Abstract
Background
In some low‐ and middle‐income countries, separate vertical programmes deliver specific life‐saving interventions but can fragment services. Strategies to integrate services aim to bring together inputs, organisation, and delivery of particular functions to increase efficiency and people's access. We examined the evidence on the effectiveness of integration strategies at the point of delivery (sometimes termed 'linkages'), including integrated delivery of tuberculosis (TB), HIV/AIDS and reproductive health programmes.
Objectives
To assess the effects of strategies to integrate primary health care services on healthcare delivery and health status in low‐ and middle‐income countries.
Search methods
We searched The Cochrane Central Register of Controlled Trials (CENTRAL) 2010, Issue 3, part of the The Cochrane Library.www.thecochranelibrary.com, including the Cochrane Effective Practice and Organisation of Care Group Specialised Register (searched 15 September 2010); MEDLINE, Ovid (1950 to August Week 5 2010) (searched 10 September 2010); EMBASE, Ovid (1980 to 2010 Week 35) (searched 10 September 2010); CINAHL, EBSCO (1980 to present) (searched 20 September 2010); Sociological Abstracts, CSA Illumina (1952 to current) (searched 10 September 2010); Social Services Abstracts, CSA Illumina (1979 to current) (searched 10 September 2010); POPLINE (1970 to current) (searched 10 September 2010); International Bibliography of the Social Sciences, Webspirs (1951 to current) (searched 01 July 2008); HealthStar (1975 to September 2005), Cab Health (1972 to 1999), and reference lists of articles. We also searched the World Health Organization (WHOLIS) library database, handsearched relevant WHO publications, and contacted experts in the field.
Selection criteria
Randomised controlled trials, non‐randomised controlled trials, controlled before and after studies, and interrupted time series analyses of integration strategies, including strengthening linkages, in primary health care services. Health services in high‐income countries, private public partnerships, and hospital inpatient care were excluded as were programmes promoting the integrated management of childhood illnesses. The main outcomes were indicators of healthcare delivery, user views, and health status.
Data collection and analysis
Two authors independently extracted data and assessed the risk of bias. The statistical results of individual studies are reported and summarised.
Main results
Five randomised trials and four controlled before and after studies were included. The interventions were complex.
Five studies added an additional component, or linked a new component, to an existing service, for example, adding family planning or HIV counselling and testing to routine services. The evidence from these studies indicated that adding on services probably increases service utilisation but probably does not improve health status outcomes, such as incident pregnancies.
Four studies compared integrated services to single, special services. Based on the included studies, fully integrating sexually transmitted infection (STI) and family planning, and maternal and child health services into routine care as opposed to delivering them as special 'vertical' services may decrease utilisation, client knowledge of and satisfaction with the services and may not result in any difference in health outcomes, such as child survival. Integrating HIV prevention and control at facility and community level improved the effectiveness of certain services (STI treatment in males) but resulted in no difference in health seeking behaviour, STI incidence, or HIV incidence in the population.
Authors' conclusions
There is some evidence that 'adding on' services (or linkages) may improve the utilisation and outputs of healthcare delivery. However, there is no evidence to date that a fuller form of integration improves healthcare delivery or health status. Available evidence suggests that full integration probably decreases the knowledge and utilisation of specific services and may not result in any improvements in health status. More rigorous studies of different strategies to promote integration over a wider range of services and settings are needed. These studies should include economic evaluation and the views of clients as clients' views will influence the uptake of integration strategies at the point of delivery and the effectiveness on community health of these strategies.
Plain language summary
Integrating healthcare services in low‐ and middle‐income countries
In some low‐ and middle‐income countries, healthcare services are organised around a specific health problem. This can cause fragmentation as people are required to visit separate clinics depending on their health problem or need. The logic is that specialist clinics lead to better care and health outcomes because skilled healthcare providers then provide the specialised services and technologies related to the healthcare need. On the other hand, separating out services for specific diseases can be inefficient for both the provider, with service duplication, and the patient who has to visit different services for their health care. For example, a mother has to go to one clinic for family planning services and another for her children to be vaccinated, or a person with HIV and TB has to go to separate clinics for each disease.
One solution is to integrate healthcare services at the point of delivery or to strengthen the linkages between the services. The purpose of integration is to improve co‐ordination and service delivery by providing services together, for example services for mothers and their children in one centre. It is believed that integration ensures that services are managed and delivered together, for an efficient and high quality service. It is also believed that integration of care leads to greater public access, including more equitable access for people from different communities and socio‐economic backgrounds, a more convenient and satisfying service, and better health overall. Others believe that, with integration of care, healthcare professionals might become overloaded or not have the specialised skills to manage specific diseases, which could lead to poor quality services and poor health.
This updated review included nine studies that evaluated integrated care or linkages in care. The studies made two types of comparison.
1) Integration of care, by adding a service to an existing service (tuberculosis (TB) or sexually transmitted infection (STI) patients were offered HIV testing and counselling; mothers attending an immunisation clinic were encouraged to have family planning services).
2) Integrated services versus single, special services (family planning, maternal and child health delivered as a special vertical programme or integrated into routine healthcare delivery).
There was some evidence from the included studies that adding on services or creating linkages to an existing service improved its use and delivery of health care but little or no evidence that fuller integration of primary healthcare services improved people's health status in low‐ or middle‐income countries. People should be aware that integration may not improve service delivery or health status.If policy makers and planners consider integrating healthcare services they should monitor and evaluate them using good study designs.
A summary of this review for policy‐makers is availablehere
Summary of findings
Background
Description of the condition
Horizontal and vertical systems
Health care, even at the first contact level, is complicated. The outputs are diverse, tailored to specific health needs, and dependent on the inputs of different groups of providers, some of whom are specialised in managing certain groups of diseases or patients. Thus a quality health service in part depends on components of the service being 'specialised'. In first contact care in low‐ and middle‐income countries this plays out in its most extreme form as series of 'vertical' programmes with resources, staff and activities contained within each silo, such as in family planning, malaria control, tuberculosis control, HIV prevention and treatment, and delivery of vaccines to prevent common childhood illnesses. There are advantages to this approach in countries where the publicly funded healthcare system is relatively weak as specialised, vertical programmes allow for central technical supervision, dedicated resources, and direct monitoring and evaluation to ensure performance. This approach is therefore thought to assure delivery of services.
On the other hand vertical systems of delivery have disadvantages. They can be extremely inefficient, with service duplication and fragmentation. The public are confronted with an array of different publicly funded activities occurring at different times and in different ways. Health managers may also find it difficult to work effectively as communication is poor between the groups; and training, supervision, drug supplies, and reporting systems are duplicated. In addition, where the imperative to deliver is very strong among external donors who fund programmes, the programmes may employ people with better conditions of service than in government services. This drains skilled and scarce human resources from the routine services. The desire by governments to meet donors' performance requirements for their programmes may also result in the prioritisation of these programmes and cause shifts in management and other support that favours vertical programmes and adversely affects the routine services.
Since the 1960s, debates about the comparative advantages and disadvantages of horizontal and vertical system approaches have often been polarised by the philosophical beliefs of proponents in each camp (Walsh 1979; Mills 1983; Wisner 1988). The debates have endured to this day, with the belief among some that integration of services is important to improve the efficiency of the health system and the quality of health care for the public.
The strategy of integration of primary health care (PHC) has received renewed attention in recent years (Frenk 2009). An emerging school of thought is that the delivery of vertical programmes and the provision of comprehensive healthcare services are not mutually exclusive. Rather they are complementary approaches within a continuum of care in complex healthcare delivery environments which require effective planning, co‐ordination and management (Unger 2003; WHO 2005; Kerber 2007).
Bundles of cost‐effective strategies
'Integration' is used in slightly different ways by various authors. With the advent of evidence‐informed approaches, better assessment and quantification of the various ingredients of first contact care have become available. For example, Bhutta and colleagues identified 37 key interventions and strategies from systematic reviews for the delivery of maternal, child and newborn health and survival interventions through primary care (Bhutta 2008). In this context integration is used to describe how to deliver a bundle of cost‐effective strategies (in child health or maternal health, for example) through the existing primary healthcare system (Ekman 2008). Nevertheless, this still conforms to a model of integration as a way of delivering a series of targeted technologies and interventions together that sometimes have been delivered as a series of 'vertical' programmes (in malaria, tuberculosis or the extended immunisation of childhood illnesses, for example). This is similar to the delivery of the Integrated Management of Childhood Illness (IMCI) strategy, which may be delivered as a fully integrated part of routine PHC or in some settings as a 'vertical' programme (WHO 1997). Another example is neglected tropical disease programmes in which integration is seen as these programmes working together with the much larger programmes of malaria control and HIV (Gyapong 2010).
Linkages between programmes
A further level of complexity has been added with the renewed popularity of the term 'linkages'. This term was used originally to describe the lowest level of integration. It preceded ‘co‐ordination’ and ‘full integration’, which were seen as more advanced forms of integration of health and social services (Leutz 1999). Linkages were based on sharing of information on request and efficient referral systems between different service providers. Co‐ordination is a more structured form of integration than linkage that includes features such as the use of a common information system, dedicated staff to improve links between different service providers (discharge planners, for example) but still operates largely through separate structures. 'Full integration' creates new services where resources from multiple systems are pooled. In the reproductive health field, terms such as 'linkages' are being used increasingly to describe and advocate for the integration of services.
A recently published policy brief from WHO and other multilateral donors advocates linkages in sexual and reproductive health (WHO/HIV/2008, WHO 2009).
This policy document is based on a systematic review, which as of June 2011 was unavailable. The policy brief concludes that the evidence from the systematic review shows that linkages lead to a reduction in HIV‐related stigma and discrimination and a better understanding and protection of individuals' rights. A 2010 publication, based on a subset of the papers included in the policy brief, more generally advocates for linkages, and concludes that existing evidence provides support for linkages. It further states that although significant gaps in the literature remain, policy makers, programme managers, and researchers should continue to advocate for, support, implement and rigorously evaluate sexual and reproductive health and HIV linkages (Kennedy 2010).
Description of the intervention
To illustrate the variety of settings and services in which integration is used in relation to health in low‐ and middle‐income countries, and to help us reach a working definition, we searched MEDLINE and Popline using general search terms such as 'integration', ‘linkages’ and 'health care delivery'. We contacted WHO and studied existing reviews to identify a variety of studies, case studies and descriptive reports describing integration at the primary healthcare level. A fuller analysis of these was previously conducted (Capdegelle 1999) and helped us develop our inclusion criteria.
Several models and descriptions of integration have been presented in the literature (WHO 1996;Capdegelle 1999; Leutz 1999; WHO/HIV/2008);
1. integration at the level of service delivery;
2. integration of management (planning, resource allocation, training and supervision, information systems); and
3. integration of organisations (co‐ordination between providers, inter‐sectoral co‐ordination, and communities) (WHO 1996; Ekman 2008).
This review focused on studies of integration at the level of service delivery.
Some examples of integration of service delivery that we identified include:
Sexually transmitted disease treatment services integrated with provision of family planning;
HIV education integrated with family planning;
Immunisation programmes integrated within primary care services;
HIV counselling and testing integrated into TB programmes; ;
TB control integrated with leprosy control;
Antenatal care and maternal child health (MCH) clinics.
Levels of care:
Integration may also occur at different levels of health care. For example, integration between family planning and child health in primary health care can be:
exclusively at the facility level where health workers provide health services;
at the facility level and in the community. These forms of integration utilise community health workers to raise awareness about services, provide information, and conduct household visits to identify people in need and to carry out some basic monitoring and service delivery.
In this review, we are concerned only with primary care, including government or non‐government agency primary healthcare services. We excluded studies concerned with collaboration between the public and private for‐profit sectors, and with hospital inpatient services.
Integration between specialist services in high‐income countries with highly sophisticated levels of care may have similar goals to integration in low‐ and middle‐income countries. However, the context is very different to poorer countries and therefore the findings of studies evaluating these programmes may not be applicable in poorer settings. This review therefore excluded studies conducted in high‐income countries, as defined by the World Bank (World Bank 2001) (details at www.worldbank.org).
Packages of care:
Some packages of care are described as integrated. Thus nutrition programmes which include a multiple array of inputs may be called an 'integrated nutrition programme'. However, they are generally implemented as a single vertical programme with several activities and are not strategies to promote integration. Similarly, the World Health Organization/UNICEF strategy 'Integrated Management of Childhood Illness' (IMCI) strategy started initially as an attempt to package case management care obtained from a series of vertical programmes (diarrhoeal disease control, acute respiratory tract infection, malaria, and nutrition) but grew to encompass prevention through immunisation, improved referral and health education (WHO 2005). This review focuses on the integration of vertical programmes into general health services at the point of delivery. We have therefore excluded ‘packages’ of care such as the Integrated Management of Childhood Illnesses (IMCI)and integrated nutrition programmes. IMCI has been evaluated in field trials and is the subject of a separate, forthcoming Cochrane review.
How the intervention might work
The present review is concerned with integration and strengthening linkages at the point of delivery. In such initiatives, providers are aiming to bring together several service functions, increase service coherence, and reduce fragmentation. For example, patients with particular health issues are often required to visit different clinics and services, which entails multiple journeys and wasted time. Here the purpose of integration is to provide services delivered together around a particular client group's needs, for example a sexually transmitted infection service (STI) combined with provision of contraceptives (family planning) or integrating services for mothers and their children. Improved efficiency at the point of delivery will include efficiency from the provider view point (in terms of better outputs for similar inputs and increased service utilisation) and from the user perspective (service more accessible or user friendly, for example). It is important to explore whether strategies that promote integrated delivery improve the efficiency of services and have an impact on health status. In areas where the public health system is relatively weak, targeted, vertical programmes may well have advantages in that they ensure delivery of a life saving technology; whereas integrated programmes with increased complexity may actually be less effective in delivering the services.
Outcomes
Integration aims to improve the services in relation to efficiency and access, thereby maximising use of resources and opportunities. For example, a primary healthcare unit is expected to cure people (using staff, procedures, and drugs); deliver vaccines (with effective cold chains, immunisation schedules, and information systems to ensure coverage); and provide reproductive health services (requiring expertise in family planning methods, skills in advising people, treatment of STIs and provision of effective follow up). Strategies to promote integration and linkages would ensure that these services were managed together to maximise efficiency and to increase opportunities for accessing the service. Thus the main intended outcomes of integration are improved efficiency, increased access to health services, improved satisfaction with care, and better health status overall.
Why it is important to do this update of the review
Initiatives to revitalize primary health care advocate integration as a key element of such renewal (Frenk 2009). Previous versions of this review have found limited rigorous evidence to inform decision making of the effectiveness of integration strategies . and advocated that further rigorous studies be conducted. This update seeks to identify, evaluate and include any new evidence on integration to inform policy making and planning of health care in low‐ and middle‐income countries.
The reasons for the original review were that a wider range of services can be offered through integration and strengthened linkages, which could reduce differences in access and utilisation of health services between geographic areas and socio‐economic groups, leading to greater equity (WHO 1996). Increased convenience for users may also lead to their increased satisfaction with services. Furthermore, some experts believe that integrated services are more likely to be sustainable, in the long term, than vertical programmes and can improve health overall (WHO 1996). However, such strategies may have unintended and unwanted outcomes; for example, health workers becoming overloaded or deskilled. Their ability and capacity to deliver specific technical services may be impaired , the quality of services may decline, service goals may not be achieved its goals and health outcomes may deteriorate. Integrated strategies may also increase the cost of service provision.
Given these debates, an update of this review was needed. We have revised the text and inclusion criteria to take into account the shifts in definitions of integration. We have also included the new term 'linkages', as a form of integration at the point of delivery, particularly in relation to the policy debates in TB, HIV and reproductive health.
Objectives
To determine whether strategies that aim to integrate primary health services or strengthen linkages at the point of delivery in low‐ and middle‐income countries:
a) improve healthcare delivery (including processes, outputs, service quality, and cost); b) produce a more coherent product (including user acceptability and satisfaction); c) improve health outcomes (including user behaviour change, morbidity or mortality).
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCT), non‐randomised controlled trials (NRCT), controlled before and after studies (CBA), and interrupted time series analyses (ITS). A NRCT was defined as a study that allocated units to intervention and control groups using methods that are not random. A CBA study was defined as one in which observations were made before and after the implementation of an intervention, both in a group that received the intervention and a control group that did not. CBA studies needed to include a minimum of two intervention and two control sites that were comparable, and contemporaneous data collection. To be eligible for inclusion, ITS studies needed to evaluate a change attributable to the intervention, have a clearly defined point in time when the intervention occurred and have at least three data points before and three after the intervention.
Types of participants
For this review, the units of study are the sites where primary care is delivered (healthcare facilities or clinics). Studies including any providers of primary health care were eligible for inclusion. For example, providers in publicly managed services (either free health services or with systems of cost recovery); in non‐governmental organisations; or in private organisations delivering services, for any kind of health problem. The review excludes studies conducted in high‐income countries as defined by the World Bank (World Bank 2001).
Types of interventions
Any management or organisational change strategy applied to existing systems that aimed to increase integration at the service delivery level in primary health. Primary health care is defined as the patient's first point of access to formal provision of health care, including general outpatient clinics of hospitals. We limited this to ambulatory or outpatient care providing formal primary health care (as the primary contact).
We excluded the following types of studies: those implemented in hospital (apart from general outpatient care) and speciality settings or inpatient care (secondary and tertiary care); those implemented in specialised hospital outpatient clinics; studies integrating service delivery across or between primary, secondary and tertiary care; studies evaluating a public, private for‐profit service mix; and studies of ''packages'' of vertical interventions such as IMCI and integrated nutrition programmes.
Types of outcome measures
We anticipated a variety of outcomes reflecting different settings. We identified the main categories of outcomes, listed below:
Primary outcomes
Healthcare delivery, as defined by providers
Utilisation, service outputs, measures of service quality and efficiency (unit cost) Unit of analysis: facility or clinic
Healthcare received, as defined by users
User views Unit of analysis: clinic users; communities
Health behaviour and status outcomes
Variables: knowledge and behaviour change, nutritional status, morbidity or mortality Unit of analysis: facilities and communities
Search methods for identification of studies
The original search strategy was used, but in the 2010 update we specifically sought for and included any study which considered linkages between TB, HIV, reproductive health, and STI services. These were always included in the review but we searched additional sources such as the bibliography of the WHO Links review to ensure we had all relevant studies (WHO/HIV/2009).
The following electronic bibliographic databases were searched:
The Cochrane Central Register of Controlled Trials (CENTRAL) 2010, Issue 3, part of the The Cochrane Library.www.thecochranelibrary.com, including the Cochrane Effective Practice and Organisation of Care Group Specialised Register (searched 15 September 2010)
MEDLINE, Ovid (1950 to August Week 5 2010) (searched 10 September 2010)
EMBASE, Ovid (1980 to 2010 Week 35) (searched 10 September 2010)
CINAHL, EBSCO (1980 to present) (searched 20 September 2010)
Sociological Abstracts, CSA Illumina (1952 to current) (searched 10 September 2010)
Social Services Abstracts, CSA Illumina (1979 to current) (searched 10 September 2010)
POPLINE (1970 to current) (searched 10 September 2010)
International Bibliography of the Social Sciences, Webspirs (1951 to current) (searched 01 July 2008)
HealthStar (1975 to September 2005)
Cab Health (1972 to 1999)
We also searched the World Health Organization (WHOLIS) library database, handsearched relevant WHO publications, and contacted experts in the field. Reference lists of studies were scanned for relevant studies and, where necessary, the authors were contacted for copies of articles.
The MEDLINE terms and strategy were translated into appropriate strategies for the other databases.
Full search strategies for all databases are included in Appendix 1.
Data collection and analysis
Selection of studies
Two authors examined the lists of references generated by the search and retrieved any likely studies. Two authors then independently assessed the retrieved studies for inclusion using a checklist for eligibility based on the inclusion criteria listed above. The methods of selection of studies followed standard guidelines from the EPOC Group (www.epoc.uottawa.ca ). Disagreements between the review authors regarding study inclusion were resolved by discussion. In the 2005 update, we moved Taylor 1987 from an included study to an excluded study as we were unable to determine how the communities were allocated, and the paper gave no reassurance that this was randomised. Subsequent correspondence with the authors provided sufficient information on the trial design and methods to address the earlier concerns, and the study was included again in the 2010 update.
Data extraction and management
Data extraction was carried out by two authors, based on the EPOC Group's data collection checklist. We extracted standard information about methods, participants, interventions, and outcomes. The results from similar integration strategies were grouped together.
All studies were complex in relation to both intervention and the evaluation methods used. We grouped studies into those that were exclusively clinic based and those that also included a substantial community component. We then further divided the studies into those where the researchers simply 'added on' one new function to an existing service, and those that made a more substantive effort to integrate delivery (as opposed to having separate vertical programmes). In studies which had more than one intervention group, but the interventions in these groups were similar, we combined the intervention groups in the analysis (Mark 2007, Nyamuryekung'e 1997). The study results were not pooled in a meta‐analysis as there was considerable heterogeneity in the content, design, settings, and outcomes of the studies. We have therefore presented a narrative summary of the study findings.
Of the four cluster randomised trials included in the review, two studies (Pope 2008; Gregson 2007) had adjusted for intra‐cluster correlation. Attempts were made to adjust for clustering in the cluster RCT's where this had not been done adequately by the authors. However, insufficient data were available to make these adjustments in the relevant studies (Huntington 1994; Nyamuryekung'e 1997).
Assessment of risk of bias in included studies
Two authors assessed the risk of bias in eligible studies using the EPOC risk of bias criteria which has been adapted from the Cochrane Collaboration criteria for assessing risk of bias (Higgins 2009). A GRADE assessment of the quality of the evidence was done using GradePro and is reported in summary of findings tables 2‐7. Criteria used for assessing the quality of the evidence included: limitations in the design and implementation of the study, indirectness of evidence, unexplained heterogeneity or inconsistency of results, imprecision of results, and publication bias.
Results
Description of studies
Included studies
Nine studies, including two sub studies contained in one publication (Taylor 1987) met the inclusion criteria. These included five randomised controlled trials (RCTs) (Huntington 1994; Nyamuryekung'e 1997; Gregson 2007; Mark 2007; Pope 2008) and four controlled before and after (CBA) studies (Tuladhar 1982; Taylor 1987 (FP); Taylor 1987 (Nutrition); Leon 2010). The latter studies had contemporaneous data collection and the control sites were comparable.
All the studies, with the exception of the Narangwal study (Taylor 1987), could be grouped into those that were exclusively clinic based and those that also included a substantial community component.
Participants
Study participants included individual patients, couples, households, and communities using primary healthcare services; and providers of primary healthcare services (Table 8, Table 9). Most of the interventions included training and additional supervision and support of the health service providers. The service providers were mainly nurses (Mark 2007; Pope 2008; Leon 2010; Gregson 2007), physicians (Nyamuryekung'e 1997), lay family health workers or auxiliary health workers (Tuladhar 1982; Taylor 1987 (FP); Taylor 1987 (Nutrition)), or an undefined category of service providers (Huntington 1994). The studies used health workers who were already working in the facilities or communities and did not recruit additional staff, with the exception of Nyamuryekung'e 1997 in which ‘visiting outreach clinicians’ were introduced.
1. Additional Table 1: Description of interventions in ''Add on'' studies.
| Study | Setting | |||
| Point of delivery | Health workers | Patients/ participants | Organisation of services | |
| Huntington 1994 | Primary care clinics providing immunisation (EPI) services | Clinic EPI service providers (not specified if nurses or other) | Women attending the clinics for immunisation of their children | Ministry of Health EPI services are fully integrated into MCH services in Togo. FP was offered as a vertical programme in the public sector |
| Leon 2010 | Primary care STI clinics | Nurses working in STI clinics | New STI clients | STI clinics were managed by local government (municipal) health departments |
| Mark 2007 | Voluntary HIV Counselling and Testing (VCT) clinic | Trained nurses, clinical officers and/or social workers | Co‐habiting couples attending the clinic | The VCT centre was established as part of a larger research project (Zambia Emory HIV Research Project) |
| Pope 2008 | Primary care TB clinics | Designated TB nurse in each clinic | New adult (>18 years) TB patients attending the clinics | TB clinics were managed by local government (municipal) health departments |
|
Taylor 1987 |
Community based PHC services provided by family health workers (FHWs) in villages, supported by local health services | FHWs based in villages (retrained auxiliary nurse midwives or lady health visitors with 1.5 years health training beyond middle school). | Children aged between 0‐ 36 months living in the villages. | FHWs received weekly supervisory visits by doctors or nurses. Referred 10% of patients to these supervisory staff or health facilities |
| Taylor 1987 | Community based PHC services provided by FHWs in villages, supported by local health services | FHWs based in villages (retrained auxiliary nurse midwives or lady health visitors with 1.5 years health training beyond middle school). | Couples living in the villages | FHWs received weekly supervisory visits by doctors or nurses. Referred 10% of patients to these supervisory staff or health facilities |
2. Additional Table 2: Description of integrated interventions compared to special or vertical programmes.
| Study | Setting | |||
| Point of delivery | Health workers | Patients/participants | Organisation of services | |
| Gregson 2007 | Integrated community and clinic based activities in communities with at least one government or mission health centre | Clinic nursing staff (trained in syndromic management of STIs) Peer educators in community sites; |
Adults (male 17‐54 years & female 15‐ 44 years) living in these communities | Two local NGOs and government MoH and Child Welfare |
| Nyamuryekung'e 1997 | Truck stops served by primary health clinics providing STI services |
Clinicians at health facilities (provided with one week of training in STI management); or clinicians who visited once every three months and saw women at sites away from health facilities. Peer health educators in all sites. |
Female sexual partners of truck drivers, living at truck stops | Intervention linked to NGO AIDS prevention project targeting truck drivers |
|
Taylor 1987 |
Community based PHC services in villages supported by local health services | Family health workers (FHWs) based in villages (retrained auxiliary nurse midwives or lady health visitors with 1.5 years health training beyond middle school). | Children aged between 0‐36 months living in the villages. | FHWs received weekly supervisory visits by doctors or nurses. Referred 10% of patients to these supervisory staff or health facilities |
| Taylor 1987 | Community based PHC in villages supported by local health services | Family health workers based in villages | Couples living in the villages | FHWs received weekly supervisory visits by doctors or nurses. Referred 10% of patients to these supervisory staff or health facilities |
|
Tuladhar 1982 |
Vertical: Special district based clinic centres and panchayats, supported by a district office Integrated: Health posts supported by a district office |
Vertical: Separate health workers and trained village midwives. Health workers are primary link with village population. Do home visits, and promote FP/MCH and deliver services. | Households with married women aged 15 to 44 years in selected wards of districts | Separate organizational structure with own management and supervisory staff for the vertical FP/MCH services |
Most facility based studies also provided additional diagnostic tests, contraceptives and drugs in the integrated arms. Gregson 2007 included additional community based information education and communication (IEC) and income generation inputs. None of the studies provided incentives for health workers or patients, to promote integration.
Interventions
Integration strategies in the included studies focused mainly on delivery arrangements, either involving professional or organisational changes, or both. No studies of governance or financial strategies to promote integration were identified or included.
There were three main areas of delivery.
Family planning:‐four studies evaluated integration around family planning services. One trial that randomised clinics examined linking family planning services to an expanded programme of immunisation (EPI) , in Togo (Huntington 1994); a CBA compared integrated family planning and maternal and child health services with vertical family planning, maternal and child health services, in Nepal (Tuladhar 1982); a RCT evaluated linking family planning services to a voluntary HIV counselling and testing service in Zambia (Mark 2007); and a CBA compared delivery of vertical and integrated family planning, child and women’s health services, in Narangwal, India (Taylor 1987 (FP).
Nutrition and infectious disease control, a CBA compared vertical and integrated nutrition and infectious disease interventions delivered by family health workers in Narangwal, India (Taylor 1987 (Nutrition).
STI treatment, HIV/AIDS prevention and control, and TB treatment: one cluster RCT compared STI services provided either through ''special'' dedicated STI services or STI services integrated in routine primary health services in Tanzania (Nyamuryekung'e 1997). Three studies assessed integration around HIV, STI, and TB services. These included a RCT of the integration of HIV testing and counselling in TB clinics (Pope 2008) and a NRCT in STI services (Leon 2010), both conducted in South Africa; and a RCT of integration of HIV prevention interventions in clinics and communities in Zimbabwe (Gregson 2007).
No included studies examined integration in neglected tropical diseases programmes.
The studies were grouped into those that either added a new service on to an existing programme, or evaluated vertical versus horizontal patterns of delivery (see Table A below).
Add‐on services
Five studies assessed adding a function to an existing vertical programme (Table 8).
Clinic based: four studies described add‐on interventions at facilities. In Togo (Huntington 1994), mothers attending an Expanded Program of Immunization (EPI) clinic were provided with individual counselling and were encouraged to attend a concurrent family planning clinic. In Zambia (Mark 2007), family planning was offered to couples attending an HIV voluntary counselling and testing service; and in South Africa (Pope 2008; Leon 2010), provider initiated HIV counselling and testing were added to TB and STI clinic services, respectively.
Clinic and community based: Taylor 1987 added a nutrition intervention or health care for infectious diseases in children, or both, through community based health workers; and family planning, women and children’s health services in addition to routine services in the clinic.
Vertical versus horizontal delivery
Four studies assessed vertical interventions compared to a fuller integration of services (Table 9).
Clinic based: at the facility level, Nyamuryekung'e 1997 compared integrated STI care through routine services with special clinics outside normal working hours, or special teams of clinicians visiting every three months, in Tanzania.
Clinic and community based: the Tuladhar 1982 study in Nepal evaluated family planning, women's and child health services either through integrated primary preventive services or through a vertical programme, including both facility and community components. Taylor 1987 compared single and multiple (integrated) special services for nutrition and child health; as well as for family planning, women’s and child health, with routine service delivery, in India. Gregson 2007 evaluated an integrated community and clinic based HIV control intervention, in Zimbabwe.
The Narangwal study was a complicated but important exception that seemed to cover several categories. This study examined one question around adding on services and another around vertical versus horizontal provision.
Add‐on services: in the first part of the study, two experimental groups were compared with routine services. Inone group nutrition care was added and in the other infection control programmes were added. A second part of the study examined whether adding family planning, women's and child health services to an existing programme was effective.
Vertical versus horizontal provision: The first part of the study examined whether delivering nutrition and infection control programmes together was better than programmes delivering them singly.The second part of the study examined whether delivering family planning, women's and child services packaged together was better than providing them singly.
These different comparisons within Taylor 1987 meant it contributed both to the evaluation of the 'add‐on' model and the 'vertical versus horizontal' data set.
Table A: Categorisation of studies into 'add on' or 'fully integrated' at facility level or community and facility levels
| Add on | Integrated versus vertical | |
| Facility | Family planning to Expanded Programme of Immunisation: Huntington 1994 Family planning to Voluntary Counselling and Testing: Mark 2007 Provider Initiated HIV counseling and testing to TB services: Pope 2008 Provider Initiatived HIV counseling and testing to STI services: Leon 2010 |
Different models of special or integrated STI treatment: Nyamuryekung 1997 |
| Community and Facility | Nutrition and child health care added to routine services: Taylor 1987 Family planning, child health and women’s health added to routine services:Taylor 1987 |
Vertical and integrated family planning/maternal and child health care programmes: : Tuladhar 1982 Single and integrated and nutrition and child health care services: Taylor 1987 Single and integrated family planning, child health,and women's health care services: Taylor 1987 Integrated HIV control: Gregson 2007 |
Excluded studies
A large number of studies of integration were identified in the search. The characteristics of studies that appeared initially to be suitable but on closer inspection did not meet the inclusion criteria are provided in the Characteristics of excluded studies table. The main reasons for excluding studies were that the study design did not meet the inclusion criteria or the intervention did not match the criteria for integration strategies that were used in this review.
Outcomes
We divided outcomes into three categories to correspond with the outcomes defined in the protocol. All nine studies included outcomes concerned with the processes and outputs of healthcare delivery. Three studies assessed the effect on knowledge and behaviours of service users (Huntington 1994; Tuladhar 1982; Gregson 2007). Five studies measured the impact on health status (Tuladhar 1982; Gregson 2007; Mark 2007; Taylor 1987 (FP and nutrition sub studies)), although the quality of data on health status was poor in two studies (Tuladhar 1982; Taylor 1987). Only one study described any aspect of users' perceptions of the service, but reported only on 'users satisfied' as a dichotomous variable (Nyamuryekung'e 1997).
Risk of bias in included studies
Our assessment of risk of bias, according to the EPOC checklist, is summarised in Table 10.
3. Additional Table 3. Risk of Bias.
| Study | Design | Allocation sequence adequately generated | Allocation concealment | Similar baseline characteristics or controlled in analysis | Blinded assessment | Incomplete outcome data adequately addressed | Contamination protection | Free of Selective Reporting of Outcomes |
| Gregson 2007 | Cluster RCT | Yes | Yes | Yes | No | Yes | Unclear | Yes |
| Huntington 1994 | Cluster RCT | Unclear | Unclear | Yes | No | Unclear | Yes | Unclear |
| Leon 2010 | Controlled before and after study | No | No | Yes | No | Yes | No | Yes |
| Mark 2007 | RCT | Yes | Yes | Yes | Unclear | Unclear | Yes | Yes |
| Nyamuryekung’e 1997 | Cluster RCT | Unclear | Unclear | Unclear | No | Unclear | Yes | Yes |
| Pope 2008 | Cluster RCT | Unclear | Unclear | Yes | No | Unclear | Yes | Yes |
| Taylor 1987 (Family Planning) |
Controlled before and after study | No | No | Yes (additional data obtained from author) | No | Unclear | Yes | No |
| Taylor 1987 (Nutrition) |
Controlled before and after study | No | No | Yes (additional data obtained from author) | No | Unclear | Yes | No |
| Tuladhar 1982 | Controlled before and after study | No | No | Yes | No | Yes | Yes | Yes |
The included RCT (Mark 2007) and one cluster RCT (Gregson 2007) adequately addressed most potential risks of bias; with the exception of blinding which was not possible under the field conditions of these trials.
Three cluster RCTs (Huntington 1994; Nyamuryekung'e 1997, Pope 2008)did not describe how the allocation sequence was generated. Most of the studies had similar baseline characteristics in the intervention and comparison sites, but did not have blinded assessments. . Of the four cluster RCTs, Pope 2008 was the only one to clearly describe adjustments in the sample size or an analysis to address intra‐cluster correlation.
The four CBA studies (Tuladhar 1982; Taylor 1987 (FP); Taylor 1987 (Nutrition); Leon 2010) each included at least two comparable groups in the intervention and control sites, and collected baseline as well as post‐intervention assessments. None of these studies sought to identify or control for potential confounders in the analysis however.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7
for the main comparison.
| Main interventions | Key Findings |
|
Add on of services | |
| 1.Does adding‐on of family planning services to primary care improve use and effectiveness of family planning compared to usual care? Table 2 | Adding on family planning to other services probably increases use of family planning; but probably results in little difference in incident pregnancies. |
| 2. Does adding on provider initiated counselling and testing (PICT) at primary health care (PHC) facilities increase HIV counselling and testing of clients attending tuberculosis or sexually transmitted infection clinics? Table 3 | Adding on PICT to TB and STI PHC clinic services probably increases the number of people receiving HIV counselling and HIV testing. |
| 3. Does adding on nutrition and child health services at facility and community level reduce mortality in children? Table 4 | The effects of adding on nutrition and child health services are uncertain because the quality of the evidence is very low |
|
Integration compared to vertical delivery | |
| 1. Does integration of sexually transmitted infection services improve utilisation and client satisfaction with care? Table 5 | Integrating STI services into routine PHC may decrease utilisation of the services, and may decrease women's satisfaction with services. |
| 2. Does integrated family planning, maternal and child health care improve family planning use and child health outcomes compared to vertical delivery of these services? Table 6 | Integration of FP and MCH services may decrease knowledge of family planning; may lead to little difference in family planning utilisation; and may lead to little or no difference in child survival. |
| 3. Does integration of HIV prevention and control at community and facility level reduce risk factors for HIV and HIV incidence? Table 7 | Integration of HIV prevention and control improves effectiveness of STI treatment in males; but results in no difference in health seeking behaviour, STI incidence or HIV incidence in the population. |
Summary of findings 2. Summary Table: Add on of family planning services.
|
1. Does adding‐on of family planning services improve use and effectiveness of family planning compared to usual care? | |||||
|
Patient or population: Facilities providing primary health services Settings: primary health services in Togo, Zambia and India Intervention: Add on of services for family planning Comparison: Routine services (with no add ons) | |||||
| Outcomes |
Illustrative comparative risks |
Relative effect [95% CI] |
No of Participants/Units | Quality of the evidence (GRADE) | |
| No add on services | Add on services | ||||
| Family planning added to Expanded Programme of Immunisation services (Huntington 1994) | |||||
| Change in number of mothers accepting family planning services | 23 more per month1 | 107 more per month (p<0.003) | 365% increase | 16 clinics | ++OO Low2 |
| Promotion of dual method contraception at a Voluntary Counseling and Testing clinic (Mark 2007) | |||||
| Couples initiating non barrier contraception | 27/82 (33%) |
133/169 (79%) |
RR 2.39 [1.74, 3.29] |
251 couples | +++O Moderate |
| Incident pregnancies occurring during a one year follow up period | 18/82 (22%) |
33/169 (19.5%) |
RR 0.89 [0.53, 1.48]3 |
251 couples | +++O Moderate |
| Family planning, child health and women's health services in primary health care (Taylor 1987 (FP)) | |||||
| Change in % of women accepting family planning methods | Effect is uncertain for adding on either individual or combined family planning, child health and women's health to existing services4. | 19 villages | +OOO Very low | ||
| CI: Confidence interval; RR: Risk OR Odds Ratio | |||||
| GRADE Working Group grades of evidence ++++ High = We are confident that the true effect lies close to that of the estimate of the effect. +++O Moderate = The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. ++OO Low = The true effect may be substantially different from the estimate of the effect. +OOO Very low = Any estimate of effect is very uncertain. | |||||
1. No denominator of total number of attendees was provided for this period.
2. 16 clinics ’’randomly’’ selected from a stratified sample of clinics, with probability of being included linked to caseload. Allocation sequence generation not clear, and no concealment and blinding. No control for clustering in study design and analysis of data.
3. High discontinuation rates of non barrier contraception, and oral contraception user failure were recorded.
4. Data reported did not include change in absolute numbers of women, but only reported percentages. No statistical analysis of results was provided. Different interventions sites started at different times, and the study was aborted one year early as a result of changes in the context.
Summary of findings 3. Summary Table: Add on of HIV Counseling and Testing.
| 2. Does adding on Provider Initiated Counseling and Testing at Primary Health facilities increase HIV counseling and testing of clients attending Tuberculosis or Sexually Transmitted Infection clinics? | |||||
|
Patient or population: Facilities providing primary health services Settings: Tuberculosis and Sexually Transmitted Infection clinics in South Africa Intervention: Integration of Provider Initiated Counseling and Testing Comparison: Routine services | |||||
| Outcomes | Illustrative comparative risks |
Relative effect [95% CI] |
No. of participants/units |
Quality of the evidence (GRADE) |
|
| No add on services | Add on services | ||||
|
Patients offered HIV testing in STI clinics1 |
3406/6027 (50.7%) |
2326/3053 (76.8%) |
RR 1.35 [1.31, 1.39] | 9080 patients seen at 21 PHC facilities | +++O Moderate |
|
Patients who received HIV testing in STI clinics1 |
2821/6027 (42.7%) |
1752/3053 (56.4%) |
RR 1.23 [1.18, 1.28] | 9080 patients seen at 21 PHC facilities | +++O Moderate |
| New adult TB patients received HIV counselling in TB clinics2 | 31/402 (7.7%) |
73/352 (20.7%) |
RR 2.69 [1.81, 3.99] | 754 patients seen at 20 TB clinics | ++++ High |
| New adult TB patients received HIV testing in TB clinics2 | 26/402 (6.5%) |
71/352 (20.2%) |
RR 3.12 [2.04, 4.77] | 754 patients seen at 20 TB clinics | ++++ High |
| CI: Confidence interval; RR: Risk Ratio; OR Odds Ratio | |||||
| GRADE Working Group grades of evidence ++++ High = We are confident that the true effect lies close to that of the estimate of the effect. +++O Moderate = The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. ++OO Low = The true effect may be substantially different from the estimate of the effect. +OOO Very low = Any estimate of effect is very uncertain. | |||||
Summary of findings 4. Summary Table: Add on of Nutrition and Child Health Services.
| 3. Does adding on nutrition and child health services at facility and community level reduce mortality in children?1 | |||||
|
Patient or population: Children under 3 years of age in rural villages Settings: Primary health services in Narangwal, India Intervention: Adding on nutrition and child health interventions at community and facility level i.e. family health workers delivering services in homes or village clinic Comparison: Routine services | |||||
| Outcomes | No add on services | Add on services |
Relative effect (95% CI) |
No. of participants or units |
Quality of the evidence (GRADE) |
|
Perinatal mortality (deaths per 1000 live and stillbirths) |
104.2 | Nutrition:60.9 Child Health:80.8 Nutrition and Child health:63.3 |
Effect is uncertain for adding on either individual or combined nutrition and child health services to existing services | 10 villages | +OOO Very low |
|
Neonatal mortality (deaths per 1000 live births) |
77.8 | Nutrition: 48.3 Child Health:46.7 Nutrition and Child health:47.4 |
Effect is uncertain for adding on either individual or combined nutrition and child health services to existing services | 10 villages | +OOO Very low |
|
Infant mortality2 (deaths per 1000 live births) |
129.2 | Nutrition:96.6 Child Health:70 Nutrition and Child health:81 |
Effect is uncertain for adding on either individual or combined nutrition and child health services to existing services | 10 villages | +OOO Very low |
| CI: Confidence interval; RR: Risk Ratio; OR Odds Ratio | |||||
| GRADE Working Group grades of evidence ++++ High = We are confident that the true effect lies close to that of the estimate of the effect. +++O Moderate = The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. ++OO Low = The true effect may be substantially different from the estimate of the effect. +OOO Very low = Any estimate of effect is very uncertain | |||||
2. Absolute numbers of deaths and the denominator population were not reported, neither were any results of statistical analyses to estimate risk.
Summary of findings 5. Summary Table: Integration of Sexually Transmitted Infection Services.
| 1. Does integration of Sexually Transmitted Infection (STI) services improve utilisation and client satisfaction with care?1 | |||||
|
Patient or population: Women living around truck stops Settings: Truck stops and associated health facilities in Tanzania Intervention: Integration of Sexually Transmitted Infection services into routine health services Comparison: Special ''vertical'' delivery models of Sexually Transmitted Infection services | |||||
| Outcomes | Vertical | Integrated |
Relative effect (95% CI) |
No. of participants or units |
Quality of the evidence (GRADE) |
|
Utilisation of STI services [Number of visits to STI services per women assessed over a one year period] |
1.32 per woman (1000/758) |
1.00 per woman (628/625) |
Not available | 7 truck stops | ++OO Low |
| Women referred to and attended STI services | 458/602 (76%) | 62/150 (41%) | RR 0.54 [0.45, 0.66] |
7 truck stops | ++OO Low |
|
Women satisfied with STI services [Number of women interviewed who were satisfied] |
78/85 (92%) | 41/53 (77%) | RR 0.84 [0.72, 0.99] |
7 truck stops | ++OO Low |
| CI: Confidence interval; RR: Risk Ratio; OR Odds Ratio | |||||
| GRADE Working Group grades of evidence ++++ High = We are confident that the true effect lies close to that of the estimate of the effect. +++O Moderate = The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. ++OO Low = The true effect may be substantially different from the estimate of the effect. +OOO Very low = Any estimate of effect is very uncertain. | |||||
Summary of findings 6. Summary Table: Integration of family planning, maternal and child health care.
|
2. Does integrated family planning, maternal and child health care improve family planning use and child health outcomes compared to vertical delivery of these services? | |||||
|
Patient or population: Couples, women and children in villages and districts Settings: Primary health services in Nepal and India Intervention: Integrated delivery of family planning, maternal, child health and nutrition services. Comparison: Routine government health services | |||||
| Outcome | Vertical | Integrated |
Relative effect (95% CI) |
No. of participants or units |
Quality of the evidence (GRADE) |
| Integration of family planning, maternal and child health into routine care (Tuladhar 1982) | |||||
|
Change in % of women using family planning |
2 to 4% Change + 2% |
2 to 5% Change +3% |
Change difference 1% | Four districts | ++OO Low |
|
Change in knowledge of family planning |
29 to 55% Change + 26% |
23 to 28% Change +5% |
Change difference ‐21% | Four districts | ++OO Low |
| Change in Infant Mortality Rate per 1000 live births1 | Change ‐ 47 | Change ‐ 25 | RR 0.53 | Four districts | ++OO Low |
| Integration of nutrition, and child health care programmes with routine care (Taylor 1987 (Nutrition)) | |||||
|
Perinatal mortality1 (deaths per 1000 live and stillbirths) |
Nutrition: 60.9 Child Health: 80.8 |
Nutrition and Child health2: 63.3 | Effect is uncertain for integrated nutrition and child health services | 10 villages | +OOO Very low |
|
Neonatal mortality1 (deaths per 1000 live births) |
Nutrition: 48.3 Child Health:46.7 |
Nutrition and Child health2: 47.4 | Effect is uncertain for integrated nutrition and child health services | 10 villages | +OOO Very low |
|
Infant mortality1 (deaths per 1000 live births) |
Nutrition:96.6 Child Health:70 |
Nutrition and Child health2:81 | Effect is uncertain for integrated nutrition and child health services | 10 villages | +OOO Very low |
| CI: Confidence interval; RR: Risk Ratio; OR Odds Ratio | |||||
| GRADE Working Group grades of evidence ++++ High = We are confident that the true effect lies close to that of the estimate of the effect. +++O Moderate = The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. ++OO Low = The true effect may be substantially different from the estimate of the effect. +OOO Very low = Any estimate of effect is very uncertain. | |||||
1. Absolute numbers of deaths and the denominator population was not reported, neither were any statistical calculations to estimate risks.
2. The combined delivery of child health and nutrition was compared to each of vertical delivery of either child health or nutrition.
Summary of findings 7. Summary Table: Integration of HIV Prevention and Control.
| 3. Does integration of HIV prevention and control at community and facility level reduce risk factors for HIV and HIV incidence?1 | |||||
|
Patient or population: Communities and health centres Settings: Primary health services in Zimbabwe Intervention: Integration of community and facility services for the prevention and control of HIV Comparison: Routine government health services | |||||
| Outcome | Vertical | Integrated |
Relative effect [95% CI] |
No. of participants and units |
Quality of the evidence (GRADE) |
|
STI treatment effectiveness Reported as symptoms stopped since STI treatment in past year |
Males 38/68 (56%) Females 127/185 (69%) |
Males 70/90 (78%) Females 129/188 (69%) |
POR 2.49[1.22, 5.10] POR 0.99[0.63,1.55] |
11980 adults in 12 communities | ++++ High |
|
Health seeking behaviour Sought treatment within 3 days of STI symptoms in last year |
Males 28/84 (33%) Females 49/272 (20%) |
Males 43/112 (38%) Females 58/272 (21%) |
POR 1.13[0.59,2.16] POR 1.14[0.7,1.77] |
11980 adults in 12 communities | ++++ High |
|
STI incidence Urethral or vaginal discharge in last year |
Males 42/993 (4%) Females 212/1425(15%) |
Males 60/1007 (6%) Females 241/1521(16%) |
POR 1.41[0.94,2.12] POR 1.10[0.90,1.35] |
11980 adults in 12 communities | ++++ High |
|
HIV Incidence/1000 person years at risk |
1.49 (89/5993) |
2.04 (123/6015) |
IRR 1.36[1.03,1.81] unadjusted IRR 1.27[0.92,1.35] adjusted |
11980 adults in 12 communities | ++++ High |
| CI: Confidence interval; IRR: incidence risk ratio; POR: prevalence odds ratio | |||||
| GRADE Working Group grades of evidence ++++ High = We are confident that the true effect lies close to that of the estimate of the effect. +++O Moderate = The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. ++OO Low = The true effect may be substantially different from the estimate of the effect. +OOO Very low = Any estimate of effect is very uncertain. | |||||
1. Gregson 2007
The studies varied extensively in their interventions as well as the outcomes measured. It was therefore not possible to do a meta‐analysis of the results. The studies were therefore reported individually (Summary of findings tables 2‐7) and summarised in the Table 1 and the narrative. Studies were too heterogeneous for us to explore factors influencing the success or otherwise of integration strategies.
Add‐on services
The key findings of studies evaluating add‐on services are included in the Table 1.
i. Facility based
In Togo (Huntington 1994, Table 2), mothers attending an EPI clinic were encouraged to attend a concurrent family planning clinic. Awareness of the availability of the family planning service increased, with a consequent increase in the number of new (P < 0.003) and total acceptors (P < 0.0001). A survey found no change in desired birth interval associated with the intervention. The providers were interviewed but they were simply asked if they thought the intervention was having an impact on referrals: the responses suggested that the bulk of providers viewed the intervention as having a positive effect on referrals. Both control and intervention clinics increased the number of EPI doses administered over the study period, suggesting that adding on services did not have a negative effect on the EPI programme (Table 11).
4. Additional Table 4: Huntington 1994: Togo (Cluster RCT of family planning integration in EPI services).
| Category | Measure and unit | Integrated (pre to post measure of change) | Vertical (pre to post measure of change | Difference |
| Health care delivery | Recall of FP message (% of EPI clients responding affirmatively) | 9% pre to 21% post. Change +12 | 8% to 9%. Change +1 | Change difference is +11 |
| Health care delivery | Awareness of FP availability at clinic (% of EPI clients responding affirmatively) | 40% (pre) to 58% (post). Change +18 (p<.001) | 32 to 36%. Change +4 | Change difference is +14 |
| Health care delivery | Total family planning clients per month (mean number from service records) | 1035 to 1311; Change +276 (p<.0001) | 704 to 768. Change +64 (NS) | Change difference +212 (p<.0001) |
| Intermediate outcomes | Provider's view: effect of message on consultations (self administered questionnaire) | Did the message have an effect? "Yes": 90%; What type of effect? "positive": 96%; "negative": 4%. | Not applicable |
In Zambia (Mark 2007), couples attending a voluntary HIV counselling and testing (VCT) centre were offered free non‐barrier contraceptives at the centre in addition to routine family planning education and referrals, provided for all clients. The couples offered family planning at the VCT centre had a significantly higher uptake of non‐barrier contraceptives at three months (RR 2.39, CI1.74 to 3.29] (Table 2). However, incident pregnancies assessed at 12 months did not differ between the intervention and control groups (RR 0.89, CI 0.53 to 1.48]). High discontinuation rates of non‐barrier contraceptives and high rates of oral contraception user failure were recorded. The use of non‐barrier contraception was not associated with decreased condom use. Client satisfaction was not assessed (Table 12).
5. Additional Table 5: Mark 2007: Zambia (RCT of family planning at VCT clinic).
| Outcome | Measure and Unit | Intervention | Control |
Difference RR [95% CI] |
| Health care delivery | % follow up intervals during which a condom was used | 62 and 58 months | 63 months | Not significant |
In South Africa (Pope 2008; Leon 2010), provider initiated HIV counselling and testing was added to services at TB clinics and STI clinics, respectively, through the training of health workers and the provision of tests and equipment. The interventions resulted in an increase of HIV counselling (RR 2.69, CI 1.81 to 3.99) and testing (RR 3.12, CI 2.04 to 4.77) for TB, and HIV testing for STI patients (RR 1.23, CI 1.18 to 1.28].(Table 3, Table 13, Table 14).
6. Additional Table 6: Pope 2008: South Africa (Cluster RCT of integrated HIV counselling and testing in TB clinics).
| Outcom Category | Measure and unit | Integrated | Control |
Difference RR [95%CI] |
| Health status | Mean % of patients tested HIV + | 8.5% (30/352) | 2.5% (10/402) | 3.43 [1.70, 6.91] |
7. Additional Table 7: Leon 2010: South Africa (CBA of PICT in routine STI services).
| Outcome Category | Measure and Unit |
Integration (PICT) |
Vertical (VCT) |
Difference RR [95%CI] |
| Health Care Delivery | Declined HIV testing as a proportion of all new STI clients | 20.4% (574/3053) |
8.1% (585/6027) |
1.94 [1.74, 2.15] |
| Health Care Delivery | Declined HIV testing as a proportion of those offered testing | 26.7% (574/2326) |
13.5% (585/3406) |
1.44 [1.30, 1.59] |
ii. Community and facility
In India (Taylor 1987), two complex interventions linked to family planning and nutrition were assessed. Both used family health workers to provide community based services in addition to routine government health services which served as the control. In one arm of the study the interventions focused on nutrition and infection control, and in the other arm on family planning, women's and child health.
The addition of community based family planning to womens' and child health services improved family planning acceptance as compared to routine services. Women's and child health outcomes were not reported. Using family planning outcomes as a measure of effectiveness, the addition of family planning to maternal and child health was reported as being more cost effective than the routine services (Table 15). However, serious limitations in study design and the early closure of the study makes the evidence of effect very uncertain (Table 2).
8. Additional Table 10: Taylor 1987: India (CBA of family planning integration with women and child health programmes).
| Outcome Category | Measure and unit | Integration (FP, child health and womens health) |
Vertical (FP and Child Health) |
Vertical (FP and Womens health) |
Control (Routine services) |
| Health Care Delivery | Cost per acceptor (1971 US $) | 13 | 27 | 39 | 39 |
| Cost per year of protection (1971 US $) | 11 | 18 | 26 | 32 | |
| Cost per birth averted (1971 US $) | 35 | 45 | 68 | 107 |
The addition of community based nutrition and infection control interventions improved nutrition indicators, and reduced the duration of illnesses and mortality when compared to the routine service sites (Table 16, Table 4). However, serious limitations in study design makes the evidence of effect uncertain.
9. Additional Table 11: Taylor 1987: India (Cluster RCT of nutrition programme integrated with health care).
| Outcome Category | Measure and unit | Integration |
Vertical (health care) |
Vertical (nutrition) |
Control (routine services) |
RR (95% CI) |
| Health Status: Mortality |
Child mortality (1‐3 year olds) Deaths /population 1‐3 years old |
13.3 | 11 | 11 | 18.6 | Not available |
| HealthStatus : Morbidity |
Cough: Number of days | 8.5 | 8.2 | 10.4 | 11.4 | Not available |
| Diarrhoea: Number of days | 5.0 | 4.9 | 5.6 | 6.3 | Not available | |
| Vomiting: Number of days | 3.5 | 3.0 | 4.1 | 5.2 | Not available | |
| Fever: Number of days | 2.9 | 2.7 | 3.7 | 4.0 | Not available |
Vertical versus integrated service delivery
The key findings of the vertical versus integrated services studies are included in Table 1. .
i. Facility based
In the Tanzania study (Nyamuryekung'e 1997), different models of delivery of STI services for women at truck stops were evaluated. Peer educators were trained to refer the women with evidence of a STI to three types of service: STI services integrated into routine health facilities (normal working hours); special after hours STI services twice a week; or a special team of clinicians visiting every three months. Utilisation, in terms of attendances per number of women at each truck stop, was similar but slightly higher in special after hours STI services and lower in the integrated services within normal working hours (Table 5). The proportion of referred women who actually attended the service was similar between the special after hours service and the visiting clinicians, and was significantly lower for the integrated STI service (RR 0.54, CI 0.45 to 0.66). Data on women's satisfaction with the service from a sample survey indicated a preference for the visiting special team (RR 0.84, CI 0.72 to 0.99). Costs per patient treated were similar but were lowest for the integrated STI service (Table 17).
10. Additional Table 8: Nyameryekung'e 1997: Tanzania (Cluster RCT of STI service models).
| Category | Measure and unit | Integrated | Vertical (special) |
Difference RR [95% CI] |
| Health care delivery | Cost per patient treated | 11.0 US $ | 11.5 US $ and 12 US $ | Not available |
ii. Community and facility
In Nepal (Tuladhar 1982), family planning and maternal and child health care were provided either through integrated primary health care services or through a vertical family planning, maternal and child health programme. Both approaches included facility based services and community components. Outcomes measured related to the delivery of the family planning programme (current use of contraceptives, knowledge of family planning, and intention to use family planning) and the impact on health status (infant mortality and child survival). The data on family planning showed that there was low overall use, and a secular modest increase between 1975 and 1978, but no difference between the two modes of delivery (Table 6). However, knowledge of family planning was higher in the vertical programme group although intention to use and the mean number of preferred children showed little difference. Infant mortality rates fell in both groups, with a greater reduction in the vertical sites, over the period of study. There was little change in child survivorship, in both sites (Table 18).
11. Additional Table 9:Tuladhar 1982: Nepal (CBA of integrated family planning and maternal and child health programme).
| Category | Measure and unit |
Integrated (Pre to post measure of change) |
Vertical (Pre to post measure of change) |
| Health care delivery | Ever used FP | 3% to 6%. Change +3% (94/3207 to 220/3667) |
3% to 6%. Change +3% (83/2769 to 202/3368) |
| Behavioural outcomes | Intention to use FP | 17% to 11%. Change ‐6% (3186/18741 to 3654/33218) |
16% to 14%. Change ‐2% (2737/17106 to 3364/24028) |
| Behavioural outcomes | Mean number of preferred children | 4.0 to 3.8 Change ‐0.2 |
3.8 to 3.5 Change ‐0.3 |
The Taylor 1987 family planning study also compared the integrated package of family planning, child and women’s health to three vertical style programmes of child health and family planning; women’s health and family planning; and family planning education alone. Although family planning acceptance increased in all intervention sites, the levels of increase were similar at the different sites (Table 6). However, serious limitations in study design makes the evidence of effect uncertain. The effects on children's and women’s health were not reported. The integrated package was reported to be more cost‐effective than the single interventions in achieving family planning outcomes including uptake, years of protection, and births averted (Table 15).
In the nutrition arm of the Taylor 1987 study, a comparison was made of an integrated package of nutrition and health care for infectious diseases to a nutrition intervention alone, and health care for infectious diseases alone. Child and infant mortality rates were decreased with all three intervention packages, compared to controls, but no difference was found between the single and combined interventions (Table 6, Table 16). However, serious limitations in study design makes the evidence of effect uncertain. Comparisons of morbidity outcomes between the intervention packages were not reported.
In Zimbabwe, Gregson 2007 evaluated a complex intervention which included facility and community based activities implemented over a three year period to improve HIV control. The activities included peer education and condom distribution to targeted groups, strengthened STI services, clinic open days with HIV/AIDS information, education and communication, and income generating projects. A wide range of outcomes was reported, many of which demonstrated little or no effect of the intervention. Positive changes that were noted included improved STI treatment effectiveness in men (self reported) (prevalence odds ratio (POR) 2.49, CI 1.22 to 5.10), and improved HIV/AIDS knowledge in men (POR 1.30, CI 1.08 to 1.55). This was not accompanied by behavioural changes, however, with no evidence of an effect on multiple casual partners (POR 1.13, CI 0.88 to 1.46) and an increase in reported unprotected sex with casual partners for men (POR 1.46, CI 1.02 to 2.09) and women (POR 6.51, CI 2.14 to 19.82). There was no change in health seeking behaviour in men or women, and no effect on reported STI (POR 1.41, CI 0.94 to 2.12) in men or women (POR 1.10, CI 0.9 to 1.35) or HIV incidence in the study population (IRR 1.27, CI 0.92 to 1.75) (Table 7, Table 19).
12. Additional Table 12: Gregson 2007: Zimbabwe (Cluster RCT of integrated community HIV prevention with clinic services).
| Outcome Category | Measure and unit |
Integration |
Control |
Difference POR (95% CI) |
| Behavioural outcomes | HIV/AIDS knowledge index, score above media | Males 55% (589/1068) Females 49% (790/1615) |
Males 48% (506/1064) Females 47% (719/1526) |
1.30 (1.08‐1.55) 1.10 (0.95‐1.27) |
| Multiple casual partners in past 3 years | Males 30% (299/1009) Females 4% (58/1438) |
Males 27% (258/963) Females 4% (50/1339) |
1.13 (0.88‐1.46) 1.61 (0.97‐2.66) |
|
| Unprotected sex with casual partners in past 3 years | Males 79% (382/486) Females 94% (128/1360 |
Males 73% (297/409) Females 79% (108/137) |
1.46 (1.02‐2.09) 6.51 (2.14‐19.82) |
User perspectives of integration
Although user’s knowledge and intentions were assessed in several of the family planning integration studies, user’s views on integrated service delivery were not ascertained. Providers' views, assessed in Huntington 1994, were limited to evaluating the family planning messages and whether this impacted on service uptake.
In the Tanzania study of STI services for women at truck stops (Nyamuryekung'e 1997) , the special STI services (after hours and outreach) were preferred by women, as reflected in attendance rates and a user satisfaction survey of a small sample (Table 5).
Economic evaluations of integration
Two studies included some form of costing or economic evaluation. The methods of the economic evaluations were not described in either of these studies, and very little data were presented. The reported results therefore need to be interpreted with caution. Taylor 1987 reported lower unit costs (cost per acceptor) for combined family planning service delivery, with the integration of family planning, child and women’s health being the most cost effective option (USD35 per estimated birth averted) as compared to family planning education alone (USD107 per estimated birth averted) (Table 15). In the nutrition study of Taylor 1987, integrated health care and nutrition were reported to be the most cost effective in improving growth and psychomotor development .
In the STI services study in Tanzania (Nyamuryekung'e 1997), the cost per patient treated was lower for STI care integrated in the general PHC services (USD11.00 per case) than in the special after hours STI clinics (USD11.5) and special outreach STI clinics (USD12.0) (Table 8). The costing was not however linked to any of the outcome measures to assess cost‐effectiveness of the different approaches. The only conclusion that can be drawn is therefore that the costs per patient treated for an STI in 1997 in Tanzania were lower for integrated STI care than for the special STI services.
Discussion
Summary of main results
After three decades of research on vertical and integrated service delivery there is some evidence of efficiency gains of integration, particularly in family planning integration (Huntington 1994; Mark 2007), HIV testing in TB and STI services (Pope 2008; Leon 2010), and STI treatment effectiveness in integrated HIV control (Gregson 2007). However, there is also evidence that in certain contexts vertical programmes perform better than fully integrated services for STI treatment, and no evidence that integration improves health outcomes. Recent studies have been more rigorous and are producing better quality evidence. However, further well designed studies of different strategies to promote integration, and the effects of integration over a wider range of service areas and settings, are needed.Very limited costing data were available in the studies included in the review, and good quality economic evaluations of integration are needed to assess cost‐effectiveness and the efficiency of service integration.
Add on of services
The results of the studies of service add ons or linkages at a facility level indicate that these interventions probably improve utilisation of services, in particular family planning and HIV counselling and testing. None of these studies, however, provided evidence of improvements in health status outcomes as a result of the add‐on services, and none assessed client satisfaction with add‐on services. The goals of integration include not only improved utilisation and efficiency of delivery of care but also improved patient satisfaction and health status. The absence of evidence of effect on patient satisfaction and health status suggests that some caution is necessary in implementing these interventions as improvements in the ''processes' of healthcare delivery may not translate automatically into improved patient satisfaction and better health outcomes.
The addition of community based interventions for family planning improved family planning uptake, and the addition of community based nutrition and child health interventions improved child nutrition, morbidity and mortality (Taylor 1987). However, the quality of the evidence from the Taylor studies was very low , and the true effect is uncertain. It is also important to note that these additional interventions involved lay health workers providing services in the community, with support from the routine facility based services. Any differences between control and intervention sites may therefore be due to the additional community based services as well as the integration across levels of care, as has been demonstrated elsewhere (Baqui 2008; Bhutta 2008).
Vertical versus integrated service delivery
The study of models of STI care (Nyamuryekung'e 1997) produced results which favoured the delivery of special or vertical services for STIs in the study context.
The preference for and higher utilisation rates of special after hours and outreach STI services by women at truck stops may reflect a desire for privacy and confidentiality as well as better access to STI services at times and places which are more convenient for these users. These findings may be relevant to similar target groups where privacy or confidentiality are an important concern for the service users, and may not be applicable to other types of services. However, the study does indicate that integrated services may not necessarily be the preferred option of all service users.
Of the integration studies which included facility and community components, the Tuladhar 1982 and Taylor 1987 studies of vertical versus integrated family planning services did not demonstrate any differences in health delivery or health status outcomes.
The integrated nutrition and healthcare intervention (Taylor 1987) found no effect on mortality between the single and combined interventions. The main impact on processes of healthcare delivery and health outcomes in the Taylor study therefore appeared to occur through adding on or linking a community based intervention to the routine services. Whether this was delivered as a single focus intervention (for example nutrition or health care alone) or a combined package of two or more interventions appears to have not resulted in any difference in effect on the outcomes measured.
The more recent well designed cluster RCT of a complex integrated community and clinic based HIV control intervention in Zimbabwe (Gregson 2007) found improvements in some health service outcomes, in particular improved STI treatment effectiveness in men. However, improved knowledge of HIV/AIDS in the men did not translate into positive behaviour changes, nor into reduced HIV and STI incidence in the study population. The study also found harmful effects in that both men and women reported increased unprotected sex with casual partners in the intervention sites. The authors explored several reasons for the failure of the intervention to achieve the intended effects. Key factors were the stage of the epidemic, which was on the decline in Zimbabwe; possible contamination by other HIV prevention and control interventions in the control sites; and the limitations of the relatively short follow‐up period to capture long‐term changes.
The three studies of facility and community based integration therefore provide conflicting results, with improved health knowledge and healthcare delivery in vertical sites in Tuladhar 1982, no evidence of effect in Taylor 1987, and mixed results in Gregson 2007. None of these three studies demonstrated an improvement in health status outcomes in the integrated service delivery sites.
Overall completeness and applicability of the evidence
The studies covered a narrow range of service delivery areas, with four of the studies assessing family planning linkages with, or integration into, other services. Other services assessed included nutrition and child health, STI treatment, TB and HIV service integration. Overall, the limited focus of studies of integration probably reflect historical policy pushes. In the 1980s, international policy makers were seeking approaches to integrate family planning programmes with child health (Lush 1999). In the late 1990s, efforts were being made to provide accessible STI services for sex workers; and the World Health Organization has since been promoting a substantive package of interventions for child health, the Integrated Management of Childhood Illnesses (WHO 1997). In the current decade the focus has been on integrating and creating linkages with sexual health, reproductive health, and HIV/AIDS services (WHO/HIV/2008), as well as the integration of TB and HIV/AIDS prevention and care.
The interventions mainly involved changes in delivery arrangements, particularly professional changes such as the training and support of existing health workers to provide additional information or services; or services provided in a different location or by an additional category of health worker. None of the studies assessed interventions which involved financing or governance arrangements to support integrated service delivery.
The actual mechanism of the integration strategy was well described in the more recent studies (Gregson 2007; Mark 2007; Pope 2008; Leon 2010) but vague in several of the earlier studies. In particular the nature of inputs such as the categories of health professionals involved, training provided, duration of the intervention, and any additional resources were poorly specified. The evaluation of integration strategies is difficult because of problems in the development, identification, documentation, and reproduction of the interventions in different settings (Campbell 2000). This is why it is important that the integration strategy (the intervention) be well defined in order to be able to compare similar interventions. Better description of interventions also enables decision‐makers to assess whether the intervention is feasible with the available resources in their settings.
Six of the studies were undertaken in African countries (South Africa, Tanzania, Togo, Zambia, and Zimbabwe) and three in Asian countries (India and Nepal). The evidence from the studies may therefore be more applicable in similar settings in Africa and Asia, but less so in other settings.
The time period during which the studies were implemented and evaluated ranged from four months (Pope 2008) to four years (Taylor 1987). Most of the outcomes assessed tended to be short‐term process outcomes, such as service utilisation and, in a few instances, longer‐term impacts on morbidity and mortality (Gregson 2007; Taylor 1987). Although most of the studies were recent, the Tuladhar (1982) and Taylor (1987) studies were conducted more than two decades ago and this may affect the applicability of these findings.
Studies focused almost exclusively on the provider side, without any consideration of the demand side. Only one of the studies examined user views, and this assessment included only a simple 'yes' or 'no' question about satisfaction with the service, in a small sample survey. No study examined user views around the coherence of the service they were using. One of the often cited reasons for integration is that it improves the service for the communities using it. Indeed, this was our starting point for this review of integration interventions ‐ to assess whether they reduced the service fragmentation experienced by users. The views of potential users are likely to influence strongly whether they use the service or not, and future studies should assess this. This review did not search for or include qualitative studies of user views and these may be an important additional source of data on this issue.
From the provider side, managers expressed concern about overloading staff with multiple tasks, and with the inherent risk of none of the services being delivered particularly well. Studies examining this would help to inform management decisions on integration strategies for particular localities.
Quality of the evidence
A total of nine studies were included in this updated review, adding three RCTs (Mark 2007, Pope 2008, Gregson 2007) and a NRCT (Leon 2010) to the previous evidence. The addition of these recent studies have improved the overall quality of the evidence largely as a result of the improved study designs. The quality of the evidence from these studies were mostly graded as being of moderate or high quality.
By comparison the Tuladhar and the Taylor studies, undertaken three decades ago, were less rigorous. The evidence from these and other previously included studies were graded as low and very low quality using the GRADE approach. The failure to measure any effect in some of these studies may be due partly to numerous biases which were not addressed in the studies. .
Potential biases in the review process
The updated review repeated and extended the earlier search strategy over an extensive range of databases and other sources. The types of studies included in the review were not limited to RCTs, but also included NRCTs, CBAs and ITS studies. There is therefore a high likelihood that all relevant rigorous studies were identified.
The more recently published studies described the study design in detail and reported fully on the data. In earlier studies the description of the study design, the interventions and the reporting of data was incomplete. Study authors were contacted to obtain further information where possible, but to some extent the inclusion, categorisation and assessment of risk of bias for earlier studies may have been biased by poor reporting.
Agreements and disagreements with other studies or reviews
Although integrated health care continues to be advocated for LMICs, there remains a lack of clear evidence of the benefits of integration (Wallace 2009, Atun 2010). This updated review identified additional evidence of the effects of integration in terms of the processes of delivery of PHC. However, the review failed to provide evidence that integrated health care impacts positively on health outcomes. A wide variety of strategies can be used to achieve integration (or linkages), and there are a range of settings within which integration could be applied. Reproductive health, HIV and TB are popular areas for studies on integration and linkages but, as this review has illustrated, the evidence is still inconclusive. This is contrary to the recent WHO/UNFPA/IPPF/UNAIDS/UCSF Policy Brief that claims, based on evidence from an unpublished systematic review, that there are clear benefits to integration (WHO/HIV/2008). A publication based on the same systematic review advocates for linkages whilst concluding that significant gaps in the literature remain (Kennedy 2010).
A shift has now occurred in the debate on integration to identifying the contexts within which either vertical or integrated programmes may be appropriate, and exploring how best to co‐ordinate such programmes with general healthcare services to achieve efficient health service delivery, continuity of care, and optimal health outcomes (Unger 2003; WHO 2005; Lawn 2008; Atun 2010). This shift does begin to address the contextual nature of strategies, which may work for certain diseases in certain populations, and to address the differences between ''add on'' and full integration approaches. However, with the absence of evidence of an effect of full integration of health care, caution needs to be exercised in advocating any one approach above another.
What is emerging is that integration is a very complex and variably understood concept, with terms such as linkages being used interchangeably with integration, resulting in some confusion. Whatever it is called, integration and linkages are difficult to evaluate in the real world settings of health systems in low‐ and middle‐income countries. To date, there is limited evidence of its effectiveness in improving health outcomes, and some evidence to suggest that it may improve efficiency but may not be appropriate in all circumstances.
Authors' conclusions
Implications for practice.
Studies of 'add‐on' services involving discrete interventions at a facility level have been the most successful in demonstrating any benefits in service delivery, but have failed to assess longer‐term health benefits. Studies of more complex integration interventions covering facility and community levels have been least successful in demonstrating any benefits of integration, to service delivery or health outcomes.
Increasingly, health decision makers are becoming aware of the importance of using evidence in policy making, and there is therefore a need for reliable research evidence to assist decision makers (Haines 2004; Lavis 2005).
However, in the absence of clear evidence that integration improves health outcomes, the way to deliver primary healthcare should remain a choice made by governments and non‐government organisations based on logical, common‐sense decisions within local contexts and taking into account budgetary and resource constraints. More importantly, decision makers should be aware that integration may not improve service delivery or health outcomes, and they should establish mechanisms to monitor and evaluate this if they decide to proceed with integration within a particular setting.
Implications for research.
Integration remains on the international policy agenda for primary health care in LMIC. One of the main justifications for integrated care at the point of delivery is to make the service easier to use and more accessible to the communities served. Yet few impact evaluations assess lay views of the service provided. This is a clear gap that should be addressed in future evaluations, using both quantitative and qualitative methods. Such studies should also seek to assess the equity implications of integration of care.
Integration should make the service more economically efficient. However, due to the inadequacies of economic evaluations and reporting in the studies, it is difficult to draw any conclusions on the economic aspects of integration. A more in‐depth analysis of the costs is required to draw any conclusions on the economic efficiency or cost‐effectiveness of integration.
Overall, international policy developments regarding integration provide an opportunity for further research to explore approaches in a variety of contexts. Policy makers and planners considering integration could introduce strategies and, where appropriate, use rigorous study designs to allow unbiased comparisons.
Ideally, they could:
use cluster randomised study design, or rigorous non‐randomised study designs;
conduct studies over a period of several years in order to properly evaluate outcomes and ensure the sustainability of any impacts;
describe carefully the intervention, in terms of how integration was implemented and the inputs needed;
identify a few sensible primary outcomes related to service quality or patient outcomes relevant to the service, such as mortality or vaccination coverage;
assess efficiency and cost‐effectiveness by including good quality economic evaluations;
assess user or lay views of the integrated services.
What's new
| Date | Event | Description |
|---|---|---|
| 21 August 2019 | Amended | A link to a summary for policy‐makers was added to the plain language summary |
History
Protocol first published: Issue 1, 2001 Review first published: Issue 4, 2001
| Date | Event | Description |
|---|---|---|
| 21 November 2010 | New search has been performed | This is an update of a published review which was last updated in 2006. The original review has been split into two reviews and the second review on Integrated Management of Childhood Illness (IMCI) programs will be published separately. |
| 21 November 2010 | New citation required but conclusions have not changed | The 2010 version includes five new studies. One of these five had been previously excluded. We have also now excluded studies evaluating Integrated Management of Childhood Illness (IMCI) and other 'packages of care', which will be covered in a separate review. The latter decision was based on an updated definition of integration which regards packages of care as an intervention which can be delivered vertically with specialised support and resources, or horizontally fully integrated into primary health care (PHC). So the package per se is not a form of integration. The update also incorporates literature related to a new donor word, "linkages". The range of service delivery areas covered in the new review is wider and includes TB, HIV, STI and reproductive health service integration. This reflects the new research. Authorship has changed as all previous authors were not available to conduct the update. |
| 22 February 2006 | New citation required and conclusions have changed | Substantive amendment |
Notes
This review is an update; the original review was first published in Issue 4, 2001 of The Cochrane Library and updated in 2006. The original review has been split into two reviews of which this update is one. The other review "Integrated management of childhood illness programmes in low‐ and middle‐income countries" will be published as a separate review.
Acknowledgements
Jane Briggs and Pierre Capdegelle were authors on the first version of this review, published in 2001. Jane participated in the 2005 update.
Marit Johansen of the Norwegian Knowledge Centre for Health Services developed the search strategy and conducted the literature searches for this update.
We are grateful for the support of the Norwegian Knowledge Centre for Health Services (update); the Department of Reproductive Health and Research (RHR) and the Organization of Health Services Delivery (OSD), World Health Organization, Geneva (original review); and the Department for International Development, UK, as part of the Effective Health Care Research Programme Consortium.
Appendices
Appendix 1. Appendix 1: search strategy
CENTRAL + DARE
#1 MeSH descriptor Delivery of Health Care, Integrated, this term only
#2 MeSH descriptor Comprehensive Health Care, this term only
#3 MeSH descriptor Continuity of Patient Care, this term only
#4 MeSH descriptor Patient‐Centered Care, this term only
#5 (comprehensive NEXT health NEXT care):ti or (comprehensive NEXT health NEXT care):ab
#6 (continuity NEAR/2 care):ti or (continuity NEAR/2 care):ab
#7 (patient NEXT centered NEXT care):ti or (patient NEXT centered NEXT care):ab
#8 (integrat* NEAR/3 (care or service* or delivery or strateg* or program* or management)):ti or (integrat* NEAR/3 (care or service* or delivery or strateg* or program* or management)):ab
#9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8)
#10 MeSH descriptor Delivery of Health Care, this term only
#11 MeSH descriptor Primary Health Care, this term only
#12 MeSH descriptor Ambulatory Care, this term only
#13 MeSH descriptor Health Care Reform, this term only
#14 MeSH descriptor Health Services, this term only
#15 MeSH descriptor Community Health Services, this term only
#16 MeSH descriptor Community Health Nursing, this term only
#17 MeSH descriptor Child Health Services, this term only
#18 MeSH descriptor Women's Health Services, this term only
#19 MeSH descriptor Family Planning Services, this term only
#20 MeSH descriptor Reproductive Health Services, this term only
#21 MeSH descriptor Maternal Health Services, this term only
#22 MeSH descriptor Postnatal Care, this term only
#23 MeSH descriptor Preconception Care, this term only
#24 MeSH descriptor Prenatal Care, this term only
#25 MeSH descriptor Preventive Health Services, this term only
#26 MeSH descriptor Diagnostic Services, this term only
#27 MeSH descriptor Adolescent Health Services, this term only
#28 MeSH descriptor Mental Health Services, this term only
#29 MeSH descriptor Community Mental Health Services, this term only
#30 MeSH descriptor Health Services for the Aged, this term only
#31 MeSH descriptor Health Services, Indigenous, this term only
#32 MeSH descriptor Ambulatory Care Facilities, this term only
#33 MeSH descriptor Mobile Health Units, this term only
#34 MeSH descriptor Rural Health Services, this term only
#35 MeSH descriptor Suburban Health Services, this term only
#36 MeSH descriptor Community Health Centers, this term only
#37 MeSH descriptor Substance Abuse Treatment Centers, this term only
#38 MeSH descriptor Community Mental Health Centers, this term only
#39 MeSH descriptor Child Guidance Clinics, this term only
#40 MeSH descriptor Maternal‐Child Health Centers, this term only
#41 MeSH descriptor Outpatient Clinics, Hospital, this term only
#42 MeSH descriptor Outpatients, this term only
#43 MeSH descriptor Health Promotion, this term only
#44 MeSH descriptor Health Education, this term only
#45 MeSH descriptor Sex Education, this term only
#46 MeSH descriptor Patient Education as Topic, this term only
#47 MeSH descriptor Primary Prevention, this term only
#48 MeSH descriptor Immunization Programs, this term only
#49 MeSH descriptor Mass Immunization, this term only
#50 MeSH descriptor Immunization, this term only
#51 MeSH descriptor Vaccination, this term only
#52 (disease NEXT control NEXT program*):ti or (disease NEXT control NEXT program*):ab
#53 (primary NEAR/3 (care or service* or clinic*)):ti,ab,kw
#54 (outpatient* NEAR/3 (care or service* or clinic*)):ti or (outpatient* NEAR/3 (care or service* or clinic*)):ab
#55 (delivery or ambulatory or postnatal or preconception or prenatal or community) NEAR/3 care:ti or (delivery or ambulatory or postnatal or preconception or prenatal or community) NEAR/3 care:ab
#56 (community or child or children or women* or family or reproductive or maternal or preventive or adolescent or mental or aged or indigenous or rural or suburban) NEAR/3 (health NEXT service*):ti or (community or child or children or women* or family or reproductive or maternal or preventive or adolescent or mental or aged or indigenous or rural or suburban) NEAR/3 (health NEXT service*):ab
#57 (community or abuse or child or children or maternal) NEAR/3 (treatment NEXT center* or health NEXT center* or clinic*):ti or (community or abuse or child or children or maternal) NEAR/3 (treatment NEXT center* or health NEXT center* or clinic*):ab
#58 (health NEXT care NEXT reform* or health NEXT service* or community NEXT health NEXT nursing or family NEXT planning NEXT service* or diagnostic NEXT service* or mobile NEXT health NEXT unit* or health NEXT promotion or health NEXT education or sex* NEXT education or patient NEXT education or primary NEXT prevention or immunization or immunisation or vaccination):ti or (health NEXT care NEXT reform* or health NEXT service* or community NEXT health NEXT nursing or family NEXT planning NEXT service* or diagnostic NEXT service* or mobile NEXT health NEXT unit* or health NEXT promotion or health NEXT education or sex* NEXT education or patient NEXT education or primary NEXT prevention or immunization or immunisation or vaccination):ab
#59 (#10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58)
#60 MeSH descriptor Referral and Consultation, this term only
#61 MeSH descriptor Interinstitutional Relations, this term only
#62 MeSH descriptor Community‐Institutional Relations, this term only
#63 (integrat*):ti or (integrat*):ab
#64 (deliver* NEAR/3 (with or within or together)):ti or (deliver* NEAR/3 (with or within or together)):ab
#65 (bring NEXT together):ti or (bring NEXT together):ab
#66 (horizontal or vertical):ti or (horizontal or vertical):ab
#67 (coordinat*):ti or (coordinat*):ab
#68 (co‐ordinat*):ti or (co‐ordinat*):ab
#69 (link*):ti or (link*):ab
#70 (multi* NEXT team*):ti or (multi* NEXT team*):ab
#71 (multi* NEAR/2 (care or service* or clinic*)):ti or (multi* NEAR/2 (care or service* or clinic*)):ab
#72 (multicare or multiservice* or multiclinic*):ti or (multicare or multiservice* or multiclinic*):ab
#73 (multiskill* or multitask*):ti or (multiskill* or multitask*):ab
#74 (multi NEXT skill* or multi NEXT task*):ti or (multi NEXT skill* or multi NEXT task*):ab
#75 (#60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74)
#76 MeSH descriptor Developing Countries, this term only
#77 MeSH descriptor Medically Underserved Area, this term only
#78 (Africa or Africa South of the Sahara or Asia or South America or Latin America or Central America):ti,ab,kw
#79 (American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libya or Lithuania or Malaysia or Mauritius or Mexico or Micronesia or Montenegro or Oman or Palau or Panama or Poland or Romania or Russia or Seychelles or Slovakia or South Africa or Saint Kitts and Nevis or Saint Lucia or Saint Vincent and the Grenadines or Turkey or Uruguay or Venezuela or Yugoslavia or Guinea or Libia or Libyan or Mayotte or Northern Mariana Islands or Russian Federation or Samoa or Serbia or Slovak Republic or St Kitts and Nevis or St Lucia or St Vincent and the Grenadines):ti,ab,kw
#80 (Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia and Herzegovina or Cameroon or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or Fiji or Georgia (Republic) or Guam or Guatemala or Guyana or Honduras or Indian Ocean Islands or Indonesia or Iran or Iraq or Jamaica or Jordan or Lesotho or Macedonia (Republic) or Marshall Islands or Micronesia or Middle East or Moldova or Morocco or Namibia or Nicaragua or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syria or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or Bosnia or Cape Verde or Gaza or Georgia or Kiribati or Macedonia or Maldives or Marshall Islands or Palestine or Syrian Arab Republic or West Bank):ti,ab,kw
#81 (Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or Democratic Republic of the Congo or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Guinea‐Bissau or Haiti or India or Kenya or Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Somalia or Sudan or Tajikistan or Tanzania or East Timor or Togo or Uganda or Uzbekistan or Vietnam or Yemen or Zambia or Zimbabwe or Burma or Congo or Kyrgyz or Lao or North Korea or Salomon Islands or Sao Tome or Timor or Viet Nam):ti,ab,kw
#82 (rural or remote or nonmetropolitan or underserved or under NEXT served or deprived or shortage) NEXT (communit* or count* or area* or region* or province* or district*):ti or (rural or remote or nonmetropolitan or underserved or under NEXT served or deprived or shortage) NEXT (communit* or count* or area* or region* or province* or district*):ab
#83 (developing or less NEXT developed or third NEXT world or under NEXT developed or poor*) NEXT (communit* or count* or district* or state* or province* or jurisdiction* or nation* or region* or area* or territor*):ti or (developing or less NEXT developed or third NEXT world or under NEXT developed or poor*) NEXT (communit* or count* or district* or state* or province* or jurisdiction* or nation* or region* or area* or territor*):ab
#84 (middle NEXT income or low NEXT income or underserved or under NEXT served or shortage) NEXT (communit* or count* or district* or state* or province* or jurisdiction* or nation* or region* or area* or territor*):ti or (middle NEXT income or low NEXT income or underserved or under NEXT served or shortage) NEXT (communit* or count* or district* or state* or province* or jurisdiction* or nation* or region* or area* or territor*):ab
#85 (lmic or lmics):ti or (lmic or lmics):ab
#86 (#76 OR #77 OR #78 OR #79 OR #80 OR #81 OR #82 OR #83 OR #84 OR #85)
#87 (#9 AND #86)
#88 (#59 AND #75 AND #86)
#89 (#87 OR #88)
MEDLINE (Ovid)
1. Delivery of Health Care, Integrated/
2. Comprehensive Health Care/
3. "Continuity of Patient Care"/
4. Patient‐Centered Care/
5. (integrat$ adj3 (care or service? or delivery or strateg$ or program$ or management)).tw.
6. integrated programs.kw.
7. or/1‐6
8. "Delivery of Health Care"/
9. Primary Health Care/
10. Ambulatory Care/
11. Health Care Reform/
12. Health Services/
13. Community Health Services/
14. Community Health Nursing/
15. Child Health Services/
16. Women's Health Services/
17. Family Planning Services/
18. Reproductive Health Services/
19. Maternal Health Services/
20. Postnatal Care/
21. Preconception Care/
22. Prenatal Care/
23. Preventive Health Services/
24. Diagnostic Services/
25. Adolescent Health Services/
26. Mental Health Services/
27. Community Mental Health Services/
28. Health Services for the Aged/
29. Health Services, Indigenous/
30. Ambulatory Care Facilities/
31. Mobile Health Units/
32. Rural Health Services/
33. Suburban Health Services/
34. Community Health Centers/
35. Substance Abuse Treatment Centers/
36. Community Mental Health Centers/
37. Child Guidance Clinics/
38. Maternal‐Child Health Centers/
39. Outpatient Clinics, Hospital/
40. Outpatients/
41. Health Promotion/
42. Health Education/
43. Sex Education/
44. Patient Education as Topic/
45. Primary Prevention/
46. Immunization Programs/
47. Mass Immunization/
48. Immunization/
49. Vaccination/
50. disease control program?.tw.
51. (primary adj3 (care or service? or clinic?)).tw.
52. primary health care.kw.
53. (outpatient? adj3 (care or service? or clinic?)).tw.
54. or/8‐53
55. "Referral and Consultation"/
56. Interinstitutional Relations/
57. Community‐Institutional Relations/
58. integrat$.tw.
59. (deliver$ adj3 (with or within or together)).tw.
60. bring together.tw.
61. horizontal.tw.
62. vertical.tw.
63. coordinat$.tw.
64. co‐ordinat$.tw.
65. link$.tw.
66. (multi$ adj team?).tw.
67. (multi$ adj2 (care or service? or clinic?)).tw.
68. (multicare or multiservice? or multiclinic?).tw.
69. multiskill$.tw.
70. multi skill$.tw.
71. multitask$.tw.
72. multi task$.tw.
73. or/55‐72
74. Developing Countries/
75. Medically Underserved Area/
76. Africa/ or "Africa South of the Sahara"/ or Asia/ or South America/ or Latin America/ or Central America/
77. (Africa or Asia or South America or Latin America or Central America).tw.
78. (American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libya or Lithuania or Malaysia or Mauritius or Mexico or Micronesia or Montenegro or Oman or Palau or Panama or Poland or Romania or Russia or Seychelles or Slovakia or South Africa or "Saint Kitts and Nevis" or Saint Lucia or "Saint Vincent and the Grenadines" or Turkey or Uruguay or Venezuela or Yugoslavia).mp. or Guinea.tw. or Libia.tw. or libyan.tw. or Mayotte.tw. or Northern Mariana Islands.tw. or Russian Federation.tw. or Samoa.tw. or Serbia.tw. or Slovak Republic.tw. or "St Kitts and Nevis".tw. or St Lucia.tw. or "St Vincent and the Grenadines".tw.
79. (Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or "Bosnia and Herzegovina" or Cameroon or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or Fiji or "Georgia (Republic)" or Guam or Guatemala or Guyana or Honduras or Indian Ocean Islands or Indonesia or Iran or Iraq or Jamaica or Jordan or Lesotho or "Macedonia (Republic)" or Marshall Islands or Micronesia or Middle East or Moldova or Morocco or Namibia or Nicaragua or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syria or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu).mp. or Bosnia.tw. or Cape Verde.tw. or Gaza.tw. or Georgia.tw. or Kiribati.tw. or Macedonia.tw. or Maldives.tw. or Marshall Islands.tw. or Palestine.tw. or Syrian Arab Republic.tw. or West Bank.tw.
80. (Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or "Democratic Republic of the Congo" or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Guinea‐Bissau or Haiti or India or Kenya or Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Somalia or Sudan or Tajikistan or Tanzania or East Timor or Togo or Uganda or Uzbekistan or Vietnam or Yemen or Zambia or Zimbabwe).mp. or Burma.tw. or Congo.tw. or Kyrgyz.tw. or Lao.tw. or North Korea.tw. or Salomon Islands.tw. or Sao Tome.tw. or Timor.tw. or Viet Nam.tw.
81. ((rural or remote or nonmetropolitan or underserved or under served or deprived or shortage) adj (communit$ or count$ or area? or region? or province? or district?)).tw.
82. ((developing or less$ developed or third world or under developed or poor$) adj (communit$ or count$ or district? or state? or province? or jurisdiction? or nation? or region? or area? or territor$)).tw.
83. ((middle income or low income or underserved or shortage) adj (communit$ or count$ or district? or state? or province? or jurisdiction? or nation? or region? or area? or territor$)).tw.
84. (lmic or lmics).tw.
85. or/74‐84
86. randomized controlled trial.pt.
87. random$.tw.
88. intervention$.tw.
89. control$.tw.
90. evaluat$.tw.
91. or/86‐90
92. Animals/
93. Humans/
94. 92 not (92 and 93)
95. (letter or editorial or comment).pt.
96. 95 not (95 and 86)
97. 91 not (94 or 96)
98. 7 and 85 and 97
99. 54 and 73 and 85 and 97
100. 98 or 99
EMBASE (Ovid)
1. Integrated Health Care System/
2. (integrat$ adj3 (care or service? or delivery or strateg$ or program$ or management)).tw.
3. or/1‐2
4. Health Care Delivery/
5. Primary Health Care/
6. Primary Medical Care/
7. Outpatient Care/
8. Ambulatory Care/
9. Ambulatory Care Nursing/
10. Health Service/
11. Community Care/
12. Community Health Nursing/
13. Community Psychiatric Nursing/
14. Community Based Rehabilitation/
15. Community Program/
16. Child Health Care/
17. Newborn Care/
18. Family Service/
19. Family Planning/
20. Birth Control/
21. Maternal Care/
22. Postnatal Care/
23. Perinatal Care/
24. Preventive Health Service/
25. Mental Health Service/
26. Elderly Care/
27. Rural Health Care/
28. Community Mental Health Center/
29. Outpatient Department/
30. Outpatient/
31. exp Health Education/
32. Sexual Education/
33. Primary Prevention/
34. Preventive Health Service/
35. Mass Immunization/
36. Immunization/
37. Vaccination/
38. disease control program?.tw.
39. (primary adj3 (care or service? or clinic?)).tw.
40. (outpatient? adj3 (care or service? or clinic?)).tw.
41. or/4‐40
42. Integration/
43. Patient Referral/
44. integrat$.tw.
45. (deliver$ adj3 (with or within or together)).tw.
46. bring together.tw.
47. horizontal.tw.
48. vertical.tw.
49. coordinat$.tw.
50. co ordinat$.tw.
51. link$.tw.
52. (multi$ adj team?).tw.
53. (multi$ adj2 (care or service? or clinic?)).tw.
54. (multicare or multiservice? or multiclinic?).tw.
55. multiskill$.tw.
56. multi skill$.tw.
57. multitask$.tw.
58. multi task$.tw.
59. or/42‐58
60. Developing Country/
61. Africa/ or "Africa South of the Sahara"/ or Asia/ or "South and Central America"/ or South America/ or Central America/
62. (Africa or Asia or South America or Latin America or Central America).tw.
63. (American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libyan Arab Jamahiriya or Lithuania or Malaysia or Mauritius or Mayotte or Mexico or Northern Mariana Islands or Oman or Palau or Panama or Poland or Romania or Russian Federation or Seychelles or Slovakia or South Africa or "Saint Kitts and Nevis" or Saint Lucia or "Saint Vincent and the Grenadines" or "Turkey (Republic)" or Uruguay or Venezuela or Yugoslavia).mp. or Guinea.tw. or Libya.tw. or Libia.tw. or Libyan.tw. or Montenegro.tw. or Russia.tw. or Samoa.tw. or Serbia.tw. or Slovak Republic.tw. or "St Kitts and Nevis".tw. or "St Lucia".tw. or "St Vincent and the Grenadines".tw. or Turkey.tw.
64. (Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or "Bosnia and Herzegovina" or Cameroon or Cape Verde or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or "Federated States of Micronesia" or Fiji or "Georgia (Republic)" or Guatemala or Guyana or Honduras or Indonesia or Iran or Iraq or Jamaica or Jordan or Kiribati or Lesotho or Maldives or "Macedonia (Republic)" or Marshall Islands or Guam or Moldova or Morocco or Namibia or Nicaragua or Palestine or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syrian Arab Republic or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu).mp. or Bosnia.tw. or Gaza.tw. or Georgia.tw. or Macedonia.tw. or Micronesia.tw. or Syria.tw. or Syrian.tw. or West Bank.tw.
65. (Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or "Democratic Republic Congo" or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Guinea‐Bissau or Haiti or India or Kenya or North Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Solomon Islands or Somalia or Sudan or Tajikistan or Tanzania or Timor‐Leste or Togo or Uganda or Uzbekistan or Viet Nam or Yemen or Zambia or Zimbabwe).mp. or Burma.tw. or Congo.tw. or Kyrgyz.tw. or Lao.tw. or Sao Tome.tw. or Timor.tw. or Vietnam.tw.
66. ((rural or remote or nonmetropolitan or underserved or under served or deprived or shortage) adj (communit$ or count$ or area? or region? or province? or district?)).tw.
67. ((developing or less$ developed or third world or under developed or poor$) adj (communit$ or count$ or district? or state? or province? or jurisdiction? or nation? or region? or area? or territor$)).tw.
68. ((middle income or low income or underserved or shortage) adj (communit$ or count$ or district? or state? or province? or jurisdiction? or nation? or region? or area? or territor$)).tw.
69. (lmic or lmics).tw.
70. or/60‐69
71. Randomized Controlled Trial/
72. Time Series Analysis/
73. random$.tw.
74. (time adj series).tw.
75. (pre test or pretest or post test or posttest).tw.
76. control$.tw.
77. intervention$.tw.
78. evaluat$.tw.
79. experiment$.tw.
80. impact.tw.
81. chang$.tw.
82. effect?.tw.
83. compar$.tw.
84. or/71‐83
85. nonhuman/
86. 84 not 85
87. 3 and 70 and 86
88. 41 and 59 and 70 and 86
89. 87 or 88
CINAHL (EBSCO)
| S87 | S85 and S86 |
| S86 | EM 200806‐ |
| S85 | S83 or S84 |
| S84 | S44 and S62 and S75 and S82 |
| S83 | S5 and S75 and S82 |
| S82 | S76 or S77 or S78 or S79 or S80 or S81 |
| S81 | TI ( random* or control* or experiment* or chang* or compar* or impact or intervention* or evaluat* or effect* or "time series" or "pre test" or "post test" or pretest or posttest ) or AB ( random*control* or experiment* or chang* or compar* or impact or intervention* or evaluat* or effect* or "time series" or "pre test" or "post test" or pretest or posttest ) |
| S80 | PT clinical trial |
| S79 | (MH "Comparative Studies") |
| S78 | (MH "Quasi‐Experimental Studies+") |
| S77 | (MH "Pretest‐Posttest Design+") |
| S76 | (MH "Clinical Trials") |
| S75 | S63 or S64 or S65 or S66 or S67 or S68 or S69 or S70 or S71 or S72 or S73 or S74 |
| S74 | TI ( "developing country" or "developing countries" or "developing nation" or "developing nations" or less* W1 "developed country" or less* W1 "developed countries" or less* W1 "developed nation" or less* W1 "developed nations" or "third world" or "under developed" or "middle income" or "low income" or "underserved country" or "underserved countries" or "underserved nation" or "underserved nations" or "under served country" or "under served countries" or "under served nation" or "under served nations" or "underserved population" or "underserved populations" or "under served population" or "under served populations" or "deprived country" or "deprived countries" or "deprived nation" or "deprived nations" or poor* W1 country or poor* W1 countries or poor* W1 nation* or poor* W1 population* or lmic or lmics ) or AB ( "developing country" or "developing countries" or "developing nation" or "developing nations" or less* W1 "developed country" or less* W1 "developed countries" or less* W1 "developed nation" or less* W1 "developed nations" or "third world" or "under developed" or "middle income" or "low income" or "underserved country" or "underserved countries" or "underserved nation" or "underserved nations" or "under served country" or "under served countries" or "under served nation" or "under served nations" or "underserved population" or "underserved populations" or "under served population" or "under served populations" or "deprived country" or "deprived countries" or "deprived nation" or "deprived nations" or poor* W1 country or poor* W1 countries or poor* W1 nation* or poor* W1 population* or lmic or lmics ) |
| S73 | MW ( Afghanistan or Bangladesh or Benin or "Burkina Faso" or Burundi or Cambodia or "Central African Republic" or Chad or Comoros or Congo or "Cote d'Ivoire" or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Haiti or India or Kenya or Korea or Kyrgyz or Kyrgyzstan or Lao or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Burma or Myanmar or Nepal or Niger or Nigeria or Pakistan or Rwanda or "Salomon Islands" or "Sao Tome" or Senegal or "Sierra Leone" or Somalia or Sudan or Tajikistan or Tanzania or Timor or Togo or Uganda or Uzbekistan or Vietnam or "Viet Nam" or Yemen or Zambia or Zimbabwe ) or TI ( Afghanistan or Bangladesh or Benin or "Burkina Faso" or Burundi or Cambodia or "Central African Republic" or Chad or Comoros or Congo or "Cote d'Ivoire" or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Haiti or India or Kenya or Korea or Kyrgyz or Kyrgyzstan or Lao or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Burma or Myanmar or Nepal or Niger or Nigeria or Pakistan or Rwanda or "Salomon Islands" or "Sao Tome" or Senegal or "Sierra Leone" or Somalia or Sudan or Tajikistan or Tanzania or Timor or Togo or Uganda or Uzbekistan or Vietnam or "Viet Nam" or Yemen or Zambia or Zimbabwe ) or AB ( Afghanistan or Bangladesh or Benin or "Burkina Faso" or Burundi or Cambodia or "Central African Republic" or Chad or Comoros or Congo or "Cote d'Ivoire" or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Haiti or India or Kenya or Korea or Kyrgyz or Kyrgyzstan or Lao or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Burma or Myanmar or Nepal or Niger or Nigeria or Pakistan or Rwanda or "Salomon Islands" or "Sao Tome" or Senegal or "Sierra Leone" or Somalia or Sudan or Tajikistan or Tanzania or Timor or Togo or Uganda or Uzbekistan or Vietnam or "Viet Nam" or Yemen or Zambia or Zimbabwe ) |
| S72 | MW ( Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or "Cape Verde" or Cameroon or China or Colombia or Congo or Cuba or Djibouti or "Dominican Republic" or Ecuador or Egypt or "El Salvador" or Fiji or Gaza or Georgia or Guam or Guatemala or Guyana or Honduras or "Indian Ocean Islands" or Indonesia or Iran or Iraq or Jamaica or Jordan or Kiribati or Lesotho or Macedonia or Maldives or "Marshall Islands" or Micronesia or "Middle East" or Moldova or Morocco or Namibia or Nicaragua or Palestin* or Paraguay or Peru or Philippines or Samoa or "Sri Lanka" or Suriname or Swaziland or Syria or "Syrian Arab Republic" or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or "West Bank" ) or TI ( Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or "Cape Verde" or Cameroon or China or Colombia or Congo or Cuba or Djibouti or "Dominican Republic" or Ecuador or Egypt or "El Salvador" or Fiji or Gaza or Georgia or Guam or Guatemala or Guyana or Honduras or "Indian Ocean Islands" or Indonesia or Iran or Iraq or Jamaica or Jordan or Kiribati or Lesotho or Macedonia or Maldives or "Marshall Islands" or Micronesia or "Middle East" or Moldova or Morocco or Namibia or Nicaragua or Palestin* or Paraguay or Peru or Philippines or Samoa or "Sri Lanka" or Suriname or Swaziland or Syria or "Syrian Arab Republic" or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or "West Bank" Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or "Cape Verde" or Cameroon or China or Colombia or Congo or Cuba or Djibouti or "Dominican Republic" or Ecuador or Egypt or "El Salvador" or Fiji or Gaza or Georgia or Guam or Guatemala or Guyana or Honduras or "Indian Ocean Islands" or Indonesia or Iran or Iraq or Jamaica or Jordan or Kiribati or Lesotho or Macedonia or Maldives or "Marshall Islands" or Micronesia or "Middle East" or Moldova or Morocco or Namibia or Nicaragua or Palestin* or Paraguay or Peru or Philippines or Samoa or "Sri Lanka" or Suriname or Swaziland or Syria or "Syrian Arab Republic" or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or "West Bank" ) or AB ( Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or "Cape Verde" or Cameroon or China or Colombia or Congo or Cuba or Djibouti or "Dominican Republic" or Ecuador or Egypt or "El Salvador" or Fiji or Gaza or Georgia or Guam or Guatemala or Guyana or Honduras or "Indian Ocean Islands" or Indonesia or Iran or Iraq or Jamaica or Jordan or Kiribati or Lesotho or Macedonia or Maldives or "Marshall Islands" or Micronesia or "Middle East" or Moldova or Morocco or Namibia or Nicaragua or Palestin* or Paraguay or Peru or Philippines or Samoa or "Sri Lanka" or Suriname or Swaziland or Syria or "Syrian Arab Republic" or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or "West Bank" ) |
| S71 | MW ( "American Samoa" or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or "Costa Rica" or Croatia or Dominica or Guinea or Gabon or Grenada or Grenadines or Hungary or Kazakhstan or Latvia or Lebanon or Libia or libyan or Libya or Lithuania or Malaysia or Mauritius or Mayotte or Mexico or Micronesia or Montenegro or Nevis or "Northern Mariana Islands" or Oman or Palau or Panama or Poland or Romania or Russia or "Russian Federation" or Samoa or "Saint Lucia" or "St Lucia" or "Saint Kitts" or "St Kitts" or "Saint Vincent" or "St Vincent" or Serbia or Seychelles or Slovakia or "Slovak Republic" or "South Africa" or Turkey or Uruguay or Venezuela or Yugoslavia ) or TI ( "American Samoa" or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or "Costa Rica" or Croatia or Dominica or Guinea or Gabon or Grenada or Grenadines or Hungary or Kazakhstan or Latvia or Lebanon or Libia or libyan or Libya or Lithuania or Malaysia or Mauritius or Mayotte or Mexico or Micronesia or Montenegro or Nevis or "Northern Mariana Islands" or Oman or Palau or Panama or Poland or Romania or Russia or "Russian Federation" or Samoa or "Saint Lucia" or "St Lucia" or "Saint Kitts" or "St Kitts" or "Saint Vincent" or "St Vincent" or Serbia or Seychelles or Slovakia or "Slovak Republic" or "South Africa" or Turkey or Uruguay or Venezuela or Yugoslavia ) or AB ( "American Samoa" or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or "Costa Rica" or Croatia or Dominica or Guinea or Gabon or Grenada or Grenadines or Hungary or Kazakhstan or Latvia or Lebanon or Libia or libyan or Libya or Lithuania or Malaysia or Mauritius or Mayotte or Mexico or Micronesia or Montenegro or Nevis or "Northern Mariana Islands" or Oman or Palau or Panama or Poland or Romania or Russia or "Russian Federation" or Samoa or "Saint Lucia" or "St Lucia" or "Saint Kitts" or "St Kitts" or "Saint Vincent" or "St Vincent" or Serbia or Seychelles or Slovakia or "Slovak Republic" or "South Africa" or Turkey or Uruguay or Venezuela or Yugoslavia ) |
| S70 | TI ( Africa or Asia or "South America" or "Latin America" or "Central America" ) or AB ( Africa or Asia or "South America" or "Latin America" or "Central America" ) |
| S69 | (MH "Asia+") |
| S68 | (MH "West Indies+") |
| S67 | (MH "South America+") |
| S66 | (MH "Latin America") |
| S65 | (MH "Central America+") |
| S64 | (MH "Africa+") |
| S63 | (MH "Developing Countries") |
| S62 | S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54 or S55 or S56 or S57 or S58 or S59 or S60 or S61 |
| S61 | TI multi W1 task* or AB multi W1 task* |
| S60 | TI multitask* or AB multitask* |
| S59 | TI multi W1 skill* or AB multi W1 skill* |
| S58 | TI multiskill* or AB multiskill* |
| S57 | TI ( multicare or multiservice* or multiclinic* ) or AB ( multicare or multiservice* or multiclinic* ) |
| S56 | TI ( multi* N2 care or multi* N2 service* or multi* N2 clinic* ) or AB ( multi* N2 care or multi* N2 service* or multi* N2 clinic* ) |
| S55 | TI multi* W1 team* or AB multi* W1 team* |
| S54 | TI co W1 ordinat* or AB co W1 ordinat* |
| S53 | TI coordinat* or AB coordinat* |
| S52 | TI vertical or AB vertical |
| S51 | TI horizontal or AB horizontal |
| S50 | TI "bring together" or AB "bring together" |
| S49 | TI ( deliver* N3 with or deliver* N3 within or deliver* N3 together ) or AB ( deliver* N3 with or deliver* N3 within or deliver* N3 together ) |
| S48 | TI integrat* or AB integrat* |
| S47 | (MH "Community‐Institutional Relations") |
| S46 | (MH "Interinstitutional Relations") |
| S45 | (MH "Referral and Consultation") |
| S44 | S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 |
| S43 | TI ( outpatient* N3 care or outpatient* N3 service* or outpatient* N3 clinic* ) or AB ( outpatient* N3 care or outpatient* N3 service* or outpatient* N3 clinic* ) |
| S42 | TI ( primary N3 care or primary N3 service* or primary N3 clinic* ) or AB ( primary N3 care or primary N3 service* or primary N3 clinic* ) |
| S41 | TI "disease control" W1 program* or AB "disease control" W1 program* |
| S40 | (MH "Immunization") |
| S39 | (MH "Immunization Programs") |
| S38 | (MH "HIV Education") |
| S37 | (MH "Diabetes Education") |
| S36 | (MH "Patient Education") |
| S35 | (MH "Sex Education") |
| S34 | (MH "Health Education") |
| S33 | (MH "Breast Feeding Promotion") |
| S32 | (MH "Health Promotion") |
| S31 | (MH "Outpatient Service") |
| S30 | (MH "Outpatients") |
| S29 | (MH "Community Health Nursing") |
| S28 | (MH "Community Health Centers") |
| S27 | (MH "Rural Health Services") |
| S26 | (MH "Mobile Health Units") |
| S25 | (MH "Ambulatory Care Facilities") |
| S24 | (MH "Health Services, Indigenous") |
| S23 | (MH "Health Services for the Aged") |
| S22 | (MH "Community Mental Health Services") |
| S21 | (MH "Mental Health Services") |
| S20 | (MH "Adolescent Health Services") |
| S19 | (MH "Diagnostic Services") |
| S18 | (MH "Preventive Health Care") |
| S17 | (MH "Prenatal Care") |
| S16 | (MH "Prepregnancy Care") |
| S15 | (MH "Postnatal Care") |
| S14 | (MH "Maternal Health Services") |
| S13 | (MH "Family Planning") |
| S12 | (MH "Women's Health Services") |
| S11 | (MH "Community Health Services") |
| S10 | (MH "Health Services") |
| S9 | (MH "Health Care Reform") |
| S8 | (MH "Ambulatory Care") |
| S7 | (MH "Primary Health Care") |
| S6 | (MH "Health Care Delivery") |
| S5 | S1 or S2 or S3 or S4 |
| S4 | TI ( integrat* N3 care or integrat* N3 service* or integrat* N3 delivery or integrat* N3 strateg* or integrat* N3 program* or integrat* N3 management ) or AB ( integrat* N3 care or integrat* N3 service* or integrat* N3 delivery or integrat* N3 strateg* or integrat* N3 program* or integrat* N3 management ) |
| S3 | (MH "Patient Centered Care") |
| S2 | (MH "Continuity of Patient Care") |
| S1 | (MH "Health Care Delivery, Integrated") |
Sociological Abstracts & Social Services Abstracts
(KW=primary health care or KW=primary care or KW=health care or KW=patient care or KW=patient centred care or KW=patient centered care or KW=ambulatory care or KW=community care or KW=family planning or KW=postnatal care or KW=prenatal care or KW=preconception care or KW=preventive care or KW=primary prevention or KW=health service* or KW=care service* or KW=diagnostic care or KW=care facility or KW=health facility or KW=care facilities or KW=health facilities or KW=health center* or KW=treatment center* or KW=health clinic* or KW=outpatient* or KW=health promotion or KW=health education or KW=sex* education or KW=patient education or KW=immunization or KW=immunisation or KW=vaccination or KW=disease control program*) and(TI=integrat* or AB=integrat* or KW=delivery system* or KW=integrated delivery system* or KW=interdisciplinary approach* or KW=coordinat* or KW=co ordinat* or KW=vertical or KW=horizontal or KW=link* or KW=multi team* or KW=multiteam* or KW=multi task* or KW=multitask* or KW=multi skill* or KW=multiskill* or KW=multicare* or KW=multiservice* or KW=multiclinic* or KW=multi care* or KW=multi service* or KW=multi clinic*) and((KW=(Developing Countries or Africa or Asia or South America or Latin America or Central America)) or(KW=(American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libya or Lithuania or Malaysia or Mauritius or Mexico or Micronesia or Montenegro or Oman or Palau or Panama or Poland or Romania or Russia or Seychelles or Slovakia or South Africa or Saint Kitts or Nevis or Saint Lucia or Saint Vincent or Grenadines or Turkey or Uruguay or Venezuela or Yugoslavia or Guinea or Libia or Libyan or Mayotte or Northern Mariana Islands or Russian Federation or Samoa or Serbia or Slovak Republic or St Kitts or St Lucia or St Vincent)) or(KW=(Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Cameroon or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or Fiji or Georgia or Guam or Guatemala or Guyana or Honduras or Indian Ocean Islands or Indonesia or Iran or Iraq or Jamaica or Jordan or Lesotho or Macedonia or Marshall Islands or Micronesia or Middle East or Moldova or Morocco or Namibia or Nicaragua or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syria or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or Cape Verde or Gaza or Kiribati or Maldives or Palestine or Syrian Arab Republic or West Bank)) or(KW=(Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or Congo or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Haiti or India or Kenya or Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Somalia or Sudan or Tajikistan or Tanzania or Timor Togo or Uganda or Uzbekistan or Vietnam or Yemen or Zambia or Zimbabwe or Burma or Kyrgyz or Lao or North Korea or Salomon Islands or Sao Tome or Viet Nam)) or(KW=(rural or remote or nonmetropolitan or underserved or under served or deprived or shortage) within 1 (communit* or count* or area* or region* or province* or district*)) or(KW=(developing or less* developed or third world or under developed or poor*) within 1 (communit* or count* or district* or state* or province* or jurisdiction* or nation* or region* or area* or territory*)) or(KW=(middle income or low income or underserved or shortage) within 1 (communit* or count* or district* or state* or province* or jurisdiction* or nation* or region* or area* or territory*)) or(KW=(lmic or lmics))) and(KW=random* or KW=intervention* or KW=control* or KW=evaluat* or KW=time series or KW=quasi experiment* or KW=pre test or KW=pretest or KW=post test or KW=posttest or KW=effect*)
POPLINE (Advanced search)
1. Title/Keyword:
(integrat* w2 program* / integrat* w2 care / integrat* w2 service* / integrat* w2 delivery / integrat* w2 strateg* / integrat* w2 management) & (random* / control* / compare* / intervention* / evaluat* / effect* / experiment* / impact / chang* / pre test / pretest / post test / posttest / pre‐post tests / time series) AND Year (2005 / 2006 / 2007 / 2008 / 2009 / 2010)
OR
2. Title/Keyword:
(primary w2 care / primary w2 service* / healthcare / health care / outpatient*) & (integrat* / coordinat* / co ordinat* / seamless) & (random* / control* / evaluat* / intervention* / comparative stud* / pre test / pretest / post test / posttest / pre‐post tests / time series) AND Year (2005 / 2006 / 2007 / 2008 / 2009 / 2010)
International Bibliography of the Social Sciences
#30 #4 and #7 and #24 and #29
#29 #25 or #26 or #27 or #28
#28 (development studies) in DE
#27 ((random*) or (clinical near1 trial) or (intervention*) or (control*) or (evaluat*) or (time series) or (pre test) or (pretest) or (post test) or (posttest) or (effect*) or (experiment*) or (impact) or (compare*)) in AB
#26 ((random*) or (clinical near1 trial) or (intervention*) or (control*) or (evaluat*) or (time series) or (pre test) or (pretest) or (post test) or (posttest) or (effect*) or (experiment*) or (impact) or (compare*)) in TI
#25 ((random*) or (clinical near1 trial) or (intervention*) or (control*) or (evaluat*) or (time series) or (pre test) or (pretest) or (post test) or (posttest) or (effect*) or (experiment*) or (impact) or (compare*)) in DE
#24 #11 or #15 or #19 or #23
#23 #20 or #21 or #22
#22 ((developing countr*) or (Africa) or (Asia) or (South America) or (Latin America) or (Central Amedica) or (rural) or (remote) or (nonmetropolitan) or (non metropolitan) or (underserved) or (under served) or (deprived) or (shortage) or (less* developed) or (third world) or (under developed) or (poor*) or (middle income) or (low income) or (lmic) or (lmics)) in AB
#21 ((developing countr*) or (Africa) or (Asia) or (South America) or (Latin America) or (Central Amedica) or (rural) or (remote) or (nonmetropolitan) or (non metropolitan) or (underserved) or (under served) or (deprived) or (shortage) or (less* developed) or (third world) or (under developed) or (poor*) or (middle income) or (low income) or (lmic) or (lmics)) in TI
#20 ((developing countr*) or (Africa) or (Asia) or (South America) or (Latin America) or (Central Amedica) or (rural) or (remote) or (nonmetropolitan) or (non metropolitan) or (underserved) or (under served) or (deprived) or (shortage) or (less* developed) or (third world) or (under developed) or (poor*) or (middle income) or (low income) or (lmic) or (lmics)) in DE
#19 #16 or #17 or #18
#18 (Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or Congo or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Guinea Bissau or Haiti or India or Kenya or Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Somalia or Sudan or Tajikistan or Tanzania or East Timor or Togo or Uganda or Uzbekistan or Vietnam or Yemen or Zambia or Zimbabwe or Burma or Kyrgyz or Lao or North Korea or Salomon Islands or Sao Tome or Timor or Viet Nam) in AB
#17 (Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or Congo or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Guinea Bissau or Haiti or India or Kenya or Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Somalia or Sudan or Tajikistan or Tanzania or East Timor or Togo or Uganda or Uzbekistan or Vietnam or Yemen or Zambia or Zimbabwe or Burma or Kyrgyz or Lao or North Korea or Salomon Islands or Sao Tome or Timor or Viet Nam) in TI
#16 (Afghanistan or Bangladesh or Benin or Burkina Faso or Burundi or Cambodia or Central African Republic or Chad or Comoros or Congo or Cote d'Ivoire or Eritrea or Ethiopia or Gambia or Ghana or Guinea or Guinea Bissau or Haiti or India or Kenya or Korea or Kyrgyzstan or Laos or Liberia or Madagascar or Malawi or Mali or Mauritania or Melanesia or Mongolia or Mozambique or Myanmar or Nepal or Niger or Nigeria or Pakistan or Papua New Guinea or Rwanda or Senegal or Sierra Leone or Somalia or Sudan or Tajikistan or Tanzania or East Timor or Togo or Uganda or Uzbekistan or Vietnam or Yemen or Zambia or Zimbabwe or Burma or Kyrgyz or Lao or North Korea or Salomon Islands or Sao Tome or Timor or Viet Nam) in DE
#15 #12 or #13 or #14
#14 (Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or Cameroon or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or Fiji or Georgia or Guam or Guatemala or Guyana or Honduras or Indian Ocean Islands or Indonesia or Iran or Iraq or Jamaica or Jordan or Lesotho or Macedonia or Marshall Islands or Micronesia or Middle East or Moldova or Morocco or Namibia or Nicaragua or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syria or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or Cape Verde or Gaza or Kiribati or Maldives or Palestine or Syrian Arab Republic or West Bank) in AB
#13 (Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or Cameroon or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or Fiji or Georgia or Guam or Guatemala or Guyana or Honduras or Indian Ocean Islands or Indonesia or Iran or Iraq or Jamaica or Jordan or Lesotho or Macedonia or Marshall Islands or Micronesia or Middle East or Moldova or Morocco or Namibia or Nicaragua or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syria or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or Cape Verde or Gaza or Kiribati or Maldives or Palestine or Syrian Arab Republic or West Bank) in TI
#12 (Albania or Algeria or Angola or Armenia or Azerbaijan or Belarus or Bhutan or Bolivia or Bosnia or Herzegovina or Cameroon or China or Colombia or Congo or Cuba or Djibouti or Dominican Republic or Ecuador or Egypt or El Salvador or Fiji or Georgia or Guam or Guatemala or Guyana or Honduras or Indian Ocean Islands or Indonesia or Iran or Iraq or Jamaica or Jordan or Lesotho or Macedonia or Marshall Islands or Micronesia or Middle East or Moldova or Morocco or Namibia or Nicaragua or Paraguay or Peru or Philippines or Samoa or Sri Lanka or Suriname or Swaziland or Syria or Thailand or Tonga or Tunisia or Turkmenistan or Ukraine or Vanuatu or Cape Verde or Gaza or Kiribati or Maldives or Palestine or Syrian Arab Republic or West Bank) in DE
#11 #8 or #9 or #10
#10 (American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libya or Lithuania or Malaysia or Mauritius or Mexico or Micronesia or Montenegro or Oman or Palau or Panama or Poland or Romania or Russia or Seychelles or Slovakia or South Africa or Saint Kitts or Nevis or Saint Lucia or "Saint Vincent and the Grenadines" or Turkey or Uruguay or Venezuela or Yugoslavia Guinea or Libia or Libyan or Mayotte or Northern Mariana Islands or Russian Federation or Samoa or Serbia or Slovak Republic or St Kitts or St Lucia or St Vincent or Grenadines) in AB
#9 (American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libya or Lithuania or Malaysia or Mauritius or Mexico or Micronesia or Montenegro or Oman or Palau or Panama or Poland or Romania or Russia or Seychelles or Slovakia or South Africa or Saint Kitts or Nevis or Saint Lucia or "Saint Vincent and the Grenadines" or Turkey or Uruguay or Venezuela or Yugoslavia Guinea or Libia or Libyan or Mayotte or Northern Mariana Islands or Russian Federation or Samoa or Serbia or Slovak Republic or St Kitts or St Lucia or St Vincent or Grenadines) in TI
#8 (American Samoa or Argentina or Belize or Botswana or Brazil or Bulgaria or Chile or Comoros or Costa Rica or Croatia or Dominica or Equatorial Guinea or Gabon or Grenada or Hungary or Kazakhstan or Latvia or Lebanon or Libya or Lithuania or Malaysia or Mauritius or Mexico or Micronesia or Montenegro or Oman or Palau or Panama or Poland or Romania or Russia or Seychelles or Slovakia or South Africa or Saint Kitts or Nevis or Saint Lucia or "Saint Vincent and the Grenadines" or Turkey or Uruguay or Venezuela or Yugoslavia Guinea or Libia or Libyan or Mayotte or Northern Mariana Islands or Russian Federation or Samoa or Serbia or Slovak Republic or St Kitts or St Lucia or St Vincent or Grenadines) in DE
#7 #5 or #6
#6 ((integrat*) or (delivery near system*) or (deliver* near2 within) or (deliver* near2 together) or (bring adj together) or (interdisciplinary) or (coordinat*) or (co‐ordinat*) or (vertical) or (horizontal) or (link*) or (multi near2 team*) or (multiteam*) or (multi near2 task*) or (multitask*) or (multi near2 skill*) or (multiskill*) or (multicare*) or (multiservice*) or (multiclinic*) or (multi near2 care*) or (multi near2 service*) or (multi near2 clinic*)) in AB
#5 ((integrat*) or (delivery near system*) or (deliver* near2 within) or (deliver* near2 together) or (bring adj together) or (interdisciplinary) or (coordinat*) or (co‐ordinat*) or (vertical) or (horizontal) or (link*) or (multi near2 team*) or (multiteam*) or (multi near2 task*) or (multitask*) or (multi near2 skill*) or (multiskill*) or (multicare*) or (multiservice*) or (multiclinic*) or (multi near2 care*) or (multi near2 service*) or (multi near2 clinic*)) in TI
#4 #1 or #2 or #3
#3 ((primary near2 care) or (primary near2 service*) or (health near2 care) or (health adj service*) or (patient near care) or (ambulatory adj care) or (ambulatory adj service*) or (community adj care) or (family adj planning) or (postnatal adj care) or (prenatal adj care) or (preconception adj care) or (preventive adj care) or (preventive adj service*) or (primary adj prevention) or (care adj service*) or (diagnostic adj care) or (diagnostic adj service*) or (care adj facility) or (health adj facility) or (care adj facilities) or (health adj facilities) or (health near2 center*) or (treatment near2 center*) or (health near2 clinic*) or (outpatient*) or (health adj promotion) or (health adj education) or (sex* adj education) or (patient adj education) or (immunization) or (immunisation) or (vaccination) or (disease near2 program*)) in AB
#2 ((primary near2 care) or (primary near2 service*) or (health near2 care) or (health adj service*) or (patient near care) or (ambulatory adj care) or (ambulatory adj service*) or (community adj care) or (family adj planning) or (postnatal adj care) or (prenatal adj care) or (preconception adj care) or (preventive adj care) or (preventive adj service*) or (primary adj prevention) or (care adj service*) or (diagnostic adj care) or (diagnostic adj service*) or (care adj facility) or (health adj facility) or (care adj facilities) or (health adj facilities) or (health near2 center*) or (treatment near2 center*) or (health near2 clinic*) or (outpatient*) or (health adj promotion) or (health adj education) or (sex* adj education) or (patient adj education) or (immunization) or (immunisation) or (vaccination) or (disease near2 program*)) in TI
#1 ((primary near2 care) or (primary near2 service*) or (health near2 care) or (health adj service*) or (patient near care) or (ambulatory adj care) or (ambulatory adj service*) or (community adj care) or (family adj planning) or (postnatal adj care) or (prenatal adj care) or (preconception adj care) or (preventive adj care) or (preventive adj service*) or (primary adj prevention) or (care adj service*) or (diagnostic adj care) or (diagnostic adj service*) or (care adj facility) or (health adj facility) or (care adj facilities) or (health adj facilities) or (health near2 center*) or (treatment near2 center*) or (health near2 clinic*) or (outpatient*) or (health adj promotion) or (health adj education) or (sex* adj education) or (patient adj education) or (immunization) or (immunisation) or (vaccination) or (disease near2 program*)) in DE
|
DATABASE SYNTAX GUIDE CENTRAL ‐ Cochrane Library Online | ||
| AND | AND operator | Includes both terms |
| OR | OR operator | Includes either both, the one or the other term |
| MeSH descriptor | Subject Heading | |
| :ti | Title word | |
| :ab | Abstract word | |
| * | Truncation | Adds non or more characters |
| NEAR/n | NEAR operator | Requires words are adjacent with n words in between ‐ regardless of word order |
| NEXT | NEXT operator | Requires words are adjacent to each other in the order typed in |
| Ovid databases | ||
| AND | AND operator | Includes both terms |
| OR | OR operator | Includes either both, the one or the other term |
| / | Subject Heading | |
| .ab. | Abstract word | |
| .tw. | Text Word | Word in title or abstract field |
| .fs. | Floating subheading | Subheading of any Subject Heading |
| .pt. | Publication type | |
| .sh. | Subject Heading | |
| .mp. | Will search in title, abstract and in Subject Heading field | |
| exp | Explode | Will include narrower terms to the Subject Heading being exploded |
| $ | Truncation/wild card | Adds non or more characters |
| $n | Truncation/wild card | Adds non to n characters |
| ? | Truncation/wild card | Adds non or one character |
| adj | Adjacency | Requires words are adjacent to each other in the order typed in |
| adjn | Adjacency | Requires words are adjacent with n words in between ‐ regardless of word order |
| ” – ” | Double quotation mark | Exact phrase searching |
| POPLINE | ||
| Subject search | Will search in title, abstract and in keyword field | |
| & | AND operator | Includes both terms |
| / | OR operator | Includes either both, the one or the other term |
| Wn | WITHIN operator | Requires words are adjacent with n words in between ‐ regardless of word order |
| * | Truncation | Adds non or more characters |
| EBSCO | ||
| MH | CINAHL Heading | |
| ? | Wildcard | Replaces a single character |
| * | Truncation | Adds non or more characters |
| Nn | Near operator | N5 finds the words if they are within five words of one another regardless of word order |
| Wn | Within operator | W5 finds the words if they are within five words of one another and in the order typed in |
| “ ‐ “ | Double quotation mark | Exact phrase searching |
| CSA | ||
| DE= | Descriptor | |
| TI= | Title word | |
| AB= | Abstract word | |
| * | Truncation | Adds non or more characters |
Data and analyses
Comparison 1. Add on of family planning at voluntary counselling and testing (VCT) clinics.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Couples Initiating non barrier contraception | 1 | 251 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.74, 3.29] |
| 2 Incident pregnancies | 1 | 251 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.53, 1.48] |
1.1. Analysis.

Comparison 1 Add on of family planning at voluntary counselling and testing (VCT) clinics, Outcome 1 Couples Initiating non barrier contraception.
1.2. Analysis.

Comparison 1 Add on of family planning at voluntary counselling and testing (VCT) clinics, Outcome 2 Incident pregnancies.
Comparison 2. Add on of HIV counselling and testing to STI services.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Offered HIV Testing as a proportion of all STI patients | 1 | 9080 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.31, 1.39] |
| 2 HIV Tested as a proportion of all STI patients | 1 | 9080 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [1.18, 1.28] |
| 3 Declined HIV testing as a proportion of all new STI clients | 1 | 9080 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [1.74, 2.15] |
| 4 Declined HIV testing as a proportion of those offered testing | 1 | 5732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.30, 1.59] |
2.1. Analysis.
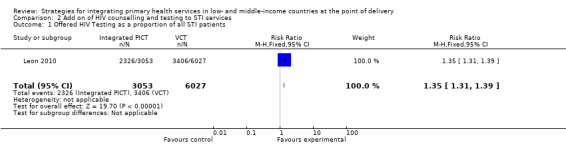
Comparison 2 Add on of HIV counselling and testing to STI services, Outcome 1 Offered HIV Testing as a proportion of all STI patients.
2.2. Analysis.
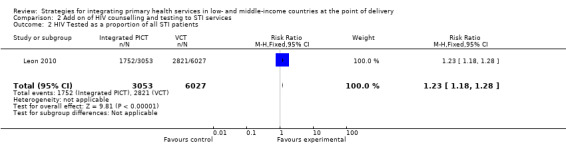
Comparison 2 Add on of HIV counselling and testing to STI services, Outcome 2 HIV Tested as a proportion of all STI patients.
2.3. Analysis.
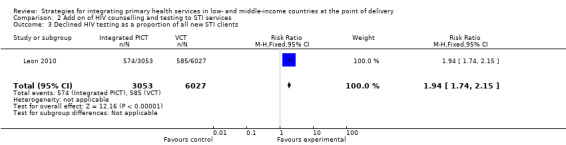
Comparison 2 Add on of HIV counselling and testing to STI services, Outcome 3 Declined HIV testing as a proportion of all new STI clients.
2.4. Analysis.
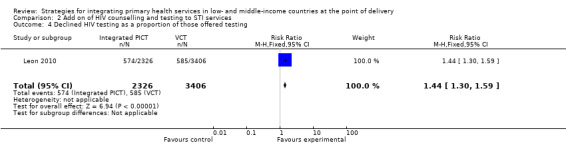
Comparison 2 Add on of HIV counselling and testing to STI services, Outcome 4 Declined HIV testing as a proportion of those offered testing.
Comparison 3. Add on of HIV counselling and testing at tuberculosis (TB) clinics.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 New adult TB patients who received counseling | 1 | 754 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.69 [1.81, 3.99] |
| 2 New adult TB patients who received HIV testing | 1 | 754 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.12 [2.04, 4.77] |
| 3 New adult TB patients tested HIV+ | 1 | 754 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.43 [1.70, 6.91] |
3.1. Analysis.

Comparison 3 Add on of HIV counselling and testing at tuberculosis (TB) clinics, Outcome 1 New adult TB patients who received counseling.
3.2. Analysis.
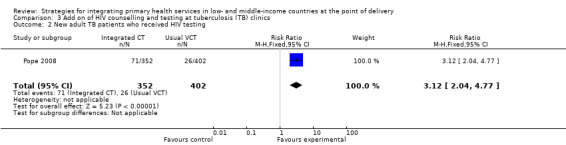
Comparison 3 Add on of HIV counselling and testing at tuberculosis (TB) clinics, Outcome 2 New adult TB patients who received HIV testing.
3.3. Analysis.
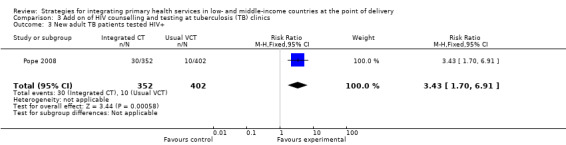
Comparison 3 Add on of HIV counselling and testing at tuberculosis (TB) clinics, Outcome 3 New adult TB patients tested HIV+.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Gregson 2007.
| Methods | Cluster randomised trial. | |
| Participants | Six pairs of matched communities (each included at least one government or mission health centre). Adults (11,980) living in these communities. |
|
| Interventions | Aim: to assess the effectiveness of integrated community HIV prevention and clinic services on reducing HIV incidence. Group 1. Peer education and condom distribution to targeted groups supported by income generating projects; strengthened sexually transmitted disease services; and clinic open days with HIV/AIDS information, education and communication (IEC). Implemented by an experienced non‐government organisation. Group 2. Routine government STI services, condom distribution, home based care, IEC. |
|
| Outcomes | Main: HIV‐1 incidence in the population; Secondary: STI incidence; STi Rx effectiveness; sexual and health seeking behaviour change; HIV/AIDS knowledge. |
|
| Notes | Study undertaken between 1998 and 2003 in Zimbabwe. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss by Ministry of Health official |
| Allocation concealment (selection bias) | Low risk | Unit of allocation was the community, and by random process |
| Blinding (performance bias and detection bias) All outcomes | High risk | Local research staff were blinded to patients initial HIV status, but not blinded to interventions |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow up in intervention and control groups was reported and noted to have affected the groups similarly. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported, including positive and negative results |
Huntington 1994.
| Methods | Cluster randomised trial in 16 selected clinics divided into two groups. | |
| Participants | 16 Clinics providing childhood immunisation (EPI) services. | |
| Interventions | Aim: to integrate family planning with the extended programme of immunisation. Groups: 1. EPI service provider encourages mothers individually at immunisation clinic to attend the family planning services that day at the same clinic, using a standard message comprising of three statements. Group 2. Usual group information‐education‐communication package. |
|
| Outcomes | 1. Attenders' family planning knowledge and practice, from pre and post surveys. 2. Providers' view, from self‐administered questionnaire. 3. New acceptors, from family planning service records. Intermediate outcome: Number of family planning clients | |
| Notes | Study undertaken between January and September 1992 in Togo | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The process of randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Clinics selected from a list of all MCH‐FP clinics were randomly allocated to test and control sites |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention was made of blinding during the implementation or assessment of the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Routine service data and exit interviews of patients used. No mention of missing data or different response rates in intervention and control sites. |
| Selective reporting (reporting bias) | Unclear risk | All data were not fully reported on |
Leon 2010.
| Methods | Controlled before and after study. | |
| Participants | 21 Primary healthcare facilities providing STI services. | |
| Interventions | Aim: To assess the effectiveness of integrating provider initiated counselling and testing (PICT) in routine services compared to existing 'special' delivery of voluntary counselling and testing (VCT) by lay counsellors. Group 1. STI nurse trained in PICT offered HIV testing as a standard part of STI care for all STI clients; Group 2: Lay counsellors provide VCT separately on same site, either on initiation by patient or medical referral. |
|
| Outcomes | 1. HIV testing rate amongst new STI clients; 2. Proportion of STI clients offered HIV testing; 3. Proportion of STI clients declining HIV testing, once offered. | |
| Notes | Study conducted between 2006 and 2007 in Cape Town, South Africa. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Intervention clinics were selected by health management |
| Allocation concealment (selection bias) | High risk | As above |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding was not feasible during implementation or assessment as health service providers facilitated the intervention and assisted with the evaluation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data was followed up. |
| Selective reporting (reporting bias) | Low risk | All outcomes described in the methods were reported on. |
Mark 2007.
| Methods | Randomised controlled trial of couples by attendance day. | |
| Participants | 251 co‐habiting couples attending a voluntary HIV counselling and testing clinic. | |
| Interventions | Aim: To promote dual‐method contraception use among HIV concordant and HIV discordant couples already using condoms for HIV prevention. 1. Family planning education and offer of non‐barrier contraceptives; 2. Intervention 1 plus a presentation; 3.Control: Family planning education and referral to an outside clinic. |
|
| Outcomes | Use of non‐barrier contraceptives; reported condom use; pregnancy incidence. | |
| Notes | Study undertaken between September 1996 and August 1997 in Zambia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Attendance days were randomised using a random number table |
| Allocation concealment (selection bias) | Low risk | Assignment was concealed from staff involved in data collection until informed consent was signed by couples |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | This was not specified in the paper |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Couples with incomplete data were removed from analysis, but no information was provided to indicate that this affected intervention and control groups similarly. |
| Selective reporting (reporting bias) | Low risk | All outcomes described in the methods were reported on. Data indicating an absence of effect were reported. |
Nyamuryekung'e 1997.
| Methods | Cluster randomised trial. | |
| Participants | Seven truck stops with peer health educations and associated health facilities. | |
| Interventions | Aim: to evaluate different approaches of delivering STI services to increase utilisation by women at truck stops. Peer health educators trained in STI and risk assessment, referred women to either: Group 1. Special STI services outside normal working hours (one at fixed location, one at site chosen by women); Group 2. STI services through normal clinics, in normal working hours (integrated). Group 3. Special team of clinicians visits every 3 months. Drugs were supplied to all three groups. |
|
| Outcomes | 1. Utilisation, from attendances/population. 2. Referrals who attended clinic. 3. User satisfaction. 4. Cost per patient treated. | |
| Notes | Study undertaken in Tanzania between July 1993 and May 1994. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated that truck stops were randomly assigned, but method of sequence generation was not described |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding (performance bias and detection bias) All outcomes | High risk | Outcomes were not assessed blindly |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not specified in the paper |
| Selective reporting (reporting bias) | Low risk | Reported on all outcomes assessed |
Pope 2008.
| Methods | Cluster randomised trial in TB clinics. | |
| Participants | 20 TB clinics (10 intervention, 10 control); 754 new adult TB patients attending the clinics. |
|
| Interventions | Aim: to evaluate the effectiveness of integrated HIV counselling, testing and care in TB services. Group 1. Training of health care workers in provider initiated HIV counseling and testing and integration of TB and HIV/AIDS care; Group 2. Routine HIV testing (opt out) for TB patients. |
|
| Outcomes |
Main: % of new adult TB patients who received HIV counseling and testing; Secondary: mean % of patients tested HIV positive; mean % of HIV positive patients prescribed cotrimoxazole, and/or referred for HIV care. |
|
| Notes | Study undertaken in South Africa between August and November 2005. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated that clinics were randomised, but method of randomisation not clearly described |
| Allocation concealment (selection bias) | Unclear risk | As per above |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not specified in the paper |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
Taylor 1987 (FP).
| Methods | Controlled before and after study. | |
| Participants | 19 villages in 5 clusters of 3‐4 villages; Couples living in the villages. |
|
| Interventions | Aim: To evaluate the inter‐relationship between health services and family planning. Interventions were provided mainly by family health workers (FHWs) who lived in villages, supported by local health services. Group 1. Family planning (FP) and child health; Group 2. FP and women's health; Group 3. FP, women's Health and child Health; Group 4. FP education only; Control. Routine government health services. |
|
| Outcomes | Family planning acceptance; Costs. |
|
| Notes | Study undertaken in India over four years between 1970 and 1974. Two groups (FPWS and FPWSCC) had implementation over 3 years, one group (FPCC) for three years, and one group (FPE) for two years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled before and after study |
| Allocation concealment (selection bias) | High risk | Controlled before and after study |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described in the study methods. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not specified in the paper |
| Selective reporting (reporting bias) | High risk | Full results provided only for selected outcomes |
Taylor 1987 (Nutrition).
| Methods | Controlled before and after study. | |
| Participants | 10 villages in four clusters of 2‐3 villages; Children aged between 0‐36 months living in the villages. |
|
| Interventions | Aim: To test the interactions of nutrition and infection control programmes in children Family health workers delivered interventions in homes or village clinic. Group 1. Nutrition alone; Group 2. Health care alone; Group 3. Nutrition and health care; Control: routine government health services. |
|
| Outcomes | Mortality; Nutrition status; Psychomotor development; Morbidity: disease episodes; Costs. |
|
| Notes | Study undertaken in India over four years between 1969 and 1973. Reported with study of integration of family planning and health care. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled before and after study |
| Allocation concealment (selection bias) | High risk | Controlled before and after study |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described in the study methods. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not specified in the paper |
| Selective reporting (reporting bias) | High risk | Full results only provided for selected outcomes |
Tuladhar 1982.
| Methods | Controlled before and after study in four selected districts, 2 with vertical programme and 2 with integrated programme. | |
| Participants | Four matched districts; Households with married women aged 15‐44 years in selected wards of districts. |
|
| Interventions | Aim: to evaluate the impact of integrated family planning and maternal and child health services on family planning use, fertility and infant mortality. Groups: 1. Integrated family planning/maternal and child health programme: 48 district offices, 298 health posts, which included family planning, nutrition monitoring, health education, immunisation, TB and leprosy case finding and treatment, referral, treatment of common illnesses, and training of traditional birth attendants. Some included antenatal, delivery and postnatal care, and malaria surveillance. Group 2. Vertical family planning/maternal and child health programme: dedicated staff at 40 district offices and 492 service centres, providing family planning, antenatal care and immunization vaccination for children under five years. |
|
| Outcomes | 1. Family planning knowledge, use and intention to use. 2. Family size preferences. 3. Infant mortality. | |
| Notes | Study undertaken in Nepal between 1975 and 1978. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled before and after study |
| Allocation concealment (selection bias) | High risk | Controlled before and after study |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding was described in the study methods. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not specified in the paper |
| Selective reporting (reporting bias) | Low risk | No apparent selective reporting, with data reported on all outcomes |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ageel 1997 | Study design was interrupted time series, but had no control group and insufficient points of measurement |
| Alisjahbana 1995 | No baseline measurement to measure change and not really integration of existing entities, but the creation of a new system |
| Alvarado 1999 | Not a before and after study, even though it had a control group |
| Arifeen 2004 | Strategy consists of package of IMCI interventions |
| Ayles 2008 | Intervention is add on of community level enhanced case finding, and household involvement in TB and HIV. Integration of TB and HIV at facility level established and not part of experimental component |
| Baqui 2008 | Study design does not meet inclusion criteria |
| Barua 1999 | A survey, not an interrupted time series or a before and after study |
| Chaturvedi 1987 | A survey study design, no before baseline measurement, but with control |
| Chaturvedi 1989 | A summary of cross‐sectional studies |
| Chen 1999 | No control group |
| De Graff 1986 | Issues about integration unclear, it seems the main intervention is an increase in health workers. Study design is a 2 site concurrent study and not included. Similar paper to the other Matlab papers (Phillips 1984; Simmons 1991) |
| DeSchampheleire 1981 | Excluded as an ITS with insufficient measurement points, and has no control group, only used national statistics as comparison group |
| Dissevelt 1980 | No control group |
| Emond 2002 | No control group |
| Fairall 2005 | Defined as a package of care for lung diseases. Similarly for IMCI, this may be delivered vertically or integrated. The study therefore does not evaluate the strategy of delivery, but rather the package of care |
| Ghandi 2009 | Observational study design which did not meet inclusion criteria |
| Grosskurth 2000 | Observational study |
| Guillemot 1980 | This was not integration but an intervention of adding specially trained staff |
| Gupta 1984 | A cross sectional study, not CBA |
| Harrison 1993 | Excluded because of its study design; it is a survey |
| Hieu 1994 | Excluded as no pre‐intervention results; results presented for the post‐intervention and a control group only |
| Htay 2003 | Cross sectional study |
| Ionescu 1986 | Not a controlled study |
| Khan 2002 | No control group |
| Kisinza 2008 | Observational study design which does not meet inclusion criteria |
| Mancini 2003 | Modelling study |
| Marsh 2002 | Trial evaluating the implementation of a nutrition programme |
| Mathews 1994 | An evaluation of a community health worker project, not of integration |
| McDougall 1978 | This is not a controlled study and it is unclear what integration is in this paper |
| Mukhopadhyay 1990 | This study design is sort of before and after, but the time period is unclear |
| Phillips 1984 | Issues about integration unclear, it seems the main intervention is an increase in health workers. Study design is a 2 site concurrent study and not included. Similar paper to the other Matlab papers (De Graff 1986; Simmons 1991) |
| Ramaseeta 1977 | A before and after study, but with no control. Integration strategy also not clear |
| Revankar 1982 | A before and after study but no control group |
| Schellenberg 2004 | Strategy consists of package of IMCI interventions |
| Semba 2001 | Evaluates adding vitamin A to EPI package |
| Simmons 1991 | Issues about integration unclear, it seems the main intervention is an increase in health workers. Study design is a 2 site concurrent study and not included. Similar paper to the other Matlab papers (Phillips 1984; De Graff 1986) |
| Sylla 1995 | This is a survey and so does not meet inclusion study design criteria |
| Tandon 1981 | This study contained no comparison group or control |
| Tandon 1988 | This study is a survey with a control group, and not a before and after study |
| Tandon 1992 | This study was excluded as it is a survey with a control group, and not a before and after study. Also the integration strategy is unclear |
| Thongkrajai 1994 | Excluded as no pre‐intervention results; results presented for the post‐intervention and a control group only |
| Van Rie 2008 | Observational study design which did not meet inclusion criteria |
| Walley 1991 | This study was a before and after study but lacked a control group |
| Xiamong 2000 | This is not an integrative strategy, but a strategy which involved giving education on AIDS |
Characteristics of ongoing studies [ordered by study ID]
Patel 2008.
| Trial name or title | Improving the outcomes of primary care attenders with common mental disorders in developing countries: a cluster RCT of a collaborative stepped care intervention in Goa, India |
| Methods | Cluster randomised controlled trial |
| Participants | Primary care facilities and primary care attenders who are detected to suffer from common mental disorders |
| Interventions | Collaborative stepped care intervention |
| Outcomes | Proportion of participants who recover from an ICD10 defined CMD; economic and disability outcomes |
| Starting date | April 2007 |
| Contact information | vikram.patel@lshtm.ac.uk |
| Notes | Last enquiry to author in November 2010. Study is due for publication in 2011 |
Differences between protocol and review
The 2010 update includes 'linkages' as part of integration in the inclusion criteria and in the search. The update excludes 'packages'' of care as a mechanism of integration, as such packages can be delivered either as 'vertical' services with special support and resources, or are added or fully integrated into routine care. Studies assessing effectiveness of packages were therefore not included.
Contributions of authors
Lilian Dudley carried out the update in 2010, working with Paul Garner who conducted the 2005 update. In the first version of this review, in 2001, Jane Briggs wrote the protocol, conducted the literature search and data extraction, drafted and redrafted the review. Pierre Capdegelle conducted an initial overview of the concepts and appraised potentially relevant studies, advised on inclusion of studies, co‐extracted the data and co‐wrote the protocol and review.
Paul Garner supported the conceptual development of the topic; helped with the protocol, data extraction, data presentation, analysis and interpretation; was commissioned to conduct the review and liaised with the World Health Organization (WHO). Philemona Hinds provided administrative support for the updated review.
Sources of support
Internal sources
International Health Division, Liverpool School of Tropical Medicine, UK.
Faculty of Health Sciences, University of Stellenbosch, South Africa.
Center for Pharmaceutical Management, Management Sciences for Health, USA.
External sources
Norwegian Knowledge Centre for the Health Services, Norway.
Department for International Development, UK.
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Gregson 2007 {published data only}
- Gregson S, Adamson S, Papaya S, Mundondo J, Nyamukapa CA, et al. Impact and process evaluation of integrated community and clinic‐based HIV‐1 control: Acluster‐randomised trial in eastern Zimbabwe. PLoS Med 2007;4:e102. [DOI: 10.1371/journal.pmed.0040102] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huntington 1994 {published data only}
- Huntington D, Aplogan A. The integration of family planning and childhood immunization services in Togo. Studies in Family Planning 1994;25(3):176‐83. [MEDLINE: ] [PubMed] [Google Scholar]
Leon 2010 {published data only}
- Leon N, Naidoo P, Mathews C, Lewin C, Lombard C. The impact of provider‐initiated (opt‐out) HIV testing and counseling of patients with sexually transmitted infection in Cape Town, South Africa: a controlled trial. Implementation Science 2010;5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mark 2007 {published data only}
- Mark KE, Meinzen‐Derr J, Stephenson R, et al. Contraception among HIV concordant and discordant couples in Zambia: A randomized controlled trial. Journal of Women's Health 2007;16(8):1200‐10. [DOI] [PubMed] [Google Scholar]
Nyamuryekung'e 1997 {published data only}
- Nyamuryekung'e K, Laukamm‐Josten U, Vuylsteke B, Mbuya C, Hamelmann C, Outwater A, et al. STD services for women at truck stop in Tanzania; evaluation of acceptable approaches. East African Medical Journal 1997;74(6):343‐7. [MEDLINE: ] [PubMed] [Google Scholar]
Pope 2008 {published data only}
- Pope DS, DeLuca AN, Kali P, et al. A cluster‐randomized trial of provider‐initiated (opt‐out) HIV counseling and testing of tuberculosis patients in South Africa. Journal of Acquired Immune Deficiency Syndromes 2008;48(2):190‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 1987 (FP) {published data only}
- Taylor CE, Parker RL. Integrating PHC services: evidence from Narangwal, India. Health Policy and Planning 1987;2(2):150‐61. [Google Scholar]
Taylor 1987 (Nutrition) {published data only}
- Taylor CE, Parker RL. Integrating PHC services: evidence from Narangwal, India. Health Policy and Planning 1987;2:150‐61. [Google Scholar]
Tuladhar 1982 {published data only}
- Tuladhar JM, Stoeckel J. The relative impacts of vertical and integrated FP/MCH programs in rural Nepal. Studies in Family Planning 1982;13(10):275‐86. [MEDLINE: ] [PubMed] [Google Scholar]
References to studies excluded from this review
Ageel 1997 {published data only}
- Ageel AR, Amin MA. Integration of schistosomiasis‐control activities into the primary‐health‐care system in the Gizan region, Saudi Arabia. Annals of Tropical Medicine and Parasitology 1997;91(8):907‐15. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Alisjahbana 1995 {published data only}
- Alisjahbana A, Williams C, Dharmayanti R, Hermawan D, Kwast BE, Koblinsky M. An integrated village maternity service to improve referral patterns in a rural area in West‐Java. International Journal of Gynaecology and Obstetrics 1995;48 Suppl:83‐94. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Alvarado 1999 {published data only}
- Alvarado R, Zepeda A, Rivero S, Rico N, Lopez S, Diaz S. Integrated maternal and infant health care in the post partum period in a poor neighbourhood in Santiago, Chile. Studies in Family Planning 1999;30(2):133‐41. [DOI] [PubMed] [Google Scholar]
Arifeen 2004 {published data only}
- Arifeen SE, Blum LS, Hoque DME, Chowdhury EK, Khan R, Black RE, et al. Integrated Management of Childhood Illness (IMCI) in Bangladesh: early findings from a cluster‐randomised study. Lancet 2004;364:1595‐602. [DOI] [PubMed] [Google Scholar]
Ayles 2008 {published data only}
- Ayles HM, Sismanidis C, Beyers N, et al. Zamstar Study Protocol: The Zambia South Africa TB and HIV reduction study: design of a 2x2 factorial community randomized trial. Trials 2008;9:63 (http://www.trialsjournal.com/content/9/1/63). [DOI: 10.1186/1745-6215-9-63] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baqui 2008 {published data only}
- Baqui A, Williams EK, Rosecrans AM, et al. Impact of an integrated nutrition and health programme on neonatal mortality in rural northern India. Bulletin of the World Health Organization 2008;86(10):794‐804. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barua 1999 {published data only}
- Barua S, Wakai S, Shwe T, Umenai T. Leprosy elimination through integrated basic health services in Myanmar: the role of midwives. Leprosy Review 1999;70(2):174‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chaturvedi 1987 {published data only}
- Chaturvedi S, Srivastava BC, Singh JV. Impact of total six years exposure to integrated child development services on growth and health status of target children in Dalmau project area (Uttar Pradesh). Indian Journal of Medical Research 1987;86:766‐74. [PubMed] [Google Scholar]
Chaturvedi 1989 {published data only}
- Chaturvedi S, Gupta SB, Srivastava BC, Nirupam S, Rastogi AK. The impact of the integrated child development services scheme in North India. Asia‐Pacific Journal of Public Health 1989;3(4):291‐6. [DOI] [PubMed] [Google Scholar]
Chen 1999 {published data only}
- Chen W, Wu K, Lin M, Tang L, Gu Z, Wang S, et al. A pilot study on malaria control by using a new strategy of combining strengthening infection source treatment and health education in mountainous areas of Hainan province. Chung‐Kuo Chi Sheng Chung Hsueh Yu Chi Sheng Chung Ping Tsa Chih [Chinese Journal of Parasitology & Parasitic Diseases] 1999;17(1):1‐4. [PubMed] [Google Scholar]
De Graff 1986 {published data only}
- Graff DS, Phillips JF, Simmons R, Chakraborty J. Integrating health services into an MCH‐FP program in Matlab, Bangladesh: an analytical update. Studies in Family Planning 1986;17(5):228‐34. [MEDLINE: ] [PubMed] [Google Scholar]
DeSchampheleire 1981 {published data only}
- Schampheleire I, Wollast E. Integrated family planning activities in maternal and child health centres in Cap Bon, Tunisia. 1. Methodology and results. Journal of Tropical Pediatrics 1981;27(4):190‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dissevelt 1980 {published data only}
- Dissevelt AG. Integrated maternal and child health services. A study at a rural health centre in Kenya. Tropical and Geographical Medicine 1980;32(1):57‐69. [MEDLINE: ] [PubMed] [Google Scholar]
Emond 2002 {published data only}
- Emond A, Pollock J, Costa N, Maranhao T, Macedo A. The effectiveness of community‐based interventions to improve maternal and infant health in the Northeast of Brazil. Pan American Journal of Public Health 2002;12(2):101‐10. [DOI] [PubMed] [Google Scholar]
Fairall 2005 {published data only}
- Fairall LR, Zwarenstein M, Bateman ED, et al. Effect of educational outreach to nurses on tuberculosis case detection and primary care of respiratory illness: pragmatic cluster randomized controlled trial.. BMJ 2005;33:750‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghandi 2009 {published data only}
- Gandhi NR, Moll AP, Lalloo U, et al. Successful integration of tuberculosis and HIV treatment in rural South Africa: the Sizonq'oba study. Journal of Acquired Immune Deficiency Syndromes 2009;50(1):37‐43. [DOI] [PubMed] [Google Scholar]
Grosskurth 2000 {published data only}
- Grosskurth H, Mwijarubi E, Todd J, Rwakatare M, Orroth K, Mayaud P, et al. Operational performance of an STD control programme in Mwanza Region, Tanzania. Sexually Transmitted Infections 2000;76(6):426‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guillemot 1980 {published data only}
- Guillemot L, Chakraborty M, Mitra PK, Dey DK. Integration of leprosy and tuberculosis control ‐ a field experiment. Leprosy in India 1980;52(4):491‐500. [MEDLINE: ] [PubMed] [Google Scholar]
Gupta 1984 {published data only}
- Gupta SB, Srivastava BC, Bhushan V, Sharma P. Impact of the integrated child development services in Uttar Pradesh. Indian Journal of Medical Research 1984;79:363‐72. [MEDLINE: ] [PubMed] [Google Scholar]
Harrison 1993 {published data only}
- Harrison D, Barron P, Glass B, Sonday S, vd Heyde Y. Far fewer missed opportunities for immunisation in an integrated child health service. South African Medical Journal 1993;83(8):575‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Hieu 1994 {unpublished data only}
- Hieu DT. Feasibility of integrating STD services and STD/HIV/AIDS prevention into the MCH/FP Programme in Vietnam. Unpublished 1994.
Htay 2003 {published data only}
- Htay TT, Sauvarin J, Khan S. Integration of post‐abortion care: the role of township medical officers and midwives in Myanmar. Reproductive Health Matters 2003;11(21):27‐36. [DOI] [PubMed] [Google Scholar]
Ionescu 1986 {published data only}
- Ionescu C, Hreniuc R, Mihaescu T. Evaluation of the integrated treatment of tuberculosis in 20 tuberculosis outpatient units [Evaluarea tratementului integrat al tuberculozei in 20 de dispensare antituberculoase]. Revista de Igiena Bacteriologie, Virusologie, Parazitologie, Epidemiologie, Pneumoftiziologie ‐ Pneumoftiziologia 1986;35(3):273‐4. [MEDLINE: ] [PubMed] [Google Scholar]
Khan 2002 {published data only}
- Khan MM, Ahmed S. Relative efficiency of government and non‐government organisations in implementing a nutrition intervention programme‐‐a case study from Bangladesh. Public Health Nutrition 2003;6(1):19‐24. [DOI] [PubMed] [Google Scholar]
Kisinza 2008 {published data only}
- Kisinza WN, Kisoka WJ, Mutalemw PP, et al. Community directed interventions for malaria, tuberculosis and vitamin A in onchocerciasis endemic districts of Tanzania. Tanzania Journal of Health Research 2008;10(4):232‐9. [DOI] [PubMed] [Google Scholar]
Mancini 2003 {published data only}
- Mancini DJ, Stecklov G, Stewart JF. The effect of structural characteristics on family planning program performance in Cote d'Ivoire and Nigeria. Social Science & Medicine 2003;56(10):2123‐37. [DOI] [PubMed] [Google Scholar]
Marsh 2002 {published data only}
- Marsh DR, Pachon H, Schroeder DG, Ha TT, Dearden K, Lang TT, et al. Design of a prospective, randomized evaluation of an integrated nutrition program in rural Viet Nam. Food & Nutrition Bulletin 2002;23(4):36‐47. [PubMed] [Google Scholar]
Mathews 1994 {published data only}
- Mathews C, Walt H, Barron P. A shotgun marriage‐‐community health workers and government health services. Qualitative evaluation of a community health worker project in Khayelitsha. South African Medical Journal 1994;84(10):659‐63. [MEDLINE: ] [PubMed] [Google Scholar]
McDougall 1978 {published data only}
- McDougall AC, Rose P. Integrated leprosy control in Guyana. Bulletin of the Pan American Health Organization 1978;12(1):11‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Mukhopadhyay 1990 {published data only}
- Mukhopadhyay SP, Halder AK, Das KK. Dr PC Sen Memorial Oration. A study of utilisation of family planning services through MCH package care in rural areas of West Bengal. Indian Journal of Public Health 1990;34(3):147‐51. [MEDLINE: ] [PubMed] [Google Scholar]
Phillips 1984 {published data only}
- Phillips JF, Simmons R, Chakraborty J, Chowdhury AI. Integrating health services into an MCH‐FP Program: lessons from Matlab, Bangladesh. Studies in Family Planning 1984;15(4):153‐61. [MEDLINE: ] [PubMed] [Google Scholar]
Ramaseeta 1977 {published data only}
- Ramaseeta T, Samputtavanich S, Ochasanendha P, Ito T. Results of five years of integration of leprosy control into the Provincial Health Service of Phuket Island, Southern Thailand. Leprosy Review 1977;48(4):261‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Revankar 1982 {published data only}
- Revankar CR, Jha SS, Dongre VV, Deshpande SS, Ganapati R. Integration of leprosy into general health services in an urban area ‐ a feasibility study. Leprosy Review 1982;53(4):297‐305. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schellenberg 2004 {published data only}
- Schellenberg JRM Armstrong, Adam T, Mshinda H, et al. Effectiveness and cost of facility‐based Integrated Management of Childhood Illness (IMCI) in Tanzania. Lancet 2004;364:1583‐94. [DOI] [PubMed] [Google Scholar]
Semba 2001 {published data only}
- Semba RD, Munasir Z, Akib A, Melikian G, Permaesih D, Muherdiyantiningsih, et al. Integration of vitamin A supplementation with the Expanded Programme on Immunization: lack of impact on morbidity or infant growth. Acta Paediatrica 2001;90(10):1107‐11. [DOI] [PubMed] [Google Scholar]
Simmons 1991 {published data only}
- Simmons GB, Balk D, Faiz KK. Cost‐effectiveness analysis of family planning programs in rural Bangladesh: evidence from Matlab. Studies in Family Planning 1991;22(2):83‐101. [MEDLINE: ] [PubMed] [Google Scholar]
Sylla 1995 {published data only}
- Sylla PM. Status of integration of the antileprosy campaign in the general health services in Senegal [Etat de l'integration de la lutte antilepreuse dans les services de sante generaux au Senegal]. Acta Leprologica 1995;9(3):117‐25. [MEDLINE: ] [PubMed] [Google Scholar]
Tandon 1981 {published data only}
- Tandon BN, Ramachandra K, Bhatnager S. Integrated child development service in India: evaluation of the delivery of nutrition and health services and the effect on the nutritional status of the children. Indian Journal of Medical Research 1981;73:385‐94. [MEDLINE: ] [PubMed] [Google Scholar]
Tandon 1988 {published data only}
- Tandon BN, Sahai A. Immunization in India: contribution of Integrated Child Development Services scheme to expanded programme of immunization. Journal of Tropical Pediatrics 1988;34(6):309‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Tandon 1992 {published data only}
- Tandon BN, Gandhi N. Immunization coverage in India for areas served by the Integrated Child Development Services programme. The Integrated Child Development Services Consultants. Bulletin of the World Health Organization 1992;70(4):461‐5. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Thongkrajai 1994 {unpublished data only}
- Thongkrajai E. Feasibility of integrating STD services and STD/HIV/AIDS prevention into MCH/FP programme in Thailand. Unpublished 1994.
Van Rie 2008 {published data only}
- Rie A, Sabue M, Jarret N, et al. Counseling and testing TB patients for HIV: evaluation of three implementation models in Kinshasa. The International Journal of Tuberculosis and Lung Disease 2008;12 Suppl 1(3):73‐8. [PubMed] [Google Scholar]
Walley 1991 {published data only}
- Walley JD, McDonald M. Integration of mother and child health services in Ethiopia. Tropical Doctor 1991;21(1):32‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Xiamong 2000 {published data only}
- Xiamong S, Yong W, Choi KH, Lurie P, Mandel J. Integrating HIV prevention education into existing family planning services: results of a controlled trial of a community level intervention for young adults in rural China. AIDS and Behaviour 2000;4(1):103‐10. [Google Scholar]
References to ongoing studies
Patel 2008 {published data only}
- Patel VH, Kirkwood B, Pednekar S, et al. Improving the outcomes of primary care attenders with common mental disorders in developing countries: a cluster RCT of a collaborative stepped care intervention in Goa, India. Study Protocol. Trials 2008;9:4 (www.trialsjournal.com). [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Atun 2010
- Atun R, Jongh T, Secci F, et al. A systematic review of the evidence on integration of targeted health interventions into health systems. Health Policy and Planning 2010;25:1‐14. [DOI] [PubMed] [Google Scholar]
Bhutta 2008
- Bhutta ZA, Ali S, Cousens S, Ali TM, Haider BA, Rizvi A, et al. Alma‐Ata: Rebirth and Revision 6 Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make?. Lancet 2008;372(9642):972‐89. [DOI] [PubMed] [Google Scholar]
Campbell 2000
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321(7262):694‐6. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Capdegelle 1999
- Capdegelle P. Integration in health services: concepts, evidence and perspectives. Masters in Community Health thesis. School of Tropical Medicine, Liverpool (unpublished) 1999.
Ekman 2008
- Ekman B, Pathmanathan I, Liljestrand J. Integrating health interventions for women, newborn babies, and children: a framework for action. Lancet 2008;372(9642):990‐1000. [DOI] [PubMed] [Google Scholar]
Frenk 2009
- Frenk J. Reinventing primary health care: the need for systems integration. Lancet 2009;374:170‐3. [DOI] [PubMed] [Google Scholar]
Gyapong 2010
- Gyapong JO, Gyapong M, Yellu N, Anakwah K, Amofah G, Bockarie M, et al. Integration of control of neglected tropical diseases into health‐care systems: challenges and opportunities. Lancet 2010;375:160‐5. [DOI] [PubMed] [Google Scholar]
Haines 2004
- Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between knowledge and action for health. Bulletin of the World Health Organization 2004;82:724‐32. [PMC free article] [PubMed] [Google Scholar]
Higgins 2009
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews. Chichester: John Wiley and Sons Ltd, 2009. [Google Scholar]
Kennedy 2010
- Kennedy C, Spaulding A, Brickley D, Almers L, Mirjahangir J, Packel L, et al. Linking sexual and reproductive health and HIV interventions: a systematic review. Journal of the International AIDS Society 2010;13(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerber 2007
- Kerber KJ, Graft‐Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet 2007;370:1358‐69. [DOI] [PubMed] [Google Scholar]
Lavis 2005
- Lavis J, Davies H, Oxman A, Denis JL, Golden‐Biddle K, Ferlie E. Towards systematic reviews that inform health care management and policy‐making.. J Health Serv Res Policy 2005;10(1):35‐48. [DOI] [PubMed] [Google Scholar]
Lawn 2008
- Lawn JE, Rohde J, Rifkin S, Were M, Paul VK, Chopra M. Alma‐Ata 30 years on: revolutionary, relevant, and time to revitalize. Lancet 2008;372:917‐27. [DOI] [PubMed] [Google Scholar]
Leutz 1999
- Leutz WN. Five laws for integrating medical and social services: Lessons from the United States and the United Kingdom. The Millbank Quarterly 1999;77(1):77‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lush 1999
- Lush L, Walt G, Cleland J, Mayhew S. The role of MCH and family planning services in HIV/STD control: is integration the answer?. African Journal of Reproductive Health 2001; Vol. 5:29‐46. [MEDLINE: ] [PubMed]
Mills 1983
- Mills A. Vertical versus horizontal health programmes in Africa: idealism, pragmatism, resources and efficiency.. Social Science & Medicine 1983;17:1971‐81. [DOI] [PubMed] [Google Scholar]
Unger 2003
- Unger JP, Paepe P, Green A. A code of best practice for disease control programmes to avoid damaging health care services in developing countries. The International Journal of Health Planning and Management 2003;18 Suppl:27‐39. [DOI] [PubMed] [Google Scholar]
Wallace 2009
- Wallace A, Dietz V, Cairns KL. Integration of immunization services with other health interventions in the developing world: what works and why? Systematic literature review. Tropical Medicine & International Health 2009;14(1):11‐9. [DOI] [PubMed] [Google Scholar]
Walsh 1979
- Walsh JA, Warren KS. Selective primary health care: an interim strategy for disease control in developing countries. New England Journal of Medicine 1979;301:967‐74. [DOI] [PubMed] [Google Scholar]
WHO 1996
- WHO. Integration of health care delivery. WHO Technical Report Series 1996; Vol. 861:1‐68. [PubMed]
WHO 1997
- WHO. Integrated management of childhood illness. Bulletin of the World Health Organization 1997; Vol. 75 Suppl 1:1‐128. [PMC free article] [PubMed]
WHO 2005
- Child and Adolescent Health and Development Website. http://www.who.int/child‐adolescent‐health/integr.htm, accessed Feb 20, 2006.
WHO 2009
- Anonymous. Linkages: evidence review and recommendations. WHO/HIV2009 Vol. http://whqlibdoc.who.int/hq/2009/WHO_HIV_2009_eng.pdf.
WHO/HIV/2008
- WHO. Sexual and reproductive health and HIV linkages: evidence review and recommendations. http://149.120.32.2/upload/lib_pub_file/807_filename_linkages_evidence_review.pdf 2008.
Wisner 1988
- Wisner B. GOBI versus PHC? Some dangers of selective primary health care. Social Science & Medicine 1988;26:963‐9. [DOI] [PubMed] [Google Scholar]
World Bank 2001
- World Bank. World development indicators. Washington: World Bank, 2001. [Google Scholar]


