Abstract
Objectives
Gathering relevant patient information during over-the-counter (OTC) consultations increases the likelihood of safe, effective and person-centred outcomes. The aim of this study was to explore the key determinants to information gathering during consultations for non-prescription medicine requests in community pharmacies in Scotland.
Design
Semi-structured interviews using the Theoretical Domains Framework (TDF), with community pharmacy teams across Scotland. Interviews explored participants’ knowledge of current guidance, skills required to elicit information and barriers and facilitators associated with this behaviour. Theory-based content analysis was undertaken using the TDF as an initial coding framework to identify key determinants and map them to salient domains. Salience was determined by prominence or variation in views. Comparative analysis was undertaken by professional role.
Results
Thirty interviews were conducted with pharmacists (n=19) and medicine counter assistants (MCAs) (n=11). Eight salient domains were identified: environmental context and resources (privacy), beliefs about consequences (patient safety), skills (communication, decision-making), social influences (patient awareness of pharmacist role), knowledge (awareness and use of standard operating procedures), social professional role and identity (perception of own role), behavioural regulation (training) and intention (to gather information). Similar domains were salient for pharmacists and MCAs; however, different beliefs were associated with different roles. Overarching themes were identified: best practice, health literacy, decision-making and professionalism.
Conclusions
Multiple influences and complexities affect the effective management of OTC consultations. While similar factors impact on both pharmacists and MCAs at a patient, professional and environmental level, subtle differences exist in how these influence their management of OTC consultations. This study highlights the importance of tailoring interventions to reflect different roles, functions and responsibilities of community pharmacy personnel.
Keywords: community pharmacy services, quality improvement, health care research, theoretical domains framework, qualitative research
Strengths and limitations of this study.
This is the first theoretically underpinned exploration of the determinants of information gathering during over-the-counter consultations in community pharmacies in Scotland.
This is also the first study to explore these determinants by professional role.
We achieved a wide representation of participants from across Scotland, however remote and rural areas were under-represented.
This study was conducted across Scotland; therefore, the results may not be generalisable to community pharmacy personnel in other countries. These findings, however, are not intended to be generalisable, but to provide an insight into the behaviour of interest to inform future research, practice and policy.
Introduction
Around 18 million general practice (GP) consultations and 650 000 emergency department (ED) consultations are for conditions which could be treated using over-the-counter (OTC) medicines supplied from community pharmacies.1 It is estimated that in the UK, consultations for minor ailments in EDs and GP cost around £1.1 billion, however equivalent health outcomes can be achieved with care provided from community pharmacies.2 Community pharmacies have been identified as an ‘under-utilised resource’ with the potential to reduce the burden on other primary care providers.3 Recently, there has been an increasing recognition of the contribution that community pharmacy can have on improving public health and a drive towards integrating pharmacy into the wider UK public health workforce.4
In 2013, the Scottish Government highlighted their commitment towards enhancing the role of the pharmacy team through ‘Prescription for Excellence’, its vision and action plan for pharmaceutical care.5 More recently, their 2017 strategy ‘Achieving Excellence in Pharmaceutical Care’6 reinforced this, encouraging people to use their community pharmacy as a first port of call for healthcare advice. This strategy highlights that it is only through making full use of the clinical capacity in community pharmacies that real gains in clinical care can be achieved.
In the UK, there are three broad categories of medicines: prescription only medicines, pharmacy only (P) and general sales list.7 OTC consultations involve P and GSL medicines. Medicine counter assistants (MCAs) are the members of community pharmacy personnel most often involved in the sale of OTC medicines.8 9 MCAs work under the supervision of a pharmacist and must complete an accredited MCA course or relevant units of a dispensing assistant or pharmacy technician course to undertake this role.10 Currently, there is no requirement for further MCA training postqualification.11 Concerns exist regarding the risks associated with the public’s enhanced access to these medicines, as well as with the ability of community pharmacy staff to ensure the safe and effective supply of reclassified medicines.12–15
One means of ensuring optimal management of these consultations is through effective information gathering.16–18 While several frameworks exist to promote information gathering, with Who, What, How long, Action to date, other existing Medication being taken (WWHAM)19 being the most commonly cited in the UK, there is substantial evidence to suggest that the information gathered during OTC consultations is sub-optimal.20 21
The Translation research in a dental setting (TRiaDS) programme, funded by NHS Education for Scotland (NES) uses a framework for the translation of guidance and translation into practice.22 The scope of the TRiaDS programme was extended in 2013 to include community pharmacy. The TRiaDS in Pharmacy (TRiaDS-P) programme comprised four stages1: a service-driven prioritisation exercise to identify priorities for community pharmacy practice improvement in Scotland. Through a systematic, service-driven prioritisation exercise, effective management of OTC consultations was selected as the target for improvement2 23; semi-structured interviews to explore the key determinants to information gathering during OTC consultations3; a national theory-based survey to identify key determinants of the target behaviour4; intervention development comprising identification of options for practice improvement interventions.
Stage 1 of the programme identified that the optimal management of OTC consultations is dependent on effective information gathering13 16 17 and as such, this formed the target behaviour of stage 2, explored by this current study, the purpose of which was to identify the key determinants to information gathering during consultations for P medicine requests in community pharmacies in Scotland.
Methods
Study design and setting
This study comprised a series of semi-structured telephone interviews underpinned by the Theoretical Domains Framework (TDF).24 The TDF was developed as a theoretical framework for use in implementation research. It includes a number of behavioural theories and constructs and proposes that determinants of healthcare professionals’ behaviour can be clustered into 14 ‘domains’. The TDF has been widely used to identify barriers and facilitators to evidence-based practice, as well as to explain variation in practice and fits into an intervention development methodology (Behaviour change wheel) that assists with developing a theory-based intervention.24–26 One of the benefits of applying this theory is the ability to assess implementation problems and support intervention design.27 In addition, interviews guided by the TDF have been found to encourage participants to consider a wider range of influences on behaviour than other interview approaches.28
Participants
Community pharmacists and MCAs working in community pharmacies across Scotland were eligible to participate. Invitations were emailed to all community pharmacists registered on the NES Portal (approximately 4000). This is a national online course booking and management system which includes information relating to all Continuing Professional Development (CPD) events offered by NES. Pharmacists must be registered on the NES Portal to participate in and received CPD accreditation for these events. Potential pharmacist participants were asked to identify MCAs within their pharmacy who were also willing to participate and to complete a brief electronic questionnaire to gather information regarding their pharmacy characteristics. A maximum variation sample was generated reflecting pharmacy type, Health Board and deprivation. This is appropriate when the sample size is small and if carefully drawn, can be as representative as a random sample.29
Data collection
Semi-structured telephone interviews were conducted using open ended questions and probing to explore information gathering during consultations in community pharmacies. The interview topic guide covered all TDF domains25 (online supplementary file 1) and was piloted with two community pharmacists before the study commenced. Pilot data were excluded from the analysis.
bmjopen-2019-029937supp001.pdf (89.1KB, pdf)
Interviews were conducted by two experienced qualitative researchers (eg, HC) and digitally recorded. Participants were advised that the interviewers were not pharmacists. The recordings were professionally transcribed and anonymised.
Data collection ceased when data saturation was achieved (ie, no new information or insights were gained).
Data handling and analysis
All transcripts were accuracy checked prior to analysis. Data were managed using NVivo V.10 software. Prior to coding, standardisation meetings were held until full agreement was met and finalised coding definitions produced (online supplementary file 2). Duplicate, independent coding was undertaken (HC, EG, RN). Theory-based content analysis was performed30 with transcript utterances classified using the TDF. Once coding at a domain level was complete, each domain was coded into specific beliefs. Beliefs tables were constructed with domains, emergent beliefs and illustrative quotations. Following the approach described by Atkins et al,27 31 the most salient beliefs were identified based on frequency and content i.e. strongly held or divergent view-points. A comparative analysis was undertaken (HC) within and across pharmacists and MCAs to explore convergent and divergent beliefs, based on the number of utterances coded to each domain. Domains were ranked for both pharmacists and MCAs (table 1). Specific beliefs within dominant domains were then explored. Where specific beliefs related to similar aspects of practice, these were grouped and overarching themes were identified.
Table 1.
Mapping to the Theoretical Domains Framework by professional role
| Domain | Pharmacists N (rank) |
MCAs N (rank) |
| Knowledge | 46 (=1) | 25 (1) |
| Environmental context and resources | 46 (=1) | 22 (2) |
| Beliefs about consequences | 32 (3) | 19 (=3) |
| Skills | 30 (=4) | 19 (=3) |
| Social professional role and identify | 30 (=4) | 12 (=6) |
| Social influences | 28 (6) | 15 (5) |
| Behavioural regulation | 27 (7) | 8 (10) |
| Intentions | 20 (8) | 12 (=6) |
| Reinforcement | 17 (9) | 10 (=8) |
| Memory, attention and decision-making | 14 (10) | 10 (=8) |
| Optimism | 9 (11) | 3 (13) |
| Emotion | 8 (12) | 6 (12) |
| Beliefs about capabilities | 7 (13) | 8 (10) |
| Goals | 1 (14) | 1 (14) |
Domains presented in order of rank by pharmacist.
Rank was derived using weighted scores. Weighted scores were derived from the number of utterances divided by the number of participants, to ensure that findings across roles were comparable.
MCA, medicine counter assistant; N, Refers to the number of utterances coded to each domain.
bmjopen-2019-029937supp002.pdf (96.2KB, pdf)
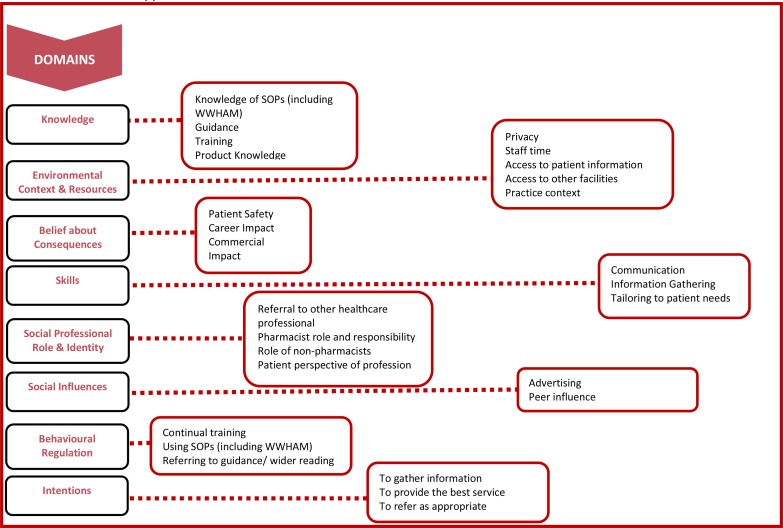
As part of the analysis process, a mapping diagram was developed (figure 1), to illustrate how the specific beliefs mapped to the salient domains. The Consolidated Criteria for Reporting Qualitative Research (COREQ) (online supplementary file 3) were employed to guide reporting of the data.32
Figure 1.
Mapping diagram illustrating salient domains and specific beliefs associated with the key determinants of quality in self‐care consultations in community pharmacies. Domains presented in order of rank by pharmacists, SOP: Standard Operating Procedure; WWHAM: Who, What, How long, Action to date, other existing Medication being taken.
bmjopen-2019-029937supp003.pdf (105.4KB, pdf)
Patient involvement
Patients were not involved in this study
Results
Sample characteristics
Forty-nine individuals indicated an interest in participation. Thirty interviews were completed (19 pharmacists; 11 MCAs), lasting between 15 and 60 min. Interviews were conducted between October 2014 and January 2015. Response rates of 70% (19/27) and 50% (11/22) were achieved for pharmacists and MCAs, respectively. The demographic characteristics of interviewees are presented in table 2.
Table 2.
Interviewee demographics (figures rounded to nearest whole number)
| Health board | Number of interviewees, % (n) | Pharmacist (MCA) | Total number of pharmacies in Scotland, % (n) |
| Ayrshire and Arran | 13 (4) | (2,2) | 8 (97) |
| Borders | 3 (1) | (1,0) | 2 (27) |
| Dumfries and Galloway | 10 (3) | (2,1) | 3 (35) |
| Fife | 0 (0) | – | 7 (85) |
| Forth Valley | 10 (3) | (2,1) | 6 (72) |
| Greater Glasgow and Clyde | 13 (4) | (2,2) | 25 (315) |
| Grampian | 27 (8) | (5,3) | 11 (131) |
| Highland | 7 (2) | (1,1) | 6 (78) |
| Lanarkshire | 10 (3) | (2,1) | 10 (121) |
| Lothian | 7 (2) | (2,0) | 15 (182) |
| Orkney | 0 (0)* | – | <1 (4) |
| Shetland | 0 (0)* | – | <1 (45) |
| Tayside | 0 (0) | – | 7 (92) |
| Western Isles | 0 (0)* | – | <1 (3) |
| SIMD† | |||
| SIMD 1 (most deprived) | 17 (5) | ||
| SIMD 2 | 37 (11) | ||
| SIMD 3 | 20 (6) | ||
| SIMD 4 | 13 (4) | ||
| SIMD 5 (least deprived) | 13 (4) | ||
| Pharmacy setting | |||
| Independent (single outlet) | 27 (8) | ||
| Small chain (2–5 outlets) | 17 (5) | ||
| Large chain define (6+ outlets) | 50 (15) | ||
| Supermarket | 7 (2) | ||
Pharmacist, n=19 (63%).
MCA, n=11 (37%).
*No R&D approval granted.
†SIMD is the Scottish Government's official tool for identifying places in Scotland suffering from deprivation, based on postcode. The information displayed here has been taken from the SIMD 2012 Scotland level population-weighted quintile.25
R&D, research and development; SIMD, Scottish Index of Multiple Deprivation.
Mapping to the TDF
All 14 domains were identified during analysis, some featuring more prominently than others. Specific beliefs and illustrative quotations are presented in table 3. Quotes are labelled using ‘PH’ to indicate a pharmacist and ‘MCA’, an MCA. Eight domains were identified as most salient to the target behaviour and are described below, followed by a comparison between pharmacist and MCA interviewees.
Table 3.
Theoretical beliefs, specific beliefs and illustrative quotes domains presented in order of dominance
| Theoretical domain | Specific belief | N | Illustrative quotations |
| Environmental context and resources | Privacy | 28 | 'Occasionally there’s a lot of other customers around the till and having to try and sort of discreetly move the customer to a quieter place if it’s something a bit more sensitive or you feel it’s inappropriate to be discussing something within earshot of other people.' PH004 |
| Staff time/resources | 13 | 'When it’s busy staff feel pressured and, you know, if they don’t feel they’ve got enough support, they let their standards slip, which is disappointing, but, if we’re all being completely honest, it happens when you’re under pressure.' PH009 | |
| Access to patient records/information | 12 | 'That’s how sometimes that you should always recommend customers to stick to the one pharmacy because if they’re changing medication all the time, we have obviously got it on computer, that we know every medication that they’re on' MCA011 | |
| Access to other support/ facilities | 9 | 'I have doctors, receptionists, nurses on tap. If I’m suspicious that there is something more serious, than the patient thinks, then I can go away and get some advice rather rapidly, which is a great help' PH007 | |
| Practice context | 6 | ‘It’s a small community pharmacy, so we tend to know most of the patients' PH006. ‘I think there’s got to be greater utilisation, of these private spaces, because I certainly wouldn’t want to openly discuss some, you know, medical issues, when I’ve got a queue of people waiting behind to me, and to my left and right-hand side.’ MCA001 | |
| Belief about consequences | Patient safety | 27 | 'If they’re taking something else that might not be necessary or something that’s not been reviewed for a while, or is potentially harmful, you know…You can sometimes gather bits of information that you can intervene for the patient’s best interest.' PH004 |
| Professional impact | 11 | ‘The worst scenario is that you get involved in legal situations or serious illness or death. It’s negligent that point of view. So, I think members of staff have to be aware that it’s an important role that they’re playing’. PH012 | |
| Commercial impact | 6 | 'if you do your consultations right, you make the right request, the customer leaves, they feel better, they’re going to come back so your business would grow…' PH009 | |
| Impact on ability to do job | 5 | ‘The more that we get out of them, then the more that we can offer them.’ MCA001 | |
| Skills | Communication skills | 26 | 'Try our best to use kind of open questions where possible. We find just having good communication skills are obviously pretty essential' PH002. 'Skills; good listening skills, good communication skills…underpinning knowledge.' PH006 |
| Tailoring | 16 | 'You’ve got to look at their body language, you’ve got to adapt your body language, to suit them. So, it’s not just standing there, smiling, and asking a few questions because that’s not going to work.' PH007 | |
| Information gathering | 7 | ‘I would say it’s more experience that I’d picked up, you know, from years of listening to what the pharmacist would say to them and, you know, it’s basically just trying to get the information, out of every patient that you need. And that gives you the best ground to, you know, help them…’ MCA003 | |
| Social influences | Patient knowledge & perspectives | 25 | 'Some people are quite, what’s the word? They’re not really very clued up, on what medicines either they’re already taking or what medicines they can get from the pharmacy' MCA003. I think it’s perhaps the perception of the patient or customer, about why we’re asking questions. I’ve always felt that the public aren’t given enough information, about what we actually do and why we’re asking questions. You know, we need to raise the profile of pharmacists' PH010 |
| Colleague/peer influence | 10 | 'if I’d picked up something new that, all three of us have been doing for many years and I thought actually this is maybe something that’s a wee bit better, let’s try this, I would pass that information onto the rest of the staff, including my colleagues.' PH017 | |
| Advertising | 8 | 'They’ve seen it on TV, or someone else has suggested it to them, so you do sometimes ask yourself the question of, “Why are they asking for this?” You know, they’re maybe self-diagnosing.' PH006 | |
| Knowledge | Knowledge of SOPs (inc. WWHAM) | 24 | 'WWHAM questions; the who, the what, the why, the how.' MCA002 |
| Knowledge of training courses | 14 | ‘Once you complete your training, especially from a healthcare assistant point of view, I don’t think… Once you finish that structured kind of training, there’s not a lot that you’re proactively pushed to do. It’s really off your own back, to maintain your own knowledge… there’s a lot of information out there, but it’s knowing where to go looking for it or actually having the inclination, to go and do it' MCA001 | |
| Patient knowledge | 12 | 'A lot of patients don’t understand that difference between the medicines…so you obviously have to just take the time to make sure that they’re aware of what they’re actually buying.' PH001 | |
| Knowledge of guidance | 11 | 'There are the guidelines from the Royal Pharmaceutical… If we have any problems, we can get in touch with one of the support people, like the National Pharmaceutical Association or a company called Numark…’ PH007 | |
| Product knowledge | 7 | 'It’s just having a better knowledge of the product that people are asking for; make sure that you are 100% familiar with all the content indications and the licence for the products.’ PH004 | |
| Social professional role and identity | Role of MCAs | 16 | 'If the public were more aware that the staff working within the pharmacy, not just the pharmacist, are trained in their jobs rather than they’ve just come off the street and they put price tickets on things' MCA005 ' |
| Professional role | 9 | 'The way a patient might approach an assistant compared with how they might consult with a pharmacist might be different. Possibly.' PH004. 'Some people don’t want to speak to a counter assistant; they want to speak to a pharmacist.' MCA006 | |
| Job satisfaction | 7 | 'Sometimes you feel like you’re doing your job and you’ve helped someone, that’s really nice' PH018 | |
| Responsibility | 7 | ‘The pharmacist should be aware of every P medicine that’s sold in the pharmacy, so they should really be listening out for things going out' PH017 | |
| Referring to other healthcare professionals | 3 | ‘If it’s a recurring problem then the pharmacist might refer them to the doctor’s and say, “You’ve been given this several times. I can only give you certain things over the counter and obviously there is a lot that a qualified doctor can prescribe”.’ MCA010 | |
| Behavioural regulation | Continual training | 16 | ‘I think there’s always scope for making sure that people’s training is up to date and, you know, making sure that any new staff that come are fully trained and review what you have and then how you sell it and that sort of thing.’ PH001 |
| SOPs (inc. WWHAM) | 11 | ‘Well, we also have our standard operating procedures, which are called SOPs, and they give the general guidelines on what you should do.’ PH007 | |
| Referring to guidance/wider reading | 8 | ‘We’re, obviously, using journals and things like that, to keep abreast of updates that we share with the staff.’ PH015 | |
| Intentions | To gather information | 15 | 'You need to start at the beginning and work your way through the process, regardless what the request is' PH001 'You’ve always got to seek information. You can’t just assume. When somebody comes in and asks for co-codamol, we don’t just sell them it. That is not what we do. It’s again back to the WWHAM questions. Always the WWHAM questions; that’s where you start from and always continue' MCA009 |
| To provide best practice | 12 | 'My intention is always to get the message across so, as long as I feel that they’ve understood me, then I’m happy. You know, we’re all humans, so maybe if someone is being slightly awkward or a wee bit rude, then you are maybe not as nice to that person or maybe not spend as much time with them. As long as you get your base message across, then I feel I’ve done my job.' PH0018 | |
| To refer to other healthcare professionals | 3 | if you couldn’t sell the medicine, then you would just say, you would just refer them to go to their own doctor' MCA004 | |
| To refer to a pharmacist | 2 | ‘If you want to hold on a wee minute, I’ll get T my pharmacist, to come out and have a wee word with you.” And sometimes that does help because, he’s a pharmacist so he knows more, you know, than what the front counter staff do. You don’t want anybody going away without helping them' MCA004 | |
| Memory, attention and decision-making processes | Administrative prompts & processes | 13 | ‘I’ve basically stuck my WWHAM questions at the side of the tills because, if you do forget, the little prompt is there.' PH009. 'I’ve got it up on a board on the wall, the four questions to ask' MCA004 |
| Patient prompts | 9 | 'Any of the vulnerable patient groups, so children, people over 60, 65, anyone with any long term chronic illness, so any of the kind of red flag indicators that, all of a sudden, you maybe delve into another set of questions' MCA001. 'If it’s for a child, or if someone was on any other medication, it would be referred to the pharmacist' PH008 | |
| Automatic processes | 2 | 'You know, we’re all so aware that it’s almost second nature' PH018 | |
| Reinforcement | Job satisfaction | 10 | ‘The incentive we have is to help the person who’s standing in front of me. I’m quite happy to do that, it being part of my job anyway. But yes, I do like to feel that I helped that person in some way.’ MCA005 |
| Impact on sales | 9 | ‘If you give them advice on how to handle something, it does work and it makes them feel better, then the chances are they’re going to come back to us.’ MCA008 | |
| Patient safety | 4 | ‘The incentive is to keep the patient safe.’ PH006 | |
| Feedback | 4 | ‘Just simple phrasing I’ve learnt previously that that kind of thing sticks with people, rather than always maybe giving financial rewards or physical rewards. A simple, “Well done,” sometimes works better.’ MCA002 | |
| Belief about capabilities | Confidence due to knowledge and experience | 8 | ‘I’m very confident that I’ve got the knowledge and the appropriate skills to make sure that things are being recommended or provided safely and appropriately.’ PH004 |
| Confidence due to ability to refer | 4 | I would say I’m fairly confident, but then if I feel I’ve not asked the right questions, I would obviously refer to my pharmacist, just to make sure I wasn’t giving them something that wouldn’t be right for them.’ MCA004 | |
| Patient impact on confidence | 3 | ‘If you do get some of these customers that come in, particular for new staff, it can be a real blow to their confidence and then the worry is that they’re not going to ask the questions to another customer and they might actually miss something that is really important.’ PH012 | |
| Optimism | Pessimism | 7 | ‘There are some patients that you just can’t win with in a way.’ PH012 |
| Positivity | 5 | ‘I’m providing the best possible care; that’s what I’d want or hope that all my staff felt as well.’ PH009 | |
| Emotion | Frustration | 4 | ‘Sometimes it’s frustrating, because you know they’re not listening or they don’t believe your advice, and go anyway, and so that’s quite frustrating.’ PH018 |
| Worry | 4 | ‘Can be slightly worried for the likes of a customer if they’re continuously buying something, like, I don’t know, if we’re talking say co-codamol.’ MCA009 | |
| Uncomfortable/Nervous | 4 | ‘You see the same people buying the same things day in day out, and it can be quite hard when you want to refuse a request. It can be very difficult; it makes a lot of staff, particularly the younger staff, feel quite uncomfortable.’ PH009 | |
| Empathy | 1 | ‘You certainly kind of empathise with their feelings.’ MCA003 | |
| Under pressure | 1 | ‘People come in, and they’ve made their made up that they want codeine linctus, for a cough, we know that therapeutically it might not be the best thing for them… feel stuck a bit between a rock and a hard place, but you make the supply, and the patient takes that medication and feels they’ve got the benefit, from it.’ MCA001 | |
| Goals | Decision to cut out questions/shorten the process | 2 | ‘I always cover the areas that are vital but sometimes if it’s busy and things like that, it can take up a good part of your time having to deal with it when there’s an easier and proper way to go about it.’ MCA008 |
MCA, medicine counter assistant; N, number of interviewees who referred to each specific belief; PH, pharmacist; SOP, standard operating procedure; WWHAM, Who, What, How long, Action to date, other existing Medication being taken.
Knowledge
(Knowledge of what information to gather)
The use of standard operating procedures (SOPs) was identified as a facilitator to information gathering. This included knowledge of the WWHAM mnemonic to determine the Who, What, How long, Action to date and any other existing Medication being taken. Most interviewees referred to this method of questioning and spoke positively about having a standardised procedure to follow. Lack of patient knowledge of their own medical history and current medication was deemed problematic.
We also have our standard operating procedures, there are the two WWHAM questions, which is an acronym, where they have to go through a set of five questions; basically, to find out what the patient needs. PH007
You have to probe patients…I think sometimes patients don’t realise that because they take medicines from the doctor, that if you take a set of medicines over the counter there can be interactions PH002
Environmental context and resources
(Factors relating to the pharmacy setting or environment that influence the gathering of information)
Lack of privacy was considered a barrier to gathering information. Having access to a private area (eg, consultation room) was perceived to facilitate information gathering, creating a greater sense of a healthcare environment rather than commercial premises. However, interviewees reported that some pharmacy users are reluctant to use them as it could be perceived (by other pharmacy users) that they have something to hide, and perhaps make them feel uncomfortable or embarrassed. Staff resources may also act as a barrier to using this confidential space, if team members leave the counter to speak privately to patients.
I think there’s got to be greater utilisation of these private spaces because I certainly wouldn’t want to openly discuss some, you know, medical issues, when I’ve got a queue of people waiting behind to me…The problem then is you have to be able to free your pharmacist, free up your counter staff, to be able to use these spaces, to get the best out of every consultation that they give. MCA001
Some people don’t want to go into the consultation room…I mean a lot of people at our pharmacy use the consultation room for the consumption of methadone and it’s just associated with that. So, there’s a lot of preconceptions involved as well PH019
Beliefs about consequences
(Perceptions about the advantages/disadvantages of gathering information)
Patient safety resonated strongly, with interviewees indicating that the health and well-being of patients was their primary concern. The consequences of adverse effects motivated interviewees to elicit information. Patient safety was also highlighted in relation to identifying substance abusers.
We need to do it (gather information) to ensure the safety of the patient; we’re not there just as a salesman, we’re there to help people get better, offer them advice and make sure that anything that we sell is going to make them better; not making them worse or interact with anything. PH0015
Skills
(The skills required to gather information)
Effective communication skills were also deemed salient to gathering information and it was highlighted that these are required to be tailored to each patient.
You need to be able to ask the right questions and tailor them to the person that you’re asking, to be able to listen to what you’re told. And you need to be able to process the information fairly quickly so that you can make the right decision. PH001
Social professional role and identify
(Perception of own role/responsibilities in relation to gathering information and comparison with other roles)
Pharmacists discussed their role and responsibility within the pharmacy team and described monitoring information gathering by MCAs and intervening when necessary. Pharmacists providing reassurance and taking overall responsibility, appeared to facilitate information gathering by MCAs.
The role of MCAs, how they perceive themselves and how patients view them was also identified from the data. MCAs suggested that in some cases patients prefer to speak to a pharmacist and this was a theme also highlighted in the pharmacist interviews.
Some people don’t want to speak to a counter assistant; they want to speak to a pharmacist. MCA006
…I don’t mean they don’t believe it, but they ask to speak to the pharmacist. The pharmacist goes out and gives them exactly the same information. And they go, oh yeah, that’s fine then…there’s more of a trust with the pharmacist… PH005
Social influences
(How interviewees perceive others see their role and how this impacts upon the ability to gather information)
A perceived lack of awareness from patients about what services a pharmacy team can offer and the training and expertise they hold, as well as their understanding of the rationale for the pharmacy team gathering this information, was identified as a barrier. This was considered to stem from the information or lack of it, that patients are provided with regarding the function/role of pharmacies.
I think they look on us as more of like shop keepers and they want to know why we want to know, they don’t realise that we really need to know the information. MCA005
I think it’s perhaps the perception of the patient or customer, about why we’re asking questions. I’ve always felt that the public aren’t given enough information, about what we actually do and why we’re asking questions. You know, I’ve always sort of suggested that we need to raise the profile of pharmacists. PH010
Behavioural regulation
(Procedures/methods of gathering information)
Having SOPs in place gave the pharmacy team the reassurance of having a clear protocol to follow. Interviewees suggested that having access to ongoing and hands on training could further facilitate information gathering during consultations.
‘Well, we also have our standard operating procedures, which are called SOPs, and they give the general guidelines on what you should do.’ PH007
Intentions
(A conscious decision to gather information)
An intention to elicit information and to provide the best service possible was evident from interviewees, who suggested that their means of providing best practice and the best possible service for patients was by gathering information. This intention to gather information and belief that by doing so they were benefiting the patient was recognised as facilitating the information gathering process during these consultations.
You’ve always got to seek information…You can’t just assume. MCA009
I would definitely still, you know, dig for that information, to make sure what they’re getting from us was what they needed, and was safe and suitable. MCA003
Pharmacists versus MCAs
Table 1 illustrates mapping to the TDF by professional role. The results demonstrate clear similarities in beliefs by role as well as distinct differences.
‘Beliefs about Consequences’ was a dominant theme across both groups as was ‘Knowledge’, ‘Environmental context and resources’ and ‘Skills’. Both groups also agreed that the impact of patient education and patients’ perspectives of the pharmacy profession (‘Social influences’) affected how they manage these consultations. When mapped to the TDF, although similar domains appeared to influence both professional roles, the specific beliefs relating to these domains tended to differ. These differences were identified most prominently within the domains, ‘Environmental context and resources’, ‘Beliefs about consequences’ and ‘Memory, attention and decision-making’ as detailed below.
Environmental context and resources
Both pharmacists and MCAs highlighted privacy as a barrier to eliciting information and they also both reported the benefits of being able to access patient records or information regarding current medication and the challenges they face when this is unavailable. Access to patients’ medical history however, appeared to be more of a concern to MCAs.
Without access to a full patient record, we can’t double check. MCA001
Pharmacists highlighted the benefits of having access to other forms of support such as other pharmacist colleagues or other healthcare professionals and also highlighted staff time as a barrier to eliciting information, reinforcing their sense of responsibility over the team and how consultations are managed. These beliefs did not feature strongly in the MCA interviews.
I have doctors, receptionists, nurses on tap. And if I’m suspicious that there is something more serious, than the patient thinks there is, then I can go away and get some advice rather rapidly. PH007
When its busy, staff feel pressured and, if they don’t feel they’ve got enough support, they let their standards slip. PH009
Beliefs about consequences
Pharmacists were more concerned than MCAs about the impact that eliciting information could have on commercial aspects of the business. They suggested that gathering information effectively may result in patients experiencing a better service and promote greater loyalty/future use of the pharmacy. Pharmacists also highlighted a concern of litigation and the potential impact this may have on their careers.
The worst scenario is that you get involved in legal situations or serious illness or death. It’s negligent… I think members of staff have to be aware that it’s an important role that they’re playing. PH012
I just want to do the best for the patient, so I want to do the best job that I can. PH011
For MCAs, the consequences of not gathering information focused on patient safety primarily and avoidance of harm.
If you give somebody the wrong medication, it can have various side effects MCA002
Memory, attention and decision-making
Although this was not one of the most salient domains overall, in relation to the prompts that facilitate gathering information from specific groups of patients, pharmacists and MCAs highlighted different factors that aided this process. Pharmacists discussed the benefits of administrative prompts such as laminated cards illustrating the WWHAM questions and other administrative procedures. MCAs suggested that patient prompts were a facilitator for them, suggesting that if the patient was a minor, pregnant or very elderly this would trigger them to ask specific questions.
We keep a print out at the till of the general questions that they should be asking. PH011
Any of the vulnerable patient groups, so children, people over, you know, over sort of 60, 65, anyone with any long- term chronic illness, so any of the kind of red flag indicators that, all of a sudden, you maybe delve into another set of questions. MCA001
A mapping diagram was developed (figure 1), to illustrate the eight most salient domains and the salient beliefs associated with these. Four overarching themes were identified to encapsulate these beliefs: best practice; health literacy; decision-making; and, professionalism.
Best practice
When considering the management of consultations, pharmacy team members reported wanting to offer best practice, to do what was best for the patient and highlighted the potential consequences if they did not achieve these goals. The consequences to the patient, in terms of safety, to the pharmacy as a business, to their own careers as well as to their own emotional well-being, were concerns of the whole pharmacy team. While the consequences of not providing best practice in some cases differed by professional role the overarching theme to provide the best possible care was evident across roles.
I’m providing the best possible care; that’s what I’d want or hope that all my staff felt as well PH009
It does make you feel good as well, though, knowing that you’ve given somebody the solid information and you’ve helped them MCA008
Health literacy
Patients appear to have a major influence on consultation management. Knowledge and understanding of their health and medication, their receptivity to providing information, as well as their understanding of services offered by pharmacy personnel, were perceived to act as barriers or facilitators to the information gathering process and consultation management. This was highlighted by both pharmacists and MCAs.
People have to take responsibility for their own health and their own medicine PH005
Decision-making
Decision-making appeared to be a substantial component of pharmacy personnel’s daily roles. This included whether to gather any information, the process used to gather information and whether to tailor their behaviour to each patient’s circumstances and behaviour. Decision-making also included whether to refer to the pharmacist (referral by MCA staff) or to another healthcare professional (referral by pharmacists). Considerable reference was made to criteria used when making these decisions, however it was apparent that this was not a standardised process, with differences between pharmacists and MCAs, as well as within and between pharmacies.
Sometimes you catch someone off guard when you start asking them questions and you might actually be dealing with them for quite a long time, longer than you would actually need to be with them … So that’s why sometimes I will admit that I do cut down the questions. MCA008
Professionalism
The concept of professionalism was particularly evident and differed between roles. MCAs perceived that they lacked credibility with patients as healthcare advisors and that patients preferred to consult a pharmacist. This was reinforced by the participant comment used earlier in this paper: ‘…there’s more of a trust with the pharmacist’. A greater sense of responsibility emerged from the pharmacists in relation to their role within the team and in respect to overseeing the management of consultations.
I think people are, on the whole, sometimes more confident to discuss with the pharmacist PH001
Discussion
This study represents the second stage of the TRiaDS-P programme, a theoretically underpinned exploration of the beliefs and key determinants of information gathering during OTC consultations in community pharmacies. Eight salient domains were identified: knowledge (awareness and use of standard operating procedures), environmental context and resources (privacy), beliefs about consequences (patient safety), skills (communication and decision-making), social professional role and identity (perception of own role), social influences (patient awareness of pharmacist role), behavioural regulation (training) and intention (to gather information). Similar domains were salient for pharmacists and MCAs; however, the specific beliefs within these domains differed by professional role. Four overarching themes were identified as part of this process: best practice, health literacy, decision-making and professionalism.
These findings suggest that in practice, pharmacy team members already know the information to be gathered during OTC consultations. However, the information that patients or consumers are willing to, or can share, is possibly a greater challenge. While lack of privacy is commonly cited as a problem in community pharmacies, having effective communication skills is also important and is likely to impact on information gathering during OTC consultations. In addition, raising public awareness of the role and function of different pharmacy team members, particularly MCAs, might also encourage more proactive information provision during these consultations.
To our knowledge this is the first application of the TDF to explore information gathering within the community pharmacy team, which included interviews with both pharmacists and MCAs, identifying convergent and divergent beliefs. We achieved representation from most Scottish Health Boards. In some of the more remote areas (eg, the islands of Orkney and Shetland), participants’ views may have differed due to the very different contexts within which they are working, particularly in terms of travel to access services, training, peer support and advice. Our sample was broadly representative of the population except for NHS Greater Glasgow and Clyde which was under-represented and NHS Grampian which was over-represented. This may have been due to the lead university being based in the latter and the strong links developed with the profession through previous studies. Our original aim was to conduct interviews with 20 pharmacists and 20 MCAs. Although fewer MCAs participated, categorical and theoretical saturation was achieved (ie, no new information or insights were gained). This study was conducted across Scotland only, therefore the results may not be generalisable to the wider population. However, as is the nature of qualitative research, these findings are not intended to be generalisable, but to provide an insight into the behaviour of interest to inform future research, practice and policy. Telephone interviews, like face-to-face interviews, allow a two-way interaction between the researcher and the participant, with the added advantage of being more cost effective and easier to schedule. It could be argued that cues picked up through body language may be missed over the telephone, however given the topic being discussed we would argue this did not have a detrimental impact on data collection.
We know from existing literature that effective consultations between pharmacy personnel and patients is fundamental to ensuring appropriate recommendations and desired patient and practitioner outcomes.12–15 33 34 Our approach is supported by the findings of Jones and colleagues’ recent study which identified time, space and a lack of qualified staff as barriers to promoting antimicrobial stewardship.35 They recommended that resources be developed to facilitate pharmacy teams providing effective self-care and compliance advice and that future research uses behavioural theory in the development of interventions.
This current study identified perceived barriers at the patient, professional and organisational level which influence effective information gathering. At the patient level, patients’ own knowledge of their medical history was cited, and it is also believed that patients are unaware of the healthcare advice and support that pharmacies can offer. The Scottish Government’s most recent strategy6 continues to focus on the need for patients to use pharmacies, including services such as Minor Ailments Service as a ‘first port of call’ for these conditions, perhaps indicating a need for greater awareness at a public health level. Previous work in this area has identified incentives which could be utilised to encourage this, such as avoiding long waiting times for GP appointments and long waits while in the surgery, however lay beliefs around the perceived inadequacy of self-medication products and perceptions about the legitimacy of pharmacists’ role as advice givers, may counteract this initiative.36 It is likely that patient’s decision-making around whether to use a pharmacy as a first port of call may be influenced on their own previous experience or their ability to afford the cost of OTC medicines.37
Linked to this, at the professional level, MCAs perceived that patients do not value their input as healthcare advisors and may prefer speaking to a pharmacist. As well as raising public awareness about the skills and expertise available within community pharmacy teams, potential interventions to address this may also target MCA perceptions about their own professional role. Currently, there is no requirement for MCA postqualification training. Specific MCA-targeted interventions might also be needed.38 Linked to this is the challenge of the least trained member of staff dealing with the majority of patients (although under the supervision of the pharmacist). This again points towards the need for additional and ongoing continual education for MCAs to support them in their role. Since this study was undertaken, the Chief Pharmaceutical Officer for Scotland funded a series of educational resources and events for MCAs, informed by these results.39 Finally, at an organisational level, access to patient records was identified as a barrier for MCAs and staff time and privacy were identified by pharmacists as being key determinants in effective information gathering during OTC consultations. The different organisational aspects identified by the different professional roles within the team highlights the importance of tailoring any interventions to meet the needs of the different roles, function and responsibilities that exists within community pharmacy.
These results illustrate the multiple influences, complexities and challenges affecting the effective management of OTC consultations and supports the need for further tailored interventions. The third stage of the TRiaDS-P programme will use these findings to inform the development of additional interventions for both pharmacists and MCAs, to optimise this behaviour and will use a systematic, theory-based approach which engages both stakeholders and health professionals.
Supplementary Material
Footnotes
Contributors: HC: manuscript production and revisions, contributed to the scientific development, conduct, data collection, analysis and interpretation of the study. EG: contributed towards scientific development, data collection, data coding, analysis and interpretation. AP: contributed to the scientific development, conduct and interpretation of the study. LY: contributed to the scientific development, conduct and interpretation of the study. ED: contributed towards data analysis and interpretation. RN: contributed towards data coding, analysis and interpretation. MW: led the scientific development, conduct and interpretation of the study.
Funding: This study was conducted as part of the TRiaDS programme of research (www.triads.org.uk) and was funded by NHS Education for Scotland. MC Watson was funded by a Health Foundation Improvement Science Fellowship. We thank the TRiaDS Research Methodology Group and all participating pharmacists and MCAs as well as the TRiaDS administrative team in particular, Trish Graham, who scheduled and co-ordinated the interviews.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Ethical approval was received from the College of Life Sciences and Medicine Ethics Review Board, University of Aberdeen (CERB/2014/4/1050). Research and Development management approval was conducted through the NHS Research Scotland Permission Co-ordinating Centre. Approval was granted by 11 of the 14 territorial Health Boards within the timeframe of the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. Fielding S, Porteous T, Ferguson J, et al. Estimating the burden of minor ailment consultations in general practices and emergency departments through retrospective review of routine data in North East Scotland. Fam Pract 2015;32:165–72. 10.1093/fampra/cmv003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Watson MC, Ferguson J, Barton GR, et al. A cohort study of influences, health outcomes and costs of patients' health-seeking behaviour for minor ailments from primary and emergency care settings. BMJ Open 2015;5:e006261 10.1136/bmjopen-2014-006261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Transforming urgent and emergency care services in England Urgent and emergency care review end of phase 1 report. appendix 1—Revised evidence base from the urgent and emergency care review. NHS England: Leeds, 2013. [Google Scholar]
- 4. Public Health England Building Capacity: realising the potential of community pharmacy assets for improving the public’s health, 2016. [Google Scholar]
- 5. Prescription for Excellence A vision and action plan for the right pharmaceutical care through integrated partnerships and innovation. Edinburgh, Scotland: The Scottish Government, 2013. [Google Scholar]
- 6. Achieving Excellence in Pharmaceutical Care A strategy for Scotland. Edinburgh, Scotland: The Scottish Government, 2017. [Google Scholar]
- 7. Bond CM. The over-the-counter pharmaceutical market – policy and practice : Health policy developments. Eurohealth. 14 3 France: Health promotionfor migrants, 2007. [Google Scholar]
- 8. Watson MC, Hart J, Johnston M, et al. Exploring the supply of non-prescription medicines from community pharmacies in Scotland. Pharm World Sci 2008;30:526–35. 10.1007/s11096-008-9202-y [DOI] [PubMed] [Google Scholar]
- 9. Flint J. Training requirements for medicines counter assistants. Pharm J 1996;256:858–9. [Google Scholar]
- 10. General Pharmaceutical Council Medicines counter assistant training. Available: https://www.pharmacyregulation.org/education/support-staff/medicines-counter-assistant [Accessed 30 Apr 2019].
- 11. Watson MC, Bond CM. The evidence-based supply of non-prescription medicines: barriers and beliefs. Int J Pharm Pract 2004;12:65–72. 10.1211/0022357023475 [DOI] [PubMed] [Google Scholar]
- 12. Studman A. Three in 10 pharmacies not following safety guidelines, finds which? investigation. which? 2018. [Google Scholar]
- 13. Sinclair HK, Bond CM, Hannaford PC. Over-The-Counter ibuprofen: how and why is it used? Int J Pharm Pract 2000;8:121–7. 10.1111/j.2042-7174.2000.tb00996.x [DOI] [Google Scholar]
- 14. Ferris D, Nyirjesy P, Sobel J, et al. Over-The-Counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynaecol 2002;99:419–24. [DOI] [PubMed] [Google Scholar]
- 15. Shi C-W, Gralnek IM, Dulai GS, et al. Consumer usage patterns of nonprescription histamine2-receptor antagonists. Am J Gastroenterol 2004;99:606–10. 10.1111/j.1572-0241.2004.04130.x [DOI] [PubMed] [Google Scholar]
- 16. Watson MC, Bond CM, Grimshaw J, et al. Factors predicting the Guideline compliant supply (or non-supply) of non-prescription medicines in the community pharmacy setting. Qual Saf Health Care 2006;15:53–7. 10.1136/qshc.2005.014720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Watson MC, Feilding S, Johnston M, et al. Consumer communication during consultations for nonprescription medicines: a theoretical exploration of beliefs, behaviours and attitudes. Int J Pharm Pract 2014. [Google Scholar]
- 18. Garner M, Watson MC. Using linguistic analysis to explore medicine counter assistants' communication during consultations for nonprescription medicines. Patient Educ Couns 2007;65:51–7. 10.1016/j.pec.2006.05.004 [DOI] [PubMed] [Google Scholar]
- 19. Blenkinsopp A, Paxton R, Blenkinsopp J. Symptoms in the pharmacy: a guide to the management of common illnesses. London: Wiley-Blackwell, 2014. [Google Scholar]
- 20. van Eikenhorst L, Salema N-E, Anderson C. A systematic review in select countries of the role of the pharmacist in consultations and sales of non-prescription medicines in community pharmacy. Res Social Adm Pharm 2017;13:17–38. 10.1016/j.sapharm.2016.02.010 [DOI] [PubMed] [Google Scholar]
- 21. Watson MC, Cleland J, Inch J, et al. Theory-based communication skills training for medicine counter assistants to improve consultations for non-prescription medicines. Med Educ 2007;41:450–9. 10.1111/j.1365-2929.2007.02723.x [DOI] [PubMed] [Google Scholar]
- 22. Clarkson JE, Ramsay CR, Eccles MP, et al. The translation research in a dental setting (triads) programme protocol. Implement Sci 2010;5 10.1186/1748-5908-5-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Newlands RS, Power A, Young L, et al. Quality improvement of community pharmacy services: a prioritisation exercise. Int J Pharm Pract 2018;26:39–48. 10.1111/ijpp.12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. 10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7 10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Francis JJ, O'Connor D, Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci 2012;7 10.1186/1748-5908-7-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Atkins L, Francis J, Islam R, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017;12 10.1186/s13012-017-0605-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dyson J, Lawton R, Jackson C, et al. Does the use of a theoretical approach tell us more about hand hygiene behaviour? the barriers and levers to hand hygiene. J Infect Prev 2011;12:17–24. 10.1177/1757177410384300 [DOI] [Google Scholar]
- 29. Seawright J, Gerring J. Case Selection Techniques in Case Study Research:A Menu of Qualitative and Quantitative Options. Political Res Q 2008;61:294–308. [Google Scholar]
- 30. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 31. Francis JJ, Stockton C, Eccles MP, et al. Evidence-Based selection of theories for designing behaviour change interventions: using methods based on theoretical construct domains to understand clinicians' blood transfusion behaviour. Br J Health Psychol 2009;14:625–46. 10.1348/135910708X397025 [DOI] [PubMed] [Google Scholar]
- 32. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 33. Olsson E, Ingman P, Ahmed B, et al. Pharmacist-patient communication in Swedish community pharmacies. Res Social Adm Pharm 2014;10:149–55. 10.1016/j.sapharm.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 34. Tully MP, Beckman-Gyllenstrand A, Bernsten CB. Factors predicting poor counselling about prescription medicines in Swedish community pharmacies. Patient Educ Couns 2011;83:3–6. 10.1016/j.pec.2010.04.029 [DOI] [PubMed] [Google Scholar]
- 35. Jones LF, Owens R, Sallis A, et al. Qualitative study using interviews and focus groups to explore the current and potential for antimicrobial stewardship in community pharmacy informed by the theoretical domains framework. BMJ Open 2018;8:e025101 10.1136/bmjopen-2018-025101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hassell K, Noyce PR, Rogers A. A review of factors that influence the use of community pharmacies as a primary health care resource. Int J Pharm Pract 1999;7:51–9. 10.1111/j.2042-7174.1999.tb00948.x [DOI] [Google Scholar]
- 37. Hassell K, Noyce PR, Rogers A, Harris J, Wilkinson J, et al. A pathway to the GP: the pharmaceutical 'consultation' as a first port of call in primary health care. Fam Pract 1997;14:498–502. 10.1093/fampra/14.6.498 [DOI] [PubMed] [Google Scholar]
- 38. Smith SM, Watson MC. The training needs, attitudes and experience of pharmacy support staff in northern Scotland. Int J Pharm Pract 2004;12:191–7. 10.1211/0022357044571 [DOI] [Google Scholar]
- 39. NHS Education for Scotland New resource: improving the quality of over-the-counter (OTC) consultations for simple analgesics: phase III. Pharmacy 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-029937supp001.pdf (89.1KB, pdf)
bmjopen-2019-029937supp002.pdf (96.2KB, pdf)
bmjopen-2019-029937supp003.pdf (105.4KB, pdf)