Abstract
OBJECTIVE
We aimed to determine optimal blood pressure (BP) thresholds for minimizing coronary artery disease (CAD) risk in people with childhood-onset type 1 diabetes.
RESEARCH DESIGN AND METHODS
The Pittsburgh Epidemiology of Diabetes Complications (EDC) Study participants without known CAD at baseline (n = 605) were included and followed for 25 years. The associations of time-weighted BP measures (systolic BP [SBP], diastolic BP [DBP], and mean arterial pressure) with incident CAD were examined by using Cox models. Areas under the receiver operating characteristic curve (AUC) were summarized by different cut points of time-weighted BPs. Risk stratification analyses were then performed on the basis of BP (<120/80 vs. ≥120/80 mmHg) and HbA1c (<8% vs. ≥8%).
RESULTS
Baseline mean age was 27 years. Half of the cohort were women and 98% were white. A dose-gradient association was observed for categorized time-weighted BPs and CAD. According to AUC, the optimal cut point for SBP was 120 mmHg and for DBP was 80 mmHg. BP ≥120/80 mmHg was associated with a 1.9 times (95% CI 1.4, 2.6) greater risk of developing CAD than that for BP <120/80 mmHg. Participants with good control of both BP and HbA1c had BP <120/80 mmHg and HbA1c <8%. Those with only high BP (hazard ratio [HR] 2.0 [95% CI 1.1, 3.9]) carried a similar risk of developing CAD as those with only high HbA1c (HR 1.6 [95% CI 0.97, 2.8]).
CONCLUSIONS
The optimal BP threshold associated with minimal CAD risk is 120/80 mmHg in young adults with childhood-onset type 1 diabetes.
Introduction
Individuals with type 1 diabetes carry a substantially higher cardiovascular risk, especially at younger ages, than the general population (1). Blood pressure (BP) begins to rise at an early age in individuals with type 1 diabetes such that hypertension (defined as BP ≥140/90 mmHg or the use of BP-lowering mediations) affects over 40% of these individuals as early as in their 30s (2). Very few studies, however, have examined the impact of chronically elevated BP, from an early phase in life, on cardiovascular outcomes in this high-risk population.
Although high BP is modifiable, it continues to be a poorly treated risk factor for adverse health outcomes in the contemporary population of individuals with type 1 diabetes (3). Current guidelines from American Diabetes Association (ADA) recommend BP targets of 130/80 mmHg in individuals with diabetes who are at high cardiovascular risk (existing cardiovascular disease or 10-year cardiovascular disease risk >15%), and 140/90 mmHg in individuals with diabetes who are at low cardiovascular risk (a 10-year cardiovascular disease risk <15%) (4). Of note, existing BP management guidelines are based on evidence exclusively from middle-aged or older populations with type 2 diabetes. However, not only might the pathogenesis of hypertension differ between individuals with type 1 diabetes and those with type 2 diabetes, but also the onset of the condition occurs at a much earlier age in the former group (5). Unfortunately, evidence based on clinical trials is absent regarding optimal BP targets in type 1 diabetes. A few observational studies of type 1 diabetes have reported that a lower BP threshold (i.e., <110 or <120 mmHg) was associated with lower cardiovascular risk (6–8); however, usually only a single baseline BP measure was examined. These limited studies and the lack of clinical trials investigating lowering BP indicate insufficient data regarding BP management targets in type 1 diabetes.
The primary aim of this study, therefore, was to determine optimal BP thresholds in terms of minimizing cardiovascular risk in young adults with long-duration childhood-onset type 1 diabetes. In addition, we examined the relative importance of long-term glycemic conditions and BP in predicting cardiovascular risk in individuals with type 1 diabetes.
Research Design and Methods
Study Population
The Pittsburgh Epidemiology of Diabetes Complications (EDC) Study includes a prospective cohort of individuals with childhood-onset type 1 diabetes who were diagnosed before 17 years of age (9). The participants were seen at diagnosis, or within 1 year of diagnosis, at the Children’s Hospital of Pittsburgh between 1950 and 1980. Although clinic based, this cohort has been shown to be epidemiologically representative of the population with type 1 diabetes in Allegheny County, Pennsylvania (10). A total of 658 eligible participants were examined at study entry (baseline) between 1986 and 1988. Participants were then assessed through biennial surveys for 25 years, and through biennial examinations for the first 10 years and again at 18 and 25 years (11). Of these participants, 605 were free from coronary artery disease (CAD) at study entry and thus comprised the study population of the present analysis. Participants were followed up to their first CAD event, death, or the 25th year of the EDC Study cohort (2011–2014).
CAD Definition
CAD status was evaluated biennially from baseline to the end of the follow-up period. A CAD event was defined as new-onset angina diagnosed by an EDC Study physician, myocardial infarction confirmed by Q-waves on an electrocardiogram (Minnesota codes 1.1 or 1.2) or hospital records, angiographic stenosis ≥50%, revascularization, or ischemic electrocardiographic changes (Minnesota codes 1.3, 4.1–4.3, 5.1–5.3, and 7.1).
Assessment of BP
BP was measured by a random-zero sphygmomanometer for the initial 10 years of the study and subsequently by an aneroid device. We compared the two BP-measuring methods in a subgroup of the EDC Study participants; BP values from the two measuring methods were highly correlated (T.J.O., unpublished data). Furthermore, in the Diabetes Prevention Program Outcomes Study (DPPOS), which was conducted in the same clinic setting as the EDC Study, a validation report was published showing that our aneroid sphygmomanometer can be used to replace a mercury sphygmomanometer (12). At each clinic visit, BP was measured three times by trained and certified research staff after the participant had been peacefully sitting for 5 min in a quiet room, according to the Hypertension Detection and Follow-up Program protocol (13). The mean of the second and third readings was used in the analysis. Mean arterial pressure (MAP) was calculated as the sum of one-third of the systolic BP (SBP) and two-thirds of the diastolic BP (DBP).
The cumulative BP (mmHg-years) was determined as a sum of the products of mean BP (mmHg) from two consecutive follow-up visits multiplied by the time interval (years) between the two visits: Cumulative BP = ([BP1 + BP2]/2) × (time2 − time1) + ([BP2 + BP3]/2) × (time3 − time2) . . . (14). This cumulative variable increases as the follow-up period progresses. The time-weighted BP (mmHg) was then obtained by dividing cumulative BP by the total follow-up time: Time-weighted BP = Cumulative BP/([time2 − time1] + [time3 − time2] + . . .) (15). This weighted variable is time-invariant and reflects the entire observed follow-up period, that is, from baseline to the first CAD event if one occurred, or to death or the 25th year follow-up otherwise. This study followed participants for 25 years, with up to eight visits during that time. In addition, the time intervals varied among the eight visits (BPs were measured at baseline and years 2, 4, 6, 8, 10, 18, and 25). In this scenario, we believe a time-weighted measure is superior to a simple mean of multiple measures for reflecting the magnitude of long-term elevated BP.
Measurement of Covariates
An “ever smoker” was defined as a person who had smoked at least 100 cigarettes in his or her lifetime. The BMI was calculated as weight (kilograms) divided by the square of height (meters). Participants self-reported biennially all medication use from the study baseline. Medication classes were determined by using the Anatomical Therapeutic Chemical Classification System and Defined Daily Dose codes.
HbA1c was measured by using ion-exchange chromatography (Isolab, Akron, OH) for the first 18 months and automated high-performance liquid chromatography (Diamat; Bio-Rad, Hercules, CA) over the subsequent 10 years; the results of the two methods were highly correlated (r = 0.95). For follow-up beyond 10 years, HbA1c was measured with a DCA 2000 analyzer (Bayer, Tarrytown, NY). The assays performed on DCA and Diamat analyzers were also highly correlated (r = 0.95). The values were converted to Diabetes Control and Complications Trial (DCCT)–aligned HbA1c values by using regression equations derived from duplicate assays (16). Time-weighted HbA1c was also calculated by using the same method as that for BP measures.
Total cholesterol was determined enzymatically (17). HDL cholesterol was measured by using a precipitation technique (heparin and manganese chloride) and a modified version of the method used in the Lipid Research Clinics Program (18). Non–HDL cholesterol was determined as total cholesterol minus HDL cholesterol. Urinary albumin was determined through immunonephelometry (19). Raised albuminuria was defined as an urinary albumin excretion rate (AER) >20 μg/min (30 mg/24 h) in at least two of three validated and timed biennial urine collections (20).
Statistical Analysis
Cumulative SBP, DBP, and MAP values were calculated at each follow-up visit until the first occurrence of a CAD event for case subjects or the end of the follow-up for all others. Each time-updated cumulative (i.e., time-varying) BP variable was included in a Cox model in order to assess the association between cumulative BP and incident CAD. The models were adjusted for covariates that have previously been demonstrated to be important predictors of CAD in the Pittsburgh EDC Study cohort (21) or those that were found to be significantly associated with outcome events in the univariate analyses. Specifically, the final models were adjusted for age, sex, diabetes duration, use of antihypertensive medications, ever smoking, raised albuminuria, BMI, HbA1c, HDL cholesterol, and non–HDL cholesterol. The repeatedly measured continuous variables—that is, BMI, HbA1c, HDL cholesterol, and non–HDL cholesterol—were adjusted as time-updated means over the follow-up. Information regarding antihypertensive medication use, ever smoking, and raised albuminuria were collected from the most recent visit before the CAD event occurred (if a case subject) or the end of follow-up (all other subjects). Age and diabetes duration were from baseline data collection. This study used a time-to-event design, and we used a Cox model in which only baseline age and diabetes duration should be included.
Cox models including time-weighted (time-invariant) BP measures were constructed in order to examine a dose-gradient association between categorized BP and incident CAD. Time-weighted SBP (<110, 110 to <120 [reference], 120 to <130, 130 to <140, ≥140 mmHg), DBP (<60, 60 to <70 [reference], 70 to <80, 80 to <90, ≥90 mmHg), and MAP (<80, 80 to <90 [reference], 90 to <100, 100 to <110, ≥110 mmHg) each were categorized into five groups and tested. Model 1 was adjusted for baseline age and diabetes duration, sex, and current antihypertensive medication use. Model 2, the fully adjusted model, was further adjusted for time-weighted HbA1c; ever smoking; raised albuminuria; and updated means of BMI, HDL cholesterol, and non–HDL cholesterol over the follow-up.
Sensitivity, specificity, and the area under the receiver operating characteristic curve (AUC) were then summarized by different BP cut points (22). The Youden index criterion (23) was also applied in order to select the optimal cutoffs.
To evaluate the relative importance of long-term elevated BP versus hyperglycemia in type 1 diabetes, we stratified the participants into four groups on the basis of time-weighted BP and time-weighted HbA1c: group 1 (the reference group) had SBP/DBP <120/80 mmHg and HbA1c <8%; group 2 (high BP only) had SBP/DBP ≥120/80 mmHg and HbA1c <8%; group 3 (high HbA1c only) had SBP/DBP <120/80 mmHg and HbA1c ≥8%); and group 4 (both high BP and high HbA1c) had SBP/DBP ≥120/80 mmHg and HbA1c ≥8%. We built Cox models to estimate the hazard ratios (HRs) among these groups, controlling for the same set of covariates as described above. With this risk stratification, we were able to estimate the HRs of high BP only, high HbA1c only, and both “high” relative to the reference of both “low.” We also applied a similar risk stratification strategy to time-weighted MAP (<90 vs. ≥90 mmHg) and HbA1c (<8% vs. ≥8%). In addition to the risk stratification analysis, we also tested the interaction effects of high BP (<120/80 vs. ≥120/80 mmHg) with HbA1c and high MAP (<90 vs. ≥90 mmHg) with HbA1c within the Cox models; model-based interaction plots were then displayed.
In addition, to understand the potential impact of the two different BP cutoffs, 120/80 and 140/90 mmHg, on CAD outcome, we estimated the population attributable risk fraction (PARF) for each of the cutoffs, using the equation PARF = (P ∗ [IExposed − IUnexposed])/Itotal, where P represents the prevalence of a given risk factor; IExposed represents event incidence rate in the exposed population; IUnexposed, the event incidence rate in the unexposed population; and Itotal, the incidence rate in the total population. In this case, a PARF represents the percentage of CAD cases in this type 1 diabetes cohort that can be attributed to BP ≥120/80 and ≥140/90 mmHg, respectively.
In the exploratory sensitivity analysis, we examined the association of high BP (time-weighted SBP/DBP ≥120/80 mmHg or time-weighted MAP ≥90 mmHg) with incident CAD in the subgroups of participants who were never treated and who were ever treated with antihypertensive medications.
A two-sided P value <0.05 was considered significant. Analyses were performed by using SAS software version 9.4 (SAS Institute, Cary, NC) and R software version 3.5.1 (R Core Team, Vienna, Austria).
Results
Among the 605 EDC Study participants who were free from clinical CAD at study entry, the mean age was 27 years and the mean diabetes duration was 19 years. The mean age at diabetes onset was 8 years. Of all the participants, half of the cohort were women; 13% took antihypertensive medications at baseline (Table 1).
Table 1.
Clinical characteristics of the study population at baseline
| Variables | Total (N = 605) | Time-weighted BP (mmHg) |
Incident CAD |
||
|---|---|---|---|---|---|
| <120/80 (n = 387) | ≥120/80 (n = 218) | No (n = 386) | Yes (n = 219) | ||
| Age, years | 27.2 (7.7) | 25.7 (7.5) | 29.8 (7.4)** | 24.8 (7.2) | 31.3 (6.8)** |
| Age at diabetes onset, years | 8.2 (4.1) | 8.0 (4.1) | 8.5 (4.0) | 8.1 (4.2) | 8.3 (3.8) |
| Diabetes duration, year | 19.0 (7.4) | 17.7 (7.1) | 21.3 (7.4)** | 16.7 (6.6) | 23.0 (7.1)** |
| Female sex, % (n) | 49.8 (301) | 57.1 (221) | 36.7 (80)** | 51.0 (197) | 47.5 (104) |
| SBP, mmHg | 112.9 (14.7) | 106.3 (8.7) | 124.6 (16.1)** | 109.9 (12.3) | 118.1 (17.1)** |
| DBP, mmHg | 72.5 (10.8) | 68.1 (7.9) | 80.2 (11.1)** | 70.8 (9.8) | 75.5 (12.0)** |
| PP, mmHg | 40.4 (10.3) | 38.1 (8.1) | 44. 4 (12.4)** | 39.1 (9.6) | 42.7 (10.7)** |
| MAP, mmHg | 85.9 (11.3) | 80.9 (7.2) | 95.0 (11.6)** | 83.8 (9.8) | 89.7 (13.0)** |
| Antihypertensive medication use, % (n) | 12.9 (78) | 5.7 (21) | 26.6 (57)** | 7.6 (28) | 23.0 (50)** |
| Hypertension, % (n) | 14.4 (87) | 3.6 (14) | 33.5 (73)** | 7.8 (30) | 26.0 (57)** |
| Pulse rate, bpm | 78 (10) | 76.9 (9.1) | 80.5 (10.6)** | 77.4 (9.8) | 79.6 (9.7)* |
| HbA1c, % (mmol/mol) | 8.8 (73) | 8.7 (72) | 8.8 (73) | 8.8 (73) | 8.7 (72) |
| Ever smoker, % (n) | 37.2 (225) | 36.2 (140) | 39.0 (85) | 30.3 (117) | 49.3 (108)** |
| BMI, kg/m2 | 23.5 (3.2) | 23.2 (3.2) | 24.1 (3.2)** | 23.2 (3.2) | 24.0 (3.2)** |
| High WHR,† % (n) | 4.8 (29) | 5.0 (19) | 4.6 (10) | 5.2 (20) | 4.2 (9) |
| Urinary AER, μg/min | 14 (7, 102) | 11 (6, 25) | 10 (12, 985)** | 11 (7, 42) | 39 (9, 470)** |
| Raised albuminuria,‡ % (n) | 44.4 (269) | 29.7 (115) | 70.6 (154)** | 36.5 (141) | 58.5 (128)** |
| Total cholesterol, mg/dL | 189.6 (41.0) | 182.7 (36.0) | 201.4 (46.2)** | 182.5 (38.9) | 202.2 (41.9)** |
| LDL cholesterol, mg/dL | 114.7 (33.8) | 107.9 (28.2) | 126.4 (39.1) | 108.0 (30.2) | 126.7 (36.6) |
| Non–HDL cholesterol, mg/dL | 135.6 (41.0) | 128.0 (36.7) | 149.6 (46.4)** | 127.6 (38.8) | 149.9 (42.9)** |
| HDL cholesterol, mg/dL | |||||
| Men | 49.5 (9.8) | 50.1 (9.9) | 48.7 (9.7) | 50.8 (10.0) | 47.3 (9.0)** |
| Women | 58.4 (12.9) | 58.4 (12.6) | 58.6 (13.7) | 58.9 (13.0) | 57.5 (12.5) |
| Triglycerides, mg/dL | 82 (60, 121) | 77 (57, 106) | 92 (66, 141)** | 76 (57, 108) | 92 (70, 140)** |
Data presented as percentage (number) are categorical variables; data are otherwise presented as the mean (SD) or median (first quantile, third quantile) and are continuous variables. PP, pulse pressure; WHR, waist-to-hip ratio.
*P < 0.05.
**P < 0.01 between comparisons of time-weighted BP <120/80 vs. ≥120/80 mmHg, and no CAD vs. CAD.
†High WHR was defined as >0.9 in men or >0.85 in women.
‡Raised albuminuria was defined as a urinary AER >20 μg/min (30 mg/24 h) in at least two of three validated and timed biennial urine collections.
A total of 219 individuals (36.2%) experienced at least one CAD event over 25 years of follow-up, for an incidence rate of 20.3 per 1,000 person-years. Compared with participants without incident CAD, those who developed CAD were more likely to be older, have a longer duration of diabetes, smoke, take antihypertensive medications, have raised albuminuria, have higher BMI, and have higher BP and non–HDL cholesterol at baseline (Table 1).
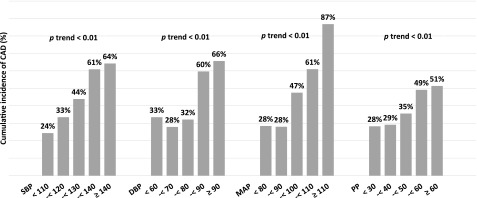
Time-weighted SBP, DBP, and MAP were all approximately normally distributed, with a mean (SD) of 116.3 mmHg (13.7 mmHg) for SBP, 72.3 mmHg (9.6 mmHg) for DBP, and 87.0 mmHg (10.1 mmHg) for MAP. Overall, the cumulative incidence of CAD over 25 years of follow-up progressively increased as time-weighted BP increased (all P for trend <0.01) (Fig. 1). At 2, 4, 6, 8, 10, 18, and 25 years of follow-up, the mean (SD) cumulative BP values were 235 (52), 497 (82), 704 (98), 933 (116), 1,144 (134), 2,104 (198), and 2,830 (261) mmHg-years for SBP, and 150 (34), 316 (53), 447 (62), 590 (71), 723 (83), 1,307 (139), and 1,735 (170) mmHg-years for DBP (Supplementary Fig. 1).
Figure 1.
Cumulative incidence of CAD by categorized timed-weighted BP over 25 years of follow-up. χ2 Test was used for testing the relation between categorized BP and cumulative incidence of CAD. PP, pulse pressure.
The time-updated cumulative SBP, DBP, and MAP were separately examined in three Cox models. All three cumulative BP measures independently and significantly predicted the risk of incident CAD after adjusting for age; sex; diabetes duration; ever smoking; raised albuminuria; antihypertensive medication use; and updated mean BMI, HbA1c, HDL cholesterol, and non–HDL cholesterol. The adjusted HR (95% CI) of incident CAD per 500 mmHg-years increase was 1.3 (1.04, 1.7) for cumulative SBP, 1.5 (1.02, 2.2) for cumulative DBP, and 1.4 (1.03, 2.0) for cumulative MAP (Supplementary Table 1).
The dose-gradient association of each time-weighted BP measure (SBP, DBP, and MAP) with incident CAD is presented in Table 2. In the fully adjusted model (model 2), for SBP, with 110 to <120 mmHg as the reference group, the HR (95% CI) associated with incident CAD for <110, 120 to <130, 130 to <140, and ≥140 mmHg was 1.1 (0.7, 1.6), 1.6 (1.1, 2.3), 1.9 (1.2, 3.0), and 2.6 (1.6, 4.5), respectively. For DBP, with 60 to <70 mmHg as the reference group, the HR (95% CI) for <60, 70 to <80, 80 to <90, and ≥90 mmHg was 0.9 (0.5, 1.7), 1.8 (1.2, 2.7), 4.5 (2.9, 6.9), and 5.6 (3.0, 10.3), respectively. For MAP, with 80 to <90 mmHg as the reference group, the HR (95% CI) for <80, 90 to <100, 100 to <110, and ≥110 mmHg was 0.9 (0.6, 1.4), 2.5 (1.7, 3.5), 2.9 (1.8, 4.9), and 8.5 (4.3, 16.8), respectively.
Table 2.
Dose-gradient associations of time-weighted BP and CAD in individuals with childhood-onset type 1 diabetes
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| SBP, mmHg | ||||
| <110 | 0.9 (0.6, 1.3) | 0.558 | 1.1 (0.7, 1.6) | 0.801 |
| 110 to <120 | Reference | Reference | ||
| 120 to <130 | 1.7 (1.1, 2.5) | 0.013 | 1.6 (1.1, 2.3) | 0.027 |
| 130 to <140 | 2.3 (1.4, 3.7) | <0.001 | 1.9 (1.2, 3.0) | 0.011 |
| ≥140 | 3.3 (2.0, 5.5) | <0.001 | 2.6 (1.6, 4.5) | <0.001 |
| DBP, mmHg | ||||
| <60 | 1.1 (0.6, 1.9) | 0.813 | 0.9 (0.5, 1.7) | 0.825 |
| 60 to <70 | Reference | Reference | ||
| 70 to <80 | 1.9 (1.3, 2.8) | <0.001 | 1.8 (1.2, 2.7) | 0.002 |
| 80 to <90 | 5.9 (3.9, 8.9) | <0.001 | 4.5 (2.9, 6.9) | <0.001 |
| ≥90 | 9.2 (5.2, 16.3) | <0.001 | 5.6 (3.0, 10.3) | <0.001 |
| MAP, mmHg | ||||
| <80 | 0.9 (0.6, 1.3) | 0.556 | 0.9 (0.6, 1.4) | 0.718 |
| 80 to <90 | Reference | Reference | ||
| 90 to <100 | 2.9 (2.1, 4.2) | <0.001 | 2.5 (1.7, 3.5) | <0.001 |
| 100 to <110 | 4.1 (2.6, 6.6) | <0.001 | 2.9 (1.8, 4.9) | <0.001 |
| ≥110 | 13.9 (7.2, 26.9) | <0.001 | 8.5 (4.3, 16.8) | <0.001 |
Model 1 was adjusted for age, sex, diabetes duration, and current use of antihypertensive medications. Model 2 was adjusted for the model 1 variables as well as time-weighted HbA1c; ever smoking; updated mean BMI, HDL cholesterol, and non–HDL cholesterol; and raised albuminuria.
The results of sensitivity, specificity, and AUC by different cut points of the time-weighted BPs are summarized in Supplementary Table 2. Among the SBP cutoffs of ≥110, ≥120, ≥130, and ≥140 mmHg, ≥120 mmHg provided the highest AUC (0.614), with a sensitivity of 48% and a specificity of 75%. In evaluating DBP with cutoffs of ≥60, ≥70, ≥80, and ≥90 mmHg, the cutoff with the highest AUC (0.605) was ≥80 mmHg. MAP ≥90 mmHg showed the best discrimination (AUC 0.621) compared with cutoffs of ≥80, ≥100, and ≥110 mmHg. According to the Youden index criterion, the optimal cutoff for SBP was 116.1 mmHg, for DBP was 78.6 mmHg, and for MAP was 91.4 mmHg.
In the tests for interaction, both of the two interaction terms—high BP (<120/80 vs. ≥120/80 mmHg) × HbA1c (HR 0.839; P = 0.086) and MAP (<90 vs. ≥90 mmHg) × HbA1c (HR 0.786; P = 0.018) showed negative β coefficients (Supplementary Fig. 2). The interaction term high BP × HbA1c is not significant but close, whereas that of MAP × HbA1c is significant. Table 3 presents stratified risk analysis for both BP and MAP by HbA1c. Compared with participants with a time-weighted BP <120/80 mmHg, those with a BP ≥120/80 mmHg carried an almost doubled increased risk of CAD (HR 1.9 [95% CI 1.4, 2.6]) in the fully adjusted model. When the participants were categorized into four groups according to time-weighted BP (<120/80 vs. ≥120/80 mmHg) and time-weighted HbA1c (<8% vs. ≥8%), the group with high BP only (BP ≥120/80 mmHg and HbA1c <8%; HR 2.0 [95% CI 1.06, 3.9]) had a similar HR for predicting CAD risk as the group with high HbA1c only (BP <120/80 mmHg and HbA1c ≥8%; HR 1.6 [95% CI 0.97, 2.8]) (Table 3). In the risk stratification analysis by MAP (<90 vs. ≥90 mmHg) and HbA1c (<8% vs. ≥8%), the group with only high MAP (MAP ≥90 mmHg and HbA1c <8%) tended to have a higher CAD risk than the group with high HbA1c only (MAP <90 mmHg and HbA1c ≥8%), though the two 95% CIs largely overlapped (HR 3.4 [95% CI 1.8, 6.5] vs. 1.9 [1.1, 3.2]).
Table 3.
Risk stratification by time-weighted BP and time-weighted HbA1c for predicting CAD risk in individuals with childhood-onset type 1 diabetes
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| HR (95% CI) |
P value | HR (95% CI) | P value | |
| SBP/DBP | ||||
| BP ≥120/80 vs. <120/80 mmHg | 2.4 (1.8, 3.3) | <0.001 | 1.9 (1.4, 2.6) | <0.001 |
| BP <120/80 mmHg and HbA1c <8% | Reference | Reference | ||
| BP ≥120/80 mmHg and HbA1c <8% | 2.3 (1.3, 4.3) | 0.007 | 2.0 (1.06, 3.9) | 0.033 |
| BP <120/80 mmHg and HbA1c ≥8% | 2.2 (1.4, 3.6) | 0.002 | 1.6 (0.97, 2.8) | 0.071 |
| BP ≥120/80 mmHg and HbA1c ≥8% | 5.8 (3.5, 9.7) | <0.001 | 3.3 (1.9, 6.0) | <0.001 |
| MAP | ||||
| MAP ≥90 vs. <90 mmHg | 3.5 (2.6, 4.7) | <0.001 | 2.6 (1.6, 3.5) | <0.001 |
| MAP <90 mmHg and HbA1c <8% | Reference | Reference | ||
| MAP ≥90 mmHg and HbA1c <8% | 4.6 (2.5, 8.4) | <0.001 | 3.4 (1.8, 6.5) | <0.001 |
| MAP <90 mmHg and HbA1c ≥8% | 2.6 (1.6, 4.2) | <0.001 | 1.9 (1.1, 3.2) | 0.016 |
| MAP ≥90 mmHg and HbA1c ≥8% | 8.5 (5.1, 14.1) | <0.001 | 4.9 (2.7, 8.7) | <0.001 |
Model 1 was adjusted for age, sex, diabetes duration, and current use of antihypertensive medications. Model 2 was adjusted for the model 1 variables plus ever smoking; updated mean BMI, HDL cholesterol, and non–HDL cholesterol; and raised albuminuria.
In the sensitivity analyses (Supplementary Table 3), a high BP (≥120/80 mmHg) was associated with a significantly higher risk in both subgroups who were never (HR 2.3 [95% CI 1.3, 4.1]) and ever (HR 2.7 [95% CI 1.7, 4.1]) treated with antihypertensive medication over the study period. (The dose-gradient association of time-weighted HbA1c and CAD is displayed in Supplementary Table 4.)
According to the PARF calculations (Supplementary Fig. 3), the BP cutoff of 140/90 mmHg had a PARF of 19.1%. The BP cutoff of 120/80 mmHg (PARF 37.4%) identified 18.3% of CAD cases within this cohort with type 1 diabetes.
Our study cohort was young at baseline (mean age 27 years), and only 50 incident stroke events (8%; including both hemorrhagic and ischemic stroke cases) were identified over the 25-year follow-up. Unfortunately, the data do not have enough power to allow us to fully examine the BP-stroke association. However, we conducted a sensitivity analysis for major atherosclerotic cardiovascular disease, a composite outcome of stroke, myocardial infarction, and cardiovascular death (Supplementary Tables 5 and 6). The results are consistent with findings for CAD outcomes. The analysis for hard CAD only (revascularization, myocardial infarction, and CAD-related death) also yielded consistent results (data not shown).
Conclusions
In this study, long-term cumulative BP independently predicted the risk of CAD in individuals who had been living with type 1 diabetes since childhood. We observed a dose-gradient association between time-weighted BP and incident CAD. Time-weighted SBP and DBP, starting from approximately 120 and 80 mmHg, respectively, strongly predicted CAD risk in this group of individuals with childhood-onset type 1 diabetes. Furthermore, chronically elevated BP and HbA1c showed comparable magnitudes of effect on long-term CAD risk prediction, indicating that BP control is at least as equally important as glycemic control for reducing cardiovascular risk in patients with type 1 diabetes.
In this study, the dose-gradient association analysis using Cox models and AUC calculations yielded consistent results to support that cutoffs of >120 mmHg for SBP and >90 mmHg for MAP maximally predicted CAD risk in this group of individuals with type 1 diabetes. DBP, starting from 70 mmHg, predicted CAD in the dose-gradient association models, whereas a cutoff of >80 mmHg showed the highest AUC. Given that a DBP <70 mmHg may increase cardiovascular risk (24,25), we suggested a cutoff of 80 mmHg for DBP in this study. Therefore we used cutoffs of 120 mmHg for SBP, 80 mmHg for DBP, and 90 mmHg for MAP for risk stratification. Time-weighted HbA1c showed a remarkably increased risk from 8%, according to the analysis of the time-weighted HbA1c categories and incident CAD in this study (Supplementary Table 4); thus we used a cutoff of 8% for risk stratification.
This study is unique in that it provides information about how chronically elevated BP during youth to midlife affects cardiovascular outcomes in type 1 diabetes. In this work we used both time-updated cumulative BP exposures (mmHg-years) and time-weighted BP (mmHg) to quantify long-term BP. A time-weighted BP accounts for the amount of time that a participant has a given BP level. Hence, it might better reflect the true BP over time than would a BP obtained on a single occasion (i.e., at baseline or current), or a simple average of multiple measures over time (i.e., an updated mean).
Although existing trial-based evidence does not support the benefit of a lower BP target (i.e., <120 mmHg) among individuals with type 2 diabetes (e.g., the ACCORD study) (26), we believe it is inappropriate to simply extrapolate findings from an older population with type 2 diabetes to a younger population with type 1 diabetes. A few observational studies conducted within cohorts with type 1 diabetes have shown a lower cardiovascular risk at lower BPs (6–8), even within the normal range denoted by current ADA recommendations (<130/80 mmHg at higher cardiovascular risk, or <140/90 mmHg at lower cardiovascular risk) (4). The findings of this study thus support even lower BPs (120/80 mmHg) for young adults with type 1 diabetes and are based on a study that included a cohort for whom the follow-up period was up to 25 years, that used time-weighted BP, and that adjusted for a wide range of potential risk factors.
In the exploratory sensitivity analyses in subgroups of patients who were never and who were ever treated with antihypertensive medications, high BP (SBP/DBP >120/80 mmHg or MAP >90 mmHg) was consistently shown to be an independent predictor of incident CAD in both subgroups, reflecting the inadequacy of BP control even in treated individuals with type 1 diabetes.
The recent results from the DCCT/Epidemiology of Diabetes Interventions and Complications (EDIC) study suggested that a BP >120/70 mmHg was associated with an increased risk of adverse renal outcomes in individuals with type 1 diabetes (27). The results of our study complement these findings, as we found a threshold of 120/80 mmHg to be associated with incident CAD. Although we also observed, based on the Cox models, that DBP was significantly associated with CAD risk beginning at 70 mmHg, the AUC was highest at the 80-mmHg cutoff. Overall, our observational data and those of others might provide support for conducting clinical trials that include individuals with type 1 diabetes in order to further test the hypothesis that tighter BP control benefits this high-risk population.
The clinical management of type 1 diabetes has traditionally focused on glycemic control (28). In this study, chronically elevated BP in participants who already had reasonably good glycemic control was independently associated with an increased risk of CAD, and the magnitude of effect was comparable to that in those who have poor glycemic control but reasonably good BP. This suggests that these two modifiable risk factors are similarly important in predicting cardiovascular risk in individuals with long-standing type 1 diabetes. Intriguingly, however, we found a “negative” interaction effect between high BP and HbA1c, such that the impact of BP is greater in those with lower HbA1c. We think these findings have major clinical implications, emphasizing the need for an initial focus on glycemic control when HbA1c is very high, but as HbA1c approaches the high end of the normal range, increased focus on BP becomes critical.
Because of the lack of interventional randomized trials with clinical outcomes related to BP management goals in type 1 diabetes, observational evidence from an epidemiologically representative and well-characterized cohort with type 1 diabetes, such as that in the EDC Study, could be important and helpful for developing clinical recommendations. Thus, if BP trials are not going to be conducted in this high-risk population, it would seem reasonable to strengthen the American Diabetes Association recommendations by embracing a lower goal of 120/80 mmHg for young and middle-aged adults with childhood-onset type 1 diabetes.
The strengths of our investigation include the well-characterized cohort of individuals with childhood-onset type 1 diabetes, the standardized measurements, the long follow-up period over 25 years, and the application of cumulative and time-weighted BP measures that are able to reflect long-term high BP. Over the entire study period, BP was measured by trained and certified research staff who strictly followed the standard protocol (13).
However, we also recognize a number of limitations. The cumulative BP in this analysis does not represent the entire history of disease (i.e., from the diagnosis of type 1 diabetes). The EDC Study is a historical, prospective study of a cohort with type 1 diabetes, and thus participants had already been exposed to the disease for a certain amount of time before entering the study (mean diabetes duration at baseline 19 years). Because of the absence of data from before baseline, we were unable to accurately estimate the BP in this left-censored period (from diabetes diagnosis to study baseline). However, when we arbitrarily estimated the cumulative BP before baseline as the product of baseline BP and baseline diabetes duration (BP1 × [time at study baseline − time at diabetes diagnosis]) and added it to the current cumulative BP measure, the results were consistent regarding the optimal BP cutoffs associated with minimal CAD risk (data not shown). In addition, because of the observational nature of the study, our interpretation of the results might not reflect the direct causal effects of a lower BP target on outcome end points. These results ideally need to be confirmed in randomized clinical trials. Our sample consists primarily of white individuals with type 1 diabetes and therefore may not be representative of other ethnic or racial groups. Furthermore, these findings focus only on CAD events; the effects of BP and glycemia on other clinical outcomes were not addressed.
In conclusion, time-weighted BP analyses suggest that a BP of 120/80 mmHg maximally predicts CAD events over 25 years of follow-up. Chronically elevated BP and glycemia are similarly important in predicting cardiovascular end points. These findings indicate the need for those setting treatment guidelines to consider lower BP goals (120/80 mmHg) than now exist (130/80 mmHg if at high cardiovascular risk or 140/90 mmHg if at lower cardiovascular risk), especially for young adults with childhood-onset type 1 diabetes, like those in the EDC Study cohort. In the absence of any pending or existing direct evidence from clinical outcome trials, which sadly do not seem likely to be conducted, such review should take place sooner than later.
Supplementary Material
Article Information
Acknowledgments. The authors thank the staff and the participants of the EDC Study for their contributions.
Funding. Research reported in this study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (grant no. R01-DK-034818) and the Rossi Memorial Fund.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.G. researched data and wrote the manuscript. M.M.B., M.F.M., and A.I.N. contributed to the discussion and reviewed and edited the manuscript. T.J.O. and T.C. researched data, contributed to the discussion, and reviewed and edited the manuscript. T.J.O. and T.C. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. This study was presented at the 79th Scientific Sessions of the American Diabetes Association, San Francisco, CA, 7–11 June 2019.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc19-0480/-/DC1.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.Miller RG, Mahajan HD, Costacou T, Sekikawa A, Anderson SJ, Orchard TJ. A contemporary estimate of total mortality and cardiovascular disease risk in young adults with type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2016;39:2296–2303 [DOI] [PMC free article] [PubMed]
- 2.Maahs DM, Kinney GL, Wadwa P, et al. . Hypertension prevalence, awareness, treatment, and control in an adult type 1 diabetes population and a comparable general population. Diabetes Care 2005;28:301–306 [DOI] [PubMed] [Google Scholar]
- 3.Miller RG, Secrest AM, Ellis D, Becker DJ, Orchard TJ. Changing impact of modifiable risk factors on the incidence of major outcomes of type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2013;36:3999–4006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association 10. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S103–S123 [DOI] [PubMed] [Google Scholar]
- 5.Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet 2012;380:601–610 [DOI] [PubMed] [Google Scholar]
- 6.Fuller JH, Stevens LK, Wang SL; WHO Multinational Study Group . Risk factors for cardiovascular mortality and morbidity: the WHO Mutinational Study of Vascular Disease in Diabetes. Diabetologia 2001;44(Suppl. 2):S54–S64 [DOI] [PubMed] [Google Scholar]
- 7.Orchard TJ, Forrest KY, Kuller LH, Becker DJ; Pittsburgh Epidemiology of Diabetes Complications Study . Lipid and blood pressure treatment goals for type 1 diabetes: 10-year incidence data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2001;24:1053–1059 [DOI] [PubMed] [Google Scholar]
- 8.Sibal L, Law HN, Gebbie J, Dashora UK, Agarwal SC, Home P. Predicting the development of macrovascular disease in people with type 1 diabetes: a 9-year follow-up study. Ann N Y Acad Sci 2006;1084:191–207 [DOI] [PubMed] [Google Scholar]
- 9.Orchard TJ, Dorman JS, Maser RE, et al. . Prevalence of complications in IDDM by sex and duration. Pittsburgh Epidemiology of Diabetes Complications Study II. Diabetes 1990;39:1116–1124 [DOI] [PubMed] [Google Scholar]
- 10.Wagener DK, Sacks JM, LaPorte RE, Macgregor JM. The Pittsburgh study of insulin-dependent diabetes mellitus. Risk for diabetes among relatives of IDDM. Diabetes 1982;31:136–144 [DOI] [PubMed] [Google Scholar]
- 11.Pambianco G, Costacou T, Ellis D, Becker DJ, Klein R, Orchard TJ. The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes 2006;55:1463–1469 [DOI] [PubMed] [Google Scholar]
- 12.Ma Y, Temprosa M, Fowler S, et al.; Diabetes Prevention Program Research Group . Evaluating the accuracy of an aneroid sphygmomanometer in a clinical trial setting. Am J Hypertens 2009;22:263–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borhani N, Kass E, Langford H, Payne G, Remington R, Stamler J. The hypertension detection and follow-up program: hypertension detection and follow-up program cooperative group. Prev Med 1976;5:207–215 [DOI] [PubMed] [Google Scholar]
- 14.Pool LR, Ning H, Wilkins J, Lloyd-Jones DM, Allen NB. Use of long-term cumulative blood pressure in cardiovascular risk prediction models. JAMA Cardiol 2018;3:1096–1100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang YX, Song L, Xing AJ, et al. . Predictive value of cumulative blood pressure for all-cause mortality and cardiovascular events. Sci Rep 2017;7:41969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prince CT, Becker DJ, Costacou T, Miller RG, Orchard TJ. Changes in glycaemic control and risk of coronary artery disease in type 1 diabetes mellitus: findings from the Pittsburgh Epidemiology of Diabetes Complications Study (EDC). Diabetologia 2007;50:2280–2288 [DOI] [PubMed] [Google Scholar]
- 17.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem 1974;20:470–475 [PubMed] [Google Scholar]
- 18.Warnick GR, Albers JJ. Heparin--Mn2+ quantitation of high-density-lipoprotein cholesterol: an ultrafiltration procedure for lipemic samples. Clin Chem 1978;24:900–904 [PubMed] [Google Scholar]
- 19.Ellis D, Coonrod BA, Dorman JS, et al. . Choice of urine sample predictive of microalbuminuria in patients with insulin-dependent diabetes mellitus. Am J Kidney Dis 1989;13:321–328 [DOI] [PubMed] [Google Scholar]
- 20.Costacou T, Orchard TJ. Cumulative kidney complication risk by 50 years of type 1 diabetes: the effects of sex, age, and calendar year at onset. Diabetes Care 2018;41:426–433 [DOI] [PMC free article] [PubMed]
- 21.Zgibor JC, Ruppert K, Orchard TJ, et al. Development of a coronary heart disease risk prediction model for type 1 diabetes: the Pittsburgh CHD in Type 1 Diabetes Risk Model. Diabetes Res Clin Pract 2010;88:314–321 [DOI] [PMC free article] [PubMed]
- 22.Robin X, Turck N, Hainard A, et al. . pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 2011;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.López-Ratón M, Rodríguez-Álvarez MX, Suárez CC, Sampedro FG. OptimalCutpoints : an R package for selecting optimal cutpoints in diagnostic tests. J Stat Softw 2014;61:1–36 [Google Scholar]
- 24.McEvoy JW, Chen Y, Rawlings A, et al. Diastolic blood pressure, subclinical myocardial damage, and cardiac events: implications for blood pressure control. J Am Coll Cardiol 2016;68:1713–1722 [DOI] [PMC free article] [PubMed]
- 25.Franklin SS, Gokhale SS, Chow VH, et al. . Does low diastolic blood pressure contribute to the risk of recurrent hypertensive cardiovascular disease events? The Framingham Heart Study. Hypertension 2015;65:299–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ACCORD Study Group; Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed]
- 27.Ku E, McCulloch CE, Mauer M, Gitelman SE, Grimes BA, Hsu C. Association between blood pressure and adverse renal events in type 1 diabetes. Diabetes Care 2016;39:2218–2224 [DOI] [PMC free article] [PubMed]
- 28.Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: the DCCT/EDIC study 30-year follow-up. Diabetes Care 2016;39:686–693
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.