Abstract
Objective To evaluate and compare the osteointegration of irradiated and non-irradiated frozen bone grafts used in 21 patients undergoing revision hip arthroplasty procedures with the Exeter technique.
Methods A retrospective study of 21 patients undergoing revision hip arthroplasty with the Exeter technique using bone tissues treated or not with gamma radiation between 2013 and 2014. The patients were divided into two groups according to the use of grafts treated or not with ionizing radiation (gamma rays); as such, these groups were classified as irradiated or non-irradiated. The osteointegration results determined by radiographic analysis of these grafts were compared in the postoperative period of 6 and 12 months.
Results Comparing the graft osteointegration in all patients at 6 and 12 months postoperatively, we noticed a significant difference in the radiographic evaluations in this period ( p = 0.031). Out of the patients studied, 7 were from the irradiated group, and 14 belonged to the non-irradiated group. No statistically significant differences were observed ( p = 0.804) regarding osteointegration when we compared the irradiated and non-irradiated groups.
Conclusion There was no significant difference in the use of irradiated or non-irradiated grafts in revision hip arthroplasty procedures with the Exeter technique.
Keywords: osteointegration, tissue bank, bone grafts, arthroplasty
Introduction
In Brazil, the most transplanted human tissue is homologous bone, followed by other transplants, such as skin, cornea and bone marrow transplants. Bone tissues are used in orthopedic and dental reconstructions, and their demand has grown over the last decade. 1
Autologous bone tissues are considered the gold standard in reconstructive surgeries because of their osteogenic, osteoinductive and osteoconductive properties; in addition, they do not cause immunological reactions. However, homologous bone tissues have advantages when compared to autologous tissues, including reduced morbidity, lack of a second surgical incision, and lower blood loss during surgery; moreover, homologous tissues enable reconstructions requiring a greater amount of graft. 2 3 4
In orthopedics, bone grafts are used mainly in scoliosis surgeries, musculoskeletal tumor resection, pseudarthrosis treatment and revision hip and knee arthroplasty with increasing procedural numbers. 2 4 The improvement of tissue banks in the preparation and supply of different types of graft increased the efficiency of bone transplants and revision arthroplasty surgeries with severe bone stock loss. 5 6 7
There is a great concern in assuring the quality of bone tissues and the safety of the recipients regarding the transmission of infectious and contagious diseases. 4
Tissue sterilization using ionizing radiation is the only process that provides a safety level of 10 −6 , that is, the probability of finding a viable organism is 1:1,000,000; in addition, this method has advantages over other sterilization procedures, such as good penetrability, absence of toxic waste, and potential use as a final sterilization, thus avoiding the risk of contamination by poststerilization manipulation. 8 Although gamma radiation from 6° Co sources has been applied in the sterilization of biological tissues for years, several authors demonstrate that this procedure can lead to structural and biological alterations according to the applied dose. 9 10 11
The present study evaluates and compares the osteointegration of irradiated and non-irradiated frozen bone grafts used in patients submitted to revision hip arthroplasty procedures.
Materials and Methods
This is a retrospective study of 21 patients undergoing revision hip arthroplasty procedures with the Exeter technique using bone tissues treated with or not gamma radiation between 2013 and 2014. A total of 14 patients were male, and 7 were female; their age ranged from 48 to 85 years (mean: 67.7 years). The study was approved by the Ethics in Research Committee, and was performed at the tissue bank in conjunction with the hip group from our institution.
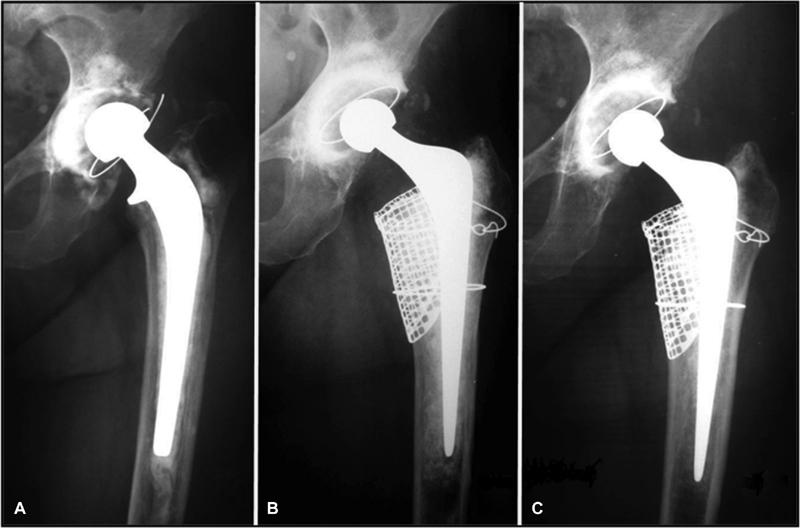
Routine preoperative and postoperative radiological evaluations, performed at the immediate postsurgical period and at 6 and 12 months after the surgery, were analyzed to determine graft osteointegration, as shown in Figure 1 .
Fig. 1.
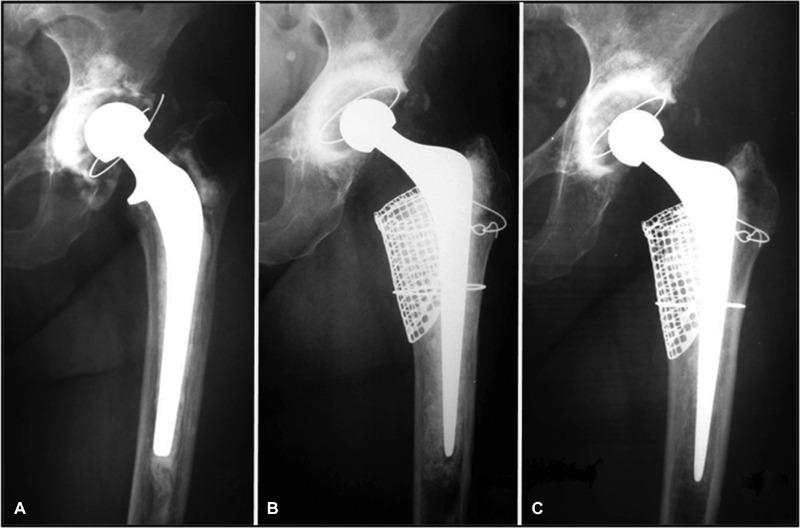
Anteroposterior hip radiographs. (A) Preoperative radiography with assessment of left acetabular and femoral bone loss. (B) Postoperative radiograph immediately after prosthesis revision with irradiated bone graft in the acetabulum and femur. (C) Postoperative radiograph at 12 months, showing bone integration of the irradiated graft in the acetabulum and femur.
The radiographical criteria proposed by Coon et al 12 and Azuma et al 13 were used to interpret the osteointegration achieved 6 and 12 months after surgery, and to stratify the patients, as shown in Table 1 .
Table 1. Bone integration classification of the impacted graft using the Exeter technique, as described by Coon et al 12 and Azuma et al 13 .
| Osteointegration classification | Conditions proposed for osteointegration classification |
|---|---|
| 1 –Total graft osteointegration | Total formation of a continuous trabecular template at the interface between the bone graft and the recipient bone, denoting the appearance of a new trabecular pattern similar to a normal bone structure in all areas of the impacted graft, followed by bone tissue reorganization, disappearance of the sclerotic line at the graft–receptor interface, and identical radiodensity between the graft and the receptor bone. |
| 2 –Partial graft osteointegration | Partial formation of a continuous trabecular template at the interface between the bone graft and the recipient bone, denoting the appearance of a new trabecular pattern similar to a normal bone structure in part of the impacted graft, followed by bone tissue reorganization, partial disappearance of the sclerotic line at the graft–receptor interface and partially identical radiodensity between the graft and the receptor bone. |
| 3 –Absence of osteointegration | There was no graft osteointegration. |
| 4 –Inability to evaluate osteointegration | Impossibility to visualize the grafts due to the presence of screens or other prosthetic devices. |
The patients were divided into two groups according to the use of grafts treated or not with ionizing radiation (gamma rays); as such, these groups were classified as irradiated or non-irradiated.
The tissues were irradiated with gamma rays at a dose of 25 kGy, with a dose rate of 0.00138 kGy/s and an approximate temperature of -70°C, since these conditions reduce undesirable radiation effects, including high doses, high energy transfer rate and heating respectively, in order to maintain their biological integrity. 4
The results were analyzed and compared between the groups. A total of 3 patients were excluded during the comparison of the irradiated and non-irradiated groups with osteointegration classification number 4. The statistical analysis was performed by result comparison using the unpaired, non-parametric Mann-Whitney Test for the statistical differences ( p < 0.05).
Results
Out of the 21 patients studied, 7 belonged to the irradiated group (use of irradiated frozen bone graft), and 14 were from the non-irradiated group (use of non-irradiated frozen bone graft). Their initial diagnoses for primary hip arthroplasty were: hip arthrosis (71.4%); femoral neck or acetabulum fracture (14.2%); femoral head necrosis (4.8%); developmental dysplasia of the hip (4.8%); and ankylosing spondylitis (4.8%). None of the evaluated cases presented infection.
The amount of bone grafts used in the patients ranged from 50 to 266 g (mean: 128.4 g).
Table 2 shows that 8 patients presented partial osteointegration at the 6-month postoperative radiographic evaluation, which evolved to total graft osteointegration at 12 months; in addition, 4 patients with no osteointegration at 6 months presented partial osteointegration 12 months after the procedure. However, 6 patients did not present osteointegration at both the 6- and 12-month examinations, and 3 patients could not be evaluated for osteointegration due to the presence of screens or other prosthetic devices. There was a significant difference between the results obtained at the 6- and 12-month evaluations ( p = 0.031).
Table 2. Report of the radiographic evaluation of osteointegration of the transplanted bone grafts in the irradiated and non-irradiated groups 6 and 12 months after surgery using the Exeter technique and according to the proposed classification.
| Groups | Patients | Osteointegration classification | |
|---|---|---|---|
| 6 months after surgery | 12 months after surgery | ||
| Irradiated | Patient #1 | 2 | 1 |
| Patient #2 | 3 | 2 | |
| Patient #3 | 2 | 1 | |
| Patient #4 | 4 | 4 | |
| Patient #5 | 3 | 3 | |
| Patient #6 | 2 | 1 | |
| Patient #7 | 3 | 3 | |
| Non-irradiated | Patient #8 | 3 | 3 |
| Patient #9 | 2 | 1 | |
| Patient #10 | 2 | 1 | |
| Patient #11 | 3 | 2 | |
| Patient #12 | 2 | 1 | |
| Patient #13 | 3 | 3 | |
| Patient #14 | 2 | 1 | |
| Patient #15 | 3 | 2 | |
| Patient #16 | 3 | 2 | |
| Patient #17 | 4 | 4 | |
| Patient #18 | 3 | 3 | |
| Patient #19 | 2 | 1 | |
| Patient #20 | 4 | 4 | |
| Patient #21 | 3 | 3 | |
Note: Osteointegration classification: 1- Total graft osteointegration; 2- Partial graft osteointegration; 3- Absence of osteointegration; 4- Inability to evaluate osteointegration.
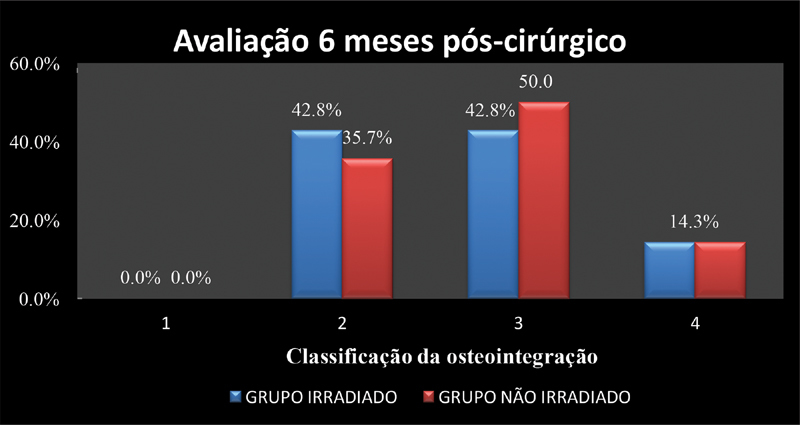
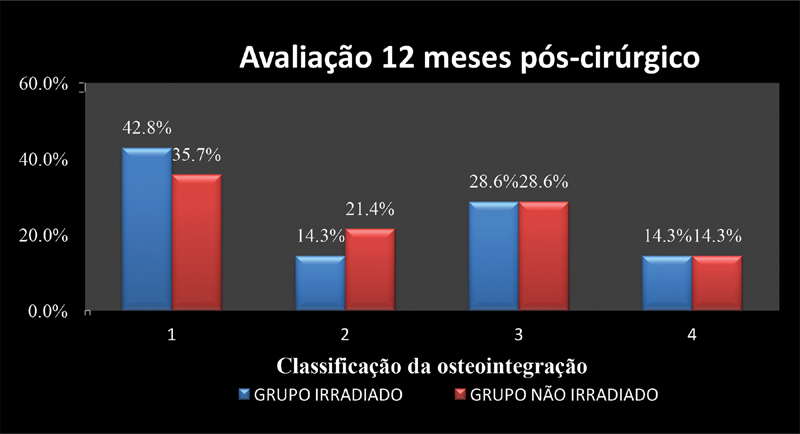
Figures 2 and 3 compare the percentage of osteointegration in the irradiated and non-irradiated groups. No statistically significant differences were found ( p = 0.804).
Fig. 2.
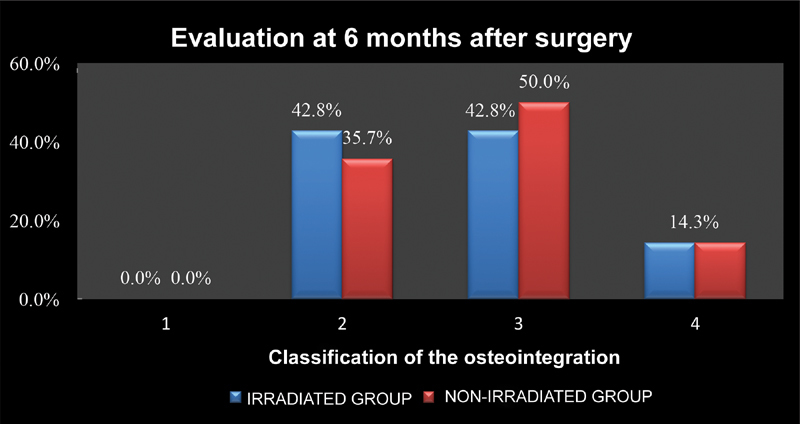
Comparison of the osteointegration percentage 6 months after revision hip arthroplasty procedures using irradiated or non-irradiated bone grafts and the Exeter technique. Osteointegration classification: 1- Total graft osteointegration; 2- Partial graft osteointegration; 3- Absence of osteointegration; 4- Inability to evaluate osteointegration.
Fig. 3.
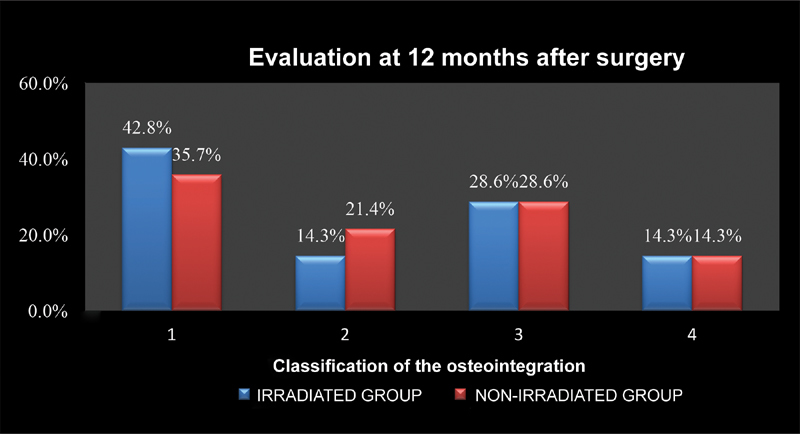
Comparison of the osteointegration percentage 12 months after revision hip arthroplasty procedures using irradiated or non-irradiated bone grafts and the Exeter technique. Osteointegration classification: 1- Total graft osteointegration; 2- Partial graft osteointegration; 3- Absence of osteointegration; 4- Inability to evaluate osteointegration.
Discussion
The Exeter technique has been applied by the hip group of our institution over the last decades. Although not the aim of this study, this technique was well-described by Wilson et al, 14 who evaluated 705 cases with a high success rate (98.8%).
In revision hip arthroplasty surgeries, the first expected event of the biological response after bone transplantation is graft consolidation, as reported by Jasty and Harris. 15 The graft can only consolidate, and, in some circumstances, it can also be integrated into the host bone. Therefore, consolidation and osteointegration are two different processes. Consolidation refers to the blending of the graft and the host bone through the formation of bone between them, whereas osteointegration is the replacement of the graft by the receptor bone through cellular reabsorption and recolonization, resulting in a progressive substitution. 16
The time for the osteointegration process to occur depends on the mechanical stability, the amount of graft used, and the biological response of the recipient. Osteointegration is extremely important for bone stock restoration and longer prosthesis durability. 17
We performed a postoperative retrospective evaluation of 21 patients submitted to revision hip arthroplasty procedures with the Exeter technique using irradiated and non-irradiated grafts. The epidemiological data of these patients, including age and gender, are only descriptive, because the number of cases was insufficient to perform a statistical analysis in this sample. However, Böhm and Bischel 18 reported that there were no differences in graft integration when age, gender, body weight and diagnosis, among other criteria, were evaluated.
There is an intense concern to guarantee tissue quality and to promote the safety of patients receiving homologous tissues regarding the transmission of infectious, contagious diseases. To reduce possible contaminations, serological screening, history and social behavior evaluation, molecular biologic tests to detect RNA from the human immunodeficiency virus (HIV) and hepatitis C virus (HCV), clinical exams and microbiological controls are carried out in bone tissue donors; in addition, the procedures are performed using aseptic techniques. 10 However, contamination during tissue collection, processing, preservation and storage is possible. 19
The microbiological safety of musculoskeletal tissues can be increased with graft sterilization.
Gamma radiation is the most used modality in tissue banks, and it is an effective method to provide terminal sterilization for biological tissues; however, there are reports of the possible deleterious effects on the mechanical and biological properties of the tissues depending on the radiation dose applied. 10 As such, lower radiation doses, ranging from 15 to 25 kGy, are often used, whereas high doses (over 25 kGy) are seldom applied.
Osteointegration analysis through follow-up radiographic images was proposed by Conn et al, 12 who considered that the graft was integrated when the radiodensity between the graft and the recipient bone was identical, with the formation of a continuous trabecular template at the graft–receptor interface; this template denotes a new trabecular pattern according to the loads applied to this region, and it is followed by bone tissue reorganization. Later, Azuma et al 13 considered the graft incorporated when the scleral line at the graft–receptor interface disappeared and normal graft density was restored. Our group decided to associate these definitions to better evaluate bone integration. However, this analysis through radiographic imaging can be subjective and difficult to interpret, especially in the presence of synthetic material, such as metal screens, acetabular reinforcing rings, and screws.
The best technique to prove osteointegration is the histological study of the transplanted graft; however, this technique is not performed routinely, mainly because of its invasiveness. 20 The comparison between osteointegration at 6 and 12 months after transplantation shows significant differences ( p = 0.031), which can be explained by the greater radiological evidences of osteointegration at 12 months.
When we compared the osteointegration between the groups using irradiated and non-irradiated grafts, we did not observe statistically significant differences, but we believe that further studies may determine if the use of irradiated bones with controlled doses of gamma radiation (25 kGy) is as effective in bone reconstructions for revision hip arthroplasty procedures as non-irradiated grafts. These results were also described by Emms et al, 21 who studied the use of irradiated grafts in acetabular reconstructions in medium and long periods of time (2 to 12 years) in 110 patients, and reported good postoperative follow-up results, comparable to those obtained with non-irradiated grafts.
Conclusion
There was no significant difference in the use of irradiated or non-irradiated grafts in revision hip arthroplasties with the Exeter technique
Conflitos de Interesse Os autores declaram não haver conflitos de interesse.
Trabalho desenvolvido no Hospital Central da Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brasil.
Work developed at Hospital Central da Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brazil.
Referências
- 1.Associação Brasileira de Transplantes de Órgãos (ABTO). Registro Brasileiro de Transplantes. Ano XXII n. 4, jan/fev 2016. Disponível em:http://www.abto.org.br/abtov03/default.aspx?mn=457&c=900&s=0
- 2.Halliday B R, English H W, Timperley A J, Gie G A, Ling R S. Femoral impaction grafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg Br. 2003;85(06):809–817. [PubMed] [Google Scholar]
- 3.Zabeu J L, Mercadante M T. Substitutos ósseos comparados ao enxerto ósseo autólogo em cirurgia ortopédica. Revisão sistemática da literatura. Rev Bras Ortop. 2008;43(03):59–68. [Google Scholar]
- 4.Antebi U, Mathor M B, Silva A F, Guimarães R P, Honda E K. Efeitos da radiação ionizante nas proteínas presentes em ossos humanos desmineralizados, liofilizados ou congelados. Rev Bras Ortop. 2016;51(02):224–230. doi: 10.1016/j.rboe.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sutherland C J, Wilde A H, Borden L S, Marks K E. A ten-year follow-up of one hundred consecutive Müller curved-stem total hip-replacement arthroplasties. J Bone Joint Surg Am. 1982;64(07):970–982. [PubMed] [Google Scholar]
- 6.Friedlaender G E, Goldberg V M. Illinois: American Academy of Orthopedic Surgeons; 1991. Bone and cartilage allografts: biology and clinical applications. [Google Scholar]
- 7.Graham N M, Stockley I. The use of structural proximal femoral allografts in complex revision hip arthroplasty. J Bone Joint Surg Br. 2004;86(03):337–343. doi: 10.1302/0301-620x.86b3.14287. [DOI] [PubMed] [Google Scholar]
- 8.Dziedzic-Goclawska A. World Scientific; Singapore: 2000. The application of ionising radiation to sterilise connective tissue allografts; pp. 57–99. [Google Scholar]
- 9.Vastel L, Masse C, Crozier E et al. Effects of gamma irradiation on mechanical properties of defatted trabecular bone allografts assessed by speed-of-sound measurement. Cell Tissue Bank. 2007;8(03):205–210. doi: 10.1007/s10561-006-9030-z. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen H, Morgan D A, Forwood M R. Sterilization of allograft bone: effects of gamma irradiation on allograft biology and biomechanics. Cell Tissue Bank. 2007;8(02):93–105. doi: 10.1007/s10561-006-9020-1. [DOI] [PubMed] [Google Scholar]
- 11.Pekkarinen T, Hietalal O, Jämsä T, Jalovaara P. Gamma irradiation and ethylene oxide in the sterilization of native reindeer bone morphogenetic protein extract. Scand J Surg. 2005;94(01):67–70. doi: 10.1177/145749690509400116. [DOI] [PubMed] [Google Scholar]
- 12.Conn R A, Peterson L F, Stauffer R N, Listrup D. Management of acetabular deficiency: long term results of bone grafting the acetabulum in total hip arthroplasty. Trans Orthop Res Soc. 1985;9:451–452. [Google Scholar]
- 13.Azuma T, Yasuda H, Okagaki K, Sakai K. Compressed allograft chips for acetabular reconstruction in revision hip arthroplasty. J Bone Joint Surg Br. 1994;76(05):740–744. [PubMed] [Google Scholar]
- 14.Wilson M J, Hook S, Whitehouse S L, Timperley A J, Gie G A. Femoral impaction bone grafting in revision hip arthroplasty: 705 cases from the originating centre. Bone Joint J. 2016;98-B(12):1611–1619. doi: 10.1302/0301-620X.98B12.37414. [DOI] [PubMed] [Google Scholar]
- 15.Jasty M, Harris W H. Salvage total hip reconstruction in patients with major acetabular bone deficiency using structural femoral head allografts. J Bone Joint Surg Br. 1990;72(01):63–67. doi: 10.1302/0301-620X.72B1.2298796. [DOI] [PubMed] [Google Scholar]
- 16.Galia C R, Moreira L F.The Biology of Bone Grafts: Recent Advances in Arthroplasty, 2012Samo K. Fokter,IntechOpen, InTech; 235–254.. DOI: 10.5772/27381. [Google Scholar]
- 17.Schreurs B W, Slooff T J, Gardeniers J W, Buma P. Acetabular reconstruction with bone impaction grafting and a cemented cup: 20 years' experience. Clin Orthop Relat Res. 2001;(393):202–215. doi: 10.1097/00003086-200112000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;(420):148–159. [PubMed] [Google Scholar]
- 19.Phillips G O. Singapura: IAEA; 1997. Module 5: Processing. In: Multimedia distance learning package on tissue banking. [Google Scholar]
- 20.Devito F S, Aristides R S, Honda E K, Chueire A G. O uso de enxerto homólogo na revisão de artroplastias do quadril com cimentação do componente acetabular. Acta Ortop Bras. 2006;14(05):280–282. [Google Scholar]
- 21.Emms N W, Buckley S C, Stockley I, Hamer A J, Kerry R M. Mid- to long-term results of irradiated allograft in acetabular reconstruction: a follow-up report. J Bone Joint Surg Br. 2009;91(11):1419–1423. doi: 10.1302/0301-620X.91B11.22274. [DOI] [PubMed] [Google Scholar]