Abstract
Background:
Syndesmotic injuries can lead to long-term complications; hence, they require careful management. Conservative treatment is adequate when 1 syndesmotic ligament is injured, but surgery is often necessary to achieve articular congruity when 3 syndesmotic ligaments are ruptured. However, there is some controversy over the best treatment for 2-ligament injuries.
Purpose:
To evaluate the effect of a controlled ankle motion (CAM) walking boot on syndesmotic instability following iatrogenic isolated anterior inferior tibiofibular ligament (AiTFL) injury and combined AiTFL/interosseous ligament (IOL) injuries in a cadaveric simulated weightbearing model.
Study Design:
Controlled laboratory study.
Methods:
Ten cadaveric specimens were dissected to expose the tibial plateau and syndesmosis. The specimens were fitted to a custom-made device, and a reproducible axial load of 750 N was applied. Iatrogenic rupture of the syndesmotic ligaments (AiTFL + IOL) was done sequentially. Uninjured syndesmoses, isolated AiTFL rupture, and combined AiTFL/IOL rupture were compared with and without axial loading (AL) and CAM boot. The distal tibiofibular relationship was evaluated using a previously validated computed tomography scan measurement system. Wilcoxon tests for paired samples and nonparametric data were used.
Results:
The only difference noted in the distal tibiofibular relationship during AL was an increase in the external rotation of the fibula when using the CAM boot. This was observed with AiTFL rupture (8.40° vs 11.17°; P = .009) and combined AiTFL/IOL rupture (8.81° vs 11.97°; P = .005).
Conclusion:
AL did not cause a significant displacement between the tibia and fibula, even when 2 ligaments were ruptured. However, the CAM boot produced a significant external rotation with 1 or 2 injured ligaments.
Clinical Relevance:
Further studies are needed to assess the capacity of the CAM walking boot to prevent malreduction when external rotation forces are applied to the ankle. Moreover, special care should be taken during the fitting of the CAM boot to avoid overinflation of the cushions.
Keywords: syndesmotic injury, weightbearing, CAM orthopaedic boot, high ankle sprain
Ankle sprains are among the most common lower-limb injuries in athletes.10,12,14,17 Typically, they involve the lower lateral ligaments of the ankle but can also affect the syndesmosis in 1% to 25% of all ankle sprains.6,9,12,16,22 The incidence of syndesmotic sprains is higher in athletes, especially those involved in contact sports or with rigid ankle immobilization in a boot.4,6,9,12,14,22,19,26–28
Syndesmotic sprains are graded according to the ligaments involved; each additional ligament is correlated with increasing instability. The tibia and the fibula are linked together by the anterior inferior tibiofibular ligament (AiTFL), posterior inferior tibiofibular ligament (PiTFL), interosseous ligament (IOL), and, finally, transverse tibiofibular ligament, also sometimes defined as the deep portion of the PiTFL.6,11,17
Adequate management of syndesmotic injuries is crucial because of the vital role that articulation plays in load distribution and walking.3,5,19,23 Inadequate diagnosis and treatment can lead to recurrent syndesmotic instability, early arthritis, pain, and poor functional outcomes.3,13,22,24,25 When all 3 ligaments (AiTFL, IOL, and PiTFL) are disrupted, there is instability and a clear diastasis of the syndesmosis that indicate the need for surgical fixation.1,6,16,17,19,22,28 When 1 ligament is ruptured (usually the AiTFL),2,25 the syndesmosis is still stable enough to treat the injury with standard nonoperative management, combining short-term immobilization and a rehabilitation program.
The diagnosis and management of 2-ligament injuries (AiTFL and IOL) are less clear. When there is no diastasis of the syndesmosis observed on radiographs, assessing injury severity becomes more challenging.16,17,28 Ogilvie-Harris et al21 showed that when more than 2 components of the syndesmosis are ruptured, there is 50% less resistance to a lateral translation, which may result in joint instability. Even if mortise radiographs seem normal, these cases can present with soft tissue damage that can lead to instability in a dynamic situation.16 Therefore, the best treatment for syndesmotic injury with disruption of 2 ligaments is still unclear.
The primary goal of the present study was to evaluate the effect of a controlled ankle motion (CAM) walking boot on syndesmotic instability following iatrogenic isolated AiTFL injury and combined AiTFL/IOL injury under weightbearing conditions. Our hypothesis was that the CAM orthopaedic boot is able to stabilize the syndesmosis in axial loading (AL), even with 2 ruptured ligaments.
Methods
We used 10 fresh-frozen paired cadaveric specimens (taken from 4 males and 1 female; average age, 71 years), from mid-thigh to toes, with all soft tissues preserved. Specimens were removed from the freezer (–22°C) 24 to 30 hours before the experiment, and thawed at room temperature. Before imaging, all specimens were dissected proximally to expose the tibial plateau and the syndesmosis distally, using an anterolateral approach (Figure 1). This study was approved by an ethics committee, and the specimens were provided by Sherbrooke University.
Figure 1.

Ankle dissection by an anterolateral approach to expose syndesmotic ligamental structures and dissect the anterior inferior tibiofibular ligament and interosseous ligament sequentially.
Radiographs confirmed that none of the specimens had suffered from severe arthritis or previous fractures. The cadaveric legs were then studied with a computed tomography (CT) scan using a custom-made device to allow stabilization and good-quality imaging.
A rectangular leg holder was designed with 3-dimensionally printed foot and tibial plateau supports. Two 12-inch fully threaded rods were inserted into both sides of the holder to facilitate manipulation. An Omegadyne load cell was installed between these 2 rods to ensure an adequate measurement of the AL force before CT imaging. The loading device was designed to simulate weightbearing by transferring a force of 750 N through the ankle. This 750-N force represents the weight of an average 168-lb person and is similar to what was used in other cadaveric studies.3,8,10,14 The leg was placed in neutral dorsiflexion to facilitate AL simulation (Figures 2 and 3). When the CAM orthopaedic boot was placed on the cadaveric leg, the inflatable cushions were inflated to their maximum, to fit each specimen correctly. Two CAM orthopaedic boots of the same model (Aircast) were used for all specimens, and there were no changes in the CAM boots during the manipulations.
Figure 2.
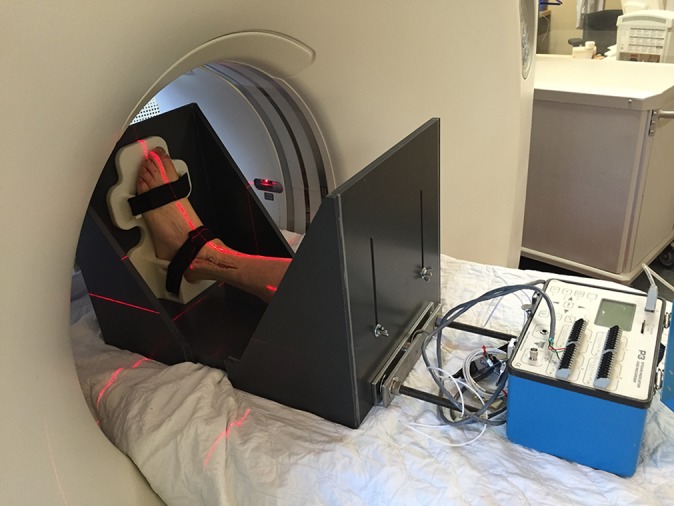
Experimental apparatus: custom-made device including a load cell applying a reproducible axial load of 750 N in the computed tomography scan.
Figure 3.

Controlled ankle motion boot inside the loading device.
Images were taken of the normal specimen with and without AL and in the CAM orthopaedic boot with AL with the help of a radiologic technologist. No external rotation forces were applied during these manipulations. Then, the same imaging sequence was repeated twice, once after the AiTFL was sectioned and again after the IOL was sectioned. Sectioning of the IOL was performed up to 10 cm proximally. The deltoid ligament was not ruptured.
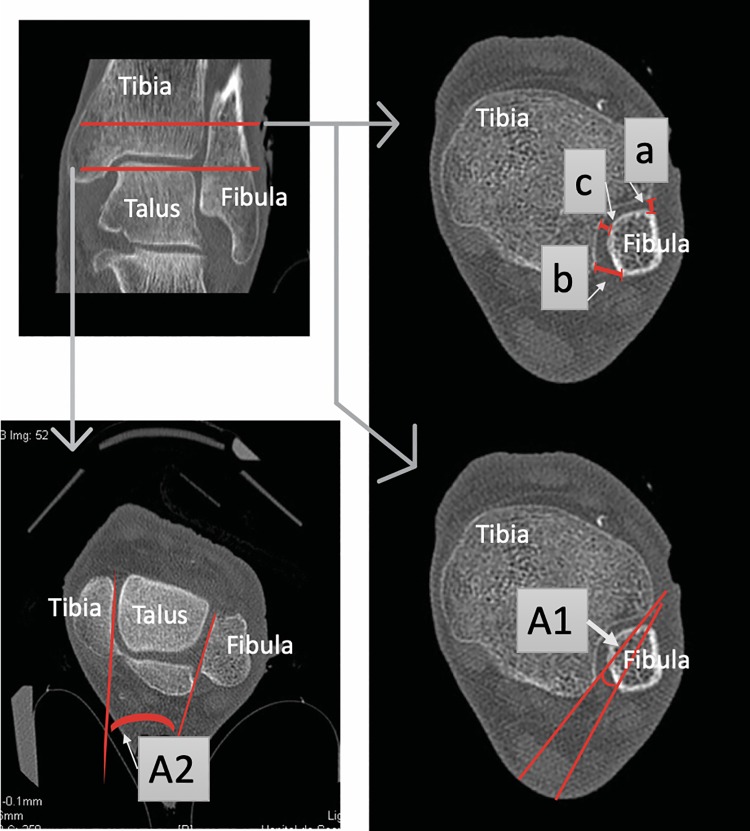
On the basis of a previously validated method,20 the distal tibiofibular relationship was evaluated on the chosen CT scan images using a series of 5 measurements: 3 length measurements (a, b, and c) and 2 angle measurements (A1 and A2) (Figure 4). All these measurements except A2 were taken on CT scan slices at 9.45 mm proximal to the tibial plafond.20 Measurement a represents the distance between the most anterior point of the incisura and the nearest most anterior point of the fibula.20 Measurement b represents the distance between the most posterior point of the incisura and the nearest most posterior point of the fibula.20 Measurement c represents the distance between the tibia and the fibula in the middle of the incisura.20 Angle A1 is calculated as the angle between a line drawn from the anterior and posterior points of the incisura and a line drawn in the fibula representing its orientation, with internal rotation being a negative angle.20 Angle A2 is measured at the level of the talar dome and represents the angle between the talar side of the 2 malleoli.20 This technique has already been validated for intra- and interobserver reliability and has shown good results, with no agreement due to chance (intraclass correlation coefficient > 0.3).20 For this reason, all measurements were performed once, by the same surgeon (M.-L.N.) who was blinded to the ligamentous condition. The CT scan was chosen because of its greater sensitivity to syndesmotic bony relationships compared with standard radiographs.7,18
Figure 4.
Computed tomography scan images of a specimen in the controlled ankle motion boot showing the 3 length (a, b, and c) and 2 angle (A1 and A2) measurements included in our analysis.
Wilcoxon tests for paired samples and nonparametric data were used to compare the different conditions. Specimens were therefore compared with themselves. Statistical analyses were conducted with SPSS Statistics 25.0 (IBM). The level of significance for this study was set at .01 to control for the multiplicity of tests and because this was a controlled experimental study. The critical P value was defined after applying a Bonferroni correction to the 6 hypotheses tested.
Results
Effect of AL on the Syndesmotic Anatomy
Table 1 summarizes the comparison of the data from specimens with an isolated AiTFL rupture and with both AiTFL and IOL ruptures, with and without AL. No significant differences (significance defined as P < .01) were found between these 2 groups (with and without AL), regardless of the number of ruptured ligaments.
Table 1.
Comparison of Ankles With and Without Axial Loading (AL) and With AL and CAM Boot in Different Ligamentous Conditionsa
| Without AL (1) | With AL (2) | With AL + CAM boot (3) | P (1 vs 2) | P (2 vs 3) | |
|---|---|---|---|---|---|
| a, mm | |||||
| Intact ankle | 3.68 ± 1.00 | 4.05 ± 1.11 | 3.87 ± 1.43 | .046 | .313 |
| AiTFL | 3.85 ± 1.24 | 4.06 ± 1.14 | 4.13 ± 0.67 | .612 | .953 |
| AiTFL + IOL | 4.46 ± 0.87 | 4.31 ± 0.68 | 4.16 ± 1.21 | .122 | .262 |
| b, mm | |||||
| Intact ankle | 7.58 ± 1.80 | 7.55 ± 1.82 | 7.33 ± 2.10 | .683 | .260 |
| AiTFL | 7.57 ± 2.15 | 7.10 ± 1.91 | 7.22 ± 2.16 | .097 | .683 |
| AiTFL + IOL | 7.19 ± 2.17 | 7.20 ± 1.98 | 7.32 ± 2.43 | .905 | .721 |
| c, mm | |||||
| Intact ankle | 2.01 ± 0.47 | 2.09 ± 0.39 | 1.96 ± 0.50 | .371 | .176 |
| AiTFL | 1.98 ± 0.55 | 2.06 ± 0.61 | 1.98 ± 0.54 | .622 | .281 |
| AiTFL + IOL | 2.06 ± 0.64 | 2.12 ± 0.57 | 1.88 ± 0.39 | .509 | .064 |
| A1, deg | |||||
| Intact ankle | –8.31 ± 6.54 | –7.98 ± 5.76 | –8.49 ± 6.44 | .575 | .444 |
| AiTFL | –6.76 ± 5.59 | –7.80 ± 5.82 | –8.39 ± 6.96 | .046 | .541 |
| AiTFL + IOL | –6.08 ± 4.23 | –7.27 ± 5.00 | –6.75 ± 5.64 | .038 | .161 |
| A2, deg | |||||
| Intact ankle | 8.63 ± 5.03 | 8.73 ± 4.35 | 9.71 ± 5.19 | .919 | .053 |
| AiTFL | 9.11 ± 4.32 | 8.40 ± 3.96 | 11.17 ± 3.65 | .123 | .009 |
| AiTFL + IOL | 9.15 ± 4.11 | 8.81 ± 3.86 | 11.97 ± 4.22 | .341 | .005 |
aHorizontal rows display each measurement (a, b, c, A1, and A2) and the different ligamentous conditions from intact ankle until both AiTFL and IOL ruptured. Data are presented as mean ± SD. Bold values indicate statistically significant difference (P < .01). AiTFL, anterior inferior tibiofibular ligament; CAM, controlled ankle motion; IOL, interosseous ligament.
Effect of CAM Orthopaedic Boot on Syndesmotic Anatomy
Specimens with a ruptured AiTFL were axially loaded and compared with themselves after being positioned in a CAM boot (Table 1). There were no significant differences in the measurements between these 2 groups, except A2 (8.40° vs 11.17°; P = .009).
This was repeated with 2 ruptured ligaments (AiTFL + IOL), and once again, only A2 was significantly different (8.81° vs 11.97°; P = .005), showing an increase in external rotation.
Discussion
The main goal of this study was to assess the effect of the CAM orthopaedic boot during AL and at varying levels of syndesmotic instability. Our primary hypothesis was that the CAM orthopaedic boot would be able to maintain syndesmotic congruity and prevent diastasis in AL, even with 2 ruptured ligaments. This hypothesis can neither be accepted nor be rejected because even without the CAM orthopaedic boot, no significant diastasis occurred.
However, there was a statistically significant increase of 3° in the external rotation of the fibula (A2) with the CAM boot in AL and 2 ruptured ligaments. This is an important finding, especially when choosing the type of immobilization. The CAM boot has posterior inflatable cushions, which could be more likely to push on the posterior aspect of the fibula and potentially cause an external rotational force. This is a possible explanation for the increase in the external rotation when the CAM boot was installed. This hypothesis should be explored in a future study by applying various degrees of quantifiable inflation to the posterior cushions. Thus, only a moderate amount of pressure should be used in the cushions to avoid an external rotation malposition that could result in a longer healing time of the AiTFL.
Overall, these results favor nonoperative treatment for a 1- or 2-ligament rupture with partial or total weightbearing, provided that external rotation can be limited. Further studies should assess whether the CAM orthopaedic boot is able to maintain syndesmotic stability when external forces are applied to the leg.
The study results suggest that single-point AL does not dramatically change syndesmotic stability. There were no significant differences between specimens with and without AL, even when simulating a 2-ligament rupture. It is possible that these results would have been different if the AL and external rotation forces were combined (simulating real-life conditions of a planted foot with a sudden change in direction). Indeed, an external rotation load has been identified as the main mechanism leading to a widening of the syndesmosis, especially when the foot is in pronation.12 These results are consistent with studies conducted by Hunt et al10 and Beumer et al.2 In the study by Hunt et al,10 no significant displacement of the fibula >5 mm and no rotational changes >1° were found between the tibia and fibula during AL alone, in 5 different conditions of ligamentous damage. However, when external rotation was applied, significant changes were observed in rotation, translation, and contact pressures within the syndesmosis, depending on ligament sectioning.10 The Beumer et al study also found the largest fibular displacements during the external rotation of the ankle. After sectioning the AiTFL, they did not find a significant displacement in the neutral position with AL,2 which is in agreement with what has been reported here. Furthermore, Massri-Pugin et al15 evaluated syndesmotic instability arthroscopically, and their results are consistent with the results from this study. Those authors reported that in order to find coronal plane syndesmotic instability with a standard 100-N lateral hook test, all 3 components of the syndesmotic complex (AiTFL, IOL, and PiTFL) had to be injured.15 However, as in the present study, no rotational force was added.15
The clinical correlation of these results could be that even with 2 major syndesmotic ligaments ruptured (AiTFL + IOL), single-event AL is not enough to create instability between the tibia and the fibula. The only concern with the CAM boot was the risk of malreduction of the tibia-fibula rotational distal relationship. The slight increase in external rotation recorded here suggests that this could potentially be avoided if the boot is not overinflated, or with the use of a regular cast, although this would need to be confirmed in future studies.
The results from the present study make it difficult to reach any clear clinical recommendation. However, if the excess external rotation seen with the CAM boot was secondary to the posterior cushions, as we hypothesized, it would be possible to say that conservative treatment, with the CAM orthopaedic boot and partial weightbearing, could be an acceptable treatment for patients with a syndesmotic lesion of up to 2 ligaments. It is, however, essential that further studies assess the stability of the syndesmosis in the same conditions with external rotation forces. To our knowledge, this is the first study to assess the ability of the CAM orthopaedic boot to maintain syndesmotic stability with weightbearing simulation and iatrogenic ligament ruptures. Further clinical studies are needed to assess the risks and benefits of conservative treatment for 2-ligament syndesmotic injury with the CAM boot rather than the more invasive surgical option, particularly regarding external rotational forces.
One of the main limitations inherent in this study is its cadaveric design. The ligaments were ruptured sequentially, without damaging the surrounding structures, which is not representative of everyday life, in which the capsule or the deltoid ligament may also be damaged. Most importantly, these specimens were only statically loaded, which does not effectively reproduce stresses encountered while walking. It is also possible that repeated testing would reveal further differences. This is an area for future study before these results can be transferred to clinical research. Finally, although the loading device was tested multiple times, it remains possible, but very unlikely, that the setup failed to deliver a correct and symmetric axial load to all the specimens.
Conclusion
The results of the present study suggest that AL alone, without any rotational forces, did not cause a significant distal tibiofibular instability even with 2 ruptured ligaments. Clinical recommendations cannot be made at this point, but 2 important research questions have come to light. First, further studies should focus on cyclical dynamic AL combined with an external rotational force to assess whether the CAM boot can maintain syndesmotic stability in these conditions. Second, the effect of the CAM boot air cushions on syndesmotic injuries needs to be more thoroughly investigated.
Acknowledgment
The authors thank Kathleen Beaumont for manuscript review and preparation.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by an educational grant by the PREMIER program. J.H.-D. has received consulting fees from Globus Medical and DePuy Synthes. S.L. has received consulting fees from Stryker. É.S. has a family member who is employed by Smith & Nephew. The Hôpital du Sacré-Cœur de Montréal has received educational and research support from Arthrex, ConMed, DePuy, Linvatec, Medacta, Smith & Nephew, Stryker, Synthes, Tornier, Wright, and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the ethics committee of the Hôpital du Sacré-Cœur de Montréal (No. 2015-1169).
References
- 1. Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc Rev. 2006;14(4):232–236. [DOI] [PubMed] [Google Scholar]
- 2. Beumer A, Valstar ER, Garling EH. et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77(3):531–540. [DOI] [PubMed] [Google Scholar]
- 3. Beumer A, Campo MM, Niesing R, Day J, Kleinrensink G-J, Swierstra BA. Screw fixation of the syndesmosis: a cadaver model comparing stainless steel and titanium screws and three and four cortical fixation. Injury. 2005;36(1):60–64. [DOI] [PubMed] [Google Scholar]
- 4. Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294–298. [DOI] [PubMed] [Google Scholar]
- 5. Close JR. Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am. 1956;38(4):761–781. [PubMed] [Google Scholar]
- 6. Del Buono A, Florio A, Boccanera MS, Maffulli N. Syndesmosis injuries of the ankle. Curr Rev Musculoskelet Med. 2013;6(4):313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ebraheim N, Lu J, Yang H. Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot Ankle Int. 1997;18(11):693–698. [DOI] [PubMed] [Google Scholar]
- 8. Ebramzadeh E, Knutsen AR, Sangiorgio SN, Brambila M, Harris TG. Biomechanical comparison of syndesmotic injury fixation methods using a cadaveric model. Foot Ankle Int. 2013;34(12):1710–1717. [DOI] [PubMed] [Google Scholar]
- 9. Hunt KJ, George E, Harris AH, Dragoo JL. Epidemiology of syndesmosis injuries in intercollegiate football: incidence and risk factors from National Collegiate Athletic Association injury surveillance system data from 2004-2005 to 2008-2009. Clin J Sport Med. 2013;23(4):278–282. [DOI] [PubMed] [Google Scholar]
- 10. Hunt KJ, Goeb Y, Behn AW, Criswell B, Chou L. Ankle joint contact loads and displacement with progressive syndesmotic injury. Foot Ankle Int. 2015;36(9):1095–1103. [DOI] [PubMed] [Google Scholar]
- 11. Lilyquist M, Shaw A, Latz K, Bogener J, Wentz B. Cadaveric analysis of the distal tibiofibular syndesmosis. Foot Ankle Int. 2016;37(8):882–890. [DOI] [PubMed] [Google Scholar]
- 12. Lin C-F, Gross MT, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6):372–384. [DOI] [PubMed] [Google Scholar]
- 13. Magan A, Golano P, Maffulli N, Khanduja V. Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull. 2014;111(1):101–115. [DOI] [PubMed] [Google Scholar]
- 14. Markolf KL, Jackson S, McAllister DR. Force and displacement measurements of the distal fibula during simulated ankle loading tests for high ankle sprains. Foot Ankle Int. 2012;33(9):779–786. [DOI] [PubMed] [Google Scholar]
- 15. Massri-Pugin J, Lubberts B, Vopat G, Guss D, Hosseini A, DiGiovani C. Effect of sequential sectioning of ligaments on syndesmotic instability in the coronal plane evaluated arthroscopically. Foot Ankle Int. 2017;38(12):1387–1393. [DOI] [PubMed] [Google Scholar]
- 16. McCollum GA, van den Bekerom MPJ, Kerkhoffs GMMJ, Calder JDF, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1328–1337. [DOI] [PubMed] [Google Scholar]
- 17. Molinari A, Stolley M, Amendola A. High ankle sprains (syndesmotic) in athletes: diagnostic challenges and review of the literature. Iowa Orthop J. 2009;29:130. [PMC free article] [PubMed] [Google Scholar]
- 18. Mukhopadhyay S, Metcalfe A, Guha AR. et al. Malreduction of syndesmosis—are we considering the anatomical variation? Injury. 2011;42:1073–1076. [DOI] [PubMed] [Google Scholar]
- 19. Mulligan EP. Evaluation and management of ankle syndesmosis injuries. Phys Ther Sport. 2011;12(2):57–69. [DOI] [PubMed] [Google Scholar]
- 20. Nault M-L, Hébert-Davies J, Laflamme G-Y. et al. CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma. 2013;27(11):638–641. [DOI] [PubMed] [Google Scholar]
- 21. Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10(5):558–560. [DOI] [PubMed] [Google Scholar]
- 22. Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014;5:173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58(3):356–357. [PubMed] [Google Scholar]
- 24. Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26(7):439–443. [DOI] [PubMed] [Google Scholar]
- 25. Valkering KP, Vergroesen DA, Nolte PA. Isolated syndesmosis ankle injury. Orthopedics. 2012;35(12):e1705–1710. [DOI] [PubMed] [Google Scholar]
- 26. Van Heest TJ, Lafferty PM. Injuries to the ankle syndesmosis. J Bone Joint Surg Am. 2014;96(7):603–613. [DOI] [PubMed] [Google Scholar]
- 27. Waterman BR, Belmont PJ, Cameron KL, Svoboda SJ, Alitz CJ, Owens BD. Risk factors for syndesmotic and medial ankle sprain: role of sex, sport, and level of competition. Am J Sports Med. 2011;39(5):992–998. [DOI] [PubMed] [Google Scholar]
- 28. Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35(7):1197–1207. [DOI] [PubMed] [Google Scholar]