Abstract
Diversity drives excellence. Diversity enhances innovation in biomedical sciences and, as it relates to novel findings and treatment of diverse populations, in the field of infectious diseases. There are many obstacles to achieving diversity in the biomedical workforce, which create challenges at the levels of recruitment, retention, education, and promotion of individuals. Here we present the challenges, opportunities, and suggestions for the field, institutions, and individuals to adopt in mitigating bias and achieving greater levels of equity, representation, and excellence in clinical practice and research. Our findings provide optimism for a bright future of fair and collaborative approaches that will enhance the power of our biomedical workforce.
Keywords: bias, biomedicine, diversity, equity, inclusion, underrepresented, women, workforce
Diversity enhances excellence and innovation. Including diverse individuals who are also different thinkers because of their lived experiences can increase the breadth and depth of biomedical and clinical inquiries to improve the scope and approach to problems that affect all corners of society. Our goal should be to foster a culture of prioritizing and sustaining diversity at all levels of the biomedical workforce, including the trainee pipeline, trainees, faculty, institutional leadership, committees, national organizations, and government. This article addresses the values of diversity, the data on inclusion and diversity in science, and approaches to improve our effort to foster this diversity.
Here we present data on the benefits of diversity to science and medicine, an extensive list of references on the gaps and paradigms for practices, and specific guidance on how institutions and individuals can promote diversity in their realms. Those who prefer the actionable guidance may read the section “What Are Ways That Our Field Can Foster a Culture of Diversity?”
WHY IS DIVERSITY BENEFICIAL TO SCIENCE?
“Diversity—defined as differences in how we see the world, how we think about the world, how we try and solve problems, the analogies we use, the metaphors, the tools we acquire, the life experiences we have—makes us better at what we do.”
Scott E. Page, Robert L. Harris, Jr, ADVANCEments in Science Lecture, Cornell University, 22 April 2015
Diversity has many facets, including background, age, gender, sexual orientation, race, ethnicity, culture, religion, geography, disability, socioeconomic status, area of expertise, level of experience, thinking style, and skill set. The benefits of engaging individuals with a wide swath of perspectives have great potential to improve our capacity to innovate. Why? Overwhelming evidence suggests that teams that include different kinds of thinkers outperform homogeneous groups on complex tasks, including improved problem solving, increased innovation, and more-accurate predictions—all of which lead to better performance and results when a diverse team is tasked to approach a given problem [1–3]. Diverse and inclusive scientific teams can generate new research questions that have yet to be asked by our field, develop methodical and analytical approaches to better understand study populations, and offer approaches to problem solving from multiple and different perspectives. Diverse groups published higher numbers of articles, and these receive more citations per article [4].
Diverse Groups Publish More Frequently and Are Cited More
A study from 2013 indicated that articles published from the United States and the United Kingdom that included an international author had a significant increase in citations over articles with authors from the same country [4]. Using surname as a proxy for ethnicity, a 2014 analysis showed that articles with 4 or 5 authors of different ethnicities had 5%–10% more citations than articles with all authors of the same ethnicity [2]. To probe the patterns of diversity driving collaborative work, AlSheblie, Rahwan, and Woon queried the scholarly database Microsoft Academic Graph [3]. They ascribed impact to particular papers published between 1958 and 2009, based on 5-year citation counts, and found that increased diversity with regard to ethnicity, age, gender, and affiliation was associated with increased 5-year citation count, with ethnic diversity having the greatest impact.
Diverse Groups Can Have Complementary Skill Sets
The Okinawa Institute of Science and Technology Graduate University (OIST) in Japan instituted a mandate that 50% of all researchers be from outside Japan. In 2012, the institute began recruiting from 6 continents and, by 2018, rose in a ranking of academic institutions in Japan based on research output. The recruitment efforts were broad, recognizing diversity of ethnicity, gender, academic background, and field of interest [5]. Mukhles Sowwan was a researcher from Jerusalem who came to OIST and recruited 10 scientists from around the world. He made 2 broad generalizations about scientific approaches, based on country of origin: researchers from large world-class universities tend to have a more global perspective, while those from countries with less developed infrastructure tend to be more detail oriented. Working together, individuals with both perspectives can complement each other and inform new approaches.
Diverse Groups Are Better Equipped to Address Health Disparities
Diverse and different thinkers can, as physicians and scientists, impact the outer boundaries of healthcare inequity by allowing their practice and research to be informed by broader social contemporary issues [6, 7]. Diverse clinical and scientific teams may be better at addressing the disparities in health outcomes observed among patients of certain racial and ethnic groups. They may be able to do so because they are interested in examining the role that nonscientific factors have in health and well being, such as adverse social determinants of health. Thus, diverse teams in academic medicine can contribute to improving the educational infrastructure to provide robust and meaningful content on diverse patient populations and biomedical problems to equip physicians with relevant knowledge to better take care of patients and begin to undo health-outcome disparities. The recruitment of diverse teams to tackle these problems can result in higher quality and meaningful clinical studies that benefit greater numbers of patients [8].
Intersectionality Allows Us to Highlight and Enrich Our Overlapping Identities
Diversity is complex at the individual or group level when intersectionality is recognized. Intersectionality is the interconnected nature of social categories, such as race, class, disability, and gender, as they apply to a given individual or group, regarded as creating overlapping and interdependent systems of discrimination or disadvantage. Valuing intersectionality in the training, development, retention, and design of scientific teams can enrich the work of research because it is informed by rich and complex heterogeneity in thinking and practice [6].
WHAT ARE THE BARRIERS TO INCREASING DIVERSITY?
Moving Through the Educational Pipeline Is a Challenge for Underrepresented Applicants
The educational pipeline poses a challenge for underrepresented students who may not have had sufficient educational exposure or support. Many have to overcome significant barriers to access education. Understanding these obstacles should help medical and biomedical graduate schools develop improved recruitment and retention programs and take an active role in promotion and outreach initiatives. Institutions should not assume that reputation alone is sufficient to recruit the top candidates among applicants from underrepresented groups. It is possible that perceived institutional culture may dissuade applicants of certain backgrounds. Outreach efforts can enforce a commitment to fostering diversity [8, 9]. Individuals from underrepresented groups may not have had access to the same resources while growing up as those from other backgrounds, who may have received advice in how to improve their curriculum vitae (CV), application, and test-taking and interview skills [10]. When students from underrepresented groups matriculate, many may experience imposter syndrome, in which an individual doubts their own achievements and fear being perceived as a fraud. This perpetuates feelings of inadequacy and isolation [11]. Stereotype threat occurs when individuals feel pressure to conform to preconceived notions about their identity. Many of these circumstances can lead to choices in subspecialty later in training, resulting in lower rates of application to various residency programs and fellowships among students from underrepresented groups [12]. The choice of advanced training relates to numerous factors, including lifestyle, competitive prerequisite requirements, and level of debt [13].
Individuals on Selection Committees May Have Biases of Which They Are Unaware
Unconscious (implicit) bias is the automatic impact of attitudes or stereotypes on our on our view of the world, actions, and decisions without our awareness [14]. Unconscious bias affects judgment and can pose a critical barrier to the recruitment and retention of a diverse biomedical workforce. We all have biases. It is important that we learn them and recognize them in our daily decision-making. The Implicit Association Test [15] is a good way to gauge individual biases because it measures the automaticity with which our brain makes associations. Biases can impact our perceived competence of applicants, even in the dearth of objective information. A nationwide study of science professors evaluated the application from a female and a male undergraduate student for a laboratory manager position in which the same CV was presented but the applicant’s name was different [16]. All found the female applicant to be more likeable, less competent, and less hirable than the male applicant, and the female candidate was offered a lower annual salary (by nearly $4000) and less mentoring than the male candidate. Another study found that letters of recommendation for medical school applications had coded language that differed between female and male applicants, including longer reference letters and more references to the applicant’s CV, publications, patients, and colleagues for men, and shorter reference letters, including more “doubt-raising items,” such as irrelevant information and nondefinitive statements, and more references the applicant’s personal life [17]. Bias can also impact on peer review. Scientists from underrepresented groups receive fewer National Institutes of Health (NIH) awards [18]. Bias can also lead to trainees, faculty, and staff feeling marginalized and not able to reach their full potential and to disparities in awards and promotions. Selection committees may not be sufficiently diverse to represent the need for recruitment of diverse trainees [18–20]. Availability bias is the human tendency to think of examples that come to mind readily and may explain why underrepresented individuals are less likely to be selected as speakers, nominated for awards, or recommended for committees [21–23].
Criteria for Admissions Can Disproportionately Disadvantage Applicants From Educationally and Economically Disadvantaged Backgrounds
Successful outcomes on standardized tests are associated with early exposure to standardized examinations and having access to test-preparation resources to develop a test-taking mind-set. Students from low socioeconomic backgrounds perform worse on standardized tests than other students, and this creates a disadvantage for these students as applicants to graduate and professional education programs. Institutional pressures to maintain status in national rankings may increase their emphasis on standardized testing and may disadvantage students from underrepresented backgrounds; emphasizing a holistic review can yield a more diverse group of incoming students [18, 24].
Medical School Curricula Can Be Based on Old Paradigms That Fail to Address Diverse Populations
Traditional medical schools have failed to address such topics as cross-cultural patient-physician interactions, health disparities, and actionable strategies to improve health outcomes for underserved communities [25]. Furthermore, physiological and genomic paradigms are based on antiquated concepts and often do not represent the patient populations for which physicians will need to care. This is an important area for medical students to reorient to the current needs of disadvantaged patient populations. In addition, evaluative measures during training may be based on subjective measures, leading to bias, rather than on objective measures and competency-based assessments. This can result in great heterogeneity in evaluations and can disadvantage introverted students whose knowledge or skill set may be less evident than that of students who are more extroverted and promote their capabilities [26]. Based on these subjective criteria, underrepresented students are less likely to be represented in the Alpha Omega Alpha Honor Medical Society [26].
Individuals With Disabilities Are Underrepresented in the Academic Medicine Workforce
While almost 20% of the United States population has a disability, a small percentage (only 2.7%) of medical students disclose that they have disabilities [27]. Individuals with disabilities are at risk for health disparities because healthcare professionals may lack appropriate understanding about the impact of disability on health. Physician education emphasizes a patient’s impairment, rather than actionable approaches to break down barriers and improve a patient’s capabilities. Medical trainees with disabilities should be supported in their desire to conduct research on individuals with disabilities, if this is their area of interest. Physicians with disabilities may be more likely to identify and encounter the structural barriers faced by disabled patients, which include policies, practices, accommodations, support, and technical standards that inhibit the achievement of better care for individuals like themselves.
Salary Discrepancies Disadvantage Physicians From Underrepresented Groups
It is well known that there are salary discrepancies across disciplines [27–29]. Women, physicians from underrepresented groups, and international physicians are disproportionately affected by this. Some cite unsubstantiated excuses, such as the claim that women have personal and social obligations that take time away from their professional obligations. Unmentored individuals may not negotiate well for salary. Salaries for researchers are further lower than those for clinicians, which disincentivizes individuals from pursuing research when clinical work can yield greater reimbursements or financial rewards [30]. The magnitude of the salary discrepancy between men and women is greater for women with multiple intersectional identities, such as nonwhite race/ethnicity, graduation from an international medical school, and identification as lesbian, gay, bisexual, transgender, or queer (LGBTQ), given the overlapping and interdependent systems of discrimination or disadvantage each identity brings. A cross-field survey of 65 000 US physicians found that women are paid significantly less across geographic regions and medical disciplines, even when controlled for work hours, age, and other potential contributors [31]. Among the lowest-salaried fields were pediatric subspecialties, with pediatric infectious diseases (median annual salary, $186 000) at the bottom. Adult infectious diseases physicians were ranked 18th among the 24 lowest compensated subspecialties. Non–US-trained physicians earned 2.5% less than US-trained physicians [32]. The low salary for infectious diseases physicians poses a barrier to promising graduates pursuing this field after completion of residency [28, 30, 31]. Within the field of infectious diseases, only 7% of trainees and 4% of Infectious Diseases Society of America (IDSA) members are African American. Similarly, only 12% of trainees and 8% of IDSA members are Hispanic [27, 31]. Trotman et al performed the largest survey of infectious diseases physicians and found that African American infectious diseases physicians were paid 7%–13% less than those from most other racial/ethnic groups [33]. Marcelin et al described more-detailed information on gender, racial, and ethnic salary disparities [34] and cited Aberg et al, who called for concerted efforts to “to establish a diversity and inclusion committee to generate the data necessary for developing a strategic plan to improve the diversity of our workforce and eliminate disparities” [32].
The Pipeline of Academic Medicine Is Leaky for Underrepresented Groups
Despite great effort to expand diversity in the biomedical workforce over the past several decades, individuals from underrepresented groups advance in careers at substantially lower rates. Although women are receiving over half of PhD degrees in the United States, they only make up 38% of full-time faculty and of that number, only 22% of tenured full-time professors are women, only 16% are deans, and only 15% are department chairs [35]. The lack of diversity among leadership makes it difficult to cultivate the careers of individuals who cannot find appropriate role models. Numerous sociocultural factors influence this including perpetual and unconscious bias that affects retention and incentives of underrepresented faculty, challenging work-life policies that preclude life events at early stages after training and creating a sense of isolation [36]. Timing of life events with critical career development milestones can disproportionately disadvantage women of childbearing age. Female and underrepresented scientists are less likely to hold NIH funding and academic leadership positions, and they experience disparities in promotion [37]. A study of 50 000 medical school faculty who were assistant or associate professors between 1980 and 1989 indicated that, by 1997, nearly 50% of white junior faculty had been promoted while only 30%–36% of underrepresented junior faculty were promoted, even when adjusted for gender, tenure status, and NIH funding [38]. This was confirmed in 128 academic medical centers in which black and Hispanic faculty were promoted less frequently than white faculty across nearly 75% of institutions. The consequences of this are clear in that the effects include the reduced ability to recruit promising underrepresented applicants in fields in which young trainees cannot find senior role models with whom they can identify [39]. “Cultural taxation” or the “minority tax” is a byproduct of this, as individuals who are underrepresented are frequently asked to serve on committees, to fill the need for representation [40]. This is even more pronounced with intersectionality, in which an individual may represent multiple interests. This can create a career burden, particularly on senior women faculty, owing to the shortage of representation on committees. This type of service is often not recognized through compensation or traditional promotion metrics.
The Approach to Fostering Diversity Permeates All Levels, Including Individuals, Institutions, National Organizations, and Government Policy
The Infectious Diseases Society of American (IDSA) has set strategic priorities to establish state-of-the-art clinical guidelines, advocate for funding for critical prevention and public health activities, lead the way in antimicrobial stewardship and combating resistance, promote the value of infectious diseases physician-scientists who focus on human immunodeficiency virus (HIV), bring the best and brightest into our field, and put infectious diseases and HIV research front, center, and into practice. The IDSA Board of Directors has launched the Inclusion, Diversity, Access and Equity Task Force (IDA&E) and recognizes that this mission relates to every level of society. “We are confident these talented professionals will successfully fulfill the task force charge to examine the workings of the Society. We are thankful they have volunteered their talent and time to ensure that diversity, inclusion and equity are reflected throughout the organization including the leadership and the strategies of IDSA,” said IDSA President Paul Auwaerter, MD, MBA, in 2018. This governance task force has been charged specifically to support diversity, inclusion, and equity through improved transparency, communication, and efficiency, and to maximize opportunities for members to engage in volunteer leadership.
HOW CAN OUR FIELD FOSTER A CULTURE OF DIVERSITY?
A key first step involves recruitment of individuals who are classically underrepresented in science. It is important to draw from a broad pool of qualified individuals. This may involve outreach, improving pipelines and marketing initiatives, and expanding the definition of excellence [41]. Importantly, recruitment efforts are coupled to retention, and therefore a strong system of support and mentoring is critical for cultivating the careers of young scientists, particularly those from underrepresented groups. It is essential to ensure that the level of diversity among admissions leadership and personnel represents the level of diversity among candidates the institution is hoping to attract and is capable of supporting. Pipeline programs to enhance mentorship and diversity have been extremely successful in advancing the career of individuals who might not otherwise have been supported through this training [42].
Combating Unconscious Bias Requires a Multifaceted Effort
Unconscious bias can be mitigated with data-driven strategies [36]. A combination of in-person workshop training with regular reminders through committee emphasis and institution-sponsored awareness campaigns have been shown to have sustainable improvement in recruitment of diverse candidates. Ways to systematically mitigate the impact of unconscious bias in recruitment and selection include developing clear criteria and standards for the position prior to recruitment efforts, developing a clear evaluation system in advance, conducting anonymous voting, and ensuring that search committees are diverse. Witteman et al reported on a study of the Canadian Institutes of Health Research, which has phased out conventional grant review in which the science and investigator are both evaluated. A new program focused on the research and allowed for the analysis of almost 24 000 grant applications between 2011 and 2016. The authors found that, with a program evaluating research background and qualifications, the gender gap was 4% in favor of male applicants; however, with the new evaluation approach emphasizing the researcher’s science, the gap was closed, resulting in only a 0.9% advantage for male applicants. This study was not randomized, and it is important to note that, in the new review process, reviewers were asked to complete unconscious bias training. which may have had an additional impact on closing the gender gap [40, 41]. Still, reviewer training can have a tremendous impact on reducing biased practices. Conference conveners can make efforts to achieve greater equity and diversity in speaker selection by making programs aware of their diversity statistics, by increasing the diversity of the convener teams, and through direct instruction to encourage diversity [43]. Individuals should promote field experts from underrepresented groups whenever asked for nominations for panels, awards, and speaking opportunities. Creating a database of experts in the field for easy access has been successful in several fields. Social media has also been effective in promoting and disseminating information about oneself and one’s colleagues [44, 45].
Leaders in Medical Education Can Aspire to Parse Genetic and Social Determinant of Health
While race has classically been linked with disease as a risk factor, it has become understood that race is more accurately a marker of vulnerability and systemic disadvantage. Our educational systems can better parse genetic predisposition, associated with ancestry, from social determinants of health. There are important differences among individuals of genomic diversity, but this can easily be conflated with social inequalities attributed to determinants such as education, incarceration, and unemployment. Medical students often feel ill equipped to consider race in clinical medicine [7]. Medical schools are developing curricula that address historical roots of racism and bias and the role that social and genetic determinants of health play in patient care. Sexual and gender minority patient population groups have not historically been emphasized in the undergraduate medical curriculum, and this is important as the LGBTQ population is at increased risk for mental illness, HIV infection, unemployment, poverty, and harassment [46]. Medical schools have begun implementing curricula that include contexts emphasizing the unique health considerations of LGBTQ and other populations [47]. Within the medical center, central initiatives can be taken to mitigate racism and bias through change in management strategies [47–49].
WHAT SHOULD INSTITUTIONS DO TO FOSTER DIVERSITY AND INCLUSION?
Identify and Define Threats to the Promotion of Diversity and Inclusion
The first step is to engage in an ongoing systemic review of policies regarding recruitment and retention, including equity in salaries and resources. Being transparent by collecting and publicizing diversity metrics can engage faculty in dialogues and promote a culture of openness and inclusivity. Institutions should conduct regular anonymous climate surveys, disseminate their results, and respond to needed circumstances [50]. These can be effective for gauging the sentiment of individuals and can provide actionable directions for change on a continuous basis.
Develop and Adhere to Policies That Reflect a Lens of Diversity and Inclusion
Recruitment efforts should include outreach efforts and inclusion initiatives to seek out excellence in numerous settings, including pipeline programs and mentoring networks [50, 51]. Standardized testing should be deemphasized for the sake of holistic review [10] and because of data that standardized testing does not predict success in physician-scientist careers. Safe spaces should be created that encourage equity and recognition of individual needs. These can include networking and support groups for specialized groups that provide education and social events [9]. Policies focused on diversity and inclusion can be extended to educational settings by using nondiscriminatory language in classrooms, curriculum-development programs, and job announcements and by encouraging trainees, faculty, and staff to participate in diversity training [52]. On a departmental level, the process of simplifying name changes and records can hold meaning for transgender people [53]. Mentorship is critical and should be made available to individuals throughout their training trajectory in various forms. Institutions can reward mentoring through incentives such as salary, educational, and research support [39] and by promoting mentors for winning mentorship awards from and participating in professional networks [54]. Faculty development programs and onboarding protocols are critical for instilling values around inclusion and unconscious bias. These practices should be included in professional development on an ongoing basis. The human resources department should have a specific diversity strategy that ensures that anyone in a leadership role receives proper diversity training. Educating the existing and future leaders is critical to this mission.
Educate and Provide Resources to Uphold Institutional Policies
Individuals working at academic institutions experience life events during their training and work that can take a toll on their wellness and can compromise their ability to succeed. By recognizing the influence of these events on an individual’s wellness and ability to function successfully, institutions can implement initiatives to help support its workforce. These initiatives have been demonstrated to improve profitability and productivity in the business world.
Family Support
For families, institutional resources can include a child development center that provides childcare, childhood education, after school and holiday programs, emergency backup daycare, nursing rooms, changing tables, parent rooms, lactation rooms, professional travel support (ie, support for travel for children and/or childcare providers) while at professional conferences, a stop-the-clock policy (to allow tenure-track faculty to request an extension of their tenure evaluation to accommodate responsibilities related to birth, adoption, illness, and elder care), recruitment packages for dual-career couples, subsidized legal fees for family services (ie, family planning), and elder care [55].
Mental Health and Wellness
To help ensure mental health and wellness, institutions can provide access to mental health services, culture activities, and a recreation office for low-priced access to concerts, performances, art exhibitions, lectures, and clubs; a robust and centralized wellness program; subsidized health benefits; and physical fitness incentives.
Enforcement of Recruitment and Retention Policy
Institutional leadership can be held accountable for salary equity and diversity at all levels if policies related to recruitment and retention of faculty that emphasize equity in all domains of diversity are enforced.
Language Support
Institutions can offer language classes to those for whom the language of the institution is not the first language, for presentation and writing skill training, for editing support, and for grant writing support.
Credit for Institutional Service
Institutions can provide credit to individuals for institutional service that will contribute to their salary and/or promotion package, so as not to disadvantage those from underrepresented groups who are asked to make contributions in the interest of fostering diversity [37, 56].
Housing
To address the housing needs of trainees and faculty, institutions can provide resources that help these individuals access affordable residential facilities near campus.
Promote Diversity Publicly
Institutions should implement clear statements to showcase their diversity and nondiscrimination. An inclusion statement should assert that the institution prohibits unlawful discrimination on the basis of race, color, national or ethnic origin, sex, age, disability, religion, sexual orientation, gender identity or expression, veteran status, marital status, or any other characteristic protected by law. A statement preventing unlawful harassment, including sexual harassment and sexual violence, is also critical [57]. Offices of diversity and inclusion should ensure compliance with the Civil Rights Act, particularly titles VI, VII, and IX; the Equal Pay Act; the Americans with Disabilities Act; Sections 503 and 504 of the Rehabilitation Act; the Age Discrimination in Employment Act and Executive Order 11246; and the California Fair Employment and Housing Act. Outreach and recruitment efforts should ensure that talent searches are broad, wide, and fair. Institutions can demonstrate their commitment to diversity through inclusion in their mission statement and core values. It can also be done by ensuring that inclusion in conveyed in branding materials by being conscious of the faces used in public displays and recipients of honors and awards. In sum, visibility and intersectional innovation should be celebrated, and institutional change arises from embracing an explicit intention to engage stakeholders in moving toward meaningful new directions [6].
Create a System of Mutual Accountability
There is a need for periodic reassessment of policies to ensure that inclusion efforts are being upheld through recruitment, curriculum, development, and academic affairs [58]. Annual appraisals and evaluations for trainees and faculty are critical to identifying gaps and should systematically include inclusivity statements to ensure that needs are being met [35, 56]. An institutional report card for diversity missions can be created and presented to the dean on an annual or more frequent basis [59]. A mistreatment or grievance committee [60], as well as ombuds office, are critical to providing a confidential forum for reporting and accountability. Finally, a policy of zero tolerance for mistreatment and harassment should be developed, with clear consequences outlined in the student and faculty handbook. Departments can be incentivized to reward diversity and inclusion.
CONCLUSIONS
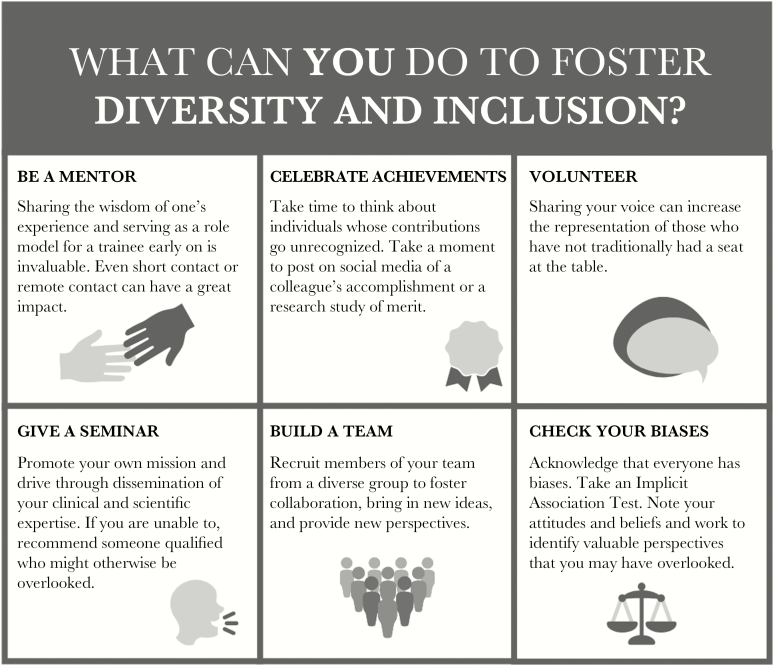
Unconscious bias is a powerful force because it can be unapparent to individuals in leadership positions. Combating unconscious bias on a daily basis is a great challenge of high importance throughout organizations and institutions as they work to overcome the marked challenges that account for underrepresentation in biomedical science and in the field of infectious diseases. Fortunately, there are studies that indicate a positive impact of unconscious bias training, but of greatest importance is the recognition that diversity is everyone’s issue. It is not something that can be left to those who are affected by underrepresentation—it must be imparted to all in leadership, even if they do not understand the affliction of underrepresentation themselves. Individuals have the power to make a difference. Figure 1 outlines steps that any one individual can take to foster diversity and inclusion. Teams are critical to shed light on alternative perspectives and to consider approaches from numerous different angles, to ensure that no one is left out.
Figure 1.
Suggested activities to foster diversity and inclusion.
The IDSA is committed to tackling these problems. The IDSA’s first effort involved establishing the Gender Disparity Task Force in 2016 to identify contributors to gender disparities and to make recommendations to address these disparities [32]. The hopeful outcome will be to increase physicians’ compensation to create equity. There is great optimism for the IDA&E that will hopefully result in a strong future for infectious diseases physicians and researchers. It will be the work of individuals, leadership, institutions, societies, and government agencies to work together to foster a culture of diversity.
Notes
Supplement sponsorship. This supplement is sponsored by the Infectious Diseases Society of America.
Disclaimer. It is not the intent of this article to be linked directly to the Infectious Disease Society of America’s Inclusion, Diversity, Access, and Equity Task Force, nor is it the authors’ intentions to discuss the scope of work assigned to this task force. This article is an independent review addressing the gaps in our understanding of the science and value of diversity.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases (grant K08AI120806 to T. H. S.).
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Page SE, Lewis E, Cantor N.. The diversity bonus: how great teams pay off in the knowledge economy. Princeton, NJ: Princeton University Press, 2017. [Google Scholar]
- 2. Freeman RB, Huang W. Collaboration: strength in diversity. Nature 2014; 513:305. [DOI] [PubMed] [Google Scholar]
- 3. AlShebli BK, Rahwan T, Woon WL. The preeminence of ethnic diversity in scientific collaboration. Nat Commun 2018; 9:5163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Adams J. Collaborations: the fourth age of research. Nature 2013; 497:557–60. [DOI] [PubMed] [Google Scholar]
- 5. Powell K. These labs are remarkably diverse - here’s why they’re winning at science. Nature 2018; 558:19–22. [DOI] [PubMed] [Google Scholar]
- 6. Eckstrand KL, Eliason J, St Cloud T, Potter J. The priority of intersectionality in academic medicine. Acad Med 2016; 91:904–7. [DOI] [PubMed] [Google Scholar]
- 7. Tsai J, Ucik L, Baldwin N, Hasslinger C, George P. Race matters? Examining and rethinking race portrayal in preclinical medical education. Acad Med 2016; 91:916–20. [DOI] [PubMed] [Google Scholar]
- 8. Eckstrand KL, Potter J, Bayer CR, Englander R. Giving context to the physician competency reference set: adapting to the needs of diverse populations. Acad Med 2016; 91:930–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Waldrop MM. Diversity: pride in science. Nature 2014; 513:297–300. [DOI] [PubMed] [Google Scholar]
- 10. Elks ML, Herbert-Carter J, Smith M, Klement B, Knight BB, Anachebe NF. Shifting the curve: fostering academic success in a diverse student body. Acad Med 2018; 93:66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Russell R. On overcoming imposter syndrome. Acad Med 2017; 92:1070. [DOI] [PubMed] [Google Scholar]
- 12. Valantine HA. 50 years to gender parity: can STEM afford to wait?: A cardiologist and NIH chief officer of scientific workforce diversity reflects on what it will take to keep women in biomedicine. IEEE Pulse 2017; 8:46–8. [DOI] [PubMed] [Google Scholar]
- 13. Colquitt WL, Zeh MC, Killian CD, Cultice JM. Effect of debt on U.S. medical school graduates’ preferences for family medicine, general internal medicine, and general pediatrics. Acad Med 1996; 71:399–411. [DOI] [PubMed] [Google Scholar]
- 14. Ross HJ. Everyday bias: identifying and navigating unconscious judgments in our daily lives. Lanham, MD: Rowman & Littlefield Publishers, 2014. [Google Scholar]
- 15. Sukhera J, Wodzinski M, Teunissen PW, Lingard L, Watling C. Striving while accepting: exploring the relationship between identity and implicit bias recognition and management. Acad Med 2018; 93:82–8. [DOI] [PubMed] [Google Scholar]
- 16. Moss-Racusin CA, Dovidio JF, Brescoll VL, Graham MJ, Handelsman J. Science faculty’s subtle gender biases favor male students. Proc Natl Acad Sci U S A 2012; 109:16474–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Trix F, Psenka C. Exploring the color of glass: letters of recommendations for female and male medical faculty. Discourse Soc 2003; 14:191–220. [Google Scholar]
- 18. Ginther DK, Kahn S, Schaffer WT. Gender, race/ethnicity, and National Institutes of Health R01 research awards: is there evidence of a double bind for women of color? Acad Med 2016; 91:1098–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Heller CA, Rúa SH, Mazumdar M, Moon JE, Bardes C, Gotto AM Jr. Diversity efforts, admissions, and national rankings: can we align priorities? Teach Learn Med 2014; 26:304–11. [DOI] [PubMed] [Google Scholar]
- 20. Grbic D, Morrison E, Sondheimer HM, Conrad SS, Milem JF. The association between a holistic review in admissions workshop and the diversity of accepted applicants and students matriculating to medical school. Acad Med 2019; 94:396–403. [DOI] [PubMed] [Google Scholar]
- 21. Lieberman SA, Ainsworth MA, Asimakis GK, et al. Effects of comprehensive educational reforms on academic success in a diverse student body. Med Educ 2010; 44:1232–40. [DOI] [PubMed] [Google Scholar]
- 22. Kalejta RF, Palmenberg AC. Gender parity trends for invited speakers at four prominent virology conference series. J Virol 2017; 91:e00739–17. doi:10.1128/JVI.00739-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Boiko JR, Anderson AJM, Gordon RA. Representation of women among academic grand rounds speakers. JAMA Intern Med 2017; 177:722–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nittrouer CL, Hebl MR, Ashburn-Nardo L, Trump-Steele RCE, Lane DM, Valian V. Gender disparities in colloquium speakers at top universities. Proc Natl Acad Sci U S A 2018; 115:104–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dogra N, Reitmanova S, Carter-Pokras O. Twelve tips for teaching diversity and embedding it in the medical curriculum. Med Teach 2009; 31:990–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bates J, Schrewe B, Ellaway RH, Teunissen PW, Watling C. Embracing standardisation and contextualisation in medical education. Med Educ 2019; 53:15–24. [DOI] [PubMed] [Google Scholar]
- 27. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med 2018; 93:540–3. [DOI] [PubMed] [Google Scholar]
- 28. Burchard EG, Silverman EK, Rosenwasser LJ, et al. Association between a sequence variant in the IL-4 gene promoter and FEV(1) in asthma. Am J Respir Crit Care Med 1999; 160:919–22. [DOI] [PubMed] [Google Scholar]
- 29. Ritter JT, Lynch JB 3rd, MacIntyre AT, Trotman R. Infectious diseases physician compensation: an improved perspective. Open Forum Infect Dis 2016; 3:ofw083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sege R, Nykiel-Bub L, Selk S. Sex differences in institutional support for junior biomedical researchers. JAMA 2015; 314:1175–7. [DOI] [PubMed] [Google Scholar]
- 31.Doximity. Doximity 2018 physician compensation report, 2018. https://blog.doximity.com/articles/doximity-2018-physician-compensation-report. Accessed 1 February 2019. [Google Scholar]
- 32. Aberg JA, Blankson J, Marrazzo J, Adimora AA. Diversity in the US infectious diseases workforce: challenges for women and underrepresented minorities. J Infect Dis 2017; 216:S606–10. [DOI] [PubMed] [Google Scholar]
- 33. Trotman R, Kim AI, MacIntyre AT, Ritter JT, Malani AN. 2017 Infectious Diseases Society of America physician compensation survey: results and analysis. Open Forum Infect Dis 2018; 5:ofy309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Marcelin JR, Bares SH, Fadul N. Improved infectious diseases physician compensation, but disparities remain for women and underrepresented minorities. Open Forum Infect Dis 2019; 6:ofz042. [DOI] [PMC free article] [PubMed]
- 35.AAMC. The state of women in academic medicine: the pipeline and pathways to leadership, 2015–2016. https://www.aamc.org/members/gwims/statistics/. Accessed 15 January 2019. [Google Scholar]
- 36. Girod S, Fassiotto M, Grewal D, et al. Reducing implicit gender leadership bias in academic medicine with an educational intervention. Acad Med 2016; 91:1143–50. [DOI] [PubMed] [Google Scholar]
- 37. Manne-Goehler J, Kapoor N, Blumenthal DM, Stead W. Sex differences in achievement and faculty rank in academic infectious diseases. Clin Infect Dis 2019. doi:10.1093/cid/ciz200 [DOI] [PubMed] [Google Scholar]
- 38. Fang D, Moy E, Colburn L, Hurley J. Racial and ethnic disparities in faculty promotion in academic medicine. JAMA 2000; 284:1085–92. [DOI] [PubMed] [Google Scholar]
- 39. Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med 2013; 88:541–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ 2015; 15:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Freeman BK, Landry A, Trevino R, Grande D, Shea JA. Understanding the leaky pipeline: perceived barriers to pursuing a career in medicine or dentistry among underrepresented-in-medicine undergraduate students. Acad Med 2016; 91:987–93. [DOI] [PubMed] [Google Scholar]
- 42. Milewicz DM, Lorenz RG, Dermody TS, Brass LF; National Association of MD-PhD Programs Executive Committee. Rescuing the physician-scientist workforce: the time for action is now. J Clin Invest 2015; 125:3742–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Casadevall A. Achieving speaker gender equity at the american society for microbiology general meeting. MBio 2015; 6:e01146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Guglielmi G. Gender bias goes away when grant reviewers focus on the science. Nature 2018; 554:14–5. [DOI] [PubMed] [Google Scholar]
- 45. Witteman HO, Hendricks M, Straus S, Tannenbaum C. Are gender gaps due to evaluations of the applicant or the science? A natural experiment at a national funding agency. Lancet 2019; 393:531–40. [DOI] [PubMed] [Google Scholar]
- 46. Hotez PJ. Crafting your scientist brand. PLoS Biol 2018; 16:e3000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ard KL, Keuroghlian AS. Training in sexual and gender minority health - expanding education to reach all clinicians. N Engl J Med 2018; 379:2388–91. [DOI] [PubMed] [Google Scholar]
- 48. Zelin NS, Hastings C, Beaulieu-Jones BR, et al. Sexual and gender minority health in medical curricula in new England: a pilot study of medical student comfort, competence and perception of curricula. Med Educ Online 2018; 23:1461513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Acosta D, Ackerman-Barger K. Breaking the silence: time to talk about race and racism. Acad Med 2017; 92:285–8. [DOI] [PubMed] [Google Scholar]
- 50. Castillo-Page L, Schoolcraft SA, Milem JF, O’Brien C. Assessing the climate and culture around diversity and inclusion in academic medicine: difficult but essential. Acad Med 2012; 87:1313. [DOI] [PubMed] [Google Scholar]
- 51. Jones HP, McGee R, Weber-Main AM, et al. Enhancing research careers: an example of a US national diversity-focused, grant-writing training and coaching experiment. BMC Proc 2017; 11:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Encandela J, Zelin NS, Solotke M, Schwartz ML. Principles and practices for developing an integrated medical school curricular sequence about sexual and gender minority health. Teach Learn Med 2019; 1–16. [DOI] [PubMed] [Google Scholar]
- 53. Carnes M, Devine PG, Baier Manwell L, et al. The effect of an intervention to break the gender bias habit for faculty at one institution: a cluster randomized, controlled trial. Acad Med 2015; 90:221–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Schwartz AL. Commentary: physician-scientist attrition: stemming the tide through national networks for training and development. Acad Med 2011; 86:1071–2. [DOI] [PubMed] [Google Scholar]
- 55. Fox G, Schwartz A, Hart KM. Work-family balance and academic advancement in medical schools. Acad Psychiatry 2006; 30:227–34. [DOI] [PubMed] [Google Scholar]
- 56. Carson TL, Aguilera A, Brown SD, et al. A seat at the table: strategic engagement in service activities for early career faculty from underrepresented groups in the academy. Acad Med 2019; doi: 10.1097/ACM.0000000000002603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mansh M, White W, Gee-Tong L, et al. Sexual and gender minority identity disclosure during undergraduate medical education: “in the closet” in medical school. Acad Med 2015; 90:634–44. [DOI] [PubMed] [Google Scholar]
- 58. Rourke J. Social accountability: a framework for medical schools to improve the health of the populations they serve. Acad Med 2018; 93:1120–4. [DOI] [PubMed] [Google Scholar]
- 59. Smith KA, Arlotta P, Watt FM, Solomon SL; Initiative on Women in Science and Engineering Working Group. Seven actionable strategies for advancing women in science, engineering, and medicine. Cell Stem Cell 2015; 16:221–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bates CK, Jagsi R, Gordon LK, et al. It is time for zero tolerance for sexual harassment in academic medicine. Acad Med 2018; 93:163–5. [DOI] [PubMed] [Google Scholar]