Abstract
Objective
Intestinal tuberculosis (ITB) and inflammatory bowel disease (IBD) frequently present with similar clinical, endoscopic and pathological features, therefore it is difficult to differentiate between them. The aim of this study was to elucidate the diagnostic delay and prognosis of ITB cases, initially misdiagnosed as IBD.
Methods
ITB cases were selected from the hospitalized patient list between April 2004 and March 2017 in a tuberculosis center in Japan. We retrospectively evaluated the initial diagnosis, clinical characteristics, endoscopic and pathological findings, bacterial examinations, treatment and prognosis.
Results
Among 66 ITB patients, ten patients were initially misdiagnosed as IBD. Seven patients were male and the median age was 60.5 years (23-74 years). After the diagnosis of IBD, all the patients were treated with mesalazine, in addition to corticosteroids in two patients and sequential azathioprine and infliximab in one. The median duration of diagnostic delay was 5.5 months (range 0.5-17 months). Eight patients had active pulmonary tuberculosis at the diagnosis of ITB. Acid-fast bacilli were confirmed in four of seven patients by reevaluation of the pathological specimens at the IBD diagnosis. Two patients needed intestinal resection and one with erroneous corticosteroid use for IBD died due to respiratory failure in spite of receiving appropriate treatment for tuberculosis.
Conclusion
ITB patients were frequently misdiagnosed and treated as IBD, thus resulting in a poor clinical outcome even after finally making a correct diagnosis and administering appropriate treatment. On diagnosis of IBD and/or treatment failure, chest radiograph and acid-fast bacilli of the pathological specimens should be carefully evaluated in order to rule out tuberculosis.
Keywords: intestinal tuberculosis, inflammatory bowel disease, misdiagnosis, pulmonary tuberculosis
Introduction
Intestinal tuberculosis may cause serious complications such as ileus, perforation and melena (1-4) though the incidence of intestinal tuberculosis (ITB) in industrialized countries including Japan is decreasing (5). On the other hand, inflammatory bowel disease (IBD), such as Crohn's disease (CD) and ulcerative colitis, which are more prevalent among European countries and United States, is currently increasing in Asian and African countries (6).
Since ITB and IBD, particularly CD, frequently present with similar clinical, endoscopic and pathological features, it is occasionally difficult to distinguish between them, thus resulting in a misdiagnosis (7,8). Though it is a rare condition, ITB could develop during the treatment of IBD with immunosuppressants (9). ITB patients, if misdiagnosed as IBD, may thus quickly deteriorate because of diagnostic and treatment delays and immunosuppression due to the use of corticosteroids and tumor necrosis factor (TNF) inhibitors.
Because there are only a few case reports concerning the misdiagnosis of ITB as IBD in Japan (10) and a few such studies in the world (11,12), little is known about clinical features, prevalence, and prognosis of those cases. The aim of this study was to elucidate the diagnostic delay and prognosis of ITB cases initially misdiagnosed as IBD.
Materials and Methods
Patient selection
ITB cases were selected from the database of hospitalized patients with tuberculosis between April 2004 and March 2017 at National Hospital Organization Tokyo National Hospital, which has the largest tuberculosis ward in the metropolitan Tokyo area and it is one of the largest tuberculosis centers in Japan. The clinical characteristics, such as age, symptoms, clinical course and prognosis together with endoscopic and pathological findings and microbiological examinations were reviewed from the medical records.
This study was approved by the ethical committees of the National Hospital Organization Tokyo National Hospital, and it was conducted according to principles expressed in the Declaration of Helsinki.
Definition of ITB and misdiagnosis as IBD
ITB was diagnosed when at least one of the following criteria was met:[1] histological demonstration of caseating granulomas, which are necrotizing granulomas in a microscopic examination, in intestinal specimens, [2] histological identification of acid-fast bacilli in intestinal specimens, [3] a positive culture of Mycobacterium tuberculosis (MTB) or a positive finding for the MTB specific nucleic acid amplification test (NAAT) from intestinal specimens, [4] clinical, endoscopic, radiographic, and/or surgical evidence of ITB associated with proven tuberculosis elsewhere with response to anti-tuberculosis treatment, and [5] clinical, endoscopic, radiographic, and/or surgical evidence of ITB, and a response to anti-tuberculosis treatment without a relapse after treatment (11,13,14).
A misdiagnosis of IBD was judged when one of the following criteria was met:[A] treatment of IBD was not effective and the histological identification of acid-fast bacilli was made in a reevaluation of specimens at the diagnosis of IBD, [B] treatment of IBD was not effective and a culture of specimens at the diagnosis of IBD were later revealed to be TB positive, and [C] treatment of IBD was not effective, however, anti-tuberculosis treatment was effective.
Pathological analysis
The pathological findings, characteristics of the granulomas and presence of acid-fast bacilli, were extracted from pathological reports written by the pathologists of the prior medical facilities. In six cases, the paraffin blocks of pathological specimens were provided from the prior medical facilities where IBD was diagnosed and acid-fast staining was newly performed in our hospital. In those cases, the pathological findings reevaluated by a pathologist from our hospital are described in the results. Large granuloma was defined as a maximum diameter of the largest granuloma >400 μm in the reevaluated cases (15,16).
Results
The incidence and temporal trend of misdiagnosis
Among 5,516 active tuberculosis patients admitted during the study period, 66 patients met the diagnostic criteria of ITB. Ten patients (15.2%) were initially misdiagnosed as IBD (Figure). There was no ITB patient who had the history of IBD or whose ITB developed during the treatment of IBD in the present study. Based on the misdiagnosis, all the patients were treated at the prior medical facilities and, then were referred to our hospital because of the diagnosis of ITB or suspected ITB. A misdiagnosis was made at primary clinics in two patients, at referral hospitals in four patients and at university hospitals in four patients. There was no increasing or decreasing trend in the incidence of misdiagnosis.
Figure.
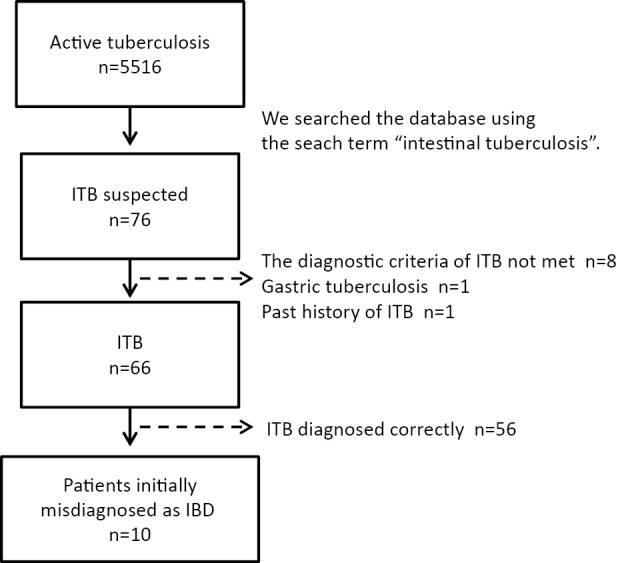
Flowchart for patient selection. ITB suspected patients were selected from the data base using the search words “intestinal tuberculosis”. After patients who met the ITB criteria were selected, we judged whether they met the criteria of misdiagnosis from the medical records. ITB: intestinal tuberculosis
Patients characteristics and the treatments for IBD
Seven patients were male and three were female, and the median age was 60.5 years (range, 23-74 years) (Table 1). The chief complaints at the diagnosis of IBD were hematochezia/positive fecal occult blood in five cases, abdominal pain in four, diarrhea in three and fever in three. All the patients were HIV negative, and one had colon cancer. After the diagnosis of IBD, all the patients were treated with mesalazine in addition to corticosteroids in two patients and sequential azathioprine and infliximab in one because of their deteriorating abdominal symptoms. In spite of the IBD treatments, the patients did not improve and were diagnosed with ITB after additional examinations (sputum in seven cases, colonoscopy in two cases, and a re-evaluation of the pathological specimen at the diagnosis of IBD in one case). The median time of diagnostic delay was 5.5 months (range 0.5-17 months).
Table 1.
Clinical Characteristics of Patients Misdiagnosed as Inflammatory Bowel Disease, Treatment and Duration of Diagnostic Delay.
| Case | Age/Sex | Initial symptom | Underlying disease | Treatment of IBD | DD (m) | Criteria of ITB |
|---|---|---|---|---|---|---|
| 1 | 52/F | AP, BW loss, diarrhea | colon cancer | mesalazine | 0.5 | (1,2†) |
| 2 | 49/F | fecal occult blood | CLD | mesalazine | 6 | (2) |
| 3 | 74/F | diarrhea | none | mesalazine | 4 | (1,3) |
| 4 | 49/M | melena | none | mesalazine | 6 | (4,5) |
| 5 | 23/M | AP, fever | none | mesalazine, AZA, infliximab | 5 | (4,5) |
| 6 | 71/M | melena | none | mesalazine, CS | 10 | (1,2) |
| 7 | 38/M | melena, fever | none | mesalazine, CS | 16 | (2,3) |
| 8 | 71/M | diarrhea, fever | DM | mesalazine | 2 | (1,2) |
| 9 | 69/M | AP, melena | CLD | mesalazine | 2 | (1) |
| 10 | 70/M | AP | depression | mesalazine | 17 | (3) |
Diagnostic criteria of ITB are as follows in brief: 1) necrotizing granulomas in intestinal specimens, 2) acid-fast bacilli (AFB) positive in intestinal specimens, 3) culture and/or nucleic acid amplification test positive from intestinal specimens, 4) ITB suspected with proven tuberculosis elsewhere, and improved by anti-tuberculous treatment, and 5) ITB suspected and improved by anti-TB treatment without relapse after treatment.
†AFB was detected in surgical specimens after initiation of anti-tuberculous treatment.
IBD: inflammatory bowel disease, DD: diagnostic delay, m: month, ITB: intestinal tuberculosis, F: female, M: male, AP: abdominal pain, BW: body weight, CLD: chronic liver disease, DM: diabetes mellitus, AZA: azathioprine, CS: corticosteroids
Endoscopic and surgical findings at the diagnosis of IBD
The diagnosis of IBD was made based on the clinical and pathological findings at the prior medical facilities. Eight patients underwent colonoscopy and three had laparotomy (two ileus cases and one abdominal abscess case) at the diagnosis of IBD (Table 2). Seven patients exhibited the involvement of the ileocecum to the ascending colon. Three patients had annular ulcers and only one had a longitudinal ulcer.
Table 2.
Affected Site, Endoscopic Findings, and Surgical Findings at the Diagnosis of Inflammatory Bowel Disease.
| Case | Affected site | Endoscopic findings | Surgical findings |
|---|---|---|---|
| 1 | ileocecum - A colon | multiple erosion | ND |
| 2 | UK | UK | ND |
| 3 | ileocecum and T colon | annular ulcer, open ileocecal valve | ND |
| 4 | T colon | superficial ulcer | ND |
| 5 | ileocecum - A colon | ND | abscess of ileocecum |
| 6 | jejunum | ND | longitudinal ulcer |
| 7 | ileocecum - A colon | open ileocecal valve, small ulcer | ND |
| 8 | ileum - A colon | ulcer | ND |
| 9 | ileum - A colon | scarring mucosa | annular ulcer of ileum |
| 10 | ileum - ileocecum | aphthous ulcer, annular ulcer | ND |
A colon: ascending colon, T colon: transverse colon, UK: unknown, ND: not done
Pathological findings of biopsy or surgical specimens
In all the patients, granulomas with or without necrosis were confirmed in the pathological specimens. In four out of seven patients (four biopsy cases and three surgical cases) whose pathological specimens at the IBD diagnosis were reevaluated, acid-fast bacilli were confirmed (Table 3). Furthermore, three cases without acid-fast bacilli detection (cases 3, 5, 9) exhibited large granulomas with necrosis, which were compatible with ITB.
Table 3.
Pathological Findings of Biopsy/surgical Specimens at the Time of Misdiagnosis.
| Case | Specimens | Necrotizing granuloma | Non-necrotizing granuloma | Large granuloma | Maximum diameter (μm) | AFB |
|---|---|---|---|---|---|---|
| 1 | Bi | (-) | (+) | UK | UK | |
| 2 † | Bi | (-) | (+) | (+) | 780 | (+) |
| 3 ‡ | Bi | (+) | (-) | (+) | UK | (-) |
| 4 | Bi | (-) | (+) | UK | UK | |
| 5 † | S | (+) | (-) | (+) | 2,060 | (-) |
| 6 † | S | (+) | (-) | (+) | 900 | (+) |
| 7 † | Bi | (-) | (+) | (+) | 610 | (+) |
| 8 † | Bi | (+) | (-) | (+) | 1,190 | (+) |
| 9 | Bi | (-) | (+) | UK | UK | |
| 9 † | S | (+) | (-) | (+) | 870 | (-) |
| 10 | Bi | (-) | (+) | UK | UK |
†: reevaluation of specimen by the pathologist of Tokyo National Hospital
‡: reevaluation of specimen by the pathologist of prior medical facility
AFB: acid-fast bacilli, Bi: biopsy specimen, S: surgical specimen, UK: unknown
Examinations at the diagnosis of ITB and clinical course
MTB was detected from sputum or intestinal tissue specimens in all the misdiagnosed patients on admission to our hospital (Table 4). All the cases, other than case 8 (streptomycin resistant), had no drug resistance for isoniazid, rifampicin, ethambutol, pyrazinamide, and streptomycin. Interferon gamma release assays (IGRAs) were positive in four out of seven QuantiFERON TB-Gold cases and in two out of two T-SPOT. TB cases at the diagnosis of ITB. Eight patients had active pulmonary tuberculosis, including one disseminated TB patient previously treated with infliximab. Though all the patients were treated with anti-tuberculosis drugs, one patient who had used corticosteroids died due to respiratory failure. In addition, two patients needed an intestinal resection because of ileus in the clinical course of ITB treatment.
Table 4.
Examinations at the Diagnosis of Intestinal Tuberculosis, Treatment and Clinical Course.
| Case | Sputum AFB smear | Specimen of culture positive | IGRA | Pulmonary TB | Pulmonary cavity | Anti-TB treatment | Operation after ITB diagnosis | Prognosis |
|---|---|---|---|---|---|---|---|---|
| 1 | (-) | sputum | NE | (+) | (-) | HREZ | enterectomy (colon cancer) | improved |
| 2 | (-) | sputum, stool | T (+) | (+) | (-) | HRS | improved | |
| 3 | (-) | intestinal tissue | T (+) | (-) | (-) | HREZ | improved | |
| 4 | (+) | sputum | Q (+) | (+) | (+) | HREZ | enterectomy (ileus) | improved |
| 5 | (-) | sputum | Q (+) | (+) | (-) | HREZ | improved | |
| 6 | (+) | sputum, stool | Q (-) | (+) | (+) | HREZ | death | |
| 7 | (-) | sputum | Q (-) | (+) | (-) | HREZ | improved | |
| 8 | (+) | sputum | Q (+) | (+) | (-) | HREZ | enterectomy (ileus) | improved |
| 9 | (+) | sputum, stool | Q (+) | (+) | (+) | HRSZ | adhesiotomy (ileus) | improved |
| 10 | (-) | intestinal tissue | Q (-) | (-) | (-) | HREZ | improved |
AFB: acid-fast bacilli, TB: tuberculosis, IGRA: interferon gamma release assay, ITB: intestinal tuberculosis, NE: not examined, T: T-SPOT. TB, Q: QuantiFERON TB-Gold, H: isoniazid, R: rifampicin, E: ethambutol, Z: pyrazinamide, S: streptomycin
Discussion
In this study, ITB cases were frequently misdiagnosed as IBD in 10 (15.2%) out of 66 ITB patients. It is notable that two ITB patients were treated with corticosteroids and one was treated with azathioprine and infliximab as IBD. The ITB patient treated with azathioprine and infliximab developed disseminated tuberculosis, and the patient treated with corticosteroids as IBD died due to respiratory failure despite the initiation of anti-tuberculosis treatment.
Seo et al. reported the temporal trends in the misdiagnosis rate between CD and ITB in South Korea (11). In this article, 83 of the 772 ITB patients (10.8%) were initially misdiagnosed as IBD between 1996 and 2014. Conversely, 494 of the 2,760 IBD patients (17.9%) were initially misdiagnosed as ITB. They suspected that the number of ITB cases misdiagnosed as CD had been increasing over the study period because gastrointestinal specialists became more concerned with CD than ITB. In many countries, including Japan, ITB cases have been decreasing and CD cases have been increasing, the same as in South Korea (5,6,17). Though we could not confirm the increasing trend of an ITB misdiagnosis in the present study, we have to be extremely careful to rule out ITB when making a diagnosis of IBD.
It is difficult to differentiate ITB from IBD because they frequently present with similar symptoms, such as abdominal pain, diarrhea and hematochezia. The colonoscopic findings, pathological features and bacterial examinations of biopsy specimens are important in the differential diagnosis. Several endoscopic findings, such as transverse/annular ulcer and ileocecal valve involvement are predictors for ITB, whereas longitudinal ulcers and a cobblestone appearance suggest the diagnosis of IBD (18,19). Though the gold standard of ITB diagnosis is the detection of MTB with specimens obtained from the intestine, the detection rate is still not satisfactory. Sekine et al. reported the sensitivities of culture, acid-fast stain and NAAT of intestinal tissue for ITB diagnosis to be 50%, 38% and 25%, respectively (13). Other reports described that the positive rate of culture was 44.1% (14) and NAAT was 47% (20) in the biopsy samples. In the present study, acid-fast bacilli were confirmed in four out of seven patients whose pathological specimens were reevaluated. At the diagnosis of IBD, a combination of the acid-fast stain, culture and NAAT of intestinal tissue would have prevented a misdiagnosis in several cases in this study and thus would have improved the prognosis of the patients. In the pathological diagnosis, necrotizing granulomas and large granulomas were typical findings of ITB (12,21) as detected in three acid-fast bacilli negative cases.
The positive rate of IGRAs at the diagnosis of ITB was 66.7% (6/9) in the present study. The decreased rate of IGRAs positive may reflect the poor condition of the patients (22). Corticosteroids had been administered in two of three cases with negative IGRAs, including one critically ill patient that resulted in death. Though a meta-analysis of IGRAs in ITB cases revealed a sensitivity of 0.74 and a specificity of 0.87 (23), levels that are slightly lower than those of active pulmonary tuberculosis (24), IGRAs can be used supplemental evaluations when making an IBD diagnosis. Especially, such examinations should be carried out before the administration of corticosteroids or TNF inhibitors.
It is reasonable that several patients of ITB have active or old pulmonary tuberculous (1,8) because most of the ITB lesions were infected through luminal transmission from the respiratory tract. Actually, in a retrospective analysis of 50 ITB patients, 32 patients (64%) had active pulmonary tuberculous lesions and seven patients (14%) had old pulmonary tuberculous lesions (13). In addition, the rates of concomitant pulmonary tuberculosis were reported to be 25% and 67% in other retrospective studies of ITB cases (25,26). In our retrospective study, it is unknown whether chest radiographs was examined at the time of a misdiagnosis of IBD. The fact that most of the misdiagnosed patients, eight out of 10, had active pulmonary tuberculosis at the diagnosis of ITB suggests chest radiographs may be helpful in making an ITB diagnosis and thus useful to reduce the rate of such a misdiagnosis.
Patients who develop active tuberculosis during treatment with TNF inhibitors sometimes show a paradoxical worsening of the preexisting lesions or the emergence of new lesions after the withdrawal of TNF inhibitors (27). This phenomenon is similar to immune reconstitution inflammatory syndrome which is widely recognized in patients infected with human immunodeficiency virus receiving antiretroviral therapy. Though disseminated TB was reported to be a risk factor for a paradoxical worsening (28), our disseminated TB case (case 5) which had been administered TNF inhibitor successfully recovered without any paradoxical worsening.
There are a few limitations associated with the present study. This study was performed in a single tuberculosis center and the number of patients with a false diagnosis was small. Though we found acid-fast bacilli were positive in a re-evaluation of the pathological specimens in many cases, we could not evaluate all the initial materials. Another limitation was that we could not retrospectively determine the accurate reasons for the diagnosis of IBD at prior medical facilities. Nevertheless, the retrospective setting was inevitable because a prospective analysis of the misdiagnosis was ethically impossible to conduct. In addition, the prospective setting itself may reduce the misdiagnosis rate of ITB and IBD.
The findings of our study demonstrated that ITB patients were frequently misdiagnosed and treated as IBD, resulting in a poor clinical outcome even after receiving a correct diagnosis and treatment. On diagnosis of IBD and/or its treatment failure, chest radiograph and acid-fast bacilli examination of the pathological specimens should be carefully evaluated in order to clearly rule out the possibility of tuberculosis.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Mamo JP, Brij SO, Enoch DA. Abdominal tuberculosis: a retrospective review of cases presenting to a UK district hospital. QJM 106: 347-354, 2013. [DOI] [PubMed] [Google Scholar]
- 2. Weledji EP, Pokam BT. Abdominal tuberculosis: is there a role for surgery? World J Gastrointest Surg 9: 174-181, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pathak P, Sahu SK, Agrawal S. Clinico-pathological profile and surgical outcome of patients of gastrointestinal tuberculosis undergoing laparotomy. Chirurgia (Bucur) 111: 487-492, 2016. [DOI] [PubMed] [Google Scholar]
- 4. Debi U, Ravisankar V, Prasad KK, Sinha SK, Sharma AK. Abdominal tuberculosis of the gastrointestinal tract: revisited. World J Gastroenterol 20: 14831-14840, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Japan Anti-Tuberculosis. Assosiation. In: Statistics of TB 2016. 1st ed Shobi, Tokyo, 2016: 24-27. [Google Scholar]
- 6. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390: 2769-2778, 2018. [DOI] [PubMed] [Google Scholar]
- 7. Akbar HO. Intestinal tuberculosis and Crohn's disease: the dilemma of similarities and misdiagnosis. BMJ Case Rep 2009: bcr04.2009.1729, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu YF, Ho CM, Yuan CT, Chen CN. Intestinal tuberculosis previously mistreated as Crohn's disease and complicated with perforation: a case report and literature review. Springerplus 4: 326, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aleric I, Katalinic D, Vcev A, Brinar M. Pulmonary actinomycosis coexisting with intestinal tuberculosis as a complication of adalimumab treatment for Crohn's disease. Acta Gastroenterol Belg 80: 544-546, 2017. [PubMed] [Google Scholar]
- 10. Moriwaki Y, Toyoda H, Kosuge T, et al. A case of hemorrhagic and perforated intestinal tuberculosis in which adequate preoperative examination could not be performed and emergency operation could not be avoided. Nihon Kyukyu Igakkai Zassi (J Jpn Assoc Acute Med) 19: 272-278, 2008(in Japanese). [Google Scholar]
- 11. Seo H, Lee S, So H, et al. Temporal trends in the misdiagnosis rates between Crohn's disease and intestinal tuberculosis. World J Gastroenterol 23: 6306-6314, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wei JP, Wu XY, Gao SY, Chen QY, Liu T, Liu G. Misdiagnosis and mistherapy of Crohn's disease as intestinal tuberculosis: case report and literature review. Medicine (Baltimore) 95: e2436, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sekine K, Nagata N, Shindo T, et al. Combined identifying granuloma and biopsy culture is useful for diagnosing intestinal tuberculosis. Int J Colorectal Dis 30: 939-945, 2015. [DOI] [PubMed] [Google Scholar]
- 14. Ye BD, Yang SK, Kim D, et al. Diagnostic sensitivity of culture and drug resistance patterns in Korean patients with intestinal tuberculosis. Int J Tuberc Lung Dis 16: 799-804, 2012. [DOI] [PubMed] [Google Scholar]
- 15. Pulimood AB, Peter S, Ramakrishna B, et al. Segmental colonoscopic biopsies in the differentiation of ileocolic tuberculosis from Crohn's disease. J Gastroenterol Hepatol 20: 688-696, 2005. [DOI] [PubMed] [Google Scholar]
- 16. Ye Z, Lin Y, Cao Q, He Y, Xue L. Granulomas as the most useful histopathological feature in distinguishing between Crohn's disease and intestinal tuberculosis in endoscopic biopsy specimens. Medicine (Baltimore) 94: e2157, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ueno F, Matsui T, Matsumoto T, Matsuoka K, Watanabe M, Hibi T, Guidelines Project Group of the Research Group of Intractable Inflammatory Bowel Disease subsidized by the Ministry of Health, Labour and Welfare of Japan and the Guidelines Committee of the Japanese Society of Gastroenterology . Evidence-based clinical practice guidelines for Crohn's disease, integrated with formal consensus of experts in Japan. J Gastroenterol 48: 31-72, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Limsrivilai J, Shreiner AB, Pongpaibul A, et al. Meta-analytic bayesian model for differentiating intestinal tuberculosis from Crohn's disease. Am J Gastroenterol 112: 415-427, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huang X, Liao WD, Yu C, et al. Differences in clinical features of Crohn's disease and intestinal tuberculosis. World J Gastroenterol 21: 3650-3656, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jin T, Fei B, Zhang Y, He X. The diagnostic value of polymerase chain reaction for Mycobacterium tuberculosis to distinguish intestinal tuberculosis from crohn's disease: A meta-analysis. Saudi J Gastroenterol 23: 3-10, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kirsch R, Pentecost M, Hall Pde M, Epstein DP, Watermeyer G, Friederich PW. Role of colonoscopic biopsy in distinguishing between Crohn's disease and intestinal tuberculosis. J Clin Pathol 59: 840-844, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hang NT, Lien LT, Kobayashi N, et al. Analysis of factors lowering sensitivity of interferon-γ release assay for tuberculosis. PLoS One 6: e23806, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen W, Fan JH, Luo W, Peng P, Su SB. Effectiveness of interferon-gamma release assays for differentiating intestinal tuberculosis from Crohn's disease: a meta-analysis. World J Gastroenterol 19: 8133-8140, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mori T. Usefulness of interferon-gamma release assays for diagnosing TB infection and problems with these assays. J Infect Chemother 15: 143-155, 2009. [DOI] [PubMed] [Google Scholar]
- 25. Cheng W, Zhang S, Li Y, Wang J, Li J. Intestinal tuberculosis: clinico-pathological profile and the importance of a high degree of suspicion. Trop Med Int Health 24: 81-90, (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 26. Kentley J, Ooi JL, Potter J, et al. Intestinal tuberculosis: a diagnostic challenge. Trop Med Int Health 22: 994-999, 2017. [DOI] [PubMed] [Google Scholar]
- 27. Arend SM, Leyten EM, Franken WP, Huisman EM, van Dissel JT. A patient with de novo tuberculosis during anti-tumor necrosis factor-alpha therapy illustrating diagnostic pitfalls and paradoxical response to treatment. Clin Infect Dis 45: 1470-1475, 2007. [DOI] [PubMed] [Google Scholar]
- 28. Rivoisy C, Tubach F, Roy C, et al. Paradoxical anti-TNF-associated TB worsening: Frequency and factors associated with IRIS. Joint Bone Spine 83: 173-178, 2016. [DOI] [PubMed] [Google Scholar]


