Abstract
Background:
Traumatic spinal cord injury (TSCI) has profound effects on the patient's health condition and function. However current treatment strategies fail in terms of cure. Thus, rehabilitative management has become the main gadget to promote patients’ residual function. The most challenging aspect of rehabilitation is high costs of inpatient rehabilitation programs and poor continuity of care while patients are transferred to home. In this regard, numerous home based rehabilitation programs have been introduced.
Objectives:
This review is an attempt to better introduce and classify different aspects of home care programs for patients with TSCI all around the world.
Methods:
A literature search was conducted in the PubMed, Medline, and Google Scholar database. Studies that addressed rehabilitative programs for patients with TSCI in their home or home-like facilities were reviewed. Reference lists from retrieved articles were also reviewed.
Results:
Home based rehabilitation can be categorized in five different but naturally relevant fields: home aids/modification, home nursing and family help, social support, home based primary care (multidisciplinary physician groups), and novel models/methods (e.g. “transitional rehabilitation” or telemedicine).
Conclusion:
Since most investigators in TSCI home based rehabilitation have only introduced their findings, there are no comparative studies available. Thus future studies should be dedicated to clinical trials evaluating clinical efficacy of different strategies. A comprehensive integrated strategy with consideration to financial and other limitations should be applied to each specific area.
Keywords: Home care, rehabilitation, spinal cord injuries
Introduction
Traumatic spinal cord injury (TSCI) has profound effects on survivors’ health condition and function.[1] Patients with TSCI face many difficulties while returning to their previous social roles. They would experience daily struggles with physical, psychological, and financial problems.[2,3] Given the high rate of traffic accidents leading to a high number of spinal cord-injured patients in Iran and many other countries, it is necessary to pay special attention to the management of these patients.[4]
Great efforts have been made to develop functional performance along with quality of life of patients with TSCI. The primary goal is to initiate rehabilitation programs as soon as possible after the patient's spinal cord problems have been stabilized. In this regard, there have been rehabilitation centers around the world in which both new technologies and expert staff are gathered to provide the highest level of patient care.[5] The ultimate goal is to help patients return to their previous function.
The cost of these rehabilitation centers is a burden to both patients and the health-care system. Patients with TSCI are not expected to be fully capable of providing an economically independent life at least for 1st years after trauma. Thus, these rehabilitation programs will be questioned as if they are affordable to run. Furthermore, the circumstances provided in these rehabilitation centers are not the same as what patients deal with, within their routine lives in home and the society. Hence, patients are not appropriately trained for real daily life.[6] The time spent in these centers is not usually enough for both patients and their family to learn their new life situations. Therefore, they would challenge numerous problems which they are not trained for.[7] Furthermore, many of these rehabilitation programs are limited in terms of education and support to patients with TSCI and does not cover their families. Hence, a patient not only has problems doing ordinary routines but also his/her family has no idea how to help them or even how to adapt their own personal life to new circumstances.[8]
The high cost of patient care in specialized centers along with their failure to prepare patients with TSCI for successful return to ordinary life has resulted in enormous studies trying to facilitate the transition period between being completely disabled and to live in an ordinary life. One of these solutions is programs based on home care. The natures of these programs have changed over the time. Novel programs have been developed in different countries which sometimes have led to outstanding results.[9,10,11,12] Recently, great efforts have been focused on lowering heavy costs of care in specialized centers and on developing efficacy of these services using the patient's own life circumstances. Patient's return to his/her routine life without complications leading to hospital admission is the main objective of these services.
To the best of our knowledge, there is no study reevaluating these rehabilitation and care programs. However, it is mandatory to understand various aspects of these methods to achieve optimal efficacy of them and to integrate them to obtain a maximum possible synergistic result. The aim of the present study is to describe a general overview of different home care programs and their components in patients with TSCI.
Methods
This study was held as a review. A literature search was conducted in the PubMed, Medline, and Google Scholar database using key terms “spinal cord injury rehabilitation,” “home care” and “home based rehabilitation.” Studies addressed rehabilitative programs for patients with TSCI in their homes or home likes and their reference lists were reviewed from January 1990 to December 2016. English language studies introducing new methods for home care with a minimum of 10 participants were included. Case reports and theoretical studies with no participants were excluded from the study. Two independent reviewers were in charge of the literature search. The study protocol was approved by the Institutional Review Board and Ethics Committee of Tehran University of Medical Sciences.
Results
Of the 113 exclusive titles matched to our search strategy, 110 full-text articles were available to screen for eligibility. Of these, 10 studies fulfilled the inclusion criteria and were included in the study. In addition, relevant titles were identified from the reference list of articles and screened for potential inclusion. Of these, 210 full-text articles were evaluated and only 5 matched the inclusion criteria. A total number of 15 articles were reviewed in this study [Figure 1 and Table 1].
Figure 1.
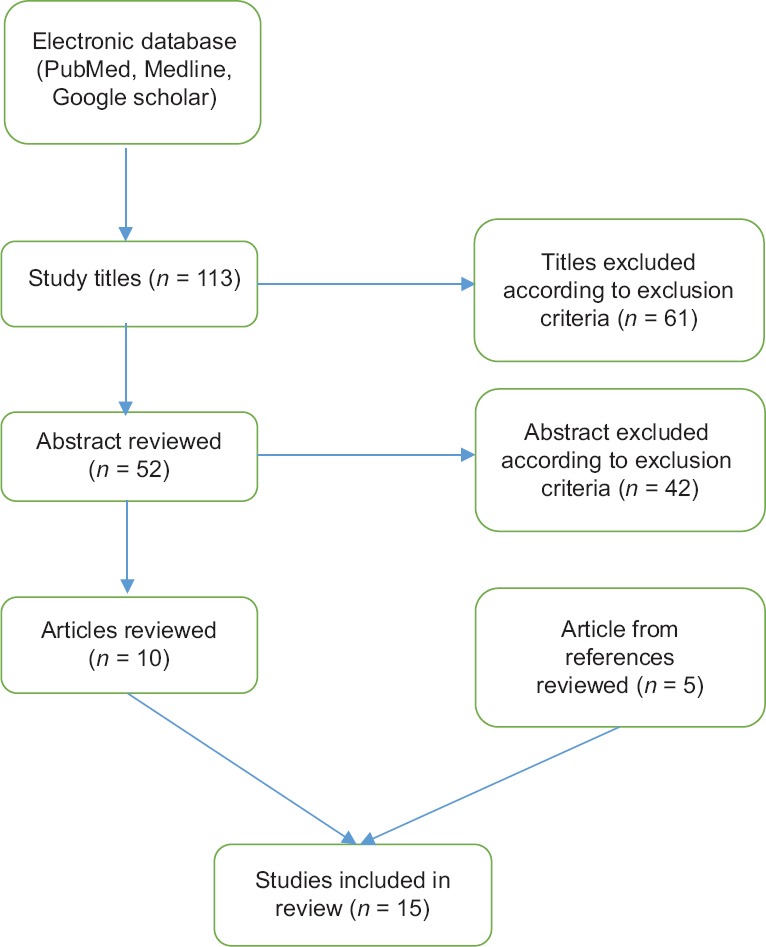
Flowchart of article selection process
Table 1.
Summary of articles reviewed
| Authors and year | Study design | Sample size | Results | Type of rehabilitation |
|---|---|---|---|---|
| Biering-Sørensen et al. (2009) | Cross-sectional | n=279 | Most common aids or adaptations reported were commode/shower chair on wheels or a seat (69%), grab bar by the toilet (41%), electrical bed (44%), special mattress (28%), lift/hoist (20%), computers (39%), and kitchen tools or cutlery with special handles (14%) | Home aids |
| Hall et al. (1999) | Cross-sectional | n=82 | Mean hospital days in the past year were 11 for the ventilator-independent group and 6 for the ventilator-assisted group. The latter group required more nursing level care, significantly more hours of care, and more paid attendants over the year | Home nursing |
| Weitzenkamp et al. (2002) | Cross-sectional | n=2154 | Differences in an interval version of the motor portion of the FIM™ instrument accounted for 26.3% of the variance in total personal care assistance hours | Home nursing |
| Beedie and Kennedy (2002) | Cross-sectional | n=95 | High quality of social support was associated with low hopelessness and depression scores, being more pronounced at week 18 postinjury | Social support |
| Elliott et al. (1992) | Cross-sectional | n=182 | Relationships which reassured the worth of die individual were predictive of lower depression scores. To a lesser extent, relationships providing a sense of social integration were also associated with lower depression scores | Social support |
| Fine et al. (2000) | Clinical interventional | n=1140 home visits | Since 1972, a hospital-based specialty home health team consisting of a registered nurse, a registered physical therapist, and a vocational rehabilitation counselor has been serving spinal cord injury patients hospitalized previously in a university-affiliated rehabilitation center. A summary of facts about this program has been presented | Home-based primary care |
| Fronek et al. (2005) | Randomized controlled trial | n=89 home care providers | Initial between-group comparisons on subscales scores showed that the control group scored significantly higher than the treatment group (trained about sexual problems) on the knowledge subscale before the training program but scored significantly lower than the treatment group immediately following the training program and at 3-month follow-up | Home-based primary care |
| Fronek et al. (2011) | Randomized controlled trial | n=37 home care providers | Training about sexual problems can have long-lasting effects on practitioner knowledge, comfort, and attitudes in addressing sexuality issues with clients | Home-based primary care |
| Wallace and Kendall (2014) | Qualitative | n=220 | A total of 1100 goals were classified into 18 different goal domains, representing most aspects of the ICF framework. Age was negatively related to vocational goals. Length of hospital stay was positively related to personal care goals but negatively related to community access and vocational goals | New models: Transitional rehab |
| Petrofsky (2001) | Pre-post trial | n=10 | Subjects only undergoing clinical therapy showed about a 50% reduction in hip drop due to therapy. However, the group that used the home training device showed almost normal gait after the 2-month period | New models: EMG biofeedback |
| Dolbow et al. (2012) | Pre-post trial | n=17 | Exercise adherence rates (71.7% and 62.9%) were well above the reported 35% in the able-bodied population, which provides evidence for the feasibility of a home-based functional electrical stimulation lower extremity cycling program. Younger adults with a history of being physically active have the highest potential for exercise adherence | New models: FES |
| Taylor et al. (1993) | Controlled trial | n=90 | There was no difference in cardiac output between the groups. However, thigh blood flow was found to be around 65% of normal values in the spinally injured group. This returned to normal values following the retraining program. The quadriceps muscle wasted to approximately 50% of its original thickness in the first 3 weeks following spinal cord injury. The retraining program increased the muscle thickness to near normal values | New models: FES |
| Kowalczewski et al. (2011) | Randomized controlled trial | n=13 | FES-ET on a workstation, supervised over the Internet, is feasible and may be effective for patients who can meet the residual motor function requirements of our study | New models: Telerehabilitation |
| Phillips et al. (2001) | Randomized controlled trial | n=111 | Preliminary evidence suggests that in-home telephone or video-based interventions do improve health-related outcomes for newly injured SCI patients | New models: Telerehabilitation |
| Van Straaten et al. (2014) | Pre-post trial | n=16 | A high-dose scapular stabilizer and rotator cuff strengthening program using telerehabilitation for supervision holds promise for shoulder pain treatment in manual wheelchair users with SCI | New models: Telerehabilitation |
FIM – Functional independence measure; FES – Functional electrical stimulation; FES-ET – FES-exercise therapy; SCI – Spinal cord injury; EMG – Electromyogram; ICF – International classification of functioning, disability and health
Home care component
Home-based rehabilitation can be categorized into five different but naturally relevant synthesizable fields:
Home aids/modification
Physical barriers in home are among the most important environmental barriers for patients with spinal cord injury to return to normal life.[13] Administration of specially designed equipment for a specific patient and applying possible changes in home or working place architecture would help to elevate patient's sense of secure and independence. These equipment consist of mechanical/electronic devices and also those used in conservative and supportive treatments. Few studies have emphasized the importance of using home aids for patients with TSCI.[5,6] Using home aids beside application of remote control technologies may result in considerable positive changes, especially in patients with high motivation to overcome their disability boundaries and lower their dependency. Therefore, it would result in higher satisfaction and quality of life.[14]
Different categories of home aids have been assessed for efficacy in previous studies. Biering-Sørensen et al. found that the most common devices used are commode/shower chair on wheels or a seat, electrical bed, grab bar by the toilet, special mattress, lift/hoist, computers, and kitchen tools or cutlery with special handles. These tools were most likely to be used by patients with cervical spinal cord injury.[15] Rigby et al. showed that phone, TV, stereo, fan, and lights are the most common electrical devices in TSCI patients’ daily life. Patients declared that utilization of these devices developed their independency, sense of value, and self-confidence.[9] Remote control devices used to adjust temperature, opening and closing doors and windows, turning lights, TV, and etc., on and off may also be useful to elevate patients’ independence and contribution to perform home chores.[16]
Health-care equipment also has a great value in maintaining patients’ health and preventing secondary complications. According to Stiens et al., examples of such equipment are as follows: “bowel and bladder supplies including catheters, leg and bed bags, laxatives, suppositories, gloves, incontinence briefs, underpads, lubricants, and digital stimulators; pulmonary ventilation equipment including continuous positive airway pressure and bi-level positive airway pressure machines, humidifiers, ventilators, and suction and inhalation-exhalation machines; Skin care supplies including pillows, foam blocks, positioning wedges, dressings, emollients, and decompression.”[16]
An occupational therapist is usually responsible for choosing the best home aids based on patient's needs. Before discharging from hospital, the occupational therapist would visit the patient's house. According to the level of the spinal cord injury and previous abilities of the patient, functional aids needed are predicted and designed. These aids can change as patient's abilities and functional goals develop.[10,16]
Constructional changes may be necessary to provide a safe and secure living place matching patients’ new needs. These changes are generally expensive and difficult to apply but occupational therapist's efforts with collaboration and consultation of other experts can be effective in this filed. As Stiens et al. have mentioned, this section of home care program can include “ramps, automatic doors, overhead installed track lift systems, reserve power generators, and emergency response systems.”[16] If the same changes can be made in the workplace, there might be a great step toward resolving occupational problems.
Home nursing and family help
Patients with spinal cord injury will spend most of their time with their families. Thus, family members have an important role in providing an effective care.[17] Involving patient's family in the rehabilitation program after educating them may have potentially beneficial effects.[18]
On the other hand, providing care for an abundantly dependent patient may put lots of pressure on family members and occasionally harm familial relationships. This issue becomes clear as if we consider mean age of patients struggling with these injuries; an individual with zero dependence in his/her previous daily life is now completely disabled seeking help of others. Therefore, it is important to pay special attention to family issues when designing a comprehensive plan for home care and to prevent putting too much pressure on family members. Especially, in the first days of returning to their home, both patients and their families face a lot of pressure; thus, an outside support is necessary.[19]
Home nursing may provide a great help for patients with TSCI, performing activities of daily living such as bathing, dressing, transfers, and bowel/bladder management. Although this nursing care prevents excessive pressure to family members, the costs can be considerable.[20,21] Nursing care has its major effect on performance limitations rather than medical issues; thus, functional disability is the best predictor of the extent of nursing care needed.[22]
Social support
TSCI is a severe catastrophic life event, causing significant psychological trauma as well.[23] Social support can be effective in means of lowering the burden of psychological trauma, depression, disappointment, and elevating life satisfaction.[24,25,26] Unfortunately, social support programs are not easily available in developing countries and patients with TSCI buckle with lots of psychological problems.[27]
It has been proposed that participation in social activities is associated with a higher quality of life more than any other factors.[28] The WHO defines participation as “a person's involvement in a life situation.”[29] According to a review by Barclay et al., factors such as “having adequate personal care assistance, having appropriate social support, having adequate special equipment, and appropriate occupational therapy” can be effective in facilitating participation of a TSCI patient and consequently in increasing quality of life.[28]
TSCI Rehab project categorizes social support into following domains: “financial planning, discharge planning, discharge services, supportive counseling, educating about and managing referral to peer/advocacy groups, education about TSCI and other relevant topics, educating about and managing referral to community/in-house services, and team conferences. Every domain has its own branching.”[30] One of the important aspects of social support is to facilitate occupational opportunities for patients with TSCI. Although it has been shown that employment has some advantages on the quality of life of a TSCI patient,[31] only up to 35% of these patients are employed.[32] Occupational therapist can have a great role in facilitating work circumstances for a TSCI patient and introducing occupational opportunities matching their remained abilities.[33]
Nongovernmental organizations are of important role in the rehabilitation process. Providing home aids, establishing rehabilitation camps, educational and supporting programs for patients, and their families are among their activities.[10] By improving patients’ understanding of themselves and their abilities, providing sport programs, and voluntary groups, they can play their role in the process of rehabilitation.[19]
Home-based primary care
Home-based primary care means scheduled appointments of multidisciplinary medical team visiting a TSCI patient in his/her home. The services provided by this team may include – but not limited by – basic medical care, nursing, social service, physical, and occupational therapy.[11] Medical services and appointment frequencies may vary based on patients’ health condition and organization provides these services. In these programs, a nurse is usually responsible for maintaining health condition by providing nursing service, and occupational therapist is in charge of promoting functional capacity through training special skills, recognition of physical barriers, and finding solutions to resolve them, providing assistive devices, and offering necessary architectural changes at home.[34]
Sexual problems are among commonly neglected issues by a multidisciplinary team because of lack of required knowledge. Few studies have evaluated effectiveness of educating multidisciplinary team about sexual problems of TSCI patient and reported magnificent results.[35,36]
In home-based primary care, along with no need to transport patients between hospital and home (which prevents subsequent complications and harms), multidisciplinary medical team can closely evaluate real-life situation of patients and provide individualized solutions and recommendations about needed home aids and architectural modification. In addition, secondary problems will be detected sooner, and in case of emergencies, patients would be timely referred to hospital and subsequent costs will be reduced.
Innovative models/methods
Transitional rehabilitation
The idea of developing this model was to make sure that rehabilitation program would continue especially shortly after transition from hospital. Transition period is very stressful for patients and their families and necessitates comprehensive support. In this model, rehabilitation strategies are designed based on patient's needs and goals to decrease hospital stay, reduce costs, and in addition to proceed rehabilitation in patient's real-life circumstance. This model consists of services such as nursing, physiotherapy, occupational therapy, and social work professionals provided by a multispecialty team. Discharging from hospital takes place 4 weeks sooner than regular discharge plan. Before initiating the program, rehabilitation objectives are defined with participation of both patients and caregivers, though further modification and reevaluation are possible. Duration of the program is 4–8 weeks and frequency of visits depends on needs and living condition of the patient.[12] Introducing this model to a patient living in a remote area can be challenging. As Wallace and Kendall have reported, transitional rehabilitation in remote areas faces five types of challenges including: (1) identification, education, coordination, and funding of local care providers; (2) Family involvement in rehabilitation; (3) contact with social and community supports; (4) specialist's support to problem solve discharge needs; and (5) skill acquisition and transfer in a community environment.”[37]
Transitional rehabilitation should be a part of a long-term rehabilitation program for patients with TSCI. Monitoring the advantages and disadvantages should be performed even after finishing the program.
High tech devices have been commonly used in the home care programs of patients with TSCI. Modern wheelchair designs, brain-based command signals, and locomotor training are only some examples of utilization of modern technology in enhancing quality of life and functional capacity of patients with TSCI.[38] Although there have been trials assessing their efficacy, recommending these devices to every patient demands further understanding of their safety profile, availability, and cost-effectiveness. In following paragraphs, we will discuss some examples of technology-based interventions specifically designed to help patients with TSCI.
Electromyogram biofeedback
Although some paraplegic patients may be able to walk after injury, it would be with some abnormalities such as Trendelenburg gait. In a gait retraining study, using a permanent biofeedback tool both in clinic and home resulted in more progression in walking skills compared to using it only in clinic.[39]
Functional electrical stimulation
Using functional electrical stimulation to improve gait skills in patients with incomplete spinal cord injury showed promising results. Increasing blood supply, preventing muscle atrophy, increasing walking speed, step width, and standing duration along with decreasing dependency to aids are among its advantages.[40] As Kirshblum et al. said, this technique had also positive effects on “upper-extremity use, bladder control, respiration, and cardiovascular and tissue health.”[38] Application of this technique as a part of home care strategy has been evaluated in some studies.[41,42,43]
Telemedicine
In this method, high tech devices such as video conference are used to connect patients with TSCI and the medical team even when they are miles away. This is especially of value for patients living in distant areas from TSCI units. The telemedicine rehabilitation team can include a physician, nurse, physical therapist, dietitian, psychologist, and recreational therapist.[44] Furthermore, surveillance of noncomprehensive programs with smaller goals such as improving hand function can be achieved using this method.[45] Several studies revealed efficacy of this technique in different aspects of rehabilitation programs of patients with TSCI.[46,47] Although this model showed promising results, further investigations should be dedicated to prove its efficacy and cost-effectiveness compared to traditional methods.[48]
Discussion
This review is an attempt to better introduce and classify different aspects of home care programs for patients with TSCI all around the world. Different fields of home care including home aids/modification, home nursing and family help, social support, home-based primary care, and novel models/methods have opened a new horizon toward a more effective rehabilitation. A great number of papers have been published in this field and yet there is an increasing trend to introduce more efficient strategies. There is still a long road to establish a safe, widely accepted, and cost-effective rehabilitation package in the setting of community and home for these patients.
Conducting clinical research in the field of TSCI rehabilitation is very difficult. Sample heterogeneity and small size, ethical problems of not delivering rehabilitation services to control group, impossibility of patient blinding, and lack of an appropriate measurement tool along with financial problems are some difficulties.[49] Hence, nearly all investigators in TSCI home-based rehabilitation have only introduced and described their findings, and there are no comparative studies performed. Thus, future studies should be dedicated to intelligently designed clinical trials to evaluate and compare clinical effectiveness of different strategies. Financial concerns are another aspect of home care that has been neglected in previous studies. Hence, there is a need to conduct cost-effectiveness studies to find the most affordable strategy.
It should be considered that rehabilitation of an individual with spinal cord injury is not just a combination of separated parts coming together, but it includes all aspects of life of a biopsychosocial person with a catastrophic disability. Hence, studies investigating the effectiveness of complete packages of rehabilitation components are mandatory.
Conclusion
Recently, rehabilitative management has become the main gadget to promote residual function of patients with TSCI. In this regard, home-based rehabilitation programs have shown potential benefits. These programs are widely variable in terms of the service they provide for patients with TSCI. Thus, findings of different studies in this field should be used to design a comprehensive integrated strategy with consideration of patient's personal, physical, financial, social, and other limitations.
Financial support and sponsorship
This study was supported by Tehran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This research has been supported by Tehran University of Medical Sciences and Health Services grant number 33156.
References
- 1.Rahimi-Movaghar V, Sayyah MK, Akbari H, Khorramirouz R, Rasouli MR, Moradi-Lakeh M, et al. Epidemiology of traumatic spinal cord injury in developing countries: A systematic review. Neuroepidemiology. 2013;41:65–85. doi: 10.1159/000350710. [DOI] [PubMed] [Google Scholar]
- 2.Johnson RL, Brooks CA, Whiteneck GG. Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord. 1996;34:470–80. doi: 10.1038/sc.1996.81. [DOI] [PubMed] [Google Scholar]
- 3.Munce SE, Wodchis WP, Guilcher SJ, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in ontario. Spinal Cord. 2013;51:64–9. doi: 10.1038/sc.2012.81. [DOI] [PubMed] [Google Scholar]
- 4.Rahimi-Movaghar V, Moradi-Lakeh M, Rasouli MR, Vaccaro AR. Burden of spinal cord injury in Tehran, Iran. Spinal Cord. 2010;48:492–7. doi: 10.1038/sc.2009.158. [DOI] [PubMed] [Google Scholar]
- 5.van Langeveld SA, Post MW, van Asbeck FW, Gregory M, Halvorsen A, Rijken H, et al. Comparing content of therapy for people with a spinal cord injury in postacute inpatient rehabilitation in Australia, Norway, and the Netherlands. Phys Ther. 2011;91:210–24. doi: 10.2522/ptj.20090417. [DOI] [PubMed] [Google Scholar]
- 6.Yoshida KK. Institutional impact on self concept among persons with spinal cord injury. Int J Rehabil Res. 1994;17:95–107. doi: 10.1097/00004356-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Brown DJ, Judd FK, Ungar GH. Continuing care of the spinal cord injured. Paraplegia. 1987;25:296–300. doi: 10.1038/sc.1987.55. [DOI] [PubMed] [Google Scholar]
- 8.Kreuter M. Spinal cord injury and partner relationships. Spinal Cord. 2000;38:2–6. doi: 10.1038/sj.sc.3100933. [DOI] [PubMed] [Google Scholar]
- 9.Rigby P, Ryan S, Joos S, Cooper B, Jutai JW, Steggles I, et al. Impact of electronic aids to daily living on the lives of persons with cervical spinal cord injuries. Assist Technol. 2005;17:89–97. doi: 10.1080/10400435.2005.10132099. [DOI] [PubMed] [Google Scholar]
- 10.Welage N, Liu KP. Review of a home and community integration programme for people with spinal cord injuries in Hong Kong and its relevance to Sri Lanka. Hong Kong J Occup Ther. 2008;18:34–9. [Google Scholar]
- 11.Hughes R. The management of patients with spinal cord injury by a hospital-based home care programme. Paraplegia. 1975;12:256–50. doi: 10.1038/sc.1974.39. [DOI] [PubMed] [Google Scholar]
- 12.Kendall MB, Ungerer G, Dorsett P. Bridging the gap: Transitional rehabilitation services for people with spinal cord injury. Disabil Rehabil. 2003;25:1008–15. doi: 10.1080/0963828031000122285. [DOI] [PubMed] [Google Scholar]
- 13.Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB, et al. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1793–803. doi: 10.1016/j.apmr.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 14.Seplowitz C. Technology and occupational therapy in the rehabilitation of the bedridden quadriplegic. Am J Occup Ther. 1984;38:743–7. doi: 10.5014/ajot.38.11.743. [DOI] [PubMed] [Google Scholar]
- 15.Biering-Sørensen T, Hansen RB, Biering-Sørensen F. Home aids and personal assistance 10-45 years after spinal cord injury. Spinal Cord. 2009;47:405–12. doi: 10.1038/sc.2008.132. [DOI] [PubMed] [Google Scholar]
- 16.Stiens SA, Fawber HL, Yuhas SA. The person with a spinal cord injury: An evolving prototype for life care planning. Phys Med Rehabil Clin N Am. 2013;24:419–44. doi: 10.1016/j.pmr.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Cruise CM, Lee MH. Delivery of rehabilitation services to people aging with a disability. Phys Med Rehabil Clin N Am. 2005;16:267–84. doi: 10.1016/j.pmr.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Nelson AL, Kelley B. Patient and family workshops: A new teaching approach for spinal cord injury. Rehabil Nurs. 1983;8:13–6. doi: 10.1002/j.2048-7940.1983.tb02477.x. [DOI] [PubMed] [Google Scholar]
- 19.Kinnersly D, Grundy D, Russell J. ABC of spinal cord injury. Transfer of care from hospital to community. Br Med J (Clin Res Ed) 1986;292:607–9. doi: 10.1136/bmj.292.6520.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall KM, Knudsen ST, Wright J, Charlifue SW, Graves DE, Werner P, et al. Follow-up study of individuals with high tetraplegia (C1-C4) 14 to 24 years postinjury. Arch Phys Med Rehabil. 1999;80:1507–13. doi: 10.1016/s0003-9993(99)90265-4. [DOI] [PubMed] [Google Scholar]
- 21.Harvey C, Wilson SE, Greene CG, Berkowitz M, Stripling TE. New estimates of the direct costs of traumatic spinal cord injuries: Results of a nationwide survey. Paraplegia. 1992;30:834–50. doi: 10.1038/sc.1992.160. [DOI] [PubMed] [Google Scholar]
- 22.Weitzenkamp DA, Whiteneck GG, Lammertse DP. Predictors of personal care assistance for people with spinal cord injury. Arch Phys Med Rehabil. 2002;83:1399–405. doi: 10.1053/apmr.2002.35087. [DOI] [PubMed] [Google Scholar]
- 23.Williams R, Murray A. Prevalence of depression after spinal cord injury: A meta-analysis. Arch Phys Med Rehabil. 2015;96:133–40. doi: 10.1016/j.apmr.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Beedie A, Kennedy P. Quality of social support predicts hopelessness and depression post spinal cord injury. J Clin Psychol Med Settings. 2002;9:227–34. [Google Scholar]
- 25.Elliott TR, Herrick SM, Witty TE, Godshall F, Spruell M. Social support and depression following spinal cord injury. Rehabil Psychol. 1992;37:37–48. [Google Scholar]
- 26.Kishi Y, Robinson RG, Forrester AW. Prospective longitudinal study of depression following spinal cord injury. J Neuropsychiatry Clin Neurosci. 1994;6:237–44. doi: 10.1176/jnp.6.3.237. [DOI] [PubMed] [Google Scholar]
- 27.Michael M, Roth K. Against all odds: A qualitative study of rehabilitation of persons with spinal cord injury in Afghanistan. Spinal Cord. 2012;50:864–8. doi: 10.1038/sc.2012.113. [DOI] [PubMed] [Google Scholar]
- 28.Barclay L, McDonald R, Lentin P. Social and community participation following spinal cord injury: A critical review. Int J Rehabil Res. 2015;38:1–9. doi: 10.1097/MRR.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 29.Dijkers M. Quality of life after spinal cord injury: A meta analysis of the effects of disablement components. Spinal Cord. 1997;35:829–40. doi: 10.1038/sj.sc.3100571. [DOI] [PubMed] [Google Scholar]
- 30.Abeyta N, Freeman ES, Primack D, Hammond FM, Dragon C, Harmon A, et al. SCIRehab project series: The social work/case management taxonomy. J Spinal Cord Med. 2009;32:336–42. doi: 10.1080/10790268.2009.11760787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil. 1998;79:1433–9. doi: 10.1016/s0003-9993(98)90240-4. [DOI] [PubMed] [Google Scholar]
- 32.Ottomanelli L, Lind L. Review of critical factors related to employment after spinal cord injury: Implications for research and vocational services. J Spinal Cord Med. 2009;32:503–31. doi: 10.1080/10790268.2009.11754553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sabata D, Bruce C, Sanford J. Preparing home health clients for work opportunities with workplace accommodation. Home Healthc Manag Pract. 2006;19:12–8. [Google Scholar]
- 34.Engstrand JL, Rn MA. The Operation of a hospital based specialty home health team: Activities and associated costs. Rehabil Nurs. 2000;25:70–5. doi: 10.1002/j.2048-7940.1978.tb00847.x. [DOI] [PubMed] [Google Scholar]
- 35.Fronek P, Booth S, Kendall M, Miller D, Geraghty T. The effectiveness of a sexuality training program for the interdisciplinary spinal cord injury rehabilitation team. Sex Disabil. 2005;23:51–63. [Google Scholar]
- 36.Fronek P, Kendall M, Booth S, Eugarde E, Geraghty T. A longitudinal study of sexuality training for the interdisciplinary rehabilitation team. Sex Disabil. 2011;29:87–100. [Google Scholar]
- 37.Wallace MA, Kendall MB. Transitional rehabilitation goals for people with spinal cord injury: Looking beyond the hospital walls. Disabil Rehabil. 2014;36:642–50. doi: 10.3109/09638288.2013.805259. [DOI] [PubMed] [Google Scholar]
- 38.Kirshblum SC, Priebe MM, Ho CH, Scelza WM, Chiodo AE, Wuermser LA, et al. Spinal cord injury medicine 3. Rehabilitation phase after acute spinal cord injury. Arch Phys Med Rehabil. 2007;88:S62–70. doi: 10.1016/j.apmr.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Petrofsky JS. The use of electromyogram biofeedback to reduce trendelenburg gait. Eur J Appl Physiol. 2001;85:491–5. doi: 10.1007/s004210100466. [DOI] [PubMed] [Google Scholar]
- 40.Nightingale EJ, Raymond J, Middleton JW, Crosbie J, Davis GM. Benefits of FES gait in a spinal cord injured population. Spinal Cord. 2007;45:646–57. doi: 10.1038/sj.sc.3102101. [DOI] [PubMed] [Google Scholar]
- 41.Dolbow DR, Gorgey AS, Ketchum JM, Moore JR, Hackett LA, Gater DR, et al. Exercise adherence during home-based functional electrical stimulation cycling by individuals with spinal cord injury. Am J Phys Med Rehabil. 2012;91:922–30. doi: 10.1097/PHM.0b013e318269d89f. [DOI] [PubMed] [Google Scholar]
- 42.Taylor PN, Ewins DJ, Fox B, Grundy D, Swain ID. Limb blood flow, cardiac output and quadriceps muscle bulk following spinal cord injury and the effect of training for the odstock functional electrical stimulation standing system. Paraplegia. 1993;31:303–10. doi: 10.1038/sc.1993.53. [DOI] [PubMed] [Google Scholar]
- 43.Johnston TE, Smith BT, Oladeji O, Betz RR, Lauer RT. Outcomes of a home cycling program using functional electrical stimulation or passive motion for children with spinal cord injury: A case series. J Spinal Cord Med. 2008;31:215–21. doi: 10.1080/10790268.2008.11760715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Galea M, Tumminia J, Garback LM. Telerehabilitation in spinal cord injury persons: A novel approach. Telemed J E Health. 2006;12:160–2. doi: 10.1089/tmj.2006.12.160. [DOI] [PubMed] [Google Scholar]
- 45.Kowalczewski J, Chong SL, Galea M, Prochazka A. In-home tele-rehabilitation improves tetraplegic hand function. Neurorehabil Neural Repair. 2011;25:412–22. doi: 10.1177/1545968310394869. [DOI] [PubMed] [Google Scholar]
- 46.Phillips VL, Vesmarovich S, Hauber R, Wiggers E, Egner A. Telehealth: Reaching out to newly injured spinal cord patients. Public Health Rep. 2001;116(Suppl 1):94–102. doi: 10.1093/phr/116.S1.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Straaten MG, Cloud BA, Morrow MM, Ludewig PM, Zhao KD. Effectiveness of home exercise on pain, function, and strength of manual wheelchair users with spinal cord injury: A high-dose shoulder program with telerehabilitation. Arch Phys Med Rehabil. 2014;95:1810–700. doi: 10.1016/j.apmr.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Woo C, Guihan M, Frick C, Gill CM, Ho CH. What's happening now! Telehealth management of spinal cord injury/disorders. J Spinal Cord Med. 2011;34:322–31. doi: 10.1179/2045772311Y.0000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Hedel HJ. Improvement in function after spinal cord injury: The black-box entitled rehabilitation. Swiss Med Wkly. 2012;142:w13673. doi: 10.4414/smw.2012.13673. [DOI] [PubMed] [Google Scholar]


