Abstract
Background:
HIV, hepatitis C virus (HCV), and alcohol-related diagnoses (ARD) independently contribute increased risk for all-cause hospitalization. We sought to determine annual medical intensive care unit (MICU) admission rates and relative risk of MICU admission between 1997 and 2014 among people with and without HIV, HCV, and ARD, using data from the largest HIV and HCV care provider in the United States.
Setting:
Veterans Health Administration.
Methods:
Annual MICU admission rates were calculated among 155,550 patients in the Veterans Aging Cohort Study by HIV, HCV, and ARD status. Adjusted rate ratios (RR) and 95% confidence intervals (CI) were estimated with Poisson regression. Significance of trends in age-adjusted admission rates were tested with generalized linear regression. Models were stratified by calendar period to identify shifts in MICU admission risk over time.
Results:
Compared to HIV−/HCV−/ARD− patients, relative risk for MICU admission decreased among HIV mono-infected patients from 61% (95% CI 1.56–1.65) in 1997–2009 to 21% (95% CI 1.16–1.27) in 2010–2014, increased among HCV mono-infected patients from 22% (95% CI 1.16–1.29) in 1997–2009 to 54% (95% CI 1.43–1.67) in 2010–2014, and remained consistent among patients with ARD only at 46% (95% CI 1.42–1.50). MICU admission rates decreased by 48% among HCV-uninfected patients (p-trend<0.0001) but did not change among HCV+ patients (p-trend=0.34).
Conclusion:
HCV infection and ARD remain key contributors to MICU admission risk. The impact of each of these conditions could be mitigated with combination of treatment of HIV, HCV, and interventions targeting unhealthy alcohol use.
Keywords: Intensive care units, HIV, Hepatitis C, Alcoholism, Electronic health records, Veterans
Introduction
People with HIV infection are living longer on combination antiretroviral therapy (ART), but continue to experience excess risk for multiple chronic conditions compared to demographically similar HIV-uninfected individuals, including pulmonary,1 cardiovascular,2 and liver disease.3 Further, these chronic medical conditions associated with aging are major contributors to risk of all-cause hospitalization4 and mortality5 and may progress more rapidly in HIV-infected (HIV+) patients. Since ART became widely available, hospitalization rates among HIV+ patients have decreased4 while rates of medical intensive care unit (MICU) admissions have remained stable or even increased.6
A growing percentage of MICU admissions among HIV+ patients are due to complications arising from hepatitis C virus (HCV) co-infection.7 HCV infection is more common in patients with HIV than their HIV-uninfected counterparts.8 Compared with HIV mono-infected patients, HCV co-infection is associated with approximately 50% increased risk of hospitalization, most often attributed to infection-related diagnoses.9 Although safe and effective treatments for HCV infection became widely available in the United States in 201410, the risk of MICU admission conferred by HCV infection before 2014 remains largely unknown.
While effective treatments for HIV and HCV infection have led to improved health outcomes, common and potentially modifiable health behaviors, such as alcohol consumption, represent the next challenge.11 A previous study showed that one-third of MICU admissions were associated with heavy alcohol consumption.12 Alcohol-related diagnoses (ARD), including alcohol use disorder and other conditions caused by alcohol (e.g., alcoholic liver disease, alcoholic gastritis), are commonly associated with conditions that lead to MICU admission among HCV+ patients.13 ARD are also common among HIV+ patients14, and sequalae such as physiologic injury15 and mortality16 occur at lower levels of alcohol exposure than among uninfected patients. Importantly, even low levels of alcohol use can aggravate deleterious effects of HIV and HCV infection on the liver.17
As HIV has become a chronic medical condition, the growing relevance of HCV infection and ARD on MICU admission requires quantification as a first step toward identifying new targets for medical intervention. We used data from an observational cohort in the Veterans Health Administration (VA), the largest HIV and HCV care provider in the United States, and Medicare, the largest healthcare insurer in the United States, to calculate annual MICU admission rates and relative risk for MICU admission between 1997 and 2014 among people living with and without HIV, HCV, and ARD.
Methods
Study design and cohort
We conducted a retrospective cohort study among patients in the Veterans Aging Cohort Study (VACS), which has been previously described.18 Briefly, VACS is a large observational cohort based on data from the national VA electronic health record system that includes all HIV+ patients in VA care (over 50,000 subjects) matched 1:2 with HIV-uninfected patients based on age, sex, race/ethnicity, and site of care. For this analysis, we calculated annual MICU admission rates among all VACS patients who were active in VA care (i.e., had at least one outpatient or inpatient visit) in each calendar year between 1997 and 2014. Baseline date was defined as the date of VACS enrollment, which is the first HIV diagnosis date within the VA for HIV+ patients or date of matching for HIV-uninfected controls. Patients were followed until their last VA visit date or death. HIV-uninfected controls (n=338) who seroconverted during follow-up were excluded. The development of VACS has been approved by the Institutional Review Boards of the VA Connecticut Healthcare System and Yale University School of Medicine, was granted a waiver of informed consent, and deemed HIPAA compliant.
MICU admission and principal diagnoses
MICU admission data were extracted from national VA and Medicare databases. VA MICU admission was identified by inpatient bed section codes 12 or 13. Bed section code 12 included cardiac ICU (CICU) admissions until 2008 when CICU was given a separate bed section code, 13. For the purposes of this analysis, MICU refers to both MICU and CICU admissions. Medicare MICU admissions were identified from MEDPAR data using MICU and CICU indicator variables. Admissions that resulted from a transfer from another unit were included in this analysis. For each MICU admission we obtained principal diagnosis for the hospitalization, according to International Classification of Diseases, Ninth Revision (ICD-9) code and categorized them as in previous studies4,7 (see Table, Supplemental Digital Content 1).
Exposure groups
Eight exposure groups were created using all combinations of HIV, HCV, and ARD status. HIV status was determined as previously described in VACS.18 HCV infection was defined by positive HCV RNA during the study period. Time-updated ARD included validated ICD-9 codes for alcohol intoxication/ingestion, alcohol-induced mental disorders, alcohol dependence syndrome, alcoholic polyneuropathy/cardiomyopathy/gastritis, and alcohol-related liver diseases (see Table, Supplemental Digital Content 1).19 Patients were classified as ARD+ if in the previous year they had at least two outpatient encounters with an ARD; they remained ARD+ thereafter.
Covariates
We extracted data on demographics including age, sex, and race/ethnicity. Age was categorized into 5-year age groups ensuring adequate numbers in each age and exposure group category when calculating age-adjusted, annual MICU admission rates. Common comorbid conditions were extracted using ICD-9 codes for psychiatric disorders, hypertension, drug use-related diagnoses, anemia, cardiovascular disease (CVD), diabetes, chronic obstructive pulmonary disorder (COPD), renal insufficiency, non-AIDS cancers, chronic hepatitis B infection, and liver diseases. Comorbidities were defined by one inpatient or two outpatient diagnostic codes (see Table, Supplemental Digital Content 1) and considered present at baseline if the diagnosis date occurred within one year before or six months after baseline date. We also extracted laboratory data, including CD4 cell count and FIB-4 (a composite measure of liver injury incorporating values for age, platelet count, AST, and ALT), and among HIV+ patients, pharmacy data to identify ART initiation.
Statistical analyses
We compared baseline demographic and clinical characteristics across the eight exposure groups using non-parametric Kruskal-Wallis tests for continuous measures and chi-square (χ2) tests for categorical measures. We calculated annual MICU admission rates by dividing the total number of MICU admissions by the number of patients at risk in a given calendar year (i.e., having at least one inpatient or outpatient visit). Patients with multiple MICU admissions could only contribute one admission per calendar year of follow-up. We estimated age-adjusted MICU admission rates, as well as rate ratios (RR) with 95% confidence intervals (95% CI) for each HIV/ARD/HCV exposure group adjusted for baseline age, comorbidity (i.e., psychiatric disorders, hypertension, drug use-related diagnoses, diabetes, cardiovascular disease, anemia, chronic obstructive pulmonary disorder, non-AIDS cancers, renal insufficiency, chronic hepatitis B, and liver diseases), and calendar year using Poisson regression. Covariates were selected based on a priori hypotheses informed by clinical relevance and because they represent potential confounders in the relationship between HIV, HCV, or ARD and risk of MICU admission, as well as availability of data. We tested for trends in annual MICU admission rates using generalized linear regression models. We estimated the individual and combined associations of HIV, HCV, and ARD with risk of MICU admission in three ways: 1) comparing HIV/HCV/ARD groups to the HIV−/HCV−/ARD− group, 2) comparing HIV/ARD groups stratified by HCV infection, and 3) comparing HCV/ARD groups stratified by HIV infection. We also stratified the study period into two eras to assess differential impacts of each exposure between 1997–2009 and 2010–2014. We selected these specific time periods to highlight findings from the most recent five years of follow-up that would be most relevant to current patients. Statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was defined as p<0.05.
Results
Cohort characteristics
Between 1997 and 2014, 155,550 patients met study inclusion criteria (contributing 1,525,267 person-years); 32% were HIV+, 13% were HCV+, and 30% had an ARD during follow-up. Median baseline age was 47 years (interquartile range [IQR] 40–54 years) (Table 1). Most patients were male (97%), 47% were black, and 40% were white. While 42% of the sample had no baseline comorbidity, 29% had only one and the remaining 28% had two or more. The most common comorbidities at baseline were psychiatric disorders (27%), hypertension (27%), drug use-related diagnoses (14%), diabetes (12%), and CVD (6%).
Table 1.
Demographic and clinical characteristics among patients receiving care in the Veterans Aging Cohort Study between 1997 and 2014, n=155,550
| Characteristic | n (%) |
|---|---|
| Exposure group | |
| HIV+ / ARD+ / HCV+ | 5144 (3.3) |
| HIV+ / ARD+ / HCV− | 9359 (6.0) |
| HIV+ / ARD− / HCV+ | 4743 (3.1) |
| HIV+ / ARD− / HCV− | 30534 (19.6) |
| HIV− / ARD+ / HCV+ | 6682 (4.3) |
| HIV− / ARD+ / HCV− | 25924 (16.7) |
| HIV− / ARD− / HCV+ | 3653 (2.4) |
| HIV− / ARD− / HCV− | 69511 (44.7) |
| Age at baseline, median (IQR) | 47 (40–54) |
| Male sex | 151,379 (97.3) |
| Race/ethnicity | |
| Black | 73,221 (47.1) |
| White | 62,084 (39.9) |
| Hispanic | 12,761 (8.2) |
| Other or unknown | 7,484 (4.8) |
| Year of VACS enrollment | |
| 1997–2001 | 82,144 (52.8) |
| 2002–2006 | 33,134 (21.3) |
| 2007–2010 | 20,659 (13.3) |
| 2011–2014 | 19,613 (12.6) |
| Comorbidities at baseline | |
| Psychiatric disorders | 41,614 (26.8) |
| Hypertension | 41,253 (26.5) |
| Drug use-related diagnoses | 21,415 (13.8) |
| Diabetes | 18,106 (11.6) |
| CVD | 9,570 (6.2) |
| Anemia | 8,369 (5.4) |
| COPD | 7,043 (4.5) |
| Non-AIDS cancers | 5,340 (3.4) |
| Renal insufficiency | 3,764 (2.4) |
| Chronic hepatitis B | 1,868 (1.2) |
| Liver diseases | 1,560 (1.0) |
| Mortality per 100 person-years | 2.6 |
| Ever MICU admission | 29,887 (19.2) |
Abbreviations: HIV - human immunodeficiency virus; VACS - Veterans Aging Cohort Study; HCV - hepatitis C virus; ARD - alcohol-related diagnosis; IQR - interquartile range; MICU - medical intensive care unit
Note: ARD status was used as an ever/never measure in this table
Each of the eight exposure groups based on HIV, HCV, and ARD had ≥3,500 patients, the largest being the group with none of the exposures (n=69,511). ARDs were more common in HCV+ patients (58%) and HIV+ patients (30%) than patients with neither HCV nor HIV (27%) (p<0.0001). Overall mortality was 2.9 deaths per 100 person-years of observation. Patients with HIV infection (irrespective of HCV infection and ARD status) had higher mortality rates than those without HIV infection (4.3 per 100 person-years vs. 1.9 per 100 person-years, p<0.0001) (see Table, Supplemental Digital Content 2).
Among HIV+ patients, 57% initiated ART within one year of VACS enrollment (i.e., diagnosis of HIV within the VA), and an additional 21% had initiated ART during the study period. In 1997, 35% of HIV+ patients had CD4 <200 cells/mm3 and 20% had CD4 ≥500 cells/mm3. At the end of the study period, only 8% of HIV+ patients had CD4 <200 cells/mm3 and 58% had CD4 ≥500 cells/mm3. Among HCV+ patients, FIB-4 scores increased over the study period. At study start, 36% had FIB-4 scores between 1.45–3.25 and 16% had scores >3.25. By 2014, 51% had FIB-4 scores between 1.45–3.25 and 24% had scores >3.25. The majority (69%) of HCV-uninfected patients had FIB-4 scores <1.45 at study start and this remained stable over the entire study period.
MICU admissions
During follow-up, 29,887 (19%) patients were admitted to a MICU for a total of 56,805 admissions; 61% had one admission, 33% had between two and four admissions, and 6% had five or more admissions. HCV+ patients experienced proportionately more MICU admissions than their HCV-uninfected counterparts in every HIV/ARD strata (42% of HCV+ had >1 admission vs. 38% of HCV-uninfected, p<0.0001) (see Table, Supplemental Digital Content 3). The majority (63%) of MICU admissions occurred within the VA while the remaining 37% were found in Medicare data (Table 2). The most common principal diagnoses for hospital stays with a MICU admission were CVD (28%), respiratory (14%), GI and liver (8%), neurologic (8%), severe sepsis or septic shock (6%), and other infections (6%).
Table 2.
Characteristics of medical intensive care unit (MICU) admissions, n=56,805
| Characteristic | n (%) |
|---|---|
| Location | |
| VA | 35,883 (63.2) |
| Medicare | 20,922 (36.8) |
| LOS per admission in days, median (IQR) | 6 (3–11) |
| Primary admission diagnosis | |
| CVD | 16,151 (28.4) |
| Respiratory | 7,682 (13.5) |
| GI and liver | 4,770 (8.4) |
| Neurologic | 4,374 (7.7) |
| Other infections | 3,611 (6.4) |
| Severe sepsis/septic shock | 3,469 (6.1) |
| Endocrine | 3,248 (5.7) |
| HIV/AIDS | 2,671 (4.7) |
| Renal insufficiency | 2,224 (3.9) |
| Non-AIDS cancers | 1,241 (2.2) |
| ARD | 950 (1.7) |
| Psychiatric disorders | 771 (1.4) |
| Drug use-related diagnoses | 344 (0.6) |
| Other | 5,299 (9.3) |
Abbreviations: IQR - interquartile range; HIV - human immunodeficiency virus; HCV - hepatitis C virus; ARD - alcohol-related diagnosis; MICU - medical intensive care unit; VA - Veterans Affairs; LOS - length of stay; CVD - cardiovascular disease; AIDS - acquired immune deficiency syndrome
More HIV+/HCV+/ARD+ patients experienced MICU admission than HIV−/HCV−/ARD− patients (34% vs. 15%, p<0.0001) (see Table, Supplemental Digital Content 3). All HCV+ (irrespective of HIV infection and ARD status) were more likely than HCV-uninfected to have principal diagnoses related to GI and liver diseases, severe sepsis/septic shock, other infections, endocrine disorders, renal insufficiency, and alcohol- and drug use-related diagnoses (all p<0.0001).
Trends in MICU admission rates
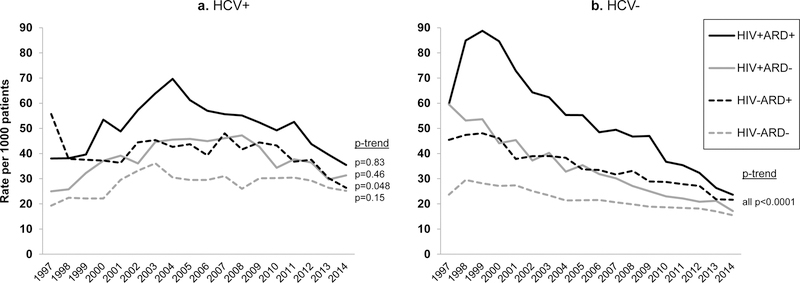
Overall, annual MICU admission rates decreased by 37% from 37.5 admissions per 1000 patients (37.5/1000) in 1997 to 23.7/1000 in 2014 (t-trend=−4.8, p<0.0001). The largest decrease was seen among HCV-uninfected patients, irrespective of HIV infection or ARD (Figure 1 with MICU admission rates decreasing by 48% over the study period from 34.0/1000 in 1997 to 17.6/1000 in 2014 (t-trend=−17.2, p<0.0001). Among HCV+ patients there was no evidence of change in MICU admission rates from 1997 to 2014 (t-trend=+1.0, p=0.34).
Figure 1.
Age-adjusted medical intensive care unit admission rates per 1000 at-risk patients enrolled in the Veterans Aging Cohort Study between 1997 and 2014, by HIV, hepatitis C virus (HCV), and time-updated alcohol-related diagnosis (ARD) Note (below figure): Patients were classified as ARD+ if in the previous year they had at least two outpatient encounters with an ARD; they remained ARD+ thereafter.
Relative risk for MICU admission
There was minimal evidence of confounding by the adjusting covariates in each exposure group, with relative differences between crude and adjusted RR ranging from 4% to 13% (Table 3). After adjusting for baseline age, baseline comorbidity, and calendar year, HIV infection and ARD were each associated with 46% increased risk of MICU admission compared to HIV−/HCV−/ARD− patients (RR 1.46, 95% CI 1.43–1.50 HIV infection; RR 1.46, 95% CI 1.42–1.50 ARD) (Table 3). HCV infection alone was associated with 33% greater risk compared to HIV−/HCV−/ARD− patients (RR 1.33, 95% CI 1.27–1.39). Models stratified by calendar period showed that HIV infection was more strongly associated with risk of MICU admission between 1997–2009 (RR 1.61, 95% CI 1.56–1.65) than between 2010–2014 (RR 1.21, 95% CI 1.16–1.27). Conversely, HCV infection was more strongly associated with MICU admission in later years (RR 1.22, 95% CI 1.16–1.29 between 1997–2009; RR 1.54, 95% CI 1.43–1.67 between 2010–2014). The association of ARD was similar in both time periods (RR 1.46, 95% CI 1.41–1.50 between 1997–2009; RR 1.44, 95% CI 1.38–1.50 between 2010–2014).
Table 3.
Risk of medical intensive care unit (MICU) admission by HIV, hepatitis C virus (HCV), alcohol-related diagnosis (ARD), and calendar era, n=155,550
| All groups | ||||||
|---|---|---|---|---|---|---|
| Crude | Adjusted | Adjusted | Adjusted | |||
| Exposure group | 1997–2014 | 1997–2014 | 1997–2009 | 2010–2014 | ||
| HIV+ | ARD+ | HCV+ | 2.26 (1.17–2.34) | 2.36 (2.26–2.46) | 2.29 (2.17–2.42) | 2.40 (2.23–2.58) |
| HCV− | 1.89 (1.83–1.95) | 2.14 (2.06–2.22) | 2.34 (2.24–2.44) | 1.75 (1.64–1.86) | ||
| ARD− | HCV+ | 1.64 (1.58–1.71) | 1.74 (1.67–1.81) | 1.66 (1.58–1.75) | 1.94 (1.80–2.09) | |
| HCV− | 1.38 (1.35–1.41) | 1.46 (1.43–1.50) | 1.61 (1.56–1.65) | 1.21 (1.16–1.27) | ||
| HIV− | ARD+ | HCV+ | 1.72 (1.66–1.79) | 1.80 (1.73–1.88) | 1.69 (1.60–1.78) | 1.91 (1.78–2.04) |
| HCV− | 1.37 (1.33–1.40) | 1.46 (1.42–1.50) | 1.46 (1.41–1.50) | 1.44 (1.38–1.50) | ||
| ARD− | HCV+ | 1.25 (1.20–1.31) | 1.33 (1.27–1.39) | 1.22 (1.16–1.29) | 1.54 (1.43–1.67) | |
| HCV− | ref | ref | ref | ref | ||
| By HIV | ||||||
| HIV+ | HCV+/ARD+ | 1.64 (1.57–1.70) | 1.62 (1.55–1.70) | 1.45 (1.37–1.53) | 1.98 (1.83–2.14) | |
| HCV+/ARD− | 1.19 (1.14–1.24) | 1.19 (1.14–1.24) | 1.04 (0.99–1.09) | 1.60 (1.48–1.73) | ||
| HCV−/ARD+ | 1.37 (1.32–1.42) | 1.33 (1.28–1.38) | 1.33 (1.28–1.39) | 1.29 (1.21–1.38) | ||
| HCV−/ARD− | ref | ref | ref | ref | ||
| HIV− | HCV+/ARD+ | 1.72 (1.66–1.79) | 1.76 (1.69–1.84) | 1.65 (1.56–1.74) | 1.88 (1.75–2.02) | |
| HCV+/ARD− | 1.25 (1.20–1.31) | 1.29 (1.23–1.35) | 1.19 (1.12–1.26) | 1.52 (1.41–1.65) | ||
| HCV−/ARD+ | 1.37 (1.33–1.41) | 1.47 (1.42–1.52) | 1.49 (1.43–1.55) | 1.36 (1.29–1.44) | ||
| HCV−/ARD− | ref | ref | ref | ref | ||
| By HCV | ||||||
| HCV+ | HIV+/ARD+ | 1.80 (1.69–1.92) | 1.78 (1.66–1.90) | 1.88 (1.73–2.04) | 1.55 (1.39–1.74) | |
| HIV+/ARD− | 1.31 (1.26–1.37) | 1.31 (1.25–1.37) | 1.36 (1.29–1.43) | 1.26 (1.17–1.35) | ||
| HIV−/ARD+ | 1.37 (1.32–1.43) | 1.36 (1.30–1.42) | 1.38 (1.31–1.46) | 1.24 (1.14–1.34) | ||
| HIV−/ARD− | ref | ref | ref | ref | ||
| HCV− | HIV+/ARD+ | 1.89 (1.83–1.95) | 2.14 (2.06–2.22) | 2.34 (2.24–2.44) | 1.75 (1.64–1.86) | |
| HIV+/ARD− | 1.38 (1.35–1.41) | 1.46 (1.43–1.50) | 1.60 (1.56–1.65) | 1.21 (1.16–1.27) | ||
| HIV−/ARD+ | 1.37 (1.33–1.40) | 1.46 (1.42–1.50) | 1.46 (1.41–1.50) | 1.44 (1.38–1.50) | ||
| HIV−/ARD− | ref | ref | ref | ref | ||
Notes: reported as RR (95% confidence intervals); models adjusted for baseline age, comorbidity (psychiatric disorders, hypertension, drug use-related diagnoses, diabetes, cardiovascular disease, anemia, chronic obstructive pulmonary disorder, non-AIDS cancers, renal insufficiency, chronic hepatitis B, and liver diseases), and calendar year
Abbreviations: HIV - human immunodeficiency virus; RR - rate ratio; CI - confidence interval; ref - referent group
We found that the effect of ARD differed depending on the presence of other exposures. For example, ARD was associated with 33% (95% CI 1.28–1.38) increased risk of MICU admission among HIV+ patients and 47% (95% CI 1.42–1.52) increased risk among HIV-uninfected patients (Table 3). Similar differential effects of ARD were observed between HCV+ and HCV-uninfected patients. Compared to patients with none of the exposures, those with all three had the highest risk of MICU admission (RR 2.36, 95% CI 2.26–2.46).
Discussion
Using a national cohort of 155,550 patients and combined data from the largest healthcare provider and insurer in the United States, we showed that HIV, HCV, and ARD were each independently associated with increased risk of MICU admission between 1997 and 2014. Compared to earlier years, risk of MICU admission in the last five years of follow-up decreased among HIV mono-infected patients but increased among HCV mono-infected patients. These findings illustrate that viral infections are associated with serious health conditions requiring MICU admission, but this association may be attenuated by effective treatments as demonstrated in HIV+ patients. Compared to HIV−/HCV−/ARD− patients, the contribution of ARD to the risk of MICU admission remained consistent over the study period. Importantly, ARD accounts for 3.3 million deaths (5.9% of all deaths) each year worldwide11 and continues to be associated with substantial MICU admission risk, signifying the urgency to address this potentially modifiable health behavior.
MICU admission rates decreased by 37% between 1997 and 2014. This differs from other national data that indicate increased MICU bed count and utilization over the past 15 years in the United States.20 Decreasing MICU use in our study may be explained by several factors, including the fixed number of acute care VA facilities, changes to criteria for MICU admission, utilization of MICU resources, or expansion of step-down units. However, we included admissions reimbursed by Medicare, which would be expected to partially offset this effect. In addition, MICU admission rates in our study were substantially higher compared with prior studies of non-surgical ICU admission among the general VA patient population. Approximately 20% of participants in our cohort had at least one MICU admission during the observation period compared with 8% in a cross-sectional study between 2009–2010.21 This may be partially explained by differing study designs, including more HIV+ patients in the VACS cohort, who have higher MICU admission rates.
MICU admission rates fell dramatically between 1997 and 2014 among patients without HCV infection, but were unchanged among patients with HCV infection, suggesting that HCV infection or associated risk factors played a role in MICU use during the study period. Without treatment, the adverse impact of HCV infection on MICU admissions could increase given the prevalence of HCV globally, estimated in 2015 at 1.0% of the general population (71.1 million infections),22 and the lag time between infection and development of HCV-related complications.23 We anticipate that the influence of HCV on MICU admission rates may change after 2014 when modern direct-acting antivirals (DAA) for treatment of HCV infection became available to VA patients. These therapies are effective in achieving sustained virologic response,10 but whether this translates to improved clinical outcomes of conditions that commonly require MICU admission, such as sequelae of hepatic decompensation, remains to be seen. The importance of optimally deploying HCV treatments is highlighted by our study’s findings of the substantial impact of HCV infection on MICU admission through 2014. Future research should investigate the impact of DAA treatment on MICU admission rates among HCV+ patients with and without HIV co-infection.
Our findings also highlight the importance of unhealthy alcohol use, a potentially modifiable health behavior, on MICU admission risk in patient populations with or without underlying HIV or HCV infection. In prior work, we showed that ARD are independently associated with all-cause hospitalization.4 Our current findings further underscore that patients with ARD also experience serious, potentially life-threatening complications that lead to MICU admission. Although the mechanism through which ARD influences MICU admission risk remains unclear, immune and neurocognitive impairments may play a role. In one study, alcohol dependence was independently associated with sepsis, septic shock, and hospital mortality among adult MICU patients.24 However, other studies suggest that MICU patients with ARD had similar25 or even lower mortality compared to those without ARD.26 Failure to detect harmful effects of ARD in MICU patients must be viewed with caution as these studies were limited by unbalanced comparator groups, with ARD groups being younger and with fewer comorbidities. It is critical to better understand the impact of ARD on important health outcomes such as MICU admission and determine how decreasing or eliminating alcohol use may offset these risks. We postulate that development and subsequent implementation of effective interventions targeting unhealthy alcohol use could reduce MICU admission risk for broad populations of patients and decrease the morbidity and mortality of patients with ARD admitted to the MICU.
Our study had limitations. First, our findings may reflect bias from admitting clinicians who have a lower threshold for admitting HCV+ patients to the MICU than other patient groups. Some HCV+ patients are at greater risk for infection and may have more significant derangements in biomarkers of infection such as lactate, a benchmark target for monitoring sepsis. Second, our analysis relied on ICD-9 codes for ARD to define alcohol exposure, which have low sensitivity for capturing true ARD status and therefore inflated MICU admission rates among those we classified as ARD-. Finally, nearly all individuals in VACS are men, which resembles the HIV population in many countries, but limits the ability to generalize our findings to other HIV cohorts with higher proportions of women.
In summary, while MICU admission rates in this large, national cohort fell dramatically between 1997 and 2014 among patients without HCV, there was essentially no change in MICU admission rates among patients with HCV infection. While the additional risk of MICU admission conferred by HIV mono-infection decreased over time, both HCV infection and ARD remained major risk factors for MICU admission between 2010 and 2014. The impact of these conditions could substantially change with the combination of safe and effective treatment for HIV and HCV infections, and interventions targeting unhealthy alcohol use.
Supplementary Material
Acknowledgements
Support for VA/CMS data is provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, and VA Information Resource Center (SDR 02–237 and 98–004). This work was supported by the US National Institutes of Health (NIH), including grants from the National Institute on Alcohol Abuse and Alcoholism [U24-AA020794, U01-AA020790, U10 AA013566-completed to ACJ] and National Heart, Lung, and Blood Institute [R01 HL090342 to KC, K24 HL087713 to LH]. The views expressed in this manuscript represent those of the authors and do not necessarily represent those of the Department of Veterans Affairs.
Source of Funding:
This work was supported by the US National Institutes of Health (NIH), including grants from the National Institute on Alcohol Abuse and Alcoholism [U24-AA020794, U01-AA020790, U10-AA013566-completed to ACJ] and National Heart, Lung, and Blood Institute [R01-HL090342 to KC, K24-HL087713 to LH].
Footnotes
Preliminary stages of this research were presented as poster presentations at:
1. International Workshop on HIV Observational Databases, Lisbon, Portugal, March 30-April 1, 2017
2. American Thoracic Society International Conference, Washington, DC, May 19–24, 2017
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Crothers K, Huang L, Goulet JL, et al. HIV infection and risk for incident pulmonary diseases in the combination antiretroviral therapy era. Am J Respir Crit Care Med 2011;183(3):388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freiberg MS, Chang CH, Skanderson M, et al. Association Between HIV Infection and the Risk of Heart Failure With Reduced Ejection Fraction and Preserved Ejection Fraction in the Antiretroviral Therapy Era: Results From the Veterans Aging Cohort Study. JAMA Cardiol 2017;2(5):536–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crum-Cianflone NF, Grandits G, Echols S, Ganesan A, Landrum M, Weintrob A. Trends and Causes of Hospitalizations Among HIV-Infected Persons During the Late HAART Era: What Is the Impact of CD4 Counts and HAART Use? J Acquir Immune Defic Syndr 2010;54:248–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rentsch C, Tate JP, Akgun KM, et al. Alcohol-Related Diagnoses and All-Cause Hospitalization Among HIV-Infected and Uninfected Patients: A Longitudinal Analysis of United States Veterans from 1997 to 2011. AIDS and Behav 2016;20(3):555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palella FJJ, Baker RK, Moorman AC, et al. Mortality in the Highly Active Antiretroviral Therapy Era: Changing Causes of Death and Disease in the HIV Outpatient Study. J Acquir Immune Defic Syndr 2006;43:27–34. [DOI] [PubMed] [Google Scholar]
- 6.Akgun KM, Pisani M, Crothers K. The changing epidemiology of HIV-infected patients in the intensive care unit. J Intensive Care Med 2011;26(3):151–164. [DOI] [PubMed] [Google Scholar]
- 7.Akgun KM, Tate JP, Pisani M, et al. Medical ICU admission diagnoses and outcomes in human immunodeficiency virus-infected and virus-uninfected veterans in the combination antiretroviral era. Crit Care Med 2013;41(6):1458–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Platt L, Easterbrook P, Gower E, et al. Prevalence and burden of HCV co-infection in people living with HIV: a global systematic review and meta-analysis. Lancet Infect Dis 2016;16(7):797–808. [DOI] [PubMed] [Google Scholar]
- 9.Crowell TA, Gebo KA, Balagopal A, et al. Impact of hepatitis coinfection on hospitalization rates and causes in a multicenter cohort of persons living with HIV. J Acquir Immune Defic Syndr 2014;65(4):429–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jakobsen JC, Nielsen EE, Feinberg J, et al. Direct-acting antivirals for chronic hepatitis C. Cochrane Database Syst Rev 2017;6:CD012143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Global status report on alcohol and health 2014.
- 12.Gacouin A, Tadie JM, Uhel F, et al. At-risk drinking is independently associated with ICU and one-year mortality in critically ill nontrauma patients. Crit Care Med 2014;42(4):860–867. [DOI] [PubMed] [Google Scholar]
- 13.Mankal PK, Abed J, Aristy JD, et al. Relative effects of heavy alcohol use and hepatitis C in decompensated chronic liver disease in a hospital inpatient population. Am J Drug Alcohol Abuse 2015;41(2):177–182. [DOI] [PubMed] [Google Scholar]
- 14.Akgun KM, Gordon K, Pisani M, et al. Risk factors for hospitalization and medical intensive care unit (MICU) admission among HIV infected Veterans. J Acquir Immune Defic Syndr 2013;62(1):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Justice AC, McGinnis KA, Tate JP, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend 2016;161:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall BDL, Tate JP, McGinnis KA, et al. Long-term alcohol use patterns and HIV disease severity. AIDS 2017;31(9):1313–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lo Re V III, Kallan MJ, Tate JP, et al. Hepatic Decompensation in Antiretroviral-Treated Patients Co-Infected With HIV and Hepatitis C Virus Compared With Hepatitis C Virus–Monoinfected Patients. Ann Intern Med 2014;160:369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fultz SL, Skanderson M, Mole L, et al. Development and verification of a “virtual” cohort using the national VA Health Information System. Med Care 2006;44(8):S25–S30. [DOI] [PubMed] [Google Scholar]
- 19.McGinnis KA, Justice AC, Kraemer KL, Saitz R, Bryant KJ, Fiellin DA. Comparing alcohol screening measures among HIV-infected and -uninfected men. Alcoholism, clinical and experimental research 2013;37(3):435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wallace DJ, Angus DC, Seymour CW, Barnato AE, Kahn JM. Critical care bed growth in the United States. A comparison of regional and national trends. Am J Respir Crit Care Med 2015;191(4):410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen LM, Render M, Sales A, Kennedy EH, Wiitala W, Hofer TP. Intensive care unit admitting patterns in the Veterans Affairs health care system. Arch Intern Med 2012;172(16):1220–1226. [DOI] [PubMed] [Google Scholar]
- 22.Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol 2017;2(3):161–176. [DOI] [PubMed] [Google Scholar]
- 23.Davis GL, Alter MJ, El-Serag H, Poynard T, Jennings LW. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology 2010;138(2):513–521. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien JM Jr., Lu B, Ali NA, et al. Alcohol dependence is independently associated with sepsis, septic shock, and hospital mortality among adult intensive care unit patients. Crit Care Med 2007;35(2):345–350. [DOI] [PubMed] [Google Scholar]
- 25.Lynch C, Pugh R, Battle C, Welsh Intensive Care Society Audit Research Group (WICSARG). A multicentre prospective evaluation of alcohol-related admissions to intensive care units in Wales. J Intensive Care Soc 2017;18(3):193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hietanen S, Ala-Kokko T, Ohtonen P, Käkelä R, Niemelä S, Liisanantti JH. Treatment Profile and 1-Year Mortality Among Nontraumatic Intensive Care Unit Patients With Alcohol-Related Health Problems. J of Intensive Care Med 2017. DOI: 10.1177/0885066617740071. Accessed Oct 5, 2018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.