Abstract
A study of clinical records and temporal bone histopathology from a woman with bilateral otosclerosis who was treated with lateral semicircular canal fenestration procedures as well as stapedectomy.
Keywords: otopathology, temporal bone, histology, otosclerosis, fenestration procedure, stapedectomy
INTRODUCTION
Otosclerosis is a condition of abnormal bony remodeling of the otic capsule that often results in stapes fixation and conductive hearing loss. One‐third of patients with otosclerosis also develop a progressive sensorineural component that exceeds typical age‐related sensorineural hearing loss.1
Valsalva first described stapes ankylosis as a cause of hearing loss in 1704. Adam Politzer described the pathology as due to “new bone, overgrowing the oval window and stapes” in 1893. This corresponded with the first era of stapes surgery, which consisted of stapes mobilization, trephination, or removal. As these procedures became more common in Europe, complications of meningitis and death were recognized and led to the denouncement and abandonment of the procedures around 1900.2
Following this, otologists continued to investigate alternative, safer methods of surgically correcting the conductive hearing loss from otosclerosis. In 1938, Julius Lempert described a breakthrough technique of an exteriorized lateral semicircular canal (SCC) fenestration via an endaural approach, performed in a single‐stage. About 50% of patients who had this procedure had improvement of their conductive hearing loss (CHL) to a 20–25 dB air‐bone gap with lasting results. This marked the rise of the fenestration era of otosclerosis surgery.2
In the 1950s, work by Samuel Rosen, John Shea, Harold Schuknecht, and Howard House resulted in the proven safety and efficacy of a transcanal stapedectomy with prosthesis placement. This operation led to superior hearing results compared to lateral SCC fenestration and marked the start of the modern era of otosclerosis surgery.
In this report, we present an otopathologic study of a woman with bilateral otosclerosis who lived and was treated during both the fenestration and stapedectomy eras of otosclerosis surgery.
MATERIAL AND METHODS
The clinical history was collected during life through enrollment in the National Institute on Deafness and Other Communication Disorders (NIDCD), National Temporal Bone, Hearing, and Balance Pathology Resource Registry. After death, both temporal bones were prepared for light microscopy by fixation in formalin (postmortem time was 19.5 hours) followed by standard processing for histologic examination, including decalcification with ethylenediamine tetra‐acetic acid and celloidin embedding. Both specimens were sectioned serially in the horizontal plane at a section thickness of 20 μm. Every 10th section was stained with hematoxylin and eosin and mounted on a glass slide. The slides were examined by light microscopy.
Two‐dimensional graphic reconstruction of the cochlea was performed using published accepted methods3 to quantify cellular and acellular elements. Hair cells were recorded as being present or absent. Presence of stereocilia (at high magnification of ×400–1,000) was the criterion used to determine whether a cell within the organ of Corti was a hair cell or not. Atrophy of the stria vascularis was estimated as a percent of normal in 10% increments. The number of cochlear neuronal cells was counted, calculated, and expressed as a percentage of normal for age‐matched control subjects.
RESULTS
This woman was born in 1923 and was diagnosed with bilateral otosclerosis as a young adult. At age 22, she underwent a right canal wall down tympanomastoidectomy with lateral SCC fenestration. Five months later, she underwent the same procedure on the left side. Twenty‐three years later, at age 45, she underwent a left stapedectomy. She lived to an age of 85 years and died of metastatic cutaneous squamous cell carcinoma.
Audiograms from when she was 74 and 85 years old were reviewed (Fig. 1). The first audiogram, performed decades after her ear operations, showed a bilateral mixed severe to profound hearing loss with excellent word recognition bilaterally. The air‐bone gaps were approximately 20–30 dB bilaterally. The second audiogram, performed 11 years later, showed significant progression to bilateral profound mixed hearing loss. The bone‐conduction thresholds were reported for the better‐hearing cochlea, but could not be attributed to a particular side due to masking dilemma. Nevertheless, she appeared to have stability of her bone‐conduction thresholds, on at least one or both sides, and the significant progression in hearing loss was likely due to widening of the air‐bone gap, that is, worsening of the conductive component of her hearing loss. The drop in her word recognition scores was likely attributable to the limits of the audiometer in presentation level due to worsened conductive hearing loss rather than a decline in her sensorineural hearing.
Figure 1.
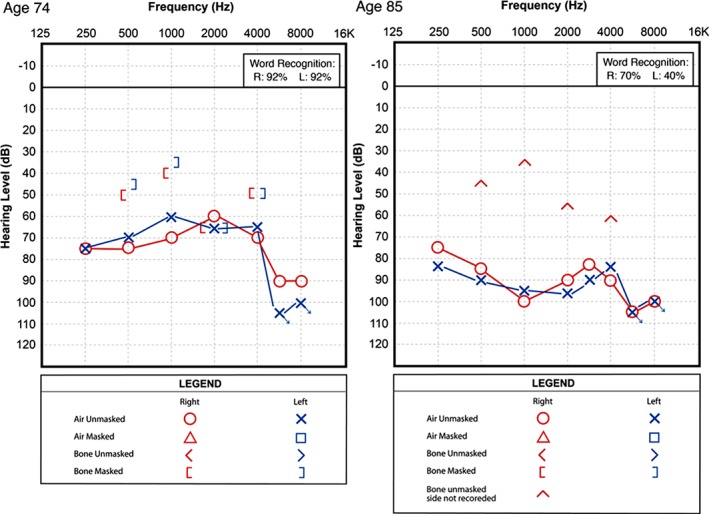
Audiograms from late in the patient's life. She previously had undergone bilateral lateral semicircular canal fenestration procedures and a left stapedectomy.
The temporal bone specimens were complete. On the right, there was some removal artifact from the saw cuts being close to the superior SCC. Otosclerosis was present causing stapes fixation (Fig. 2A). A canal wall down tympanomastoidectomy was evident with a patent lateral SCC fistula with a thick fibrous seal (Fig. 2B). Many outer and inner hair cells had degenerated, there was moderate to severe loss of spiral ganglion neurons, and there was mild to moderate loss of vestibular neurosensory elements. The round window membrane was unobstructed, meaning there was a viable window as a pressure outlet for the fluid‐filled cochlear system to enable transmission of sound pressure waves that entered through the fenestration.
Figure 2.
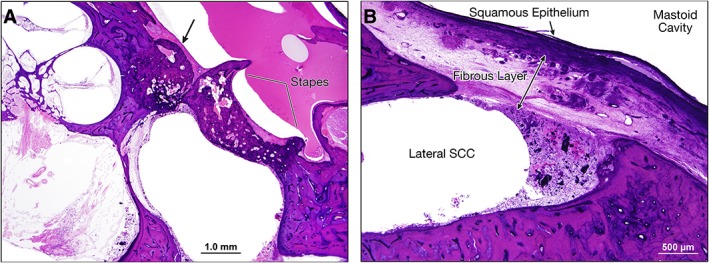
Right ear, hematoxylin and eosin (H&E) stain. (A) Scaled section showing fixation of the thickened stapes footplate with an anterior focus of otosclerosis (denoted by the arrow). Moderate to severe loss of spiral ganglion neurons is evident. (B) Section at twice the previous magnification demonstrating the lateral SCC fenestration with a thick overlying fibrous layer and squamous epithelium. The fenestration was patent, as bony regrowth had not occurred to close the window. SCC = semicircular canal.
On the left, a canal wall down tympanomastoidectomy was evident with a patent lateral SCC fistula with a thick fibrous seal (Fig. 3A). New bone growth was also present within the fibrous tissue sealing the fistula. Otosclerosis was present around the oval window. A total stapedectomy had been performed with placement of a wire loop malleus attachment prosthesis (Fig. 3B, 3C). There was some osteitis on the malleus at points in contact with the wire prosthesis (Fig. 3D). This ear also demonstrated moderate to severe loss of spiral ganglion neurons, some loss of outer hair cells, and moderate degeneration of the stria vascularis (Fig. 3E, 3F). The round window membrane was unobstructed.
Figure 3.
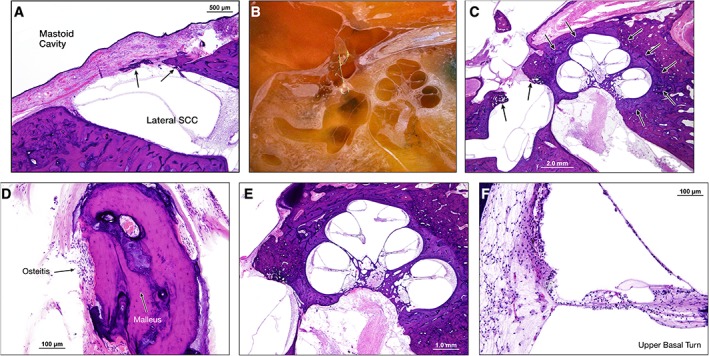
Left ear, hematoxylin and eosin (H&E) stain. (A) Similar to the right ear, there is a patent lateral SCC fenestration between mastoid cavity (left) and lateral SCC (right). A thick fibrous layer covered by squamous epithelium separates the two spaces. Some bone regrowth is evident (arrows). (B) Specimen, during sectioning and prior to staining, demonstrating previous stapedectomy with a wire loop prosthesis attached to the malleus and extending to the oval window fenestration. (C) Section showing otosclerosis (indicated by arrows) anterior and posterior to the oval window, surrounding the cochlea and anterior to the internal auditory canal. The stapes footplate is absent, suggesting the patient likely had a total stapedectomy. (D) Section of the malleus with osteitis from the wire loop prosthesis. (E) Cochlea showing degeneration of spiral ganglion neurons. (F) Section of the upper basal turn of the cochlea showing some outer hair cell loss and degeneration of the stria vascularis. SCC = semicircular canal.
DISCUSSION
This case is a temporal bone histology study of a woman who had bilateral otosclerosis and was treated with both lateral SCC fenestration procedures and a stapedectomy. She had bilateral mixed hearing loss late in life. The histology demonstrates the pathologic findings of otosclerosis, with otospongiotic changes around the oval windows and cochleae, and sensorineural hearing loss, with degeneration of the neurosensory elements. It also demonstrates the histologic results of lateral SCC fenestration and a total stapedectomy with a malleus attachment wire loop prosthesis.
The association between the patient's audiometric findings and her temporal bone histopathology is interesting. In her audiogram from when she was 74 years old, there was bilateral mixed loss with an air‐bone gap of 20–30 dB, with bilateral Carhart notches. This approximates the best possible hearing result from fenestration procedures.4 For the left ear, which also had a stapedectomy and thus three mobile windows, it is impossible to determine the relative contributions of the two procedures on the patient's conductive hearing loss. We also cannot explain the increased air‐bone gap between her audiograms at 74 and 85 years old; perhaps this was really reflective of worsened sensorineural hearing with inaccurate bone conduction measurements due to masking error or dilemma. Her sensorineural hearing loss may be due to a combination of age‐related degeneration of hair cells and spiral ganglion neural elements, surgical trauma, and otosclerosis. Pathologic findings associated with increased sensorineural hearing loss due to otosclerosis include involvement of the cochlear endosteum at multiple sites around the cochlea. Notably, the cochlear endosteal layer was not involved by otosclerosis in either ear in this case.
The acoustic mechanics of a lateral SCC fenestration have previously been described,4 and are summarized in Figure 4. Briefly, the fenestration acts as a new cochlear window that replaces the immobilized oval window. In this configuration, the driving window, that is, the fenestration, is not coupled to the tympanic membrane (TM) and ossicular chain, which reduces the effective stimulus to the new window by an amount equivalent to the middle‐ear gain of 20–30 dB. However, this loss is much less than the 50–60 dB loss that results from stapes fixation without fenestration.4 Thickening of the fibrous seal or new bone formation over the lateral SCC fenestration, as seen in this case, may account for additional conductive hearing loss.
Figure 4.
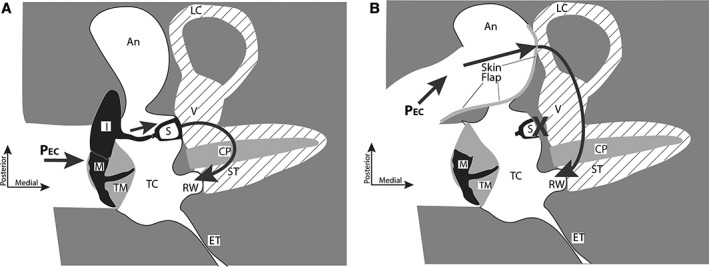
Two‐dimensional schematics of three‐dimensional views of the right middle ear from a superior view. (A) In the normal middle ear, ear‐canal sound pressure (PEC) produces ossicular motion that drives the cochlear lymphs (shaded with diagonal lines). The motion of the nearly incompressible lymphs and the cochlear partition (CP) depends on the low‐impedance of the round window (RW) that moves in the opposite direction from the stapes (S). (B) In an otosclerotic ear with fixed stapes (X), after a canal‐wall down exposure of the mastoid antrum (labeled An), removal of the incus and fenestration of the lateral canal (LC) covered by a flap of ear canal skin, sound pressure directly moves the lymphs behind the skin‐covered fenestra. This motion is again balanced by an opposite motion of the RW. Other labeled anatomical structures include: ET = eustachian tube; I = incus; M = malleus; ST = scala tympani; TC = tympanic cavity; TM = tympanic membrane; V = vestibule of the inner ear.
Acknowledgments
We are grateful to Garyfallia Pagonis, Meng Yu Zhu, Barbara Burgess, Diane Jones, and Jennifer T. O'Malley for technical assistance.
This work was presented at the Mass. Eye and Ear Otopathology Conference, Boston, MA, Oct 18, 2017.
Conflict of Interest: There are no conflicts of interest relevant to this work.
Financial Support: This work was supported by NIH grants U24DC013983 and R01DC00194.
BIBLIOGRAPHY
- 1. Ishai R, Halpin CF, Shin JJ, MJ MK, Quesnel AM. Long‐term incidence and degree of sensorineural hearing loss in otosclerosis. Otol Neurotol 2016;37(10):1489–1496. [DOI] [PubMed] [Google Scholar]
- 2. Shea JJ Jr. A personal history of stapedectomy. Am J Otol 1998;19(5 suppl):S2–S12. [PubMed] [Google Scholar]
- 3. Schuknecht HF. Pathology of the Ear. 2nd ed. New York, NY: Lea and Febiger; 1993. [Google Scholar]
- 4. Merchant SN, Ravicz ME, Voss SE, Peake WT, Rosowski JJ. Toynbee Memorial Lecture 1997. Middle ear mechanics in normal, diseased and reconstructed ears. J Laryngol Otol 1998;112(8):715–731. [DOI] [PubMed] [Google Scholar]


