Abstract
Objectives
To demonstrate that an in‐office superior laryngeal nerve (SLN) block with lidocaine and steroids is an effective alternative to neuromodulators for patients with neurogenic cough.
Study Design
Retrospective study.
Methods
A retrospective review of 10 patients who underwent in office nerve block to the laryngeal nerve (SLN) for neurogenic cough. Demographic data and pre‐ and postcough survey index are the measure outcomes. Follow‐up was 3–6 months.
Results
We find that all patients in this study that underwent an SLN block showed significant improvement in cough severity index (CSI). The average number of blocks was 2.3. The mean follow‐up time from the first SLN block is 3.4 months. The mean CSI improvement 16.30. 95% confidence interval, 11.44–21.16; P < .0001. All patients in this study completed at least one session of cough suppression therapy with speech language pathology (SLP). No patients were on neuromodulators at the time of the SLN block.
Conclusions
There is a role for in‐office SLN block with lidocaine and steroids for patients with neurogenic cough, and can be an effective alternative to neuromodulators.
Level of Evidence
NA
Keywords: Neurogenic cough, superior laryngeal nerve block, cough survey index
INTRODUCTION
Neurogenic cough has been widely studied as a diagnosis of exclusion in patients with chronic cough symptoms. Neurogenic cough is defined as a chronic cough (more than 8 weeks duration) and a diagnosis entertained based on a strong history, absence of positive objective testing and findings, and based on the clinician's experience.1 The common causes of chronic cough are within the upper airway cough syndrome and include a variety of rhinosinus conditions, asthma, gastroesophageal reflux disease, and nonasthmatic eosinophilic bronchitis.2 Neurogenic cough can be a part of a larger symptom complex, or when a solo diagnosis, is believed to arise from a sensory neuropathy, with laryngeal hypersensitivity from the superior laryngeal nerve (SLN).3 The mechanism of this sensory neuropathy is believed to be viral‐induced injury to the SLN.1 The internal branch of the SLN is the sensory innervation of the larynx above the vocal folds, and it enters the thyrohyoid membrane just above the superior laryngeal artery. Patients with a sensory neuropathy or neurogenic cough typically cough with activities that involved laryngeal function such as talking, laughing, positional changes, and external manipulation of the neck.4 Laryngeal examination is the recommended clinical evaluation.1 The possibility of a coexisting vocal fold paresis on videostroboscopy might mean that the motor branch of the recurrent laryngeal nerve is also involved.5
The treatments for neurogenic cough include behavioral and medical management. Respiratory retraining therapy done teaches cough suppression strategies and techniques to help patients break the vicious cycle of cough, in the hopes that feedback loop suppresses the hypersensitivity reflex.6, 7 Respiratory retraining therapy is performed by experienced and well‐trained speech language pathology (SLP). Medical management in the form of neuromodulators is the other arm for therapy, with multiple medications shown to be beneficial including amitriptyline and c‐aminobutyric acid (GABA) analogs (gabapentin and pregabalin), including opiates.4, 8 These medications involve some form of titration regimen; all of the medications have their individual side effect profiles. Patient compliance and willingness to trial neuromodulators, as well as the cost of medications, makes medical management less than ideal.
In general, therapeutic nerve blocks of peripheral nerves have been found to be effective, and in the pain management and anesthesia literature, SLN blocks with steroids and lidocaine have been described to effectively anesthetize the larynx for airway manipulation and pain control.9 Simpson et al published the first preliminary study for SLN blockade with lidocaine:steroids in patients with neurogenic cough.10 However, the existence of other papers demonstrating the feasibility and efficacy of this in office procedure with the established technique as described by Simpson et al is surprisingly absent. This article aims to elaborate on the effectiveness of SLN block for chronic neurogenic cough patients by using cough severity index (CSI) scores, and in our study, demonstrate this technique as an alternative to neuromodulator therapy. Our data support that hypothesis that SLN block is a comparable and safe alternative to treating neurogenic cough patients with promising results.
METHODS
Under an institutional review board‐approved protocol, the medical records of all adult patients seen in the clinic from 2017 to 2019 who underwent SLN block were reviewed. Patients were identified by chronic cough ICD‐10 code (R05) and Current Procedural Terminology code for vagal nerve block (64408). All patients in this study had a complete review of their medical record. Pre‐ and post‐treatment cough survey index questionnaire scores were recorded for each patient. Patients were excluded if they had incomplete medical information, had any additional comorbidities that may account for cough, or had a prior history or were currently on neuromodulators. Patients who had undergone respiratory retraining therapy with SLP before the study were not excluded. All patients met with the providing laryngologist (VKD) and SLP team in a multidisciplinary fashion on the first consultation, and all treatment options were discussed (ie, respiratory retraining therapy, neuromodulators, and SLN block).
The SLN block was done in office, according to the technique described by Simpson et al.10 Two milliliters or a 50:50 solution of triamcinolone acetonide 200 mg/5 mL and 1% lidocaine with 1:100,000 epinephrine was injected into the internal branch of the SLN at the thyrohyoid membrane. All patients underwent a single SLN block at one visit. The laterality of the block was decided upon by palpating a point along the thyrohyoid space that would trigger a cough. Injections were directed to the trigger point in this study. In patients who found no improvement in cough symptoms, a contralateral SLN block was performed 2–3 weeks later, independent of any palpable trigger point to the opposite side. No concurrent bilateral SLN blocks were performed. SLN blocks were repeated in patients at 2‐week intervals, who had transient improvement in cough with no relief.
Medical chart review included patient demographics, previous cough work up, indications for SLN block procedure, and CSI scores before and after the final treatment.11 The number of SLN blocks and injectable substances were recorded as well. Statistical analysis was done with parametric values analyzed using the paired Student's t test.
RESULTS
A total of 10 patients underwent SLN block for treatment of neurogenic cough between 2017 and 2019. All 10 patients were included in the analysis. Table 1 displays demographics, number of SLN blocks, laterality of SLN block, number of respiratory retraining therapy sessions with our SLP team, and pre‐ and post‐treatment CSI scores, as well as length of follow‐up for each patient. All patients were diagnosed with neurogenic cough based upon previous workup by gastroenterology, pulmonology, allergy, and review of medication lists. The mean age of the patient population was 54 (range: 34–71), with three males and seven females. The mean duration of cough prior to initial SLN block was 10 years (range: 1.5–20 years). Only one patient had a relatively short duration of cough symptoms (1.5 years). All patients were evaluated by gastroenterology, pulmonology, and allergy as well as had a complete review of their medication list, with all being treated for all three contributors for cough: asthma, gastroesophageal reflux disease, or allergy. Empiric treatment included steroid inhalers, proton pump inhibitors, antihistamines, and nasal steroids for at minimum, 4–6 week trials. All patients had a negative chest x‐ray within the past year. All patients were not previously or currently on neuromodulators for cough treatment. All patients underwent at least one session of respiratory retraining therapy with our SLP team, with seven undergoing multiple sessions. The mean number of SLP sessions prior to SLN block was 2.4 sessions.
Table 1.
Demographics of Patients Who Underwent SLN Block.
| Patient | Age | Sex | Duration of Cough (yr) | SLP Treatments (n) | Number of SLN Blocks | Laterality of Initial Block | Pre‐CSI | Post‐CSI | Follow‐Up Time (mo) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 71 | F | 20 | Yes (4) | 3 | Left | 38 | 20 | 6 |
| 2 | 46 | F | 10 | Yes (6) | 3 | Left | 10 | 9 | 4 |
| 3 | 50 | F | 10 | Yes (2) | 2 | Right | 36 | 11 | 3 |
| 4 | 58 | M | 1.5 | Yes (1) | 2 | Left | 35 | 13 | 2 |
| 5 | 34 | M | 7 | Yes (2) | 2 | Left | 22 | 1 | 2 |
| 6 | 66 | F | 18 | Yes (3) | 2 | Right | 27 | 13 | 2.5 |
| 7 | 63 | F | 15 | Yes (1) | 3 | Right | 25 | 11 | 5 |
| 8 | 64 | F | 4 | Yes (2) | 2 | Right | 30 | 9 | 2 |
| 9 | 41 | M | 15 | Yes (2) | 2 | Left | 23 | 10 | 5 |
| 10 | 46 | F | 5 | Yes (1) | 2 | Left | 21 | 7 | 3 |
CSI = cough severity index; SLN = superior laryngeal nerve; SLP = speech language pathology.
All patients (100%) reported improvement in their cough with the SLN block. All patients underwent at least two SLN blocks total, one to each SLN, within 2 weeks apart. The decision on laterality of the initial SLN block was determined by palpation of the thyrohyoid space bilaterally. When palpation of one side induced either a trigger to cough or cough itself, that side was used as the initial side for injection. Four patients had right‐sided SLN blocks, and six patients had left‐sided SLN blocks, as the initial block. Patients who had no improvement in their cough symptoms returned for a block to the contralateral SLN from the initial block, approximately 2–3 weeks later. Most patients reported improvement in their cough within 1–2 weeks after the procedure. Overall, patients underwent an average of 2.3 SLN block procedures.2, 3 The mean interval between blocks was 14–15 days. The mean follow‐up time was 3.4 months (range: 2–6 months).
CSI scores were obtained for all patients at initial presentation and at the most recent follow‐up visit, after the final SLN block. There was a statistically significant decrease in CSI scores after treatment, with a mean CSI improvement of 16.30. 95% confidence interval, 11.44–21.16; P < .0001 (Fig. 1).
Figure 1.
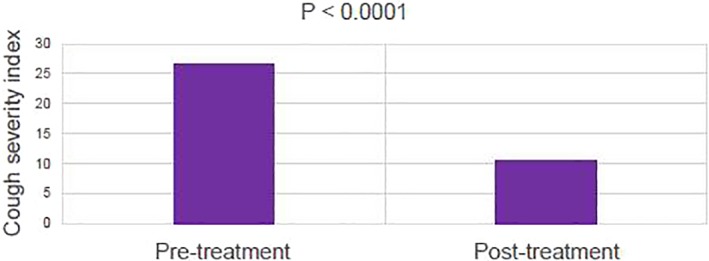
Pre‐ and post‐treatment mean cough severity index scores for patients who underwent superior laryngeal nerve block for treatment of chronic cough.
There was no complication associated with any of the patients in this study. Two patients noted transient laryngeal anesthesia within the first 24 hours which was described by these patients as “numbness” or “tingling” that did not interfere with phonation or swallowing. There were no complications as it related to laryngospasm, dysphagia, dysphonia, or aspiration. There was no swelling or pain in the location of injection as reported by each patient.
DISCUSSION
Cough is the fifth most common complaint that brings patients to primary care and otolaryngology offices a year.1 Those with neurogenic cough are debilitated by the chronicity of their cough, as well as the failure of empiric therapies for causes that are organic in origin. In turn, there is increased desperation and frustration on the part of patients and providers who treat neurogenic cough, in an effort to improve quality of life. Patients who are diagnosed with neurogenic cough are given the option for pharmacologic treatment in the form of neuromodulators and nonpharmacologic treatment in the form of behavioral therapy with respiratory retraining. While beneficial, neuromodulators are not effective universally for all patients with neurogenic cough. The common complaints include side effect profile, difficulty complying with titration protocols, and cost. SLN blocks, which have been described in other fields as a form of anesthesia or pain control, may be an alternative to medical management of cough. This study reproduces results similar to Simpson et al, the only other paper describing the use of this technique for neurogenic cough,10 and affirms the potential for SLN blocks to be an equal and alternative treatment to neuromodulators. Data from our study demonstrate a success rate in all patients who received the SLN block in office, with a statistically significant improvement in CSI scores. Furthermore, there were no complications from the procedure. Our study is different from Simpson et al in that no patients were concurrently treated with neuromodulators during the SLN block. Among our 10 patients, all were compliant in returning within 2 weeks for the contralateral SLN block and follow‐up. All patients required more than one SLN block, which may be inherent to the study cohort. Overall, all patients found relief in their cough symptoms after an average of 2.4 blocks.
The advantages and disadvantages of SLN block have been described previously.10 Overall, it is a low‐cost procedure with most materials available in clinic. It is relatively noninvasive, not requiring preprocedure anesthesia, and can be performed by a single provider. In our study, all 10 patients were given informed options for all treatments available, and voluntarily chose SLN block after an initial SLP consultation. No patient expressed the desire to change to another treatment option during the course of the SLN block. Furthermore, all patients tolerated the procedure well without complications. SLN block avoids the side effect of neuromodulators and therefore is a reasonably sought out alternative for patients. Disadvantages of the SLN block include need for repeatable injections. This was not a complaint made by this patient cohort. The most serious complication, embolization of particulate steroids into the arterial circulation, did not occur in this study. However, it is important to emphasize how to prevent this technically, by drawing back on the syringe and aspirating prior to injection.
Other procedural treatments for neurogenic cough have been described, including Botox to the laryngeal musculature and injection augmentation.12, 13 In those with glottic insufficiency, injection augmentation is felt to reduce laryngeal trauma and by feedback, reduce cough symptoms.14
Our study is retrospective and has its inherent limitations. Our study cohort had a cough for an average of 10 years, which is relatively more chronic than Simpson et al. Patient recollection of symptoms, duration of cough, and improvement in cough over the course of nerve block treatment were not standardized. Small sample size is a limiting factor as well. Future investigations aim to look at a larger sample size, as well as attempt to characterize cough and changes in cough symptoms over the course of this therapy. Ultimately, the efficacy of the nerve block agents should be evaluated against placebo in a randomized prospective study.
CONCLUSIONS
In conclusion, our study affirms the efficacy and feasibility of SLN block for neurogenic cough patients. For our patients who underwent SLN block, their cough improved. SLN block is also a treatment option patients chose over other treatment modalities. SLN block is a feasible and safe alternative for patients who may not want to undergo pharmacologic treatment for their cough. The risk profile is low and the benefits are significant. More studies are need to describe the results of this potential treatment for patients with cough. Further studies are required to determine longitudinal outcomes, as well as efficacy of the procedure when directly compared to placebo and neuromodulators for neurogenic cough.
There are no financial disclosure or conflicts of interest by the author
Oral presentation at Triological Society, Combined Meeting of Otolaryngologists, Austin, Texas, USA on May 4, 2019.
BIBLIOGRAPHY
- 1. Altman KW, Noordzij JP, Rosen CA, Cohen S, Sulica L. Neurogenic cough. Laryngoscope 2015;125:1675–1681. [DOI] [PubMed] [Google Scholar]
- 2. Irwin RS, French CL, Chang A, et al. Classification of cough as a symptom in adults and management algorithms. Chest 2018;153(1):196–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee B, Woo P. Chronic cough as a sign of laryngeal sensory neuropathy: diagnosis and treatment. Ann Otol Rhinol Laryngol 2005;114:253–257. [DOI] [PubMed] [Google Scholar]
- 4. Bastian RW, Vaidya AM, Delsupehe KG. Sensory neuropathic cough: a common and treatable cause of chronic cough. Otolaryngol Head Neck Surg 2006;135:17–21. [DOI] [PubMed] [Google Scholar]
- 5. Sulica L. The superior laryngeal nerve: function and dysfunction. Otolaryngol Clin North Am 2004;37:183–201. [DOI] [PubMed] [Google Scholar]
- 6. Vertigan AE, Theodoros DG, Gibson PG, Winkworth AL. Efficacy of speech pathology management for chronic cough: a randomized placebo controlled trial of treatment efficacy. Thorax 2006;61:1065–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ryan NM, Vertigan AE, Bone S, Gibson PG. Cough reflex sensitivity improves with speech language pathology management of refractory chronic cough. Cough 2010;6:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nalamachu S, Morley‐Forster P. Diagnosing and managing postherpetic neuralgia. Drugs Aging 2012;29:863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Doyle DJ. Airway anesthesia: theory and practice. Anesthesiol Clin 2015;33(2):291–304. [DOI] [PubMed] [Google Scholar]
- 10. Simpson CB, Tibbetts KM, Loochtan MJ, Dominguez LM. Treatment of chronic neurogenic cough with in‐office superior laryngeal nerve block. Laryngoscope 2018;128:1898–1903. [DOI] [PubMed] [Google Scholar]
- 11. Shembel AC, Rosen CA, Zullo TG, Gartner‐Schmidt JL. Development and validation of the cough severity index: a severity index for chronic cough related to the upper airway. Laryngoscope 2013;123(8):1931–1936. [DOI] [PubMed] [Google Scholar]
- 12. Sasieta HC, Iyer VN, Orbelo DM, et al. Bilateral thyroarytenoid botulinum toxin type A injection for the treatment of refractory chronic cough. JAMA Otolaryngol Head Neck Surg 2016;142:881–888. [DOI] [PubMed] [Google Scholar]
- 13. Crawley BK, Murry T, Sulica L. Injection augmentation for chronic cough. J Voice 2015;29:763–767. [DOI] [PubMed] [Google Scholar]
- 14. Litts JK, Fink DS, Clary MS. The effect of vocal fold augmentation on cough symptoms in the presence of glottic insufficiency. Laryngoscope 2018. Jun;128(6):1316–1319. [DOI] [PubMed] [Google Scholar]


