Abstract
Purpose
This study quantified toe-walking trends and treatment decisions in patients with autism spectrum disorder (ASD) in the United States between 2005 and 2016 using a large national private-payer database.
Methods
A retrospective database review was performed on paediatric patients with ASD, and for International Classification of Diseases-9/10 diagnosis codes for toe-walking. Patients were filtered based on treatment type by Current Procedural Terminology (CPT) code. Continued toe-walking rates were assessed for each patient population and treatment group. A Pearson’s chi-squared test was used to evaluate differences in group characteristics.
Results
Of 2 221 009 paediatric patients in the database, 5739 patients had a diagnosis of ASD, and 8.4% of patients with ASD also had a diagnosis of toe-walking (n = 484). For typically developing children in the database, 0.47% of patients had a diagnosis of persistent toe-walking. In all, 59.3% of ASD patients underwent physical therapy, 7.4% serial casting and 3.3% surgical correction, compared with 38.1%, 3.6% and 1.2% of normally developing children, respectively (chi-square 6.4031; p < 0.040699). Without intervention, 63.6% of patients with ASD continued to toe-walk within ten years of their diagnosis, with 19.3% of patients without ASD (chi-square 82.9762; p < 0.0001).
Conclusion
This study supports the association between a greater prevalence of toe-walking in children with ASD. We showed that patients with ASD and toe-walking receive surgical correction at nearly triple the rate of children without ASD who toe-walk. The continued rate of toe-walking is comparable between treatment groups as well as between ASD and typically developing children. Typically developing children have higher rates of toe-walking resolution without intervention than children with ASD.
Level of evidence
Level II
Keywords: autism, toe-walking, treatment trends
Introduction
Toe-walking is an abnormal gait pattern that can be seen in children during development. The majority of toe-walking cases will regress naturally within six months or after two years of age; children who continue beyond this time are dignosed with persistent toe-walking.1 While long-term effects of toe-walking have not yet been fully elucidated, many gait changes have been noted in patients with long-standing toe-walking.2,3 Toe-walking can be observed in variety of conditions, including cerebral palsy (CP), muscular dystrophy, Charcot-Marie-Tooth Disease and other neuropathies and myopathies, due to anatomical pathology present in the extremities of these patients.4-6 Idiopathic toe-walking (ITW) is the diagnosis of persistent toe-walking in the absence of these neuro-motor conditions.
The prevalence of persistent ITW in children is estimated at around 2.1% and has been associated with language disorders and other developmental delays.5-8 In contrast, the prevalence of persistent ITW in patients with neuropsychiatric conditions has been reported to be as high as 41%.5 Patients with autism spectrum disorder (ASD) in particular have been noted to have an increased prevalence of ITW.4,9-11 While the underlying mechanism behind the increased rates of toe-walking in patients with ASD remains widely unknown, it is believed to be associated with underlying differences in tactile/sensory responses that are often seen in patients with this neuropsychiatric disease.4,6,12,13
The prevalence of ASD is increasing and the causes have been under investigation. Current data suggested that the increase in prevalence in the past 30 years is not due to the changes in diagnostic criteria14. The criteria for ASD are: three social-communication criteria (lack of socio-emotional reciprocity, deficits in non-verbal communication, impairment in developing and maintaining relationships) and two out of four non-social criteria (stereotypic behaviours, restricted interests, cognitive inflexibility, sensory aberrations). The diagnosis of autism or CP should raise suspicion of the other. Based on a systematic review that investigated co-occurrence of CP and autism15, the prevalence of autism in CP varies widely from 2% to 30%, while the prevalence of CP in ASD varies from 2.9% to 4.3%.
According to Schoenecker and Rich16 patients with persistent toe-walking are recommended to undergo conservative management including physical therapy or serial casting before surgical options.17,18 Studies investigating the effectiveness of these treatment options are varied, with the natural history of sustained ITW remaining uncertain.1,2,17,18,20,21 To our knowledge, current ITW treatment guidelines do not include specific recommendations for patients with comorbid conditions like ASD, and nonoperative treatments may be more challenging in patients with ASD if the patient has difficulty complying with instructions, sensitivity to tactile foot sensations/manipulation or is disturbed by the noise of cast saws. Medical treatment decisions should consider family preference, severity of the patient’s condition, as well as any comorbid conditions.
Our study aims to determine the rates at which patients with and without ASD who have persistent toe-walking are treated with various techniques (e.g. physical therapy, casting or tendon lengthening surgery), and compare secondary demographic characteristics and toe-walking outcomes of these patients. We hypothesize that patients with a diagnosis of ASD who present with persistent toe-walking are more likely to be treated with surgery because of the sensorineural aberrations of children with ASD that may complicate treatment with non-surgical measures.
Methods
We conducted a retrospective database review of patients within the PearlDiver Patient Record Database (PearlDiver Technologies Inc, Warsaw, Indiana). PearlDiver is a commercially available searchable online database with information submitted by private insurance companies for patients with orthopaedic diagnoses. The database includes 11 million patients and 117 million records between the years 2005 and 2016. The PearlDiver database does not include any patient data from Medicare, Medicaid or uninsured patients. We chose this database for this study because it is formed through record collections across all age groups including paediatric patients from multiple private payer insurance agencies, the largest contribution of which is from the UnitedHealth Group (Minnetonka, Minnesota).2,7-9
We identified our study population using International Classification of Diseases (ICD)-9-CM, ICD-10-CM and Current Procedural Terminology (CPT) codes22-24, and then filtered based on the patient’s age under 19 years old. We compiled all known toe-walking diagnosis codes (ICD-9-D-7812, ICD-10-D-M6700, ICD-10-D-M6701, ICD-10-D-M6702, ICD-10-D-R2689) and queried patients in our database between the years of 2006 and 2016. Diagnosis of persistent toe-walking for each patient was determined if a diagnosis of toe-walking appeared within their patient chart on more than one encounter, separated by at least six months according to literature definitions.25 We then searched for patients using ICD-9 and ICD-10 diagnosis codes for autism-related diagnoses including ASD (F84.0; 299.0), autistic disorder (299.0), Asperger’s syndrome (F84.5; 299.80) and pervasive developmental disorder (F84.9; 299.9). Next, we filtered all patients by age, including only paediatric patients 18 years or younger, and further filtered out patients with comorbid neuro-motor conditions, including CP, Charcot Marie Tooth, etc.
We subsequently stratified patients based on treatment types, namely physical therapy, foot and ankle casting procedures and surgical procedures. We used ICD-9, ICD-10 and CPT codes to determine the various treatments that were pursued based on the timing of each of the treatments following the toe-walking diagnosis. The breakdown of ICD-9, ICD-10 and CPT codes that were used to query the patient population can be seen in the Table 1. We collected secondary demographic information on all patients within our study population including gender, geographic region, comorbid conditions and any diagnosis of intellectual disability or language delay. Finally, we searched for patients within these queried populations that retained a toe-walking diagnosis code two years following intervention.
Table 1.
International classification of Diseases (ICD)-9, ICD-10 and Current Procedural Terminology (CPT) code descriptions
| Type | ICD-9, ICD-10, CPT | Descriptions |
|---|---|---|
| Toe-walking | ICD-9-D-7812, ICD-10-D-M6700, ICD-10-D-M6701, ICD-10-D-M6702, ICD-10-D-R2689 | Abnormality of gait, tightened Achilles tendon |
| Autism spectrum disorder | ICD-9-D-29900, ICD-9-D-29901, ICD-9-D-29980, ICD-10-D-F840, ICD-10-D-F845, ICD-10-D-F848 | Autistic disorder, Asperger’s syndrome, pervasive developmental disorders not otherwise specified, autism spectrum disorder |
| Neuro-orthopaedic disease | ICD-10-D-G729, ICD-10-D-G809, ICD-10-D-G710 | Cerebral palsy, muscular dystrophy, Charcot-Marie-Tooth |
| Intellectual disability | ICD-9-317, ICD-9-D-3180: ICD-9-D-3182, ICD-9-D-3189. ICD-10-D-F70:ICD-10-D-F73, ICD-19F78. ICD-9-D-31539 | Mild, moderate, severe, profound, and unspecified intellectual disabilities. Speech and language developmental delay |
| Physical therapy | CPT-97001, CPT-97110, CPT-97112, CPT-97760, CPT-S9131 | Physical therapy evaluation, lower leg stretching, Achilles stretching |
| Casting | CPT-29425, CPT-29405 | Lower leg cast, lower leg splint |
| Surgical intervention | CPT-27605, CPT-27606, CPT-27687, CPT-27685, CPT-27654, CPT-28238, CPT-28208 | Tenotomy, percutaneous, Achilles, gastrocnemius recession, open tendo-Achilles lengthening |
A Pearson’s chi-squared test was used to evaluate differences in treatment decisions and the prevalence in patients with versus without an autism-related diagnosis. All statistical analysis was calculated using R Programming (R Project for Statistical Computing, Vienna, Austria).
Results
Toe-walking prevalence and patient characteristics
There were 2 221 009 paediatric patients under the age of 19 years within the PearlDiver Private Payer Database. Of these paediatric patients, there were 5739 patients with ASD. Overall, there were 508 paediatric patients total with a neuro-orthopaedic condition, and 14 014 (0.6%) children with an intellectual disability or language developmental delay. In all, 10 480 patients had persistent toe-walking in the absence of a neuro-orthopaedic condition or ASD.
In all, 8.4% of patients with a diagnosis of ASD also had a diagnosis of toe-walking (n = 484). For typically developing children, 0.47% of patients had a diagnosis of persistent toe-walking. A total of 21.5% (n = 1236) of children with ASD had a comorbid intellectual disability. There was no significant difference in prevalence of toe-walking in patients with ASD and intellectual disability as compared with patients with ASD without an intellectual disability.
In all, 56.8% of patients with both ASD and toe-walking were also diagnosed with intellectual disability. For patients with toe-walking without ASD, 11.1% of patients had an intellectual disability or language development delay. There was almost a 3:1 male to female ratio in patients with ASD and toe-walking (362:122), while there was roughly 1:1 (5703:4777) male to female ratio for children with toe-walking in the absence of ASD.
Treatment decisions
In all, 59.3% (n = 287) of patients with ASD and persistent toe-walking underwent physical therapy, 7.4% (n = 36) underwent serial casting and 3.3% (n = 16) underwent surgical correction for their gait abnormality. There was no documented toe-walking treatment for 30.0% (n = 145) of these patients. Of the 10 480 patients with toe-walking without a diagnosis of ASD, 57.2% (n = 5995) of patients did not have a documented toe-walking intervention. Of the typically developing children, 38.1% (n = 3989) underwent physical therapy, 3.6% (n = 374) serial casting and 1.2% (n = 122) underwent surgical correction (chi-square 6.4; p = 0.041). Of patients who were treated surgically, 54.4% (n = 68) of patients without a diagnosis of ASD were first treated with serial casting prior to surgical intervention. In comparison, for patients with ASD and persistent toe-walking, 31.25% (n = 5) patients were first treated with serial casting before a surgical option was pursued (chi-square 0.98; p = 0.32) (Fig. 1). There were no other significant differences in demographic factors between the two groups.
Fig. 1.
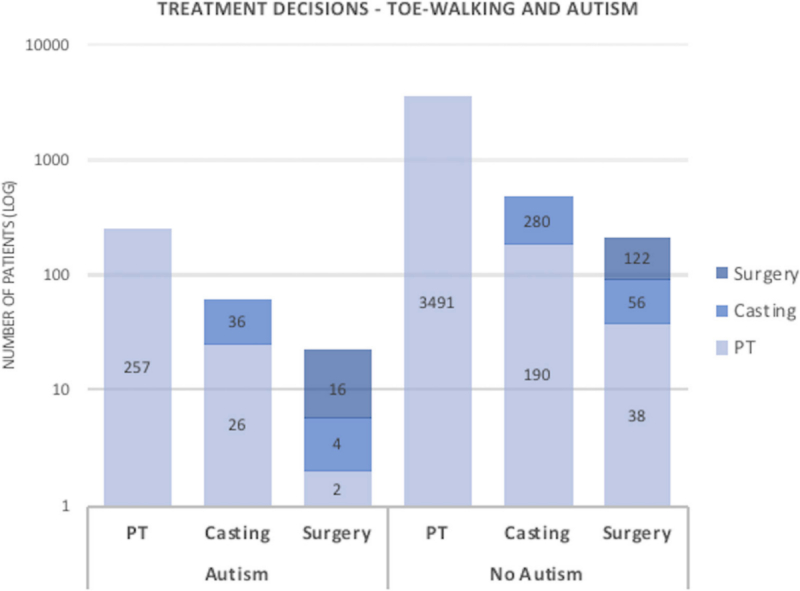
Treatment decisions (PT, physical therapy).
Patient outcomes
For patients with ASD and toe-walking that were treated with physical therapy alone, 63.8% (n = 183) patients continued to toe-walk within two years of treatment. In all, 47.2% (n = 17) of patients that were treated with casting alone continued to toe-walk within two years of treatment, while 48.1% (n = 13) that had undergone both physical therapy and casting continued to toe-walk within two years of final treatment. Of the patients with ASD and toe-walking that were treated surgically, 75% (n = 12) of patients continued to toe-walk within two years of treatment, and 100% (n = 5) of those who had first underwent casting prior to surgical intervention.
In comparison, for toe-walkers without ASD, 54.0% (n = 2154) continued to toe-walk after being treated with physical therapy alone. A total of 52.9% (n = 198) continued to toe-walk following treatment with casting, and 63.4% (n = 137) with a combination of physical therapy and casting. For patients that were treated surgically, 67.2% (n = 68) continued to toe-walk following invention. For the patients that had received casting prior to surgery, 71.2% (n = 47) of patients continued to toe-walk following surgery (chi-square 2.9901; p = 0.224241).
Finally, for patients that did not receive any documented intervention, 63.6% (n = 91) of patients with ASD continued to toe-walk within ten years of their diagnosis, while 19.3% (n = 1159) of patients without a diagnosis of ASD continued to toe-walk within ten years of their first documented toe-walking diagnosis (chi-square 83.0; p < 0.0001) (Table 2).
Table 2.
Breakdown of treatment decisions and toe-walking continuation
| Surgery | Casting | PT | No intervention* | Total | ||
|---|---|---|---|---|---|---|
| Autism and toe-walking | n | 16 | 36 | 287 | 145 | 484 |
| cTW, n (%) | 12 (75) | 17 (47.2) | 183 (63.7) | 91 (63.6) | ||
| Toe-walking without autism | n | 122 | 374 | 3989 | 5995 | 10 480 |
| cTW, n (%) | 68 (55.7) | 198 (52.9) | 2154 (54.0) | 1159 (19.33) |
chi-square 98.0017; p < 0.0001
cTW, continued toe-walking
Discussion
Previous studies looking at the prevalence of persistent toe-walking in patients with a neuropsychiatric disease demonstrated a prevalence of around 40.1%, about 20 times greater than that of the normal population (2.1%).4,5 These studies, however, included less than 40 patients with ASD, and have been generalized to neuropsychiatric conditions as a whole. Our study is currently the largest of its kind to evaluate the prevalence of persistent toe-walking in patients with ASD. Our results demonstrate that roughly 9% of patients with ASD have a diagnosis of toe-walking as compared with less than 0.5% of children with no ASD diagnosis. These results add to the growing body of literature demonstrating increased rates of ITW in patients with ASD. Our results further support the link between intellectual disability/language developmental delay and toe-walking in patients without a diagnosis of ASD.6,26
Treatment trends in patients with toe-walking and ASD, however, have not been compared with those seen in typically developing children. Patients with ASD and persistent toe-walking get surgery to correct the issue at almost three times the rate that patients with persistent toe-walking and no ASD undergo surgical intervention (3.7% versus 1.2%). In addition, over half of patients with toe-walking without ASD who had pursued a surgical option had serial casting prior to invasive intervention, compared with less than 40% of patients with ASD. Patients with ASD also underwent casting as a treatment in larger amounts than their non-ASD counterparts (7.4% to 3.5%). Despite the senior author’s (SF) clinical experience of sustained improvement in gait in ASD patients treated surgically, this study found surgical correction outcomes for patients with ASD lower than those seen for patients without ASD, thus it is important to counsel families as to how the underlying neurological condition may lessen the rate of treatment success.
The literature surrounding the efficacy of treatment methods for toe-walking are varied. Long-term effects of toe-walking still have not been fully elucidated, though biomechanical as well as gait changes have been noted in patients with toe-walking over many years.19,27 Dietz and Khunsree20 concluded that toe-walking treatments are largely cosmetic in nature, and that, if parents wish to correct this abnormal gait, surgical correction is often the most effective, and rapid, method to do so. Weiss et al8 on the other hand, noted that regardless of intervention, there remains a high probability that patients continue to toe-walk.2,18,27 Our results demonstrate poor rates of toe-walking resolution in patients with ASD, although it is possible that the diagnosis code of toe-walking was retained in the medical records of patients treated for toe-walking even though the toe-walking had resolved. It is also possible that ASD patients have underlying neurophysiological difference that result in a higher percentage of persistent toe-walking as compared with typically developing children (i.e. a less favourable natural history than ITW patients).
Orthopaedic decisions often take many factors into consideration when determining which treatment option to pursue. Our study demonstrates that although the research surrounding the efficacy of various treatment techniques to address persistent toe-walking is limited, surgical options are more likely to be pursued in patients with ASD than in typically developing patients. The decision-making process for parents of patients with ASD offers unique challenges compared with that of parents of typically developing children. Studies have reported barriers in communication, physicians’ lack of knowledge about specific ASD treatments and community resources and uncertainty about the paediatricians’ role in making treatment recommendations for a child with ASD.28 It is imperative that surgeons recognize any underlying biases that may influence their decision to operate or pursue casting in a patient with sensorineural sensitivities in order to reach the best decision for the patient and family. It is also possible that the three-fold higher rate of surgical treatment in ASD patients is related to a higher incidence of contracture development in this patient population, but this database review study does not allow us to assess the degree or incidence of gastrocsoleus contractures.
Our study has some limitations. Of note, the patient population from the PearlDiver is a selected population; its information is acquired only through private payer medical claims. It does not include patients with Medicaid. However, given the database’s large size, the patient population likely remains representative. Furthermore, our study is retrospective and observational, thus preventing causal inferences. Over the years, ASD diagnoses have increased in incidence, with accounts of less severe forms of autism than previously reported.29-31 It is possible that our patient population may not have severe variants of autism disease that may be linked to even greater gait abnormalities. As in other large database studies, this study is dependent on accurate coding of diagnoses in the database.
Despite these limitations, our large dataset allowed us to assess toe-walking treatment trends in patients with and without ASD. Future prospective studies are needed to evaluate the efficacy of these treatment techniques in patients with ASD compared with typically developing children. Results from this study may help surgeons with treatment recommendations, and eventually develop evidence-based treatments. In addition, the evaluation of paediatric orthopaedic surgeon rationales for pursuing various treatment modalities within these patient populations would help both surgeons and parents facilitate conversations about treatment decisions for a child with toe-walking and ASD.
Conclusion
A greater prevalence of toe-walking in children with ASD as compared with typically developing patients has been reported. Using a national private-payer database, this study supports this association. We also identified treatment patterns within the study population, showing that patients with ASD and toe-walking receive surgical correction for their gait abnormality at nearly triple the rate of children without a diagnosis of ASD who toe-walk. For patients with toe-walking and ASD who undergo surgical correction, serial casting was used less frequently prior to surgical intervention. All treatment decisions demonstrate comparable rates of toe-walking resolution, with patients without ASD ‘outgrowing’ their toe-walking without intervention at a greater level than patients with ASD.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: We did not require IRB clearance for this project, and no human participants and/or animals were involved.
Informed consent: No informed consent was necessary in this study, as all patient data was de-identified prior to collection in the PearlDiver database. No informed consent was necessary in this study, as all patient data was de-identified prior to collection in the PearlDiver database.
ICMJE Conflict of interest statement
None declared.
Author Contributions
Each author listed above contributed significantly to, and is willing to take public responsibility for, one or more aspects of the study. All authors participated in the study design and analysis and interpretation of the data. All authors were actively involved in drafting and the critical revision of the manuscript and have given final approval of the version to be submitted.
References
- 1.Ruzbarsky JJ, Scher D, Dodwell E. Toe walking: causes, epidemiology, assessment, and treatment. Curr Opin Pediatr 2016;28:40-46. [DOI] [PubMed] [Google Scholar]
- 2.Davies K, Black A, Hunt M, Holsti L. Long-term gait outcomes following conservative management of idiopathic toe walking. Gait Posture 2018;62:214-219. [DOI] [PubMed] [Google Scholar]
- 3.Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthop Trauma 2016;30:232-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrow WJ, Jaworski M, Accardo PJ. Persistent toe walking in autism. J Child Neurol 2011;26:619-621. [DOI] [PubMed] [Google Scholar]
- 5.Engström P, Tedroff K. Idiopathic toe-walking: prevalence and natural history from birth to ten years of age. J Bone Joint Surg [Am] 2018;100:640-647. [DOI] [PubMed] [Google Scholar]
- 6.Accardo P, Whitman B. Toe walking. A marker for language disorders in the developmentally disabled. Clin Pediatr (Phila) 1989;28:347-350. [DOI] [PubMed] [Google Scholar]
- 7.Accardo P, Morrow J, Heaney MS, Whitman B, Tomazic T. Toe walking and language development. Clin Pediatr (Phila) 1992;31:158-160. [DOI] [PubMed] [Google Scholar]
- 8.Weiss MJ, Moran MF, Parker ME, Foley JT. Gait analysis of teenagers and young adults diagnosed with autism and severe verbal communication disorders. Front Integr Nuerosci 2013;7:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ming X, Brimacombe M, Wagner GC. Prevalence of motor impairment in autism spectrum disorders. Brain Dev 2007;29:565-570. [DOI] [PubMed] [Google Scholar]
- 10.Shetreat-Klein M, Shinnar S, Rapin I. Abnormalities of joint mobility and gait in children with autism spectrum disorders. Brain Dev 2014;36:91-96. [DOI] [PubMed] [Google Scholar]
- 11.Kindregan D, Gallagher L, Gormley J. Gait deviations in children with autism spectrum disorders: a review. Autism Res Treat 2015;2015:741480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Güçlü B, Tanidir C, Mukaddes NM, Ünal F. Tactile sensitivity of normal and autistic children. Somatosens Mot Res 2007;24:21-33. [DOI] [PubMed] [Google Scholar]
- 13.Sala DA, Shulman LH, Kennedy RF, Grant AD, Chu ML. Idiopathic toe-walking: a review. Dev Med Child Neurol 41:846-848. [DOI] [PubMed] [Google Scholar]
- 14.Fung LK, Hardan AY. Autism in DSM-5 under the microscope: implications to patients, families, clinicians, and researchers. Asian J Psychiatr. 2014;11:93-97. [DOI] [PubMed] [Google Scholar]
- 15.Craig F, Savino R, Trabacca A A systematic review of comorbidity between cerebral palsy, autism spectrum disorders and Attention Deficit Hyperactivity Disorder. Eur J Paediatr Neurol. 2019. January;23(1):31-42. [DOI] [PubMed] [Google Scholar]
- 16.Schoenecker PL, Rich MM. The Lower Extremity: Morrisy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopaedic. 6th ed. Philadelphia, PA: Lippincott Wilkins Williams; 2006:1204-1206. [Google Scholar]
- 17.Fox A, Deakin S, Pettigrew G, Paton R. Serial casting in the treatment of idiopathic toe-walkers and review of the literature. Acta Orthop Belg 2006;72:722-730. [PubMed] [Google Scholar]
- 18.van Bemmel AF, van de Graaf VA, van den Bekerom MPJ, Vergroesen DA. Outcome after conservative and operative treatment of children with idiopathic toe walking: a systematic review of literature. Musculoskelet Surg 2014;98:87-93. [DOI] [PubMed] [Google Scholar]
- 19.listed No authors. Evidence-based care guideline for management of idiopathic toe walking in children and young adults ages 2 through 21 years. Cincinnati Children’s Hospital Medical Center. NGC:008544 — Guidelines International Network. https://www.g-i-n.net/library/health-topics-collection/guidelines/ahrq-us/evidence-based-care-guideline-for-management-of-idiopathic-toe-walking-in-children-and-young-adults-ages-2-through-21-years.-cincinnati-childrens-hospital-medical-center.-ngc-008544 (date last accessed 10 July 2018).
- 20.Dietz F, Khunsree S. Idiopathic toe walking: to treat or not to treat, that is the question. Iowa Orthop J 2012;32:184-188. [PMC free article] [PubMed] [Google Scholar]
- 21.Pomarino D, Ramírez Llamas J, Martin S, Pomarino A. Literature review of idiopathic toe walking: etiology, prevalence, classification, and treatment. Foot Ankle Spec 2017;10:337-342. [DOI] [PubMed] [Google Scholar]
- 22.2018 ICD-10 CM and GEMs - Centers for Medicare & Medicaid Services [Internet]. Cms.gov. 2019. [cited 14 June 2019]. Available from: https://www.cms.gov/Medicare/Coding/ICD10/2018-ICD-10-CM-and-GEMs.html. [Google Scholar]
- 23.ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles - Centers for Medicare & Medicaid Services [Internet]. Cms.gov. 2014. [cited 14 June 2019]. Available from: https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html. [Google Scholar]
- 24.CPT® (Current Procedural Terminology) [Internet]. American Medical Association. 2019. [cited 14 June 2019]. Available from: https://www.ama-assn.org/amaone/cpt-current-procedural-terminology. [Google Scholar]
- 25.Sivaramakrishnan S, Seal A. Fifteen-minute consultation: A child with toe walking. Arch Dis Child Educ Pract Ed 2015;100:238-241. [DOI] [PubMed] [Google Scholar]
- 26.Accardo PJ, Barrow W. Toe walking in autism: further observations. J Child Neurol 2015;30:606-609. [DOI] [PubMed] [Google Scholar]
- 27.McMulkin ML, Baird GO, Caskey PM, Ferguson RL. Comprehensive outcomes of surgically treated idiopathic toe walkers. J Pediatr Orthop 2006;26:606-611. [DOI] [PubMed] [Google Scholar]
- 28.Levy SE, Frasso R, Colantonio S, et al. Shared decision making and treatment decisions for young children with autism spectrum disorder. Acad Pediatr 2016;16:571-578. [DOI] [PubMed] [Google Scholar]
- 29.Fombonne E. Epidemiology of pervasive developmental disorders. Pediatr Res 2009;65:591-598. [DOI] [PubMed] [Google Scholar]
- 30.Powell JE, Edwards A, Edwards M, et al. Changes in the incidence of childhood autism and other autistic spectrum disorders in preschool children from two areas of the West Midlands, UK. Dev Med Child Neurol 2000;42:624-628. [DOI] [PubMed] [Google Scholar]
- 31.Barbaresi WJ, Colligan RC, Weaver AL, Katusic SK. The incidence of clinically diagnosed versus research-identified autism in Olmsted County, Minnesota, 1976-1997: results from a retrospective, population-based study. J Autism Dev Disord 2009;39:464-470. [DOI] [PMC free article] [PubMed] [Google Scholar]


