Abstract
Objective
To study trends of infant mortality rate (IMR) and neonatal mortality rate in Greece during the period 2004–2016 and explore the role of sociodemographic factors in the years of crisis.
Design
Nationwide individual data for live births and infant (0–11 months) deaths provided by the Hellenic Statistical Authority were examined using Poisson, joinpoint regression and interrupted time series (ITS) analyses.
Setting
Greece.
Participants
All infant deaths (n=4862) over the 13-year period, of which 87.2% were born to Greek mothers, and respective live births.
Main outcome measures
Evolution of IMR (0–364 days), early (<7 days) neonatal mortality rate (ENMR), late (7–27 days) neonatal mortality rate (LNMR) and post neonatal (28–364 days) mortality rate (PNMR) trends, by maternal nationality, place of residence and Human Development Index (HDI).
Results
By Poisson regression, overall, during the study period, among infants of Greek mothers, IMR and PNMR declined significantly (−0.9%; 95% CI −1.7% to −0.1% and −1.6%; −3.0% to −0.2% annually, respectively), although differentially by place of residence (IMRurban: −2.1%; −2.9% to −1.3%, IMRrural: +10.6%; 7.6% to 13.6%). By contrast, among infants of non-Greek mothers, the low starting IMR/ENMR/LNMR/PNMR increased significantly (max ENMR:+12.5%; 8.6% to 16.5%) leading to a non-significant time–trend pattern overall in Greece. The inverse associations of HDI with IMR, ENMR and PNMR were restricted to Greek mothers’ infants. Joinpoint regression analyses among Greek mothers’ infants indicated non-significant increasing trends of IMR and ENMR following the crisis (+9.3%, 2012–2016, p=0.07 and +10.2%, 2011–2016, p=0.06, respectively). By contrast, the high (+17.1%; 8.1% to 26.9%, p=0.002) IMR increases among non-Greek infants were restricted to 2004–2011 and equalised to those of Greek mothers’ infants thereafter. ITS analyses in preset years (2008, 2010, 2012) identified significantly increasing trends in IMR, LNMR and PNMR after 2012, and in ENMR after 2010, among Greek mothers’ infants.
Conclusions
HDI and rural residence were significantly associated with IMR. The strongly decreasing IMR trends among Greek-mothers’ infants were stagnated after a lag time of ~4 years of crisis approximating the previously sharply increasing trends among non-Greeks.
Keywords: neonates, mortality rates, infant deaths, perinatal care, financial crisis
Strengths and limitations of this study.
Longest follow-up period of national data, as contrasted to previously Greek-based studies.
Maternal ethnicity is for the first time considered in the analyses explaining part, if not most, of the heterogeneity of trends through the study period.
Three complimentary statistical methodologies were used to describe the overall evolution of infant mortality and its components.
Absence of a linkage system between birth and death data.
Data on the role of biological factors or specific causes of infant death are missing.
Introduction
Socioeconomic factors have repeatedly been recognised as strong determinants of the health status of the population, including infants.1–3 Economic indicators, such as the per capita gross national product, were suggested to be at least as important contributors of infant mortality (IM) as narrowly defined factors relating to provision of medical care, for example, the relative number of doctors or hospital beds in a community.1 Not surprisingly, the recent economic crisis of ~2008, has been linked with declines in population and child health reflected also by increased IM rates (IMR).4 5 It is worth noting that in European Union countries, even a minor 1% cut in government healthcare spending was associated with significant increases in all mortality metrics, including neonatal and post neonatal IM.6
On the contrary, associations between the crisis and increased mortality have been questioned in other studies showing that most indicators of population health, apart from those relevant to suicides and mental health, continued improving after crisis initiation.7–10 Moreover, the economic crisis has been associated with some beneficial effects, that is, decline in rates of road traffic accidents, and smoking cessation.4 9 Reasonably, the impact of the crisis on health depends on several factors including the duration and intensity of the recession, the level of healthcare achieved prior to the recession and the type of austerity measures applied, but also on the type of the population studied with the most vulnerable groups being disproportionally affected.4 11 12 Due to the latter, it was proposed that studies should focus on analysing separately the subgroups most influenced by the crisis instead of presenting results as averages in a population.4
Greece has been markedly affected and still suffering the recent economic crisis. Between 2008 and 2016, the country’s gross domestic product (GDP) per capita dropped by 26%, unemployment rate increased by more than 200% (from 7.6% to 23.3%) and the median disposable income decreased by 35%.13 14 The Gini index, which measures income inequality, increased by 22% and the proportion of individuals at risk of poverty or social exclusion climbed to almost 36% in 2016. Total health expenditures and government expenditure on healthcare were both decreased by 34% per capita over the period 2008–2016,13 14 whereas unmet healthcare needs increased.15 Besides, during the last years, Greece experienced large refugee flows16 17 with an anticipated negative impact on the country’s economy and population health indicators. Adverse effects of financial crisis on perinatal factors, such as low birth weight, preterm birth and stillbirth rates, have been also observed18 19; however, sparse data exist regarding the potential association of the crisis with IMR. It has been initially reported that during the period 2003–2012, IMR in Greece did not differ between the precrisis and crisis period whereas a later study showed that IMR increased between 2010 and 2015 as contrasted to the steady decrease observed during the preceding decade.20 21 Ecological correlations may be prone, however, to fallacies, whereas the different parts shaping the two main components of IM, namely neonatal (NM) and post neonatal mortality (PNM), should have been distinctly examined along with other factors possibly influencing the infants’ health, especially socioeconomic status and access to healthcare delivery.
The aims of the current study were to explore time trends in early (<7 days of life) and late (7–27 days) NM, PNM (28–364 days) and total IM (0–364 days) in Greece during the period 2004–2016 after taking into account nationality and place of residence, as well as changes in the Human Development Index (HDI) during the study period as a proxy of individual and collective measures of socioeconomic impact and healthcare access.
Materials and methods
Following personal contact and a signed agreement, individual data for all live births and infant (0–11 months) deaths were provided by the Hellenic Statistical Authority (ELSTAT) for a 13-year period (2004–2016) in two separate files: one including live births, and a second one, infant deaths; linkage of the two files was not possible as the personal identification number was not available in ELSTAT. Information on maternal demographic characteristics, such as nationality and place of residence, as well as on the infants’ age at death, was also provided.
Mortality rates were calculated for infant (ΙΜ), early neonatal (0–6 days) (ENM), late neonatal (7–27 days) (LNM) and post neonatal (28–364 days) period (PNM) using respective numbers of deaths over the number of live births per year. Annual percent of change (APC) during the study period was initially estimated through univariate Poisson regression analysis using the underlying population of each set as an offset variable. Subsequently, data were stratified and analysed by maternal nationality (Greek vs non-Greek) and place of residence (urban/semiurban vs rural). Joinpoint regression analysis22 was thereafter applied to automatically derive, by a software programme, different segments in the mortality evolution curves overall as well as those by maternal nationality and place of residence. In details, the Joinpoint regression analysis is applied to study varying trends over time in order to identify the time point(s) in which the trend significantly changes. The location of the joinpoint is not known a priori and is to be estimated from the data. Therefore, the software takes trend data (eg, IMR) and fits the simplest joinpoint model based on the data. The user supplies the minimum and maximum number of joinpoints. The algorithm starts with the minimum number of joinpoint (eg, 0 joinpoints, which is a straight line) and tests whether more joinpoints are statistically significant and must be added to the model (up to that maximum number). Significance is tested using a Monte Carlo Permutation method. In all models examined in this study, a minimum number of 0 joinpoints and a maximum 1 of 2 joinpoints were tested. Interrupted time series (ITS) analyses were also undertaken as a sensitivity analysis to further explore the effect of crisis on IMR and its components in alternative prespecified years, notably 2008, considered to indicate the initiation of the crisis in Greece—as the value of the GDP of the country was maximum at that year but dropped afterwards13—and in two successive periods 2 years apart (2010 and 2012), to control for possible time lags in observing the impact of the crisis. All ITS models were verified and appropriately adjusted for possible autocorrelation; autoregressive integrated moving average models were used to control for autocorrelation and to estimate treatment effects over multiple periods. In our ITS analysis, a slope ‘<year of interest’ is fitted until the introduction of the crisis, ‘>year of interest’ represents the change in the level of the mortality immediately following the initiation of the crisis and ‘change of slope’ represents the differences between precrisis and postcrisis intervention slopes.
HDI is a summary measure of average achievements of a country’s population in three areas including life expectancy, education and per capita income indicators. Annual HDI values for the underlying populations in the year of death were extracted from the United Nations Development Programme website (http://hdr.undp.org/en/composite/HDI), whereas Poisson regression analysis was used to explore the association of 1 SD of HDI with total IM and its components. All statistical analyses were performed using the SAS software (V.9.4, SAS Institute), Stata software programme, V.13 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, Texas, USA: StataCorp LP) and Joinpoint Regression Program (Joinpoint Regression Program, V.4.5.0.1, June 2017; Statistical Methodology and Applications Branch, Surveillance Research Programme, National Cancer Institute).
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for design or implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
The annual average number of live births during the study period was 105 077, ranging from a high 118 302 (2008) to a low 91 847 live births in 2015. The annual average proportion of Greek mothers was 83.7%, whereas the remaining were mainly economic migrants. During the period 2004–2016, a total of 4862 infant deaths were recorded of whom 4238 (87.2%) were of infants born to Greek mothers, whereas among the remaining 615 deaths of infants born to non-Greek mothers, 298 (48.5%) were of infants born to Albanian mothers, 146 (23.7%) of infants born to mothers from Balkan countries and countries of the former Soviet Union, 77 (12.5%) from Asia, 47 (7.6%) from countries of the European Union or other developed countries and 47 (7.6%) from Africa. During the early and late neonatal period, 2107 (43.3%) and 1136 (23.4%) deaths occurred, respectively, whereas another 1617 (33.3%) of deaths were recorded in the post neonatal period. The annual average IMR was 3.5 over 1000 live births, whereas the corresponding figures for the early, late and post neonatal period were 1.5‰, 0.8‰ and 1.2‰, respectively. The number of live births and infant deaths, total IMR per 1000 live births in infants born to Greek and non-Greek mothers as well as HDI values in Greece during the study period are shown in table 1. Moreover, infant deaths and total IMR by place of residence (urban/semiurban vs rural) are shown in online supplementary table 1.
Table 1.
Live births, infant deaths, total infant mortality rates (IMR) per 1000 live births in infants born to Greek and non-Greek mothers, and Human Development Index (HDI), in Greece during the period 2004–2016
| Year | Infants born to Greek mothers | Infants born to non-Greek mothers | HDI | ||||
| Live births (N) |
Infant deaths (N) | Mortality rates/1000 live births | Live births (N) |
Infant deaths (N) | Mortality rates/1000 live births | ||
| 2004 | 88 805 | 403 | 4.5 | 16 825 | 26 | 1.5 | 0.835 |
| 2005 | 89 819 | 383 | 4.3 | 17 678 | 26 | 1.5 | 0.845 |
| 2006 | 92 590 | 379 | 4.1 | 19 396 | 36 | 1.9 | 0.851 |
| 2007 | 91 462 | 359 | 3.9 | 20 412 | 38 | 1.9 | 0.849 |
| 2008 | 96 329 | 281 | 2.9 | 21 931 | 32 | 1.5 | 0.857 |
| 2009 | 95 640 | 307 | 3.2 | 22 244 | 58 | 2.6 | 0.858 |
| 2010 | 93 209 | 355 | 3.8 | 21 351 | 80 | 3.7 | 0.856 |
| 2011 | 87 445 | 282 | 3.2 | 18 680 | 74 | 4.0 | 0.852 |
| 2012 | 84 868 | 241 | 2.8 | 15 153 | 52 | 3.4 | 0.854 |
| 2013 | 80 938 | 292 | 3.6 | 13 063 | 53 | 4.1 | 0.856 |
| 2014 | 79 985 | 298 | 3.7 | 12 144 | 47 | 3.9 | 0.864 |
| 2015 | 79 919 | 320 | 4.0 | 11 919 | 44 | 3.7 | 0.866 |
| 2016 | 80 166 | 338 | 4.2 | 12 721 | 49 | 3.9 | 0.868 |
Excluding missing maternal nationality values.
bmjopen-2018-025287supp001.pdf (390.4KB, pdf)
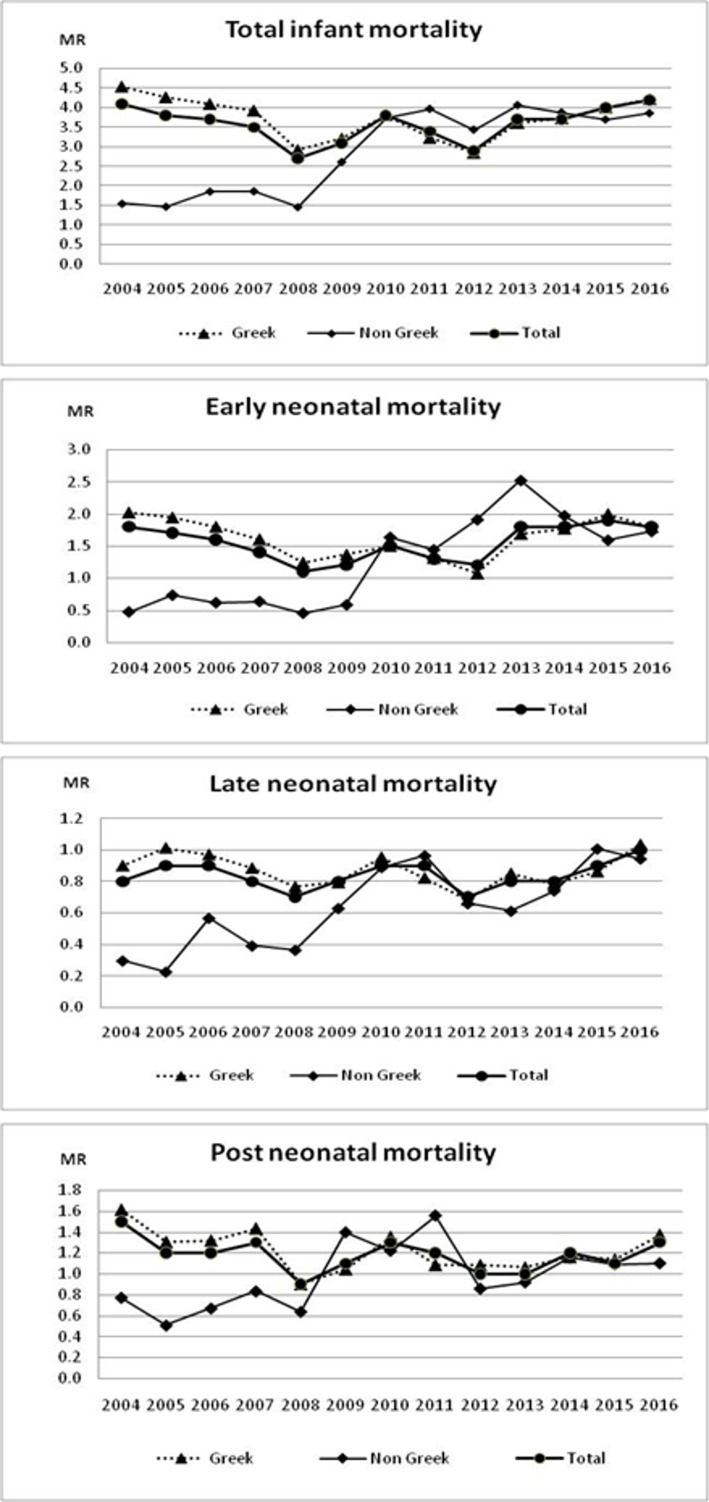
Of note, in the beginning of the study period in 2004, notably well before the initiation of the crisis, IMR and its components were twofold to fourfold higher among infants born to Greek mothers in comparison with rates in infants born to non-Greek origin mothers. During the subsequent 4–5 years, however, rates among Greeks followed downward trends, whereas among non-Greeks inflated reaching almost similar values to those observed in infants born to Greek mothers (figure 1).
Figure 1.
Evolution of infant early, late and post neonatal mortality rates in Greece (2004–2016) overall and by maternal nationality. MR, mortality rate/s.
Overall, during the study period, among infants born to Greek mothers, Poisson regression analyses showed decreasing trends in IMR and PNM rate (PNMR) (−0.9%; 95% CI −1.7% to −0.1% and −1.6%; −3.0% to −0.2% annually, respectively, p=0.02 for each), whereas no significant change in ENM rate (ENMR) and LNM rate (LNMR) was observed (table 2). Interestingly, mortality trends changed differentially by place of residence; significant decline of IMR trends (−2.1%; −2.9% to −1.3% annually, p<0.0001) and all its components was observed among infants born to Greek mothers living in urban areas, whereas among infants born to Greek mothers in rural areas, a significant increase of IMR (+10.6%; 7.6% to 13.6% annually, p=0.002), ENMR (+24.1%; 17.0% to 31.5% annually, p<0.0001) and LNMR trend (+12.7%; 6.5% to 19.2% annually, p<0.0001) was observed (table 2). By contrast, among infants of non-Greek mothers, the low starting IMR increased significantly (+9.4%; 6.9% to 11.9% annually, p<0.0001) due to significant increases of ENMR, LNMR and PNMR (max ENMR: +12.5%; 8.6% to 16.5% annually, p<0.0001) leading to a non-significant pattern of IMR evolution for Greece overall (p=0.50) (table 2). Further analysis by nationality of non-Greek mothers showed significant increases of IMR trends in all ethnic groups with average annual percent change 7.6% (95% CI 4.2% to 11.1%) in infants born to Albanian mothers, 8.6% (3.7% to 13.8%) in infants born to mothers from Balkan countries and countries of the former Soviet Union, 9.4% (2.8% to 16.3%) in infants born to mothers from Asia, 9.4% (1.1% to 18.3%) in infants born to mothers from countries of the European Union or other developed countries and 21.1% (11.0% to 32.3%) in infants born to mothers from Africa. HDI trends increased significantly, by 0.1% (95% CI 0.06% to 0.13%) annually, during the study period. Inverse associations of HDI with IMR, ENMR and PNMR, restricted to Greek mothers’ infants, were observed (table 2).
Table 2.
Poisson regression derived changes and 95% CI of infant (IMR), early (ENMR), late (LNMR) and post neonatal mortality rates (PNMR): annual percent of change (APC) for place of residence and maternal nationality (2004–2016); percept of change (PC) for 1 SD of Human Development Index (HDI) controlling for year of birth
| IMR | ENMR | LNMR | PNMR | |||||||||
| N | APC (95% CI) | P value | N | APC (95% CI) | P value | N | APC (95% CI) | P value | N | APC (95% CI) | Pvalue | |
| Maternal nationality | ||||||||||||
| Greek | 4238 | −0.9 (−1.7 to −0.1) | 0.02 | 1849 | −0.6 (−1.8 to 0.7) | 0.35 | 995 | −0.6 (−2.3 to 1.1) | 0.46 | 1393 | −1.6 (−3.0 to –0.2) | 0.02 |
| Non-Greek | 615 | 9.4 (6.9 to 11.9) | <0.0001 | 258 | 12.5 (8.6 to 16.5) | <0.0001 | 138 | 8.0 (3.1 to 13.2) | 0.001 | 218 | 4.4 (0.6 to 8.4) | 0.02 |
| All* | 4862 | 0.3 (−0.5 to 1.0) | 0.50 | 2107 | 0.9 (−0.3 to 2.1) | 0.13 | 1136 | 0.4 (−1.2 to 2.0) | 0.65 | 1617 | −0.9 (−2.2 to 0.5) | 0.20 |
| Urbanisation | ||||||||||||
| Urban–semiurban | ||||||||||||
| Greek | 3850 | −2.1 (−2.9 to −1.3) | <0.0001 | 1738 | −2.0 (−3.3 to –0.8) | 0.002 | 906 | −1.8 (−3.5 to 0.0) | 0.05 | 1206 | −2.4 (−3.9 to –0.9) | 0.002 |
| Non-Greek | 563 | 8.8 (6.3 to 11.4) | <0.0001 | 243 | 13.2 (9.2 to 17.4) | <0.0001 | 123 | 6.7 (1.5 to 12.2) | 0.01 | 197 | 4.9 (0.9 to 9.2) | 0.02 |
| Any* | 4421 | −0.8 (−1.6 to 0.0) | 0.05 | 1981 | −0.3 (−1.5 to 0.9) | 0.61 | 1037 | −0.8 (−2.4 to 0.9) | 0.36 | 1408 | −1.5 (−2.9 to 0.0) | 0.04 |
| Rural | ||||||||||||
| Greek | 388 | 10.6 (7.6 to 13.6) | 0.002 | 108 | 24.1 (17.0 to 31.5) | <0.0001 | 93 | 12.7 (6.5 to 19.2) | <0.0001 | 187 | 3.3 (−0.6 to 7.4) | 0.09 |
| Non-Greek | 38 | 14.0 (4.0 to 24.9) | 0.005 | 10 | 15.5 (−2.4 to 36.8) | 0.09 | 11 | 18.1 (0.3 to 39.0) | 0.05 | 17 | 4.9 (−7.6 to 19.1) | 0.46 |
| Any* | 427 | 10.9 (8.1 to 13.9) | <0.0001 | 118 | 24.3 (17.6 to 31.4) | <0.0001 | 104 | 14.7 (8.6 to 21.1) | <0.0001 | 205 | 3.0 (−0.7 to 6.9) | 0.11 |
| HDI | ||||||||
| PC | PC | PC | PC | |||||
| Greek | −8.6 (−14.8 to −1.9) | 0.01 | −11.3 (−20.8 to –1.4) | 0.03 | 3.5 (−10.9 to 20.1) | 0.66 | −12.3 (−22.2 to –1.2) | 0.03 |
| Non-Greek | −5.7 (−25.0 to 18.7) | 0.62 | −19.8 (−44.8 to 16.6) | 0.25 | 20.0 (−28.6 to 101.7) | 0.49 | −1.3 (−30.7 to 40.5) | 0.94 |
| All* | −9.5 (−15.3 to −3.2) | 0.004 | −14.0 (−22.3 to –4.7) | 0.004 | 3.3 (−10.4 to 19.3) | 0.65 | −11.4 (−20.8 to –0.7) | 0.04 |
*Including missing maternal nationality values.
In order to examine whether IMR, in our study population, might have been influenced by any variation in the registration of births in cases of uncertain viability, we analysed separately the infant deaths in the first day of life; trends of IMR in this age group, over the study period, were non-significant (average annual percent change: −1.22%; 95% CI −3.79% to 1.42%; p=0.36).
By Joinpoint regression analyses, a break was identified in the IMR curve among infants born to Greek mothers restricting the decreasing IMR trend to the period 2004–2012 (−4.5%; 95% CI −7.6% to −1.3% annually, p=0.01); a significant decline in ENMR trend until 2011 (−6.5%; 95% CI −11.4% to −1.4% annually, p=0.02) was also found (table 3). Of note, however, in the most recent study period following the crisis, non-significant increasing trends of IMR (2012–2016: +9.3% annually, p=0.07) and ENMR (2011–2016: +10.2% annually, p=0.06) were observed. By contrast, among infants born to non-Greek mothers, the high IMR increases (+17.1%; 95% CI 8.1% to 26.9% annually, p=0.002) were restricted to the period 2004–2011 with no statistically significant change thereafter (2011–2016); no break was identified for ENMR curve. Significant increases in IMR and ENMR trends after the year 2008 were observed in the total study population, whereas no break was found for LNMR and PNMR measures in Greeks, non-Greeks or the total study population (table 3).
Table 3.
Joinpoint regression derived annual percent of change (APC) and 95% CIs of infant (IMR), early neonatal (ENMR), late neonatal (LNMR) and post neonatal (PNMR) mortality rates by maternal nationality
| IMR | ENMR | |||||||
| Time period | N | APC (95% CI) | P value | Time period | N | APC (95% CI) | P value | |
| Greek | 2004–2012 | 2870 | −4.5 (−7.6 to −1.3) | 0.01 | 2004–2011 | 1118 | −6.5 (−11.4, to −1.4) | 0.02 |
| 2012–2016 | 1368 | 9.3 (−1.1 to 20.9) | 0.07 | 2011–2016 | 731 | 10.2 (−0.4 to 21.9) | 0.06 | |
| Non-Greek | 2004–2011 | 333 | 17.1 (8.1 to 26.9) | 0.002 | 2004–2016 | 258 | 13.8 (6.7 to 21.3) | 0.001 |
| 2011–2016 | 282 | 0.2 (−11.5 to 13.5) | 0.97 | |||||
| All* | 2004–2008 | 1807 | −7.5 (−14.6 to 0.3) | 0.06 | 2004–2008 | 780 | −10.7 (−19.9 to −0.5) | 0.04 |
| 2008–2016 | 3055 | 3.6 (0.7 to 6.6) | 0.02 | 2008–2016 | 1327 | 6.1 (2.1 to 10.3) | 0.01 | |
| LNMR | PNMR | |||||||
| Time period | N | APC (95% CI) | P value | Time period | N | APC (95% CI) | P value | |
| Greek | 2004–16 | 995 | −0.6 (−2.5 to 1.4) | 0.54 | 2004–16 | 1393 | −1.7 (−4.0 to 0.8) | 0.16 |
| Non-Greek | 2004–16 | 138 | 9.1 (3.5 to 14.9) | 0.003 | 2004–16 | 218 | 4.7 (−0.8 to 10.6) | 0.09 |
| All* | 2004–16 | 1136 | 0.6 (−1.3 to 2.5) | 0.48 | 2004–16 | 1617 | −0.8 (−3.0 to 1.4) | 0.42 |
No break in the time period examined was identified for ENMR in non-Greeks, as well as for LNMR and PNMR measures in Greeks, non-Greeks or the total study population.
*Including missing maternal nationality values.
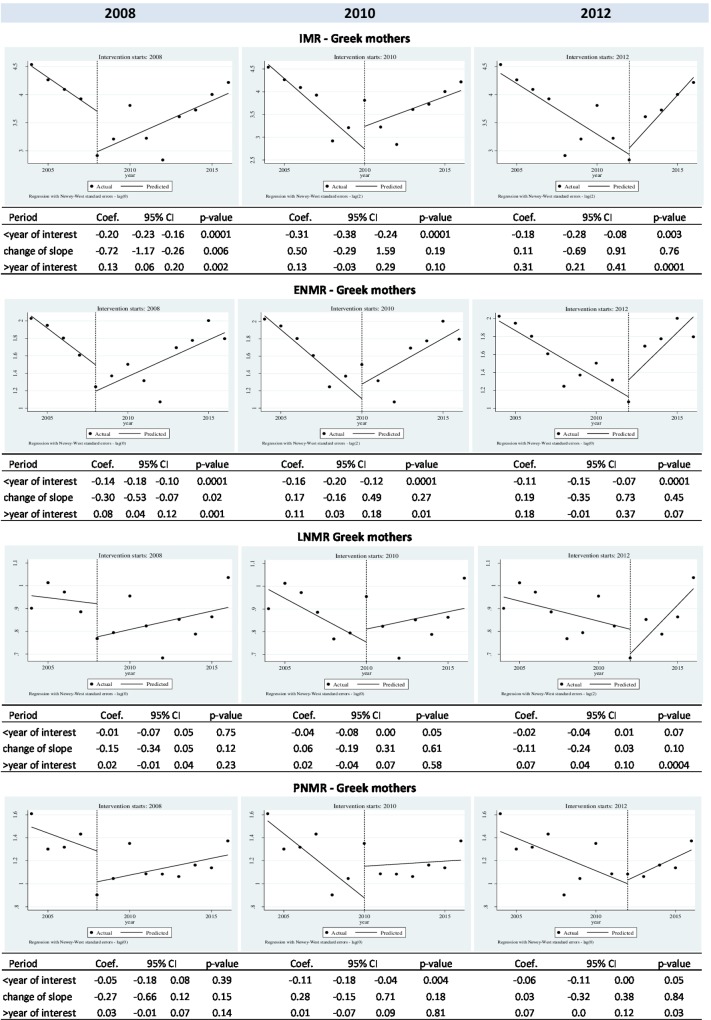
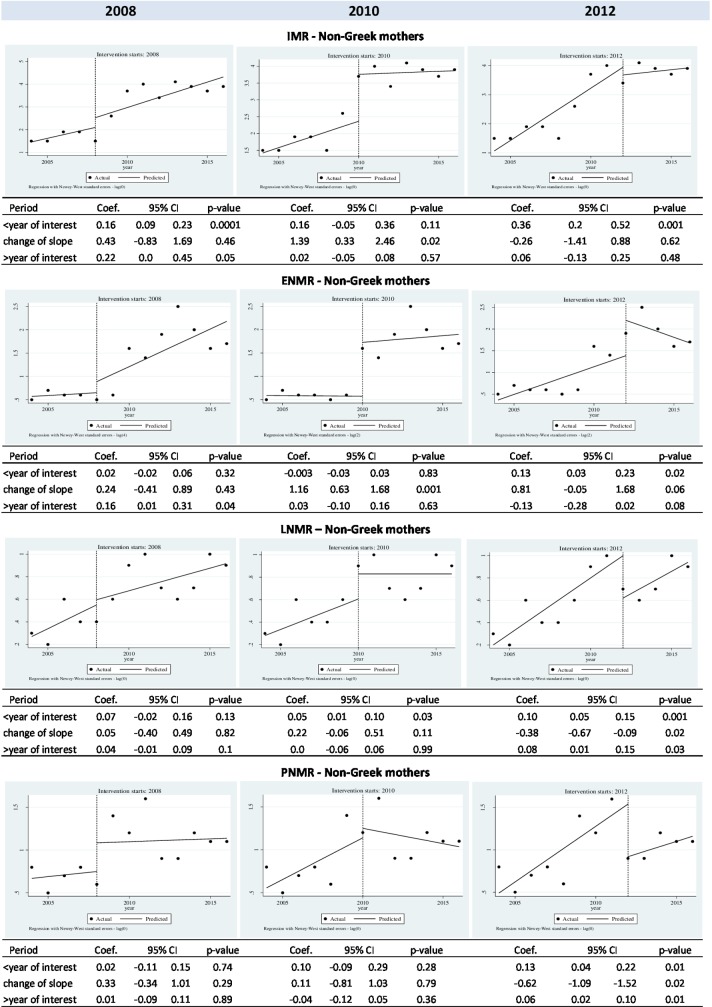
The results of ITS analyses in the preset years 2008, 2010 and 2012 are shown in figures 2 and 3. Compared with the joinpoint regression showing non-significant increases in IMR from 2012 to 2016 for infants born to Greek mothers, ITS analysis showed a significant increase in IMR (p=0.0001) in this population during the same time period and further identified significant increases in LNMR (p=0.0004) and PNMR trends (p=0.03). Regarding the non-significant increases of ENMR trends after the year 2011 by Joinpoint regression in infants born to Greek mothers (p=0.06), ITS analysis showed a non-significant increase during the post 2012 time period (p=0.07); however, a significant increase during the post 2010 time period in these infants was observed (p=0.01) (figure 2). In infants born to non-Greek mothers, while a significant increase in IMR trends was found by Joinpoint regression analyses during the period 2004–2011, by ITS analyses—depending on when the year of interest was being defined (2010 or 2012)—the increase was either not significant (2004–2010, p=0.11) or significant (2004–2012, p=0.001); no change in IMR was identified by ITS analysis over the 2010–2016 or 2012–2016 time periods in non-Greek mothers’ infants (figure 3).
Figure 2.
Interrupted time series analyses for evolution of infant (IMR), early (ENMR), late (LNMR) and post neonatal mortality rates (PNMR) in alternative prespecified years of interest (2008, 2010 and 2012) in infants born to Greek mothers.
Figure 3.
Interrupted time series analyses for evolution of infant (IMR), early (ENMR), late (LNMR) and post neonatal mortality rates (PNMR) in alternative prespecified years of interest (2008, 2010 and 2012) in infants born to non-Greek mothers.
Discussion
Trends of neonatal and infant mortality in Greece, spanning from 2004—before the initiation of crisis in 2008—to 2016, are not homogeneous, given significant increases in the relatively small proportion of infants born to non-Greek nationality mothers as contrasted to declining IMR trends among Greek mothers’ infants, differentials by place of residence and also increases in IM indices among Greek mothers’ infants noted ~4 years after the crisis initiation. Specifically, the ‘brake’ of 2012 identified, by Jointpoint regression analysis, non-significant increases of ~10% annually, in IMR and ENMR trends, whereas by ITS analyses, significant increases in IMR, LNMR and PNMR trends were observed thereafter among infants born to Greek mothers, a fact indicating how sensitive the results are depending on the statistical method used. Changes in HDI during the study period were also reflected in the inverse associations of HDI with ENMR and IMR, but also PNMR, among infants born to Greek mothers.
Strengths of the present investigation, as contrasted to previously Greek-based published studies,9 18 20 21 23 include the longest follow-up period of national data, namely since 2004, before the crisis, when the first data on maternal ethnicity became electronically available, to the latest available year 2016. Of great importance is also the fact that, for the first time, the maternal ethnicity was considered in the analyses explaining part, if not most, of the heterogeneity of trends through the study period. To this end, three complimentary statistical methodologies were used to describe the overall evolution depicted in figure 1. Thus, we were able to enhance the validity of the results pertaining to the study of the evolution of individual IMR components, namely ENMR, LNMR and PNMR, in association with socioeconomic factors (ie, maternal nationality, place of residence and HDI) for which individual data have been available on a nationwide level among both deaths and live births during the study period. Calculation of IMR and its components was based on the number of live births; yet, the absence of a linkage system between birth and death data consists a limitation of the study. The absence of a linkage system, as well as that of other official registries in Greece, has not allowed use of known determinants of socioeconomic deprivation or social coherence, such as parental education, employment/occupation, marital status, family income and household size, neither were data on the role of biological factors, such as parental age, gestational age and birth weight, or multiplicity of pregnancy available for both the live births and deaths series.5 19 24 Besides, the study period, with available information on maternal nationality and place of residence, was rather short leading to ITS analyses with few data points; however, ITS analysis can be used even for few observations; no log transformation is needed but the results should be interpreted with caution as the power depends on various factors.25 Lastly, analyses by specific cause of infant death were not set among the outcome measures of this study.
Assessing migration as a determinant of perinatal health outcome and infant death in the developed countries is a complex undertaking resulting in conflicting results of published studies. Specifically, some studies have shown that ethnic minority is a significant risk factor for unfavourable perinatal outcomes and increased neonatal and infant mortality,18 26–33 especially if it coincides with a financial crisis, as was the case in Greece. Factors possibly contributing to the increased risk for poorer outcomes among children born to migrants include socioeconomic disadvantage, poor communication, discrimination, reduced utilisation of health facilities, low quality of care, and also stress and consanguinity or differing attitudes to screening and termination of pregnancy associated with preterm birth, low birth weight or congenital anomalies and lethal inherited diseases.26 30 34–36 By contrast, other studies present similar or even better perinatal health outcomes among some migrant groups than among natives (‘healthy migrant effect/paradox’).26–28 37 38 Refugees have been recognised as the most vulnerable group suffering increased severe neonatal morbidity and infant mortality risk,26 28 although no absolutely clear pattern regarding refugee or non-refugee status among migrants has been identified.34
Ιn our study, starting rates of IMR and its components among infants born to non-Greek mothers were lower compared with those of Greek mothers. Of note, the ratio of non-Greek infants among live births during 2009–2016 versus 2004–2008 was only 1.32, whereas the respective figure among infant deaths was almost threefold (data not shown). Actually, in the precrisis era, non-Greek mothers of newborns comprised mainly economic migrants, most of them of Albanian nationality living for many years, or even born, in Greece. After 2008, Greece experienced an influx of refugees with the majority of them fleeing from war and terror in Syria, Occupied Palestinian Territory, but also from Afghanistan, Iraq and other countries.16 17 It could be suggested that changes in the homogeneity of foreign mothers during the study period, in association with the country’s economic difficulties, might have led from the ‘healthy migrant effect’, observed before 2008, to the deterioration of IM indicators and IMR trends, afterwards, in infants born to non-Greek mothers. We did observe significant increases in IMR trends in all ethnic groups of non-Greek mothers during the study period, especially in infants born to mothers from Africa; however, as the numbers by individual maternal nationality were rather small, this issue needs to be further studied.
Simultaneously with immigration to/through Greece, the country experienced the third wave of mass emigration in the 20th and 21st centuries; over 400 000 Greek citizens left Greece since the onset of the economic crisis, in 2008, seeking new opportunities and employment in other countries, mainly Germany, the UK and the Netherlands.39 40 The current emigration wave of Greeks involved mostly highly educated people (the so called ‘brain-drain’) of young age, leading to a decrease in the number of Greek women of childbearing age.41 This fact, along with the decrease in the fertility rate by almost 10% between 2008 and 2016, contributes significantly to the reduction in the annual number of live births in Greece by almost 23% during the period of the economic crisis.41 42 Furthermore, the flow of mostly affluent and well-educated people going outside Greece could also contribute to increases in IMR among Greek children following the crisis.
Indeed, the strongly decreasing IMR trends among Greek infants were stagnated after a lag time of ~4 years of crisis and equalised with the previously sharply increasing trends among non-Greek maternal nationality infants; this time lag is reasonable43 and in line with previous findings showing that following reductions in the government healthcare spending in Europe, the greatest negative effect on neonatal and post neonatal mortality was 4 and 5 years later, respectively.6 The irony is that the period 2012–2016, during which the crisis was deepening13 14 and stricter economic austerity measures were applied,44 disparities gap in IMR trends diminished against the Greek population; IMR trends deteriorated only in infants born to Greek mothers, whereas in infants born to non-Greek mothers, IMR trends approached an anelastic highest value up to 2011 with no statistically significant change thereafter.
Disparities in IMR exist across geographic areas even in well-developed countries; that is, IMR in the USA vary by urbanisation level of maternal residency being lowest in large urban counties but highest in rural areas.45 Rural women may face health challenges related to geographic barriers to care (less timely and/or appropriate care) and physician shortages, but they may also present differences in a number of socioeconomic and demographic risk factors, such as less education, lower income, younger age at pregnancy or greater number of children, in comparison with their urban counterparts.46 47 The increasing IMR trends during the study period in infants born to Greek mothers living in rural areas, as opposed to the declining IMR trends in those born to Greek mothers living in urban/semiurban areas, is worrisome. Specific causes should be further studied and addressed. Regarding infants born to non-Greek mothers, the increasing IMR trends despite living in urban areas can be explained by previous reports showing that other risk factors, that is, young maternal age (<20 years) or maternal ethnic minority, may be more powerful than place of residence.47
Among the three IMR components, ENMR seemed to be the most ‘sensitive’ in reflecting adverse impacts on child health. Specifically, ENMR was overall positively associated with rural place of residence of Greek mothers' children and also presented the most sizeable increase among IM indices in non-Greeks (table 2). Moreover, among the three IM components, ENMR was the first or the only one, depending on the statistical method used, that increased after the crisis initiation in infants born to Greek mothers. ENMR, in developed countries, including Greece, represents more than 70% of neonatal deaths on account mainly of prematurity/low birth weight and congenital anomalies.14 48–51 Actually, it reflects perinatal health and care during pregnancy and labour, and also postnatal care in the first week of life.50 Increased incidence of impaired perinatal parameters including low birth weight, prematurity and increased maternal age and rate of caesarian section has been reported during the years of the economic decline in Greece.18 19 Cuts in public health expenditures between 2008 and 2016, reduction in healthcare workforce and paediatric nurses as well as reduction in the number of obstetrics beds, obstetricians and midwifes (−45.5%, −60.2% and −27.5%, respectively)14 could possibly explain, at least in part, the observed positive ENMR trends during the postcrisis period in Greece.
The exact mechanisms leading to the disparities in trends of neonatal and infant mortality observed in this study remain to be further explored. Specific maternal, family and infant features, including detailed and punctual information on the causes of infant deaths, would have shed more light on the links between IMR trends and socioeconomic factors but were beyond the scope of this article and left for future research. Meanwhile, policies and programmes should be implemented to mitigate the negative impact of the crisis on population and infant health in Greece. Vulnerable groups, such as mothers of non-Greek nationality, of low income or of rural place of residence, should be specifically addressed and their rights to health protected. Barriers in the access of refugees to the Greek healthcare system have been identified; they are mostly related to language, culture and inadequate information about the healthcare system, but also include difficulties in the coordination of Health Services, transportation problems, issues in obtaining expertise medical assessment in the camps, lack of continuity of care, financial difficulties in making out-of-pocket payments for health and social care services and administrative barriers, among others.52 In response, the Greek government and several non-governmental organisations initiated commendable actions, that is, National Health System services free of charge for uninsured and vulnerable social groups including asylum seekers, translation services in public hospitals, access to specialist care/treatment with gynecologists (mostly women), midwives, dentists, psychologists and psychiatrists being lately included in the camp clinics.52 These actions may have prevented deterioration of IMR which are being kept at steady levels after 2011–2012 in infants of non-Greek mothers. Efforts should be continued and intensified, however, to ensure equity with local populations. Strong governmental integration policy for minorities paired with initiatives to improve social coherence, a deeply rooted mechanism for protection of health among those in need in the Greek society, along with further improvements in primary healthcare delivery could help to alleviate the cost in infant lives and ensure healthy adulthood.32 51 Irrespective of the crisis, improvements in the quality of perinatal and neonatal care, including centralisation of very preterm deliveries, establishment of regional perinatal centres, monitoring of the implementation of evidence-based practices in maternity and neonatal units, as well as increase in health expenditures, healthcare workforce, number of doctors and midwifes/nurses, could decrease ENMR, eventually leading to overall decrease in IMR in Greece.50
Supplementary Material
Acknowledgments
ELSTAT has provided individual anonymised data.
Footnotes
Contributors: EP and GC were involved in the initial conception of the study. All authors contributed to the design, analysis and interpretation of data. TS, ND and EP developed the first draft of the manuscript and all authors critically revised it and approved the final version. ND, AA and CM performed the statistical analyses. EE reviewed statistics and contributed significantly for ITS analyses. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The corresponding author ensures that all the journal’s administrative requirements are properly completed.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon request from ELSTAT (http://www.statistics.gr/el/statistical-data-request)
Patient consent for publication: Not required.
References
- 1. Petridou E, Valadian I, Trichopoulos D, et al. Medical services and socioeconomic factors: Determinants of infant mortality in Greece. Hygie 1989;3:20–3. [PubMed] [Google Scholar]
- 2. WHO. The determinants of health. http://www.who.int/hia/evidence/doh/en (Accessed 30/5/2018).
- 3. Zylbersztejn A, Gilbert R, Hjern A, et al. Child mortality in England compared with Sweden: a birth cohort study. Lancet 2018;391:2008–18. 10.1016/S0140-6736(18)30670-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rajmil L, Fernandez de Sanmamed MJ, Choonara I, et al. International Network for Research in Inequalities in Child Health (INRICH). Impact of the 2008 economic and financial crisis on child health: a systematic review. Int J Environ Res Public Health 2014;11:6528–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Glonti K, Gordeev VS, Goryakin Y, et al. A systematic review on health resilience to economic crises. PLoS One 2015;10:e0123117 10.1371/journal.pone.0123117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Budhdeo S, Watkins J, Atun R, et al. Changes in government spending on healthcare and population mortality in the European union, 1995–2010: a cross-sectional ecological study. J R Soc Med 2015;108:490–8. 10.1177/0141076815600907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tapia Granados JA, Rodriguez JM. Health, economic crisis, and austerity: A comparison of Greece, Finland and Iceland. Health Policy 2015;119:941–53. 10.1016/j.healthpol.2015.04.009 [DOI] [PubMed] [Google Scholar]
- 8. Regidor E, Barrio G, Bravo MJ, et al. Has health in Spain been declining since the economic crisis? J Epidemiol Community Health 2014;68:280–2. 10.1136/jech-2013-202944 [DOI] [PubMed] [Google Scholar]
- 9. Laliotis I, Ioannidis JPA, Stavropoulou C. Total and cause-specific mortality before and after the onset of the Greek economic crisis: an interrupted time-series analysis. Lancet Public Health 2016;1:e56–e65. 10.1016/S2468-2667(16)30018-4 [DOI] [PubMed] [Google Scholar]
- 10. Parmar D, Stavropoulou C, Ioannidis JP. Health outcomes during the 2008 financial crisis in Europe: systematic literature review. BMJ 2016;354:i4588 10.1136/bmj.i4588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O’Donnell C, Burns N, Dowrick C, et al. Health-care access for migrants in Europe. Lancet 2013;382:393 10.1016/S0140-6736(13)61666-9 [DOI] [PubMed] [Google Scholar]
- 12. Karanikolos M, Heino P, McKee M, et al. Effects of the Global Financial Crisis on Health in High-Income Oecd Countries: A Narrative Review. Int J Health Serv 2016;46:208–40. 10.1177/0020731416637160 [DOI] [PubMed] [Google Scholar]
- 13. Organisation for Economic Co-operation and Development OECD data. 2016. https://data.oecd.org [Accessed 30 May 2018].
- 14. Hellenic Statistical Authority Statistics. 2016. www.statistics.gr [Accessed 30 May 2018].
- 15. Zavras D, Zavras AI, Kyriopoulos II, et al. Economic crisis, austerity and unmet healthcare needs: the case of Greece. BMC Health Serv Res 2016;16:309 10.1186/s12913-016-1557-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. European Union. The EU and the migration crisis. 2017. http://publications.europa.eu
- 17. Mertens E, Rockenschaub G, Economopoulou A, et al. Assessment of public health issues of migrants at the Greek-Turkish border, April 2011. Euro Surveill 2012;17:pii: 20056. [PubMed] [Google Scholar]
- 18. Zografaki I, Papamichail D, Panagiotopoulos T. Adverse effect of the financial crisis in Greece on perinatal factors. Eur J Public Health 2018;28:1116–21. 10.1093/eurpub/cky078 [DOI] [PubMed] [Google Scholar]
- 19. Sdona E, Papamichail D, Ragkou E, et al. Greek economic crisis and impaired perinatal parameters: experience from a public maternity hospital. J Matern Fetal Neonatal Med 2018;31:2371–5. 10.1080/14767058.2017.1342803 [DOI] [PubMed] [Google Scholar]
- 20. Michas G, Varytimiadi A, Chasiotis I, et al. Maternal and child mortality in Greece. Lancet 2014;383:691–2. 10.1016/S0140-6736(14)60251-8 [DOI] [PubMed] [Google Scholar]
- 21. Filippidis FT, Gerovasili V, Millett C, et al. Medium-term impact of the economic crisis on mortality, health-related behaviours and access to healthcare in Greece. Sci Rep 2017;7:46423 10.1038/srep46423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- 23. Simou E, Koutsogeorgou E. Effects of the economic crisis on health and healthcare in Greece in the literature from 2009 to 2013: a systematic review. Health Policy 2014;115:111–9. 10.1016/j.healthpol.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 24. Petridou ET, Georgakis MK, Erdmann F, et al. Advanced parental age as risk factor for childhood acute lymphoblastic leukemia: results from studies of the Childhood Leukemia International Consortium. Eur J Epidemiol 2018;33:965–76. 10.1007/s10654-018-0402-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 2017;46:348–55. 10.1093/ije/dyw098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gissler M, Alexander S, MacFarlane A, et al. Stillbirths and infant deaths among migrants in industrialized countries. Acta Obstet Gynecol Scand 2009;88:134–48. 10.1080/00016340802603805 [DOI] [PubMed] [Google Scholar]
- 27. Gagnon AJ, Zimbeck M, Zeitlin J, et al. Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med 2009;69:934–46. 10.1016/j.socscimed.2009.06.027 [DOI] [PubMed] [Google Scholar]
- 28. Wanigaratne S, Cole DC, Bassil K, et al. Severe Neonatal Morbidity Among Births to Refugee Women. Matern Child Health J 2016;20:2189–98. 10.1007/s10995-016-2047-4 [DOI] [PubMed] [Google Scholar]
- 29. Puthussery S. Perinatal outcomes among migrant mothers in the United Kingdom: Is it a matter of biology, behaviour, policy, social determinants or access to health care? Best Pract Res Clin Obstet Gynaecol 2016;32:39–49. 10.1016/j.bpobgyn.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 30. Wanner P, Bollini P. The contribution of the foreign population to the high level of infant mortality in Switzerland: a demographic analysis. BMC Pregnancy Childbirth 2017;17:151 10.1186/s12884-017-1332-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cantarutti A, Franchi M, Monzio Compagnoni M, et al. Mother’s education and the risk of several neonatal outcomes: an evidence from an Italian population-based study. BMC Pregnancy Childbirth 2017;17:221 10.1186/s12884-017-1418-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bollini P, Pampallona S, Wanner P, et al. Pregnancy outcome of migrant women and integration policy: a systematic review of the international literature. Soc Sci Med 2009;68:452–61. 10.1016/j.socscimed.2008.10.018 [DOI] [PubMed] [Google Scholar]
- 33. Gotsens M, Malmusi D, Villarroel N, et al. Health inequality between immigrants and natives in Spain: the loss of the healthy immigrant effect in times of economic crisis. Eur J Public Health 2015;25:923–9. 10.1093/eurpub/ckv126 [DOI] [PubMed] [Google Scholar]
- 34. Nybo Andersen AM, Gundlund A, Villadsen SF. Stillbirth and congenital anomalies in migrants in Europe. Best Pract Res Clin Obstet Gynaecol 2016;32:50–9. 10.1016/j.bpobgyn.2015.09.004 [DOI] [PubMed] [Google Scholar]
- 35. Di Renzo GC, Tosto V, Giardina I. The biological basis and prevention of preterm birth. Best Pract Res Clin Obstet Gynaecol 2018;52:13–22. 10.1016/j.bpobgyn.2018.01.022 [DOI] [PubMed] [Google Scholar]
- 36. Wanigaratne S, Cole DC, Bassil K, et al. The influence of refugee status and secondary migration on preterm birth. J Epidemiol Community Health 2016;70:622–8. 10.1136/jech-2015-206529 [DOI] [PubMed] [Google Scholar]
- 37. Kirby RS. Perinatal outcomes and nativity: does place of birth really influence infant health? Birth 2011;38:354–6. 10.1111/j.1523-536X.2011.00505.x [DOI] [PubMed] [Google Scholar]
- 38. Sdona E, Papamichail D, Ragkou E, et al. Migration status and perinatal parameters in a Greek public maternity hospital: an illustration of the "healthy immigrant effect". J Matern Fetal Neonatal Med 2019;32:62-6 10.1080/14767058.2017.1371131 [DOI] [PubMed] [Google Scholar]
- 39. Eurostat. Emigration by age group, sex and citizenship. http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=migr_emi1ctz&lang=en [Accessed 04/04/2018].
- 40. Cavounidis J. The changing face of emigration: Harnessing the potential of the New Greek Diaspora. Washington, DC: Migration Policy Institute, 2015. [Google Scholar]
- 41. Vrachnis N, Vlachadis N, Iliodromiti Z, et al. Greece’s birth rates and the economic crisis. Lancet 2014;383:692–3. 10.1016/S0140-6736(14)60252-X [DOI] [PubMed] [Google Scholar]
- 42. Eurostat, “Fertility indicators”. http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_find&lang=en [Accessed 20/09/2018].
- 43. Karanikolos M, Mladovsky P, Cylus J, et al. Financial crisis, austerity, and health in Europe. Lancet 2013;381:1323–31. 10.1016/S0140-6736(13)60102-6 [DOI] [PubMed] [Google Scholar]
- 44. Burki T. Health under austerity in Greece. Lancet 2018;391:525–6. 10.1016/S0140-6736(18)30242-3 [DOI] [PubMed] [Google Scholar]
- 45. Ely DM, Driscoll AK, Mathews TJ. Infant mortality rates in rural and urban areas in the United States, 2014. NCHS data brief, No 285. Hyattsville, MD: National Center for Health Statistics, 2017. [PubMed] [Google Scholar]
- 46. Van de Poel E, O’Donnell O, Van Doorslaer E. What explains the rural-urban gap in infant mortality: household or community characteristics? Demography 2009;46:827–50. 10.1353/dem.0.0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Harris DE, Aboueissa AM, Baugh N, et al. Impact of rurality on maternal and infant health indicators and outcomes in Maine. Rural Remote Health 2015;15:3278. [PubMed] [Google Scholar]
- 48. Heron M. Deaths: Leading Causes for 2015. Natl Vital Stat Rep 2017;66:1–76. [PubMed] [Google Scholar]
- 49. Roncancio CP, Misnaza SP, Peña IC, et al. Trends and characteristics of fetal and neonatal mortality due to congenital anomalies, Colombia 1999-2008. J Matern Fetal Neonatal Med 2018;31:1748–55. 10.1080/14767058.2017.1326901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lehtonen L, Gimeno A, Parra-Llorca A, et al. Early neonatal death: A challenge worldwide. Semin Fetal Neonatal Med 2017;22:153–60. 10.1016/j.siny.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 51. Alexander M, Harding M, Lamarche C. Quantifying the impact of economic crises on infant mortality in advanced economies. Appl Econ 2011;43:3313–23. 10.1080/00036840903559620 [DOI] [Google Scholar]
- 52. Kotsiou OS, Kotsios P, Srivastava DS, et al. Impact of the Refugee Crisis on the Greek Healthcare System: A Long Road to Ithaca. Int J Environ Res Public Health 2018;15:1790 10.3390/ijerph15081790 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-025287supp001.pdf (390.4KB, pdf)