Abstract
Purpose
To determine the incidence of ocular hypertension following surgery for rhegmatogenous retinal detachment in the first 3 months postoperatively and to determine their outcomes in terms of visual acuity, control of IOP, and changes in cup:disc ratio.
Patients and methods
A single center prospective cohort study was done involving patients who underwent retinal surgery for rhegmatogenous retinal detachment. The patients were followed up for 3 months postoperatively and were monitored for development of ocular hypertension. The primary outcome measures were changes in IOP, visual acuity, and cup:disc ratio.
Results
Of the 52 eyes enrolled in the study, 19 eyes developed ocular hypertension in the first 3 months postoperatively, giving an incidence rate of 36.5% (95% CI, 48.9–76.0%). Analysis of mean IOP trends shows that most cases of IOP elevations occur in the first day postoperatively with a sustained elevation up to the first month and then returning to normal levels by the 3rd month. There is a significant increase in mean cup:disc ratio among patients who developed ocular hypertension (p=0.047). Visual acuity trends show that mean visual acuity significantly improved from baseline among cases who maintained normal IOP (p=0.002) as compared to those who developed ocular hypertension (p=0.97), although the difference in final visual acuity at the end of 3 months between groups was not statistically significant (p=0.30).
Conclusion
Ocular hypertension may complicate retinal reattachment surgery. Control of IOP in the acute setting is essential to prevent development of secondary glaucoma.
Keywords: intraocular pressure, ocular hypertension, retinal detachment surgery, secondary glaucoma
Introduction
Ocular hypertension may develop as a complication of vitreoretinal surgery. The incidence of ocular hypertension following vitreoretinal surgery varies depending on various factors, including baseline characteristics of the eye being operated on, specific techniques used in vitreoretinal surgery, and severity of postoperative intraocular inflammation.1,2 The etiology of increased intraocular pressure (IOP) in the postoperative period has likewise been linked to various mechanisms including inflammation, expansion of intravitreal tamponade agents, pupillary block, ciliary body edema, corticosteroid response, and fibrin formation.4 Despite the identification of the numerous mechanisms explaining the rise in IOP, most ophthalmologists would agree that increased IOP following vitreoretinal surgery is usually multifactorial.4 Previous studies which have examined the incidence of elevated IOP after vitreoretinal surgery have been varied in their conclusions with a range of 8.4–36% in the first 2 days postoperatively.1–6
Postoperative eyes have altered intraocular milieu that makes management of these cases more difficult.7,8 Secondary glaucoma invariably develops when ocular hypertension is left untreated, leading to the characteristic changes in optic disc appearance and functional visual field deficits. Secondary glaucoma portends a poorer visual prognosis despite successful retinal re-attachment.8
The primary objective of the study is to determine the incidence of ocular hypertension among patients who underwent surgery for rhegmatogenous retinal detachment. The secondary objective is to describe the outcomes of cases in terms of status of angles, visual acuity, and management for control of IOP.
Materials and methods
Study design
A single-center prospective cohort study was conducted at the Out-Patient Department of the Department of Ophthalmology and Visual Sciences, Sentro Oftalmologico Jose Rizal, Philippine General Hospital. This study adhered to the tenets of the Declaration of Helsinki. The design of the study was approved by the Institutional Review Board and Research Ethics Board of the Philippine General Hospital. Written informed consent was obtained from all patients.
Patient selection and recruitment
The cases comprised of patients of the Surgical Retina Clinic of the Sentro Oftalmologico Jose Rizal of the Philippine General Hospital. Inclusion criteria included patients who were aged 18 and above, diagnosed with rhegmatogenous retinal detachment, and will undergo surgery for repair of retinal detachment. Exclusion criteria included patients with previously diagnosed glaucoma or conditions associated with glaucoma, preoperative application of medications that can alter IOP (including topical or oral ocular hypotensive medications and corticosteroids), clinical findings warranting a diagnosis of glaucoma suspect on preoperative eye examination, and presence of other ocular diseases which may alter IOP (for example, diabetic retinopathy, choroidal detachment, uveitis). Patients were recruited for the study if they satisfied the inclusion and exclusion criteria.
Sample size determination
The sample size was calculated with a margin of error pegged at 10% and a CI of 90%. Assuming a possible 5% loss to follow-up, a sample of 45 eyes was calculated.
Data collection
All subjects underwent a baseline eye examination conducted by the investigators consisting of visual acuity determination, slit lamp examination of the anterior segment, Goldmann applanation tonometry, and optic nerve evaluation using slit lamp biomicroscopy.
Retinal detachment surgery was done by the Surgical Retina service of the Philippine General Hospital. The retinal re-attachment procedures (eg, pars plana vitrectomy, endolaser, endodiathermy, injection of a tamponade agent) that was done on the subjects were determined by the physicians of the Surgical Retina service.
Afterward, postoperative examination was done by the investigators. Repeat visual acuity determination, slit lamp examination of the anterior segment, Goldmann applanation tonometry, gonioscopy, and optic nerve evaluation using slit lamp biomicroscopy were done. Eye examinations were done at 24 hrs, 1 week, 2 weeks, 1 month, and 3 months postoperatively.
Outcome measures
The primary outcome measure was development of ocular hypertension and secondary glaucoma, with parameters including IOP and visible enlargement in cup:disc ratio. Ocular hypertension was defined as IOP greater than 21 mmHg as measured by Goldmann applanation tonometry.
The management done for cases who develop ocular hypertension was decided by the physicians of the Surgical Retina service (or the Glaucoma service if referral to a glaucoma specialist was deemed necessary). A descriptive analysis of the management of secondary glaucoma was done. Among subjects who develop secondary glaucoma, information regarding management and its success rate was obtained.
Statistical analysis
The incidence rates were computed and analyzed using Kaplan–Meier survival analysis. The t-test was employed for statistical analysis of outcome variables which included IOP, cup:disc ratio, and visual acuity.
Results
A total of 64 patients were recruited to study after having met the inclusion and exclusion criteria. Of the recruited patients, 60 underwent vitreoretinal surgery as planned. There were 4 dropouts – 1 patient had the surgery deferred due to financial constraints, 2 patients had scheduling conflicts, and 1 patient elected not to undergo surgery. Of these 60 patients, there were 8 dropouts during the postoperative period due to inability to follow-up to the prescribed schedule. A total of 52 eyes from 52 patients formed the cohort and were included in the analysis.
The age of the study participants ranged from 20 to 72 years with a mean age of 45 years. The cohort comprised of 35 males and 14 females. The demographics and baseline characteristics of the cohort are given in Table 1.
Table 1.
Baseline patient characteristics of cohort
| Feature | Value |
|---|---|
| General features | |
| Age, mean ± SD, years | 47.5±14.7 |
| Sex, male/female, n | 35/17 |
| Laterality, right/left, n | 23/29 |
| Pertinent ophthalmic history, n | |
| Lattice degeneration | 29 |
| Postsurgical | 3 |
| Trauma | 5 |
| Idiopathic | 15 |
| Ophthalmic features | |
| Visual acuity, mean ± SD, logMAR units | 1.41±0.64 |
| IOP, mean ± SD, mmHg | 9.9±4.6 |
| Cup:disc ratio, mean ± SD | 0.35±0.05 |
The study participants underwent retinal reattachment surgery as deemed necessary by the Surgical Retina service. All 52 eyes underwent a standard 23-gauge pars plana vitrectomy, of which 29 eyes also required combined placement of a silicone scleral buckle attached with a silicone encircling band. Phacoemulsification with posterior chamber intraocular lens implantation was done for 7 of the 23 eyes who underwent pars plana vitrectomy alone and 6 of the 29 eyes who underwent combined scleral buckling and pars plana vitrectomy. Fifty eyes (21 of the 23 eyes which underwent pars plana vitrectomy alone and all 29 eyes which underwent combined scleral buckling and pars plana vitrectomy) were filled with silicone oil tamponade with a kinematic viscosity of 1000 centistokes, while the 2 remaining eyes were filled with 20% perfluoropropane (C3F8) gas to achieve a 25% fill of the globe to account for postoperative gas expansion. At the end of the surgery, subconjunctival triamcinolone was injected for each eye. Postoperative medical management included topical moxifloxacin, prednisolone, and atropine. Topical or oral hypotensive medications were added as deemed necessary by the Surgical Retina service. The procedures done and the corresponding number of participants who underwent each procedure are outlined in Table 2.
Table 2.
Distribution of patients undergoing retinal reattachment procedures
| Retinal re-attachment surgery | Number of participants |
|---|---|
| Pars plana vitrectomy alone | |
| With phacoemulsification, silicone oil tamponade | 7 |
| Without phacoemulsification, silicone oil tamponade | 14 |
| Without phacoemulsification, C3F8 tamponade | 2 |
| Combined pars plana vitrectomy and scleral buckling | |
| Without phacoemulsification, silicone oil tamponade | 6 |
| With phacoemulsification, silicone oil tamponade | 23 |
IOP trends in the acute postoperative period
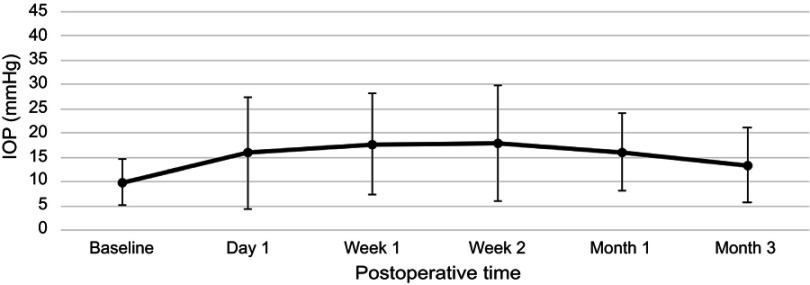
The mean baseline IOP of patients preoperatively was 9.90±4.63 mmHg. There is a trend for increased IOP from baseline beginning in the first postoperative day (p=0.0004), sustained in the first week (p=0.00005), second week (p=0.0004), and first month (p=0.000004) postoperatively. In the third month postoperatively, there is a decrease in mean IOP compared to the first month postoperatively (p-value =0.04), but the value still represents an increase from the baseline IOP (p=0.006). The IOP trends are shown in Figure 1.
Figure 1.
Mean IOP trend of cohort in the postoperative period.
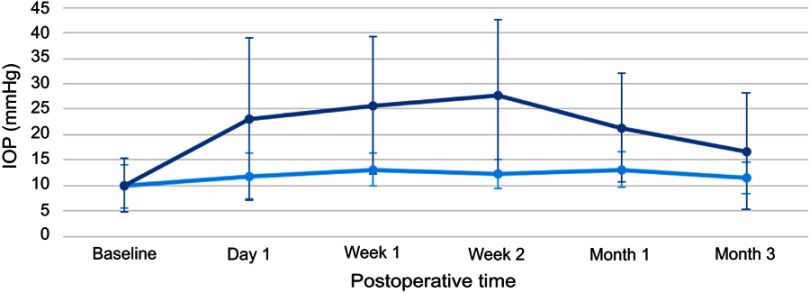
A total of 19 eyes experienced ocular hypertension during the 3-month postoperative period, which gives an incidence rate of 36.5% (95% CI, 48.9–76.0%) by Kaplan–Meier analysis. Among the cases of ocular hypertension, 14 (74% of cases) eyes only had transient elevation which had resolved by the end of the 3-month postoperative period. Only 5 (26% of cases) eyes had persistently elevated IOP. An analysis of those who developed elevations in IOP showed there is a trend for increased IOP similar to the overall trend in IOP for the entire cohort, wherein there is a significant increase from baseline IOP beginning in the first day postoperatively which is maintained throughout the first month postoperatively, decreasing at the third month but still increased from baseline. The trend in IOP among cases with ocular hypertension compared to those who maintained normal IOP is shown in Figure 2. The study showed that most cases (47.37% or 9 of 19 eyes) experienced the first elevation in IOP at the first postoperative day.
Figure 2.
Comparison of mean IOP trend of cases with ocular hypertension (dark blue) and cases maintaining normal IOP (light blue) in the postoperative period.
Comparing the proportion of those who developed ocular hypertension per procedure, the study showed that 39.2% (95% CI, 40.7–77.9%) of cases who underwent combined scleral buckling with pars plana vitrectomy and silicone oil injection had elevated IOP as compared to 36.4% (95% CI, 40.8–82.0%) of cases who underwent pars plana vitrectomy alone with silicone oil injection. The difference in incidence rates between the two procedures was not statistically significant by Kaplan–Meier analysis (p=0.85). There were 2 cases who underwent vitrectomy with C3F8 injection, and 1 of them (50%) developed an increase in IOP during the postoperative period. Compared with similar cases who underwent vitrectomy but used silicone oil as tamponade, the difference in incidence rate of ocular hypertension is not significant (p=0.95). However, since there were only 2 cases who underwent surgery using C3F8 gas as tamponade, statistical analysis of this subgroup may not be meaningful due to low subgroup sample size.
A separate subgroup analysis was done to determine the effect of phacoemulsification on IOP trends. Among cases who underwent pars plana vitrectomy alone, the incidence rate of ocular hypertension was 35.3% for cases with phacoemulsification and 37.1% for cases without phacoemulsification. The difference in incidence rates between the procedures was likewise not statistically significant by Kaplan–Meier analysis (p=0.99). A similar trend was seen for the incidence rate of ocular hypertension among cases who underwent combined scleral buckling and pars plana vitrectomy, with an incidence rate of 39.0% among cases with phacoemulsification and 39.7% among cases without phacoemulsification (p=0.54).
Status of angles
Gonioscopy of patients with ocular hypertension showed a total of 17 eyes had open angles (90%). Of the 17 eyes with open angles, 3 of them had silicone oil droplets in the superior quadrant of the angles. The remaining 2 eyes (10%) developed angle closure at varied points in their postoperative course. The first case developed angle closure at the first month postoperatively due to development of iris bombe from 360-degree posterior synechiae. The other case initially had open angles with silicone oil droplets in the superior quadrant of the angles. However, in the third month postoperatively, there was a note of peripheral anterior synechiae formation closing the superior aspect of the temporal and nasal quadrants of the angles.
Change in cup:disc ratio
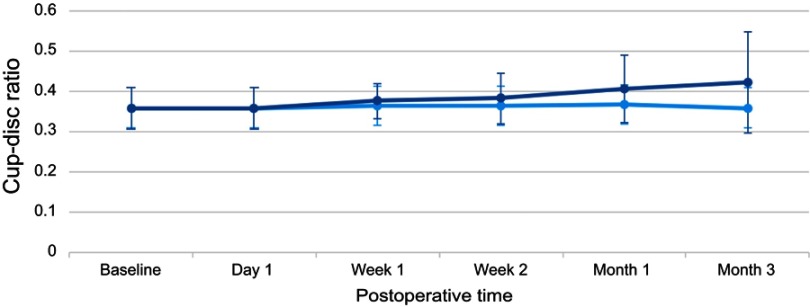
Among patients who did not have elevated IOP during the postoperative period, there is no significant change in cup:disc ratio at the end of the 3-month observation period (p=1). Among patients who did experience ocular hypertension, there is a statistically significant increase in mean cup:disc ratio from 0.36 preoperatively to 0.42 at the end of the 3-month observation period (p=0.047). The trend in cup:disc ratio is shown in Figure 3.
Figure 3.
Comparison of mean cup:disc ratio of cases with ocular hypertension (dark blue) and cases maintaining normal IOP (light blue) in the postoperative period.
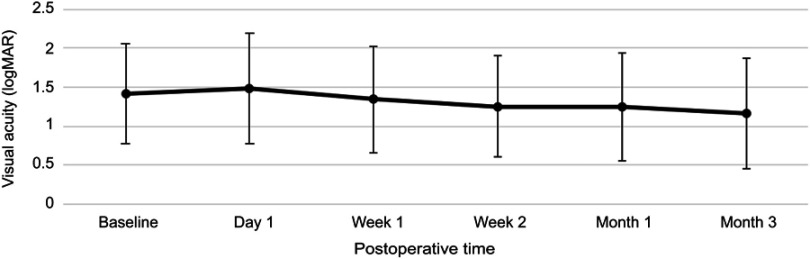
Visual acuity outcomes of patients
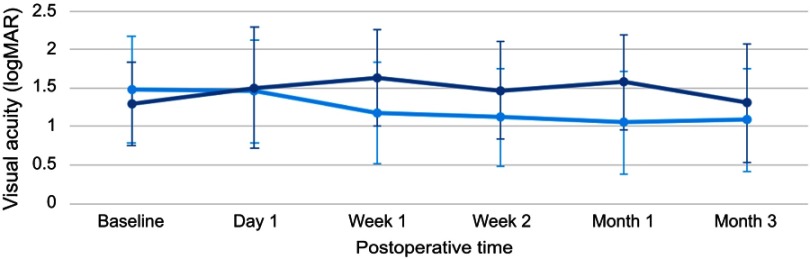
There is a trend for improvement in visual acuity following successful retinal reattachment surgery, as shown in Figure 4. There is a significant improvement in mean visual acuity from 1.41 logMAR units preoperatively to 1.16 logMAR units at the end of the 3-month observation period (p=0.02). A comparison of visual acuity between patients who had ocular hypertension during the postoperative period versus those who had normal IOP during this time showed that compared to baseline (Figure 5), significant improvement at 3 months postoperatively was achieved with those who had normal IOP during the postoperative period (p=0.002). In comparison, those who experienced ocular hypertension showed no significant improvement in visual acuity by 3 months (p=0.97). However, there is no statistically significant difference in the visual acuity by 3 months of those who had normal IOP versus those who had ocular hypertension (p=0.30).
Figure 4.
Mean visual acuity trend of cohort in the postoperative period.
Figure 5.
Comparison of mean visual acuity of cases with ocular hypertension (dark blue) and cases maintaining normal IOP (light blue) in the postoperative period.
Management of secondary glaucoma
All patients who experienced an elevation in IOP were initially started on a course of oral carbonic anhydrase inhibitors, specifically acetazolamide. Topical medications including beta-blockers, alpha agonists, and carbonic anhydrase inhibitors were started or added as needed to achieve further reduction in IOP. The choice of medical or surgical therapy given to each patient was decided by their attending physicians on the basis of severity and expected duration of IOP elevation.
Among the managed cases, 13 eyes (68%) were able to be weaned off topical and oral hypotensive medications by the third month postoperatively. A total of 2 eyes (11%) remained on topical medications at the end of the third postoperative month. The remaining number of eyes required additional management to achieve lower IOP. One eye (5%) required laser iridotomy using an Nd:YAG laser, another eye (5%) was managed with transscleral cyclophotocoagulation, and 2 eyes (11%) were managed by early removal of silicone oil. The time it took for IOP to return to the normal following intervention was varied, with most cases requiring 2 weeks to 1 month.
Discussion
Transient and sustained elevation of IOP is a relatively common occurrence following surgery to repair retinal detachment. The reported range of incidence of IOP elevation in the literature ranges from 4.8% to 44%, while modern literature reports a range of 11.6–12.9%.9–15 The calculated incidence obtained from the study is consistent with rates reported in other studies. Corollary to the previously mentioned findings, the study showed that the majority of patients who underwent vitreoretinal surgery did not experience any elevation in IOP in the postoperative period. However, the study did show that vitreoretinal surgery slightly increases IOP from baseline in the late postoperative period.
The elevation in IOP usually occurs in the first few weeks of vitreoretinal surgery, and most cases have an open angle mechanism.12 The finding shows that initial postoperative inflammation may be more contributory to the increases in IOP. Other possible mechanisms of open angle glaucoma include corticosteroid response, expansion of injected intraocular tamponade material without angle closure, and blood-mediated mechanisms.16–19 The initial increase in IOP is sustained initially up to the first postoperative month. However, postoperative inflammation eventually subsides resulting in decrease in IOP by the third postoperative month in most cases. While most cases of elevation in IOP occur within the first postoperative month, it may still occur at any point in the postoperative period.
Among the procedures done for retinal reattachment, scleral buckling with vitrectomy and silicone oil injection had a slightly higher incidence rate than vitrectomy with silicone oil injection alone. This is contrary to the reported incidence in literature where incidence of secondary glaucoma is with scleral buckling ranges from 1.4% to 4.4%, while that for vitrectomy has a wider range from 7.9% to 44.4%.18 The discrepancy in the reported incidence can be explained by noting that the cited studies in literature examined incidence after scleral buckling procedures alone, while this study examined incidence with scleral buckling combined with vitrectomy. This may also explain why the difference between the then determined incidence rate between the procedures was not statistically significant. The calculated incidence rates for scleral buckling combined with vitrectomy and silicone oil injection and for vitrectomy and silicone oil injection alone fall well within the reported range of incidence in literature.
In addition to the procedure of retinal surgery performed, studies have also shown that the choice of intraocular tamponade also affects IOP after surgery. Common choices for intraocular tamponade after retinal reattachment include silicone oil and intraocular expansile gases. Gas tamponade, which includes air, perfluoropropane (C3F8), and sulfur hexafluoride (SF6), tends to increase IOP in the postoperative period due to gas expansion in the acute postoperative period.16 The study showed that ocular hypertension occurs but is also transient one case which used 20% C3F8 tamponade. However, since there were only 2 cases in the cohort who used this form of tamponade, the results for that particular subgroup are not statistically meaningful. Lastly, the effect of different kinematic viscosities when using silicone oil may also affect IOP trends after surgery. However, studies have shown inconclusive results on whether using higher viscosity silicone oil results in increased incidence of ocular hypertension.19 Since all 50 eyes in the cohort who had silicone oil tamponade were injected with 1000 centistoke silicone oil, the effect of varying concentration and density of silicone oil on IOP trends is beyond the scope of this study.
Most cases of elevated IOP would undergo resolution leading to no significant difference between preoperative and late postoperative pressures.19–22 All cases were initially managed by giving oral and/or topical hypotensive medications, which resulted in most cases being able to be weaned off medications. Since most cases of ocular hypertension following retinal surgery are transient, a short course of oral hypotensive therapy was deemed appropriate for most of the cases. Cases with persistently elevated IOP would need additional management options depending on the mechanism of secondary glaucoma, with options including laser iridotomy, cyclophotocoagulation, early removal of silicone oil, and even considering filtering surgery. The variations with which the cases were managed, including the use of various medications and other modalities of treatment, reflect that there is no universally agreed-upon management when dealing with postoperative ocular hypertension. Each case is managed individually to address not only the onset, magnitude, and duration of increased pressure, but also its presumed underlying mechanism.
Conclusion
Transient and sustained elevation of IOP is a complication of surgery for repair of rhegmatogenous retinal detachment and can lead to secondary glaucoma. While most cases are transient and only require topical and oral medications, some cases may require additional interventions such as laser iridotomy, laser cyclophotocoagulation, and repeat surgery to achieve adequate control of IOP. Controlled IOP within the statistically normal range may be associated with a better improvement in terms of postoperative visual acuity in the acute postoperative period.
Acknowledgment
The authors would like to thank the Department of Ophthalmology and Visual Sciences of the Philippine General Hospital for their support in accomplishing this work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Budenz DL, Taba KE, Feur MS, et al. Surgical management of secondary glaucoma after pars plana vitrectomy and silicone oil injection for complex retinal detachment. Ophthalmology. 2001;108(9):1628–1632. doi: 10.1016/s0161-6420(01)00658-3 [DOI] [PubMed] [Google Scholar]
- 2.Chang S, Lincoff HA, Coleman D, et al. Perflourocarbon gases in vitreous surgery. Ophthalmology. 1985;92:651–656. doi: 10.1016/s0161-6420(85)33985-4 [DOI] [PubMed] [Google Scholar]
- 3.Aaberg TM, Van Horn DL. Late complications of pars plana vitreous surgery. Ophthalmology. 1978;85:126. doi: 10.1016/S0161-6420(78)35683-9 [DOI] [PubMed] [Google Scholar]
- 4.Anderson NG, Finemand MS, Brown GC. Incidence of intraocular pressure spike and other adverse events after vitreoretinal surgery. Ophthalmology. 2006;113:1. doi: 10.1016/j.ophtha.2006.04.029 [DOI] [PubMed] [Google Scholar]
- 5.De Corral LR, Cohen SB, Peyman GA. Effect of intravitreal silicone oil on intraocular pressure. Ophthalmic Surg. 1987;18:446–449. [PubMed] [Google Scholar]
- 6.Han DP, Lewis H, Lambrou FH Jr, et al. Mechanisms of intraocular pressure elevation after pars plana vitrectomy. Ophthalmology. 1989;96:1357. doi: 10.1016/S0161-6420(89)32715-1 [DOI] [PubMed] [Google Scholar]
- 7.Hayreh SS, Baines JAB. Occlusion of the vortex veins: an experimental study. Br J Ophthalmol. 1973;57:17–23. doi: 10.1136/bjo.57.4.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henderer JD, Budenz DL, Flynn HW, et al. Elevated intraocular pressure and hypotony following silicone oil retinal tamponade for complex retinal detachment: incidence and risk factors. Arch Ophthalmol. 1999;117:189–195. doi: 10.1001/archopht.117.2.189 [DOI] [PubMed] [Google Scholar]
- 9.Honavar SG, Goyal M, Majji AB, et al. Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999;10:169–176. doi: 10.1016/S0161-6420(99)90017-9 [DOI] [PubMed] [Google Scholar]
- 10.Faulborn J, Conway BP, Machemer R. Surgical complications of pars plana vitreous surgery. Ophthalmology. 1978;85:116. doi: 10.1016/S0161-6420(78)35684-0 [DOI] [PubMed] [Google Scholar]
- 11.Ghartey KN, Teolentine FI, Freeman HM, et al. Close vitreous surgery. XVII. Results and complications of pars plana vitrectomy. Arch Ophthalmol. 1980;98:1248. doi: 10.1001/archopht.1980.01020040495022 [DOI] [PubMed] [Google Scholar]
- 12.The Silicone Study Group. Vitrectomy with silicone oil or sulfur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 1. Arch Ophthalmol. 1992;110:770–779. doi: 10.1001/archopht.1992.01080180042027 [DOI] [PubMed] [Google Scholar]
- 13.The Silicone Study Group. Vitrectomy with silicone oil or perflouropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 2. Arch Ophthalmol. 1992;110:780–792. doi: 10.1001/archopht.1992.01080180052028 [DOI] [PubMed] [Google Scholar]
- 14.Koreen L, Yoshida N, Escariao P, et al. Incidence of, risk factors for, and combined mechanism of late-onset open angle glaucoma after vitrectomy. Retina. 2012;1:160–167. doi: 10.1097/IAE.0b013e318217fffb [DOI] [PubMed] [Google Scholar]
- 15.Kornmann H. Glaucoma management after vitreoretinal surgeries. Curr Opin Ophthalmol. 2016;03:125–131. doi: 10.1097/ICU.0000000000000238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tranos P, Bhar G, Little B. Postoperative intraocular pressure spikes: the need to treat. Eye. 2004;18(7):673–679. doi: 10.1038/sj.eye.6701319 [DOI] [PubMed] [Google Scholar]
- 17.Lalezary M, Kim SJ, Jiramongkolchai K, et al. Long-term trends in intraocular pressure after pars plana vitrectomy. Retina. 2011;31(4):679–685. doi: 10.1097/IAE.0b013e3181ff0d5a [DOI] [PubMed] [Google Scholar]
- 18.Mangouritsas G, Mourtzoukos S, Portaliou D, et al. Glaucoma associated with management of rhegmatogenous retinal detachment. Clin Ophthalmol. 2013;7:727–734. doi: 10.2147/OPTH.S42792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moisseiev J, Barak A, Manaim T, et al. Removal of silicone oil in the management of glaucoma in eyes with emulsified silicone. Retina. 1993;13:290–295. [DOI] [PubMed] [Google Scholar]
- 20.Sidoti PA, Minckler DS, Baerveldt G, et al. Aqueous tube shunt to a pre-existing episcleral encircling element in the treatment of complicated glaucomas. Ophthalmology. 1994;101:1036–1043. doi: 10.1016/s0161-6420(94)31221-8 [DOI] [PubMed] [Google Scholar]
- 21.Tsai JC, Lee MB, Wu Dunn D, et al. Incidence of acute intraocular pressure elevation after panretinal photocoagulation. J Glaucoma. 1995;4(1):45–48. [PubMed] [Google Scholar]
- 22.Wong D, Kumar I, Quah SA, et al. Comparison of postoperative intraocular pressure in patients with Densiron 68 vs conventional silicone oil: a case control study. Eye. 2009;23:1. [DOI] [PubMed] [Google Scholar]