Abstract
Background and objective
Stent-assisted coil embolization is a well-established treatment of intracranial wide-necked aneurysms. The Neuroform Atlas Stent System is a new generation microstent designed to enhance coil support, conformability, deliverability, and improve deployment accuracy. We present the 1-year efficacy and angiographic results of the Humanitarian Device Exemption (HDE) cohort from the Atlas Investigational Device Exemption (IDE) clinical trial.
Method
The Atlas IDE trial is a prospective, multicenter, single-arm, open-label study of unruptured wide-necked intracranial aneurysms treated with the Neuroform Atlas stent and approved coils. The primary efficacy endpoint was the rate of 12-month complete aneurysm angiographic occlusion (Raymond class I) without target aneurysm retreatment or significant parent artery stenosis (>50%) at the target location. The primary safety endpoint was the rate of major ipsilateral stroke or neurological death within 12 months. Imaging core laboratory and Clinical EventsCommittee adjudicated the primary endpoints.
Results
30 patients were enrolled at eight US centers, with 27 patients completing the 12-month angiographic follow-up. The mean age was 59.4±11.8 years and 24/30 patients (80%) were women. The mean aneurysm size was 5.3±1.7 mm and the dome:neck ratio was 1.1±0.2. Procedural technical success of Neuroform Atlas Stent deployment was 100%. 27 patients completed 12-month angiographic follow-up and 30 patients completed their 6-month follow-up. When applying the last observation carried forward method, the primary efficacy endpoint was observed in 26/30 patients (86.7%, 95% CI 69.3% to 96.2%) compared with 25/27 patients (92.6%, 95% CI 75.7% to 99.1%) who completed the 12-month angiographic follow-up. The primary safety endpoint of stroke occurred in one patient (3.3%), who made a complete clinical recovery at discharge. There were no neurological deaths.
Conclusion
The Neuroform Atlas stent in conjunction with coils demonstrated a high rate of complete aneurysm occlusion at 12-month angiographic follow-up, with an improved safety profile in the HDE cohort.
Clinical trial.gov registration number
NCT0234058; Results
Keywords: atlas stent, cerebral aneurysm, stent-assisted coiling, ATLAS, neuroform, wide-neck aneurysm
Introduction
Stent-assisted coil embolization is a well-established endovascular approach for treating wide-necked intracranial aneurysms and has expanded the proportion of patients amenable to endovascular therapy.1–5 The Neuroform Microdelivery Stent System (Stryker Neurovascular, Fremont, California, USA) was the first device approved by the Food and Drug Administration (FDA) via a Humanitarian Device Exemption (HDE) in 2002 to treat wide-necked intracranial aneurysms, and subsequent product iterations (Neuroform EZ and EZ3) were approved via HDE supplements.
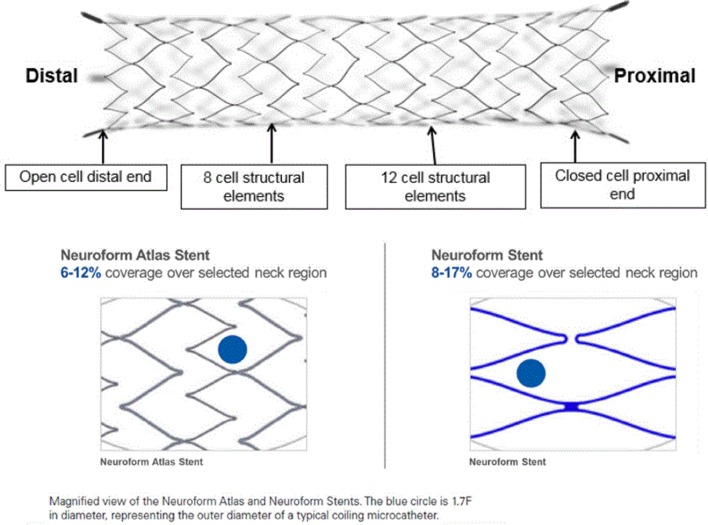
The Neuroform Atlas Stent System is a new generation Neuroform stent with design enhancements to allow for a lower profile delivery (via 0.0165 inch inner diameter microcatheter versus 0.027 inch inner diameter microcatheter), better scaffolding due to smaller cell sizes, improved trackability, and higher conformability to the vessel wall than the previous generation Neuroform microstents (figure 1).
Figure 1.
Neuroform Atlas stent design attributes.
Here we present the 1-year results for the first 30 patients enrolled in the prospective Atlas Investigational Device Exemption (IDE) study.
Method
The Atlas IDE study was a prospective multicenter, open-label, single-arm, stent-assisted wide-necked intracranial saccular aneurysm coiling study approved by the Institutional Review Board at each participating site. The national principal investigators (OOZ and BTJ) have full access to the data and statistical analysis support.
Enrollment, inclusion and exclusion criteria
Patients were considered enrolled in the study if they met all the inclusion criteria and none of the exclusion criteria and signed the informed consent form. Key inclusion criteria were: 18–80 years of age, wide-necked intracranial aneurysm (neck ≥4 mm or dome-to-neck ratio <2), parent vessel diameter of 2.0–4.5 mm, the aneurysm is intracranial (encompassing the entire posterior circulation and aneurysms at or distal to the superior hypophyseal artery in the anterior circulation). The key exclusion criteria were: multiple untreated intracranial aneurysms, acutely ruptured aneurysm within 14 days of enrollment, Hunt and Hess (H&H) scale ≥3 or modified Rankin scale (mRS) of ≥4, intracranial mass or vascular malformation, prior treatment with stent-assisted coil embolization, Moyamoya disease, underlying parent artery atherosclerosis, and/or absolute contraindication to angiography or antiplatelet therapy (online supplementary table I).
neurintsurg-2018-014455supp001.docx (14.6KB, docx)
Clinical and imaging follow-up schedule
All patients enrolled in the HDE cohort were followed up clinically through hospital discharge and at 2±1 months, 6±1 months, and 12±2 months post-procedure for the following assessments: neurological evaluation, National Institute of Health Stroke Scale (NIHSS), mRS, H&H scale as appropriate, antiplatelet regimen compliance, adverse events, and Quality of Life assessment. Digital subtraction angiography was required at 12±2 months to determine the rate of complete aneurysm occlusion.
Primary efficacy outcome
The primary study efficacy outcome was the 12-month angiographic complete aneurysm occlusion rate (defined as 100% angiographic occlusion or Raymond class I,6 7 see online supplementary figure 1) without retreatment and without parent artery stenosis (>50%) at the target location. The occlusion rate was assessed by an independent imaging core laboratory (UCSF Interventional Radiology Research Laboratory).
neurintsurg-2018-014455supp002.jpg (385.1KB, jpg)
Primary safety outcome
The primary safety endpoint was the rate of any major ipsilateral stroke or neurological death within 12 months following the procedure. Safety data were compared with a performance goal based on published rates of procedural and long-term morbidities for an aneurysm primary coiling, balloon-assisted coiling, or stent-assisted coiling. An independent Clinical Events Committee adjudicated prespecified primary endpoint events and serious device-related events.
Secondary study outcomes
The study also evaluated the following secondary endpoints: (1) technical success (defined as the proportion of patients in whom the Neuroform Atlas stent was successfully delivered and deployed at the target aneurysm neck location), (2) incidence of post-procedural major ipsilateral stroke, (3) incidence of site-reported device-related serious adverse events, (4) functional clinical outcome as defined by the mRS, (5) all-cause mortality, (6) rate of target aneurysm occlusion and recanalization, (7) target aneurysm retreatment rate, (8) stent migration at the 12-month angiogram, and (9) parent artery patency at 12 months post procedure.
Device description
The Neuroform Atlas stent is a laser cut, nitinol, self-expanding microstent. It has a unique hybrid design with closed cells proximally to facilitate microcatheter re-crossing and open cells distally to allow for better anchoring and wall apposition (figure 1). These changes from the Neuroform EZ were intended to reduce foreshortening and enhance the stent deliverability, wall apposition, and coil scaffolding (see online supplementary table II comparing the Neuroform Atlas stent with the Neuroform EZ stent).
neurintsurg-2018-014455supp003.docx (77.2KB, docx)
The stent is available in three diameter sizes (3.0, 4.0, and 4.5 mm) and four length sizes (15, 21, 24, and 30 mm) and intended for use in vessel sizes of 2–4.5 mm in diameter (see online supplementary table III). For each given diameter, the stent will expand another 0.5 mm if unconstrained. The sheath and delivery wire are used to transfer the stent into a 0.0165–0.0170 inch inner diameter Excelsior SL-10 or XT-17 microcatheter (Stryker Neurovascular, Fremont, California, USA), compared with the Neuroform EZ stent which requires a larger inner diameter (0.027 inch) microcatheter.
neurintsurg-2018-014455supp004.docx (13KB, docx)
Procedure description
Patients who were considered for treatment were pretreated with daily oral aspirin (81–325 mg) and clopidogrel (75 mg) for at least 5 days before the procedure, including the day of the procedure. A loading dose of 325 mg aspirin and 300 mg clopidogrel the day before the procedure or 650 mg aspirin and 600 mg clopidogrel administered at least 6 hours prior to the procedure was allowed. Platelet function assays were not mandatory per the protocol. Intra-procedure anticoagulation and monitoring using intravenous heparin to maintain activated clotting time between 250–300 s were recommended as per the study site standard of care.
The aneurysm neck was crossed using the Excelsior SL-10 or XT-17 microcatheter over a 0.14 inch microguidewire. The Neuroform Atlas stent was then transferred into the microcatheter via the loading sheath followed by advancement with the delivery wire to the distal end of the microcatheter. The stent was deployed across the neck of the aneurysm by stabilizing the delivery wire and withdrawing the microcatheter using a pin and pull technique.
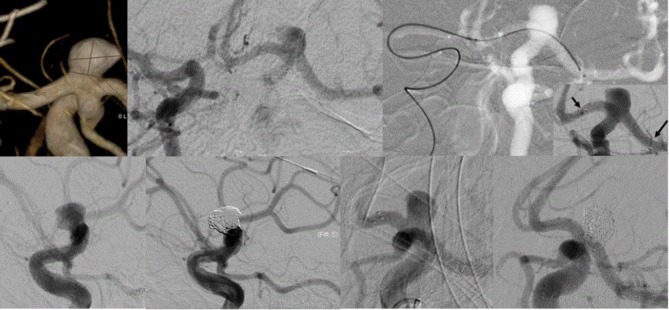
The aneurysm was coiled by either re-crossing the stent with the microcatheter or jailing a second microcatheter within the aneurysm. Baseline and post-coiling images were required. All images were transferred to the core imaging laboratory after the procedure for independent adjudication. Medical records were provided to the Clinical Events Committee if an adverse event required adjudication. Following the procedure, patients were maintained on dual antiplatelet therapy for at least 3 months and aspirin for life. Figure 2 is an example of this procedural approach.
Results
Thirty patients were enrolled between June 30, 2015 and September 24, 2015. All 30 patients completed clinical and imaging follow-up at 6 months, and 27/30 patients completed in-person 12-month clinical follow-up within or outside the study 12-month time window. Three patients who missed the in-person 12-month clinical follow-up were contacted by telephone, confirming no serious adverse event. A total of 27/30 patients completed the angiographic follow-up by February 3, 2017; 26 within the 12-month time window and one patient outside the 12-month time window. Data lock took place in March 2017. FDA approval under the HDE pathway was obtained on November 2, 2017.
All patients were successfully treated with the Atlas stent-assisted coil embolization as intended. The mean patient age was 59.4±11.8 years. Patients were predominantly female (80.0%) and white (83.3%) (table 1). Hypertension was the most common comorbidity (73.3%), followed by hyperlipidemia (56.7%). Current smokers comprised 30% of the patients. Five aneurysms had been previously treated; two by coiling and three by clipping. The target aneurysm was previously ruptured in two patients, although no patients were treated within 3 months of rupture. The mean aneurysm size (calculated as the maximum of height, width or depth) was 5.3±1.7 mm. Mean aneurysm neck width was 3.9±1.1 mm (range 1.6–7.0 mm) and 100% of patients had a dome:neck ratio <2. The majority (80.0%) of the treated aneurysms were in the anterior circulation. The anterior communicating artery was the most common aneurysm location (54.2%) in the anterior circulation, while the basilar apex (50.0%) was the most common location in the posterior circulation (table 1).
Table 1.
Baseline demographics and aneurysm characteristics
| n=30 Patients/30 Aneurysms | |
| Age (years) | |
| Mean±SD (N) | 59.4±11.8 (30) |
| Median (Q1–Q3) | 58.5 (53.0–68.0) |
| Min–Max | 31.0–79.0 |
| Height (cm) | |
| Mean±SD (N) | 164.5±9.7 (30) |
| Median (Q1–Q3) | 161.1 (157.5–167.6) |
| Min–Max | 152.4–195.6 |
| Weight (kg) | |
| Mean±SD (N) | 77.6±19.6 (30) |
| Median (Q1–Q3) | 73.5 (65.4–90.9) |
| Min–Max | 45.6–142.0 |
| Body mass index | |
| Mean±SD (N) | 28.5±5.4 (30) |
| Median (Q1–Q3) | 26.7 (25.3–31.7) |
| Min–Max | 19.6–38.4 |
| Gender, female | 80.0% (24/30) |
| Race, white | 83.3% (25/30) |
| Comorbidities | |
| Coronary artery disease | 16.7% (5/30) |
| Chronic obstructive pulmonary disorder | 23.3% (7/30) |
| Hyperlipidemia/hypercholesterolemia | 56.7% (17/30) |
| Hypertension | 73.3% (22/30) |
| Diabetes mellitus | 30.0% (9/30) |
| Current smoker | 30.0% (9/30) |
| Past smoker | 43.3% (13/30) |
| Previous transient ischemic attack | 13.3% (4/30) |
| Previous ischemic stroke | 13.3% (4/30) |
| Previous hemorrhagic stroke | 10.0% (3/30) |
| Previously ruptured target aneurysm | 6.7% (2/30) |
| History of multiple aneurysms | 16.7% (5/30) |
| Other significant medical history* | 80.0% (24/30) |
| Anterior circulation aneurysm location | 80.0% (24/30) |
| Aneurysm size (mm)† | |
| Mean±SD (N) | 5.3±1.7 (30) |
| Median (Q1–Q3) | 5.3 (4.0–6.7) |
| Min–Max | 2.5–9.0 |
| Aneurysm neck width (mm) | |
| Mean±SD (N) | 3.9±1.1 (30) |
| Median (Q1–Q3) | 4.0 (3.2–4.4) |
| Min–Max | 1.6–7.0 |
| Dome:neck ratio‡ | |
| Mean±SD (N) | 1.1±0.2 (28) |
| Median (Q1–Q3) | 1.1 (1.1–1.3) |
| Min–Max | 0.6–1.5 |
| Parent vessel diameter proximal and distal to the aneurysm neck (mm) | |
| Mean±SD (N) | 2.9±0.6 (30), 2.6±0.6 (30) |
| Median (Q1–Q3) | 2.9 (2.3–3.3), 2.4 (2.1–3.0)) |
| Min–Max | 2.0–4.4, 2.0–4.5 |
| Exact aneurysm location | |
| Anterior communicating artery | 43.3% (13/30) |
| Middle cerebral artery bifurcation | 10% (3/30) |
| ICA–ophthalmic artery | 6.7% (2/30) |
| ICA–posterior communicating artery | 3.3% (1/30) |
| ICA bifurcation/terminus | 3.3% (1/30) |
| Supraclinoid carotid artery | 10% (3/30) |
| Superior hypophyseal | 3.3% (1/30) |
| Basilar apex | 10% (3/30) |
| Basilar trunk | 3.3% (1/30) |
| Superior cerebellar artery | 3.3% (1/30) |
| Vertebrobasilar junction | 3.3% (1/30) |
*Other significant medical history included 114 reports of other findings in 24 patients. The most frequently reported findings were headaches/migraines (n=14), dizziness (n=7), neck/back pain (n=5), seizures (n=4), and gastroesophageal reflux disease (n=4). All other significant medical history findings were reported to occur in three or fewer patients.
†Aneurysm size calculated as a maximum of three dimensions (anteroposterior plane, lateral plane, height).
‡Dome size calculated as a minimum of two widths (anteroposterior plane, lateral plane).
ICA, internal carotid artery.
Procedural details and technical success
Procedural technical success was achieved in all patients. Mean procedure duration was 115.6±54.5 min (range 40–235 min). The majority of patients (90.0%) were implanted with a single stent. Three patients (10.0%) were implanted with two stents in a pre-planned manner to form a Y-stent configuration. The overall success rate of attempted stent implantation, on a per device basis, was 97.1% (33/34). One stent did not transfer from the storage sheath to the microcatheter hub and was not deployed, thus requiring a second device that deployed successfully.
Primary efficacy endpoints
When the three patients missing 12-month angiographic data were imputed using the last observation carried forward method, the overall complete occlusion rate (Raymond class I) was 86.7% (26/30) (95% CI 69.3%, 96.2%). Of these patients, 83.3% (25/30) (95% CI 65.3% to 94.4%) met the composite primary efficacy endpoint of complete occlusion with no retreatment or significant parent artery stenosis at the target location (table 2).
Table 2.
Core Laboratory angiographic and Clinical Event Committee safety primary endpoints
| Core laboratory angiographic occlusion findings | Post-procedure | 12 Months | 12 Months |
| n=30 (95% CI) | n=27 (95% CI) | n=30 (95% CI) | |
| By available angiography | Imputed by LOCF* | ||
| Raymond class | |||
| Complete 100% occlusion (Class I) | 60.0% (18/30) (40.6% to 77.3%) | 92.6% (25/27) (75.7% to 99.1%) | 86.7% (26/30) (69.3% to 96.2%) |
| With no stenosis (≤50%) | 60.0% (18/30) (40.6% to 77.3%) | 88.9% (24/27) (70.8% to 97.6%) | 83.3% (25/30) (65.3% to 94.4%) |
| Residual neck† (Class II) | 26.7% (8/30) (12.3% to 45.9%) | 0.0% (0/27) (0.0% to 12.8%) | 0.0% (0/30) (0.0% to 11.6%) |
| Residual aneurysm‡ (Class III) | 10.0% (3/30) (2.1% to 26.5%) | 7.4% (2/27) (0.9% to 24.3%) | 10.0% (3/30) (2.1% to 26.5%) |
| Not assessable | 3.3% (1/30) (0.1% to 17.2%) | 0.0% (0/27) (0.0% to 12.8%) | 3.3% (1/30) (0.1% to 17.2%) |
| Parent artery stenosis | |||
| 0–25% | 100.0% (30/30) (88.4% to 100.0%) | 96.3% (26/27) (81.0% to 99.9%) | 93.3% (28/30) (77.9% to 99.2%) |
| 26–50% | 0.0% (0/30) (0.0% to 11.6%) | 0.0% (0/27) (0.0% to 12.8%) | 3.3% (1/30) (0.1% to 17.2%) |
| 51–70% | 0.0% (0/30) (0.0% to 11.6%) | 0.0% (0/27) (0.0% to 12.8%) | 0.0% (0/30) (0.0% to 11.6%) |
| 71–99% | 0.0% (0/30) (0.0% to 11.6%) | 3.7% (1/27) (0.1% to 19.0%) | 3.3% (1/30) (0.1% to 17.2%) |
| Clinical Event Committee adjudicated safety endpoint | % Patients (n/N) | 95% CI§ |
| Any major ipsilateral stroke or neurological death | 3.3% (1/30) | 0.1% to 17.2% |
| Major ipsilateral stroke | 3.3% (1/30) | 0.1% to 17.2% |
| Neurological death/permanent disability | 0.0% (0/30) | 0.0% to 11.6% |
*LOCF, last observed carried forward.
†95–99% aneurysm occlusion.
‡<95% aneurysm occlusion.
§Clopper–Pearson exact CI.
The complete occlusion rate (Raymond class I) was 92.6% (25/27) (95% CI 75.7% to 99.1%) of patients who completed the 12-month angiographic follow-up (table 2). No patients required retreatment and one subject had >50% target location stenosis, yielding an occlusion rate without stenosis of 88.9% (95% CI 70.8% to 97.6%) in patients with available 12-month angiographic data.
Primary safety endpoints
No neurological death occurred within 12 months of follow-up. One patient (3.3% (95% CI 0.1% to 17.2%)) met the primary safety endpoint of major ipsilateral stroke (table 2). The subject developed confusion with slowing of speech and right-sided weakness a few hours after the procedure and demonstrated punctate foci of acute ischemic injury on MRI. The symptoms resolved within 48 hours. The patient was discharged home with a mRS score of 0. This was reported as a procedural stroke. The independent Clinical Event Committee (CEC) adjudicated the event as a major ipsilateral stroke that was both device- and procedure-related.
Secondary study endpoints
One subject (1/27; 3.7%) had severe stenosis (defined as 71–99%) of the parent target artery at 12 months. This subject experienced no clinical serious adverse events and all mRS and NIHSS scores were 0 throughout the 12-month follow-up period. There was no evidence of stent migration or thromboembolism in any of the 27 cases evaluated at 12 months. Apposition of the Neuroform Atlas stent to the parent artery wall was noted to be excellent in all cases by the core laboratory. Core laboratory analysis confirmed that perforators or branch arteries covered by the stent remained patent at the 12-month follow-up in all evaluable patients (25/27; 92.6% (95% CI 75.7% to 99.1%)). In one subject the branch artery/perforator was not clearly patent at 12 months, but no clinical adverse events were reported. In another subject the images were not evaluable (1/27; 3.7%). No patients in this cohort experienced a site-reported device-related serious adverse event. One subject experienced intra-procedural subarachnoid hemorrhage due to aneurysm rupture caused by coil packing, with no neurological deficit other than a headache. The patient was classified as H&H scale 2 post-procedure with mRS 1 (due to a headache) and was scored the same at all follow-up visits.
At the 12-month follow-up, NIHSS scores were obtained for 25 of the 27 patients who had clinic visits, with a mean NIHSS score of 0.2±0.4. NIHSS scores were not available for five patients due to missed visits (3/5) or missed NIHSS assessments (2/5). At the 12-month follow-up, mRS scores were available for 25 patients, all of whom had mRS scores of 0 or 1 (25/25; 100.0%). Twenty-three (23/25; 92.0%) patients had mRS scores of 0 and two patients (2/25; 8.0%) had mRS scores of 1 (one of which was due to a headache). The mRS scores were not available for two of the 27 patients who completed the 12-month visit. Of the three patients who did not complete the 12-month visit, two were contacted by the site and the telephone interview mRS assessment score was 0.
Discussion
The Neuroform Atlas Stent System demonstrated excellent efficacy and safety in treating wide-necked intracranial aneurysms. The HDE cohort showed a high rate of complete aneurysm occlusion of 86.7%, without restenosis or retreatment in 83.3% of patients, and a low risk of ipsilateral stroke with 100% of patients achieving normal or near normal neurological function (mRS 0–1) at 1-year follow-up without any neurological death.
The HDE cohort study results are comparable with previously published stent-assisted coiling data.8-12 In a 2016 meta-analysis of 14 observational studies involving 2698 mixed open and closed cell type stent-assisted coiling,1 the pooled immediate occlusion rate for stent-assisted coiling was 57.7% (range 20.2–89.2%) versus 60% (95% CI 40.6% to 77.3%) for the Atlas HDE cohort. The long-term occlusion rate was 87.6% in the meta-analysis compared with 92.6% in our study. The mortality rate was 1.4% (range 0–27.5%) compared with 0% in the current Atlas HDE cohort.
In an earlier 2014 meta-analysis of 47 studies comparing the first-generation open cell Neuroform and closed cell Enterprise stents (Cerenovus, New Brunswick, New Jersey, USA), 4238 aneurysms were treated with stent-assisted coil embolization with a mean follow-up of 14.1 months.2 The overall initial and long-term 100% complete occlusion rates were 53% and 69%, respectively, versus 60% and 92.6% in the Atlas HDE cohort, respectively. Similarly, the safety profile compares well in the Atlas HDE cohort compared with this meta-analysis (permanent morbidity and mortality were 3.9%, and 2.3%, respectively, versus 3.3% and 0% (95% CI 0% to 11.6%), respectively, in the Atlas HDE cohort).
The results of the Atlas HDE cohort compare favorably with those of the braided design aneurysmal microstent study. For example, a recent LVIS stent (MicroVention, Aliso Viejo, California, USA) HDE study of 31 patients reported a technical success rate of 93.1% with ≥90% occlusion rate of 92.9% and complete occlusion rate of 75% at 6 months angiography, with 0% morbidity and mortality.8 Another 30 patient multicenter retrospective study using the braided LVIS Jr microstent demonstrated 3.3% morbidity rate with no mortality and complete occlusion rate of 76% (21/25) Raymond class I on a mean follow-up of 5.2 months, with one patient reporting permanent complications (3.3%).9 The Canadian LVIS Jr multicenter registry of 102 patients demonstrated a complete long-term occlusion rate (defined as Raymond class I) of 68%, with 3% permanent neurological deficits, and 1% overall mortality rate.10
A recently published result of a retrospective Neuroform Atlas stent-assisted coil embolization single-center experience which examined 48 patients with 55 aneurysms was consistent with our HDE cohort findings.11 In their study the microstent was deployed via different 0.0165–0.017 inch microcatheters and the Eclipse-2 balloon (Balt, France), which resulted in 100% technical success rate with an 83.7% complete occlusion rate at mean follow-up of 8.7 months. The safety profile demonstrated one minor stroke in one patient (1/48; 2%) and no neurological death (0%).11
In summary, the newly designed Neuroform Atlas stent provides potential advantages over Neuroform EZ and LVIS stents (see online supplementary tables II and III). First, its compatibility with a 0.165 inch inner diameter microcatheter across all Atlas stent diameter and length sizes makes it practical in all aneurysm locations. Second, its higher number of connecter and alternating cell numbers from 8 to 12 provides better scaffolding and coil stability within the aneurysm lumen. Third, the accuracy of deployment is very high with less foreshortening than braided stents. Fourth, the conformability around acute angles is an advantage of the open cell design with alternating cell size design. However, the lack of re-sheathability remains a challenge to the open design nitinol stents.
Study limitations
Despite the independent core laboratory, Clinical Event Committee, and prospective study design, this is still a small sample size study. In addition, most of the aneurysms in the current cohort are small in size, with an interquartile median size ranging between 4 and 6.7 mm. The smaller aneurysms are less likely to recur and potentially have a higher chance of progressive occlusion over time. A further limitation is the lack of data on how the decision to treat these small aneurysms is made. One assumption is that it might be related to the evolution of the field and clinical practice pattern of treating smaller aneurysms due to enhanced safety and efficacy profiles of endovascular therapy over time. However, this is also likely to be related to a multifactorial complex decision-making process to proceed with aneurysm treatment. This might be related, in part, to aneurysm size, shape, location, risk factors known to increase future risk of aneurysm rupture, and patient anxiety.
Conclusion
Neuroform Atlas stent-assisted coil embolization was associated with high 1-year complete occlusion rates and favorable safety profiles in patients with wide-necked aneurysms. Particularly encouraging was the increase in Raymond I occlusion rates from 60% immediately post-procedure to 86.7% at 1 year.12 Another important observation from the current study is the fact that the majority of the aneurysm (three-quarters) are less than 7 mm in size, reflective of the changing practice of treating smaller size aneurysms with stent-assisted coiling.
Figure 2.
A middle-aged patient with 9 mm internal carotid artery-terminus aneurysm with contralateral access via SL-10 microcatheter, avoiding Y-stent, and demonstrating the trackability of the Neuroform Atlas stent (upper row), with complete occlusion at 12 months follow-up (lower row).
Footnotes
BTJ and OOZ contributed equally.
Contributors: All authors contributed to the final draft with revisions, edits, and contents and also participated in enrolling subjects.
Funding: This work was sponsored by Stryker Neurovascular, Fremont, California, USA.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Phan K, Huo YR, Jia F, et al. . Meta-analysis of stent-assisted coiling versus coiling-only for the treatment of intracranial aneurysms. J Clin Neurosci 2016;31:15–22. 10.1016/j.jocn.2016.01.035 [DOI] [PubMed] [Google Scholar]
- 2. King B, Vaziri S, Singla A, et al. . Clinical and angiographic outcomes after stent-assisted coiling of cerebral aneurysms with Enterprise and Neuroform stents: a comparative analysis of the literature. J Neurointerv Surg 2015;7:905–9. 10.1136/neurintsurg-2014-011457 [DOI] [PubMed] [Google Scholar]
- 3. Chalouhi N, Jabbour P, Singhal S, et al. . Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke 2013;44:1348–53. 10.1161/STROKEAHA.111.000641 [DOI] [PubMed] [Google Scholar]
- 4. Kabbasch C, Liebig T, Faymonville A, et al. . Initial clinical experience with a new self-expanding nitinol microstent for the treatment of wide-neck intracranial cerebral aneurysms: the Acandis Acclino Stent. J Vasc Interv Neurol 2015;8:1–6. [PMC free article] [PubMed] [Google Scholar]
- 5. Food and Drug Administration. H020002 - Summary of Safety and Probable Benefit. Neuroform Microdelivery Stent System. 2002. http://www.accessdata.fda.gov/cdrh_docs/pdf2/H020002B.pdf
- 6. Raymond J, Guilbert F, Weill A, et al. . Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003;34:1398–403. 10.1161/01.STR.0000073841.88563.E9 [DOI] [PubMed] [Google Scholar]
- 7. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke 2001;32:1998–2004. 10.1161/hs0901.095600 [DOI] [PubMed] [Google Scholar]
- 8. Fiorella D, Arthur A, Boulos A, et al. . Final results of the US humanitarian device exemption study of the low-profile visualized intraluminal support (LVIS) device. J Neurointerv Surg 2016;8:894–7. 10.1136/neurintsurg-2015-011937 [DOI] [PubMed] [Google Scholar]
- 9. Samaniego EA, Mendez AA, Nguyen TN, et al. . LVIS Jr device for Y-stent-assisted coil embolization of wide-neck intracranial aneurysms: a multicenter experience. Interv Neurol 2018;7:271–83. 10.1159/000487545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shankar JJS, Quateen A, Weill A, et al. . Canadian Registry of LVIS Jr for Treatment of Intracranial Aneurysms (CaRLA). J Neurointerv Surg 2017;9:849–53. 10.1136/neurintsurg-2016-012611 [DOI] [PubMed] [Google Scholar]
- 11. Cay F, Peker A, Arat A. Stent-assisted coiling of cerebral aneurysms with the Neuroform Atlas stent. Interv Neuroradiol 2018;24:263–9. 10.1177/1591019917753710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hetts SW, Turk A, English JD, et al. . Stent-assisted coiling versus coiling alone in unruptured intracranial aneurysms in the matrix and platinum science trial: safety, efficacy, and mid-term outcomes. AJNR Am J Neuroradiol 2014;35:698–705. 10.3174/ajnr.A3755 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2018-014455supp001.docx (14.6KB, docx)
neurintsurg-2018-014455supp002.jpg (385.1KB, jpg)
neurintsurg-2018-014455supp003.docx (77.2KB, docx)
neurintsurg-2018-014455supp004.docx (13KB, docx)