Abstract
Purpose
Therapy of juvenile neurogenic flatfoot (JNF) with subtalar arthroereisis (SA) is currently under critical clinical investigation. In this retrospective matched pair analysis, the radiological outcome after arthroereisis in paediatric patients with infantile cerebral palsy and JNF was compared with children with juvenile flatfeet (JF) without neurological diseases.
Methods
From October 2007 to April 2018 80 patients with 149 flatfeet underwent surgery with SA. Inclusion criteria were: 1) JNF or JF with age at surgery ≤ 13 years; 2) treatment with SA; 3) presence of three sets of biplane radiographs (preoperative, postoperative and follow-up (FU)). The radiographs were analyzed for: 1) navicular-cuboidal-index (NCI); 2) talocalcaneal angle anteroposterior; 3) talocalcaneal angle lateral; 4) calcaneal-pitch (CP); and 5) talometatarsal-index (TMTI). Following this, 25 patients with 38 flatfeet could be included.
Results
The mean age at SA of the JNF group was 9.2 years (JF group: 9.3 years) and the mean time of FU was 35.2 months (JF group: 39.4 months). In comparison with preoperatively, a significant decrease of the NCI was seen in both groups (p = ≤ 0.05 and p = ≤ 0.001) in the FU radiographs. The analysis of CP and TMTI in the JF group also resulted in a significant improvement (p = ≤ 0.001 and p = ≤ 0.05). Overall, the comparison between the JNF and JF group showed no significant differences in regard to the analyzed postoperative parameters.
Conclusion
Based on this data, treatment of flatfeet by SA in patient with neurological disorders shows an improvement of radiological parameters comparable with neurologically unimpaired patients and might be considered as additional treatment option.
Level of evidence:
IV
Keywords: pes planus, flatfoot, subtalar arthroereisis, cerebral palsy
Introduction
Various neurological diseases in children, e.g. infantile cerebral palsy (ICP) or tethered cord syndrome, can cause juvenile neurogenic flatfoot (JNF).1,2 Insufficiency of the longitudinal-arch-building muscles, especially of the Musculus tibialis posterior has a major impact in the pathogenesis of JNF. In addition, the valgus position of the heel results in a secondary shortening of the Achilles tendon and thus the development of a pes equinus. In neurologically unimpaired children, being overweight, male gender and older age are considered as risk factors for development of juvenile flatfeet (JF).3,4 In both cases, structural changes can lead to a rigid flatfoot. The optimal therapy is still discussed controversially, and treatment recommendations especially differ between JNF and JF. In normally developed children with JF, the therapy consists of initial conservative management with strengthening of the longitudinal-arch-building muscles and walking barefoot.5 In case of conservative therapy failure, pain or loss of range of movement, surgical treatment is recommended. Here, various surgical options, such as subtalar arthroereisis (SA), subtalar arthrodesis, calcaneus osteotomies (e.g. Evans-osteotomy or Dwyer-osteotomy) and/or muscle tendon transfers6-10 have been evaluated. For the conservative treatment of neurologically impaired children with JNF a large variety of orthoses, insoles or plaster retention therapies are used. Given that the neurological disorders cannot be influenced the mean goal of therapy for JNF is a better mobilization of the children whereas in patients with JF the development of a physiological foot is desired.11 If conservative therapy fails or a replacement for an orthosis seems reasonable, surgical treatment with similar surgical techniques as in JF can be performed. However, the treatment of JNF with SA is seen rather sceptically12 as strengthening of the longitudinal-arch-building muscles – which is essential for the success of the SA – is not possible in JNF.
To further evaluate the outcome of SA we conducted a retrospective matched pair study of paediatric patients with cerebral palsy and JNF in comparison with patients without neurological disease.
The primary hypothesis was that JNF will show an inferior radiological outcome following SA in comparison with JF.
Patients and methods
Patients
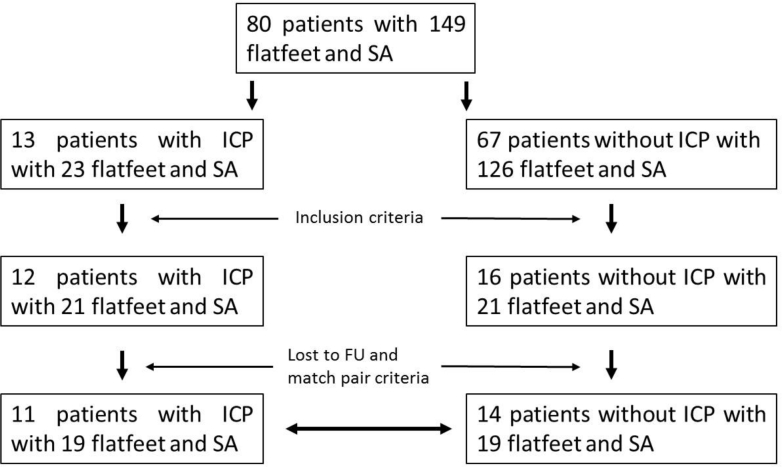
In the period between October 2007 to April 2018 80 patients with 149 flatfeet have been treated by SA in our department. In all, 25 of them met our match pair criteria (Fig. 1). The study group consists of 11 patients (ICP) with 19 JNF which were compared with 14 patients with 19 JF (control group).
Fig. 1.
Study and control group (SA, subtalar arthroereisis; ICP, infantile cerebral palsy; FU, follow-up).
Included were children with: 1) JNF or JF with age at surgery ≤ 13 years; 2) treatment with SA; 3) presence of three sets of biplane radiographs (preoperative, postoperative and follow-up (FU)) under full weight-bearing with anteroposterior (AP) and lateral view.
Match pair criteria were: 1) same age at index surgery with SA (± one year); 2) comparable navicular-cuboidal-index (NCI) ≤ 25% preoperatively; and 3) a comparable FU period.
Methods
The following demographic parameters were assessed: 1) mean age at surgery; 2) gender; 3) affected side; 4) Gross Motor Function Classification System (It’s the link, here should be a reference number) score of ICP patients; and 5) additional soft-tissue surgery. The routine radiographs were analyzed for the following established parameters and indices: 1) NCI (relative overlap of Os naviculare and Os cuboideum lateral view); 2) talocalcaneal angle lateral (TCA lat); 3) talocalcaneal angle AP (TCA AP, kite angle); 4) calcaneal-pitch (CP); and 5) talometatarsal-index (TMTI) (Fig. 2).
Fig. 2.
(a) Preoperative lateral view of an eight-year-old boy with infantile cerebral palsy (ICP) (navicular-cuboidal-index (NCI) 53.3%; talocalcaneal angle lateral (TCA lat) 48.2°; calcaneal-pitch (CP) 8.6°); (b) postoperative control; (c) one-year postoperative; (d) two-years postoperatively and after implant removal with physiological foot position (NCI 26.3%; TCA lat 32.1°; CP 17.5°) (*CP; #TCA lat; +NCI).
Measurements were conducted by the first (HK) and fourth (CL) authors using a certified radiographic image viewer (Sectra Workstation IDS7, Linköping, Sweden).
Treatment protocol SA
Examination of calf muscle length by dorsal flexion of the ankle joint while the subtalar joint is held in realigned position in hindfoot correction is carried out. In case of additional equinus deformity, calf muscle or Achilles tendon lengthening (e.g. Baumann- or Strayer-technique) is performed, when dorsal flexion of the upper ankle joint is below 5°. In blood-arrest, disinfection and lateral incision (1 cm to 2 cm) over the sinus tarsi is carried out. Then the subcutaneous tissue is prepared with exposure of the sinus tarsi. The subtalar joint complex is reducted and a Kirschner-wire inserted in the calcaneus below the lateral process of the talus in cranio-caudal direction. The correct position of the wire is controlled with an image intensifier in two planes and if necessary corrected. The Kirschner-wire is over-drilled and a 7.0 mm cannulated cancellous bone screw (length 25 mm to 30 mm) is screwed in the calcaneus (the correct position is achieved when the screw is below the lateral process of the talus). Then, the result is clinically and radiologically evaluated, and afterwards a subcutaneous and intracutaneous skin suture is performed. Then, a final clinical examination of the range of movement is carried out.
Full weight-bearing immediately postoperatively is allowed. In case of pain, partial weight-bearing on crutches was advised.
Statistical analysis
Results are presented as mean value (sd) or standard error of the mean (sem) using IBM SPSS Statistics Version 23 (Armonk, NY, USA).
Statistical significance was calculated by the unpaired Student’s t-test, using IBM SPSS Statistics Version 23. A p-value < 0.05 was considered significant.
Results
The mean age at surgery of the JNF group was 9.2 years (sd 2.2; 5 to 13). The mean FU to the first postoperative control radiograph was 6.0 months (sd 5.4; 0 to 19) and 35.2 months (sd 27.9; 7 to 100) to the last FU examination. In all, 13 cases (68.4%) were male. An additional soft-tissue procedure (intramuscular lengthening (recession) of the gastrocnemius muscles (Baumann procedure)) was conducted in six cases (31.6%). Nine JNF (47.4%) presented with a GMFCS level II and six (31.6%) with a GMFCS level III (Table 1).
Table 1.
Age at operation in years
| Match | Age at operation | Sex | ICP | GMFCS score | Side | NCI preoperatively | NCI postoperatively | NCI FU | FU, mths | Operation |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 9 | M | Y | 4 | R | 51 | 28 | 26 | 7 | A |
| 1 | 9 | M | N | L | 54 | 19 | 13 | 8 | A | |
| 2 | 9 | M | Y | 4 | L | 53 | 39 | 29 | 7 | A |
| 2 | 9 | M | N | R | 66 | 9 | 13 | 8 | A | |
| 3 | 9 | F | Y | 1 | R | 63 | 18 | 6 | 100 | A |
| 3 | 9 | M | N | R | 63 | 46 | 27 | 75 | A | |
| 4 | 9 | M | Y | 3 | R | 54 | 26 | 4 | 62 | A |
| 4 | 9 | F | N | L | 46 | 31 | 29 | 48 | A | |
| 5 | 9 | M | Y | 3 | L | 64 | 17 | 6 | 62 | A |
| 5 | 9 | M | N | L | 47 | 15 | 35 | 75 | A | |
| 6 | 13 | M | Y | 2 | R | 17 | 22 | 25 | 8 | A |
| 6 | 13 | M | N | L | 27 | 18 | 14 | 29 | A | |
| 7 | 13 | M | Y | 2 | L | 28 | 15 | 45 | 8 | A |
| 7 | 13 | M | N | L | 38 | 4 | 11 | 10 | A | |
| 8 | 11 | F | Y | 3 | R | 37 | 36 | 45 | 27 | A |
| 8 | 11 | F | N | R | 36 | 19 | 22 | 33 | A | |
| 9 | 11 | F | Y | 3 | L | 42 | 18 | 42 | 27 | A+B |
| 9 | 11 | F | N | R | 63 | 22 | 35 | 31 | A+B | |
| 10 | 7 | F | Y | 2 | R | 37 | 21 | 15 | 28 | A+B |
| 10 | 8 | M | N | R | 39 | 16 | 27 | 53 | A+B | |
| 11 | 7 | F | Y | 2 | L | 45 | 34 | 18 | 28 | A+B |
| 11 | 7 | F | N | L | 45 | 44 | 58 | 35 | A+AL | |
| 12 | 8 | M | Y | 2 | L | 53 | 25 | 51 | 21 | A+B |
| 12 | 8 | M | N | R | 56 | 28 | 31 | 15 | A | |
| 13 | 10 | M | Y | 2 | R | 70 | 67 | 52 | 14 | A+B |
| 13 | 10 | F | N | L | 53 | 27 | 13 | 39 | A | |
| 14 | 10 | M | Y | 2 | L | 71 | 10 | 15 | 14 | A+B |
| 14 | 10 | M | N | L | 60 | 37 | 5 | 22 | A | |
| 15 | 9 | M | Y | 2 | R | 22 | 14 | 1 | 19 | A+B |
| 15 | 10 | M | N | L | 20 | 8 | 12 | 79 | A | |
| 16 | 9 | M | Y | 2 | L | 23 | 28 | 27 | 19 | A+B |
| 16 | 10 | M | N | R | 27 | 15 | 5 | 78 | A | |
| 17 | 11 | M | Y | 1 | L | 40 | 15 | 14 | 42 | A+B |
| 17 | 11 | F | N | R | 36 | 19 | 22 | 33 | A | |
| 18 | 5 | M | Y | 3 | R | 47 | 48 | 60 | 79 | A+B |
| 18 | 5 | M | N | R | 40 | 35 | 71 | 28 | A | |
| 19 | 5 | M | Y | 3 | L | 40 | 35 | 71 | 79 | A+B |
| 19 | 5 | M | N | R | 39 | 38 | 38 | 28 | A |
ICP: infantile cerebral palsy; GMFCS: Gross Motor Function Classification System; NCI: navicular-cuboidal-index (in %); FU: follow-up; A, arthroereisis; B, Baumann procedure; AL, lengthening of Achilles tendon
The mean age at surgery in the JF group was 9.3 years (sd 2.2; 5 to 13) and mean FU to the first postoperative control radiograph was 8.1 months (sd 14.3; 1 to 65) and 39.4 months (sd 22.8; 8 to 79) to the last FU examination. In all, 13 (68.4%) of the cases were male. A total of 14 cases were treated solely with SA (73.7%), four with SA and additional Baumann procedure (21.1%) and in one case with SA and lengthening of Achilles tendon (5.1%).
Postoperative complications were not detected.
Comparison of the radiological parameters within the JNF group
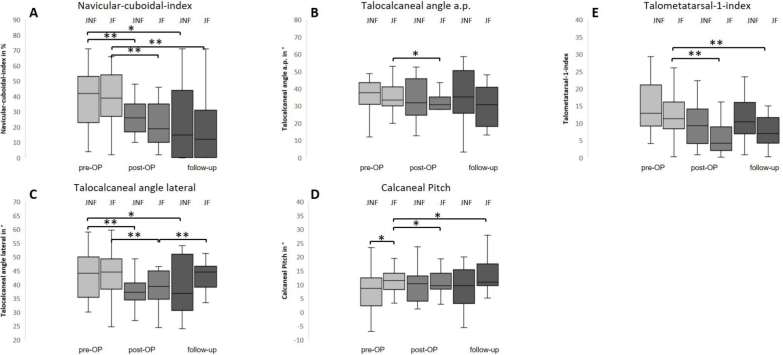
A significant decrease of the NCI was seen in comparison of preoperative (45.4%) to postoperative (27.7%), respectively FU (22.9%) (p = ≤ 0.001 and p = ≤ 0.05) (Fig. 3). Likewise, an improvement of the TCA lat. preoperatively in comparison with postoperatively and FU was detected (p = ≤ 0.001 and p = ≤ 0.05) (Table 2).
Table 2.
Mean values of CP, TCA AP, TCA lat and NCI, TMTI preoperative, postoperative and FU of the juvenile flatfeet (JF, no ICP) group and juvenile neurogenic flatfeet (JNF, ICP) group
| ICP | No ICP | t-test ICP vs no ICP | |
|---|---|---|---|
| Calcaneal pitch (CP) | |||
| Preoperative | 7.2° | 11.4° | 0.045* |
| Postoperative | 10.7° | 11.4° | n.s. |
| FU | 10.1° | 13.6°** | n.s. |
| Talocalcaneal angle anteroposterior (TCA AP) | |||
| Preoperative | 36.7° | 35.0° | n.s. |
| Postoperative | 33.8° | 30.7°* | n.s. |
| FU | 36.2° | 30.4° | n.s. |
| Talometatarsal index (TMTI) | |||
| Preoperative | 15.4 | 11.8 | n.s. |
| Postoperative | 11.8 | 5.9** | n.s. |
| FU | 12.5 | 7.6** | n.s. |
| Talocalcaneal angle lateral (TCA lat) | |||
| Preoperative | 43.1° | 44.0° | n.s. |
| Postoperative | 36.8°** | 39.2°** | n.s. |
| FU | 38.6°* | 42.9°** | n.s. |
| Navicular-cuboidal-index (NCI) | |||
| Preoperative | 45.4% | 45.0% | n.s. |
| Postoperative | 27.7%** | 23.3%** | n.s. |
| FU | 22.9%* | 23.4%** | n.s. |
ICP: infantile cerebral palsy; FU: follow-up; n.s.: no significance
The comparison between both groups shows a significant difference of the CP preoperative (p = 0.045), the other values show no significant (n.s.) differences
*p ≤ 0.05, **p ≤ 0.001 = significant changes within the JF or JNF group in comparison of preoperative, postoperative and FU
Fig. 3.
(a) Navicular-cuboidal-index (NCI): significant improvement of the index in comparison of preoperative with postoperative and follow-up (FU) in both groups (*p ≤ 0.05; **p ≤ 0.001); (b) talocalcaneal angle a.p. (TCA AP): improvement of the values preoperatively compared with FU in the juvenile flatfeet (JF) group, no permanent improvement (preoperative to FU); (c) talocalcaneal angle lateral (TCA lat): significant improvement of the angle in both groups, deterioration again in the JF group; (d) calcaneal-pitch (CP): improvement in the JF group preoperatively and postoperatively compared with FU. Moreover, detection of a significant higher CP in the JF group compared to the juvenile neurogenic flatfeet (JNF) group preoperatively; (e) talometatarsal-1-index (TMTI): improvement of the index in comparison between preoperative and postoperative and FU in the JF group (n = 38) (pre-OP: preoperative; post-OP: postoperative, JF: juvenile flatfeet, JNF: juvenile neurogenic flatfeet).
Comparison of the radiological parameters within the JF group
Our data show an improvement in three parameters (Fig. 3): 1) the NCI showed a significant decrease preoperatively (45.0%) compared with postoperatively (23.3%, p = ≤ 0.001) and preoperatively to FU (23.4%, p = ≤ 0.001); 2) the CP preoperatively compared with postoperatively and FU was significantly increased (p = ≤ 0.05); and 3) the examination of the TMTI showed an improvement preoperatively compared with postoperatively (p=≤0.001) and at FU (p = ≤ 0.001). The analysis of the TCA lat and AP showed initially a significant decrease (p = ≤ 0.001 and p = ≤ 0.001, respectively). However, a significant deterioration of the TCA lat in the FU control compared with postoperatively (p = ≤ 0.001) was seen. A permanent improvement of the TCA AP could not be seen (preoperative to FU) (Table 2).
Comparison of the radiological parameters between JNF and JF
A significant difference of the radiological parameters between JNF and JF was only detected for the CP preoperatively (p = ≤ 0.05). All other parameters showed no significant differences between the two matched pair study groups (Fig. 3, Table 2).
The interrater reliability of the radiographic measurements was calculated at 0.81.
Discussion
The treatment of JNF with SA is still discussed controversially. Recent studies report good success rates in treating JNF with SA compared with other treatment modalities. However, opponents view the treatment SA rather sceptically.9,12-14
We could show in a matched-pair study design, that SA results in a significant improvement of the flatfoot deformity in children with and without neurological impairment by ICP. In both, JNF and JF, a significant decrease of the NCI was seen. In addition, CP and TMTI also improved in the group without ICP. In summary, no relevant negative effect of surgery on outcome compared with preoperatively was seen. The comparison of the two groups revealed only a significant change of CP preoperatively. In both groups, relevant complications after surgery were not detected.
Therapy recommendations for treatment of JNF are diverse and still under critical investigation.13 Currently, especially calcaneal osteotomies, muscle tendon transfers and arthrodeses are conducted. Evan’s calcaneal lengthening osteotomy, for example, has shown good results in treatment of JNF in many studies.14,15 Zeifang et al16 showed in their prospective study excellent and good outcomes in 65.2% of JNF treated with Evan’s osteotomy (poor outcome: 15.2%). However, the main disadvantages of calcaneal osteotomies are invasiveness and a long rehabilitation time with partial weight-bearing until the osteotomy is consolidated. Muscle tendon transfers or combined interventions are also successful in treating flatfeet in both healthy and neurological patients.17-19 Being less invasive than calcaneal osteotomies, these surgical options also have a longer recovery time with partial weight-bearing and/or plaster retention therapy. Further therapy options for JNF are different types of arthrodeses. Here, Bollmann et al20 showed a significant improvement in long-term examinations of radiological parameters after Grice-Green subtalar arthrodesis but the loss of range of movement in the subtalar joint must be critically considered in those young patients.
Therefore, SA is recently being discussed as another alternative minimally invasive treatment option. However, there is no consensus as to whether SA is useful in treating flatfeet in patients with neurological diseases.1,12 Smith et al12 showed that arthroereisis with the Sta-Peg system (Smith-Design, Wright Medical, Memphis, TN, USA) is not successful in patients with ICP and the authors connect the therapy failure to the disorder in the muscles. Related to this, one main aspect in discussion is that the success of SA is based not only on the mechanical blocking of the subtalar joint and calcaneus but also by influence of the proprioceptive system and herewith muscle groups that actively raise the longitudinal arch of the foot.
Until now, this additional effect by SA has not been proven in children with neurological diseases. However, other authors assume that the spastic malposition cannot only be explained by hyperfunction of a muscle group but also by weakness of the antagonist muscles.11,21 JNF can be related to shortening of the gastrocnemius muscle and/or spastic peroneal muscles respectively to weakness of the extensors and supinators. In our study we have not seen children with spastic peroneal muscles. But the improvement of the radiological parameters in patients with JNF could be an explanation for the success of SA even in neurological flatfeet with or without shortening of the gastrocnemius muscle. Confirming our findings, recent studies showed a successful mid-term outcome of nonfusion SA using a subtalar joint stabilizer in comparison with Dennyson-Fulford subtalar arthrodesis.9
Another advantage of SA is the low complication rate postoperatively22,23 in comparison with osteotomies and arthodeses.16,20 This is also consistent with our results. No complications occurred in either of our two groups. Nevertheless, soft-tissue procedures like operations according to Baumann or Strayer respectively for Achilles tendon lengthening are necessary to treat flatfeet with a pes equinus component.24,25
Limitations of our study are that further analysis of subgroups according to the different GMFCS levels was not suitable because of the relatively small patient group which is mainly based on the restrictive inclusion criteria for the matched-pair design. Furthermore, the impact of additional soft-tissue surgery with plaster treatment postoperatively is not further analyzed. Clinical scores were also not collected, because these could not be adequately assessed due to the underlying neurological disease. In addition, further analyses such as gait analysis, pedobarography and energy consumption are needed to supplement the results. Therefore, the focus was on the radiological outcome.
Conclusion
Based on this data, treatment of flatfeet by SA in patient with neurological disorders shows an improvement of radiological parameters comparable with neurologically unimpaired patients and might be considered as additional treatment option.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (Ethics committee vote of the local University, study no. 5571).
Informed consent: Not required for this type of study.
ICMJE Conflict of interest statement
All author declare that they have no conflict of interest.
Author Contributions
HK: analyzed data and wrote the paper.
CL, MH and MR: collected data.
BW and RK: analyzed data.
RK and HP: initiated and supervised the project.
References
- 1.Molayem I, Persiani P, Marcovici LL, Rosi S, Calistri A, Villani C. Complications following correction of the planovalgus foot in cerebral palsy by arthroereisis. Acta Orthop Belg 2009;75:374-379. [PubMed] [Google Scholar]
- 2.Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg [Am] 1995;77-A:500-512. [DOI] [PubMed] [Google Scholar]
- 3.Chang J-H, Wang S-H, Kuo C-L, et al. Prevalence of flexible flatfoot in Taiwanese school-aged children in relation to obesity, gender, and age. Eur J Pediatr 2010;169:447-452. [DOI] [PubMed] [Google Scholar]
- 4.Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics 2006;118:634-639. [DOI] [PubMed] [Google Scholar]
- 5.Panichawit C, Bovonsunthonchai S, Vachalathiti R, Limpasutirachata K. Effects of foot muscles training on plantar pressure distribution during gait, foot muscle strength, and foot function in persons with flexible flatfoot. J Med Assoc Thai 2015;98(suppl 5):S12-S17. [PubMed] [Google Scholar]
- 6.Barg A, Hörterer H, Jacxsens M, et al. Dwyer osteotomy : lateral sliding osteotomy of calcaneus. Oper Orthop Traumatol 2015;27:283-297. [DOI] [PubMed] [Google Scholar]
- 7.Evans D. Calcaneo-valgus deformity. J Bone Joint Surg [Br] 1975;57-B:270-278. [PubMed] [Google Scholar]
- 8.Sekiya JK, Saltzman CL. Long term follow-up of medial column fusion and tibialis anterior transposition for adolescent flatfoot deformity. Iowa Orthop J 1997;17:121-129. [PMC free article] [PubMed] [Google Scholar]
- 9.Wen J, Liu H, Xiao S, et al. Comparison of mid-term efficacy of spastic flatfoot in ambulant children with cerebral palsy by 2 different methods. Medicine (Baltimore) 2017;96:e7044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Pellegrin M, Moharamzadeh D, Strobl WM, et al. Subtalar extra-articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children. J Child Orthop 2014;8:479-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hefti F. Kinderorthopädie in der Praxis. Heidelberg: Springer-Verlag, 2015. [Google Scholar]
- 12.Smith PA, Millar EA, Sullivan RC. Sta-Peg arthroereisis for treatment of the planovalgus foot in cerebral palsy. Clin Podiatr Med Surg 2000;17:459-469. [PubMed] [Google Scholar]
- 13.Frances JM, Feldman DS. Management of idiopathic and nonidiopathic flatfoot. Instr Course Lect 2015;64:429-440. [PubMed] [Google Scholar]
- 14.Waizy H, Plaass C, Brandt M, et al. Extra-articular arthroereisis according to Grice/Green versus calcaneal lengthening according to Evans: retrospective comparison for therapy of neurogenic pes planovalgus. Orthopade 2013;42:409-417. [DOI] [PubMed] [Google Scholar]
- 15.Rhodes J, Mansour A, Frickman A, et al. Comparison of allograft and bovine xenograft in calcaneal lengthening osteotomy for flatfoot deformity in cerebral palsy. J Pediatr Orthop 2017;37:e202-e208. [DOI] [PubMed] [Google Scholar]
- 16.Zeifang F, Breusch SJ, Döderlein L. Evans calcaneal lengthening procedure for spastic flexible flatfoot in 32 patients (46 feet) with a followup of 3 to 9 years. Foot Ankle Int 2006;27:500-507. [DOI] [PubMed] [Google Scholar]
- 17.Ramanujam CL, Stapleton JJ, Zgonis T. Tibialis anterior tendon transfer for posterior tibial tendon insufficiency. Clin Podiatr Med Surg 2016;33:21-28. [DOI] [PubMed] [Google Scholar]
- 18.Samaila E, Bonetti I, Bruno C, Argentini E, Magnan B. Navicular tenosuspension with anterior tibialis tendon (Young procedure) associated to calcaneo-stop for the treatment of paediatric flexible flatfoot: clinical and ultrasound study. Acta Biomed 2016;87(suppl 1):69-74. [PubMed] [Google Scholar]
- 19.Kou JX, Balasubramaniam M, Kippe M, Fortin PT. Functional results of posterior tibial tendon reconstruction, calcaneal osteotomy, and gastrocnemius recession. Foot Ankle Int 2012;33:602-611. [DOI] [PubMed] [Google Scholar]
- 20.Bollmann C, Franz A, Raabe J. The Grice-Green subtalar arthrodesis using a fibular bone graft—follow-up of 92 patients. Z Orthop Unfall 2015;153:93-98. [DOI] [PubMed] [Google Scholar]
- 21.Schweizer K, Romkes J, Brunner R. The association between premature plantarflexor muscle activity, muscle strength, and equinus gait in patients with various pathologies. Res Dev Disabil 2013;34:2676-2683. [DOI] [PubMed] [Google Scholar]
- 22.Metcalfe SA, Bowling FL, Reeves ND. Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: a critical review of the literature. Foot Ankle Int 2011;32:1127-1139. [DOI] [PubMed] [Google Scholar]
- 23.Smyth NA, Aiyer AA, Kaplan JR, Carmody CA, Kadakia AR. Adult-acquired flatfoot deformity. Eur J Orthop Surg Traumatol 2017;27:433-439. [DOI] [PubMed] [Google Scholar]
- 24.Nelson SC, Haycock DM, Little ER. Flexible flatfoot treatment with arthroereisis: radiographic improvement and child health survey analysis. J Foot Ankle Surg 2004;43:144-155. [DOI] [PubMed] [Google Scholar]
- 25.Rong K, Ge WT, Li XC Xu XY. Mid-term results of intramuscular lengthening of gastrocnemius and/or soleus to correct equinus deformity in flatfoot. Foot Ankle Int 2015;36:1223-1228. [DOI] [PubMed] [Google Scholar]