Abstract
To catalyze national scale up of PrEP for HIV serodiscordant couples in public health facilities in Kenya, the Partners Scale-Up Project, using a two-day case-based interactive curriculum, trained health care providers working in 24 high volume facilities in central and western Kenya on PrEP service delivery. Using a standardized test with questions about PrEP and antiretroviral-based HIV prevention we assessed gain in knowledge and confidence gain by comparing pre-and post-training test scores. We explored experiences of the training through key informant interviews after clinics started delivering PrEP. Of 716 health care providers trained, 235 (32.9%) were nurses, 144 (20.2%) were clinical officers and 155 (21.7%) were HIV counsellors. There was a significant improvement between the means of pre-test and post-test scores (61.7% (SD 17.4) vs 86.4% (SD 12.7) p<0.001). The proportion of those who reported being ‘very comfortable’ providing care to HIV serodiscordant couples increased from 22.8% to 67.3% (p<0.001). Key themes that training increasing both knowledge of PrEP and confidence to deliver PrEP to HIV serodiscordant couples emerged from interviews. This short, standardized training resulted in a substantial increase in knowledge of PrEP and in the confidence of the health providers to provide PrEP to HIV serodiscordant couples.
Trial registration:
Keywords: PrEP scale up, HIV serodiscordant couples, public HIV care clinics, health care providers, training, Kenya
Introduction
Pre-exposure prophylaxis (PrEP), in which HIV uninfected persons use an antiretroviral medication to avoid acquiring HIV, is highly effective in preventing HIV (Baeten et al., 2012; Choopanya et al., 2013; Grant et al., 2010; Thigpen et al., 2012) and demonstration projects have shown that people at risk of acquiring HIV are willing to use PrEP effectively (Baeten et al., 2016; McCormack et al., 2016; Molina et al., 2017). In 2012, the U.S Food and Drug Administration approved the combination of tenofovir disoproxil fumarate and emtricitabine (TDF/FTC) for use as daily PrEP and in 2015 the World Health Organization issued strong recommendations for use of PrEP as a prevention choice for people at substantial risk of HIV infection (World Health Organization, 2015). Many countries are now recommending roll out of PrEP in combination with other HIV prevention approaches for reducing new HIV infections and achieving their HIV prevention targets (National AIDS and STI Control Programme (NASCOP), 2016). For many countries, in order to attain maximal population-level impact of reducing new HIV infections, PrEP will need to be scaled up in public health facilities, in a manner similar to the success of public health delivery of HIV treatment and testing.
For successful roll out of new HIV prevention bio-behavioral interventions such as PrEP, it is critical that health care providers be equipped with knowledge on how to deliver them (Uwimana, Zarowsky, Hausler, & Jackson, 2012; Wynn, Bristow, Ross, Schenker, & Klausner, 2015). Providing accurate information to health care providers through training and mentorship, including how to identify eligible persons and provide culturally appropriate PrEP services, is essential in ensuring successful scale up and integration of PrEP into routine care (Krakower & Mayer, 2016). Surveys done in high-income countries have shown that health care providers, including those working in HIV care clinics, have often been slow to take up prescribing of PrEP (Karris, Beekmann, Mehta, Anderson, & Polgreen, 2014; Krakower et al., 2015; Petroll et al., 2017), with limited knowledge about PrEP identified as a major barrier to prescribing (Krakower & Mayer, 2016; Walsh & Petroll, 2017).
Data on training approaches for health workers in resource-limited settings to deliver PrEP are limited. Within an on-going scale up project, in collaboration with the National AIDS and STI Control Program (NASCOP) of the Ministry of Health in Kenya, we developed PrEP training materials and trained health providers. We triangulate information from various sources to evaluate the adequacy and impact of the training on knowledge gain among the health care providers attending the training and their self-reported efficacy to deliver PrEP to HIV serodiscordant couples.
Context
Kenya has a generalized HIV epidemic and 4.8% of the adult population lives with HIV, with an estimated 50,000 new infections annually (Joint United Nations Programme on HIV/AIDS (UNAIDS), 2017; UNAIDS). Almost 5% of all couples in Kenya are estimated to be in a HIV serodiscordant partnership (i.e., one member is HIV infected and the other uninfected) (National AIDS and STI Control Programme (NASCOP)). In 2016, the Ministry of Health in Kenya issued guidelines that recommended provision of PrEP to people at risk of acquiring HIV including, HIV uninfected persons in HIV serodiscordant partnerships, those with multiple partners, those engaging in transactional sex, those with recent STI diagnosis or those who inject drugs, among others (National AIDS and STI Control Programme (NASCOP), 2016, 2017). Specifically, for HIV serodiscordant couples, it is recommended that PrEP is discontinued when the HIV positive partner achieves viral suppression after initiation of combination antiretroviral therapy, provided there is no other HIV risk in the partnership. In May 2017, the Ministry of Health formally launched PrEP services and HIV clinics in public health facilities were proposed as one of the PrEP delivery avenues. HIV clinics in Kenya serve over one million HIV infected people and provide regular clinical and laboratory monitoring and prophylaxis and treatment of opportunistic infections. While HIV prevention services have not been a large component of the work of HIV care clinics, HIV uninfected partners in HIV serodiscordant partnerships have been encouraged to receive risk reduction counselling and HIV testing regularly in these clinics. The staff in the clinics typically includes clinical officers, nurses, pharmaceutical technologists, laboratory technicians, data clerks and HIV testing service providers (U.S. Centers for Diseases Control and Kenya Ministry of Health, 2013).
Theoretical Framework
Our framework (Figure 1) for training evaluation was adapted from two existing frameworks. The consolidated framework of implementation research (CFIR) which has 37 constructs within 5 domains, lays out factors that are considered important for the successful implementation of a new innovation and its integration into routine practice(Damschroder et al., 2009). Training health providers targets the “Characteristics of individuals” domain. We evaluated two constructs within this domain. Knowledge and beliefs about the intervention describes the health providers attitudes and values placed on the intervention and familiarity with the facts and principles related to the intervention. Self-efficacy is the belief that an individual has in their own capacity to perform the activities required to deliver the intervention. Our framework is also an adaptation of the training evaluation framework described by O’Malley et al. where the more immediate outcomes of the training are measured in health care providers but the impact of the training is also observed at the facility level and population level (the last not described in this paper, as the project is ongoing) (O’Malley, Perdue, & Petracca, 2013). The framework also takes into account situational factors at the individual and facility level that may affect both the delivery of the training and of PrEP implementation in the HIV clinics. We posited that by training with an effective PrEP curriculum, health care providers will gain knowledge about PrEP and how to deliver PrEP services in HIV care clinics and will gain confidence in their ability to deliver PrEP. As a result, they will begin to initiate eligible people on PrEP in the facility, leading to adoption of integrated PrEP services in the clinic.
Figure 1.
Training evaluation framework
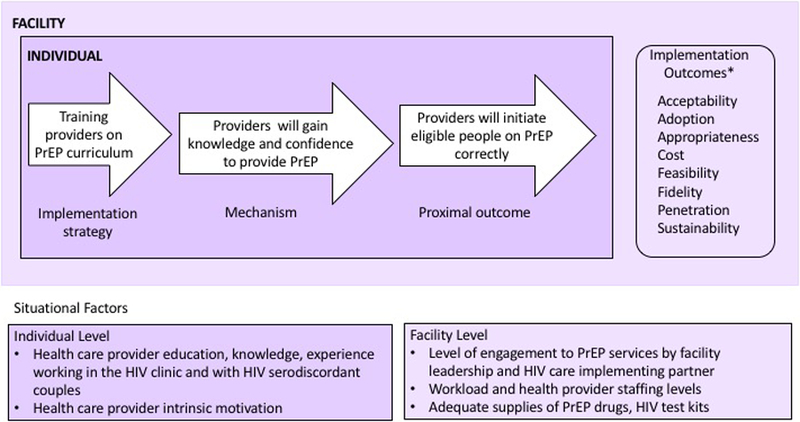
Adapted from “A framework for outcome-level evaluation of in-service training of health care workers”(O’Malley, et al., 2013) *Implementation outcomes are determined at the facility level (Proctor et al., 2011).
Methods
The Partners Scale-Up Project is an implementation science project that aims to catalyze national scale up of PrEP for HIV serodiscordant couples and document facilitators and barriers of PrEP implementation in twenty-four public HIV care clinics in Kerugoya, Kiambu, Murang’a, Nairobi and Nyeri counties of central Kenya and Homa Bay, Kisumu, Migori and Siaya counties of western Kenya (Clinicaltrials.gov ) (Mugwanya et al., 2018). We selected high volume clinics, based on the number of HIV infected clients in active follow up and the number of new clients initiating ART in the facility monthly. Activities for the project include training and providing technical assistance to health workers, without providing additional staffing at facilities or directly altering the existing infrastructure. The findings of this project are anticipated to inform the government process of rolling out PrEP throughout the country.
Development and delivery of training content
The two-day training curriculum was developed by the National AIDS and STI Control Program (NASCOP) in collaboration with implementing partners, who are members of the national PrEP Technical Working Group (TWG). The training curriculum covered topics that are pertinent to tasks performed by health care providers delivering PrEP and included modules on clinical case management of oral PrEP, commodity management for oral PrEP and monitoring and evaluation of PrEP services. Specifically, for the Partners Scale-Up Project training we included a module on HIV treatment as prevention (TasP) and provision of PrEP to the HIV uninfected person in a HIV serodiscordant partnership until the HIV infected partner achieves viral suppression with effective ART use or achieves desired conception. The training included didactic sessions, discussions of case studies, role plays and practical exercises. Topics covered during the training are listed in Table 1. The introduction to a session was done with the entire class and follow up discussions conducted in small groups. The training facilitators were trained project staff, many of whom had worked for the Partners PrEP Study (Baeten, et al., 2012) and/or the Partners Demonstration Project (Baeten, et al., 2016), and hence were experienced in clinic-based delivery of PrEP in research settings.
Table 1:
Topics covered in the two-day PrEP training
| Session 1: Introduction and Course Overview |
| • The purpose, process and logistics of the training were explained |
| • The pre-training test was administered |
|
Session 2: Guidelines on ART |
| • Benefits of ART were explained |
| • Concept of “treatment as prevention” was introduced |
| • Eligibility for ART was discussed |
|
Session 3: Guidelines on PrEP |
| • PrEP was defined |
| • Differences between PEP and PrEP were explained |
| • Benefits and side effects of PrEP were discussed |
|
Session 4: PrEP eligibility and delivery components |
| • PrEP eligibility and contra-indications were described |
| • PrEP service delivery components were discussed |
| • PrEP discontinuation criteria were explained |
|
Session 5: Risk Assessment and Indication for PrEP |
| • Clinic scenario to enhance learning on risk assessment and indication for PrEP |
| • Completion of clinic encounter form |
|
Session 6: Working with Serodiscordant Couples (SDC) |
| • Explained importance of providing quality integrated care to SDC |
| • A couple shared their experience with PrEP and ART |
| • Clinic scenario to enhance learning on initiating PrEP in a SDC |
|
Session 7: PrEP in special circumstances & Commodity management |
| • Clinic scenario to enhance learning on PrEP delivery in pregnancy |
| • Clinic scenario to enhance learning on PrEP commodity management in facilities |
|
Session 8: A male with multiple male sexual partners |
| • Clinic scenario to enhance learning on PrEP delivery among high risk MSM and how to manage seroconversion |
|
Session 9: Clinic flow activity |
| • Participants reflected on integration of PrEP delivery in their facilities and identified appropriate staff and locations for activities involved in PrEP delivery |
|
Session 10: Next steps |
| • Participants described resources and activities required to begin PrEP delivery in their facilities |
| • Post-training test was administered. |
Development of the clinical encounter form
In collaboration with NASCOP and drawing from our experience in delivery of PrEP in clinical trials and demonstration projects we developed the clinical encounter form to facilitate programmatic clinic-based delivery of PrEP (see Appendix file 1). The form has sections for the client’s demographic information, behavioral risk assessment, and medical eligibility. Details at PrEP initiation, including willingness to use, regimen and number of bottles prescribed are documented. On follow-up visits, medical assessments and side effects experienced are recorded. Self-reported adherence, behavioral risk assessments and any follow up tests, including HIV test are also documented. A determination of whether to continue PrEP use is made. The next appointment date is also indicated.
Identification of health care providers for training
Together with management from the health facilities we identified cadres of staff working in the facility who are either likely to come into contact with persons at risk of acquiring HIV and hence eligible for PrEP, or likely to be involved in the PrEP delivery service at the HIV care clinic. HIV clinic managers were included in the training as they would facilitate service provision.
Evaluation of the training
We developed a pre-/post-test that was based on the key concepts that we expected the health providers to learn from the training. Two members of the team came up with an initial fifteen questions. These were presented to the project’s core team who revised the wording on some of the questions and dropped others, leaving ten questions that assessed knowledge of ART and PrEP eligibility, indications, benefits and side effects of PrEP and benefits of attending to couples together (Table 2). There was an additional question to assess how comfortable the providers felt providing care to HIV serodiscordant couples. Prior to the start of the training, participants completed the pre-test and the same tool was administered at the end of the second day of training.
Table 2:
Questions administered in the pre-and post- training test
| 1 | Which of the following people is NOT likely to transmit HIV to their HIV-uninfected partner? |
| a. A man who has a high CD4 and does not want to take ART | |
| b. A woman who has been on ART for 1 month | |
| c. A woman who has been on ART for 5 years and has an undetectable viral load | |
| d. They all have the same likelihood of transmitting HIV | |
| 2 | True or False: All HIV-infected people in Kenya are eligible for ART |
| a. True | |
| b. False | |
| 3 | Which of the following is true about PrEP: |
| a. It is taken daily | |
| b. A person needs to take 7 doses before it is effective | |
| c. A person needs to be confirmed HIV negative | |
| d. All of the above | |
| 4 | A HIV-uninfected person on PrEP is NOT likely to: |
| a. Contract HIV | |
| b. Get resistance | |
| c. Get pregnant | |
| d. Only a & b | |
| e. All of the above | |
| 5 | True or False: PrEP is safe for women to use in pregnancy and breastfeeding. |
| a. True | |
| b. False | |
| 6 | Which of the following is NOT eligible for PrEP: |
| a. Serodiscordant couple, HIV-infected not on ART | |
| b. Serodiscordant couple, HIV-infected on ART trying to conceive | |
| c. An HIV-uninfected person with a habit of having sex while taking alcohol | |
| d. An HIV-uninfected person with signs of acute HIV infection | |
| 7 | PrEP can help some people with the following: |
| a. Prevent HIV | |
| b. Feel more intimate in their relationship | |
| c. Feel empowered | |
| d. All of the above | |
| e. None of the above | |
| 8 | True or False: PrEP should be taken by HIV-uninfected in HIV discordant relationships for the rest of their life, regardless of if the HIV-infected person is on ART. |
| a. True | |
| b. False | |
| 9 | A HIV infected person has a partner. What is the chance that the partner is HIV negative? |
| a. 10% | |
| b. 50% | |
| c. 80% | |
| d. 100% | |
| 10 | Which of the following is NOT an advantage of providing couples-based care: |
| a. Couples hear messages together, allowing for shared understanding | |
| b. Care focuses on the HIV-infected partner only | |
| c. Couples work together to make decisions about treatment and care | |
| d. Both members of couple can engage in risk reduction and prevention decisions | |
Qualitative interviews with 41 health providers involved in PrEP delivery were conducted, using a semi-structured guide to gain a deeper understanding of the PrEP provision process and integration into routine service delivery, after clinics had started PrEP delivery. We purposively sampled providers who attended the training and were involved in PrEP service delivery at the HIV care clinic. The recorded interviews were conducted in English, recorded and transcribed verbatim.
Analysis
A paired t-test was performed to compare pre-test and post-test mean knowledge scores and one-way ANOVA to determine differences in performance by health provider cadre among those who completed both tests. Categorical variables were summarized as proportions and continuous variables as means. To assess the change in comfort health care providers felt in delivering care to HIV serodiscordant couples before and after the training we did a two-sample test of proportions. Statistical analyses were conducted using Stata (StataCorp, College Station, TX). Transcripts from key informant interviews (KII) were analyzed using a combination of inductive and deductive approaches. After development of the codebook, two analysts coded all the transcripts supported by Dedoose software (www.dedoose.com). Inconsistent results were reviewed by the coders until consensus was reached.
Ethics approval and consent to participate
Ethical approval for Partners Scale-Up Project activities was obtained from the University of Washington Human Subjects Division and the Scientific and Ethics Review Unit of the Kenya Medical Research Institute. The pre-and post-test assessments were linked by a number and not the providers’ identifiable information. Written informed consent was obtained for the qualitative interviews.
Results
Between January and July 2017, we conducted 22 trainings sessions among 716 health care providers in central and western regions of Kenya. Of those trained, 235 (32.9%) were nurses, 144 (20.2%) were clinical officers and 155 (21.7%) were HIV counsellors. The total number of health care providers who completed the pre-test and post-test assessment was 605 (84.5%) and 652 (91.1%) respectively. Three-quarters (541(75.6%)) of the participants did both assessments.
Pre-training knowledge:
On the pre-training test, the mean score was 61.7% (standard deviation [SD] 17.4). Health providers had a mean score above 80% on questions related to eligibility for ART, safety of PrEP in pregnancy and breastfeeding and on the advantages of providing couples-based care (Figure 2). There were knowledge gaps in topics related to treatment as prevention, prescribing PrEP, additional benefits of PrEP and the prevalence of HIV discordance among HIV infected persons in stable partnerships.
Figure 2.
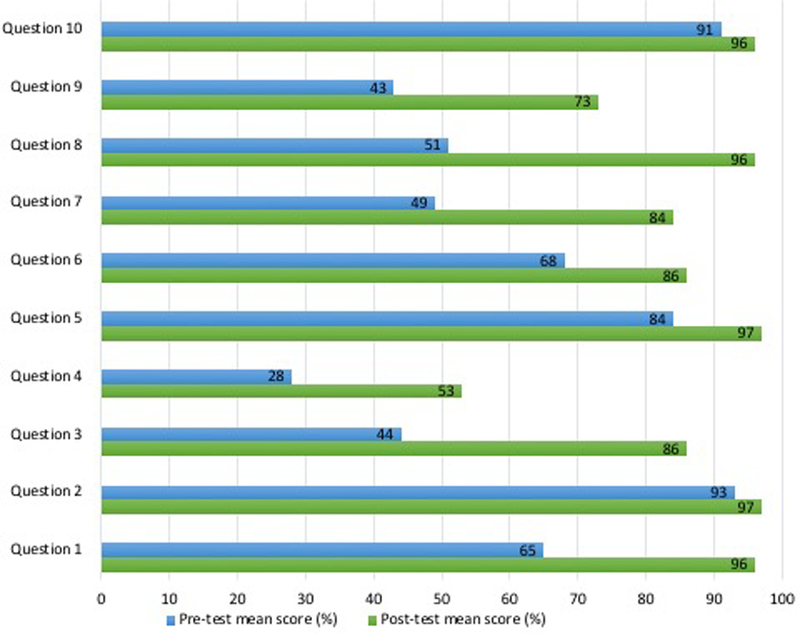
Mean pretest and posttest scores, by question
Knowledge gain
The mean post-test score was 86.4% (SD 12.7). Clinical officers, pharmacy staff and the managers had the highest (>90%) post-test mean scores (Table 3). There was an overall increase of 24.7% (95% CI 23.3%−26.1%, p<0.001) in the mean scores among those who completed both the pre-test and post-test evaluations. This improvement was observed across all cadres, however laboratory technicians and data staff had the greatest increase in mean scores between the pre-test and post-test assessment. Additionally, for all questions in the evaluation, comparing the pre-test and post-test there was a statistically significant increase in the proportion of participants who marked the correct responses (Figure 2).
Table 3:
Pretest and Posttest mean scores, by cadre
| Cadre | N = 714* n (%) |
Pre-test mean (95% CI) scores (n = 540**) |
Post-test mean (95% CI) scores (n = 540**) |
|---|---|---|---|
| Nurse | 235 (32.9) | 62.5 (59.9, 65.1) | 88.4 (86.7, 90.0) |
| HIV Counselor | 155 (21.7) | 57.7 (55.0, 60.4) | 80.2 (77.6, 82.8) |
| Clinical Officer | 144 (20.2) | 70.0 (67.1, 72.9) | 90.5 (88.6, 92.3) |
| Pharmacy | 39 (5.5) | 69.7 (64.0, 75.4) | 90.7 (87.5, 94.4) |
| Data Officer | 39 (5.5) | 47.9 (40.9, 54.7) | 80.0 (75.3, 84.7) |
| Laboratory Technician | 35 (4.9) | 55.9 (49.3, 62.6) | 88.6 (83.1, 94.2) |
| Manager | 21 (2.9) | 66.2 (53.4, 78.9) | 93.1 (86.8, 99.3) |
| Other | 46 (6.4) | 52.4 (47.7, 57.0) | 82.4 (77.3, 87.4) |
The change between the pre-test and post-test mean scores was statistically significant (P<0.001) for all cadres.
2 individuals were missing cadre data
540 trainees completed both pre- and post-tests and had complete data
Efficacy providing care to SDC
When asked the question “How comfortable do you feel providing care to an HIV serodiscordant couple”, close to a third (160 [29.6%]) of providers reported being very uncomfortable, uncomfortable or unsure prior to training. This reduced to 63 (11.7%) after the training (Figure 3). The proportion of providers who reported being ‘very comfortable’ providing care to HIV serodiscordant couples increased from 119 (22.8%) to 363 (67.3%) (p<0.001) after the training.
Figure 3.
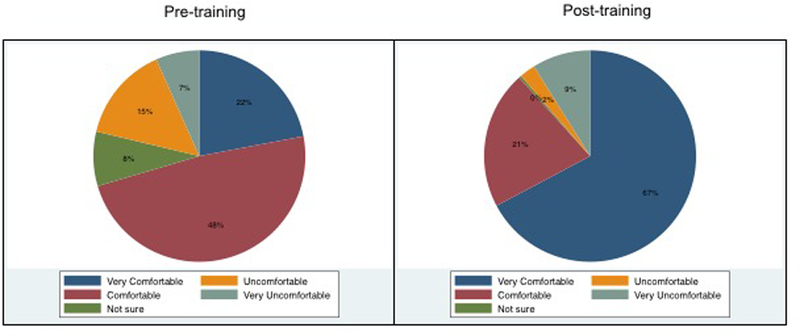
Comfort of health providers to provide care to HIV serodiscordant couples
Experiences and Adequacy of the training
Results from the key informant interviews also reflected increased knowledge of PrEP. They stated that misconceptions they may have had about PrEP were addressed during the training.
“..my concerns were tackled during the training, the concern that I was having about resistance and the sensitization of the clients about the drug. Those kinds of things that were not clear about the exposure to the drug I think they were made clear during the training.” (KII, Counsellor)
“…some healthcare workers who had an issue because they were thinking that now it [PrEP] will increase the spread because people are now going to start having condom-less sex, so I think those were myths that were ironed out in the training that happened.” (KII, Social worker)
The training also gave providers the confidence to start identifying persons eligible for PrEP and provide PrEP services in their HIV care clinics.
“….. immediately we did the training…, we started talking to the clients that we were meeting …. we started talking to them about issues related to PrEP especially to those who have an indication for PrEP ….” (KII, Clinical officer)
“personally, I have been able to embrace it [PrEP] with the experience and also the training that we had so we are able to practice...” (KII, Clinical officer)
However, the interviewees requested that more health care providers be trained on PrEP delivery. They stated that providers who had not attended the training were not comfortable and willing to provide PrEP. PrEP work in the HIV care clinics was left to those persons who had attended the training and they felt overwhelmed. Training additional providers would ease their work load, reduce waiting time for the clients coming for PrEP service and facilitate faster integration into routine service delivery.
“my wish is that everybody to undergo that PrEP training so that in the whole CCC [clinic] set up we can be comfortable with handling these clients” (KII, Nurse)
“…more information on PrEP, more training to everyone so that more people can embrace it …. if everybody gets the knowledge and full information about PrEP delivery, it will be integrated …” (KII, Nurse)
Discussion
Within the on-going national scale up of PrEP delivery for HIV serodiscordant couples in Kenya, a two-day case-based interactive training curriculum resulted in a significant increase in knowledge gain and confidence by all cadres to deliver PrEP services to HIV serodiscordant couples in public HIV care clinics. To our knowledge this is the first evaluation of a national PrEP training curriculum for health care providers in a resource-limited country.
The CFIR framework proposes that health providers with adequate knowledge and familiarity with the facts, principles and truths about the intervention may be more likely to facilitate its integration into routine practice. Additionally, providers who believe that they are able to deliver PrEP will be more likely to do so and result in positive implementation outcomes. Other program interventions have reported that self-efficacy and knowledge and beliefs about the intervention influenced uptake and integration of interventions into routine care (Edelman et al., 2016; Garbutt et al., 2018; Shoemaker, Curran, Swan, Teeter, & Thomas, 2017).
As expected health care providers had a dearth of knowledge on indications, eligibility and duration of PrEP use prior to the training. In HIV serodiscordant couples, PrEP interfaces with ART use for treatment and prevention; we found that despite release of Kenyan guidelines on use of ART for treating and preventing HIV infection a year prior to the training more than a third of the health care providers failed to respond to the question addressing the concept of treatment as prevention correctly on the pre-test and during the training we observed that many were surprised to learn that with viral suppression the risk of HIV transmission is minimal (National AIDS and STI Control Programme (NASCOP), 2016).
Health care workers reported that the training was adequate in preparing them to deliver PrEP. Some participants at the training were based in departments other than the HIV care clinic and thus not expected to be actively involved in providing PrEP services. It is likely that the entire team at the HIV care clinic could not be released to attend the two-day training as this would interfere with delivery of care and treatment services at the clinic. There is therefore need to train additional providers involved in PrEP delivery and possibly use alternative training strategies (Chien et al., 2016; Kang et al., 2014; Spach et al., 2016). For instance, the training curriculum could be broken down into modules that can be delivered in the facility, to those who will be actively involved in PrEP, at a time that is convenient for the health facility.
Triangulation of information from different data sources strengthened our ability to evaluate the impact and adequacy of the training. A limitation of this evaluation is that we did not assess retention of knowledge and skills after the training or the effect of training on quality of PrEP service delivery. Additionally, this analysis was done based on information in the pre-and post-test forms. The forms did not collect demographic information or any other factors, beyond cadre, that may influence performance on the pre-and post-test kits. Nevertheless, the range of staff cadres reflects the spectrum of care providers in public clinics in Kenya, making the lessons learned broadly generalizable to that country and more generally to eastern and southern Africa as well.
This short interactive training approach resulted in an increase in the knowledge and self-reported comfort of health care providers to provide PrEP as part of a combination treatment and prevention package to HIV serodiscordant couples and can be utilized by programs in the region to ignite PrEP delivery in HIV care clinics within public health facilities.
Supplementary Material
Appendix 1: Clinical Encounter Form.
Acknowledgements
We are grateful to the staff in all the participating HIV care clinics.
The Partners Scale-Up Project trainers: Josephine Odoyo, Elizabeth Wamoni, Merceline Awuor, Annabel Dollah, Peter Michira, Peter Mogere, Sylvia Mugalla, Euticus Mwangi, John Njoroge, Bernard Nyerere, Joel Odondi, Fernandos Ongolly, Meresa Oyier.
Funding
The Partners Scale-Up Project is supported by the National Institute of Mental Health of the US National Institutes of Health under grant R01 MH095507 and the Bill & Melinda Gates Foundation under grant OPP1056051.
Footnotes
Competing interests
The authors declare they have no competing interests
References
- Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. (2012). Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New England Journal of Medicine, 367(5), 399–410. doi: 10.1056/NEJMoa1108524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeten JM, Heffron R, Kidoguchi L, Mugo NR, Katabira E, Bukusi EA, et al. (2016). Integrated Delivery of Antiretroviral Treatment and Pre-exposure Prophylaxis to HIV-1-Serodiscordant Couples: A Prospective Implementation Study in Kenya and Uganda. PLOS Medicine, 13(8), e1002099. doi: 10.1371/journal.pmed.1002099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien E, Phiri K, Schooley A, Chivwala M, Hamilton J, & Hoffman RM (2016). Successes and Challenges of HIV Mentoring in Malawi: The Mentee Perspective. PLOS One, 11(6), e0158258. doi: 10.1371/journal.pone.0158258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. (2013). Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet, 381(9883), 2083–2090. doi: 10.1016/s0140-6736(13)61127-7 [DOI] [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, & Lowery JC (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science, 4, 50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Hansen NB, Cutter CJ, Danton C, Fiellin LE, O’Connor PG, et al. (2016). Implementation of integrated stepped care for unhealthy alcohol use in HIV clinics. Addiction Science & Clinical Practice, 11(1), 1. doi: 10.1186/s13722-015-0048-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbutt JM, Dodd S, Walling E, Lee AA, Kulka K, & Lobb R (2018). Barriers and facilitators to HPV vaccination in primary care practices: a mixed methods study using the Consolidated Framework for Implementation Research. BMC Family Practice, 19(1), 53. doi: 10.1186/s12875-018-0750-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine, 363(27), 2587–2599. doi: 10.1056/NEJMoa1011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2017). UNAIDS DATA 2017 [PubMed] [Google Scholar]
- Kang H, Yip B, Chau W, Nohpal De La Rosa A, Hall D, Barrios R, et al. (2014). Continuing professional development in HIV chronic disease management for primary care providers. Medical Teacher, 1–4. doi: 10.3109/0142159x.2014.970623 [DOI] [PubMed] [Google Scholar]
- Karris MY, Beekmann SE, Mehta SR, Anderson CM, & Polgreen PM (2014). Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clinical Infectious Diseases, 58(5), 704–712. doi: 10.1093/cid/cit796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakower DS, & Mayer KH (2016). The role of healthcare providers in the roll out of preexposure prophylaxis. Current Opinion in HIV and AIDS, 11(1), 41–48. doi: 10.1097/coh.0000000000000206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakower DS, Oldenburg CE, Mitty JA, Wilson IB, Kurth AE, Maloney KM, et al. (2015). Knowledge, Beliefs and Practices Regarding Antiretroviral Medications for HIV Prevention: Results from a Survey of Healthcare Providers in New England. PLOS One, 10(7), e0132398. doi: 10.1371/journal.pone.0132398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. (2016). Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet, 387(10013), 53–60. doi: 10.1016/s0140-6736(15)00056-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina JM, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. (2017). Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. The Lancet HIV, 4(9), e402–e410. doi: 10.1016/s2352-3018(17)30089-9 [DOI] [PubMed] [Google Scholar]
- Mugwanya KK, Irungu E, Bukusi E, Mugo NR, Odoyo J, Wamoni E, et al. (2018). Scale up of PrEP integrated in public health HIV care clinics: a protocol for a stepped-wedge cluster-randomized rollout in Kenya. Implementation Science, 13(1), 118. doi: 10.1186/s13012-018-0809-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National AIDS and STI Control Programme (NASCOP). Kenya AIDS Indicator Survey 2012: Final Report Nairobi Kenya, NASCOP. [Google Scholar]
- National AIDS and STI Control Programme (NASCOP). (2016). Guidelines on Use of Antiretroviral Drugs for Treating and Preventing HIV Infections in Kenya
- National AIDS and STI Control Programme (NASCOP). (2017). Framework for the Implementation of Pre-exposure Prophylaxis of HIV in Kenya Nairobi, Kenya. [Google Scholar]
- O’Malley G, Perdue T, & Petracca F (2013). A framework for outcome-level evaluation of in-service training of health care workers. Human Resources for Health, 11, 50. doi: 10.1186/1478-4491-11-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, & Kelly JA (2017). PrEP Awareness, Familiarity, Comfort, and Prescribing Experience among US Primary Care Providers and HIV Specialists. AIDS and Behaviour, 21(5), 1256–1267. doi: 10.1007/s10461-016-1625-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. (2011). Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health, 38(2), 65–76. doi: 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoemaker SJ, Curran GM, Swan H, Teeter BS, & Thomas J (2017). Application of the Consolidated Framework for Implementation Research to community pharmacy: A framework for implementation research on pharmacy services. Research in Social and Administrative Pharmacy, 13(5), 905–913. doi: 10.1016/j.sapharm.2017.06.001 [DOI] [PubMed] [Google Scholar]
- Spach DH, Wood BR, Karpenko A, Unruh KT, Kinney RG, Roscoe C, et al. (2016). Creating a National HIV Curriculum. Journal of the Association of Nurses AIDS Care, 27(3), 261–273. doi: 10.1016/j.jana.2016.02.002 [DOI] [PubMed] [Google Scholar]
- Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. (2012). Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. New England Journal of Medicine, 367(5), 423–434. doi: 10.1056/NEJMoa1110711 [DOI] [PubMed] [Google Scholar]
- U.S. Centers for Diseases Control and Kenya Ministry of Health. (2013). Report of a Cost Study of HIV Treatment Programs in Kenya Atlanta, GA (USA) and Nairobi, Kenya. [Google Scholar]
- UNAIDS. Country factsheets. Kenya 2017 Retrieved October 21, 2018, from http://aidsinfo.unaids.org/
- Uwimana J, Zarowsky C, Hausler H, & Jackson D (2012). Training community care workers to provide comprehensive TB/HIV/PMTCT integrated care in KwaZulu-Natal: lessons learnt. Tropical Medicine & International Health, 17(4), 488–496. doi: 10.1111/j.1365-3156.2011.02951.x [DOI] [PubMed] [Google Scholar]
- Walsh JL, & Petroll AE (2017). Factors Related to Pre-exposure Prophylaxis Prescription by U.S. Primary Care Physicians. American Journal of Preventive Medicine, 52(6), e165–e172. doi: 10.1016/j.amepre.2017.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2015). Guidelines on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV [PubMed]
- Wynn A, Bristow CC, Ross D, Schenker I, & Klausner JD (2015). A program evaluation report of a rapid scale-up of a high-volume medical male circumcision site, KwaZulu-Natal, South Africa, 2010–2013. BMC Health Services Research, 15, 235. doi: 10.1186/s12913-015-0904-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Clinical Encounter Form.


