Abstract
Objectives To evaluate the factors that influence the outcome of osteosynthesis after closed reduction of the fracture of the femoral neck in young adult patients.
Methods A retrospective study was conducted, reviewing the data of patients operated in a large orthopedic hospital from 2003 to 2011; a total of 81 patients met the inclusion criteria. The time interval between the fracture and the surgery, the initial fracture deviation, the quality of the reduction, and the placement of the implant were evaluated.
Results The present study observed a strong relationship between the quality of the reduction and therapeutic success. The degree of the initial deviation and the time elapsed between the initial trauma and the osteosynthesis did not influence the surgical outcome regarding bone consolidation. The correct positioning of the implants was associated with a satisfactory evolution in the postoperative period.
Conclusion The quality of the reduction and the positioning of the implants are factors that influence the results of osteosynthesis in fractures of the femoral neck in young adult patients.
Keywords: femoral neck, femoral head necrosis, femoral neck fractures, pseudoarthrosis
Introduction
Proximal femoral fractures are a public health problem directly associated with increased morbidity and mortality rates. Only 50% of the patients with proximal femoral fractures are fully rehabilitated and can resume their previously performed activities. 1 In all age groups, ∼ 50% of the proximal femoral fractures occur in the region of the femoral neck. Femoral head, trochanteric, and subtrochanteric fractures comprise the other half, demonstrating the high prevalence and social and economic impact of this injury in the spectrum of proximal femoral lesions. 2
Femoral neck fractures have a bimodal distribution. In patients > 60 years old, these lesions are usually associated with low-energy traumas and decreased bone mass in the proximal femur. In patients < 60 years old, this fracture is related to higher energy traumas and associated systemic injuries. 3
The main objectives of the treatment of femoral neck fractures are regional anatomy restoration, bone stock preservation, and rapid functional recovery of the limb. 4 The surgical treatment can be total or partial arthroplasty, or osteosynthesis based on the fracture pattern and on the characteristics of the patient. Osteosynthesis options include screw fixation, fixation with hip sliding screw associated with tube plate, or angled plate associated with antirotation screws.
The use of osteosynthesis in the treatment of this fracture is still debated. A recent study showed better outcomes in patients treated with arthroplasty, especially in those > 65 years old. 5 Fixation would be indicated for the treatment of nondeviated fractures and in cases in which, despite the deviation, the patient is < 60 years old. In this situation, the preservation of the cephalic segment of the femur would avoid the need for arthroplasty, as well as its complications, in a young individual. However, the incidence of femoral neck osteosynthesis complications, such as avascular femoral head necrosis (AFHN), lack of fracture consolidation, and fixation failure, made this subject controversial in the literature. 6 Another frequent complication is femoral shortening due to fracture focus impingement, which may alter the offset of the hip. Zielinski et al 7 performed a randomized, multicenter study with 76 patients submitted to femoral neck fracture osteosynthesis who presented some degree of shortening after the consolidation of the fracture. These authors studied the gait pattern and the motor force of the hip compared with the contralateral side. They concluded that young patients are able to compensate the shortening resulting from the consolidation of the femoral neck fracture, and that few cases required the use of insole compensation.
One factor related to the poor prognosis in the treatment of this lesion through osteosynthesis is the long time elapsed between the time of the fracture and the surgical procedure. It is believed that earlier fracture fixations result in better functional outcomes and in a lower tendency for synthesis failure and for AFHN. The favorable prognosis of early fixation would be associated with the rapid restoration of local blood flow and with the reduction of secondary damage. Fracture reduction and fixation within 12 hours are deemed ideal. Surgical stabilization after 24 hours would be associated with worse results and with a higher incidence of surgical failure, which, in this case, would be attributed to the late fixation of the lesion. 8 Other factors, such as initial fracture deviation, the reduction obtained during surgery, and the type of implant used, also seem to directly influence the final outcome of the surgical treatment. 9 Thus, information that helps surgeons in the therapeutic management of this fracture is fundamental for the reduction of complication and failure rates. In the present study, we have identified patient factors that may directly influence the outcome of femoral neck osteosynthesis, and we suggest criteria to support the surgeon when deciding the best therapeutic approach for such fractures, particularly in young adults.
Material and Methods
Between August 2003 and August 2011, 845 patients were admitted with femoral neck fractures to a large orthopedic hospital. Men and women ≤ 60 years old with femoral neck fracture related to high- or moderate-energy traumas and who were treated with closed reduction and internal fixation with 3 cannulated screws, arranged in an inverted triangle configuration, were included in the study. 10 Patients < 15 years old, with femoral neck pathological fractures or septic arthritis, with no radiographic documentation in at least 2 views (anteroposterior [AP] and lateral views), or with low-quality radiographic documentation, with a diagnosis of AFHN previous to the fixation of the fracture, time between fracture and surgical treatment > 42 days, loss of clinical follow-up before the end of the 36-month observation period, as well as patients submitted to other osteosynthesis techniques than those used in the present study, or submitted to hip arthroplasty, were excluded.
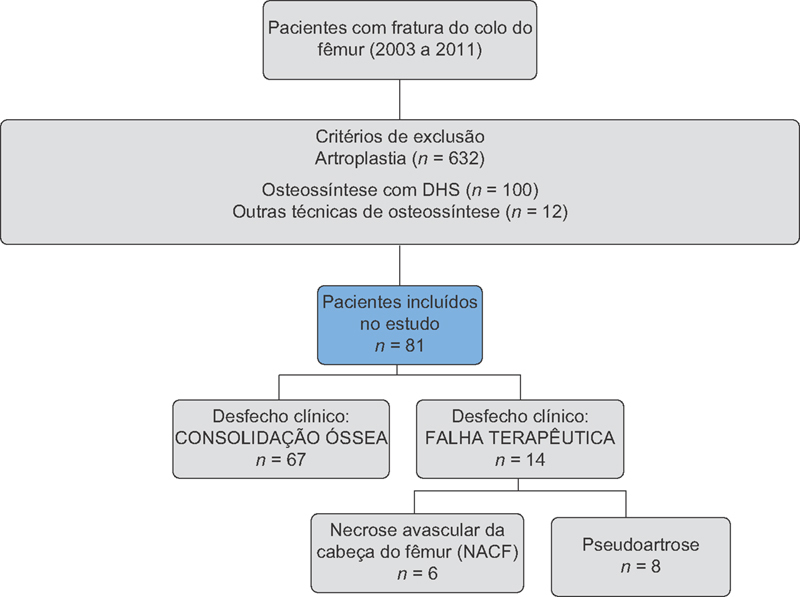
The application of the inclusion and exclusion criteria reduced the initial sample of 845 patients to 81 individuals. From the initial amount, 632 patients (74.8%) were excluded from the study because they had undergone an arthroplasty; 112 (13.25%) were excluded because they had been submitted to other osteosynthesis techniques, and 20 (2.4%) patients did not have complete medical documentation, did not follow the outpatient reassessment routine, or were outside the age range of the present study.
This is an observational, longitudinal, retrospective, analytical, and comparative study. The present study was performed through the review of medical records with an evolutionary analysis of the complementary exams. The lesions were analyzed by radiographic images with good technical quality by three independent observers experienced in the treatment of femoral fractures who work at the Trauma Specialized Care Center (CAE Trauma) of the hospital. The lesions were classified according to the initial deviation by serial visualization of simple, AP and lateral hip radiographs. The lesions were stratified according to the Garden classification criteria 11 into types I and II if there was no deviation, and into types III and IV if there was any deviation.
All of the patients underwent the same surgical procedure performed by the CAE Trauma surgeons. The surgery consisted of closed fracture reduction in an orthopedic traction table, under radioscopic control, followed by internal fixation with 3 7.0 mm cannulated screws. No patient required intracapsular hematoma drainage. At the postoperative period, the mobilization of the affected limb was stimulated early, while partial load bearing was stimulated as soon as it was tolerated by the patient. Total load bearing was only allowed after radiographic confirmation of the consolidation of the fracture.
The quality of the reduction was evaluated in 2 anteroposterior and lateral radiographs, and it was deemed satisfactory when the deviation of the focus of the fracture was < 2 mm and the Garden angles were of 160° and 180°, respectively. The positioning of the screws was considered adequate when the distance between their tip and the subchondral bone was < 5 mm, the distal screw was at the small trochanter or above it, and the angle between the parallel screws was < 10°. 12
From the active search in the medical records, the demographic data and information about the characteristics of the lesions (time elapsed between the occurrence of the fracture and the treatment, mechanism of the trauma, and initial deviation grade of the lesion), the treatment and the clinical evolution of the patient (consolidation, AFHN diagnosis, or lack of consolidation associated with synthesis failure) were obtained.
All of the patients were followed-up with periodic outpatient visits for at least 36 months. The re-evaluation routine followed the CAE Trauma protocol, which consists of serial consultations at 15 days, 1 month, 3 months, and 6 months after the procedure, in addition to an annual review. The time elapsed between the treatment and the occurrence of a complication (lack of consolidation or AFHN) was obtained for all of the patients, and was expressed in months.
The consolidation of the fracture was determined in all of the patients through clinical examination and analysis of AP and lateral proximal femoral radiographic images. This evaluation was performed by three CAE Trauma surgeons, who independently reviewed all of the radiographic documentation, separated into unidentified envelopes. Consolidation was defined by the absence of symptoms during the clinical examination and by the functional recovery of the patient associated with a radiographic image of bone formation and the disappearance of the fracture line at the lesion site in the femoral neck. 13
The clinical diagnosis of lack of consolidation was established in patients with clinical symptoms characterized by progressive pain and functional disability of the operated limb. The radiographic diagnosis of lack of consolidation was made through the observation of a persistent fracture line in the femoral neck associated with signs of implant failure and of loss of reduction.
The diagnosis of AFHN was confirmed based on the classification by Ficat et al 14 and on conventional radiographs in AP and lateral views. The clinical diagnosis of AFHN was confirmed in patients with progressive inguinal pain aggravated by physical exertion.
After a serial evaluation at 36 months postsurgery, the patients with consolidated fractures who resumed daily activities were allocated at the Consolidation group. The patients who needed surgical revision, either due to AFHN or to lack of consolidation, constituted the Failure group.
The Research Ethics Committee from the Instituto Nacional de Traumatologia e Ortopedia approved the terms of the present study, which was exempted from Informed Consent Form signature requirements.
Numerical data (quantitative variables) were expressed as mean ± standard deviation (SD), median, minimum, and maximum values. Categorical data (qualitative variables) were expressed as frequency ( n ) and percentage (%). The distribution analysis of the numerical data (gaussian or normal distribution) was determined by the Shapiro-Wilk test. The comparison of treatment groups regarding age and time between the fracture and the surgical treatment was performed by the Mann-Whitney test, because these variables presented a non-normal distribution. The time elapsed between the surgery and the detection of failure was compared by the Student t-test. The Fisher exact test was used to analyze categorical data. The relative risk of development of failure was determined according to the reference parameters. The statistical analysis was performed in the GraphPad Prism version 5.00 for Windows software (GraphPad Software, San Diego, CA, USA).
The present project was authorized by the Research Ethics Committee of our institution and it was approved under the number 919.66.
Results
The 81 patients were allocated into two groups: Consolidation or Failure; the latter group was subdivided into AFHN or lack of consolidation, according to the reason for therapeutic failure. Thus, 67 patients were included in the Consolidation group, and 14 in the Failure group ( Fig. 1 ).
Fig. 1.
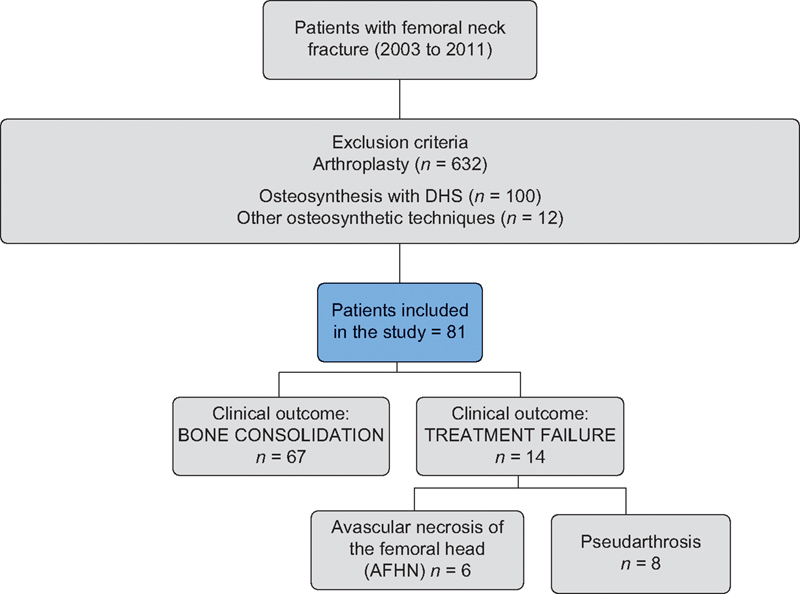
Experimental design, final sample and groups according to the outcome of the treatment. DHS, dynamic hip screw.
The median age was 44 years old (range: 16–60 years old) in the Consolidation group, and 45 years old (range: 19–59 years old) in the Failure group, with no statistical difference ( p = 0.955).
The two groups were homogeneous regarding gender, diabetes mellitus, smoking, and surgical risk according to the American Society of Anesthesiologists (ASA). These variables did not influence the surgical outcome in the studied groups ( Table 1 ).
Table 1. Categorical demographic variables according to the fracture clinical outcome group.
| Variable | Category | Consolidation ( n = 67) |
Failure ( n = 14) | p-value a | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Gender | Male | 10 | 71,4 | 1.000 | ||
| Female | 22 | 32.8 | 4 | 28.6 | ||
| Diabetes mellitus | Yes | 4 | 6.0 | 0 | 0 | 1.000 |
| No | 63 | 94.0 | 14 | 100 | ||
| ASA b | I | 28 | 53.8 | 6 | 50.0 | 1.000 |
| II and III | 24 | 46.1 | 6 | 50.0 | ||
| Smoker | Yes | 16 | 23.9 | 5 | 35.7 | 0.502 |
| No | 51 | 76.1 | 9 | 64.3 | ||
Abbreviation: ASA, American Society of Anesthesiologists risk score.
Fisher exact test.
Documentation failure in 15 patients from the Consolidation group ( n = 52), and in 2 patients from the Failure group ( n = 12).
Time Elapsed between the Fracture and the Surgical Treatment
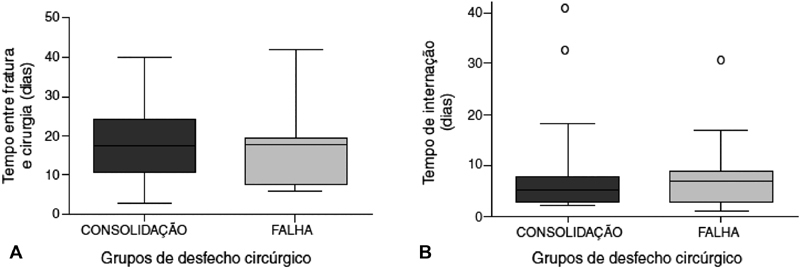
The median time elapsed between the fracture and the surgery in the Consolidation group was of 17 days (range: 3–40 days). In the Failure group, the median was of 17 days (range: 6–42 days). No statistically significant difference was observed between the groups ( p = 0.648) ( Fig. 2A ).
Fig. 2.
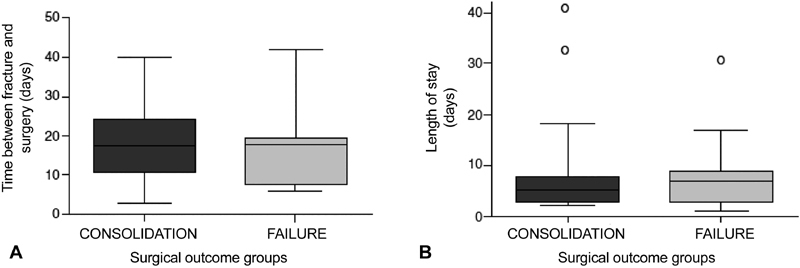
Follow-up of patients with surgically-treated femoral neck fractures who evolved with therapeutic failure (avascular femoral head necrosis or lack of consolidation) or with bone consolidation. A, time elapsed between fracture and surgery. B, hospital length of stay. The horizontal lines at the ends of the rectangles represent the interquartile range values, and the extremities of the bars represent the minimum and maximum values found in each group.
There was no difference in the length of hospital stay between the groups. The median period was of 6 days (range: 1–31 days) for the Failure group, and of 6 days (range: 2–41 days) for the Consolidation group ( Fig. 2B ).
Influence of the Initial Fracture Deviation on the Outcome
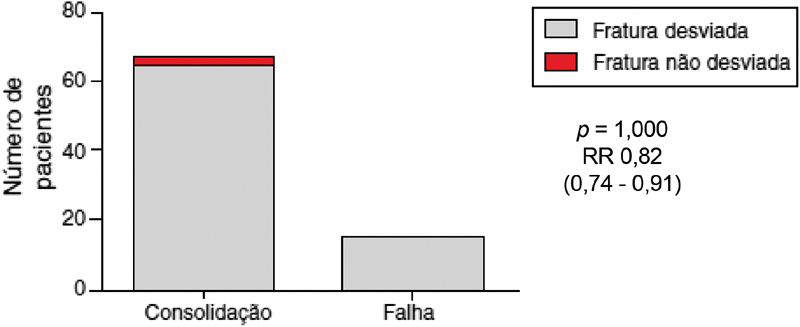
Only 3 patients (3.7%) had no fracture deviation. All (100%; 14/14) of the patients from the Failure group presented an initial fracture deviation, whereas 95.5% patients (64/67) from the Consolidation group presented a deviation; there was no statistical difference ( p = 1.000) ( Fig. 3 ).
Fig. 3.
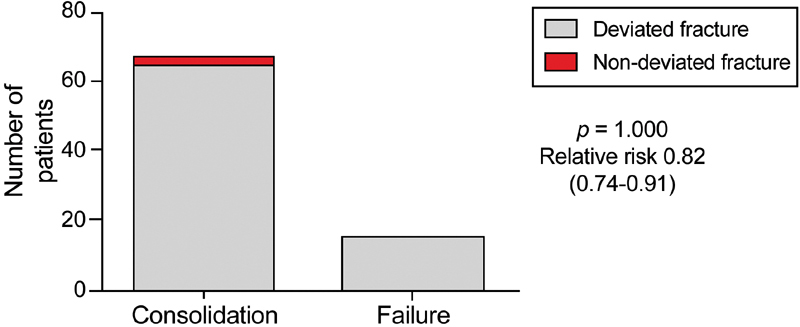
Influence of femoral neck fracture deviation on the outcome of the surgical treatment in young patients. Fisher exact test. RR, relative risk (confidence interval).
Quality of the Reduction of the Fracture
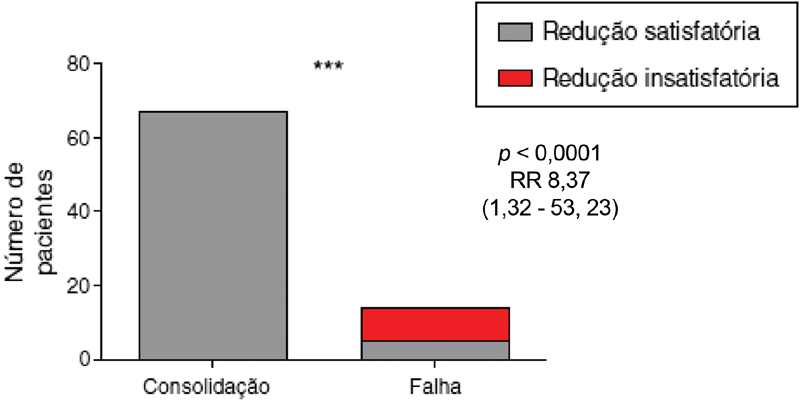
Regarding the quality of the reduction of the fracture, all of the patients evolving with bone consolidation had a satisfactory reduction (67/67). In the Failure group, the reduction was satisfactory in 5 patients (35.7%), and unsatisfactory in 9 individuals (64.3%). The risk of failure was 8.37 times greater when the reduction was inadequate ( p < 0.0001) ( Fig. 4 ).
Fig. 4.
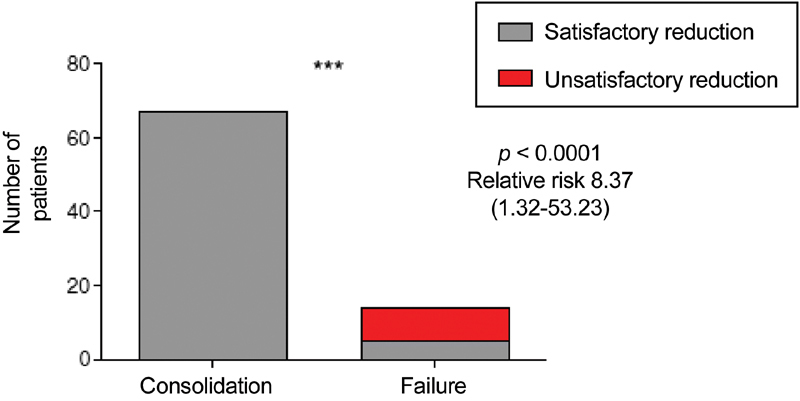
Surgical treatment outcome of femoral neck fractures in young patients as a function of fracture reduction. The reduction was considered satisfactory when the alignment was 160° in anteroposterior views and 180° in profile views. Fisher exact test. RR, relative risk (confidence interval).
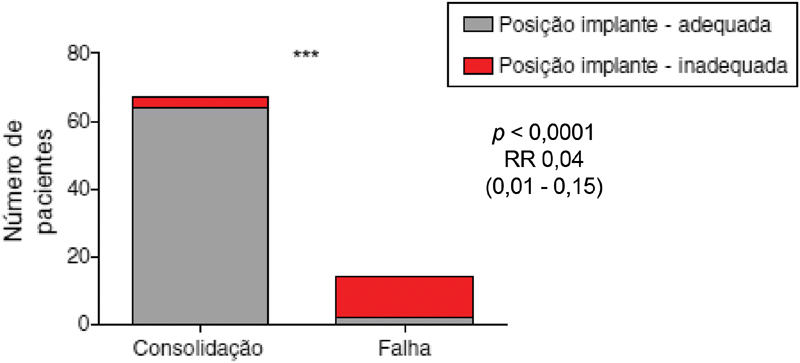
Positioning of the Implants
In the Consolidation group, 95.5% (64/67) of the patients presented adequate implant placement; in contrast, in the Failure group, the positioning was inadequate in 85.7% (12/14) of the cases ( p < 0.001). The correct positioning was a protective factor for failure, as shown by the relative risk of 0.04 (confidence interval [CI]: 0.01–0.15) ( Fig. 5 ).
Fig. 5.
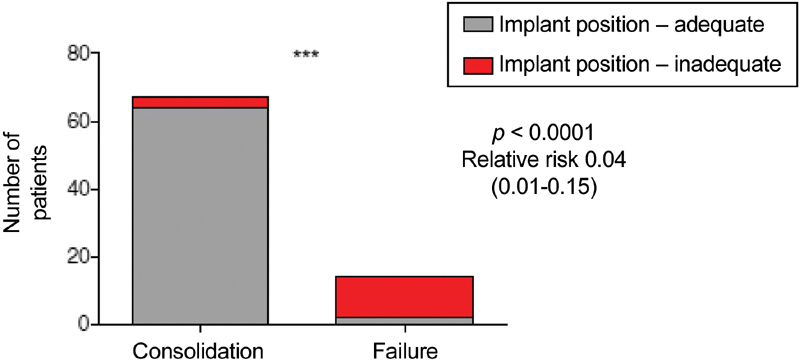
Surgical treatment outcome of femoral neck fractures in young patients as a function of implant positioning. Fisher exact test. RR, relative risk (confidence interval).
The fracture was classified as deviated in the six patients from the Failure group who presented with AFHN. Among them, 2 patients presented satisfactory reduction with adequate implant placement. In the remaining four patients, the reduction was unsatisfactory, and the positioning of the implant was inadequate.
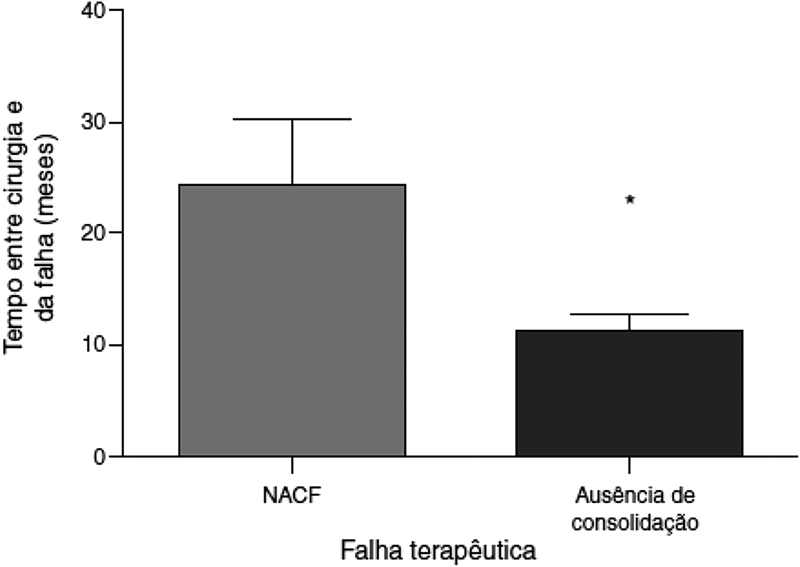
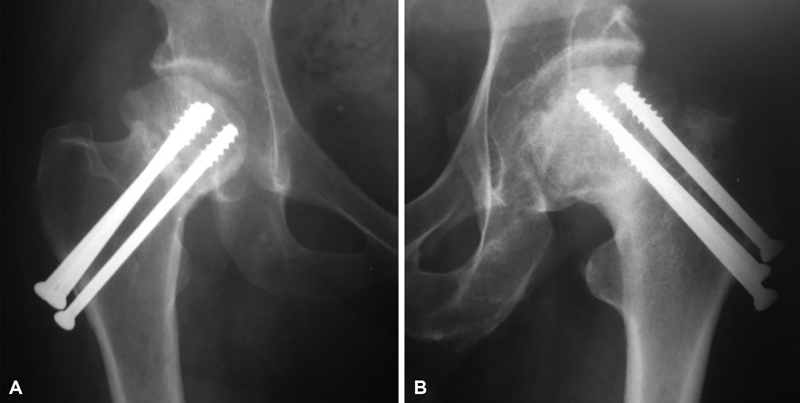
Time Elapsed between the Treatment of the Fracture and the Occurrence of Complication
The time elapsed between the surgical treatment and the detection of therapeutic failure ranged from 5.7 to 49.1 months. Analyzing the outcomes separately, it was observed that this period was higher for patients with AFHN (24.4 ± 11.4 months) compared to those with no bone consolidation (11.3 ± 4.2 months) ( Fig. 6 ). All of the six cases of AFHN were classified as stage III according to the classification by Ficat et al, 14 that is, loss of femoral head sphericity with no acetabular lesion ( Fig. 7 ).
Fig. 6.
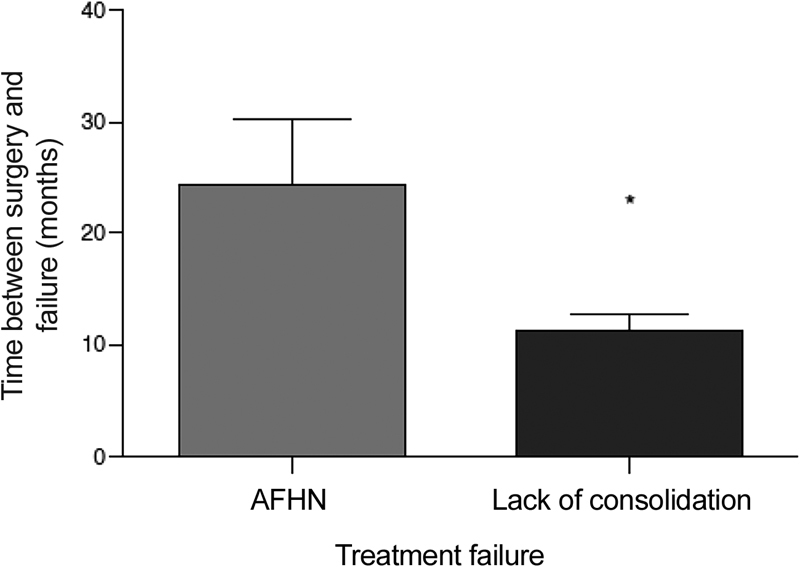
Time between surgery and diagnosis of therapeutic failure. AFHN, avascular femoral head necrosis.
Fig. 7.
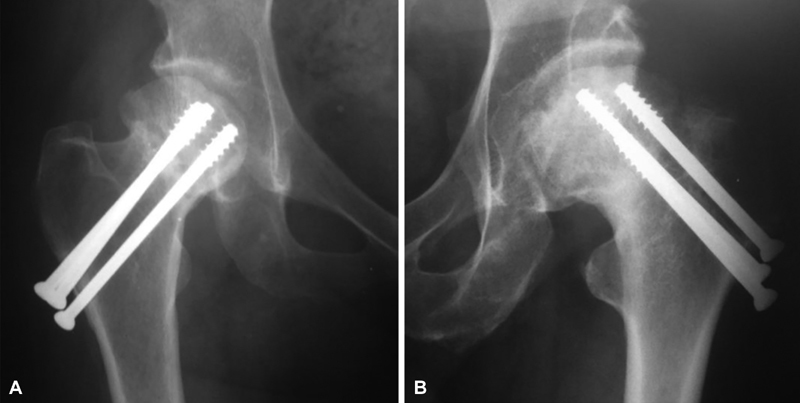
Avascular femoral head necrosis. A, patient with satisfactory reduction and adequate implant positioning. B, Patient with unsatisfactory reduction and inadequate implant positioning.
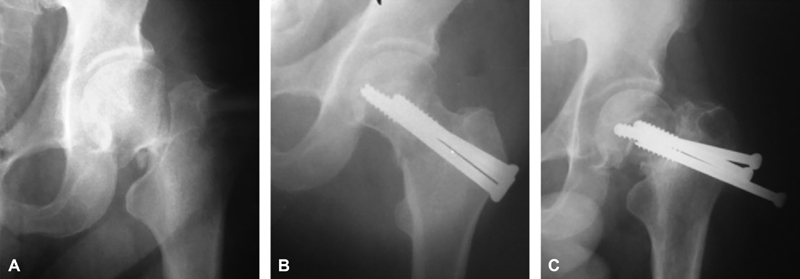
All of the patients with no consolidation had a deviated fracture. Of these, reduction was satisfactory in three patients, and it was unsatisfactory in five individuals. The positioning of the implant was considered inadequate in all of these cases ( Fig. 8 ).
Fig. 8.
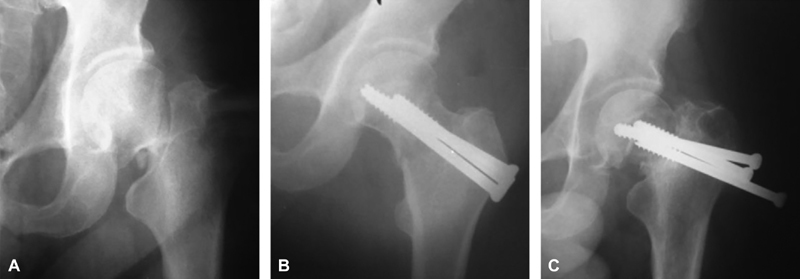
Radiographic evolution of a femoral neck fracture in a patient with no consolidation. A, Deviated fracture. B, Surgical treatment with satisfactory reduction and inadequate implant positioning. C, Evolution to lack of bone consolidation and osteosynthesis failure.
Discussion
Preservation of the femoral head by osteosynthesis is desirable in young patients with fractures of the femoral neck, because bone consolidation occurring in the absence of AFHN leads to satisfactory results, preserving the anatomy and the function of the joint. 15 However, due to fracture instability and to the difficulty in obtaining a stable assembly for the maintenance of the reduction, it can be very challenging due to the high incidence of failure. 16 The failure rates of therapeutic reduction depend on some factors that may be controlled, such as the quality of the reduction and the positioning of the osteosynthesis implants. 9 Other factors are independent and could also influence the final outcome, such as the initial fracture deviation and the time elapsed between the fracture and its surgical treatment. 8
The ideal timing for the surgical correction of fractures of the femoral neck is controversial. Authors advocating early surgery suggest that the main advantage of immediate reduction of the fracture is the decrease of the potential compression of retinacular vessels by deviated fragments and the decompression of the hematoma, which increases the intracapsular pressure, improving the blood flow to the femoral head and minimizing the risk of the development of AFHN. 8 These authors reviewed retrospectively the early fixation of fractures of the femoral neck within 12 hours and the delayed fixation after > 12 hours in 38 patients with a mean age of 46 years old. Avascular femoral head necrosis occurred in 16% of the patients submitted to late fixation. In contrast, Upadhyay et al, 17 in a prospective and randomized study with 92 patients < 50 years old presenting with fractures of the femoral neck, did not observe a significant difference in the consolidation rate and in the incidence of AFHN compared with surgeries performed within 48 hours after the trauma.
In our study, the time elapsed between the occurrence of the fracture and its surgical treatment did not influence the clinical outcomes. Similar results were obtained in other series, 9 18 which also did not observe an association between early fixation and favorable lesion evolution.
In a review by Papakostidis et al, 19 the authors concluded that late fixation, after > 24 hours, is related to an increase in the incidence of pseudarthrosis, but they did not find a relation with the development of AFHN. Our study did not observe a higher incidence of pseudarthrosis in patients submitted to a later fixation. However, our sample consisted of patients whose fractures occurred > 3 days previously, compromising the comparison with the results of the aforementioned review. 19
An important aspect to be discussed is hematoma drainage. The classic report by Swiontkowski et al 20 advocates capsular decompression as an important practice to avoid AFHN. These authors believed that an increased capsular pressure would lead to local vascular injury and to subsequent bone tissue necrosis. However, Wong et al 21 showed that this type of decompression should be discouraged, since they did not observe an association between previous hematoma drainage and a reduction in the rate of necrosis. These authors related the incidence of necrosis to the initial trauma and to the grade of deviation of the fracture, which account for the rupture of the retinacular vessels at the moment of the injury.
Capsular hematoma drainage was not performed in our study; in addition, the AFHN rates were not high, which was consistent with the literature. Kakar et al 22 published a multinational study, which corroborated our practice, in which they evaluated the routine of surgeons in the treatment of fractures of the femoral neck. In their study, 90% of the surgeons reported failure to aspirate a fracture hematoma prior to the osteosynthesis procedure, emphasizing that the quality of the reduction and that the implant used would be the most important factors for satisfactory outcomes.
Some authors believe that the initial deviation of the fracture, which is associated with the energy grade of the trauma, is directly related to the operative outcome. 23 24 25 In our series, this factor could not be proven, since only 3 patients from the total sample ( n = 81) had nondeviated fractures. Since this sample is composed by young patients with better bone quality, it is possible that a high- or moderate-energy trauma would be necessary to cause a deviated fracture. We believe that the initial deviation may be related to ischemia, and that the AFHN is due to the intimate regional anatomic relationship with retinacular vessels, that is, the high energy of the trauma. However, our study does not allow us to affirm or to dismiss this correlation.
The reduction within the patterns described by Garden 11 seems to be a determining factor in the postoperative evolution of fractures of the femoral neck submitted to osteosynthesis. Several studies report higher success rates when a good reduction is obtained. 8 26 27
Our study found similar results, since a satisfactory reduction had a strong association with consolidation of bone fractures. In patients with inadequate reduction, the chance of failure was 8.3 times higher when compared with patients with adequate reduction. We believe that the correct alignment of the fracture with varus correction and retroversion is paramount in the treatment of fractures of the femoral neck, because it provides a favorable mechanical environment for the consolidation of the bone. 9
Conclusion
The most important factors influencing the final result of osteosynthesis in fractures of the femoral neck in young patients are the quality of the reduction and the correct application of the surgical technique. The time elapsed between the fracture and the surgery does not seem to be related to the surgical outcome. Our study could not establish if the initial deviation was a determining factor in the surgical outcome.
Conflitos de Interesses Os autores declaram não haver conflitos de interesses.
Trabalho desenvolvido no Centro de Atenção Especializada de Trauma (CAE Trauma), Instituto Nacional de Traumatologia e Ortopedia (Into), Rio de Janeiro, RJ, Brasil. Publicado originalmente por Elsevier Editora Ltda.
Work performed at the Centro de Atenção Especializada de Trauma (CAE Trauma), Instituto Nacional de Traumatologia e Ortopedia (Into), Rio de Janeiro, RJ, Brazil .Originally Published by Elsevier Editora Ltda.
Referências
- 1.Loizou C L, Parker M J. Avascular necrosis after internal fixation of intracapsular hip fractures; a study of the outcome for 1023 patients. Injury. 2009;40(11):1143–1146. doi: 10.1016/j.injury.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 2.Karagas M R, Lu-Yao G L, Barrett J A, Beach M L, Baron J A. Heterogeneity of hip fracture: age, race, sex, and geographic patterns of femoral neck and trochanteric fractures among the US elderly. Am J Epidemiol. 1996;143(07):677–682. doi: 10.1093/oxfordjournals.aje.a008800. [DOI] [PubMed] [Google Scholar]
- 3.Protzman R R, Burkhalter W E. Femoral-neck fractures in young adults. J Bone Joint Surg Am. 1976;58(05):689–695. [PubMed] [Google Scholar]
- 4.Stockton D J, Lefaivre K A, Deakin D E et al. Incidence, magnitude, and predictors of shortening in young femoral neck fractures. J Orthop Trauma. 2015;29(09):e293–e298. doi: 10.1097/BOT.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 5.Rogmark C, Fenstad A M, Leonardsson O et al. Posterior approach and uncemented stems increases the risk of reoperation after hemiarthroplasties in elderly hip fracture patients. Acta Orthop. 2014;85(01):18–25. doi: 10.3109/17453674.2014.885356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heetveld M J, Rogmark C, Frihagen F, Keating J. Internal fixation versus arthroplasty for displaced femoral neck fractures: what is the evidence? J Orthop Trauma. 2009;23(06):395–402. doi: 10.1097/BOT.0b013e318176147d. [DOI] [PubMed] [Google Scholar]
- 7.Zielinski S M, Keijsers N L, Praet S F et al. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopedics. 2013;36(07):e849–e858. doi: 10.3928/01477447-20130624-13. [DOI] [PubMed] [Google Scholar]
- 8.Jain R, Koo M, Kreder H J, Schemitsch E H, Davey J R, Mahomed N N. Comparison of early and delayed fixation of subcapital hip fractures in patients sixty years of age or less. J Bone Joint Surg Am. 2002;84(09):1605–1612. doi: 10.2106/00004623-200209000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Araujo T P, Guimarães T M, Andrade-Silva F B, Kojima K E, Silva JdosS. Influence of time to surgery on the incidence of complications in femoral neck fracture treated with cannulated screws. Injury. 2014;45(05) 05:S36–S39. doi: 10.1016/S0020-1383(14)70019-1. [DOI] [PubMed] [Google Scholar]
- 10.Asnis S E, Wanek-Sgaglione L. Intracapsular fractures of the femoral neck. Results of cannulated screw fixation. J Bone Joint Surg Am. 1994;76(12):1793–1803. doi: 10.2106/00004623-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Garden R S. The structure and function of the proximal end of the femur. J Bone Joint Surg Br. 1961;43(03):576–589. [Google Scholar]
- 12.Lindequist S, Törnkvist H. Quality of reduction and cortical screw support in femoral neck fractures. An analysis of 72 fractures with a new computerized measuring method. J Orthop Trauma. 1995;9(03):215–221. doi: 10.1097/00005131-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Frank T, Osterhoff G, Sprague S, Garibaldi A, Bhandari M, Slobogean G P; FAITH Investigators.The Radiographic Union Score for Hip (RUSH) Identifies Radiographic Nonunion of Femoral Neck Fractures Clin Orthop Relat Res 2016474061396–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ficat R P, Arlet J. Forage-biopsie de la tete femorale dans I'osteonecrose primative, Observations histo-pathologiques portant sur huit forages. Rev Rhum. 1964;31:257–264. [Google Scholar]
- 15.Bosch U, Schreiber T, Krettek C. Reduction and fixation of displaced intracapsular fractures of the proximal femur. Clin Orthop Relat Res. 2002;(399):59–71. doi: 10.1097/00003086-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Heetveld M J, Raaymakers E L, Luitse J S, Gouma D J. Rating of internal fixation and clinical outcome in displaced femoral neck fractures: a prospective multicenter study. Clin Orthop Relat Res. 2007;454(454):207–213. doi: 10.1097/01.blo.0000238867.15228.8d. [DOI] [PubMed] [Google Scholar]
- 17.Upadhyay A, Jain P, Mishra P, Maini L, Gautum V K, Dhaon B K. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004;86(07):1035–1040. doi: 10.1302/0301-620x.86b7.15047. [DOI] [PubMed] [Google Scholar]
- 18.Razik F, Alexopoulos A S, El-Osta B et al. Time to internal fixation of femoral neck fractures in patients under sixty years--does this matter in the development of osteonecrosis of femoral head? Int Orthop. 2012;36(10):2127–2132. doi: 10.1007/s00264-012-1619-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papakostidis C, Panagiotopoulos A, Piccioli A, Giannoudis P V. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury. 2015;46(03):459–466. doi: 10.1016/j.injury.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 20.Bhandari M, Tornetta P, III, Hanson B, Swiontkowski M F. Optimal internal fixation for femoral neck fractures: multiple screws or sliding hip screws? J Orthop Trauma. 2009;23(06):403–407. doi: 10.1097/BOT.0b013e318176191f. [DOI] [PubMed] [Google Scholar]
- 21.Wong T C, Yeung S H, Ip F K. The effectiveness of capsular decompression for internal fixation of intracapsular hip fractures. J Orthop Surg (Hong Kong) 2007;15(03):282–285. doi: 10.1177/230949900701500307. [DOI] [PubMed] [Google Scholar]
- 22.Kakar S, Tornetta P, III, Schemitsch E H et al. Technical considerations in the operative management of femoral neck fractures in elderly patients: a multinational survey. J Trauma. 2007;63(03):641–646. doi: 10.1097/01.ta.0000249296.55245.97. [DOI] [PubMed] [Google Scholar]
- 23.Crosby J M, Parker M J. Femoral neck collapse after internal fixation of an intracapsular hip fracture: Does it indicate a poor outcome? Injury. 2016;47(12):2760–2763. doi: 10.1016/j.injury.2016.10.021. [DOI] [PubMed] [Google Scholar]
- 24.Kahlenberg C A, Richardson S S, Schairer W W, Cross M B. Rates and Risk Factors of Conversion Hip Arthroplasty After Closed Reduction Percutaneous Hip Pinning for Femoral Neck Fractures-A Population Analysis. J Arthroplasty. 2018;33(03):771–776. doi: 10.1016/j.arth.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Gardner S, Weaver M J, Jerabek S, Rodriguez E, Vrahas M, Harris M. Predictors of early failure in young patients with displaced femoral neck fractures. J Orthop. 2014;12(02):75–80. doi: 10.1016/j.jor.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haidukewych G J, Rothwell W S, Jacofsky D J, Torchia M E, Berry D J. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004;86(08):1711–1716. doi: 10.2106/00004623-200408000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Yang J J, Lin L C, Chao K H et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am. 2013;95(01):61–69. doi: 10.2106/JBJS.K.01081. [DOI] [PubMed] [Google Scholar]