Abstract
Background.
Violent injuries are a leading cause of morbidity and mortality among youths. Little is known about adolescents’ patterns of and risk factors for repeat assault injuries, yet understanding who is at risk for repeated assaults is important for intervention and prevention efforts. Investigating these questions in population-based adolescent samples is particularly critical.
Objectives.
To estimate the five-year cumulative incidence of and risk factors for repeat ED visits for assault injury among adolescents experiencing an index assault visit, and compare the method of injury for adolescents’ first and second visits.
Methods.
Statewide, longitudinal data from California was used to follow 17,845 adolescents who reported to an ED with assault-related injuries in 2010. Incidence rate ratios were estimated to examine risk factors for repeat assault injury within one year and five years following the index visit.
Results.
A total of 3,273 (18.3%) of assaulted adolescents experienced ≥1 additional assault injury ED visit over the full follow-up period. Only 37.3% of these repeat assaults occurred within the first year following the index assault. Of adolescents with a repeat assault injury, the method of injury often changed and followed no clear pattern. Sociodemographic characteristics (e.g., older age, Black race) and history of prior ED visits for assault and mental health problems predicted increased risk of repeat assault.
Conclusion.
Previous work may underestimate the rate of repeated assault among adolescents. Adolescents with a history of violence involvement and mental health problems are at elevated risk for repeated assault, and should be targeted for intervention.
Keywords: assault, adolescent, longitudinal, violence
Introduction
Violent injuries are a leading cause of morbidity and mortality among youths. In the United States, homicide is the second leading cause of death among 15-to-19-year-olds, and the fourth leading cause of death among 10–14-year-olds.1 Nonfatal assault-related injuries were responsible for more than 394,000 emergency department visits in 2016 among 10–19-year-olds.2 A national survey of U.S. adolescents found, compared to the general population, assault-injured adolescents are disproportionately likely to be male, of Black or Hispanic race/ethnicity,3 and to live in areas with low socioeconomic status.4 Assaulted adolescents are also more likely than their non-assaulted peers to have had injuries in the past year, including fight-related injuries requiring medical treatment.5
Considerably less is known, however, about adolescents’ patterns of and risk factors for repeat assault injuries, despite evidence that adolescents with serious violence-related injuries are at high risk for subsequent nonfatal or fatal assault injury.4,6 Understanding who is at risk for repeat assaults would allow health professionals to target high-risk adolescents for intervention to prevent future assault injury.
Studies attempting to examine the outcomes and risk factors for assault injury via hospital data typically utilized data from single hospitals located in urban areas. One study from Wisconsin examined health records for 495 patients who visited a Milwaukee emergency department for nonfatal firearm injuries.4 The majority of these patients were male (85%) and Black (82%), and 17% had a prior history of violent injury. They found that individuals who did not receive social worker intervention on their initial visit, and those discharged into police custody, were more likely to have a repeat ED visits due to a violent injury. Another study, conducted in an urban area of Michigan, followed a cohort of 349 assaulted adolescents and 250 non-assaulted adolescents who were treated at a level 1 trauma center for two years.6 Researchers found that female sex, minority race, illicit drug use, and posttraumatic stress disorder at the index visit were predictive of ED recidivism or death from assault-related injuries within 24 months. They also found that 48% of repeaters were injured via the same mechanism as their first visit.
Previous studies utilizing hospital data share a set of common limitations. These studies relied on data from single hospitals, clinics or networks, and followed fewer than 500 assault patients over the course of the study, which limits the generalizability of the findings as well as statistical power.4,6–9 Additionally, these studies all collected data from urban metropolitan areas, again limiting their broader generalizability and ability to examine risk factors of potential interest. For example, while prior research indicates that assault victimization occurs at lower rates in rural communities compared to urban areas, there is no research examining whether urbanicity is associated with risk of repeat assault injury.10 Furthermore, studies from different cities and locations yield conflicting reports of who the at-risk population are.4,6 Lastly, the studies mentioned above are limited in their ability to examine long-term patterns, due to their one- to two-year follow up periods.4,6,7,9
To address these gaps in the literature and provide a population-based assessment of repeat assault injury among adolescents, this study used individual-level emergency department patient data from all licensed hospitals within the state of California to (1) estimate the five-year cumulative incidence and average number of repeat ED visits for assault injury among adolescents experiencing an index assault ED visit, and (2) determine how a broad range of risk factors were associated with adolescents’ risk of experiencing a repeat ED visit for assault injury. Specifically, the risk factors of interest included patient age, race, gender, insurance type, and prior ED utilization for assault injury, drug use, mental health problems, self-harm and alcohol use, as well as whether the patient resided in an urban or rural location. These factors were selected based on evidence from prior literature indicating their potential importance, as well as their availability within the administrative dataset.
Methods
Data
Data from the California Office of Statewide Health and Planning and Development’s (OSHPD) restricted emergency department data (ED) and hospital patient discharge data (PDD) files for the period 2006–2015 were utilized for this study. The ED dataset contains all records of patients treated in a licensed emergency department and discharged or transferred to another facility. PDD data were used to identify patients treated in an emergency department and admitted directly for inpatient treatment at that facility.
The cohort was defined as all adolescents aged 10 to 19 years who made an emergency department visit for assault injury in 2010. Patients who reported living in a zip code outside of the state of California were excluded. To track a patient through time, OSHPD’s “record linkage number” (RLN) was utilized. RLNs are encrypted social security numbers; they are unique to an individual and follow them throughout subsequent hospital encounters anywhere in the state, allowing researchers to track individuals’ utilization of hospital-based services within the state of California both retrospectively and prospectively. Only assault injury visits with an RLN present were included in the study.
Case definition
Assault patients were identified using International Classification of Disease-9th revision, Clinical Modification (ICD-9-CM)11 external cause-of-injury codes (E-codes). Adolescents were classified as assault patients if the primary, secondary, or tertiary ICD-9-CM code for that visit was E960.xx-E968.xx (excluding E960.1 which indicates rape related assault injury). A patient’s first visit for assault injury in the year 2010 was considered his or her index visit. Assault injuries were classified by cause using a five-level categorical variable. This classification used the first listed E-code for assault, and included fight/brawl, firearm, cutting/piercing, child abuse, and all other causes (including assault by caustic substance, poisoning, hanging/strangulation, submersion/drowning, and unspecified means).
Dependent Variable
The outcome of interest was assault patients’ total number of visits to the emergency department for assault injury following their index assault visit, over the follow-up period. Repeat ED assault visits were defined using the same criteria as the index assault (codes E960.xx-E968.xx). Follow-up began the date after each patient’s index visit and ended 365 days after the index visit (for the one-year follow-up period) or on September 30th, 2015 (for the five-year follow-up period). We censored all patient follow-up on Sept. 30, 2015 to avoid injury diagnosis misclassification problems related to the mandatory transition from ICD-9-CM to ICD-10-CM coding on October 1st, 2015.12
Covariates
Age was categorized into two groups based on the patient’s age at their index visit: 10–14 years and 15–19 years. This stratification of age was done because previous research has shown that older adolescents have higher rates of assault compared to younger adolescents.13 Patient sex was classified as male or female. Patient race/ethnicity was based on information provided at the patient’s index visit and grouped into 5 categories: White, Black, Hispanic, Asian/Pacific Islander, and other. Patient insurance status, which is used as a proxy for family socio-economic status, was based on the expected payer at index visit and grouped into 4 categories: private, Medicaid, self-pay, and other.
Patients’ prior emergency department records from 2006 (the earliest year available) to 2009 were then linked to their 2010 record to construct covariates related to prior ED utilization. For each patient, a variable totaling all ED visits they made for any reason in the 4 years prior to 2010 (2006–2009) was created. ICD-9-CM and Clinical Classification Software (CCS) codes were used to identify the conditions that patients presented with at each prior visit. CCS codes aggregate ICD-9-CM diagnoses into discrete, clinically meaningful categories.14 Prior history of assault was classified as having been diagnosed with an external injury code of E960.xx-968.xx (excluding ICD-9-CM code E960.1) within the first three ICD-9-CM diagnoses. Variables were created in the same way for prior ED visit for substance use (CCS codes 660 or 661), mental health condition (CCS codes 650–659, 662, 663, and 670), and deliberate self-harm (ICD-9-CM codes E950.0-E958).
Urbanicity of each patient’s residential zip code was defined using the U.S. Department of Agriculture’s Rural-Urban Commuting Areas (RUCA) 2010 geographic taxonomy, Version 3.10 (collapsed into metropolitan, micropolitan, and small town/rural categories).15 RUCA codes utilize measures of population density, urbanization, and daily commuting patterns to identify zip codes as metropolitan, micropolitan, and small town/rural. Urbanicity was included in the analysis because of documented differences in rates of violence among urban and rural populations.10
Statistical analysis
We first estimated the one- and five-year cumulative incidence and average number of repeat ED visits for assault injury among study adolescents. Because the outcome variable was coded as a count variable negative binomial regression was used to estimate incidence rate ratios (IRRs).16 Akaike information criterion (AIC) and Bayesian information criterion (BIC) fit indices, and the statistically significant dispersion parameters, indicated that negative binomial models were a better fit for the data than Poisson models. Rate ratio models included terms for patient sex, age, race, insurance, total visit count during 2006–2009, and patient histories of prior ED utilization for drug use, alcohol use, mental health conditions, and deliberate self-harm. Two versions of the model were assessed: one estimating risk of repeat assault visits within one year after the index visit in 2010, and a second estimating risk repeat assault through September 30th 2015 (an average of 4.75 years of follow-up). Stata v14 (StataCorp, College Station, TX) was used for all analyses.
Results
Sample characteristics
A total of 17,655 adolescents presented to a California ED with an assault injury in 2010. Demographic characteristics of the study population are shown in Table 1. Among all adolescents who presented to an ED with assault injuries, 68.3% were male, and 84.4% were aged 15–19 at the time of their index assault. A majority of assaulted patients were either Hispanic (41.5%) or White (29.3%). The most common form of insurance used was Medicaid (46.3%), followed by private insurance (30.4%) and self-pay (19.4%). Among these assaulted adolescents, 7.3% had a previous visit to the ED for assault-related injury between 2006 and 2009. A large majority of adolescents reported living in metropolitan zip codes (93.1%), followed by micropolitan (5.2%) and rural (1.8%) zip codes.
Table 1:
Demographic and visit history characteristics among adolescent assault patients in California, 2010.
| Assault Injuries N=17,655 |
||
|---|---|---|
| N | % | |
| Sex at index visit | ||
| Male | 12,062 | 68.32 |
| Female | 5,593 | 31.68 |
| Age category at index visit | ||
| 10–14 | 2,739 | 15.51 |
| 15–19 | 14,916 | 84.49 |
| Race/ethnicity at index visit | ||
| White | 5,172 | 29.29 |
| Black | 3,521 | 19.94 |
| Hispanic | 7,326 | 41.5 |
| Asian | 433 | 2.45 |
| Other | 1,203 | 6.81 |
| Insurance status at index visit | ||
| Private | 5,358 | 30.35 |
| MediCaid | 8,167 | 46.26 |
| Self-Pay | 3,421 | 19.38 |
| Other | 709 | 4.02 |
| Rurality at index visit | ||
| Metropolitan | 16,393 | 93.06 |
| Micropolitan | 907 | 5.15 |
| Small Town/Rural | 315 | 1.79 |
| History of ED utilization, 2006–2009 | ||
| Assault | 1,285 | 7.28 |
| Suicide Attempt | 283 | 1.60 |
| Metal Health | 1,694 | 9.60 |
| substance abuse | 995 | 5.64 |
Fight/brawl was listed as the primary cause in nearly half (48.9%) of the index assault injuries. After fight/brawl, the most common primary causes were cutting/piercing (7.5%), firearms (5.5%), and child abuse (5.1%). Distribution of assault injury types differed by gender, age, and race (Table 2). Males were more likely than females to suffer assault injuries due to fighting, cutting/piercing, and firearms. Conversely, females were more likely than males to sustain assault injuries from child abuse. Black and Hispanic adolescents had a higher proportion of assault injuries caused by firearms (10.5% and 6.0 %, respectively) when compared to White adolescents (1.5%). Among the 3,222 adolescents who had a repeat visit for assault injuries, the cause of the assault injury at the second visit often differed from cause of injury at the index visit (Figure 1). For adolescents with index assault injuries for fights/brawls, cutting/piercing, and all other causes, injuries for fighting/brawling were the most common cause of injury at the second assault visit. However, among adolescents who were injured via firearm at their index visit and who had a second assault visit, firearm injury was the most common single cause of injury (41.2%) at their second visit (Supplemental Table 1).
Table 2:
Type of assault injury at index visit, stratified by patient gender, age, race/ethnicity, and rurality of zipcode.
| Fight/Brawl N=8,632 |
Firearm N=973 |
Cutting/Piercing N=1,319 |
Child Abuse N=901 |
All Other N=5,831 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||||
| Male | 5,956 | 69.0% | 868 | 89.2% | 1,128 | 85.5% | 241 | 26.6% | 3,869 | 66.4% |
| Female | 2,676 | 31.0% | 105 | 10.8% | 190 | 14.4% | 660 | 73.3% | 1,962 | 33.6% |
| Age | ||||||||||
| 10–14 | 1,592 | 18.4% | 45 | 4.6% | 61 | 4.6% | 196 | 21.8% | 845 | 14.5% |
| 15–19 | 7,040 | 81.6% | 928 | 95.4% | 1,258 | 95.4% | 705 | 78.3% | 4,986 | 85.5% |
| Race/Ethnicity | ||||||||||
| White | 2,858 | 33.1% | 78 | 8.0% | 286 | 21.7% | 264 | 29.3% | 1,686 | 28.9% |
| Black | 1,622 | 18.8% | 369 | 37.9% | 204 | 15.4% | 230 | 25.5% | 1,096 | 18.8% |
| Hispanic | 3,343 | 38.7% | 440 | 45.2% | 701 | 53.2% | 316 | 35.1% | 2,526 | 43.3% |
| Asian | 182 | 2.1% | 28 | 2.8% | 36 | 2.7% | 30 | 3.3% | 157 | 2.7% |
| Other | 627 | 7.3% | 58 | 5.9% | 92 | 7.0% | 61 | 6.8% | 366 | 6.3% |
| Rurality | ||||||||||
| Metropolitan | 7,909 | 91.8% | 943 | 97.6% | 1,229 | 93.6% | 848 | 94.1% | 5,464 | 93.9% |
| Micropolitan | 511 | 5.9% | 21 | 2.2% | 67 | 5.1% | 39 | 4.3% | 269 | 4.6% |
| Small Town/Rural | 195 | 2.3% | 2 | 0.2% | 17 | 1.3% | 14 | 1.6% | 87 | 1.5% |
Figure 1.
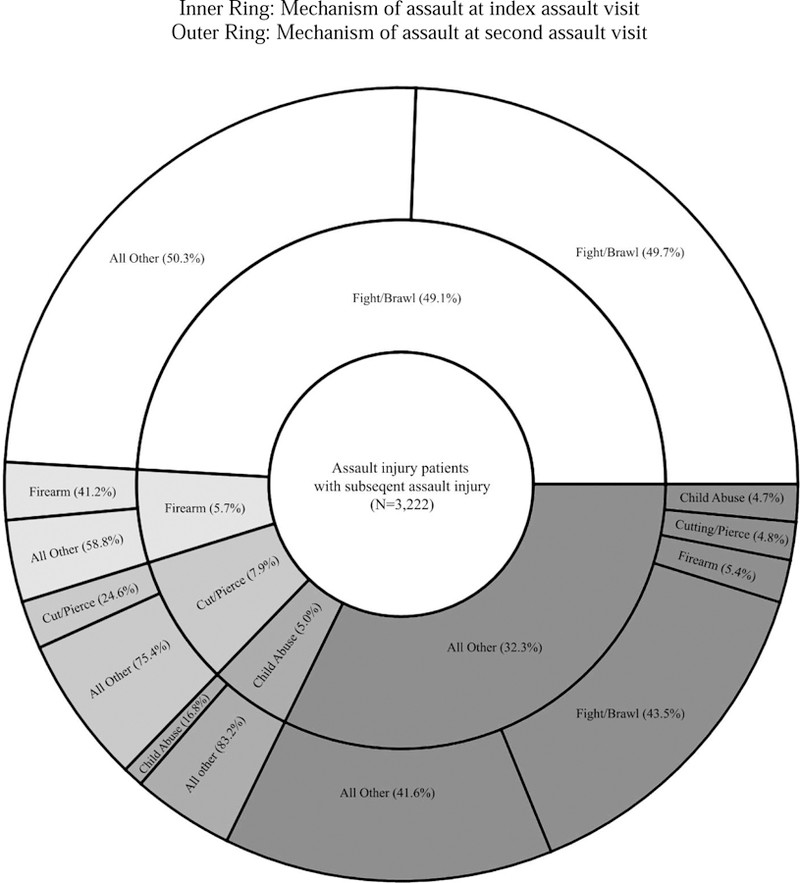
Conjunction between injury mechanism at first and second assault injuries, among adolescent patients with a second assault injury visit
Cumulative incidence and average number of repeat assault visits
Of all the assaulted adolescent ED patients, 1,197 had a repeat assault injury within one year of their index visit (one-year cumulative incidence of 6.8%), and 3,222 adolescents had a repeat assault injury over the entire course of the observation period (five-year cumulative incidence of 18.2%). Of the 18% of adolescents who had any repeat visit for assault injury during follow-up, they averaged 1.41 (SD=0.92, range=1 to 19) visits to the ED between their index visit in 2010 through September 30th, 2015.
Risk factors for repeat assault
Analysis of repeat assault ED visits within the first year, with all predictor variables included in the model, indicated that females were at lower risk than males for any repeat assault (RR= 0.75; 95% CI=0.65, 0.85). Adolescents aged 15–19 years were at 1.85 times higher risk (95% CI=1.50, 2.28) compared to those aged 10–14 years. Compared to White adolescents, Black adolescents were at greater risk (RR=1.29; 95% CI=1.09, 1.53), and Asian/Pacific Islanders were at lower risk (RR=0.57; 95% CI= 0.34, 0.97), for repeat assault. Compared to adolescents with private insurance, adolescents with Medicaid had 1.33 (95% CI=1.15, 1.54) times higher risk of repeat assault injury.
For each additional visit made to the ED between 2006–2009, the patient’s risk of having a repeat assault injury increased by 6% (RR=1.06, 95% CI=1.04, 1.08). Assault patients with a prior history of ED visits for assault or mental health problems were especially likely to present with repeat assault within one year (RR=1.58, 95% CI=1.32, 1.90; and RR=1.66, 95% CI=1.39, 1.97, respectively). Prior history of ED utilization for self-harm and substance use, however, were not associated with risk of repeat assault. Living in a micropolitan or rural environment was also not significantly associated with one-year risk of repeat assault injury.
When examining repeat assault visits through September 30th 2015, risk patterns were similar to the one-year follow-up results (see Table 3). However, in some cases, the magnitude of effect changed. Older age was less strongly associated with repeat assault over the five-year follow-up period (RR=1.27, 95% CI=1.14, 1.42), but the association between prior history of assault and risk of repeat assault grew stronger when examining the entire follow-up period (RR=1.84, 95% CI=1.64, 2.06).
Table 3:
Risk factors for subsequent assault ED visit among adolescents with an index assault visit in 2010.
| One year follow-up | Full follow-up | |||
|---|---|---|---|---|
| RR | (95% CI) | RR | (95% CI) | |
| Sex at index visit | ||||
| Male | ||||
| Female | 0.75 | (0.65, 0.85) | 0.88 | (0.81, 0.95) |
| Age category at index visit | ||||
| 10–14 | ||||
| 15–19 | 1.85 | (1.50, 2.28) | 1.27 | (1.14, 1.42) |
| Race/ethnicity at index visit | ||||
| White | ||||
| Black | 1.29 | (1.09, 1.53) | 1.42 | (1.27, 1.58) |
| Hispanic | 1.12 | (0.97, 1.29) | 1.05 | (0.96, 1.16) |
| Asian | 0.57 | (0.34, 0.97) | 0.42 | (0.28, 0.62) |
| Other | 1.04 | (0.80, 1.35) | 1.07 | (0.91, 1.26) |
| Insurance status at index visit | ||||
| Private | ||||
| Medicaid | 1.33 | (1.15, 1.54) | 1.43 | (1.30, 1.57) |
| Self-Pay | 1.15 | (0.97, 1.37) | 1.17 | (1.04, 1.33) |
| Other | 1.26 | (0.93, 1.71) | 1.23 | (1.02, 1.49) |
| Rurality at index visit | ||||
| Metropolitan | ||||
| Micropolitan | 1.16 | (0.91, 1.47) | 0.91 | (0.78, 1.06) |
| Small town/rural | 1.20 | (0.81, 1.76) | 0.88 | (0.68, 1.14) |
| History of ED utilization, 2006–2009 | ||||
| Any assault visit | 1.58 | (1.32, 1.90) | 1.84 | (1.64, 2.06) |
| Any self-harm visit | 1.02 | (0.69, 1.51) | 1.08 | (0.83, 1.40) |
| Any mental health visit | 1.66 | (1.39, 1.97) | 1.49 | (1.34, 1.67) |
| Any substance use visit | 1.17 | (0.94, 1.44) | 1.17 | (1.02, 1.34) |
| Total ED visit count | 1.06 | (1.04, 1.08) | 1.07 | (1.06, 1.08) |
Bivariate rate ratios (RR) estimated using negative binomial model with log link and robust SEs.16
Note: Bolded estimates are statistically significant (P-value < 0.05)
Discussion
This study followed assaulted adolescents for an average of 5.3 years. Over this time, nearly one in every five adolescents with an index assault in 2010 (18.2%) returned to the ED because of injuries sustained in a repeat assault. Significantly less than half (37.2%) of these repeat assaults occurred within the first year after the index assault, indicating that prior studies that followed their patient populations for only one year may have significantly underestimated the rate of repeated assault. Prior studies, most of which used samples from single hospital networks, found cumulative incidences ranging from 1% to 44%, with most estimates concentrated in the low end of that range.7–9 Results from our study, which relied on statewide hospital data and had an extended follow-up period, provide a more population-representative estimate of the rate of repeat assault among adolescents.
Consistent with prior literature, we found that Black adolescents and those on Medicaid were disproportionately represented among those experiencing assault-related injuries.6,17,18 Findings from this study diverge from previous studies, however, in observing that Hispanic adolescents were not at higher risk of repeat assault injuries. A national study of adolescents suggested that Hispanic adolescents are victimized at higher rates compared to their non-Hispanic peers.19,20 It is possible the reduced association between assault injury and Hispanic ethnicity is due to demographic differences between California and the rest of the United States, or to variability in the association between race/ethnicity and any assault vs. repeated assault.
Additionally, we found that prior visits to the hospital setting for a variety of conditions were predictive of future assault injury following the index visit for assault. First, prior assault injury was found to be predictive of future assault injury, which is in line with previous research.21–23 Other studies found that interventional programs which target adolescents who report assault injuries in the emergency setting successfully reduce rates of re-victimization.5,24
Secondly, we found that individuals with prior ED visits for mental health problems were at increased risk of future assault injury after the index visit. Previous studies have found a similar pattern, and hypothesize that temporally prior exposure to violence increased the risk of developing these mental health problems.19,22 Another line of research suggests that adolescents who suffer from serious psychological disorder experience elevated rates of violence victimization compared to their psychologically healthy peers.25 These bodies of evidence indicate that this relationship is bidirectional; adolescents who suffer from violence victimization have higher rates of psychological disorders. Regardless, successfully treating adolescents for anxiety disorders, mood disorders, and self-harm behavior may prevent some proportion of assault-related injuries.
Lastly, we found that substance use-related ED visits were predictive of future assault injury following the index visit, albeit only when examining the full follow-up period. Prior research indicates that alcohol consumption is related to aggression and assault injury among ED patients.24,26,27 Previous studies have demonstrated that therapy and interventions involving controlling or limiting substances such as alcohol and drugs can lead to decreased risk of future injury.24
Prior research indicates that rates of assault are lower in rural areas compared to urban areas. We found that the risk of repeated assault injury was no different for rural vs. urban adolescents.10 Addressing assault within non-urban communities should still be considered a priority, as these adolescents experience similar risk for repeat assault injury compared to their urban peers.
Limitations
This study had several limitations. First, not every ED assault patient provided a valid social security number (SSN) upon arrival to the emergency department. Analysis of the visits with and without unique identifiers indicated that there were few substantial differences between these groups (see Supplemental Table 2). Despite this, marginalized populations such as undocumented individuals may not be accounted for in the analysis, because they would not have a registered SSN, and results may not be generalizable to adolescents who do not provide their SSNs at the time of an ED visit. Second, not all instances of assault result in injuries which require emergency treatment. Individuals with less severe assault injuries may seek treatment at clinics or other non-emergency settings, or may not seek treatment at all; our results cannot be extrapolated to these more minor injuries. Third, the utilization of California hospital data limits the generalizability of the findings to other states. Lastly, visits that study patients made to non-Californian hospitals were not observable, and we thus may have underestimated the rate and characteristics of some repeat assaults.
Strengths
This study utilized statewide hospital data with a long follow-up period. The ability to use these population-based data allowed for more accurate measures of the incidence of repeat assault injury. Furthermore, our ability to explicitly examine patients’ prior ED utilization patterns as predictors of repeat assault before the index assault injury, as well as the multi-year follow up time, enabled the research team to better understand longitudinal outcomes and injury patterns among the cohort of assaulted adolescents. Lastly, this study was unique in that the data utilized allowed researchers to follow adolescents to any emergency department visits made to any Californian hospital, not just the original facility.
Conclusions
Within the state of California, a majority of adolescents who suffer repeated assault injuries experience the second assault more than one year after the initial assault, underscoring their enduring vulnerability to violence. Key patient characteristics, often easily ascertainable in ED settings, predicted increased risk of a subsequent assault, with important implications for intervention targeting. The negative consequences associated with experiencing assault – including subsequent mental health problems, disability, and lost days in education or work settings,19,21,28– may be exacerbated among adolescents who are involved in multiple violent altercations, indicating that these patients should be referred for follow-up services and carefully monitored.
Supplementary Material
Article Summary.
1. Why is this topic important?
Violent injuries are a leading cause of morbidity and mortality among adolescents aged 10–19 years. Prior research has examined rates and method of injury among adolescents reporting to the emergency department for assault, but less is known about incidence of and risk factors for subsequent assault injury.
2. What does this study attempt to show?
This study examines data on adolescents who reported to California emergency departments for assault, followed for a period of 5 years. We compare the method of assault at the index visit to the second assault visit, estimate the time between first and second assault injury, and explore the socio-demographic factors which predict future assault injury.
3. What are the key findings?
A total of 3,273 (18.3%) of assaulted adolescents experienced ≥1 additional assault injury ED visit over the full follow-up period; 37.3% of these repeat assaults occurred within the first year after an index assault visit.
For most assault-injured adolescents with a repeat assault injury, the most common mechanism of injury at second assault was fight/brawl. However, among adolescents injured via firearm at their index visit who had a second assault visit, firearm injury was the most common single cause of injury at second visit.
Sociodemographic characteristics (e.g., older age, Black race) and history of prior ED visits for assault and mental health problems predicted increased risk of repeat assault.
4. How is patient care impacted?
Because a larger proportion of adolescents experience repeat assault than previously reported, assault intervention at adolescent patients’ initial visits should be strongly considered.
Acknowledgments
This project was funded, in part, through National Institutes of Health grant R15 MH113108-01 to Sidra Goldman-Mellor, Paul Brown, Deborah Wiebe, Paul Gruene-wald, and Magdelena Cerdá, and a Hellman Fellows Fund award to Sidra Goldman-Mellor.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data Statement
It is stated policy of the California Office of Statewide Health and Planning Department (OSHPD) that researchers may not share or distribute datasets provided to them by OSHPD. Datasets are available by individual researcher request at OSHPD’s website.
References
- 1.National Center for Injury Prevention and Control. WISQUARS injury mortality statistics https://webappa.cdc.gov/cgi-bin/broker.exe. Accessed September 18, 2018.
- 2.Center for Disease Control and Prevention. Non-fatal injury data https://www.cdc.gov/injury/wisqars/nonfatal.html. Published 2018. Accessed September 18, 2018.
- 3.Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, Resnick HS. Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. J Community Psychol 2000;28(6):625–641. [Google Scholar]
- 4.Lim HJ, Mccart M, Davies WH, Calhoun A, Melzer-Lange MD. Risk for repeat emergency department visits for violent injuries in youth firearm victims. Clin Med Trauma Intensive Med 2009;2(306):1–7. [Google Scholar]
- 5.Cheng TL, Schwarz D, Brenner RA, et al. Adolescent assault injury: Risk and protective factors and locations of contact for intervention. Pediatrics 2003;112(4):931 LP-938. http://pediatrics.aappublications.org/content/112/4/931.abstract. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham RM, Carter PM, Ranney M, et al. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury. JAMA Pediatr 2015;169(1):63. doi: 10.1001/jamapediatrics.2014.1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hedges BE, Dimsdale JE, Hoyt DB, Berry C, Leitz K. Characteristics of repeat trauma patients, San Diego County. Am J Public Health 1995;85(7):1008–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poole GV, Griswold JA, Thaggard K, Rhodes RS Trauma is a recurrent disease. Surgery 1993;113(6):608–611. http://www.ncbi.nlm.nih.gov/pubmed/8506517. [PubMed] [Google Scholar]
- 9.Cooper C, Eslinger D, Nash D, Zawahri J Al, Stolley P Repeat victims of violence. Am J Emerg Med 2001;19(5):438. doi: 10.1016/S0735-6757(01)80084-X [DOI] [Google Scholar]
- 10.Duhart DT. Urban, suburban, and rural victimization, 1993–98.; 2000 Washington DC; US Department of Justice; https://www.bjs.gov/content/pub/pdf/usrv98.pdf. [Google Scholar]
- 11.Centers for Disease Control and Prevention. ICD-9-CM: International classification of diseases, 9th revision, clinical modification https://www.cdc.gov/nchs/icd/icd9cm.htm. Published 2014. Accessed September 18, 2018.
- 12.Injury Surveillance Workgroup 9. The Transition from ICD-9-CM to ICD-10-CM: Guidance for Analysis and Reporting of Injuries by Mechanism and Intent; 2016. http://c.ymcdn.com/sites/www.safestates.org/resource/resmgr/isw9/ISW9_FINAL_Report.pdf.
- 13.Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, Walton MA. Characteristics of youth seeking emergency care for assault injuries. Pediatrics 2014;133(1):e96–e105. doi: 10.1542/peds.2013-1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS) 2015 U.S. Agency for Healthcare Research and Quality; Rockville, MD; 2015. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/CCSUsersGuide.pdf. [Google Scholar]
- 15.U.S. Department of Agriculture. [September 18, 2018];Rural-Urban commuting area codes, Version 3.10. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx. Published 2014. Accessed.
- 16.Mullahy J Specification and testing of some modified count data models. J Econom 1986;33(3):341–365. doi: 10.1016/0304-4076(86)90002-3 [DOI] [Google Scholar]
- 17.Kalesan B, Vyliparambil MAA, Bogue E, et al. Race and ethnicity, neighborhood poverty and pediatric firearm hospitalizations in the United States. Ann Epidemiol 2016;26(1):1–6. doi: 10.1016/j.annepidem.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 18.Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Soc Sci Med 2006;62(1):13–27. doi: 10.1016/j.socscimed.2005.05.030 [DOI] [PubMed] [Google Scholar]
- 19.Kilpatrick, Ruggiero Dean G., Acierno R Kenneth J., Saunders BE, Resnick HS, et al. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. J Consult Clin Psychol 2003;71(4):692–700. doi: 10.1037/0022-006X.71.4.692 [DOI] [PubMed] [Google Scholar]
- 20.Kilpatrick DG, Saunders BE, Smith DW. Youth Victimization: Prevalence and Implications https://www.ncjrs.gov/pdffiles1/nij/194972.pdf U.S. Department of Justice; Washington D.C.; 2003. [Google Scholar]
- 21.Benedini KM, Fagan AA, Gibson CL. The cycle of victimization: The relationship between childhood maltreatment and adolescent peer victimization. Child Abuse Negl 2016;59:111–121. doi: 10.1016/j.chiabu.2016.08.003 [DOI] [PubMed] [Google Scholar]
- 22.Menard S Short and Long-Term Consequences of Adolescent Victimization U.S. Department of Justice; Washington, D.C; 2002. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=psyc3&AN=1997-04609-004%0Ahttp://bf4dv7zn3u.search.serialssolutions.com.myaccess.library.utoronto.ca/?url_ver=Z39.88-2004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&rfr_id=info:sid/Ovid:ps. [Google Scholar]
- 23.Cunningham R, Knox L, Fein J, et al. Before and after the trauma bay: The prevention of violent injury among youth. Ann Emerg Med 2009;53(4):490–500. doi: 10.1016/j.annemergmed.2008.11.014 [DOI] [PubMed] [Google Scholar]
- 24.Walton MA, Chermack ST, Shope JT, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents. J Am Med Assoc 2010;304(5):527–535. http://c.ymcdn.com/sites/www.safestates.org/resource/resmgr/isw9/ISW9_FINAL_Report.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: ‘Much ado about nothing’? Psychol Med 2010;40:717–729. doi: 10.1017/S0033291709991383 [DOI] [PubMed] [Google Scholar]
- 26.Clark DB, Lesnick L, Hegedus AM. Traumas and other adverse life events in adolescents with alcohol abuse and dependence. J Am Acad Child Adolesc Psychiatry 1997;36(12):1744–1751. doi: 10.1097/00004583-199712000-00023 [DOI] [PubMed] [Google Scholar]
- 27.Elder RW, Shults RA, Swahn MH, Strife BJ, Ryan GW. Alcohol-related emergency department visits among people ages 13–25 years. J Stud Alcohol 2004;65:297–300. [DOI] [PubMed] [Google Scholar]
- 28.Duncan RD, Saunders BE, Kilpatrick DG, Hanson RF, Resnick HS. Childhood physical assault as a risk factor for PTSD, depression, and substance abuse: Findings from a national survey. Am J Orthopsychiatry 1996;66(3):437–448. doi: 10.1037/h0080194 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


