Abstract
Background:
Carotid endarterectomy (CEA) is widely performed under operative microscopes. They provide magnified and stereoscopic vision of operative field suitable for precise maneuver. However, the microscope has some shortcomings, which are a narrow field-of-view, shallow depth-of-field, and the operator's fatigue due to fixed gaze posture through eyepieces. To overcome them, we introduced ORBEYE™ Surgical Microscope, which was 4K ultra high-definition three-dimensional (3D) system. We present our initial experience of the system for CEA and discuss its usefulness compared with the operating microscopes.
Methods:
A 66-year-old male presented to our department for the treatment of the left internal carotid artery severe stenosis. He underwent CEA using the ORBEYE™ Surgical Microscope.
Results:
The surgery was successfully completed only under the system without complication. The microscope was set over the operative field. Its wide field-of-view, deep depth of field, and smooth digital zooming allowed minimal repositioning of the microscope. The system provided high quality stereoscopic image of the surgical site, which enables us to perform precise surgery. The 55-inch 4K 3D monitor remarkably contributed to a reduction of the surgeons’ fatigue.
Conclusions:
The ORBEYE™ Surgical Microscope, incorporating 4K 3D video technology, has overcome shortcomings of the operative microscope. This system is highly feasible for CEA and has the certain possibility for other neurovascular surgeries.
Keywords: Carotid endarterectomy, microscope, neurosurgery, ORBEYE
Introduction
The neurosurgery under an operating microscope was introduced in the 1960 by Yaşargil.[1] Moreover, vascular neurosurgery under operative microscope was first reported by Spetzler et al. in 1986.[2] After the publication, microneurosurgery has become a gold standard procedure for vascular neurosurgeons.[3] The microscope provides clear three-dimensional (3D) stereoscopic vision with high magnification of the operative field which enables neurosurgeons a precise procedure during dissection of vessels, neural structures, tumors, and brain tissue. However, a state-of-art operative microscope has two major shortcomings: (1) The shallow depth of field needs frequent repositioning of the microscope to the operative field.[4] (2) Operator's eyes are enforced to fix to the eyepieces of the microscope, leading to their fatigue. For such reasons, longer depth of field and neurosurgeon-friendly monitor system would be welcome to the operative microscope.
Carotid endarterectomy (CEA) is an established treatment for carotid stenosis. The surgery can contribute better clinical outcome than optimal medical treatment for not only symptomatic patients but also asymptomatic patients.[5,6] One of the most crucial steps of this surgery is a manipulation of a distal end of carotid plaque. After removal of the carotid plaque, a precise fixation of the intima of the distal internal carotid artery (ICA) is required for the prevention of postoperative acute occlusion or restenosis.[3] Microsurgical repair of the diseased artery allows the neurosurgeon to manipulate elaborately. On the other hand, the shallow depth-of-field and narrow field-of-view of the operative microscope compels neurosurgeons to reposition the microscope frequently during the surgery, leading to the surgeon's fatigue. Thus, the microsurgical CEA is sometimes hesitated.
An Exoscope, high-definition video telescope operating monitor system to perform microsurgery has recently been proposed an alternative to the operating microscope.[4] This system enables the neurosurgeon to execute the operation by its high magnified images on a high-definition display. The major advantages of the scope compared with the operative microscope are the deep depth-of-field and wide field of view.[4,7,8] However, the system provides 2D views. Thus, the operators are required to develop eye-hand coordination for microsurgical procedures with the usage of the system. This is the major shortcoming of the Exoscope.
To overcome the weak points of the operative microscope and Exoscope listed above, we innovated ultra-high definition 3D-surgical microscope system, ORBEYE™ Surgical Microscope (OLYMPUS, Tokyo, Japan) for CEA. We report here our initial experience of the system and its usefulness and future perspective in vascular neurosurgery.
Materials and Methods
Case presentation
A 66-year-old male with asymptomatic progressive left ICA stenosis was referred to our hospital. His 3D-computed tomography angiography (3D-CTA) revealed left ICA severe stenosis (NASCET 87%) [Figure 1a]. Neck magnetic resonance imaging study (MRI) revealed left ICA severe stenosis due to high volume plaque, which was high intensity on T1-weighted and time of flight images [Figure 1b]. His initial clinical diagnosis was asymptomatic progressive left ICA severe stenosis with vulnerable plaque, and he was decided to undergo CEA. Written informed consent for the surgery was obtained from him and his family, though separate consent for using the ORBEYE™ Surgical Microscope was considered unnecessary because the microscope was approved medical device in ordinary medical care.
Figure 1.
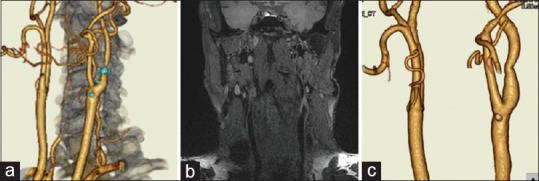
Preoperative three-dimensional computed tomography angiography (a) and neck magnetic resonance imaging study (b) revealed left internal carotid artery severe stenosis due to high volume plaque. Postoperative three-dimensional computed tomography angiography showed disappearance of left internal carotid artery stenosis (c)
Operative procedures
The ORBEYE™ surgical microscope was used in this surgery, with initial onsite support by the manufacturer. Briefly, this system consists of two of the Sony's 4K (4096 × 2160 pixels) Exmor R™ CMOS image sensors, providing a high-sensitivity, low noise, and a wide color range image, which is displayed on a 55-inch monitor [Figure 2a]. The observers are allowed for active 3D vision with passive light 3D glasses [Figure 2b]. The OPMI PENTERO operative microscope (Carl Zeiss AG, Jena, Germany) was prepared as backup.
Figure 2.

Operating room setup with the ORBEYE™ Surgical Microscope (a) and intraoperative finding (b). The microscope coming from the surgeon's left-frontal side is held over the surgical field resulting in no obstacle between the surgeon and the monitor. The operator, the assistant and the entire operating staff using three-dimensional glasses have the same view as the operator
The CEA was performed in the ordinal way as we described elsewhere.[9] The ORBEYE™ Surgical Microscope provided surgeons with an excellent surgical view with good clarity, contrast, and color in 3D images. During the surgery, the operator should adjust the position of the ORBEYE™ Surgical Microscope far less than the ordinal binocular microscope due to its deeper depth-of-field. Moreover, the operator and the assistant could perform the surgery in an agreeable posture throughout the surgery which was provided by its ergonomic design.
The surgery was successfully completed in a skin-to-skin manner using the ORBEYE™ surgical microscope without switching to the OPMI PENTERO. The operation time was 3 hours and 4 minutes, and total intraoperative bleeding was 28 ml.
Postoperative course
The patient's postoperative course was uneventful. His postoperative imaging studies demonstrated no ischemic lesion of diffusion-weighted image on MRI and good patency and disappearance of the stenosis of right ICA on 3D-CTA [Figure 1c]. He discharged home on the 8th postoperative day.
Discussion
In our experience, the ORBEYE™ Surgical Microscope is a progressive optical tool with clear advantages over the surgical microscope or 2D Exoscopes in terms of its high-resolution 3D surgical images and ergonomics.
CEA under operative microsurgery was first reported by Spetzler et al. in 1986[2] and microneurosurgery has become a gold standard procedure for vascular neurosurgeons thereafter.[3] The microscope produces highly-magnified stereoscopic images while providing highly-detailed surgical views. On the other hand, a state-of-art operative microscope has two major shortcomings: (1) The shallow depth of field needs frequent repositioning of the microscope to the operative field.[4] (2) Operators’ eyes are enforced to fix to the eyepieces of the scope, leading to their fatigue. The less ergonomics may become an inconvenience for surgeons when they perform relatively look-up surgery in awkward arm-extension posture, i.e., manipulation of the distal end of the atheromatous plaque in CEA [Figure 3a].[9] Thus, longer depth of field and more neurosurgeon-friendly operating monitor system would be welcome.
Figure 3.
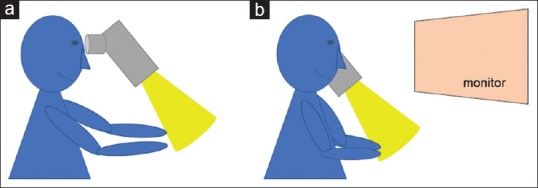
Schematic representations of operator's posture in awkward scope angle under the binocular surgical microscope (a) and the ORBEYE™ Surgical Microscope (b). Note the difference in the arm angle
An Exoscope, high-definition video telescope operating monitor system to perform microneurosurgery has been proposed an alternative to the operating microscope.[4,10,11] It provides surgeons with high-quality surgical image with adequate magnification. The major advantages of the Exoscope are its wide field-of-view and long depth-of-field in comparison with the operative microscope.[4] Moreover, the Exoscope provides ergonomic advantage by separating the surgeons from the eye pieces of the microscope and displaying the operative image ahead of the surgeons on a high-definition monitor.[10] The separating prevents the surgeons to be enforced keeping discomfortable positions at awkward angles. On the other hand, early Exoscope provides only 2D views, becoming the major shortcoming of the Exoscope, lack of stereoscopy of depth perception. Thus, stereopsis was required to improve hand-eye coordination for microsurgical procedures with the usage of the Exoscope, such as taking hold the needle and stitch up when suturing arteriotomy in case of CEA.[4]
A newly developed the ORBEYE™ surgical microscope, which is a kind of Exoscope, was launched in the united states and Japan on October 5, 2017.[12,13] This microscope offers 4K ultra-high-definition, 3D imaging for surgeons. They can operate while observing surgical field images on a 55-inch 4K monitor with special 3D light glasses. The system allows the operator and assistant to perform procedures in their comfortable position without fixing their gaze to eyepieces, leading a reduction in their fatigue [Figure 3b].[12,13] In our experience, the surgeon was able to operate the CEA under the ORBEYE™ surgical microscope without any discomfort about his posture, even in an awkward scope angle as removal of distal end of the high-positioned carotid plaque or making stitches on distal arteriotomy. After the completion of the surgery under the ORBEYE™ Surgical Microscope, he felt less stiff back than the ordinary CEA under surgical microscope. Thus, the unsurpassed ergonomics is one of the major advantages of the ORBEYE™ surgical microscope. Moreover the layout of operating room equipment and surgeons could be more flexibly arranged, allowing surgeons to observe vital signs or regional oxygen saturation of the patient with a glance during the surgery [Figure 2b]. Moreover, as the large 55-inch monitor enables the entire operating team to view the same 3D image with the glasses, it improves efficiency and education by allowing information to be shared with the anesthesiologist, nurses, and medical students.
On the other hand, there was a difficulty for the assistant to manipulate from his position. Under the ordinal operating microscope, the surgical field could be arranged as required for an operating surgeon and an assistant. On the contrary, the ORBEYE™ surgical microscope provides only one direction of the surgical field on the monitor which is the most suitable for an operator. Hence, the assistant is enforced to perform surgical manipulation after compensating for the view on the monitor by suitably rotating the surgical field in his head, making manipulation from the position of an assistant uncomfortable.[12] One of the possible solutions for this problem may be a virtual reality system for each operating surgeon that presents the surgical field in the real-world direction.[12] Moreover, the other possible solution may be dual the ORBEYE™ surgical microscope-monitor systems or head-mounted monitor system for each operating surgeon.
The major limitation of this report is the technical report of one surgical case without learning curve. More experience with the ORBEYE™ surgical microscope would contribute a real improvement of surgical results, especially operation time, and subjective sensations of operators.
Conclusion
This is the first report of a vascular surgery under the ORBEYE™ surgical microscope. Its highly ergonomic technology and high-resolution 3D optical system allow surgeons to perform safe and precise surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yaşargil MG. A legacy of microneurosurgery: Memoirs, lessons, and axioms. Neurosurgery. 1999;45:1025–92. doi: 10.1097/00006123-199911000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Spetzler RF, Martin N, Hadley MN, Thompson RA, Wilkinson E, Raudzens PA, et al. Microsurgical endarterectomy under barbiturate protection: A prospective study. J Neurosurg. 1986;65:63–73. doi: 10.3171/jns.1986.65.1.0063. [DOI] [PubMed] [Google Scholar]
- 3.Reinert M, Mono ML, Kuhlen D, Mariani L, Barth A, Beck J, et al. Restenosis after microsurgical non-patch carotid endarterectomy in 586 patients. Acta Neurochir (Wien) 2012;154:423–31. doi: 10.1007/s00701-011-1233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishiyama K. From exoscope into the next generation. J Korean Neurosurg Soc. 2017;60:289–93. doi: 10.3340/jkns.2017.0202.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothwell PM, Eliasziw M, Gutnikov SA, Fox AJ, Taylor DW, Mayberg MR, et al. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet. 2003;361:107–16. doi: 10.1016/s0140-6736(03)12228-3. [DOI] [PubMed] [Google Scholar]
- 6.Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, et al. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: Randomised controlled trial. Lancet. 2004;363:1491–502. doi: 10.1016/S0140-6736(04)16146-1. [DOI] [PubMed] [Google Scholar]
- 7.Mamelak AN, Nobuto T, Berci G. Initial clinical experience with a high-definition exoscope system for microneurosurgery. Neurosurgery. 2010;67:476–83. doi: 10.1227/01.NEU.0000372204.85227.BF. [DOI] [PubMed] [Google Scholar]
- 8.Frykman PK, Duel BP, Gangi A, Williams JA, Berci G, Freedman AL, et al. Evaluation of a video telescopic operating microscope (VITOM) for pediatric surgery and urology: A preliminary report. J Laparoendosc Adv Surg Tech A. 2013;23:639–43. doi: 10.1089/lap.2013.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Izumo T, Morofuji Y, Fujimoto T, Sadakata E, Hiu T, Horie N, et al. The orthodox techniques of carotid endarterectomy. Neurosurg Emerg. 2017;22:93–6. [Google Scholar]
- 10.Moisi MD, Hoang K, Tubbs RS, Page J, Fisahn C, Paulson D, et al. Advancement of surgical visualization methods: Comparison study between traditional microscopic surgery and a novel robotic optoelectronic visualization tool for spinal surgery. World Neurosurg. 2017;98:273–7. doi: 10.1016/j.wneu.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Parihar V, Yadav YR, Kher Y, Ratre S, Sethi A, Sharma D, et al. Learning neuroendoscopy with an exoscope system (video telescopic operating monitor): Early clinical results. Asian J Neurosurg. 2016;11:421–6. doi: 10.4103/1793-5482.145551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takahashi S, Toda M, Nishimoto M, Ishihara E, Miwa T, Akiyama T, et al. Pros and cons of using ORBEYE™ for microneurosurgery. Clin Neurol Neurosurg. 2018;174:57–62. doi: 10.1016/j.clineuro.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 13.ORBEYE. [Last accessed on 2018 Oct 19]. Available from: http://www.olympus-global.com/news/2017/nr00611.html .


