We describe the development of an information sharing system between the EHR and the child welfare database to improve health care delivery for children in custody.
Abstract
There are ∼443 000 children in child protective custody (ie, foster care) in the United States. Children in protective custody have more medical, behavioral, and developmental problems that require health care services than the general population. These health problems are compounded by poor information exchange impeding care coordination. Health care providers often do not know which of their patients are in protective custody and are not privy to the critical social history collected by child protective services, including placement history and maltreatment history. Meanwhile, the custodial child protection agency and designated caregivers (ie, foster caregivers and kinship providers) often lack vital elements of the health history of children in their care, which can result in poor health care delivery such as medication lapses, immunization delay, and poor chronic disease management. In this case study, we address this critical component of health care delivery for a vulnerable population by describing a process of developing an information sharing system between health care and child welfare organizations in collaboration with child protection community partners. Lessons learned include recommended steps for improved information sharing: (1) develop shared community vision, (2) determine shareable information components, (3) implement and analyze information sharing approaches, and (4) evaluate information sharing efforts. A successful example of advocating for improvement of information sharing for youth in protective custody is explored to highlight these steps. In collaboration with child protective services, pediatricians can improve information sharing to impact both health care delivery and child protection outcomes.
When children experience maltreatment and are believed to be unsafe in their homes, child protective services can obtain protective custody and place the child into a temporary alternate living placement (ie, foster care), most often with a nonrelative foster caregiver or a kinship provider.1 Because of a number of factors, including the recent opioid crisis, the number of children in custody has increased from 397 966 in 2012 to 442 995 in 2017,2 resulting in more pediatricians facing caring for the health needs of this vulnerable population. Children in protective custody have increased health problems and poor health compared with children in the general population,1,3–7 in part because of challenges with continuity in health care delivery.3 Even when health care is mandated8 and there are qualified providers to administer health care,9,10 a critical gap in information sharing remains. This gap is likely related to (1) technical barriers, including disparate, fragmented data sources originating from multiple health care providers spanning geography and institutions; (2) data sharing and privacy issues; (3) identifying who should have access to what and when; and (4) lack of funding to support these efforts.
Without information sharing, efficient and high-quality care cannot be provided to this vulnerable population, and the effectiveness of current programs cannot be measured. In Table 1, we provide 2 hypothetical, illustrative case stories to demonstrate the value of information sharing for children in custody.
TABLE 1.
To Describe Some of the Potential Benefits of Improved Data Sharing for Children in Custody, 2 Use Cases That Motivated the Development of IDENTITY Are Described
| Context | Case |
|---|---|
| Hospital provider IDENTITY use | A 5-year-old boy is hospitalized for aggressive behaviors. When he is ready for discharge, his biological mother comes to the hospital, signs his paperwork, and takes him home. After the fact, hospital staff identifies that the child is in protective custody and should not have been discharged to the biological mother. While child protective services is attempting to locate him and his mother, he is physically abused. With IDENTITY, the medical staff could have been alerted that the child was in protective custody with contact information for his child protection worker and precautions could have been taken to ensure safe discharge. |
| Child protection worker IDENTITY use | A 2-year-old girl comes into protective custody because of maternal homelessness and mental health issues. The biological mother surrenders the child with no report of medical problems. When the child is seen in the foster care clinic 5 d later, it is identified that the child received positive test results for HIV, is supposed to be on HIV medications, and is supposed to be on home oxygen after a recent hospitalization with opportunistic pneumonia. Symptoms have worsened by the time the child is evaluated and the medical history is discovered. With IDENTITY, a child protection worker could have looked up the child at the time of placement and identified her medical history, her current medication list, and upcoming medical appointments and prevented a gap in care. |
Technology offers a solution via automated data linkage with secure, accessible sharing of information between community partners. Technology has revolutionized health care in the form of the e-health record (EHR) and has improved child protection through child welfare information databases. Historically, electronic records systems have been siloed; however, linking and sharing data across health care systems has been demonstrated by programs such as health information exchanges.11 Similarly, the Internet-based health record Health Passport,12 implemented in 2008 for the state of Texas, allowed for information exchange between child welfare and health care systems, as did the University of Pittsburgh Medical Center for You Medicaid plan13 implemented in 2008 in Allegheny County, Pennsylvania and Foster Health Link,14 a pilot electronic medical record system developed in Ventura County, California.
Unfortunately, existing solutions were not the right fit for our community, and stakeholders recognized that we needed to create a novel information sharing system that was centralized and easily accessible (ie, Web based). Our children’s hospital had biomedical informatics expertise and the internal funding needed; therefore, our information sharing model was designed to be hospital driven. With this case study, we provide an overview of our system architecture and approach to privacy and data governance concerns to assist teams in other communities in advocating for and leading similar endeavors. We also provide initial system metrics and highlight successes of our program to date.
Methods and Processes
In 2018, there were 7601 reports screened in for investigation by Hamilton County Job and Family Services (ie, children’s services; HCJFS). Of those, 3407 children were placed in out-of-home care, a placement rate of 18.1 per 1000 children in Hamilton County, Ohio. Children in custody on July 1, 2018, were 50% African American and ranged from age 0 to 21 (38% <6 years of age; 33% ≥12 years of age). Top reasons for placement included physical abuse (20%), dependency (19%), and neglect (20%). Fifty-three percent were placed in nonrelative foster homes, with 27% in kinship homes, 10% in congregate care, and 8% in independent living placements.15
Cincinnati Children’s Hospital Medical Center (CCHMC), a 629-bed level 1 trauma center, has contracted with HCJFS to provide health care for all custody youth through the CCHMC Comprehensive Health Evaluations for Cincinnati’s Kids Foster Care Center at the time of entry into custody and with every placement change,9 ensuring that all custody youth are represented within the CCHMC EHR.
Our data sharing project, Integrated Data Environment to Enhance Outcomes in Custody Youth (IDENTITY), was initially conceived by members of CCHMC. In partnership with HCJFS, a team of clinicians, researchers, informaticians, and application developers proposed a 3-year development plan. Funding was granted through the Cincinnati Children’s Research Foundation, dedicated to support multi-disciplinary initiatives focused on new or expanded clinical, research, or education programs. A 1-year planning grant supported the hospital leadership team in developing the data sharing agreement: a 0.25 full-time equivalent (FTE) child abuse pediatrician, a 0.25 FTE child welfare researcher, and a 0.25 FTE biomedical informaticist. In 2017, a 3-year grant to create IDENTITY was awarded to continue leadership team salary support as well as a 1.0 FTE applications analyst at HCJFS dedicated to the IDENTITY project and $300 000 for the design and build of IDENTITY.
IDENTITY links 2 data sets, the Epic EHR (Epic, Verona, WI) installed at CCHMC in 2008 and the child welfare database State Automated Child Welfare Information System (SACWIS) enacted in Hamilton County, Ohio, in 2008. The US child protection system mandates use of a data collection and reporting system, and Ohio, like 33 other states, uses SACWIS. SACWIS is a comprehensive automated case management tool used to support child protective services and to report data to the Adoption and Foster Care Analysis Reporting System and the National Child Abuse and Neglect Data System.
Conversations among stakeholders frustrated with poor information sharing started in the community as early as 2000, as child protection workers as well as collaborators such as guardians ad litem and court-appointed special advocates became vexed with their inability to get health information for children in custody in a timely manner. The group recognized the need for other potential stakeholders, including health care providers, mental health providers, mentors, caregivers, and health information technology experts and invited them to join the conversation. In Hamilton County, foster caregivers reported that 80% of the time, they received no medical information at all about children at the time of placement.16 The group formalized in 2014, developing a regular quarterly meeting schedule with a goal “to plan and implement an integrated, cross-systems electronic information exchange for the purpose of coordination of mental and physical health care for children and youth in foster care in Hamilton County” (Greater Cincinnati Welfare Data Hub report, unpublished). The formalization of a work group was necessary to ensure that different perspectives were identified and that the project had momentum to move forward.
Shortly thereafter, stakeholders participated in a structured brainstorming session to identify all elements of data that could be shared between child protection and health care systems. Data elements were reduced to the minimum number of unique but necessary items and mapped under themes of (1) demographics useful for linking data across systems; and (2) data, including child protection data, to be shared with the health care system and medical data to be shared with the child protection system. Participants then ranked and prioritized each of these items by significance.
A new legal agreement was designed by hospital attorneys in collaboration with child protection attorneys to support data sharing. A critical item of discussion was that child protective services could only share data on children currently in their custody, so our data sharing approach had to be able to incorporate data regarding new children in custody and drop data for children no longer in custody. It was also determined during the data sharing agreement process that initial access would be limited to HCJFS child protection workers and CCHMC health care providers, with a goal to add additional users in the future.
The first hurdle in building IDENTITY was developing an automatable and scalable solution for linking records between SACWIS and the EHR. If a child was matched incorrectly to health care records, this could have serious consequences such as erroneous health care or inadvertent protected health information disclosures. The IDENTITY matching algorithm identifies a unique SACWIS and EHR potential link through deterministic and nondeterministic matching.17 At the time of testing, 90% of children in HCJFS custody were matched by using deterministic matching, which demonstrated 100% specificity, and 9% were matched by using nondeterministic matching, which demonstrated 99% specificity. The remaining 1% required manual matches or had no match in the EHR. Because nondeterministic matching was not 100% accurate, it was determined that an administrator would review and confirm all nondeterministic matches before EHR data could be revealed in the data portal. A “match dispute” feature was added, allowing any user to dispute a linkage resulting in immediate removal from view pending administrator review.
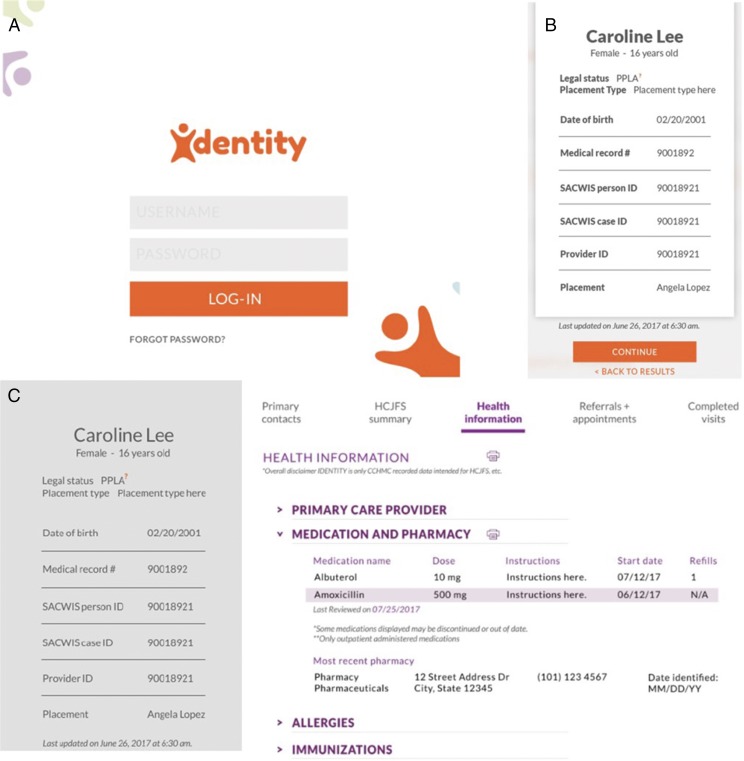
A design firm, Live Well Collaborative, completed 53 interviews with 18 child protection staff and 9 health care providers to determine preferred data display. Tabs on the home screen were identified to allow each user to get to their most prioritized data quickly. Many iterations of a design with feedback from both user types over a 3-month period resulted in a final prototype (Fig 1). Feedback from the final design included comments such as “It looks really intuitive,” “It took 5 minutes to learn how to navigate,” and “This is a marriage between SACWIS and Epic.”
FIGURE 1.
A, Login screen for IDENTITY. B, The child’s case snapshot summary is shown. C, The case summary, child welfare, and EHR data are displayed (health information tab is shown). No true protected health information is included in this figure. ID, identification number; N/A, not available; PPLA, planned permanent living arrangement.
The application architecture and associated data are stored and maintained by CCHMC. Twice daily, a new list of youth and updated related SACWIS data are received from HCJFS via secure file transfer protocol. This list is matched to health care data and replaces the previous list to ensure youth no longer in custody are not displayed. The data are displayed in IDENTITY, which is Web based and stand alone, with automatic logout if inactive for 30 minutes. All data accessed by users is archived to allow for audits in the case of security concerns.
Two login screens are provided for the application on the basis of user type: “Users” and “Administrators.” Most employees were given User access, which allowed a read-only view of the front-facing part of IDENTITY. Users could interact with the application by disputing a match, reporting that they believed a SACWIS record and EHR record appeared incorrectly matched, and could submit questions and suggestions to the support team. “Administrators” were additionally given access to the administrative functions within IDENTITY, allowing them to add and remove users, match SACWIS and EHR records, and respond to disputed matches.
Over time, it was identified that not all users needed access to the same information. Some hospital professionals, including access services (eg, scheduling and registration) and billing professionals did not require access to the child’s social history. To protect privacy as much as possible, IDENTITY QuickView was developed for nonclinical hospital personnel, which eliminates data fields involving social history, maltreatment history, and medical history and retains demographics, health insurance, current custody and placement, and contact information.
Outcomes
The pilot system launched April 9, 2018, with 66 child protection caseworkers and 5 clinicians. Pilot users identified that IDENTITY helped to streamline communication. Health care (including mental health) providers were able to find updated custody and placement information quickly and could get accurate maltreatment history to inform mental health treatment plans. Caseworkers had improved immunization record access to promote faster enrollment in school and up-to-date medical insurance information to improve access to care. Pilot testing concluded in June 2018.
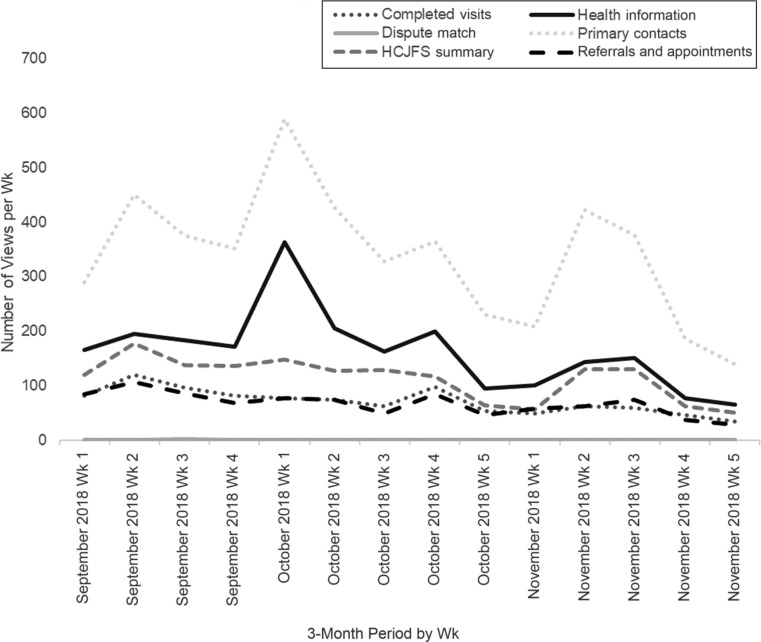
As of November 2018, IDENTITY has spread to 651 users; 365 at HCJFS and 286 at CCHMC. A train-the-trainer approach was used to facilitate spread, and HCJFS trainers began including IDENTITY training as part of new employee orientation. Response to IDENTITY has been overwhelmingly positive, with expansion to a second site underway. At the time of this report, 398 users had accessed the application (62% of HCJFS users and 60% of CCHMC users). An average of 70 users (64% HCJFS and 36% CCHMC) have been accessing IDENTITY weekly, looking at an average of 212 children’s records per week (53% by HCJFS users and 47% by CCHMC users). The most common HCJFS users are frontline caseworkers. The most commonly accessed sections aside from the search function include “Primary Contacts,” which lists the child’s caseworker, supervisor, section chief, guardian ad litem or court-appointed special advocate, and primary care doctor with relevant e-mail addresses and phone numbers and “Health Information,” which displays a child’s diagnoses, allergies, medications, and surgical history (Fig 2). Printing is also tracked because it is believed to represent a proxy for sharing the information with others such as the foster caregiver, and the most commonly printed pages include “Immunizations” and “Health Information.” The adoption and positive response to IDENTITY has been vital to the planned expansion to additional counties and health care institutions.
FIGURE 2.
Features viewed in IDENTITY by week across a 3-month period. For some data, the number of views was stable over time (eg, completed visits and referrals), whereas for other data, frequency of views varied (eg, primary contacts).
Lessons Learned
In this report, we describe the development and implementation of a novel information sharing platform, IDENTITY, for children in protective custody with the goal of improving health care delivery. This is the first successfully implemented linking and near real-time information sharing application for children in custody led by a children’s hospital. Improved data sharing can benefit the nearly 3000 children per year in HCJFS custody through improved health care delivery, with potential expansion to the >5000 children per year with HCJFS involvement. Data sharing initiatives such as IDENTITY may be applicable to other populations such as youth involved with juvenile justice, homeless youth, and other vulnerable populations that touch multiple systems.
Although characteristics of the health care and protective custody systems may vary from place to place, we recommend that others consider 4 components when adapting these efforts in other settings.
Develop Shared Community Vision
The challenge of information sharing between the health care system and child protection must be recognized by all collaborators. The health care and child protection systems must recognize the limitations in the current system as well as the harmful impact lack of information sharing has on children in custody. This will create the impetus for additional improvements and next steps.
Determine Shareable Information Components
Agreeing on the need for information exchange is typically straightforward; however, deciding on what data elements should be shared and how to most efficiently share information can be challenging. Attempting to share too much information may result in an unwieldy tool that makes the most important pieces impossible to identify. Caseworkers, who are not medical experts, might entirely miss the important diagnoses and recommendations when they receive a copy of the complete medical record for a child without structure and prioritization. A health care provider would equally struggle to effectively make use of a complete child protection system record within the context of a primary care encounter. Similarly, sharing too little information can be a waste of valuable resources, particularly if it is insufficient to help with decision-making for caseworkers and health care providers. To find the right balance for the project, it is essential that all perspectives be included to answer the questions of (1) what pieces of information should be shared, (2) what pieces of information can be shared, and (3) how to prioritize needs and strive to identify the minimum necessary elements.
After data elements are identified, the next crucial step is a data sharing agreement. This can be time-consuming and was 1 of the most challenging pieces for our team, taking nearly 1 year to get into place. Having early formal consultation with legal representation can be beneficial to ensure the project moves forward smoothly and that each partner feels recognized and engaged. This is also an opportunity to develop shared language and improved communication between community partners.
Implement, Analyze, and Sustain Information Sharing Approaches
Involving biomedical informatics and information technology experts early in planning for novel data sharing applications will make implementation easier and can improve system design because they will have a clear grasp of the shared vision, have had an opportunity to explore options from the environmental scan, and will know the discrete elements of data that need to be shared.
For a new information sharing technology to be successfully employed, it must be intuitive and user-friendly. Because information is shared across disciplines, it is critical that definitions be incorporated into the data sharing platform to avoid miscommunication. For example, displaying the legal status of a planned permanent living arrangement may be obvious to a child protection worker but could mean nothing to a pediatrician, and similarly, sharing a laboratory result without context is not beneficial to a caseworker.
Finally, sustainability must be considered at the outset and should include all collaborators. With IDENTITY, sustainability occurred in 3 primary forms: (1) demonstrating hospital-based value through improved care delivery and cost savings, (2) demonstrating child welfare-based value through improved staff productivity and child well-being, and (3) communicating impact to organizational and government leaders to support ongoing investment and public-private partnership. For IDENTITY, this is being accomplished through a strong evaluation plan.
Evaluate Information Sharing Efforts
At each step of the process, careful evaluation is a necessity to ensure what is being developed aligns with the original shared vision of the stakeholders. Therefore, it is critical that stakeholders participate from conception all the way through rollout. Evaluation metrics may include usage metrics (eg, number of users and number of records accessed), user satisfaction (eg, qualitative feedback), health outcomes (eg, immunization rates and appointment completion rates), and child welfare outcomes (eg, placement stability).
Creating a novel information sharing application for health care providers and community partners comes with challenges. Building a data portal is costly and will require secure funding streams. Health care providers looking to create a program like this are encouraged to leverage funding from all sources, both intra- and extramural. We believe that our work creating such a system can be directly applied to other systems looking to accomplish similar goals thereby decreasing costs. In the next 2 years, we will be spreading the IDENTITY system to a second hospital system and county child welfare organization in Ohio and plan to evaluate the reduction in startup costs while beginning the commercialization process. In addition, there is opportunity for direct health care cost amelioration with decreased no-show rates and more timely and accurate communication of health insurance information to improve hospital billing practices.
It is important to note that data sharing applications will still have limitations, which can create opportunities for improvement. The IDENTITY system currently does not have integration into the EHR and SACWIS, resulting in the necessity for dual logins, and does not allow for communication within the application. Additionally, user uptake in a new system can be a barrier to implementation. At the time of this report, although there has been significant uptake of IDENTITY, only 61% of individuals with access are using the system regularly. In the final year of this grant, user uptake will be a focus and will be addressed by interviews and focus groups with high and low users to add additional features and updates, such as creating an EHR flag to alert CCHMC users that a child is in custody and has information available in IDENTITY.
Poor information exchange has been widely recognized to be a problem for this population, resulting in poor outcomes for children and financial burdens for health care systems and child protection system alike. We have begun using IDENTITY to identify redundancies and errors between the 2 data systems (eg, different last names). Funders have been eager to see this project come to fruition and have been interested in expansion to other geographic areas as well as other data sets, such as education and court data. Adding features such as reminders about overdue follow-up and unscheduled referrals is another goal. Additional evaluation is necessary to measure the impact of IDENTITY on outcomes such as health status, missed appointments, Medicaid billing practices (eg, identification of new Medicaid number and timely billing), placement stability, caregiver confidence in health management, and child protection worker efficiency.
Conclusions
Children in custody have worse health status compared with the general population in part because of poor information sharing between the health care system and the child protection system. It is possible to use technology to improve information sharing between 2 different system by linking, merging, and displaying information from 2 data sets, displayed in this report by the work on the IDENTITY data sharing system. To successfully advocate for improved information sharing, it is important to start with a shared vision from community stakeholders, identify information needed across systems, analyze and implement a data sharing approach, and evaluate the information sharing efforts.
Acknowledgments
We thank Kristine Flinchum and HCJFS for their efforts and support of this project as well as Jay Gholap for his work obtaining data on usage for the results. We also thank Dr. Judy Harmony for her work in the community gathering stakeholders and preparing the Greater Cincinnati Child Welfare Data Hub report. We also acknowledge the efforts of Saad Jaka, Heather Gragg, Hannah Kramer, and Kelsey Reichert from the Xavier University Health Services Administration for background research.
Glossary
- CCHMC
Cincinnati Children’s Hospital Medical Center
- EHR
e-health record
- FTE
full-time equivalent
- HCJFS
Hamilton County Job and Family Services
- IDENTITY
Integrated Data Environment to Enhance Outcomes in Custody Youth
- SACWIS
State Automated Child Welfare Information System
Footnotes
Drs Greiner, Beal, and Dexheimer, Mr Divekar, Mr Patel, and Dr Hall made substantial intellectual contributions in drafting the article and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funding was secured from the Academic Research Committee at Cincinnati Children’s Hospital Medical Center and through the National Center for Advancing Translational Sciences of the National Institutes of Health under award number 1UL1TR001425-01. Dr Beal’s time was supported through a grant award from the National Institutes of Health 1K01DA041620-01A1. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Beal SJ, Greiner MV. Children in nonparental care: health and social risks. Pediatr Res. 2016;79(1–2):184–190 [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau The AFCARS report. Preliminary FY 2017 estimates as of August 10, 2018. 2018. Available at: https://www.acf.hhs.gov/sites/default/files/cb/afcarsreport25.pdf. Accessed June 13, 2019
- 3.Council on Foster Care; Adoption, and Kinship Care; Committee on Adolescence, and Council on Early Childhood . Health care issues for children and adolescents in foster care and kinship care. Pediatrics. 2015;136(4). Available at: www.pediatrics.org/cgi/content/full/136/4/e1131 [DOI] [PubMed] [Google Scholar]
- 4.Jee SH, Simms MD. Health and well-being of children in foster care placement. Pediatr Rev. 2006;27(1):34–36 [DOI] [PubMed] [Google Scholar]
- 5.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2000;106(4 suppl):909–918 [PubMed] [Google Scholar]
- 6.Chernoff R, Combs-Orme T, Risley-Curtiss C, Heisler A. Assessing the health status of children entering foster care. Pediatrics. 1994;93(4):594–601 [PubMed] [Google Scholar]
- 7.Stein RE, Hurlburt MS, Heneghan AM, et al. Chronic conditions among children investigated by child welfare: a national sample. Pediatrics. 2013;131(3):455–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell KA, Thomas AM, Cook LJ, Keenan HT. Longitudinal experiences of children remaining at home after a first-time investigation for suspected maltreatment. J Pediatr. 2012;161(2):340–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greiner MV, Beal SJ. Developing a health care system for children in foster care. Health Promot Pract. 2018;19(4):621–628 [DOI] [PubMed] [Google Scholar]
- 10.Task Force on Health Care for Children in Foster Care, American Academy of Pediatrics Fostering health: health care for children and adolescents in foster care. 2005. Available at: www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-foster-care-america/Documents/FosteringHealthBook.pdf. Accessed July 6, 2017
- 11.Vest JR, Gamm LD. Health information exchange: persistent challenges and new strategies. J Am Med Inform Assoc. 2010;17(3):288–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centene Corporation Health passport. 2018. Available at: https://www.fostercaretx.com/for-providers/health-passport.html. Accessed August 31, 2018
- 13.Mamula KB. UPMC Health Plan part of pilot program to improve foster kids’ care. Pittsburgh Business Times January 19, 2007. Available at https://www.upmchealthplan.com/pdf/NewsPdf/2007_01_19_PBT.pdf. Accessed June 14, 2019
- 14.Foster VC Kids Foster health link. 2015. Available at: http://fostervckids.org/fhl/. Accessed June 13, 2019
- 15.Public Children Services Association of Ohio The 2018–2019 Public Children Services Association of Ohio factbook, Hamilton County profile. 2019. Available at: www.pcsao.org/pdf/factbook/2019/Hamilton.pdf. Accessed June 13, 2019
- 16.Greiner MV, Ross J, Brown CM, Beal SJ, Sherman SN. Foster caregivers’ perspectives on the medical challenges of children placed in their care: implications for pediatricians caring for children in foster care. Clin Pediatr (Phila). 2015;54(9):853–861 [DOI] [PubMed] [Google Scholar]
- 17.Dexheimer JW, Beal SJ, Divekar P, Hall ES, Patel V, Greiner MV. Automated patient matching for electronic health record and child welfare databases [published online ahead of print March 12, 2019]. J Technol Hum Serv. doi: 10.1080/15228835.2019.1578327 [DOI] [PMC free article] [PubMed] [Google Scholar]