Abstract
Background
Established tibial nonunions rarely heal without secondary intervention; revision surgery is the most common intervention. Herein, we evaluated the clinical outcomes of patients with tibial nonunion treated with a new technique – minimally invasive percutaneous plate osteosynthesis (MIPPO) – combined with a new onionskin-like autologous bone grafting method.
Material/Methods
From 2010 to 2013, 18 patients with tibial nonunions (average bone defect: 9.5 mm) were treated with MIPPO technology combined with onionskin-like autologous bone grafting. Indices for clinical evaluation included operative time, fluoroscopy time, blood loss, hospital stay, healing time, postoperative complaints, radiographic performances, the Short Musculoskeletal Function Assessment (SMFA) questionnaire, and the American Orthopedic Foot & Ankle Society (AOFAS) ankle-hindfoot score.
Results
The average operation and fluoroscopy times for tibial nonunion were 65 min and 15.5 s, respectively, with a total blood loss of 107.7 mL. The mean duration of hospital stay was 12.8 days. The mean follow-up time was 11.9 months, and all patients achieved radiologically confirmed bony healing in an average time of 13.1 weeks. No lower-leg deformity, fixation failure, infection, and vascular, or nerve injuries were recorded in any patient, and only 4 patients complained of slight limb pain upon total weight-bearing at the end of follow-up. The SMFA and AOFAS ankle-hindfoot scores of patients were graded excellent in 14 (77.8%) and good in 4 (22.2%), indicating high functional recovery.
Conclusions
MIPPO technology combined with onionskin bone grafting is an efficient method to treat patients with tibial nonunion, especially for patients with poor soft tissue condition.
MeSH Keywords: Bone Transplantation, Fracture Fixation, Tibia
Background
Bone nonunion is a major problem in orthopedics, and tibial nonunion is the most common type, with an incidence of about 12% [1]. When long-bone fractures are accompanied by open injury, the incidence of bone nonunion increases up to 17%, and the rate of delayed union of fracture is 5% [2]. The tibial nutrient artery provides two-thirds of the blood supply to the tibia, passes through the lateral third of the tibial shaft, and then enters the bone marrow cavity in the compact bone for a short distance. Factors such as high-energy trauma, infection, and iatrogenic factors (e.g., excessive periosteal stripping, blood supply destruction, and lack of soft-tissue protection) can cause tibial nonunion [3]. Patients with tibial nonunion usually present with concomitant muscle atrophy in the lower leg and require repeated surgeries, often leading to a complete loss of confidence, as well as discouragement and depression.
Conventional open reduction and internal fixation for the treatment of bone nonunion can result in many complications, including skin necrosis, soft-tissue infections, nerve and vascular injury, and delayed bony unions [4,5]. Minimally invasive percutaneous plate osteosynthesis (MIPPO) technology has been widely applied in the treatment of various cases of trauma, including tibial nonunion. The MIPPO technology can reduce major injury to soft tissues and exhibits good clinical outcomes without direct exposure of the fracture site [6–10].
As the criterion standard for treatment of bone nonunion, researchers have investigated the effect of various bone graft types to repair tibial nonunion [11]. Numerous bone grafting approaches have been advocated for the treatment of delayed union and nonunion fractures, including open bone grafting, minimally invasive bone grafting, and central bone grafting [12]. However, these techniques reportedly involve complications such as nerve injury, infection, iliac bony fracture, bone nonunion recurrence, poor soft-tissue condition, and painful scars [13–15]. Therefore, a new autologous bone grafting method to overcome the disadvantages of the present techniques is needed.
In this article, we retrospectively analyzed the medical records of 18 patients diagnosed with tibial nonunion and treated with MIPPO technology combined with a new bone grafting method – onionskin autologous bone grafting (Figure 1). Indices for clinical evaluation including operative time, fluoroscopy times, blood loss, hospital stay, healing time, postoperative complaints, radiographic performances, and limb function recovery were investigated to evaluate the clinical outcomes of this new treatment method.
Figure 1.
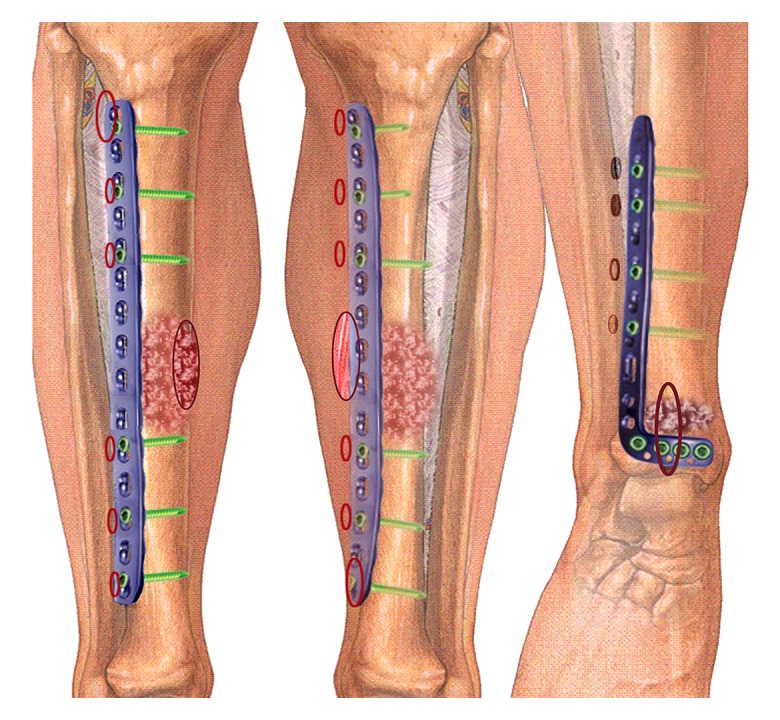
Scheme of minimally invasive percutaneous plate osteosynthesis (MIPPO) combined with onionskin-like autologous bone grafting in the treatment of tibial nonunion.
Material and Methods
Ethics approval and patient characteristics
The study was approved by the Ethics Committee of the Second Hospital of Jilin University. From 2010 to 2013, 18 patients admitted to our department with tibial nonunion (average bone defect: 9.5 mm) and treated with MIPPO technology combined with onionskin-like autologous bone grafting were included in this study (Figure 2). The mean age of patients was 41.9 years (range: 24–57). Each case of nonunion was classified by its location in the tibia: proximal (4 patients), middle (4 patients), distal (9 patients), or middle and distal (1 patient) thirds of the tibia. Ten patients sustained multiple fractures, including femoral fracture and comminuted tibiofibular fracture. One patient had a nerve injury, 1 patient had a vascular injury, and 6 patients had open fractures of the tibia and fibula. Anterolateral plates were used in 11 cases, medial plates were used in 6 cases, and both anterolateral and medial plates were used in 1 case (Table 1).
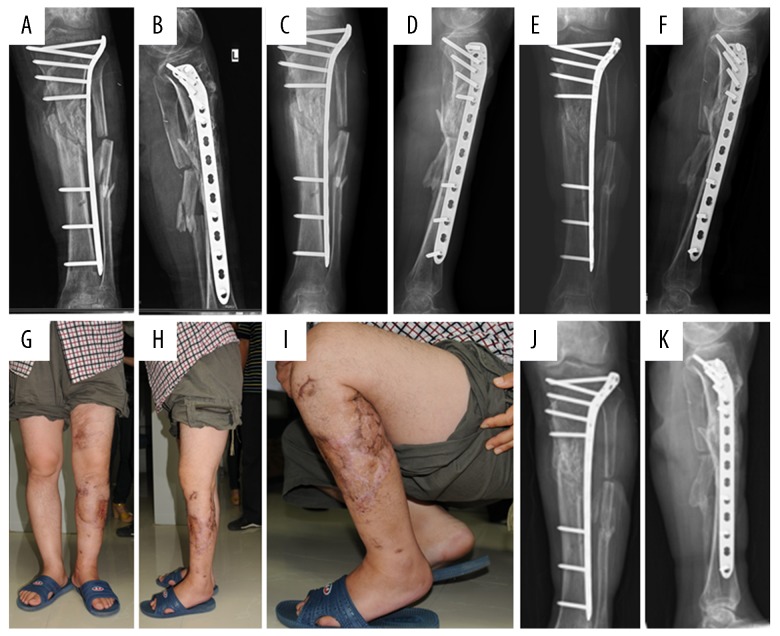
Figure 2.
A male patient with open comminuted fracture of the left tibiofibular and upper leg degloving injury. (A, B) Radiography showed comminuted fracture of the upper segment of the left tibiofibula with obvious displacement. (C, D) Soft tissue condition indicated the anterior and lateral skins of the upper left leg were torn and sutured and extensively leathered. (E, F) Postoperative radiography after emergency second-stage clearance showed that the position of the external fixator was acceptable. (G–L) Radiographic examinations showed poor alignment, and no callus formation at 1 and 3 months after surgery, as well as extensive scarring on the medial part of the upper leg.
Table 1.
Patients’ general characteristics.
| Case | Age (years) | Sex | Side | Location in tibia | Grade | The initial operation | Bone defect(mm) |
|---|---|---|---|---|---|---|---|
| 1 | 49 | M | L | Distal | A1 | External fixator | 6 |
| 2 | 51 | M | L | Distal | B2 | External fixator | 12 |
| 3 | 57 | M | R | Distal | A2-1 | External fixator | 5 |
| 4 | 48 | M | L | Mid-shaft | A2-1 | Intramedullary nail | 7 |
| 5 | 32 | M | L | Mid-shaft | A2-1 | Intramedullary nail | 9 |
| 6 | 57 | M | R | Mid-shaft/distal | A1 | External fixator | 8 |
| 7 | 46 | M | R | Distal | A2-2 | LCP | 6 |
| 8 | 24 | M | R | Distal | A2-2 | External fixator | 15 |
| 9 | 41 | M | R | Distal | B1 | LCP | 17 |
| 10 | 40 | M | L | Proximal | B1 | External fixator | 16 |
| 11 | 39 | M | R | Distal | A2-1 | External fixator | 6 |
| 12 | 46 | M | L | Proximal | B2 | LCP | 14 |
| 13 | 48 | M | L | Mid-shaft | A2-1 | External fixator | 7 |
| 14 | 33 | M | L | Distal | A2-2 | Intramedullary nail | 8 |
| 15 | 37 | M | L | Proximal | B1 | External fixator (with LISS plate) | 18 |
| 16 | 43 | M | R | Distal | A2-2 | External fixator | 6 |
| 17 | 36 | M | R | Mid-shaft | A1 | Intramedullary nail | 8 |
| 18 | 28 | M | L | Mid-shaft | A2-2 | External fixator | 4 |
All fractures were caused by high-speed injuries, including motor vehicle accidents (motorcycle or car) and falls from height. The patients were initially treated with external or internal fixation, but tibial nonunion occurred 6 months later, making re-operation inevitable. According to the tibial fracture nonunion classification by Paley et al., 4 patients in our study were classified with type A1 (mobile nonunion with <1 cm of bone loss), 5 patients with type A2-1 (stiff nonunion with no deformity and <1 cm of bone loss), 5 patients with type A2-2 (stiff nonunion with a fixed deformity and <1 cm of bone loss), 3 patients with type B1 (bony defect >1 cm with no shortening of the limb), 1 patient with type B2 (bony defect >1 cm with loss of bone length), and no patients with type B3 (bone defect >1 cm and limb shortening) (Table 1).
Operative technique
Each operation was performed under general or epidural anesthesia with the patient positioned supine. To enhance the presentation of the iliac crest and shift the bulk of the abdominal wall, a bolster was placed under the ipsilateral buttock. A 5-cm-long skin incision was made. Blunt dissection was carried out using a periosteum elevator to reach the iliac medial crest, cancellous and cortical bones were obtained from the inner table of the ileum, and the incision was closed. The obtained bone was cut into strips measuring 2–3-mm wide and 40–50-mm long.
The original internal or external fixation was removed using minimally invasive techniques (external fixation was required to be removed 2 weeks before surgery, and the results of blood tests, erythrocyte sedimentation rate, and C-reactive protein levels indicative of no infection) and a 3–4-cm skin incision was made above the tibial nonunion. The surgeon removed the fibrous tissue from the nonunion; freshened the ends of the fragments; opened the medullary cavity; and stripped 1–2 mm of the broken end of the periosteum by using a pith nucleus clamp, bone knife, small spatula, and little bite forceps; and then filled the defect at the nonunion with corticocancellous bone obtained through the iliac bone by using hemostatic forceps. Six small incisions were required for the plate implantation, each of which was 8–10 mm long. Finally, the incisions were closed with sutures and a subcutaneous drain was inserted (Figure 3).
Figure 3.
Intraoperative images: (A) A small incision to remove the regenerated tissue from the nonunion location, (B) MIPPO technique was used to insert the plate, (C, D) onionskin-like bone grafting was performed, (E) postoperative incision image showed minimal invasion. (F, G) Postoperative radiographic examination showed that the plate was in good position with well-reduced tibiofibula fracture, and sufficient bone grafting.
Onionskin autologous bone grafting
The onionskin autologous bone grafting procedure included the following steps: (1) The periosteum and scar tissue around the broken end of the bone were peeled off by about 2.0 mm. (2) The region other than the cortical bone was implanted with cancellous bone particles (section A). (3) The area corresponding to the cortical bone at both ends was implanted with cancellous bone strips (section B). (4) The medullary cavity area, namely the area inside the cortical bone, was implanted with the elongated cancellous and cortical bone strips. Usually the cancellous bone faces outward and the length must exceed the gap of nonunion (section C). (5) The plate was percutaneously implanted (Synthes, Switzerland, section D). (6) The screws were inserted to bridge and fix the plate and bone graft area. (7) Finally, the cancellous bone was implanted into the gap next to the bone plate (section E) (Figure 4).
Figure 4.
“Onionskin” bone graft procedures and cross-sectional schematic of onionskin-like bone graft.
Postoperative attention and follow-up
After surgery, each patient was discharged, with permission to walk with crutches, but no weight-bearing was allowed on the involved leg for 2 weeks. Partial weight-bearing was allowed after 2 weeks and gradually increased until the radiographic criteria for early consolidation were met. Full weight-bearing was allowed 6–8 weeks later.
All patients required limb function investigation and radiographic examinations at 1, 3, 6, 12, and 24 months postoperatively. Clinical healing was defined as the ability of the patient to bear weight painlessly on the affected limb and a lack of pain response when manual stress was applied across the site of nonunion by an examiner. Radiographic results were assessed by measuring tibial angulation, shortening, and healing at the last follow-up. The Short Musculoskeletal Function Assessment (SMFA) questionnaire and American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot score were used to evaluate the postoperative function outcomes of patients at each visit [16].
Results
A total of 18 patients underwent MIPPO combined with a new onionskin-like autologous bone grafting intervention for tibial nonunion and completed the follow-up until at least 3 months postoperatively. The average operation and fluoroscopy times for tibial nonunion were 65.0 min (range: 45–90 min) and 15.5 s (range: 10–24 s), respectively, with a total blood loss for 107.7 mL (range: 90–130 mL). The average hospital stay was 12.8 days (range: 8–18 days) (Table 2).
Table 2.
The operation and hospital stay information summary.
| Case | Plate position | Bone graft incision | Incision length (cm) | Relationship between incision and plate | Operative time (min) | Fluoroscopy times | Blood loss (mL) | Hospital stay (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | Anterolateral | Anterolateral | 4.0 | Ipsilateral | 90 | 15 | 130 | 12 |
| 2 | Anterolateral | Anterolateral | 5.5 | Ipsilateral | 70 | 17 | 100 | 15 |
| 3 | Medial | Anterolateral | 5.5 | Contralateral | 65 | 10 | 90 | 18 |
| 4 | Anterolateral | Anterolateral | 5.0 | Ipsilateral | 85 | 13 | 90 | 17 |
| 5 | Anterolateral | Anterolateral | 4.0 | Ipsilateral | 50 | 18 | 100 | 8 |
| 6 | Anterolateral/medial | Anterolateral | 5.0 | Ipsilateral | 60 | 12 | 105 | 8 |
| 7 | Medial | Anterolateral | 5.5 | Contralateral | 55 | 24 | 110 | 9 |
| 8 | Anterolateral | Anterolateral | 4.0 | Ipsilateral | 45 | 14 | 120 | 9 |
| 9 | Anterolateral | Anterolateral | 5.0 | Ipsilateral | 70 | 16 | 130 | 10 |
| 10 | Anterolateral | Anterolateral | 5.5 | Ipsilateral | 55 | 18 | 130 | 15 |
| 11 | Medial | Anterolateral | 4.5 | Contralateral | 60 | 19 | 95 | 16 |
| 12 | Anterolateral | Anterolateral | 4.5 | Ipsilateral | 75 | 21 | 105 | 10 |
| 13 | Medial | Anterolateral | 5.0 | Contralateral | 80 | 11 | 95 | 15 |
| 14 | Medial | Anterolateral | 5.5 | Contralateral | 75 | 16 | 100 | 14 |
| 15 | Anterolateral | Anterolateral | 5.5 | Ipsilateral | 55 | 12 | 120 | 14 |
| 16 | Anterolateral | Medial | 5.0 | Contralateral | 45 | 10 | 105 | 9 |
| 17 | Anterolateral | Anterolateral | 4.5 | Ipsilateral | 60 | 12 | 120 | 17 |
| 18 | Anterolateral | Anterolateral | 5.0 | Ipsilateral | 75 | 22 | 95 | 15 |
The mean follow-up time was 11.9 months (range: 7–23 months), and all patients began partial weight-bearing ambulation at 3–4 months postoperatively. The radiological examinations confirmed that all patients achieved bony healing by an average time of 13.1 weeks (range: 4–24 weeks). On the basis of the radiographic assessment, no patient experienced loss of reduction or loss of fixation (Figure 5). Meanwhile, no lower-leg deformity, fixation failure, infection, and vascular or nerve injuries were recorded in any patients, and only 4 patients (22.2%) complained of slight limb pain upon full weight-bearing at the end of the follow-up period. Furthermore, implant removal was done in 11 patients (61.1%), and 16 patients (88.9%) resumed work at the end of the follow-up period (Table 3).
Figure 5.
Postoperative radiographic examinations and functional status: (A, B) Extensive callus formation in the nonunion space seen 1 month after surgery, (C, D, and G–I) Tibial nonunion almost healed, with good functional status. (E, F) The regenerated bone seen in good shape at 7 months after surgery. (J, K) The shape of regenerated bone was almost normal at 17 months after surgery.
Table 3.
Follow-up of the involved patients.
| Case | Union | Infection | LLD | Deformity | Pain | Implant remove | Back to work | Healing time (weeks) | Follow-up time (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Yes | No | No | No | No | No | Yes | 4 | 7 |
| 2 | Yes | No | No | No | No | Yes | Yes | 18 | 18 |
| 3 | Yes | No | No | No | No | Yes | Yes | 16 | 15 |
| 4 | Yes | No | No | No | Slightly | Yes | Yes | 12 | 9 |
| 5 | Yes | No | No | No | No | Yes | Yes | 14 | 9 |
| 6 | Yes | No | No | No | No | No | Yes | 24 | 10 |
| 7 | Yes | No | No | No | Slightly | Yes | Yes | 12 | 8 |
| 8 | Yes | No | No | No | No | Yes | Yes | 12 | 12 |
| 9 | Yes | No | No | No | Slightly | Yes | Yes | 16 | 15 |
| 10 | Yes | No | No | No | No | No | Yes | 7 | 9 |
| 11 | Yes | No | No | No | No | No | Yes | 12 | 7 |
| 12 | Yes | No | No | No | No | No | No | 12 | 8 |
| 13 | Yes | No | No | No | No | Yes | Yes | 13 | 14 |
| 14 | Yes | No | No | No | No | No | No | 8 | 8 |
| 15 | Yes | No | No | No | No | Yes | Yes | 8 | 11 |
| 16 | Yes | No | No | No | No | Yes | Yes | 12 | 12 |
| 17 | Yes | No | No | No | Slightly | No | Yes | 24 | 12 |
| 18 | Yes | No | No | No | No | Yes | Yes | 12 | 23 |
LLD – leg-length discrepancy.
The SMFA scores were collected from the six-week postoperative follow-up. According to the questionnaire, the average bothersome, activities of daily living (ADL), emotion, arm and hand, mobility, and function scores were 22.7, 50.9, 39.7, 5.3, 42.6, and 35.4, respectively. Meanwhile, the AOFAS ankle-hindfoot scores were assessed at the final follow-up. The result showed that the average score of these patients was 91.9, and were graded as excellent in 14 cases (77.8%, 90.0–100.0) and good in 4 cases (22.2%, 75.0–89.0) (Table 4).
Table 4.
Functional outcome scores on the SMFA questionnaire assessed at 6 weeks and AOFAS ankle-hindfoot score assessed at final visit.
| Case | Bothersome | ADL | Emotion | Arm & hand | Mobility | Function | AOFAS ankle-hindfoot score |
|---|---|---|---|---|---|---|---|
| 1 | 22 | 64 | 35 | 7 | 42 | 43 | 98 |
| 2 | 34 | 62 | 42 | 3 | 41 | 34 | 92 |
| 3 | 20 | 48 | 42 | 6 | 48 | 36 | 95 |
| 4 | 36 | 43 | 31 | 3 | 37 | 24 | 76 |
| 5 | 18 | 51 | 47 | 6 | 47 | 39 | 97 |
| 6 | 14 | 50 | 46 | 7 | 44 | 36 | 93 |
| 7 | 27 | 61 | 33 | 7 | 36 | 30 | 90 |
| 8 | 20 | 40 | 42 | 6 | 45 | 35 | 94 |
| 9 | 31 | 39 | 40 | 6 | 35 | 24 | 78 |
| 10 | 28 | 48 | 46 | 3 | 48 | 42 | 97 |
| 11 | 15 | 52 | 43 | 5 | 46 | 46 | 100 |
| 12 | 10 | 49 | 41 | 6 | 47 | 36 | 93 |
| 13 | 27 | 57 | 37 | 4 | 44 | 34 | 92 |
| 14 | 20 | 60 | 38 | 5 | 40 | 30 | 89 |
| 15 | 16 | 43 | 41 | 7 | 45 | 38 | 95 |
| 16 | 19 | 48 | 40 | 3 | 44 | 43 | 97 |
| 17 | 30 | 52 | 32 | 5 | 34 | 26 | 82 |
| 18 | 22 | 50 | 38 | 6 | 43 | 41 | 96 |
ADL – activity of daily living.
Discussion
In the treatment of bone nonunion, bone grafting has irreplaceable functions, including stimulating the fracture end, filling the tissue defect, and producing new blood to promote fracture healing [11]. Autologous bone grafting is the criterion standard and is the most frequently applied method in the treatment of nonunion because of its osteoinductive and osteoconductive properties and the capacity of introducing new osteogenic bone marrow cells to the fracture site [17].
Traditional open bone grafting usually requires a large incision, wound debridement, opening of the medullary cavity, bone transplantation into the fracture end, and stabilization of the fracture end with internal fixation. The incision is usually 10–20-mm longer than the plate and requires extensive periosteal stripping, although there are advantages of clear exposure and effective anatomical reduction of open bone grafting, with bone union rates of 70–95%. However, obvious weaknesses are observed, including major operation trauma, significant bleeding, long healing time, and a higher risk of surgical complications, rendering this procedure especially unsuitable for patients with poor soft tissue condition [18,19].
Minimally invasive bone grafting methods obtain bone grafts from the iliac crest and drive them into the hole across the fracture line using complicated equipment. Its advantages, such as small incision, faster recovery, and less trauma and pain, make it a good choice for surgeons. However, the high cost of the complicated equipment and high technical requirements are widely criticized [20]. Central bone grafting places the cancellous graft in the newly created central space between the tibia and fibula. By reducing the risk of neurovascular injury, this method is relatively simple and safe. However, major operative trauma, significant bleeding, and longer healing time are observed and limit its wide application [15].
To overcome these problems, we developed a new method, called onionskin bone grafting. In this method, the surgeon can choose the regions with good skin or muscle tissue condition. By effectively removing fibrous scar tissue and bone sclerosis of the bone defect area, as well as protecting the blood supply of the bone defect area, the risk of infection is reduced, and the bone defect repair process is accelerated. The average incision length is about 3–4 cm (the incision should be appropriately extended as needed). The main tools used in onionskin bone grafting are common, including a pith nucleus clamp, small knife, small spatula, and little bite forceps. Compared with other bone grafting methods, the benefits of our technique include small incision, less physiological interference, faster healing, and use of simple and convenient surgical instruments.
Bone nonunion is usually accompanied by fixation failure such as plate breakage and screw loosening, which both require replacement involving internal fixation [21]. Here, we removed the original plate by using a minimally invasive method consisting of percutaneous removal of the screws and plate through small incisions. A new plate was implanted using MIPPO technology from another small incision, which effectively protected the blood supply of the bone periosteum, stabilized the fractured end, and provided favorable conditions for nonunion healing.
Various treatment methods have been attempted to cure tibial nonunion. For instance, reamed intramedullary exchange nailing including correction of axis alignment was shown to be a safe and effective treatment for tibial nonunion, with a high rate of bone healing and good functional long-term outcome [22]. Richmond et al. reported that patients with distal tibial nonunions treated with statically locked intramedullary nails achieved high healing rate (29/32, 90.6%) [23]. Bryce et al. reported that 87 of 94 patients who had aseptic tibial nonunions (92.6%) healed following slow gradual compression across the nonunion site with a circular external fixator [24]. Our results showed MIPPO technology combined with onionskin bone grafting in all 18 cases achieved clinical bony healing (100%), indicating a higher healing rate than that reported in previous studies. The average healing time was 13.1 weeks (range: 4–24 weeks) with scarified SMFA scores and no obvious complications including deformities, fixation failure, infection, vascular or nerve injuries, or skin necrosis. These data verified that this novel method is a safe and effective intervention for the treatment of tibial nonunion, even if the treated patients have poor soft-tissue condition.
The previously mentioned mainstream bone grafting technique includes structural bone grafting, iliac bone grafting, and granule bone grafting. MIPPO combined with onionskin-like autologous bone grafting has several advantages: (1) A limited small incision is applied to clean the end of the bone nonunion leading to less bleeding. (2) The periosteum and scar are not removed and hence, the local soft-tissue blood supply is protected. (3) Autologous iliac bone graft can provide bone conduction matrix, osteoinductive factors, and osteoblasts to achieve bone conduction, osteoinduction, and osteogenesis, respectively. (4) The technique of onionskin bone grafting can provide sufficient mechanical support, and the implanted cancellous bone strip acts as a bridge, which is conducive to fracture healing. (5) The overall infection rate is low, as supported by no reports of infections in our study. (6) No skin necrosis occurred in this study, and patients were very satisfied with the length of the incision. (7) The patients’ postoperative function was good and the nonunion healing rate was high with limited complications, which significantly shortened the duration of hospital stay and reduced costs.
Our study has several limitations. First, the technique is slightly complicated, as it is a combination of MIPPO technology, small-incision end-cleaning technology, minimally invasive bone grafting technology, and bone nonunion technology. Hence, it is only suitable for very skilled practitioners. Second, the formation of callus is mostly limited to the end of the bone, with much less external callus formation around it. The bone strength is slightly lower than normal bone tissue after healing of the nonunion. Third, this study’s retrospective design prevents comparisons with other technical groups. Lastly, the sample size of this study was small and the follow-up period was short.
Conclusions
The innovative application of MIPPO technology combined with a new onionskin autologous bone grafting technique can preserve bone blood supply, promote fracture healing, and reduce the risk of infection and re-fracture. This is a very promising treatment for tibial nonunion, and it is especially suited for patients with poor soft-tissue condition.
Acknowledgments
We would like to thank Prof. Jincheng Wang who provided encouragement to write this paper and gave valuable advice.
Footnotes
Source of support: This study was supported by the National Natural Science Foundation of China (Grant Nos. 81171681, 81701811, 81671804, and 81772456), the Scientific Development Program of Jilin Province (Grant Nos. 20190304123YY, 20180623050TC and 20180201041SF), the Program of Jilin Provincial Health Department (Grant Nos. 2017F007, 2016Q021 and 2016C037), the Cultivation Program from the Second Hospital of Jilin University for National Natural Science Foundation (Grant No. KYPY2018-01), and the Youth Talents Promotion Project of Jilin Province (Grant No. 192004)
References
- 1.Bell A, Templeman D, Weinlein JC. Nonunion of the femur and tibia: An update. Orthop Clin N Am. 2016;47(2):365–75. doi: 10.1016/j.ocl.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 2.Westgeest J, Weber D, Dulai SK, et al. Factors associated with development of nonunion or delayed healing after an open long bone fracture: A prospective cohort study of 736 subjects. J Orthop Trauma. 2016;30(3):149–55. doi: 10.1097/BOT.0000000000000488. [DOI] [PubMed] [Google Scholar]
- 3.Ma H, Zhao J, Yu B, Ye B. A gross anatomic study of distal tibia and fibula for single-incision approach. J Orthop Surg Res. 2014;9:28. doi: 10.1186/1749-799X-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allende C, Allende BT. Post-traumatic distal humerus non-union: Open reduction and internal fixation: long-term results. Int Orthop. 2009;33(5):1289–94. doi: 10.1007/s00264-008-0650-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dy CJ, Little MT, Berkes MB, et al. Meta-analysis of re-operation, nonunion, and infection after open reduction and internal fixation of patella fractures. J Trauma Acute Care Surg. 2012;73(4):928–32. doi: 10.1097/TA.0b013e31825168b6. [DOI] [PubMed] [Google Scholar]
- 6.Lai TC, Fleming JJ. Minimally invasive plate osteosynthesis for distal tibia fractures. Clin Podiatr Med Surg. 2018;35(2):223–32. doi: 10.1016/j.cpm.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: Minimally invasive plate osteosynthesis. Injury. 2004;35:615–20. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004;35:608–14. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Ghera S, Santori FS, Calderaro M, Giorgini TL. Minimally invasive plate osteosynthesis in distal tibial fractures: Pitfalls and surgical guidelines. Orthopedics. 2004;27:903–5. doi: 10.3928/0147-7447-20040901-09. [DOI] [PubMed] [Google Scholar]
- 10.Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect. 2004;53:471–75. [PubMed] [Google Scholar]
- 11.Fillingham Y, Jacobs J. Bone grafts and their substitutes. Bone Joint J. 2016;98(1 Suppl A):6–9. doi: 10.1302/0301-620X.98B.36350. [DOI] [PubMed] [Google Scholar]
- 12.Sun SG, Zhang Y, Zheng LH, et al. Application of locking plate in long-bone atrophic nonunion following external fixation. Orthopedics. 2011;34:358. doi: 10.3928/01477447-20110317-12. [DOI] [PubMed] [Google Scholar]
- 13.Kettunen J, Mäkelä EA, Turunen V, et al. Percutaneous bone grafting in the treatment of the delayed union and non-union of tibial fractures. Injury. 2002;33:239–45. doi: 10.1016/s0020-1383(01)00075-4. [DOI] [PubMed] [Google Scholar]
- 14.Gulan G, Jotanović Z, Jurdana H, et al. Treatment of infected tibial nonunion with bone defect using central bone grafting technique. Coll Antropol. 2012;36(2):617–21. [PubMed] [Google Scholar]
- 15.Ryzewicz M, Morgan SJ. Central bone grafting for nonunion of fractures of the tibia. J Bone Joint Surg Br. 2009;91:522–29. doi: 10.1302/0301-620X.91B4.21399. [DOI] [PubMed] [Google Scholar]
- 16.Gross SC, Galos DK, Taormina DP, et al. Can tibial shaft fractures bear weight after intramedullary nailing? A randomized controlled trial. J Orthop Trauma. 2016;30(7):370–75. doi: 10.1097/BOT.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 17.Higgins TF, Marchand LS. Basic science and clinical application of reamed sources for autogenous bone graft harvest. J Am Acad Orthop Surg. 2018;26(12):420–28. doi: 10.5435/JAAOS-D-16-00512. [DOI] [PubMed] [Google Scholar]
- 18.Kusnezov N, Prabhakar G, Dallo M, et al. Bone grafting via reamer-irrigator-aspirator for nonunion of open Gustilo-Anderson type III tibial fractures treated with multiplanar external fixator. SICOT J. 2017;3:30. doi: 10.1051/sicotj/2017002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egol KA, Nauth A, Lee M, et al. Bone grafting: Sourcing, timing, strategies, and alternatives. J Orthop Trauma. 2015;29(Suppl 12):S10–14. doi: 10.1097/BOT.0000000000000460. [DOI] [PubMed] [Google Scholar]
- 20.Bushnell BD, Dahners LE. The syringe technique for minimally invasive bone grafting. J Orthop Trauma. 2005;19(9):650–55. doi: 10.1097/01.bot.0000174376.68657.4b. [DOI] [PubMed] [Google Scholar]
- 21.Barrera-Ochoa S, Rodríguez-Alabau S, Sallent A, et al. Volar locking plate breakage after nonunion of a distal radius osteotomy. Case Rep Med. 2016;2016 doi: 10.1155/2016/6836190. 6836190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hierholzer C, Friederichs J, Glowalla C, et al. Reamed intramedullary exchange nailing in the operative treatment of aseptic tibial shaft nonunion. Int Orthop. 2017;41(8):1647–53. doi: 10.1007/s00264-016-3317-x. [DOI] [PubMed] [Google Scholar]
- 23.Richmond J, Colleran K, Borens O, et al. Nonunions of the distal tibia treated by reamed intramedullary nailing. J Orthop Trauma. 2004;18:603–10. doi: 10.1097/00005131-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Cunningham BA, O’Connor DP, Brinker MR. High rate of union for aseptic distal tibial nonunions in adults treated with slow gradual compression via circular external fixation. J Orthop Trauma. 2018;32(6):301–5. doi: 10.1097/BOT.0000000000001141. [DOI] [PubMed] [Google Scholar]