a 70° view.12,13 This paper investigates whether arthroscopic surgery is a promising alternative to open reduction, in particular after failed attempts of conservative closed reduction. The following criteria were examined to compare the two reductions: residual acetabular dysplasia, osteonecrosis, redislocation of the hip and other postoperative complications.
Materials and methods
The open and arthroscopic reductions were performed between 1 January 2000 and 3 January 2014 at the Paediatric Orthopaedic Center Level III. An observation period of two years was chosen with an annual radiological check-up. Only the results after a two-year follow-up are explained and discussed in this paper, since the effects are better recognizable. The data collection was based on existing patient files, operation reports and radiographs.
The following inclusion criteria were used:
presence of Graf’s grade IV hip dysplasia on at least one side at the time of the first ambulant examination;
patients not older than two years at the time of the first surgical reduction;
patients with at least one unsuccessful conservative reduction attempt.
The selected radiographs were taken at three points in time. Immediately before the operation and approximately one and two years after the operation. Exclusion criteria were the absence of several radiographs and the presence of a teratological hip dislocation.
By these criteria, the patient population needed to be reduced from 117 to 66 patients, thereof 49 reduced openly and 17 arthroscopically (Fig. 1).
Fig. 1.
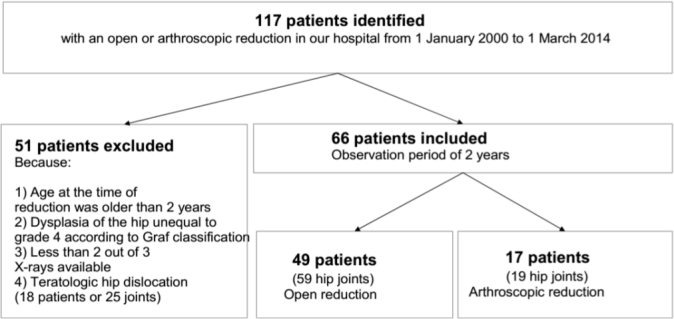
Derivation of patient population.
Through a look at various risk factors such as age at reduction, sex and operation side, the character of the investigated patient population is revealed (Table 1). The mean age of reduction was nearly identical in both groups (Table 1). A pathological acetabular (AC) angle was found much more frequently in the arthroscopic group (84% arthroscopic versus 61% open). Evidence of pathological development due to delayed appearance of the ossific nucleus (no ossific nucleus over seven months of age) was given in eight hips. This concerned three (16%) arthroscopically and five (9%) openly reduced hips. The degree of dislocation was observed at 70% before open reduction and at 84% before arthroscopic reduction. Due to lacking or minor quality of radiographs, for some hips no data could be derived.
Table 1.
Characteristics of patient population
| Variable | Open reduction | Arthroscopic reduction | Exact significance (2-sided) chi-square |
|---|---|---|---|
| Patients | 49 | 17 | |
| Hips | 59 | 19 | |
| Mean age at reduction, mths (range) | 9.47 (1 to 24) | 9.89 (3 to 21) | |
| Sex ratio (male:female) | 5:44 | 3:14 | |
| Side distribution (right:left) | 27:32 | 9:10 | |
| Side distribution (unilateral:bilateral) | 39:10 | 15:2 | |
| Preoperative characteristics | |||
| Mean AC angle (range) | 33.78° (23° to 45°) | 37.37° (30° to 55°) | |
| AC angle (normal:pathologic) | 21:33 | 3:16 | p = 0.090 |
| Ossific nucleus (present:absent) | 25:29 | 6:13 | p = 0.295 |
| Occurrence of ossific nucleus (normal:delayed) | 49:5 | 16:3 | p = 0.421 |
| Preoperative severity of dislocation, % (n/N) | |||
| Grade I | 0 (0/53) | 0 (0/19) | p = 0.363 |
| Grade II | 30.2 (16/53) | 15.8 (3/19) | |
| Grade III | 41.5 (22/53) | 52.6 (10/19) | |
| Grade IV | 28.3 (15/53) | 31.6 (6/19) |
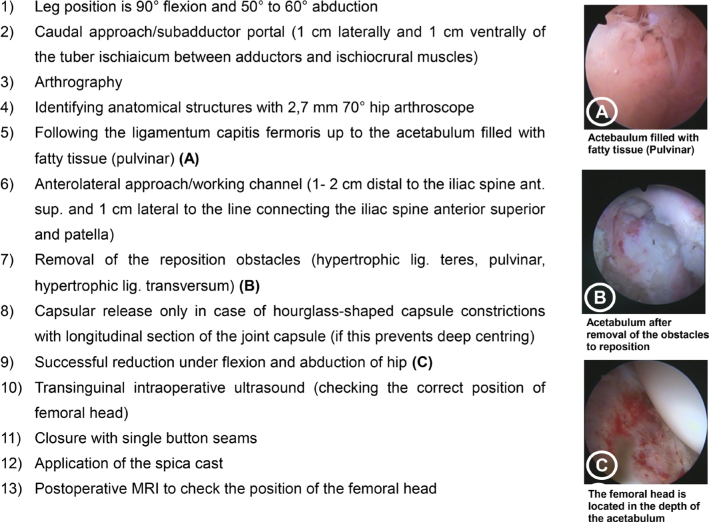
The open reductions were performed by five surgeons (without intraoperative arthrography) according to the procedures already described in the literature.5,6,14 Postoperatively, a ventral ultrasound was performed, but no MRI. The arthroscopic reduction was performed by only two surgeons following a newer procedure as described in Figure 2.
Fig. 2.
Procedure of arthroscopic reduction (based on Eberhardt et al11,13).
Table 2 compares the groups with respect to the investigated reduction. Significant differences in the removal of the obstacles to reduction were found in the tenotomy of the iliopsoas muscle, an inverted labrum and in the intraoperative transfixing of the hip with Kirschner-wire (Table 2). The postoperative management was identical in both groups with a three-times four-week plaster treatment and subsequent therapy in an abduction splint.
Table 2.
Comparison of open and arthroscopic reduction
| Variable | Open (59 hips) | Arthroscopic (19 hips) | Exact significance (2-sided) chi-square |
|---|---|---|---|
| Length of reduction | 1 hr 30 mins | 2 hrs 17 mins | p = 0.000* |
| Reduction with concomitant osteotomies, % (n/N) | 21 (11/52) | 32 (6/19) | p = 0.365 |
| Intraoperative transfixing of the hip, % (n/N) | 47 (25/53) | 0 (0/19) | p = 0.000 |
| Obstacles to reduction, % (n/N) | |||
| Resection of hypertrophic ligamentum teres | 87 (46/53) | 95 (18/19) | p = 0.672 |
| Resection of hypertrophic pulvinar | 92 (49/53) | 100 (19/19) | p = 0.567 |
| Incision to resection of hypertrophic transverse ligament | 55 (29/53) | 42 (8/19) | p = 0.811* |
| Capsulotomy or capsular release | 81 (43/53) | 89 (17/19) | p = 0.497 |
| Tenotomy of the iliopsoas muscle | 43 (23/53) | 5 (1/19) | p = 0.002 |
| Inverted labrum | 40 (21/53) | 5 (1/19) | p = 0.007 |
| Adductor tenotomy | 19 (10/52) | 10 (2/19) | p = 0.494 |
Asymptotic (2-sided) chi-square
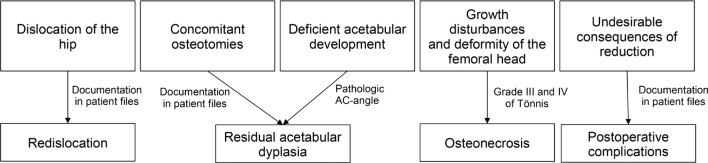
After two years of follow-up, the mean age was 33 months (range 23 months to 52 months) after open reduction versus 34 months (range 13 months to 57 months) after arthroscopic reduction. The four considered target variables were the occurrence of general postoperative complications, osteonecrosis, redislocation and residual acetabular dysplasia (Fig. 3).
Fig. 3.
Target variables.
For the determination of radiological parameters Gimp v2.8.2 (Open Source, licensed by GNU v3) and MB- Ruler v5.0 (Markus Bader Softwaresolutions, Iffezheim, Germany) were used and for statistical evaluation SPSS v22 (IBM Corporation, Armonk, New York) was used. As model for statistical analysis to explain group differences, we used the binary logistic regression with an independent variable (here: ‘type of reduction’) and estimates with which probability pj (y = 1) and a dependent variable (here: osteonecrosis, residual acetabular dysplasia and redislocation).15,16 However, in the group of arthroscopic reduction there were only 19 observations resulting in a kind of statistical instability. Due to fewer cases, only a limited number of parameters could be considered in the models. Therefore, parameters such as preoperative age, preoperative grade of dislocation, preoperative grade of dysplasia, sex, presence of ossific nucleus and transfixing with Kirschner-wire were added and removed iteratively in order to identify the model with the best quality. For redislocation it was not possible to perform binary logistic regression without additional investigations due to structural zeros. In these cases, a chi-square test was first used to determine whether there was a significant relationship between the dependent variable (redislocation) and the most important independent variable (reduction). A bootstrap mode was then performed for verification.
Results
Preoperative evidence for the development of osteonecrosis due to a missing ossificial nucleus was already present in eight hips, and thereof two openly reduced hips developed osteonecrosis after two years control. A total of 11 hips (16%) of 67 hips examined showed severe osteonecrosis, ten (20%) after open reduction and one (6%) after arthroscopic reduction. However, no statistically significant difference could be observed (p = 0.334) (Table 3). This one arthroscopic case of osteonecrosis appeared on a patient with bilateral dislocation. By comparing bilateral and unilateral cases, no significant differences (between 0% and 10%) were found with respect to the occurrence of complications. Only in the arthroscopic group was the difference in osteonecrosis nearly 20%, but on a very small case basis (one case, i.e. one bilateral patient affected on one side).
Table 3.
Occurences of osteonecrosis, redislocation and residual dysplasia
| Variable | Open (59 hips) | Arthroscopic (19 hips) | Significance of binary logistic regression |
|---|---|---|---|
| Osteonecrosis, % (n/N) | 20 (10/50) | 5.9 (1/17) | p = 0.334 |
| Redislocation, % (n/N) | 28.8 (17/59) | 0 (0/19) | p = 0.005 |
| Residual dysplasia, % (n/N) | 62 (31/50) | 23.5 (4/17) | p = 0.002 |
| Mean postoperative AC angle (range) | 25.96° (13° to 40°) | 22.65° (11° to 34°) | p = 0.075* |
| Pathological AC angle | 50 (25/50) | 23.5 (4/17) | p = 0.088** |
Asymptotic (2-sided) chi-square
Exact Significance (2-sided) chi-square
Among intraoperative obstacles to reduction (Table 2) and thus possible risk factors for the occurrence of osteonecrosis, a statistically significant correlation was only found in an inverted labrum (p = 0.02) after chi-square test.
Redislocation was documented in 17 hips (22%) of 78 hips, only after open reduction (17 of 59 cases, 29%). The probability of developing a redislocation after open reduction was statistically significant (p = 0.005) (Table 3). Residual dysplasia was observed in 35 hips (52%) of 67 observed hips. There were four cases (23.5 %) after arthroscopic compared with 31 cases (62 %) after open reduction. There was a statistically significant correlation (p = 0.002) (Table 3). The mean postoperative AC angle was 26° after open reduction (range 13° to 40°) and 23° (range 11° to 34°) after arthroscopic reduction. A total of 25 hips (50%) of the open reduction group were characterized as severe or extremely dysplastic joints, though, only four (23.5 %) were part of the arthroscopic group (Table 3).
The different numbers between pathological AC angle and residual dysplasia results from the fact that some hips with residual dysplasia already received concomitant osteotomies before their radiological evaluation. A secondary procedure due to a redislocation or residual acetabular dysplasia was necessary exclusively after open reduction (Table 4). The secondary procedure concerned 18 hips (30%). In all, 14 hips received a secondary or more open reductions. An additional concomitant osteotomy during open reduction was necessary in eight of these 14 joints due to treat residual acetabular dysplasia (two hips received two open reductions with concomitant osteotomy). Only a sole concomitant osteotomy was performed on four hips.
Table 4.
Occurrences of secondary procedures
| Variable, % (n/N) | Open (59 hips) | Arthroscopic (19 hips) | Exact significance (2-sided) chi-square |
|---|---|---|---|
| Secondary procedures | 30.5 (18/59) | 0 (0/19) | p = 0.004 |
| Secondary open reduction | 24 (14/59) | 0 (0/19) | p = 0.017 |
| Secondary concomitant osteotomy | 20 (12/59) | 0 (0/19) | p = 0.032 |
| Secondary open reduction with concomitant osteotomy | 13.5 (8/59)* | 0 (0/19) | |
| Sole concomitant osteotomy | 7 (4/59) | 0 (0/19) |
Postoperative complications associated with reduction such as dislocation or break of Kirschner-wire, septic arthritis or postoperative haemoglobin value of less than 9 g/dl are presented in Table 5.
Table 5.
Occurrences of complications of reduction
| Variable, % (n/N) | Open (59 hips) | Arthroscopic (19 hips) | Exact significance (2-sided) chi-square |
|---|---|---|---|
| Dislocation of Kirschner-wire | 7 (4/59) | 0 (0/19) | p = 0.567 |
| Wire migrated abdominal | 2 (1/59) | 0 (0/19) | p = 1.000 |
| Septic arthritis | 2 (1/59) | 0 (0/19) | p = 1.000 |
| Break of Kirschner-wire | 2 (1/59) | 0 (0/19) | p = 1.000 |
| Haemoglobin value below 9 g/dl | 38 (20/52) | 9 (1/11) | p = 0.082 |
Discussion
The focus of this study was on answering the question of to what extent arthroscopic reduction represents a possible alternative to the established open reduction. The primary objective of the treatment of patients with developmental dysplasia of the hip (DDH) should be a stable and centred reduction as well as the avoidance of complications with negative effects on the further development of the child.
Osteonecrosis (grade III and IV according to Tönnis) was much more frequently observed in the open compared with arthroscopic reduction (20% versus 5.9%), yet without statistical significance (Table 3). In the literature osteonecrosis is reported in 6% to 48%.5,17-20
Better results for arthroscopic reduction are also confirmed by some authors10,12 who assume that a reduction in osteonecrosis can be achieved by a more gentle, arthroscopic approach (Fig. 2).
In open reduction, only the ventral approach after Smith-Peterson or an inguinal incision is performed. For the arthroscopic procedure, however, a 1-cm minimally invasive approach was chosen. Additional vascular injuries, which occur by capsulotomy during open reduction, can be avoided by the arthroscopic procedure. Therefore, Akazawa et al21 points out that in open reduction the incision of the capsule should be performed under vision and close to the acetabular margin to avoid injury and to ensure sufficient blood supply to the femoral head.
Increased joint pressure in the hip joint can also cause damage and necrosis of the femoral head. Despite an average operation length of 2.17 hours for the arthroscopic reduction of hips considered in our study (Table 2), it is questionable whether this duration is sufficient to cause osteonecrosis. However, increased postoperative joint pressure can be reduced by the tenotomy of the tendon of the iliopsoas muscle.6
A shortened iliopsoas tendon surrounds the joint capsule from extraarticular and can prevent a successful reduction.11 In arthroscopic reduction, it is possible both to remove intra-articular obstacles of reduction very well and to perform a tenotomy of the iliopsoas muscle. Whether this is necessary can be assessed during the ventral capsule release and it is only performed if required (Fig. 2).
However, due to the proximity of the psoas tendon to anatomical structures, an arthroscopic cleavage of the joint capsule from intra- to extra-articular should, according to Eberhardt et al,11 be precisely weighed due to the risks such as nerve and blood vessel injuries. In the group of arthroscopically reduced hips, this procedure was not performed on any hip joint. In contrast, about half of all openly reduced hips underwent such an intervention. After a tenotomy of the iliopsoas muscle, osteonecrosis was observed less frequently, but without a statistically significant correlation. In our opinion, the role of tenotomy of the tendon of the iliopsoas muscle should be investigated in further studies.
According to Luhmann et al,22 adductor tenotomy is advisable (for patients where the reduction is possible) if a contracture in abduction with a low ‘safe zone’ (according to Ramsey23) of less than 30° exists.
The omission of adductor tenotomy is listed in some studies as a possible risk factor for the development of osteonecrosis.14,24 Both Salter et al24 and Dhar et al25 consider adductor tenotomy, for example in the treatment of children with DDH, to be an important procedure for minimizing osteonecrosis. On the other hand, other studies could not prove any significant risk minimization in adductor tenotomy and the development of osteonecrosis.19,22,26,27 Likewise, our study did not reveal a significant correlation between an adductor tenotomy and the reduction of the osteonecrosis risk.
The variable ‘redislocation’ is very important as it is usually associated with repeated surgical interventions. Redislocation occurred in 28.8% of the hips after open reduction and no further reductions were observed after arthroscopic reduction; this appeared to be statistically significant. It could be explained by a better overview of the anatomical structures during arthroscopic reduction, since some structures are difficult to identify.12 Also, the view into the acetabulum is more complete by the arthroscopic reduction compared with an open approach such as the ventrolateral approach.10 Arthroscopic reduction allows better and complete removal of intra-articular soft-tissue obstacles from the acetabulum and allows a safe, deep and stable concentric reduction.
Eberhardt et al11 was able to use the arthroscopic procedure to identify in particular a narrowing of the hip joint capsule as the main obstacle to reduction, which could be eliminated with the aid of an arthroscopic capsule release and enabled stable reduction. Both a long, narrow and isthmus-like capsule and an overstretched and loose capsule can prevent reduction or contribute insufficiently to the stabilization of the femoral head in the acetabulum.6 The capsule release only has the sense to allow a passage of the femoral head with a narrowed hourglass-shaped joint capsule. A T-shaped capsule opening of the joint – as always in the open procedure – is completely omitted. Also, a capsule suture is not necessary in the arthroscopic procedure. With open reduction, the joint capsule must be opened wide to get a safe overview of the acetabulum. Afterwards, a tightening suture of the joint capsule is of particular importance, as it must withstand excessive capsule tension especially in the first weeks after reduction to prevent further subtension or redislocation.28 Bursting or stretching of the suture are feared complications.28 A loose joint capsule can cause antetorsion of the femoral neck and lateralization of the femoral head.6
In contrast to this, a capsule release is performed ‘on demand’ by the arthroscopic procedure. The joint capsule is opened under vision only to the extent that the femoral head can be reduced, which leads to a considerably smaller joint capsule incision compared with the open procedure. Furthermore, the capsule does not have to be closed during arthroscopic surgery. This makes the procedure much smaller and more gentle than open reduction. In open reduction, on the other hand, the arthrotomy serves to gain an overview of the acetabular component in order to clear it out.
A radiological diagnosis of residual acetabular dysplasia or renewed surgical treatment due to a lack of roofing was made in 62% of the openly reduced hips versus 23.5% of the arthroscopically reduced hips. Depending on the treatment strategy, residual acetabular dysplasia rates between 0% and approximately 35% are described in the literature.29 The residual dysplasia rate in the open reduction group is thus significantly higher than the literature data, which can be explained on the one hand by the severity of the present grade of sonographic dysplasia (grade IV according to Graf) and on the other hand by the age of the children (older than six months after surgery). An unstable joint centring with a long persistent sub- or dislocation position can lead to residual dysplasia due to the loss of the stimulating relationship between femoral head and acetabulum.30 Since the optimal development of the roof of the acetabulum essentially depends on successful depth adjustment of the femoral head,5,31 patients whose hip joints are off-centre are particularly at risk of developing residual dysplasia. The strong remodelling potential of the hip joint within the first six weeks of life must also be considered.32 During this period, a strong maturation and differentiation of the hip joint takes place,32 which decreases after the fourth month of life.33 At that time the maturation plateau of the acetabulum develops and with increasing age hip maturation is expected to decrease.32,33 A later start of treatment can reduce the success of treatment due to the lower development and maturation potential of the hip joints and lead to residual dysplasia.32
The arthroscopic group, on the other hand, showed a statistically significant lower rate of residual dysplasia despite poorer preoperative femoral head roofing (Table 1). This became clear when a pathological AC angle was determined after two years of observation (open: 50% versus arthroscopic: 23.5%) (Table 3). Causes for these differences could be the already described inadequate joint centring after open reduction.
In addition, there is an indication for secondary concomitant osteotomies in the case of permanently pathological AC angles in the course of residual dysplasia during childhood development.32,34 These secondary procedures can lead to an increase in the rate of osteonecrosis.9
In a recent study, good results were achieved by an arthroscopic method without temotomy of the psoas.35 Therein, no redislocation and only a low rate of femoral head necrosis was observed, confirming our results.
To sum up, this study revealed that a minimally invasive technique (arthroscopic reduction) could lead to promising results for patients with severe hip dislocation. Better treatment results were observed by arthroscopic reduction in comparison with open reduction for redislocation, residual acetabular dysplasia, osteonecrosis and postoperative complications. Therefore, the arthroscopic procedure should be continued and tested in further studies, not only by the authors, but also in other clinics in order to broaden the empirical base.
However, the exact figures should be evaluated cautiously, as this study has some limitations and the role of risk factors is controversially discussed in literature. The results presented here are a starting point for further scientific work and provide a first contribution to the comparison of the new arthroscopic and the established open reduction method.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: This work is a retrospective study which is completely based on patient data existing beforehand. This work does not contain any experiments with human participants or animals performed by any of the authors. This work is part of a dissertation at Philipps University Marburg whose ethics committee accepted the subject and the research approach.
Informed consent: Not required for this work.
ICMJE Conflict of interest statement
None of the authors have any conflict of interest to declare. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this work.
Author Contributions
CP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing first draft.
OE: Conceptualization, Formal analysis, Supervision.
TW: Supervision.
FFF: Conceptualization, Formal analysis, Methodology, Validation, Writing review and editing.
References
- 1.Baumgart K, Mellerowicz H. Hüftdysplasie In: Hoffmann R, Zacher J, eds. Orthopädie und Unfallchirugie. Stuttgart, New York: Thieme, 2006:579-598. [Google Scholar]
- 2.Niethard FU, Pfeil J, Biberthaler P. Orthopädie und Unfallchirurgie. 78 Tabellen (6th ed). Stuttgart, New York: Thieme, 2009. [Google Scholar]
- 3.Niethard FU, Weber M, Heller K-D. compact Orthopädie. Alles für Station und Facharztprüfung; 41 Tabellen. Stuttgart, New York: Thieme, 2005. [Google Scholar]
- 4.Rössler H, Pitzen P, Rüther W, Steinhagen J. Orthopädie und Unfallchirurgie (19th ed). München: Elsevier, Urban & Fischer, 2007. [Google Scholar]
- 5.Hefti F. Die kindliche Hüftdysplasie und ihre Behandlungsmöglichkeiten Meyer R-P, Gächter A, Kappeler U, eds. Hüftchirurgie in der Praxis. Berlin: Springer, 2005:67-94. [Google Scholar]
- 6.Tönnis D. Die angeborene Hüftdysplasie und Hüftluxation im Kindes- und Erwachsenenalter. Grundlagen, Diagnostik, konservative und operative Behandlung. Berlin: Springer, 1984. [Google Scholar]
- 7.Tschauner C, Fürntrath F, Saba Y, Berghold A, Radl R. Developmental dysplasia of the hip: impact of sonographic newborn hip screening on the outcome of early treated decentered hip joints-a single center retrospective comparative cohort study based on Graf’s method of hip ultrasonography. J Child Orthop 2011;5:415-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clarke NM, Jowett AJ, Parker L. The surgical treatment of established congenital dislocation of the hip: results of surgery after planned delayed intervention following the appearance of the capital femoral ossific nucleus. J Pediatr Orthop 2005;25:434-439. [DOI] [PubMed] [Google Scholar]
- 9.Pospischill R, Weninger J, Ganger R, Altenhuber J, Grill F. Does open reduction of the developmental dislocated hip increase the risk of osteonecrosis? Clin Orthop Relat Res 2012;470:250-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bulut O, Oztürk H, Tezeren G, Bulut S. Arthroscopic-assisted surgical treatment for developmental dislocation of the hip. Arthroscopy 2005;21:574-579. [DOI] [PubMed] [Google Scholar]
- 11.Eberhardt O, Wirth T, Fernandez FF. Arthroscopic anatomy of the dislocated hip in infants and obstacles preventing reduction. Arthroscopy 2015;31:1052-1059. [DOI] [PubMed] [Google Scholar]
- 12.Oztürk H, Oztemür Z, Bulut O, Tezeren G, Bulut S. Arthroscopic-assisted surgical treatment for developmental dislocation of the hip before the age of 18 months. Arch Orthop Trauma Surg 2013;133:1289-1294. [DOI] [PubMed] [Google Scholar]
- 13.Eberhardt O, Wirth T, Fernandez FF. Arthroscopic reduction and acetabuloplasty for the treatment of dislocated hips in children of walking age: a preliminary report. Arch Orthop Trauma Surg 2014;134:1587-1594. [DOI] [PubMed] [Google Scholar]
- 14.Pfeil J. Hüftchirurgie. Heidelberg: Steinkopff, 2008. [Google Scholar]
- 15.Bittmann F. Einführung in die logistische Regression mit SPSS 2015. http://www.felix-bittmann.de/downloads/artikel/einfuehrung_logit_regression_mit_SPSS.pdf (date last accessed 24 July 2019).
- 16.Fromm S. Binäre logistische Regressionsanalyse: eine Einführung für Sozialwissenschaftler mit SPSS für Windows. Bamberg: Universitaet Bamberg, Professur für Methoden der empirischen Sozialforschung, 2005. [Google Scholar]
- 17.Gardner ROE, Bradley CS, Sharma OP, et al. Long-term outcome following medial open reduction in developmental dysplasia of the hip: a retrospective cohort study. J Child Orthop 2016;10:179-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCluskey WP, Bassett GS, Mora-Garcia G, MacEwen GD. Treatment of failed open reduction for congenital dislocation of the hip. J Pediatr Orthop 1989;9:633-639. [DOI] [PubMed] [Google Scholar]
- 19.Roposch A, Odeh O, Doria AS, Wedge JH. The presence of an ossific nucleus does not protect against osteonecrosis after treatment of developmental dysplasia of the hip. Clin Orthop Relat Res 2011;469:2838-2845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sllamniku S, Bytyqi C, Murtezani A, Haxhija EQ. Correlation between avascular necrosis and the presence of the ossific nucleus when treating developmental dysplasia of the hip. J Child Orthop 2013;7:501-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akazawa H, Oda K, Mitani S, et al. Surgical management of hip dislocation in children with arthrogryposis multiplex congenita. J Bone Joint Surg [Br] 1998;80-B:636-640. [DOI] [PubMed] [Google Scholar]
- 22.Luhmann SJ, Schoenecker PL, Anderson AM, Bassett GS. The prognostic importance of the ossific nucleus in the treatment of congenital dysplasia of the hip. J Bone Joint Surg [Am] 1998;80-A:1719-1727. [DOI] [PubMed] [Google Scholar]
- 23.Ramsey PL, Lasser S, MacEwen GD. Congenital dislocation of the hip. J Bone Joint Surg [Am] 1976;58-A:1000-1004. [PubMed] [Google Scholar]
- 24.Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg 1969;12:44-61. [PubMed] [Google Scholar]
- 25.Dhar S, Taylor JF, Jones WA, Owen R. Early open reduction for congenital dislocation of the hip. J Bone Joint Surg [Br] 1990;72-B:175-180. [DOI] [PubMed] [Google Scholar]
- 26.Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg [Am] 1980;62-A:876-888. [PubMed] [Google Scholar]
- 27.Segal LS, Boal DK, Borthwick L, et al. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop 1999;19:177-184. [DOI] [PubMed] [Google Scholar]
- 28.Kershaw CJ, Ware HE, Pattinson R, Fixsen JA. Revision of failed open reduction of congenital dislocation of the hip. J Bone Joint Surg [Br] 1993;75-B:744-749. [DOI] [PubMed] [Google Scholar]
- 29.Novais EN, Hill MK, Carry PM, Heyn PC. Is age or surgical approach associated with osteonecrosis in patients with developmental dysplasia of the hip? A meta-analysis. Clin Orthop Relat Res 2016;474:1166-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doyle SM, Bowen JR. Types of persistent dysplasia in congenital dislocation of the hip. Acta Orthop Belg 1999;65:266-276. [PubMed] [Google Scholar]
- 31.Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. J Pediatr Orthop 1994;14:3-8. [DOI] [PubMed] [Google Scholar]
- 32.Matthiessen H. Wachstum und Reifung. Becken, Hüfte. 114 Tabellen Tschauner C, ed. Orthopädie und orthopädische Chirurgie. Stuttgart, New York: Thieme, 2004:120–133. [Google Scholar]
- 33.Tschauner C, Klapsch W, Baumgartner A, Graf R. ‘Reifungskurve’ des sonographischen Alpha-Winkels nach GRAF unbehandelter Hüftgelenke im ersten Lebensjahr. Z Orthop Ihre Grenzgeb 1994;132:502-504. [DOI] [PubMed] [Google Scholar]
- 34.Pothmann M, Cordier W. Protrahierte Hüftreifungsstörung im Kindesalter. Becken, Hüfte. 114 Tabellen Tschauner C, ed. Orthopädie und orthopädische Chirurgie. Stuttgart, New York: Thieme, 2004:141-155. [Google Scholar]
- 35.Duman S, Camurcu Y, Sofu H, et al. Arthroscopic versus open, medial approach, surgical reduction for developmental dysplasia of the hip in patients under 18 months of age. Acta Orthop 2019;90:292-296. [DOI] [PMC free article] [PubMed] [Google Scholar]