Abstract
We present a case of cervical myelopathy secondary to ossification of the cruciform ligament (also known as cruciate ligament). This is a rare phenomenon that, to the best of our knowledge, has only been reported 16 times previously in literature. We have added a review of literature after our case presentation. We hope that by doing so, we may aid clinicians reach early diagnosis so as to be able to better manage this rare disease.
Keywords: Cruciform ligament, ossification, spine
Introduction
Ossification of the cruciform ligament (also known as cruciate ligament) of atlas is a rare phenomenon.[1,2,3,4] To the best of our knowledge, there have been only 16 cases reported in literature thus far. In this article, we present a case of cervical myelopathy secondary to ossification of the cruciform ligament of atlas. We have also provided a concise review of literature pertaining to this pathology.
Case Report
A 48-year-old male presented to our neurosurgery clinic with a complaint of pain in the bilateral lower limbs along with progressive weakness in all four extremities for the past 4 years as well as urinary incontinence for the past 1 year. He became bed bound and catheter dependent. He was treated for suspected cervical spine tuberculosis for 6 months by antituberculosis therapy at an outside institute, but there were no confirmatory tests done. He did not provide us with any other relevant history.
On examination, he was a middle-aged male with a body mass index of 30 kg/m2 and wheel chair bound. He was alert, awake, and oriented to time, place, and person. He did not exhibit any cranial nerve deficits. His motor examination showed normal bulk, increased tone, and power of 0/5 in all muscle groups of both upper and lower limbs bilaterally. He also had hyperactive deep tendon reflexes of the biceps, triceps, brachioradialis, patellar, and Achilles tendons. Planters were up going along with sustained clonus bilaterally. Anal tone was lax.
Computed tomography (CT) scan [Figures 1 and 2] showed ossification of the entire cruciform ligament along with pseudarthrosis of C1 and C2 vertebra. Magnetic resonance imaging (MRI) [Figure 3] revealed severe cervical cord stenosis.
Figure 1.
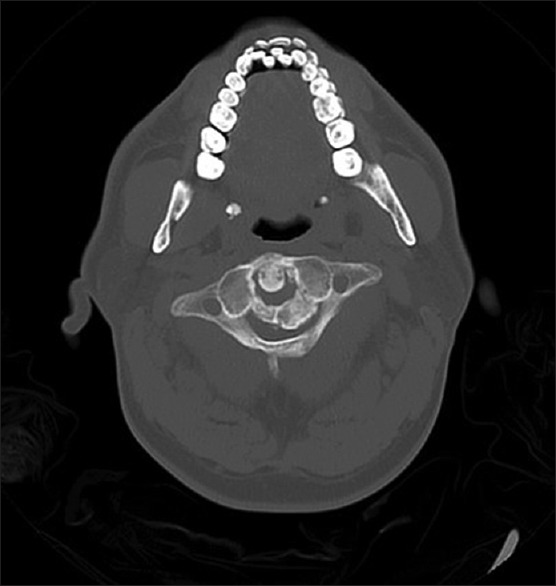
Computed tomography axial section showing ossification of the entire transverse ligament
Figure 2.

Computed tomography scan, sagittal image showing pseudoarthrosis of atlas along with ossification of longitudinal band of cruciform ligament
Figure 3.

T2 magnetic resonance imaging cervical spine sagittal section showing severe cord compression. Unidentified bright object in spine visualized in the magnetic resonance imaging was most likely secondary to ligament hypertrophy
The patient was explained in detail about the following three options: prolonged application of hard collar, halo ring traction, and surgical decompression. Due to chronic nature of his symptoms and belonging to a remote area making regular follow-ups difficult in case of halo traction and hard collar, the patient opted for surgical decompression. He was counseled about the risks including but not limited to cervical cord injury, visceral injury, failed decompression, and persistence of symptoms. After developing an understanding on risks and benefits, informed consent was taken and we did a neuronavigation-guided transoral decompression of C1 and C2. Highly vascular pseudarthrosis along C1 and C2 anterior arches and ossification of cruciate ligament (both transverse and longitudinal components) were noticed. Maximum safe debulking was performed.
Due to the main bulk of the ossified ligament seen anterior to the cord as well as the anterior compression of the cervical spine, we opted for an anterior approach as opposed to a posterior or 360 approach. Our patient and his family were kept in confidence that there may be a need of another procedure if complete debulking could not be done anteriorly.
Postoperative CT [Figures 4 and 5] scan was also performed which showed nonvisualization of the anterior tubercle, anterior arch, part of posterior arch of the atlas, and dens and pedicle of axis vertebra, with resultant widening of the spinal canal. Postoperative MRI was not done as the patient showed subjective and objective improvement. He had severe financial issues and MRI is a costly investigation in our country.
Figure 4.

Postoperative computed tomography scan showing removal of most of the transverse ligament
Figure 5.

Postoperative sagittal image revealing excision of pseudarthrosis bone and ossified longitudinal band
He was shifted to the intensive care unit for 24 h postoperatively and later shifted out. His neurological signs improved after 2 weeks with a power of 4/5 in the left hand and 3/5 both proximally and distally in left the lower limb, right upper limb, and lower limb. He had no pain or any other postoperative complication. Physiotherapy and rehabilitation program were initiated. On 3-month follow-up, he was able to stand with support and his motor examination improved to 4+ power in all groups bilaterally in both upper and lower limbs.
Discussion
Ossification of the atlantal ligament was first described in literature in 1978 by a case report on two patients by Wackenham.[5,6] Another three cases were then published in 1979 by Dietemann. Please note that the above-mentioned articles were only available in French and we, to the best of our efforts, were unable to find full-text English translations. They have therefore not been included in Table 1 that contains a summary of cases of atlantal ligament ossification reported in the literature to date.
Table 1.
Previously published case reports available in English text on ossification of the atlantal ligaments
| Article | Patient | Clinical features | Radiological findings | Management | Outcome |
|---|---|---|---|---|---|
| Hayashi et al., 1998[9] | 68, male | Progressive spastic quadriparesis below C5 Disturbed pain and touch sensation in all four limbs Bowel and bladder dysfunction |
X-ray: Ossified mass at the back of dens, anterior shift of atlas CT: High-density mass around the dens, which contained an area of low density T1 MR: High-intensity mass lesion at the back of dens T2 MR: Spinal canal stenosis at cervicomedullary junction |
Suboccipital decompression and resection of posterior arch of atlas C4-C6 laminoplasty |
Spasticity in lower extremities resolved Physical therapy helped regain full range of motion of limbs Paresthesia and sphincter disturbances resolved |
| Tsuruta et al., 2003[8] | 79, female | Occipitalgia and impaired gait Right-sided hemiparesis Bilateral loss of sensations in upper limbs Hyperreflexia Positive Babinski’s and Hoffman’s |
X-ray: Reduced spinal canal diameter and anterior position of the posterior arch of atlas MRI: Spinal cord compression at atlas and C3-C4 vertebrae CT myelography: Narrowing of spinal canal and ossification of transverse ligament |
Atlas laminectomy | Occipitalgia resolved and right hemiparesis improved |
| Griesdale et al., 2003[10] | 70, female | Numbness in lower extremities, left hand, and trunk Weakness in left hand, deltoid, and hip flexors Buzzing sensation down the left side with neck extension History of tuberculous, peritonitis, and carpal tunnel syndrome. Increased tone in lower extremities Brisk reflexes Spastic gait |
X-ray: C1-C2 instability, increase in atlantodental interval from 4 mm in the neutral position to 9 mm in flexion CT: Minimal calcification MRI: Retro-odontoid, extradural mass-causing spinal cord compression. Hypointense on T1 and hyperintense on T2. Minimal enhancement with gadolinium |
Transoral resection of the odontoid and extradural retro-odontoid mass. Posterior C1-C2 stabilization with right-sided transarticular screw and interlaminar fusion |
Complete resolution of symptoms at 6 months |
| Wang et al., 2004[5] | 66, male | Neck pain with limited neck motion Paresis and weakness of all four extremities Gait disturbance Hyperactive reflexes Hoffman and Babinski reflexes bilaterally positive Bilateral sustained ankle clonus Hypoesthesia below the angle of the sternum bilaterally |
X-ray: Diffuse densification of vertebral bodies CT: OTAL Ossification of posterior longitudinal ligament at C2 Ossification of posterior longitudinal ligament from C3 to C7 |
Halo ring traction with 4 kg weight Hard cervical brace protection |
Symptoms improved with conservative management JOA score increased from 7 to 13 |
| Wang et al., 2004[5] | 60, male | Moderate motor weakness of the upper extremity Hyperactive reflexes Hoffman and Babinski reflexes bilaterally positive Bilateral sustained ankle clonus Bilateral hypoesthesia on upper extremity |
X-ray: Ossification of posterior longitudinal ligament at C1-C7 CT: OTAL at C1 (posterior to the dens) and ossification of posterior longitudinal ligament at C2-C7 |
Halo ring traction with 4 kg weight Hard cervical brace protection |
JOA score increased from 8 to 12 |
| Shoda et al., 2005[4] | 70, male | Progressive neck pain and numbness of extremities Spastic quadriparesis Spastic gaitxybHyperreflexia Frequent urination |
X-ray and CT: Ossification of posterior atlantoaxial membrane and transverse atlantal ligament | Decompressive resection of the posterior arc of the atlas and laminectomy of the axis | Marked improvement in symptoms |
| Tang et al., 2010[1] | 58, female | Neck pain and limited neck motion Numbness of all 4 limbs Disturbance of Gait Hyperactive reflexes Positive Hoffmann’s sign in left hand |
X-ray: Hypoplastic posterior arch of atlas, hypertrophic dens, stenosis of the spinal canal at the level of atlas CT: marked stenosis at C1 Hypoplastic but intact posterior arch of the atlas, partially ossified transverse ligament, and hypertrophic dens |
Decompressive resection of posterior arch of the atlas | Improvement in numbness and gait |
| Proietti et al., 2011[3] | 53, female | Progressive neck pain, suboccipital headache and limited motion of cervical spine Spastic quadriparesis Numbness of extremities Hyperactive reflexes Bilateral Babinski and Hoffmann signs Loss of fine motor skills Spastic broad-based and hesitant gait |
CT: Hypoplastic posterior arch of the atlas, ossification of the transverse ligament and ossification localized Between odontoidal apex and occipital lamina |
C1 laminectomy and fixation with two lateral mass Polyaxial screws in the atlas and two bilateral crossing C2 laminar screws C1-C2 fusion was performed with autologous iliac crest bone graft |
Improvement in neurological functions |
| Sasaji et al., 2011[2] | 76, female | Numbness and clumsiness in upper limbs Gait disturbance |
X-ray: Irreducible atlantoaxial subluxation CT: OTAL, coalition of atlanto-occipital joints and osteoarthritis of the atlantoaxial joints with degenerated dens MR: Spinal cord compression at C1 by the ossification of TLA and AAS |
Decompressive resection of posterior arch of atlas and laminectomy of C3 and C4 | Improvement in symptoms |
| Bokhari and Baeesa 2012[7] |
68, female | Chronic cervicalgia Significant quadriparesis Hypoesthesia of the upper extremities Hyperreflexia Positive Babinski’s sign. Gait disturbance |
X-ray: Degenerative disks at multiple levels MR: Canal stenosis and cord compression at atlas CT: Canal stenosis, hypoplastic posterior arch of atlas, OTAL |
Laminectomy of hypoplastic posterior arch of the atlas | Improvement in symptoms with physiotherapy |
| Zhang et al., 2014[6] | 64, male | Lower extremity weakness and clumsiness Gait disturbance Hyperactive reflexes in lower extremity Positive Hoffmann’s sign in the left hand |
X-ray: Continuous arch from C1 to C5. Disappearance of bilateral sacroiliac joint space CT scan: OTAL, Posterior longitudinal ligament from C2 to C5 and thoracic spine, ligamentum flavum in the thoracic spine |
Decompressive laminectomy for thoracic spine Conservative management for OTAL |
MR – Magnetic resonance; MRI – Magnetic resonance imaging; CT – Computed tomography; JOA – Japanese orthopedic association; TLA – Transverse ligament of the atlas; OTAL – Ossification of transverse atlantal ligament; AAS – Atlanto-axial subluxation
Cervical canal stenosis is a rare occurrence at the level of the atlas. This is due to a protective regional anatomy. The canal diameter at the retrodental level is around 17–25 mm, whereas the spinal cord diameter is between 10 and 12 mm. Consequently, for compression to occur at, this level would require a significantly large lesion or a compromise of the bony canal (congenital anomalies, trauma, intervention).[6,7]
Ossification of the atlantal ligament may be due to calcium phosphate metabolic disease, obesity, diabetes mellitus, aging, and dynamic factors such as trauma.[8,9] High amounts of fluoride have also been suggested as a possible cause by Wang et al.[5] A possible etiological cause in our patient could not be recognized. Ossification of the atlantal ligament may also be associated with other developmental anomalies at the craniovertebral junction such as hypoplasia of the atlas.[5,7,8]
Clinically, the disease presents as neck pain, stiffness, and features of myelopathy.[10] Treatment is controversial and should be tailored to the severity of the patient's presentation. Wang et al.[5] reported success with conservative therapies such as hard collar and halo ring traction. Others favored surgical decompression.
Table 1 provided detailed summary on the presentation, imaging findings, treatment, and prognosis of previously reported patients with ossification of the atlantal ligament.
Conclusion
We report a rare case of atlantal ligament ossification that presented to our institution in June 2018. Our patient was managed surgically and has shown improvement in his symptoms. We are hopeful that with further rehabilitation and physical therapy, he will continue to improve. By supplementing our case report with a review of literature, we hope to provide a detailed overview of this disease so as to help clinicians better manage this rare entity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tang JG, Hou SX, Shang WL, Wu WW. Cervical myelopathy caused by anomalies at the level of atlas. Spine (Phila Pa 1976) 2010;35:E77–9. doi: 10.1097/BRS.0b013e3181bb14e5. [DOI] [PubMed] [Google Scholar]
- 2.Sasaji T, Kawahara C, Matsumoto F. Ossification of transverse ligament of atlas causing cervical myelopathy: A case report and review of the literature. Case Rep Med. 2011;2011:238748. doi: 10.1155/2011/238748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Proietti L, Scaramuzzo L, Sessa S, Schirò GR, Logroscino CA. Cervical myelopathy due to ossification of the transverse atlantal ligament: A Caucasian case report operated on and literature analysis. Orthop Traumatol Surg Res. 2012;98:470–4. doi: 10.1016/j.otsr.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Shoda N, Anamizu Y, Yonezawa N, Ishibashi H, Yamamoto S. Ossification of the posterior atlantoaxial membrane and the transverse atlantal ligament. Spine (Phila Pa 1976) 2005;30:E248–50. doi: 10.1097/01.brs.0000160996.82470.c0. [DOI] [PubMed] [Google Scholar]
- 5.Wang W, Kong L, Zhao H, Jia Z. Ossification of the transverse atlantal ligament associated with fluorosis: A report of two cases and review of the literature. Spine (Phila Pa 1976) 2004;29:E75–8. doi: 10.1097/01.brs.0000109762.46805.63. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Z, Liu Z, Zhu J. Ossification of the transverse atlantal ligament in ankylosing spondylitis – A case report. Biomed Res. 2014;25:617–9. [Google Scholar]
- 7.Bokhari R, Baeesa S. Atlas hypoplasia and ossification of the transverse atlantal ligament: A rare cause of cervical myelopathy. Case Rep Neurol Med. 2012;2012:893284. doi: 10.1155/2012/893284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsuruta W, Yanaka K, Okazaki M, Matsumura A, Nose T. Cervical myelopathy caused by hypoplasia of the atlas and ossification of the transverse ligament – Case report. Neurol Med Chir (Tokyo) 2003;43:55–9. doi: 10.2176/nmc.43.55. [DOI] [PubMed] [Google Scholar]
- 9.Hayashi T, Hirose Y, Sagoh M, Murakami H. Ossification of transverse ligament of the atlas associated with atlanto-axial dislocation – Case report. Neurol Med Chir (Tokyo) 1998;38:425–8. doi: 10.2176/nmc.38.425. [DOI] [PubMed] [Google Scholar]
- 10.Griesdale DE, Jr, Boyd M, Sahjpaul RL. Pseudogout of the transverse atlantal ligament: An unusual cause of cervical myelopathy. Can J Neurol Sci. 2004;31:273–5. doi: 10.1017/s0317167100053968. [DOI] [PubMed] [Google Scholar]


