Abstract
Objective: The burden of mental disorders continues to grow with significant impacts on health. This study aimed to investigate the prevalence of stress, anxiety, and depression in Yazd adult population and to examine the associated socioeconomic factors.
Method : In a 2-step cluster sampling process, 10 000 residents of Yazd Greater Area (200 clusters of 50) were selected during 2014-2015. The short version of Depression, Anxiety and Stress Scale (DASS) Questionnaire was used to assess relevant depression, anxiety, and stress. Data were analyzed by chi-square test. All statistical analyses were done using SPSS version 16.0. P-values less than 0.05 were considered statistically significant.
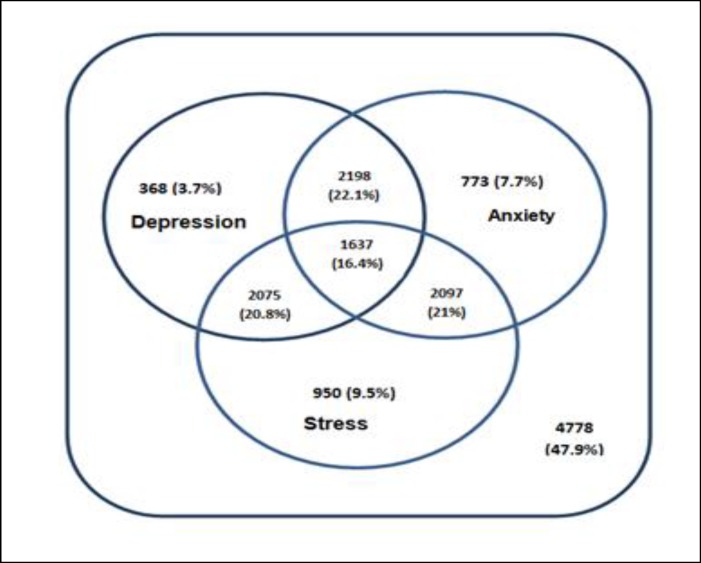
Results: Depression, anxiety, and stress were seen in 29%, 32.2%, and 34.8% of adult residents of Yazd Greater Area, respectively. The symptoms of the disorders were moderate, severe, and very severe in 18.2%, 20.2%, and 23.4% of the population, respectively. Also, a significant difference was found between the symptoms of depression, anxiety, and stress and sex, age group, education, employment, marriage status, and country of birth. Of the total population under study, 3.7% were depressed, 7.7% were anxious, 9.5% had stress alone and 16.4% had symptoms of all the 3 disorders. Frequency of depression among Zoroastrians was more than muslims (42.1% vs 29.7%).
Conclusion: Despite achievemments in higher education and economic development of Yazd population over the past 2 decades, the trend of these disorders has alarmingly been increased. Considering the findings, it is necessary to develop evidence-based and appropriate community-based primary and secondary mental health prevention programs.
Key Words: Anxiety, Anxiety and Stress Scale (DASS), Depression, Iran, Prevalence, Stress
Mental health is one of the most important health indicators that causes considerable morbidity (1). According to the World Health Organization (WHO) report in 2008, one every five adults experienced mental disorders in the past year and 29.2% had a history of mental illness during their lifetime (2). To improve mental health, WHO has developed an evidence-based mental health program for the years 2013-2020 (3).
Depression is a mood disorder which is characterized by short-term emotional responses to a serious health condition associated with impaired daily functioning accompanied by symptoms, such as sadness and frustration, feelings of guilt, insensibility, and loss of interest (4).
Depression is a common psychiatric disorder in the world, affecting more than 300 million people worldwide (5, 6). Anxiety disorders are defined as a group of mental disorders characterized by an unpleasant feeling with uneasiness or worry about future events or the fear of responding to current events. It may occur without an identifiable triggering stimulus (4). In 2013, one out of every nine people in the world had at least one of the anxiety disorders (7, 8). In stress, a person's lack of compliance with environmental conditions leads to psychological and biological changes, and the person is at risk of becoming ill (9).
Nearly a quarter of adults in the United States have psychiatric disorders, and almost half of them experience at least one mental illness during their lives (10). A systematic review and meta-analysis for global prevalence showed that the countries of Eastern Asia show an estimated one-year/lifetime prevalence less than other areas. The prevalence of one year among sub-Saharan African countries is low, while the highest lifetime prevalence was reported in Anglo-Celtic countries (11).
The prevalence of having mental disorder over the past 12 months among Iranian population aged 18-64 years in 2011 was 23.6%, followed by anxiety disorders (15.6%). Two thirds of the patients had moderate to severe mental disorders (12). Recent findings indicated an increase in the prevalence of psychiatric disorders between 1999 and 2015 in Iranian adults (2). There is a variation in the prevalence of mental disorders in different Iranian provinces and across various groups from 11.7% to 38.9%. It is necessary to conduct further studies on the general population and use validated inventories to monitor changes in the future (13, 14).
Several studies reported the prevalence of mental disorders in Yazd province. However, estimations from previous studies demonstrated inconsistency in the prevalence of mental disorders, especially depression, reporting the highest prevalence of depression (54.3%) in Iran (15) and the lowest level of happiness among the Iranian provinces (16). These differences may be due to non-representative sampling or using different inventories. Given that a large population-based study on psychiatric disorders has not been conducted in Yazd until now, such study was needed. Most similar studies were conducted on small groups of Yazd population, such as diabetic patients (17), college students (18), and truck drivers (19).
This study aimed to investigate the prevalence and associated predictors of stress, anxiety, and depression in Yazd adult population using data from a large population-based study and associated predictors.
Comparison of findings with previous population-based studies may help health system managers to design and implement appropriate interventional strategies for health promotion.
Materials and Methods
Yazd Health Study (YaHS) is a prospective study conducted to determine the prevalence of non-communicable diseases and associated risk factors in Yazd Greater Area. Details of the methodology were published elsewhere (20).
In a nutshell, the population frame of YaHS was adults aged 20-69 years living in Yazd Greater Area. In a 2-step cluster sampling process, 10 000 participants (200 clusters of 50) were selected during 2014-2015. Data were collected using a questionnaire. DASS (Depression, Anxiety and Stress Scale) Questionnaire (short form) was used, which is a different, simple, and approved instrument for assessing depression, anxiety, and stress both in clinical settings and in the community (21, 22). DASS is a short screening tool that measures depression, anxiety, and stress by a 21-item self-report questionnaire. For each disorder, seven questions are considered, and the final score is obtained by the total score of the questions related to it. Each question was scored using a Likert scale, ranging from 0 (did not apply to me at all/never) to three (applied to me very much, or most of the time/almost always). Higher scores indicated a higher level of disorder by a specific classification scoring. Individuals are classified as normal, mild, moderate, severe, and very severe based on their responses. Various studies have shown high concurrent validity for Beck Depression Inventory, Beck Anxiety Inventory, and DASS. Also, this tool can detect stress symptoms from depression and anxiety (23). Comparing the results from DASS-21 with the diagnosis of psychiatric interviews showed the sensitivity and specificity of 75% to 89% for this tool and its potential for accurate screening of depression, anxiety, and stress (24, 25). The reliability and validity of the translated version of the Persian questionnaire was confirmed for an Iranian population (26, 27). Sahebi et al reported a Cronbach’s alpha of 0.77, 0.79, and 0.78 for depression, anxiety, and stress subscales, respectively. The correlation coefficient of this inventory was 0.7 with Beck’s Inventory, 0.67 with Zung Anxiety Test, and 0.49 with Perceived Stress Inventory (26).
For direct age standardization of the prevalence rates, Yazd population details were obtained from the Statistical Center of Iran. Categorical variables were presented as frequencies and percentages. The prevalence of depression, anxiety, and stress was described as proportions. Chi square test was used for categorical variables to analyze the differences in demographic variables between the groups. All statistical analyses were done using SPSS version 16. P-values less than 0.05 were considered statistically significant.
This study was approved by Ethics Committee of Shahid Sadoughi University of Medical Sciences (No. 17/1/73941). Informed consent was obtained from all the participants.
Results
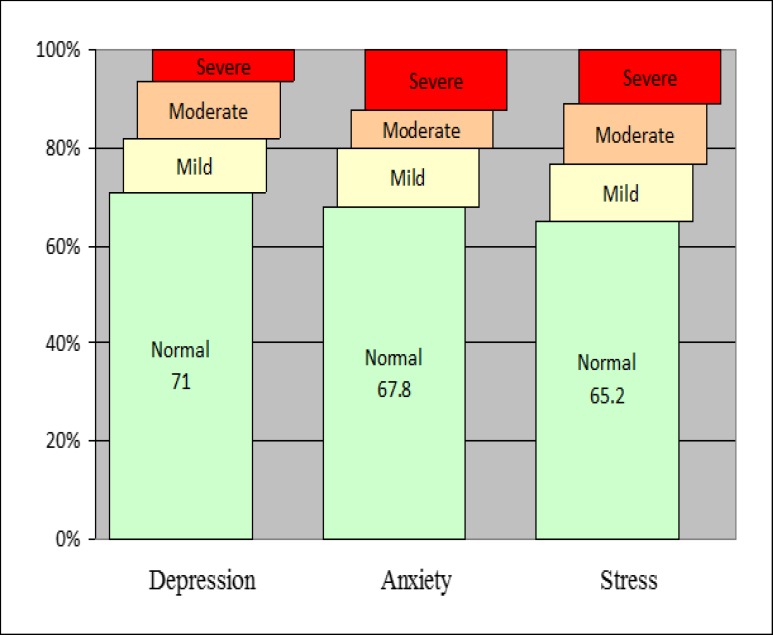
A total of 9965 people participated in this study. Depression, anxiety, and stress were found in 29%, 32.2%, and 34.8% of adult residents of Yazd Greater Area. The symptoms of the disorders were moderate to very severe in 18.2%, 20.2%, and 23.4% of the population, respectively (Figure 1).
Figure 1.
Prevalence of Age-Standardized Depression, Anxiety, and Stress in Adults Aged 20-69 Years Living in Yazd, Iran, During 2014–2015
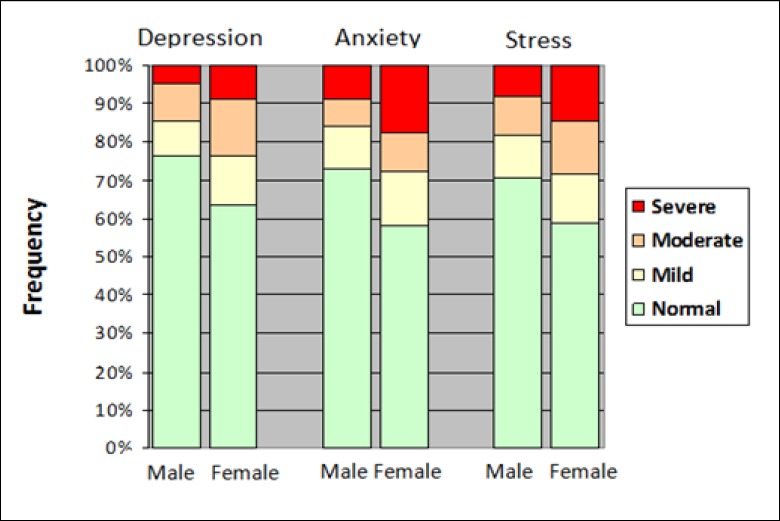
Figure 2 demonstrates that the prevalence of depressive symptoms was significantly higher in women than in men (36.5 vs 23.7%).
Figure 2.
Prevalence of Age-Standardized Depression, Anxiety, and Stress by Sex in Adults Aged 20-69 Years Living in Yazd, Iran, During 2014–2015
The prevalence and severity of symptoms in older adults were significantly higher than the younger population. There was a significant difference between the symptoms of depression and education, employment, marriage status, and country of birth. The prevalence was higher in less educated, unemployed, uninsured, and immigrants. Frequency of depression among Zoroastrians was more than Muslims (42.1 vs 29.7%) (Table 1). Also, 28.9% of the population had a history of depression, which was higher in people with severe depressive symptoms compared to the rest. Table 1 demonstrates the prevalence and severity of depressive symptoms in adolescents according to demographic variables.
Table 1.
Prevalence of Depression According to Various Factors in Yazd Adult Population Aged 20-69 Years during 2014–2015 (n = 9965)
| Subgroups | Normal | Depression | P value | ||
|---|---|---|---|---|---|
| Mild | Moderate | Severe & Very Severe | |||
| Crude | 6926 (69.9%) | 1098 (11.1%) | 1208 (12.2%) | 681 (6.9%) | |
| Age group | |||||
| 20-29 | 1449 (73.8%) | 195 (9.9%) | 201 (10.2%) | 118 (6%) | <0.0001 |
| 30-39 | 1416 (69.9%) | 224 (11.1%) | 247 (12.2%) | 138 (6.8%) | |
| 40-49 | 1411 (68.9%) | 242 (11.8%) | 265 (12.9%) | 131 (6.4%) | |
| 50-59 | 1378 (70%) | 198 (10.1%) | 230 (11.7%) | 163 (8.3%) | |
| 60-69 | 1272 (66.7%) | 239 (12.5%) | 265 (13.9%) | 131 (6.9%) | |
| Education | |||||
| Primary school and less | 1635 (63.2%) | 325 (12.6%) | 387 (15%) | 240 (9.3%) | <0.0001 |
| High school | 1871 (66.8%) | 340 (12.1%) | 380 (13.6%) | 211 (7.5%) | |
| Diploma& Graduate diploma | 2181 (74.4%) | 274 (9.3%) | 311 (10.6%) | 166 (5.7%) | |
| BSc | 1005 (77.8%) | 120 (9.3%) | 108 (8.4%) | 58 (4.5%) | |
| MSc. and Doctorate | 197 (77.6%) | 28 (11%) | 22 (8.7%) | 7 (2.8%) | |
| History of depression | |||||
| Yes | 169 (28.9%) | 99 (16.9%) | 149 (25.5%) | 168 (28.7%) | <0.0001 |
| No | 6678 (72.8%) | 974 (10.6%) | 1038 (11.3%) | 489 (5.3%) | |
| Employment | |||||
| Employed | 2994 (76.3%) | 360 (9.2%) | 389 (9.9%) | 183 (4.7%) | <0.0001 |
| Unemployed | 2371 (62%) | 493 (12.9%) | 586 (15.3%) | 375 (9.8%) | |
| Housewife | 1482 (72.7%) | 221 (10.8%) | 220 (10.8%) | 116 (5.7%) | |
| Insurance | |||||
| Not insured | 326 (60.7%) | 66 (12.3%) | 83 (15.5%) | 62 (11.5%) | <0.0001 |
| Insured | 6536 (70.6%) | 1008 (10.9%) | 1102 (11.9%) | 615 (6.6%) | |
| Migration status | |||||
| Native | 5245 (70.4%) | 813 (10.9%) | 894 (12%) | 496 (6.7%) | <0.001 |
| From within the province | 654 (69.9%) | 110 (11.8%) | 123 (13.1%) | 49 (5.2%) | |
| From other provinces | 855 (67.6%) | 145 (11.5%) | 156 (12.3%) | 109 (8.6%) | |
| From overseas | 130 (60.5%) | 23 (10.7%) | 35 (16.3%) | 27 (12.6%) | |
| Marriage status | |||||
| Married | 6002 (71.2%) | 902 (10.7%) | 990 (11.7%) | 536 (6.4%) | <0.0001 |
| Single | 727 (69%) | 118 (11.2%) | 125 (11.9%) | 84 (8%) | |
| Widowed | 178 (46.8%) | 68 (17.9%) | 79 (20.8%) | 55 (14.5%) | |
| Divorced | 21 (38.2%) | 9 (16.4%) | 14 (25.5%) | 11 (20%) | |
| Country of birth | |||||
| Iranian | 6754 (70%) | 1068 (11.1%) | 1173 (12.2%) | 654 (6.8%) | <0.001 |
| Non-Iranian | 130 (60.5%) | 23 (10.7%) | 35 (16.3%) | 27 (12.6%) | |
| Religion | |||||
| Muslim | 6696 (70.3%) | 1034 (10.8%) | 1148 (12%) | 653 (6.9%) | <0.0001 |
| Zoroastrian | 136 (57.9%) | 41 (17.4%) | 42 (17.9%) | 16 (6.8%) | |
Table 2 shows that 32.2% of the adults had symptoms of anxiety, which was more in women compared to men (41.9 vs 36.7%, P-value <0.0001) (Figure 2). As age increased and education decreased, the prevalence and severity of anxiety significantly increased. Employed, insured, and those with Iranian nationality were less anxious than others (P-value <0.0001). Widowed and divorced women had the highest frequency of anxiety and single people had the lowest level.
Table 2.
Prevalence of Anxiety According to Various Factors in Yazd Adult Population Aged 20-69 Years during 2014–2015 (n = 9965)
| Subgroups | Normal | Anxiety | P value | ||
|---|---|---|---|---|---|
| Mild | Moderate | Severe & Very Severe | |||
| Crude | 6508 (65.7%) | 1239 (12.5%) | 852 (8.6%) | 1314 (13.3%) | |
| Age group | |||||
| 20-29 | 1406 (71.6%) | 217 (11.1%) | 131 (6.7%) | 209 (10.6%) | <0.0001 |
| 30-39 | 1382 (68.2%) | 245 (12.1%) | 140 (6.9%) | 258 (12.7%) | |
| 40-49 | 1343 (65.5%) | 249 (12.2%) | 186 (9.1%) | 271 (13.2%) | |
| 50-59 | 1239 (62.9%) | 272 (13.8%) | 171 (8.7%) | 287 (14.6%) | |
| 60-69 | 1138 (59.7%) | 256 (13.4%) | 224 (11.7%) | 289 (15.2%) | |
| Education | |||||
| Primary school and less | 1464 (56.6%) | 354 (13.7%) | 288 (11.1%) | 481 (18.6%) | <0.0001 |
| High school | 1756 (62.7%) | 371 (13.2%) | 261 (9.3%) | 414 (14.8%) | |
| Diploma, Graduate Diploma | 2080 (70.9%) | 337 (11.5%) | 216 (7.4%) | 299 (10.2%) | |
| BSc | 978 (75.8%) | 145 (11.2%) | 65 (5%) | 103 (8%) | |
| MSc. and Doctorate | 189 (74.4%) | 33 (13%) | 16 (6.3%) | 16 (6.3%) | |
| History of depression | |||||
| Yes | 163 (27.9%) | 91 (15.6%) | 89 (15.2%) | 242 (41.4%) | <0.0001 |
| No | 6247 (68.4%) | 1139 (12.4%) | 740 (8.1%) | 1026 (11.2%) | |
| Employment | |||||
| Employed | 2892 (73.7%) | 414 (10.5%) | 249 (6.3%) | 371 (9.4%) | <0.0001 |
| Unemployed | 2146 (56.1%) | 558 (14.6%) | 413 (10.8%) | 708 (18.5%) | |
| Housewife | 1396 (68.5%) | 251 (12.3%) | 174 (8.5%) | 218 (10.7%) | |
| Insurance | |||||
| Not insured | 322 (60%) | 64 (11.9%) | 46 (8.6%) | 105 (19.6%) | <0.0001 |
| Insured | 6130 (66.2%) | 1157 (12.5%) | 786 (8.5%) | 1188 (12.8%) | |
| Migration status | |||||
| Native | 4929 (66.2%) | 925 (12.4%) | 632 (8.5%) | 962 (12.9%) | <0.0001 |
| From within the province | 611 (65.3%) | 126 (13.5%) | 96 (10.3%) | 103 (11%) | |
| From other provinces | 812 (64.2%) | 163 (12.9%) | 103 (8.1%) | 187 (14.8%) | |
| From overseas | 112 (52.1%) | 24 (11.2%) | 20 (9.3%) | 59 (27.4%) | |
| Marriage status | |||||
| Married | 5569 (66.1%) | 1081 (12.8%) | 701 (8.3%) | 1079 (12.8%) | <0.0001 |
| Single | 752 (71.3%) | 105 (10%) | 74 (7%) | 123 (11.7%) | |
| Widowed | 162 (42.6%) | 51 (13.4%) | 68 (17.9%) | 99 (26.1%) | |
| Divorced | 22 (40%) | 6 (10.9%) | 7 (12.7%) | 20 (36.4%) | |
| Country of birth | |||||
| Iranian | 6352 (65.8%) | 1214 (12.6%) | 831 (8.6%) | 1252 (13%) | <0.0001 |
| Non-Iranian | 112 (52.1%) | 24 (11.2%) | 20 (9.3%) | 59 (27.4%) | |
| Religion | |||||
| Muslim | 6264 (65.7%) | 1226 (12.6%) | 839 (8.6%) | 1288 (13.2%) | <0.0001 |
| Zoroastrian | 149 (63.4%) | 30 (12.8%) | 21 (8.9%) | 35 (14.9%) | |
There was no significant difference in the frequency of anxiety symptoms among Muslims and Zoroastrians.
Women had 11.8% more stress than men. Moderate to severe intensity of stress was also significantly higher in women (Table 3). Younger adults aged 20-29 years were more under stress than other age groups, and stress significantly decreased with increase in years of education.
Table 3.
Prevalence of Stress According to Various Factors in Yazd Adult Population Aged 20-69 Years during 2014–2015 (n = 9965)
| Subgroups | Normal | Stress | P value | ||
|---|---|---|---|---|---|
| Mild | Moderate | Severe & Very Severe | |||
| Crude | 6445 (65%) | 1149 (11.6%) | 1205 (12.2%) | 1114 (11.2%) | |
| Age group | |||||
| 20-29 | 1317(67.1%) | 215 (11%) | 241 (12.3%) | 190 (9.7%) | 0.033 |
| 30-39 | 1278 (63.1%) | 241 (11.9%) | 267 (13.2%) | 239 (11.8%) | |
| 40-49 | 1310 (63.9%) | 254 (12.4%) | 267 (13%) | 218 (10.6%) | |
| 50-59 | 1281 (65.1%) | 214 (10.9%) | 223 (11.3%) | 251 (12.7%) | |
| 60-69 | 1259 (66%) | 225 (11.8%) | 207 (10.9%) | 216 (11.3%) | |
| Education | |||||
| Primary school and less | 1492 (57.7%) | 310 (12%) | 378 (14.6%) | 407 (15.7%) | <0.0001 |
| High school | 1813 (64.7%) | 340 (12.1%) | 326 (11.6%) | 323 (11.5%) | |
| Diploma& Graduate Diploma | 2003 (68.3%) | 329 (11.2%) | 332 (11.3%) | 268 (9.1%) | |
| BSc | 934 (72.3%) | 125 (9.7%) | 137 (10.6%) | 95 (7.4%) | |
| MSc. and Doctorate | 176 (69.3%) | 35 (13.8%) | 26 (10.2%) | 17 (6.7%) | |
| History of depression | |||||
| Yes | 188 (32.1%) | 76 (13%) | 108 (18.5%) | 213 (36.4%) | <0.0001 |
| No | 6174 (67.3%) | 1051 (11.5%) | 1074 (11.7%) | 880 (9.6%) | |
| Employment | |||||
| Employed | 2737 (69.7%) | 458 (11.7%) | 408 (10.4%) | 323 (8.2%) | <0.0001 |
| Unemployed | 2329 (60.9%) | 436 (11.4%) | 502 (13.1%) | 558 (14.6%) | |
| Housewife | 1300 (63.8%) | 236 (11.6%) | 280 (13.7%) | 223 (10.9%) | |
| Insurance | |||||
| Not insured | 326 (60.7%) | 66 (12.3%) | 83 (15.5%) | 62 (11.5%) | <0.0001 |
| Insured | 6536 (70.6%) | 1008 (10.9%) | 1102 (11.9%) | 615 (6.6%) | |
| Migration status | |||||
| Native | 4984 (66.9%) | 823 (11%) | 853 (11.5%) | 788 (10.6%) | <0.0001 |
| From within the province | 530 (56.6%) | 129 (13.8%) | 156 (16.7%) | 121 (12.9%) | |
| From other provinces | 769 (60.8%) | 166 (13.1%) | 168 (13.3%) | 162 (12.8%) | |
| From overseas | 119 (55.3%) | 28 (13%) | 27 (12.6%) | 41 (19.1%) | |
| Marriage status | |||||
| Married | 5557 (65.9%) | 969 (11.5%) | 1001 (11.9%) | 903 (10.7%) | <0.0001 |
| Single | 687 (65.2%) | 117 (11.1%) | 131 (12.4%) | 119 (11.3%) | |
| Widowed | 186 (48.9%) | 52 (13.7%) | 55 (14.5%) | 87 (22.9%) | |
| Divorced | 21 (38.2%) | 8 (14.5%) | 17 (30.9%) | 9 (16.4%) | |
| Country of birth | |||||
| Iranian | 6283 (65.1%) | 1118 (11.6%) | 1177 (12.2%) | 1071 (11.1%) | 0.002 |
| Non-Iranian | 119 (55.3%) | 28 (13%) | 27 (12.6%) | 41 (19.1%) | |
| Religion | |||||
| Muslim | 6214 (65.2%) | 1097 (11.5%) | 1141 (12%) | 1079 (11.3%) | 0.003 |
| Zoroastrian | 135 (57.4%) | 31 (13.2%) | 46 (19.6%) | 23 (9.8%) | |
There was less stress in the employed and insured people. Immigrants both from other provinces of Iran and other countries were more likely to be stressed compared to non-migrant Yazd residents (P-value = 0.003).
Of the participants, 47.9% did not have any symptoms of depression, anxiety, and stress. Moreover, 3.7% were depressed, 7.7 were anxious, 9.5% had stress, and 16.4% had symptoms of all the 3 disorders. Figure 3 shows the coincidence of the presence of symptoms of depression, anxiety, and stress in individuals.
Figure 3.
Overlap of Depression, Anxiety, and Stress in Adults Aged 20-69 Years Living in Yazd, Iran, During 2014–2015
Discussion
The prevalence of mental disorders has increased in Yazd population over the last two decades (1, 28). Approximately, half of Yazd population (52.1%) had a mild to severe major depression, anxiety, and stress, and 16.4% had symptoms of all the 3 disorders.
Three National Mental Health Surveys in Iran in 2001, 2002, and 2012 reported a prevalence of psychiatric disorders of 21.0%, 17.1%, and 23.6%, respectively (1, 12, 14). The difference in the results could be due to using different inventories, including Beck, Schizophrenia and Affective Disorders Scale (SADS), Composite International Diagnostic Interview (CIDI), and General Health Questionnaire (GHQ), different range of psychiatric disorders and age range/sample size of the studies. However, this increase may be true to some extent, particularly because the prevalence of these psychiatric disorders in Yazd population is alarmingly high compared to the Iranian national average.
Our findings are similar to those of three studies in Tehran, which reported a prevalence of psychiatric disorders of 21.5%, 34.3%, and 39.7%, respectively, in the years 2000, 2009, and 2012 using the GHQ-28 questionnaire (28-30). This can be due to the similarity of the GHQ-28 inventory in measuring anxiety and depression in target groups. High prevalence of mental disorders in Yazd, similar to a cosmopolitan city such as Tehran, is not expected and more studies should be conducted on the role of socioeconomic factors, such as urbanization, industrialization, and migration.
Ahmadi et al reported that the prevalence of psychiatric sorders in Yazd children and adolescents was as high as 35.5% (anxiety, 22.2%) in 2016, which is consistent with our findings and justifies the high prevalence in adults as well (31). With the lack of community-based preventive intervention programs for younger age groups, the high incidence of mental disorders in adults is expected.
The increasing trend of psychiatric disorders in adulthood and high prevalence of these disorders in childhood mandate a comprehensive prevention programs and life skills training to reduce the incidence of mental disorders in Yazd adult population(31). In 2015, 23.4% of Iranian adult populations were suspected of having at least 1 mental disorder, and the prevalence of anxiety and somatization symptoms was higher than social dysfunction and depression symptoms (2). Considering that psychiatric disorders consisted of 4 alignments in this study, it can be said that prevalence of depression (29%), anxiety (32.3), and stress (34.8%) is reasonably high in Yazd Greater Area.
Our finding showed that the prevalence of psychiatric disorders was significantly higher in women than in men in Yazd. Depression (36.5% vs 23.7%), anxiety (41.9% vs 26.7%), and stress (40.9% vs 29.1%) were all higher in women than in men in Yaz. Similarly, according to a study in Iran (2011), using CIDI and MDQ inventories, it was found that 26.5% of women and 20.8% of men had psychiatric disorders, anxiety disorder (19.4% vs 12%), and mood disorders (17.3 vs 11.9) (12).
In all the mentioned three national studies, results were indicative of higher prevalence of psychiatric disorders in women compared to men (27.6% vs 14.9%; 27.9% vs 28.6%; 42.4% vs 36.4%), which is consistant with findings of this study (28). Other studies reported that common mental disorders are more common in women than in men in other countries (32, 33). This difference can be attributed to socioeconomic disadvantage, cultural constraints, and violence. Women are more likely to express mental health problems than men. Evidence suggests the role of sex hormones in such gender differences (34).
This study showed that the prevalence and severity of depression was significantly higher in older adults, immigrants, less educated, unemployed, and uninsured people. These findings are in line with the study by Mohammadi et al in which psychiatric disorder is more prevalent in adults aged 41-55 years compared to other adult age groups.(1).
There was an association between place of birth and depression, anxiety, and stress symptoms in this study. Those born in other provinces and countries were more depressed, anxious, and stressful than those who were born in Yazd, similar to other studies (35, 36). The higher prevalence of depression in immigrants and religious minorities was also similar to that of other studies, which may be due to the differences in language, culture, and pattern of receiving health care (37).
This study revealed that anxiety was more common in women, those with higher income, less educated, unemployed, uninsured, widowed, and divorced indviduals. These findings are consistent with the reults of the Noorbala et al study that showed the risk of mental disorder increases with age, illiteracy/lower education, divorce, widownesss, unemployment, and being chronically ill (2, 38).
Findings of this study are consistent with the results of numerous studies on the relationship between socioeconomic status, marital status (39, 40), older age (41), lower education (42), unemployment (43) and higher prevalence of psychiatric disorders. Biological changes and disabilities in older age, economic problems in the unemployed, inability to control social problems in people with less education, and social constraints in divorced people may explain the higher rate of psychiatric disorders in these groups, similar to the findings of other studies conducted in Iran (2) and in the world (11). These social determinants of health were identified as psychosocial risk factors that increase mental disorders. However, more studies are needed to confirm the association between these factors and mental disorders.
Limitation
This study had several limitations. In this study, only the symptoms of depression, anxiety, and stress were examined, and other important psychiatric disorders, such as personality disorders, were not reported. Like most large population-based studies, a validated questionnaire was filled by trained interviewers to assess depression, anxiety, and stress. Thus, this cross-sectional analysis may not confirm cause and effect relationships.
However, the main strength of this study was population representativeness. This study investigated common mental disorders and relevant predictors. Therefore, this study might have underestimated the overall mental disorders and provided a conservative result.
Conclusion
Over the past 2 decades, the trend of depression, anxiety, and stress has been increased in Yazd Greater Area. This demands more root-cause analysis and ethiologic and interventional studies to investigate the causes of this high prevalence and to prevent and control these disorders. More studies are needed to evaluate the contribution of probable factors, such as daily stress, social media, interpersonal skills, and economic problems.
Acknowledgment
We thank people of Yazd for giving their time to Yazd health study. We aknowledge Shahid Sadoughi University for funding the study and Yazd Central Health for collaboration in conducting this study.
Conflict of Interest
None.
References
- 1.Mohammadi MR, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, et al. An epidemiological survey of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noorbala AA FS, Kamali K, Bagheri Yazdi SA, Hajebi A, Mousavi MT, Akhondzadeh S, Faghihzadeh E, Nouri B. Mental health survey of the adult population of Iran in 2015. Arch Iran Med. 2017;20(3):128–134. [PubMed] [Google Scholar]
- 3.World Health Organization. Mental health action plan 2013‐2020. Geneva: WHO; 2013. [Google Scholar]
- 4.Wahed WYA, Hassan SK. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria Journal of Medicine. 2017;53(1):77–84. [Google Scholar]
- 5.World Health Organization. Depression and Other Common Mental Disorders. Geneva: Global Health Estimates; 2017. [Google Scholar]
- 6.GBD 2015 Disease, Injury Incidence, Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Association D-AP. Diagnostic and statistical manual of mental disorders. Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- 8.Craske MG SM. Anxiety. Lancet. 2016;388(10063):3048–59. doi: 10.1016/S0140-6736(16)30381-6. [DOI] [PubMed] [Google Scholar]
- 9.Cohen S, Kessler RC, Gordon LU. Strategies for measuring stress in studies of psychiatric and physical disorders. Measuring stress: A guide for health and social scientists. 1995. pp. 3–26. [Google Scholar]
- 10.Reeves WC, Pratt LA, Thompson W, Dhingra SS, McKnight-Eily LR, Harrison L, et al. Mental illness surveillance among adults in the United States. MMWR Suppl. 2011;60(3):1–29. [PubMed] [Google Scholar]
- 11.Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiol. 2014;43(2):476–93. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iran Med. 2015;18(2):76–84. [PubMed] [Google Scholar]
- 13.Noorbala AA, Akhondzadeh S. Mental health study process into prevalence of mental disorders in iran. Arch Iran Med. 2015;18(2):74–5. [PubMed] [Google Scholar]
- 14.Yousefi-Nooraie R, Mohammadi MR, Salesian N, Amin-Esmaeeli M, Mansouri N, Mesgarpour B, et al. Prevalence of psychiatric disorders in Iran: A systematic review. Iran J Psychiatry. 2007;2:137–50. [Google Scholar]
- 15.Fallahzadeh H MM, Nikokaran J. Prevalence of depression, anxiety and stress in Yazd (2013) [In Persian] TB. 2016;15(3):155–64. [Google Scholar]
- 16.Montazeri A OS, Azin A, Aeenparast A, Jahangiri K, Sadighi J, et al. Happiness among iranian population findings from the iranian health perception survey(IHPS) [In Persian] Payesh. 2012;11(4):467–75. [Google Scholar]
- 17.Mazloomy S, Mirzaei A, Mohammadi S. Study of depression prevalence in the patients with type II diabetes referring to Yazd diabetes research centers in 2008 [In Persian] TOLOO-E-BEHDASHT. 2008;7(1-2):30–6. [Google Scholar]
- 18.Baghiani Moghadam M-H EM-H, Rahimi B, Aminian A-H, Aram M. Assessment of depression among college students in health and nursing Yazd University of Medical Sciences in 2008 [In Persian] Journal of Medical Education Development Center. 2011;6(1):17–24. [Google Scholar]
- 19.Vakili M, Eslami Farsani S, Hossein S, Dehghani Tafti M. Prevalence of depression and its related factors among truck drivers in Yazd Province-2008 [In Persian] Iran Occupational Health. 2010;6(4):69–76. [Google Scholar]
- 20.Mirzaei M S-AA, Mirzaei M, Mohsenpour MA. Cohort Profile: The Yazd Health Study (YaHS): a population-based study of adults aged 20–70 years (study design and baseline population data) International Journal of Epidemiology. 2018;47(3):697–8h. doi: 10.1093/ije/dyx231. [DOI] [PubMed] [Google Scholar]
- 21.Norton PJ. Depression Anxiety and Stress Scales (DASS-21): Psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20(3):253–65. doi: 10.1080/10615800701309279. [DOI] [PubMed] [Google Scholar]
- 22.Bener A, Alsulaiman R, Doodson L, El Ayoubi H. Comparison of Reliability and Validity of the Breast Cancer depression anxiety stress scales (DASS-21) with the Beck Depression Inventory-(BDI-II) and Hospital Anxiety and Depression Scale (HADS) Int J Behav Res Psychol. 2016;4(4):197–203. [Google Scholar]
- 23.Habibi M, Dehghani M, Pooravari M, Salehi S. Confirmatory Factor Analysis of Persian Version of Depression, Anxiety and Stress (DASS-42): Non-Clinical Sample. Razavi International Journal of Medicine. 2017;5(4) [Google Scholar]
- 24.Beaufort IN, De Weert-Van Oene GH, Buwalda VA, de Leeuw JRJ, Goudriaan AE. The Depression, Anxiety and Stress Scale (DASS-21) as a Screener for Depression in Substance Use Disorder Inpatients: A Pilot Study. Eur Addict Res. 2017;23(5):260–268. doi: 10.1159/000485182. [DOI] [PubMed] [Google Scholar]
- 25.Tran TD, Tran T, Fisher J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC psychiatry. 2013;13:24. doi: 10.1186/1471-244X-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sahebi A AM, Salari R. Validation of Depression Anxiety and Stress Scale (DASS-21) for an Iranian population [In Persian] Journal of Iranian Psychologists. 2005;1(4):36–54. [Google Scholar]
- 27.Samani S JB. A Study On The Reliability And Validity Of The Short Form Of The Depression Anxiety Stress Scale (Dass-21)[In Persian] Journal Of Social Sciences And Humanities Of Shiraz University. 2007;26(3):65–77. [Google Scholar]
- 28.Noorbala AA DB, Riazi-Isfahani S. Evaluation of mental disorders incidence trend in Iran[In Persian] daneshvarmed. 2014;21(112):1–10. [Google Scholar]
- 29.Ahmadvand A, Sepehrmanesh Z, Ghoreishi FS, Afshinmajd S. Prevalence of psychiatric disorders in the general population of Kashan, Iran. Archives of Iranian medicine. 2012;15(4):205–9. [PubMed] [Google Scholar]
- 30.Noorbala AA, Bagheri Yazdi SA, Asadi Lari M, Mahdavi V, Reza M. Mental health status of individuals fifteen years and older in Tehran-Iran (2009) [In Persian] Iranian journal of psychiatry and clinical psychology. 2011;16(4):479–83. [Google Scholar]
- 31.Ahmadi A, Sadr Bafghi SM, Yassini Ardekani SM, Mirzaei M, Hooshyari Z, Alavi SS, et al. Epidemiology of psychiatric disorders and the relevant comorbidities in childeren and adolescents of Yazd province in Iran. Iran J of Psychiatry. 2018;14(1):1–15. [Google Scholar]
- 32.Baradaran Eftekhari M, Setareh Forouzan A, Mirabzadeh A, Sajadi H, Dejman M, Rafiee H, et al. Mental Health Priorities in Iranian Women: Overview of Social Determinants of Mental Health. Iran J Psychiatry. 2014;9(4):241–7. [PMC free article] [PubMed] [Google Scholar]
- 33.Kvrgic S, Harhaji S, Jovanovic VM, Nikolic EA, Radic I, Cankovic S, et al. Gender differences in mental health among adult population in Vojvodina, Serbia. Iran J Public Health. 2013;42(8):833–41. [PMC free article] [PubMed] [Google Scholar]
- 34.Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry. 2017;4(1):73–82. doi: 10.1016/S2215-0366(16)30358-3. [DOI] [PubMed] [Google Scholar]
- 35.Divkolaye NSH, Burkle Jr FM. The Enduring Health Challenges of Afghan Immigrants and Refugees in Iran: A Systematic Review. PLoS Curr. 2017:9. doi: 10.1371/currents.dis.449b4c549951e359363a90a7f4cf8fc4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, et al. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183(12):E959–67. doi: 10.1503/cmaj.090292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iqbal S, Ahmad R, Ayub N. Level of depression among adolescents of religious minorities and their dominant counterparts in Pakistan. J Child Adolesc Ment Health. 2012;24(2):163–71. doi: 10.2989/17280583.2012.735506. [DOI] [PubMed] [Google Scholar]
- 38.Noorbala A, Yazdi SB, Yasamy M, Mohammad K. Mental health survey of the adult population in Iran. Br J Psychiatry. 2004;184:70–3. doi: 10.1192/bjp.184.1.70. [DOI] [PubMed] [Google Scholar]
- 39.Kingston S. Economic adversity and depressive symptoms in mothers: Do marital status and perceived social support matter? Am J Community Psychol. 2013;52(3-4):359–66. doi: 10.1007/s10464-013-9601-7. [DOI] [PubMed] [Google Scholar]
- 40.Silva M, Loureiro A, Cardoso G. Social determinants of mental health: a review of the evidence. The European Journal of Psychiatry. 2016;30(4):259–92. [Google Scholar]
- 41.Dong X, Chen R, Li C, Simon MA. Understanding depressive symptoms among community-dwelling Chinese older adults in the greater Chicago area. J Aging Health. 2014;26(7):1155–71. doi: 10.1177/0898264314527611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Waerden JE, Hoefnagels C, Hosman CM, Jansen MW. Defining subgroups of low socioeconomic status women at risk for depressive symptoms: the importance of perceived stress and cumulative risks. Int J Soc Psychiatry. 2014;60(8):772–82. doi: 10.1177/0020764014522751. [DOI] [PubMed] [Google Scholar]
- 43.Stankunas M, Kalediene R, Starkuviene S, Kapustinskiene V. Duration of unemployment and depression: a cross-sectional survey in Lithuania. BMC Public Health. 2006;6:174. doi: 10.1186/1471-2458-6-174. [DOI] [PMC free article] [PubMed] [Google Scholar]