Abstract
Youth exiting foster care represent a unique, at-risk population in that they receive supportive health services while under the umbrella of the foster care system, but access to care can drop precipitously upon release from foster custody. Traditional means of substance use treatment may not meet the needs of this vulnerable population. Mobile interventions, however, have demonstrated high acceptability and efficacy across a range of mental and physical health issues. The specific advantages to mobile interventions dovetail well with the barriers faced by youth exiting foster care. This study describes the feasibility, acceptability, and initial efficacy of iHeLP, a computer- and mobile phone-based intervention based in Motivational Interviewing for reducing substance use among youth exiting foster care (n = 33). Participants were randomly assigned to either iHeLP or a contact control, each of which lasted six months. Feasibility was evaluated through eligibility and enrollment rates at baseline, and retention and intervention reach rates 3, 6, 9, and 12 months later. Acceptability was measured through a 5-item satisfaction measure and exit interviews. The two groups were then compared on a monthly measure of substance use. Study enrollment, retention, response rate, engagement, and satisfaction were all very good. Participants receiving iHeLP reported higher percent days abstinent than the control group, with effect sizes ranging from 0.32 to 0.62. Technology-based interventions such as iHeLP may be attractive to this population and support efforts towards reductions in substance use.
Keywords: Foster Care, Tailored Intervention, Brief Intervention, Mobile Health, Substance Use
1. Introduction
1.1. Substance Use among Youth in Foster Care
Each year, over 7 million U.S. children and adolescents are involved in reports of abuse and neglect (U.S. Department of Health and Human Services, 2017). Given the substantial impact that abuse, neglect, and child welfare involvement can have on adolescent and young adult development, public health officials have asserted that maltreatment warrants as much research attention as other concerns affecting young people, such as HIV/AIDS, smoking, and obesity (Butchart, Harvey, Mian, & Furniss, 2006). Although maltreatment is related to a host of poor outcomes in adolescence and young adulthood, it appears to have a uniquely strong relationship with substance use (Dube et al., 2003; Dube et al., 2006). In particular, exposure to Adverse Childhood Experiences (ACEs) – including physical and emotional neglect, physical, sexual, and emotional abuse, domestic violence, parental substance use, parental mental illness, parental separation, and parental incarceration – is significantly associated with substance use among young people. While exposure to any one of these experiences corresponds with an increased likelihood of using alcohol or drugs, the cumulative exposure to multiple ACEs exponentially increases risk for youth substance use (Dube et al., 2003; Dube et al., 2006).
Exposure to ACEs is more common, occurs earlier in life, and accumulates more frequently among youth in foster care (Bramlett & Radel, 2014; Stambaugh et al., 2013). Such exposure may partially explain the tendency for foster youth to misuse substances at earlier ages than in the general population (Gabrielli, Jackson, & Brown, 2016) and report higher rates of “hard” drug use and problematic substance use (Braciszewski & Stout, 2012). For example, in a nationally representative sample, alcohol use disorders occurred up to four times more often among adolescents with a history of foster care compared to those without (Pilowsky & Wu, 2006). Rates of substance use also appear to be higher among youth removed from their home compared to maltreated youth who remain with their biological parents (Traube, James, Zhang, & Landsverk, 2012; U.S. Department of Health and Human Services, 2005). Lifetime rates of non-alcohol substance use disorders for older adolescents in foster care have reached as high as 14% (Keller, Salazar, & Courtney, 2010) – two to three times higher than corresponding national general population data (Center for Behavioral Health Statistics and Quality [CBHSQ], 2016_S1_Reference11). After youth exit the child welfare system, diagnostic rates escalate rapidly. Specifically, the largest longitudinal study of youth exiting foster care (the Midwest Study) reported an increase of 11% and 13% for alcohol and substance use disorders, respectively, in the first year post-exit (Courtney et al., 2005), while general population emerging adults experience an increase of only 1–2% over this same period of time (Substance Abuse and Mental Health Services Administration, 2009). Comprehensive substance use services are clearly needed to reduce these high levels of substance use within foster care and prevent the substantial increase in problematic alcohol and drug use post-foster care.
1.2. Substance Use Interventions for Youth in Foster Care
The availability of screening, assessment, and treatment services for substance use is essential during adolescence and young adulthood, as early substance use initiation is highly associated with subsequent problematic use (Dawson, Goldstein, Chou, Ruan, & Grant, 2008; King & Chassin, 2007). Despite the need for these resources, less than 10% of U.S. adolescents who misuse substances receive appropriate services (CBHSQ, 2016). For foster youth, availability of care is scarce, as screening and assessment of substance use appears to be rare across child welfare systems (McCarthy, Van Buren, & Irvine, 2007). Entry into foster care is a potentially critical point for determining the health needs of these vulnerable young people. However, in the few states where screening and assessment are occurring, the accompanying procedures have been reported to not fully fit the needs of the population, with treatment services severely lacking in supportive resources (McCarthy et al., 2007).
While availability of substance use services within child welfare appears to need greater support, accessibility is also a significant issue, with two primary categories of barriers. First, youth in foster care face many of the same challenges that are common to other adolescents seeking substance use services. For example, many young people do not believe help is needed, reporting that substance use experimentation is normal for their age (Wu & Ringwalt, 2006). Indeed, rates of past 30-day alcohol and drug use are generally highest during young adulthood and tend to fade as individuals age (Substance Abuse and Mental Health Services Administration, 2017). These fluctuations also contain normative variations, with few people reporting serious problems, a bolus indicating experimentation, and a substantial minority not participating, with the vast majority graduating to abstinence or low risk use over time. Injunctive and descriptive norms about substance use, however, can skew perceptions about peer alcohol and drug use (Borsari & Carey, 2003; Neighbors, Geisner, & Lee, 2008), downplaying the need for treatment. For marijuana, in particular, there is a strong, growing national trend towards adolescents decreasing their perception of harm from smoking, with over 20% indicating that marijuana poses no risk of harm (Sarvet et al., 2018). Adolescents in the general population have also indicated that, once they have identified a need for services, they do not know where to find such help (CBHSQ, 2016). Youth in foster care are predominately directed to substance use services within community mental health, where navigation of yet another complex system of care can lead to poor utilization (Shin, 2005; Simms, Dubowitz, & Szilagyi, 2000). Confidentiality and stigma continue to be strong roadblocks for people of all ages, adolescents included (Rickwood, Deane, & Wison, 2007), preventing access to behavior change services. Finally, young people have reported difficulty articulating the extent of their problems to adult service providers, feeling that adults do not understand the complexity of their lives (Rice & Dolgin, 2008).
In addition to these barriers that cut across many young people, youth in foster care, as well as their caregivers, have reported important population-specific challenges to accessing substance use treatment. Abuse, neglect, and subsequent residential mobility do not provide a solid foundation from which to build close, healthy bonds. While the mismatch between maltreatment and interpersonal connectedness is more direct, frequent mobility (i.e., changing foster care providers, group homes, schools) can prevent young people from creating important relationships with caregivers whom they can trust. For example, over half of youth participating in the Midwest Study experienced 4 or more school changes and 3 or more home placements during their time in foster care, while over one-third attended more than 6 schools while placed within child welfare (Courtney, Terao, & Bost, 2004). As a result, youth in foster care may be reluctant to discuss stigmatizing issues, such as mental health and substance use, with adults whom they may have recently met and may not be entrusted to their care for very long.
This specific issue of trust was made very clear in early work our team conducted, attempting to create a substance use intervention for this vulnerable group. In our focus groups with foster care staff, parents, and administrators, we proposed the use of brief interventions, which have shown strong efficacy for reducing adolescent substance use in several contexts, including school settings (Mitchell et al., 2012), pediatric primary care (D’Amico, Miles, Stern, & Meredith, 2008), and emergency departments (Spirito et al., 2004). Participants felt that the bond necessary to share information about substance use would be difficult to form with youth in foster care, given the noted difficulties in establishing trust (Braciszewski, Moore, & Stout, 2014). They added that, if an interventionist and young person were to make a solid connection, taking that person away from the youth would repeat a negative pattern all too familiar to this population.
Finally, access to substance use services often requires identification and encouragement by social supports of the impacted individual (e.g., friends, family, teachers). Unfortunately, many foster care stakeholders do not receive appropriate training in recognizing and addressing adolescent substance use (American Academy of Child and Adolescent Psychiatry and Child Welfare League of America, 2002; Schroeder, Lemieux, & Pogue, 2008). Our focus groups with youth who had recently exited care echoed these statements, as most felt judged and punished for using alcohol and drugs, rather than receiving help from those responsible for their care (Braciszewski, Tran, et al., 2018). Foster parents have duly noted a need for such assistance. In a recent survey, 40% of current foster parents had fostered a youth with significant substance use problems, but less than two-thirds received any training for parenting a youth with these unique needs (Meyers, Kaynak, Clements, Bresani, & White, 2013). Taken together, successful interventions need to address the systematic barriers particular to this population.
1.3. Leveraging Technology to Improve Access to Care
As internet and mobile technology continue to permeate society across demographic characteristics (Pew Research Center, 2017a, 2017b), more psychosocial interventions are being delivered via computers, tablets, and cell phones, increasing access to empirically-supported treatment for many marginalized groups. Efficacy has been demonstrated using these media for several health care issues, including mental health (Ebert et al., 2015; Proudfoot et al., 2013; Richards & Richardson, 2012), smoking cessation (Bock et al., 2013; Whittaker, McRobbie, Bullen, Rodgers, & Gu, 2016), and substance use (Marsch, Carroll, & Kiluk, 2014; Mason, Ola, Zaharakis, & Zhang, 2015). In addition to the vast reach of these approaches, technology-driven interventions can promote honest reporting on sensitive topics (Butler, Villapiano, & Malinow, 2009) and be tailored to any unique population (Ondersma, Chase, Svikis, & Schuster, 2005; Tzilos Wernette, Plegue, Kahler, Sen, & Zlotnick, 2018), increasing the likelihood of effectiveness with cost savings at a premium. While behavior change may occur for some individuals, these low burden approaches also have the strong potential to facilitate connections and help-seeking behavior (National Action Alliance for Suicide Prevention Research Prioritization Task Force, 2014), opening people’s minds to traditional treatment they may not have otherwise sought. Finally, technology-based interventions can be available anywhere, at any time for each individual, reducing the negative impact of housing instability. In sum, the advantages noted here are well-suited to mitigate the barriers specific to youth in foster care, while offering empirically-supported interventions via a delivery system to which the population is accustomed to using.
1.4. Current Study
Even when compared to other at-risk populations (e.g., youth in child welfare not removed from the home), youth in foster care report very high rates of substance use, which then substantially increase upon emancipation. Unfortunately, reliable and acceptable programs for reducing substance use in this population rarely exist. Indeed, to our knowledge, there are no interventions specifically designed to address substance use among foster youth in the scientific literature. Thus, in response to the significant need for an accessible empirically-supported substance use intervention for youth who have experienced foster care, we developed and sought to test initial efficacy for iHeLP (Interactive Healthy Lifestyle Preparation), a computer- and mobile phone-based substance use intervention that dynamically adapts to fluid levels of motivation to change substance use. We hypothesized that, compared to a contact-control, youth receiving iHeLP would report higher abstinence rates from their drug of choice and that abstinence would increase over time. In addition, we hypothesized that intervention delivery would be feasible and acceptable to both groups.
2. Method
2.1. Participants
Young adults who had recently exited foster care were recruited from a large New England agency that provides post-foster care transition services. Inclusion criteria were: (1) 18–19 years old; (2) no more than 2 years removed from foster care; (3) a score of moderate or severe risk on the Alcohol, Smoking, and Substance Involvement Screening Test (WHO ASSIST Working Group, 2002); (4) not currently in or seeking substance abuse treatment; (5) owning a mobile phone; and (6) using text messaging at least weekly.
2.2. Procedure
Young people were recruited for initial eligibility screening through two primary mechanisms. First, flyers were posted throughout the agency, inviting young people to be screened for a general health study for former foster youth aged 18 or 19. Second, agency staff directly referred individuals to study interviewers using the same criteria; that is, 18 and 19 year old youth being served at the agency were asked if they were interested in hearing more about a health study. Study staff were provided a private office at the agency in which they could recruit participants and conduct eligibility screenings. Youth who were interested in learning more about the study were given a brief overview and invited to complete screening questions using a tablet PC and headphones for privacy and confidentiality. Once participants were identified as eligible, the research assistant explained the study goals and invited the young person to participate. Those who agreed were contacted by phone to set up a baseline interview, which generally took place at the participant’s home or a mutually-agreed upon public setting (e.g., library, coffee shop).
At the baseline interview, youth provided informed consent, completed study assessment measures, and engaged in the computerized component of iHeLP. Baseline interviews lasted approximately two hours, for which participants were given a $40 gift card. Youth were assigned to iHeLP or the control group using an urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994), which separated participants by gender and baseline substance use frequency. The urn design uses adaptive probabilities for group assignment that are systematically biased toward balance (for a full description see Stout et al., 1994). This procedure is most appropriate for small trials (Hedden, Woolson, & Malcolm, 2006), where imbalance on such factors can occur with larger probability (e.g., the last 5 participants being assigned to the same group within a coin flip design; Lachin, 1988). Both conditions were designed to last six months with follow-up interviews 3, 6, 9, and 12 months after the baseline assessment. Follow-up interviews lasted roughly 1–1.5 hours, for which participants were given a $25 gift card. The majority of study interviews were conducted in person (93 of 147), including all baseline interviews; the remainder were completed over the phone due to participant scheduling preference and other constraints. At the final interview, participants from both conditions completed an audio-recorded exit interview. Study procedures were reviewed and approved by (the Pacific Institute for Research and Evaluation Institutional Review Board).
2.3. Intervention
Those assigned to iHeLP completed a 20-minute computerized intervention that was theoretically-driven and consistent with Motivational Interviewing (MI; Miller & Rollnick, 2013), a client-centered counseling style that facilitates internal motivation to change through alignment with deeply held beliefs, values, and goals. MI-based approaches have been successful in reducing substance use among young people (Grant, Pedersen, Osilla, Kulesza, & D’amico, 2016; Jensen et al., 2011; Tevyaw & Monti, 2004), including in single-session formats (Burke, Arkowitz, & Menchola, 2003; Hettema, Steele, & Miller, 2005; Vasilaki, Hosier, & Cox, 2006). iHeLP is also guided by the FRAMES (Miller & Sanchez, 1994) approach to brief interventions. FRAMES involves six major elements found in effective, brief clinical trials (Miller & Sanchez, 1994): (1) Constructive, non-confrontational Feedback, tailored to the individual; (2) Emphasizing personal control and Responsibility; (3) Provision of nonjudgmental Advice through educational information or suggestions; (4) Offering a Menu of options or strategies; (5) Displaying Empathy; and (6) Promoting feelings of Self-efficacy.
The computerized component of iHeLP was developed and delivered using Computerized Intervention Authoring Software (CIAS; Ondersma et al., 2005), which allows for easily modifiable and tailored screening, assessment, and intervention. CIAS is unique in its approach by utilizing a three-dimensional cartoon character (Peedy the Parrot) to narrate intervention content and guide the participant through the session. Peedy is capable of over 50 animated expressions, which can maximally mimic one-on-one conversations. Participants interact with Peedy on a Tablet PC, wearing headphones to maximize confidentiality and understanding due to any possible reading difficulties.
iHeLP was tailored to participants in several ways. First, intervention content was specific to each participant’s substance of choice. If a young person endorsed hazardous use of more than one substance, they were asked which substance they wanted to “have a conversation with Peedy about.” This approach follows the MI principle of autonomy, where individuals are encouraged to express their right to and capacity for self-direction (Miller & Rollnick, 2013). All intervention participants then received substance-specific psychoeducation, presented in a gain-focused manner. Following a question about substance use goals (i.e., reducing/quitting vs. not), iHeLP was further tailored to individual readiness to change. Specifically, participants who did not express an interest in cutting down/quitting their substance of choice received intervention content consistent with engagement and building motivation to change (Miller & Rollnick, 2013). Youth who were interested in changing their level of substance use were provided an opportunity to state their reasons for change, set a change goal with Peedy, and review relapse prevention strategies. Upon completion, all participants were asked to provide a “Readiness Ruler” score; that is, “On a scale of 0 to 10, how ready are you to make a change (quit or cut down) in your use of [drug of choice]?”
The day after youth completed the computerized component of iHeLP, they began receiving one-way daily text messages tailored to their final readiness score, following an approach consistent with MI (Miller & Rollnick, 2013) and the Transtheoretical Model (TTM; Prochaska & DiClemente, 1992). Specifically, youth reporting a low readiness/interest in change (i.e., Pre-contemplation) after the computerized intervention received message content that appropriate for someone who may not see substance use as a problem (e.g., “How would your life be different if you reduced your alcohol use?”). Participants who reported a moderate or high level of readiness to change were treated in a similar fashion. That is, if participants reported moderate readiness for change, they received text message content suited for someone ambivalent about change; those who expressed a higher level of readiness were provided message content reflecting an active plan for making changes and support for relapse prevention.
However, the processes of behavior change are often fluid, which necessitate adaptation within interventions (Resnicow & Page, 2008). Thus, each week we sent participants “poll questions” to assess study outcomes (e.g., heavy drinking episodes) and readiness to change (via the Readiness Ruler). If participants responded with a Readiness Ruler score that would alter their TTM stage, weekly text message content, thereafter, reflected that change. Based on feedback from earlier iterations of iHeLP (Braciszewski, Tzilos Wernette, et al., 2018), participants also received weekly feedback on their substance use, as well as twice-monthly reminders of self-identified reasons to change, methods of change, and downsides to using substances.
Control group participants also completed a 20-minute intervention with Peedy the Parrot on the Tablet PC focused on diet and exercise, the structure of which mirrored iHeLP (i.e., psychoeducation, readiness, pros and cons, behavior change goals). One-way text message content involved general motivational statements and rhetorical questions (e.g., “Be yourself. Everyone else is already taken.”). Both arms of the study lasted six months, with participants receiving one text messages every day for the first three months and one message every other day, thereafter.
2.4. Measures
2.4.1. Feasibility
Feasibility was measured in several ways. We first calculated eligibility rates as the number of youth who met eligibility criteria divided by the number screened. We also examined enrollment rates defined as the number of young people who enrolled divided by the number eligible. Successful randomization was determined by examining frequency of condition assignment across gender and pre-baseline substance use frequency. Retention was measured using the rate of on-time follow-up interview completion and the rate of data collection completion, given that the primary outcome could be collected retrospectively. Finally, we assessed feasibility of intervention delivery using the response rate to the weekly poll questions, rate of disengagement with the text messaging component, and loss of cell phone coverage.
2.4.2. Acceptability
Following the computerized component of iHeLP, participants answered questions on ease of use, satisfaction with the narrator, overall interest in the computerized portion, respectfulness of the narrator, and the extent to which the computerized component was bothersome. These items were developed for use with CIAS software and have been used in previous studies (Ondersma et al., 2005). Items were assessed on a Likert scale ranging from 1 (not at all) to 5 (very much). In addition, participants provided qualitative feedback concerning intervention format, content, and utility during a short exit interview at the final follow-up. Specifically, we asked for global feedback about the computerized and texting components (e.g., things you liked, things you would change), length of the program (too long, too short), texting frequency, utility of speaking with a support person (e.g., professional, peer), experiences with the goal and feedback messages, and alternative topics to present in the intervention (e.g., trauma, depression).
2.4.3. Substance use frequency
The Timeline Follow Back (TLFB; Sobell & Sobell, 1992) captured self-reported substance use for a variety of drugs including tobacco, alcohol, marijuana, cocaine, amphetamines, inhalants, sedatives, hallucinogens, opioids, prescription opioids, bath salts, and synthetic cannabinoids. Participants reported the number of days they used each substance per week over the past 90 days or since the last interview. The TLFB is a widely used measure of substance use outcomes and has been shown to have robust reliability for myriad substances (Wray, Braciszewski, Zywiak, & Stout, 2016; Robinson, Sobell, Sobell, & Leo, 2014; Sobell & Sobell, 1992), methods of data collection (Sobell, Brown, Leo, & Sobell, 1996), and lengths of retrospective recall (Janssen, Braciszewski, Vose-O’Neal, & Stout, 2017). The primary outcome of interest was the percent days abstinent of each participant’s drug of choice. Given participant report of days used per week, we calculated percent days of abstinence in 30-day increments for each period of non-missing follow-up data.
Substance use frequency was also assessed via weekly poll questions, sent only to intervention participants, asking about drug of choice use in the last week (e.g., “How many days in the last week did you smoke marijuana? (PLEASE REPLY WITH A NUMBER, 0–7)”). To provide equal attention across groups, control participants were asked weekly about their consumption of healthy foods and use of exercise in the past week. Finally, participants were asked to provide 12-panel urine drug screens at each interview to assess both feasibility of data collection and accuracy of self-report on the TLFB.
2.4.4. Substance use consequences
The Short Inventory of Problems – Alcohol and Drugs (Blanchard, Morgenstern, Morgan, Lobouvie, & Bux, 2003) is a shortened version of the Inventory of Drug Use Consequences. It consists 15 self-report items on consequences from alcohol and drug consumption. Items (e.g., “I have taken foolish risks when I have been drinking/using drugs.”) refer to the past 3 months, are rated on a Likert scale (0 = never to 3 = daily or almost daily), and are summed for a total score.
2.4.5. Abstinence self-efficacy
The Brief Situational Confidence Questionnaire (Breslin, Sobell, Sobell, & Agrawal, 2000) is an 8-item measure of abstinence self-efficacy in varying situations (e.g., negative emotional/physical states, positive emotional/physical states, social pressure). Answers are provided on a Likert scale anchored at 0% and 100% confident that the participant can remain abstinent in that situation. Scores are then averaged across situations.
2.4.6. Depressive symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) is a 20-item self-report measure of past week depressive symptomatology and is noted for its wide use in depression research. Participants rate how much they have felt each item on a scale from 0 (rarely or none of the time) to 4 (most or all of the time). Items are summed with a score of 16 or higher suggesting clinically meaningful depression.
2.5. Data Analytic Strategy
We calculated descriptive statistics for the feasibility and acceptability data, as well as t-tests and chi-squares to compare iHeLP and control participants on demographic variables, baseline characteristics, poll question responses, and satisfaction with the computerized component. Audio recordings of exit interviews were transcribed verbatim for analysis. Given that the questions were direct (e.g., “What did you think of the texting occurring once per day, then once every other day?”), a thematic analysis was not appropriate. Rather, we examined the transcripts for common strengths and weaknesses, count data on specific aspects of iHeLP (e.g., intervention duration: shorter, longer, just right), and suggestions to modify iHeLP. These analyses were conducted using Dedoose (SocioCultural Research Consultants, 2016), a web-based software for facilitating mixed methods data analysis.
When analyzing all outcome data, we used repeated measures hierarchical linear modeling and MPlus software (Muthén & Muthén, 1998–2015) to investigate group differences in monthly percent days abstinent (PDA) for drug of choice at each of the four follow-up interviews, as well as linear change over the full 12-month follow-up period. HLM is robust to missing data, allows for comparison across more than two waves of data, and is most appropriate for nested data, such as these (i.e., observations nested within individuals; Raudenbush & Bryk, 2002; Singer & Willett, 2003). Mplus uses Full Information Maximum Likelihood estimation of missing values, which computes parameter estimates on the basis of all available data, including incomplete cases (Muthén & Muthén, 1998–2015).
To examine TLFB outcomes and intervention effects over the course of the study (e.g., immediate effects, sustained effects), we first calculated monthly rates (i.e., past 30 days) of drug of choice PDA across the 12-month study period. We then ran individual HLM analyses with time centered at different follow-up points (i.e., 1, 3, 6, 9, and 12 month). In each of these models, intervention condition was entered as a dichotomous variable (iHeLP: 1; control: 0) predicting both intercept (i.e., group differences in past 30-day substance use at that time point) and slope (i.e., group differences in monthly substance use change over time). We also used pre-intervention data (aggregated TLFB data from the 90 days prior to baseline) as a covariate in TLFB outcome analyses, predicting both intercept and slope. Similarly, we used HLM to examine group differences and changes over time in abstinence self-efficacy and substance use consequences. Intervention condition and baseline levels of these variables were used to predict both intercept (at 3, 6, 9, and 12 months) and slope. Finally, we calculated the correlation between weekly TLFB and poll question data on days of drug of choice use in the previous week.
3. Results
3.1. Feasibility
Eligibility rates were high; of the 127 youth who were screened, nearly two-fifths (39%; n = 50) met the inclusion criteria endorsing, among other things, at least a moderate problem with substance use. Reasons for being ineligible were infrequent substance use (40%), no history of substance use (35%), no cell phone (18%), and other (e.g., doesn’t text, currently in treatment; 7%). Of the 50 eligible young people, 33 (66%) enrolled and were randomized to one of the study conditions. Those who did not participate cited non-interest (35%) or being too busy to participate (24%); the remainder could not be contacted to determine a specific reason for non-enrollment. Randomization was equivalent across gender (χ2 = 0.02, p = 0.88) and baseline substance use frequency (χ2 = 0.79, p = 0.37).
The final sample was slightly more female (n = 17) than male, while 42% indicated a Hispanic/Latino ethnicity. With regard to racial categories, 52% were Caucasian, 27% were African-American, 18% endorsed more than one race, and 3% indicated their race as “other.” Participants were, on average, 18.91 years old (SD = 0.47), had 11.56 years of education (SD = 0.72, range = 10 – 12), were in foster care for 4.80 years (SD = 4.13, range = 0.2 – 17), and had 4.55 placements (SD = 3.02, range = 1 – 13). More than half (58%) were employed. Most participants (72%; n = 24) scored in the moderate to severe range in only one ASSIST substance category, while four met this threshold for two substances and five others were rated as having problematic substance use for three to six categories. Demographic characteristics for each group are shown in Table 1.
Table 1.
Baseline demographics for the intervention and control groups.
| iHeLP (n = 14) | Control (n = 19) | ||
|---|---|---|---|
| Variable | n (%) | χ2 | |
| Gender | 0.02 | ||
| Female | 7 (50) | 10 (53) | |
| Ethnicity | 0.57 | ||
| Hispanic/Latino | 7 (50) | 7 (37) | |
| Race | 1.59 | ||
| Caucasian | 4 (29) | 5 (26) | |
| Black/African American | 7 (50) | 10 (53) | |
| Other | 1 (7) | 0 (0) | |
| More than one | 2 (14) | 4 (21) | |
| Employed | 12 (63) | 7 (50) | 0.57 |
| CES-D depression | 9 (64) | 13(68) | 0.06 |
| M (SD) | t | ||
| Age | 18.99 (0.42) | 18.84 (0.50) | −0.94 |
| Years of education | 11.54 (0.78) | 11.58 (0.69) | 0.15 |
| Number of foster care placements | 4.79 (3.24) | 4.37 (2.93) | −0.39 |
| Years in foster care | 4.11 (2.97) | 5.32 (4.83) | 0.82 |
| Number of substance use problems | 1.50 (1.16) | 1.79 (1.58) | 0.58 |
| ASSIST score on drug of choice | 17.79 (7.59) | 17.16 (10.64) | −0.19 |
| SIP-AD total score | 5.43 (4.16) | 4.47 (4.27) | −0.64 |
| BSCQ average score | 55.71 (27.95) | 63.95 (25.65) | 0.88 |
| CES-D total score | 25.00 (13.82) | 20.95 (10.61) | −0.95 |
| Drug of choice PDA1 | |||
| Pre-baseline | 34.05 (40.00) | 26.32 (35.38) | −0.59 |
| 1 month | 60.46 (38.43) | 39.36 (38.51) | −1.51 |
| 3 months | 53.02 (39.42) | 37.90 (39.26) | −1.06 |
| 6 months | 65.48 (36.25) | 30.49 (41.14) | −2.39* |
| 9 months | 62.80 (38.87) | 29.91 (39.38) | −2.20* |
| 12 months | 65.26 (41.10) | 40.56 (38.25) | −1.55 |
Percent days abstinent;
p<.05.
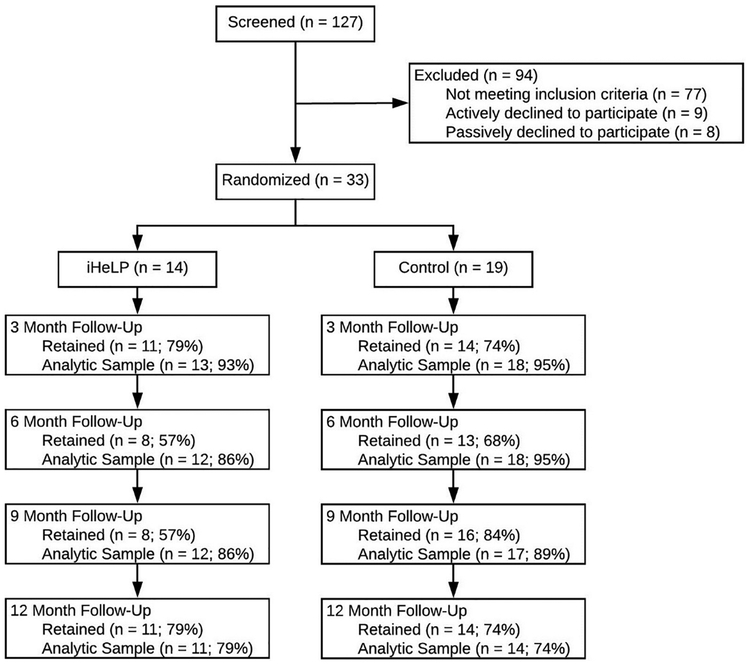
On time follow-up interview retention ranged from 64% to 76%, while data retention (i.e., retrospective TLFB reports) averaged 87% across the four waves of data collection (see CONSORT diagram). Specifically, follow-up data rates were 94% (3 months), 91% (6 months), 88% (9 months, and 76% (12 months). Outcome data were collected for at least one follow-up interview for all but two participants, while all but three participants provided outcome data for at least two subsequent interviews. No differences were found when comparing youth who did not complete any of the follow-up interviews (n = 2) and participants who were retained. Furthermore, groups did not differ with regard to missing data, either in absolute terms (i.e., any missing data; iHeLP: 3, control: 5, χ2 = 0.10, p = 0.75) or volume (i.e., months of missing data; iHeLP: M(SD) = 1.57 (3.69), control: 1.21 (2.97), t = −0.31, p = 0.76).
Finally, response to the weekly poll questions was very good, with an aggregate response rate of 80% and each participant averaging 73% (SD = 29, range: 0 to 100). Mean poll question response rates for iHeLP (M = 76, SD = 31) did not significantly differ from the control group (M = 71, SD = 28; t(31) = −0.51, p = 0.6109). Throughout the study, only one participant disengaged from the text messaging component completely after the baseline interview, as evidenced by a 0% poll question response rate. Approximately half of participants changed their phone number throughout the study, though new phone numbers were obtained within a week or less, as missed poll questions prompted use of participant locator contacts. Two participants lost cell phone coverage during the study for more extended periods of time, re-gaining coverage within six weeks. All other participants maintained consisted cell phone coverage over the study duration. Finally, three participants had extended periods of absence from receiving text messaging content due to long-term hospitalization (n = 2) and jail (n = 1).
3.2. Acceptability
Satisfaction with the computerized component, collected at the end of the baseline interview, was positive, with most participants liking the narrator, finding the computer easy to work with, thinking the narrator was interesting to work with, and finding the narrator to be respectful; participants did not find Peedy or the computerized portion as a whole to be bothersome (see Table 2). The intervention and control groups did not significantly differ on any of these measures.
Table 2.
Immediate satisfaction with the computerized brief intervention (CBI).
| Total (n = 33) | iHeLP (n = 14) | Control (n = 19) | ||
|---|---|---|---|---|
| Item | M (SD) | t | ||
| Liked working with narrator | 4.00 (1.12) | 3.93 (1.07) | 4.05 (1.18) | 0.31 |
| SBI was easy to use | 4.91 (0.38) | 4.79 (0.58) | 5.00 (0.00) | 1.38 |
| Narrator was interesting to work with | 3.97 (1.13) | 3.86 (1.03) | 4.05 (1.22) | 0.48 |
| Narrator was respectful | 4.94 (0.24) | 4.93 (0.27) | 4.95 (0.23) | 0.22 |
| SBI was bothersome | 1.67 (1.02) | 1.43 (0.85) | 1.84 (1.12) | 1.16 |
Twenty-one youth completed an exit interview (iHeLP: 10, control: 11) regarding their interaction with the intervention. All participants gave positive comments about the approach, particularly the texting aspect. Participants felt it was helpful to have the computer read all of the content and that the questions made them think more deeply about their choices. A participant summed up this feeling well:
“…the questions that [Peedy] asked made me want to be healthier…after being specific about my lifestyle, it made me want to [be healthier].”
The only negative assessment of the computerized component that was mentioned with frequency was the “old looking” presentation on the tablet. Users indicated that the interface was not smooth and the animation was slow. Participants had strongly positive feelings about the texting component, stating that it made them think, built motivation, was easy to use, and felt like someone else was caring about their health. New iHeLP components suggested in our previous open trial (biweekly goal reminders and weekly feedback on substance use; Braciszewski, Tzilos Wernette, et al., 2018) were very well received. All participants indicated that the goal reminders were helpful to keep on track and that feedback on progress was empowering and provided specific motivation for not smoking marijuana. One person reported:
“I think it’s cool that they’re congratulating you on the progress that you’re making. It’s nice to hear that you’re making progress and that…people see it.”
Salient suggestions for future iterations of iHeLP included more information on the overlap of substance use with depression, anxiety, and trauma symptoms, continuing the intervention for longer than six months, allowing users to increase/decrease the number of texts they receive throughout the intervention, and providing a virtual space for anonymously communicating with other peers and professionals about specific troubles.
3.3. Outcomes
After controlling for substance use in the three months prior to baseline, iHeLP participants reported significantly more percent days abstinent (PDA) from their drug of choice on the TLFB compared to the control group at each wave of data collection (Table 3). Effect sizes for these differences were medium, ranging from 0.32 to 0.56. Receipt of iHeLP was not significantly associated with linear growth (i.e., increases) in drug of choice PDA over time (β = 1.24, p = 0.42). Two control group participants screened into the study as low risk for marijuana problems, but moderate risk for alcohol problems (i.e., drug of choice = alcohol), while the remainder of participants reported marijuana as their drug of choice. Subsequently, at the baseline interview and 1-month follow-up, these two participants reported very low alcohol use and frequent marijuana use. Thus, we re-ran the analyses using marijuana PDA outcomes for all participants. Results were slightly stronger, with effect sizes ranging from 0.40 to 0.62. There was also an added significant group effect at 1-month. Retrospective weekly TLFB data and weekly poll question data on drug of choice use were highly correlated (r(201) = 0.56, p < .0001). Urine drug screen completion rates at each interview wave ranged from 18% to 39%, precluding formal data analyses.
Table 3.
Reported percent days abstinent (PDA) from drug of choice over time.
| β (SE) | t | d (95% CI) | |
|---|---|---|---|
| 1 Month | |||
| Intercept (β00) | 17.60 (6.56) | 2.68** | |
| Pre-baseline PDA (β01) | 0.72 (0.12) | 6.13*** | |
| Group (β02) | 15.68 (8.83) | 1.78 | 0.32 (−0.40, 1.04) |
| 3 Months | |||
| Intercept (β00) | 16.36 (5.47) | 2.99** | |
| Pre-baseline PDA (β01) | 0.70 (0.10) | 7.12*** | |
| Group (β02) | 18.15 (7.37) | 2.46* | 0.46 (−0.26, 1.18) |
| 6 Months | |||
| Intercept (β00) | 14.50 (5.43) | 2.67** | |
| Pre-baseline PDA (β01) | 0.66 (0.10) | 6.83*** | |
| Group (β02) | 21.86 (7.36) | 2.97** | 0.56 (−0.16, 1.29) |
| 9 Months | |||
| Intercept (β00) | 12.64 (7.23) | 1.75 | |
| Pre-baseline PDA (β01) | 0.63 (0.13) | 4 89*** | |
| Group (β02) | 25.56 (9.81) | 2.60** | 0.47 (−0.26, 1.19) |
| 12 Months | |||
| Intercept (β00) | 10.78 (9.91) | 1.09 | |
| Pre-baseline PDA (β01) | 0.60 (0.18) | 3.39** | |
| Group (β02) | 29.27 (13.45) | 2.18* | 0.40 (−0.32, 1.12) |
| Slope | |||
| Intercept (β00) | −0.62 (1.14) | −0.55 | |
| Pre-baseline PDA (β01) | −0.01 (0.02) | −0.54 | |
| Group (β02) | 1.24 (1.54) | 0.80 |
p < .05;
p < .01;
p < .001
Among iHeLP participants, Readiness Ruler scores increased significantly over time (β = 0.132, p < 0.05), covarying for baseline readiness to change. After accounting for baseline levels of situational confidence, group differences were not significant at 3, 6, 9, or 12 month follow-up interviews. iHeLP participants, however, did have significantly steeper increases in situational confidence over time (β = 2.74, p < 0.05). Groups did not significantly differ at any time point or in change over time on substance use consequences.
4. Discussion
The current study suggests that a technology-based substance use intervention is acceptable to youth exiting the foster care system. In addition, iHeLP proved feasible to deliver and showed excellent preliminary evidence that such an approach could be impactful with regard to reducing marijuana use in this population. Access to substance use services for this vulnerable population remains sparse (McCarthy et al., 2007) and may decline over time, as youth exit the system (Ringeisen, Casanueva, Urato, & Stambaugh, 2009); thus, the design of attractive and accessible means of reducing alcohol and drug use among youth in foster care is a high priority. While more work remains to be done, there is a strong foundation from which to expand and improve technology-based substance use services for youth who are exiting the foster care system.
Given the familiarity young people have with technology and their preference for using technology for health-related concerns (Pilowsky & Wu, 2013), we were not surprised that iHeLP was acceptable to participants. Indeed, the similarity in satisfaction scores between the intervention and control groups suggests, at least partly, that this modality appeals to the population, irrespective of content. In fact, given that many young people are reluctant to discuss substance use with treatment providers, it is conceivable that the control group may have reported higher satisfaction ratings, with the intervention group turned off by having to discuss such issues. Our finding that the ratings were not significantly different suggests that our nonthreatening intervention tool may have an important advantage over traditional approaches. Results from the exit interviews further support this interpretation, as satisfaction with the text messaging component mirrored our previous quantitative work in this area, where youth exiting care were highly supportive of using mobile phones to deliver intervention content (Braciszewski, Tzilos Wernette, et al., 2018). In addition, participants suggested that we offer iHeLP for longer than six months and extend care beyond the text messages to contact with other peers or professionals. Participants clarified that these would not be ongoing sessions, but rather check-ins, as needed. Other researchers have incorporated similar models into technology-based interventions, including a weekly “The Doctor Is In” chat room for participants in a Facebook-based smoking cessation intervention (Ramo et al., 2015) and a discussion board for those in an online alcohol intervention (Linke, Brown, & Wallace, 2004). Such features, moderated by the research team or a clinician, could augment care by increasing perceived social support and motivation for change. While social support is one of the strongest predictors of long-term substance use recovery (Kelly, Hoeppner, Stout, & Pagano, 2012), youth who have been exposed to maltreatment and other ACEs report smaller social support networks (Ford, Clark, & Stansfeld, 2011). Thus, researchers and clinicians should leverage all available efforts to increase the prevalence of this key factor in decreasing problematic substance use.
Our messages covered the topics of depression and anxiety at a cursory level; however, exit interviews revealed that these topics are very salient to youth exiting care. Indeed, nearly two-thirds of our sample reached the CES-D threshold for depression at baseline, which is over six times higher than national rates for young adults (10.6%; Center for Behavioral Health Statistics and Quality, 2017). In addition, prevalence rates of Posttraumatic Stress Disorder (PTSD) range from 14% to 16% (Courtney et al., 2004; McMillen et al., 2005) for youth in foster care, a level that is twice as high as the general population (Merikangas et al., 2010). Given the strong connections between exposure to trauma, PTSD, major depression, and substance use (Giaconia et al., 2000; Kilpatrick et al., 2003), future intervention development work should investigate the addition of content that addresses the reciprocal influence of mental health and substance use.
Feasibility of recruitment, enrollment, and intervention delivery was also strong. Eligibility rates reached nearly 40%; while this provides reassurance for researchers interested in testing new substance use interventions with youth exiting care, it also supports previous work identifying these vulnerable young people as substantially at risk for problematic substance use (Pilowsky & Wu, 2006; Vaughn, Ollie, McMillen, Scott Jr, & Munson, 2007; White, O’Brien, White, Pecora, & Phillips, 2008). Our threshold for substance use – scoring in the moderate or severe range on the ASSIST – is relatively high. Thus, it is concerning that such a large number of individuals would meet this criterion.
Enrollment was also successful, given the noted difficulties recruiting high-risk and vulnerable populations and the lower recruitment rates noted for prevention versus treatment studies (Cooper et al., 2015; Cramer & Spilker, 1991). In a similar brief alcohol intervention pilot study, 81 youth were identified as eligible, yet 74% completed the baseline survey and 61% of individuals assigned to the intervention condition actually received the intervention (D’Amico et al., 2008), owing to delays between screening/surveying and intervention implementation, as was the case with our sample. Indeed, a recent text messaging study reported higher enrollment rates (87%; Suffoletto, Callaway, Kristan, Kraemer, & Clark, 2012) using procedures that involved enrollment immediately upon a positive screen. Other text messaging interventions for substance use of similar duration to ours report enrollment rates between 28% and 92% (Bock et al., 2013; Free et al., 2011; Free et al., 2009; Haug, Meyer, Schorr, Bauer, & John, 2009; Haug, Schaub, Venzin, Meyer, & John, 2013; Moore et al., 2013; Naughton, Prevost, Gilbert, & Sutton, 2012; Whittaker et al., 2011). Although our rates were similar to that of others, future work in this area may benefit from conducting the baseline intervention immediately upon positive screening. Overall, we feel confident that interest in a technology-based intervention, desire to understand more about one’s substance use, or a combination of both were strong motivating factors in choosing to enroll. Indeed, our previous work has indicated that this population is eager for a substance use intervention, provided it fits their needs (Braciszewski, Tran, et al., 2018; Braciszewski, Tzilos Wernette, et al., 2018).
Retention was also solid, with only two participants dropping out within weeks of the baseline interview and responding to less than 30% of the poll questions. While most technology-based intervention studies have not involved long-term follow-up (Kazemi et al., 2017), 3- to 9-month retention rates have ranged from 34% to 87% (Moore et al., 2013; Shrier, Rhoads, Burke, Walls, & Blood, 2014; Suffoletto et al., 2012; Suffoletto et al., 2015). One study utilizing a smartphone application reported 12-month retention rates of 78% (Gustafson et al., 2014); thus, our overall rate of 87% and 12-month rate of 76% stand near the top of other reported work. Participants were also responsive throughout the study, via poll questions and interviews. Over three-quarters provided a full year of substance use data after the baseline interview. Given that nearly 50% of former foster youth have reported significant housing instability and subsequent mobility (Fowler, Toro, & Miles, 2009) and up to 25% have reported criminal justice involvement (Courtney et al., 2005), we are very pleased with these follow-up rates. With regard to poll questions, we are equally encouraged by the 80% overall response rate, especially given the timeframe of our study (6 months) compared to others that collect real time data in the natural environment (1–2 months; Garcia et al., 2014; Gwaltney, Bartolomei, Colby, & Kahler, 2008; Phillips, Phillips, Lalonde, & Dykema, 2014; Schnall et al., 2013). Other recent text messaging studies have reported long-term response rates ranging from 43% to 81% (Naughton et al., 2012; Shrier et al., 2014; Suffoletto et al., 2014), though most have reported significant non-response to texts, a noted flaw in many mHealth-related studies (Kazemi et al., 2017). Finally, many participants changed their phone numbers over the course of the study, briefly reducing their exposure to intervention content or, post-intervention, their ability to respond to poll questions. Our methods for obtaining updated contact information proved robust; future work in this area will likely require such methods, as vulnerable populations may be at risk of losing cell phone coverage more often than individuals in the general population.
Our small pilot trial also showed moderate effect sizes for substance use outcomes (namely, marijuana). Computer-based interventions for alcohol and drugs have shown success in previous trials, though their impact almost always subsides after 6–9 months (Moore, Fazzino, Garnet, Cutter, & Barry, 2011; Rooke, Thorsteinsson, Karpin, Copeland, & Allsop, 2010), even with booster sessions. The addition of a dynamically-tailored text messaging component extended these effects to one year, six months after the end of the intervention, a rare finding in the literature on technology-based interventions (Kazemi et al., 2017). Given the low cost associated with these approaches (Newman, Szkodny, Llera, & Przeworski, 2011), reduced staff burden (Bishop, Bryant, Giles, Hansen, & Dusenbury, 2006), and our participants’ desire to receive messaging for a longer period of time than we proposed, this approach has strong potential for sustained impact.
4.1. Limitations
Technology-based interventions will not be a panacea for all health-related problems and our study is not without limitations. First, our trial was small and while follow-up data collection was very good, a fully-powered trial will be more informative as to whether iHeLP is truly a feasible, long-term intervention for youth exiting foster care. Second, biological confirmation of substance use proved to be difficult. Participants often refused to provide urine drug screens, stating that they had many negative experiences with these requests from case managers, group home leaders, and other authority figures, which fits with reports in our previous work (Braciszewski, Tran, et al., 2018). However, the majority of our participants did not achieve or desire to achieve complete abstinence; rather, most significantly reduced the frequency with which they smoked marijuana. Such a change would only be revealed on a very sensitive urine drug screen, the resources for which were not available in this small trial. Third, a goal of this study was to develop an intervention that could address any one of 13 substances often used by young people. However, each of our participants ultimately reported using marijuana most frequently. Thus, we cannot conclude whether the results of this study are generalizable to the use of other drugs. Finally, all of our data are retrospective self-report; however, the TLFB has shown very strong reliability at lengthy follow-up time periods (Janssen, Braciszewski, Vose-O’Neal, & Stout, 2017). We are also encouraged by the high correlation between the TLFB data and the more proximal poll question data on weekly substance use.
4.2. Future Research
As researchers and clinicians continue to develop and provide innovative substance use services for youth in and exiting from foster care, asking for youth input in the design and execution of different approaches is essential. Previous work has indicated that when individuals are involved in the creation of interventions, they are more likely to engage (D’Amico & Edelen, 2007). As the landscape of marijuana use in the US continues to shift with the policy changes and legalization of recreational use across several states, interventions will need to address increased use among youth. As we refine iHeLP, we plan to incorporate the suggestions noted here, namely the ability to contact others for social support and answers to health-related questions, and allowing some components of the intervention to be customizable (e.g., frequency of text messages). Given the interplay between mental health status and substance use, it may be useful to have poll questions to track both domains at the same time. Relatedly, participants may reduce one substance while increase the use of another; thus, future technology-based interventions should adapt to such changes and provide tailored content relevant to current behavior. Furthermore, this type of intervention may prove valuable with other populations that could benefit from long-term monitoring and support without major involvement of treatment professionals. Such populations could be found among former prisoners, persons in remote areas with less access to traditional intervention services, armed forces deployed remotely, or underage youth who typically do not access traditional services. Further research needs to be done on the optimum duration of continued support for different populations, and different addiction and psychological severity. If it is to be used for long periods of time, further experimentation needs to be done on tailoring the frequency of contact as goals are met, or the risk of relapse may be enhanced. Our computer and text messaging approach may be less suitable for persons with high levels of psychological impairment (e.g., high levels of depression, anxiety, or psychotic symptoms) or cognitive impairment. In the near future, our work will focus on refining iHeLP and testing it within a fully-powered randomized controlled trial, with additional measures of cost-effectiveness. If iHeLP were to be implemented within child welfare settings, a financial analysis of its impact would be paramount.
Fig. 1.
CONSORT diagram. Retained refers to the number of participants providing data at the time of the interview; analytical samples are higher due to retrospective reporting at future interviews.
Highlights.
Youth who have experienced foster care report high levels of substance use.
Traditional approaches to substance use service provision may not meet the unique needs of this population.
We developed a computer- and mobile phone-based intervention for reducing substance use among youth exiting foster care (iHeLP).
Feasibility, acceptability, and preliminary efficacy of iHeLP were strong.
Technology-based interventions may be an engaging alternative to reduce substance use among youth exiting foster care.
Acknowledgements
This work was supported by the National Institute on Drug Abuse (R34DA034822).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
References
- American Academy of Child and Adolescent Psychiatry and Child Welfare League of America. (2002). AACAP/CWLA policy statement on mental health and substance use screening and assessment of children in foster care. Retrieved October 31, 2016, from www.aacap.org [Google Scholar]
- Bishop D, Bryant KS, Giles SM, Hansen WB, & Dusenbury L (2006). Simplifying the delivery of a prevention program with web-based enhancements. Journal of Primary Prevention, 27(4), 433. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Lobouvie EW, & Bux DA (2003). Assessing consequences of substance use: Psychometric properties of the inventory of drug use consequences. Psychology Of Addictive Behaviors, 17(4), 328–331. Retrieved from http://ezproxy.pire.org:2048/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=14640829&site=ehost-live [DOI] [PubMed] [Google Scholar]
- Bock BC, Heron KE, Jennings EG, Morrow KM, Cobb V, Magee JC, … Foster R (2013). A text message delivered smoking cessation intervention: The initial trial of TXT-2-QUIT, a randomized, controlled trial. JMIR MHealth and UHealth, 1(2), e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, & Carey KB (2003). Descriptive and injunctive norms in college drinking: A meta-analytic integration. Journal of Studies on Alcohol, 64(3), 331–341. doi: 10.15288/jsa.2003.64.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braciszewski JM, & Stout RL (2012). Substance use among current and former foster youth: A systematic review. Children and Youth Services Review, 34(12), 2337–2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braciszewski JM, Moore RS, & Stout RL (2014). Rationale for a new direction in foster youth substance use disorder prevention. Journal of Substance Use, 19(1–2), 108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braciszewski JM, Tran TB, Moore RS Bock BC Tzilos GK Chamberlain P … Vose-O'Neal A (2018). Feeling heard and not judged: Foster youths’ perspectives on substance use services. Child Maltreatment, 23(1), 85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braciszewski JM, Tzilos Wernette GK, Moore RS Tran TB Bock BC Stout RL, … Vose-O’Neal A (2018). Developing a tailored substance use intervention for youth exiting foster care. Child Abuse & Neglect, 77, 211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramlett MD, & Radel LF (2014). Adverse family experiences among children in nonparental care, 2011–2012. National Health Statistics Report, 74(4), 1–8. [PubMed] [Google Scholar]
- Breslin FC, Sobell LC, Sobell MB, & Agrawal S (2000). A comparison of a brief and long version of the Situational Confidence Questionnaire. Behaviour Research and Therapy, 38(12), 1211–1220. Retrieved from http://ezproxy.pire.org:2048/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=11104185&site=ehost-live [DOI] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, & Menchola M (2003). The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology, 71(5), 843–861. [DOI] [PubMed] [Google Scholar]
- Butchart A, Harvey AP, Mian M, & Furniss T (2006). Preventing child maltreatment: A guide to taking action and generating evidence. Geneva: World Health Organization. [Google Scholar]
- Butler SF, Villapiano A, & Malinow A (2009). The effect of computer-mediated administration on self-disclosure of problems on the Addiction Severity Index. Journal of Addiction Medicine, 3(4), 194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2016). 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2017). 2016 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Cooper CL, Hind D, Duncan R, Walters S, Lartey A, Lee E, & Bradburn M (2015). A rapid review indicated higher recruitment rates in treatment trials than in prevention trials. Journal of Clinical Epidemiology, 68(3), 347–354. [DOI] [PubMed] [Google Scholar]
- Courtney ME, Dworsky A, Ruth G, Keller T, Havlicek J, & Bost N (2005). Midwest evaluation of the adult functioning of former foster youth: Outcomes at age 19. Chicago, IL: Chapin Hall Center for Children at the University of Chicago. [Google Scholar]
- Courtney ME, Terao S, & Bost N (2004). Midwest evaluation of the adult functioning of former foster youth: Conditions of youth preparing to leave state care. Chicago, IL: Chapin Hall Center for Children at the University of Chicago. [Google Scholar]
- Cramer JA, & Spilker B (1991). Patient compliance in medical practice and clinical trials (Vol. 1). New York: Raven Press [Google Scholar]
- D’Amico EJ, & Edelen MO (2007). Pilot test of Project CHOICE: A voluntary afterschool intervention for middle school youth. Psychology of Addictive Behaviors, 21(4), 592–598. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JN, Stern SA, & Meredith LS (2008). Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment, 35(1), 53–61. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Chou SP, Ruan WJ, & Grant BF (2008). Age at first drink and the first incidence of adult‐onset DSM‐IV alcohol use disorders. Alcoholism: Clinical And Experimental Research, 32(12), 2149–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, & Anda RF (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics, 111(3), 564–572. [DOI] [PubMed] [Google Scholar]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, & Anda RF (2006). Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health, 38(4), e1–e10. [DOI] [PubMed] [Google Scholar]
- Ebert DD, Zarski A-C, Christensen H, Stikkelbroek Y, Cuijpers P, Berking M, & Riper H (2015). Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. PLoS One, 10(3), e0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford E, Clark C, & Stansfeld SA (2011). The influence of childhood adversity on social relations and mental health at mid-life. Journal of Affective Disorders, 133(1), 320–327. [DOI] [PubMed] [Google Scholar]
- Fowler PJ, Toro PA, & Miles BW (2009). Pathways to and from homelessness and associated psychosocial outcomes among adolescents leaving the foster care system. American Journal of Public Health, 99(8), 1453–1458. doi: 10.2105/ajph.2008.142547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Weiwei Z, … Roberts I (2011). Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet, 378(9785), 49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C, Whittaker R, Knight R, Abramsky T, Rodgers A, & Roberts I (2009). Txt2stop: a pilot randomised controlled trial of mobile phone-based smoking cessation support. Tobacco Control, 18(2), 88–91. [DOI] [PubMed] [Google Scholar]
- Gabrielli J, Jackson Y, & Brown S (2016). Associations between maltreatment history and severity of substance use behavior in youth in foster care. Child Maltreatment, 21(4), 298–307. [DOI] [PubMed] [Google Scholar]
- Garcia C, Hardeman RR, Kwon G, Lando-King E, Zhang L, Genis T, … Kinder E (2014). Teenagers and texting: Use of a youth ecological momentary assessment system in trajectory health research with latina adolescents. JMIR MHealth and UHealth, 2(1), e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Hauf AC, Paradis AD, Wasserman MS, & Langhammer DM (2000). Comorbidity of substance use and post-traumatic stress disorders in a community sample of adolescents. American Journal of Orthopsychiatry, 70(2), 253–262. doi: 10.1037/h0087634. [DOI] [PubMed] [Google Scholar]
- Grant S, Pedersen ER, Osilla KC, Kulesza M, & D’amico EJ (2016). Reviewing and interpreting the effects of brief alcohol interventions: Comment on a Cochrane review about motivational interviewing for young adults. Addiction, 111(9), 1521–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih M-Y, Atwood AK, Johnson RA, Boyle MG, … Dillenburg L (2014). A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA psychiatry, 71(5), 566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwaltney CJ, Bartolomei R, Colby SM, & Kahler CW (2008). Ecological momentary assessment of adolescent smoking cessation: A feasibility study. Nicotine & Tobacco Research, 10(7), 1185–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug S, Meyer C, Schorr G, Bauer S, & John U (2009). Continuous individual support of smoking cessation using text messaging: a pilot experimental study. Nicotine & Tobacco Research, 11(8), 915–923. [DOI] [PubMed] [Google Scholar]
- Haug S, Schaub MP, Venzin V, Meyer C, & John U (2013). Efficacy of a text message-based smoking cessation intervention for young people: a cluster randomized controlled trial. Journal of medical Internet research, 15(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Woolson RF, & Malcolm RJ (2006). Randomization in substance abuse clinical trials. Substance Abuse Treatment, Prevention, and Policy, 1(1), 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, & Miller WR (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1, 91–111. [DOI] [PubMed] [Google Scholar]
- Janssen T, Braciszewski JM, Vose-O’Neal A, & Stout RL (2017). A comparison of long- vs. short-term recall of substance use and HIV risk behaviors. Journal of Studies on Alcohol and Drugs, 78(3), 458–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, & Steele RG (2011). Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology, 79(4), 433–440. [DOI] [PubMed] [Google Scholar]
- Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA, & Matta LA (2017). A systematic review of the mHealth interventions to prevent alcohol and substance abuse. Journal of Health Communication, 22(5), 413–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Hoeppner B, Stout RL, & Pagano ME (2012). Determining the relative importance of the mechanisms of behavior change within Alcoholics Anonymous: A multiple mediator analysis. Addiction, 107(2), 289–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71(4), 692. [DOI] [PubMed] [Google Scholar]
- King KM, & Chassin L (2007). A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. Journal of Studies on Alcohol and Drugs, 68(2), 256–265. [DOI] [PubMed] [Google Scholar]
- Lachin JM (1988). Properties of simple randomization in clinical trials. Controlled Clinical Trials, 9(4), 312–326. [DOI] [PubMed] [Google Scholar]
- Linke S, Brown A, & Wallace P (2004). Down your drink: a web-based intervention for people with excessive alcohol consumption. Alcohol and Alcoholism, 39(1), 29–32. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Carroll KM, & Kiluk BD (2014). Technology-based interventions for the treatment and recovery management of substance use disorders: A JSAT special issue. Journal of Substance Abuse Treatment, 46(1), 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M, Ola B, Zaharakis N, & Zhang J (2015). Text messaging interventions for adolescent and young adult substance use: A meta-analysis. Prevention Science, 16(2), 181–188. [DOI] [PubMed] [Google Scholar]
- McCarthy J, Van Buren E, & Irvine M (2007). Child and family services reviews: 2001–2004: A mental health analysis. Washington, DC: Georgetown University. [Google Scholar]
- McMillen JC, Zima BT, Scott LD, Auslander WF, Munson MR, Ollie MT, & Spitznagel EL (2005). Prevalence of psychiatric disorders among older youths in the foster care system. Journal of the American Academy of Child & Adolescent Psychiatry, 44(1), 88–95. doi: 10.1097/01.chi.0000145806.24274.d2. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J. p., Burstein M, Swanson SA, Avenevoli S, Cui L, … Swendsen J (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers K, Kaynak Ö, Clements I, Bresani E, & White T (2013). Underserved parents, underserved youth: Considering foster parent willingness to foster substance-using adolescents. Children and Youth Services Review, 35(9), 1650–1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (Eds.). (2013). Motivational interviewing: Helping people change. The Guilford Press: New York. [Google Scholar]
- Miller WR, & Sanchez VC (1994). Motivating young adults for treatment and lifestyle change In Howard GS & Nathan PE (Eds.), Alcohol use and misuse by young adults. (pp. 55–81). Notre Dame, IN: University of Notre Dame Press. [Google Scholar]
- Mitchell SG, Gryczynski J, Gonzales A, Moseley A, Peterson T, O’Grady KE, & Schwartz RP (2012). Screening, Brief Intervention, and Referral to Treatment (SBIRT) for substance use in a school‐based program: Services and outcomes. The American Journal on Addictions, 21(s1), S5–S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BA, Fazzino T, Garnet B, Cutter CJ, & Barry DT (2011). Computer-based interventions for drug use disorders: A systematic review. Journal of Substance Abuse Treatment, 40(3), 215–223. doi: 10.1016/j.jsat.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SC, Crompton K, van Goozen S, van den Bree M, Bunney J, & Lydall E (2013). A feasibility study of short message service text messaging as a surveillance tool for alcohol consumption and vehicle for interventions in university students. BMC public health, 13(1), 1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2015). MPlus user’s guide. Seventh Edition Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Action Alliance for Suicide Prevention Research Prioritization Task Force. (2014). A Prioritized Research Agenda for Suicide Prevention: An Action Plan to Save Lives. Retrieved from https://actionallianceforsuicideprevention.org/sites/actionallianceforsuicideprevention.org/files/Agenda.pdf
- Naughton F, Prevost AT, Gilbert H, & Sutton S (2012). Randomized controlled trial evaluation of a tailored leaflet and SMS text message self-help intervention for pregnant smokers (MiQuit). Nicotine & Tobacco Research, 14(5), 569–577. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Geisner IM, & Lee CM (2008). Perceived marijuana norms and social expectancies among entering college student marijuana users. Psychology of Addictive Behaviors, 22(3), 433. [DOI] [PubMed] [Google Scholar]
- Newman MG, Szkodny LE, Llera SJ, & Przeworski A (2011). A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: Is human contact necessary for therapeutic efficacy? Clinical Psychology Review, 31(1), 178–186. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Chase SK, Svikis DS, & Schuster CR (2005). Computer-based brief motivational intervention for perinatal drug use. Journal of Substance Abuse Treatment, 28(4), 305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. (2017a). Internet/broadband fact sheet. Retrieved March 21, 2018, from http://www.pewinternet.org/fact-sheet/internet-broadband/ [Google Scholar]
- Pew Research Center. (2017b). Mobile fact sheet. Retrieved March 21, 2018, from http://www.pewinternet.org/fact-sheet/mobile/ [Google Scholar]
- Phillips MM, Phillips KT, Lalonde TL, & Dykema KR (2014). Feasibility of text messaging for ecological momentary assessment of marijuana use in college students. Psychological Assessment, 26(3), 947–957. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, & Wu L-T (2013). Screening instruments for substance use and brief interventions targeting adolescents in primary care: A literature review. Addictive Behaviors, 38, 2146–2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilowsky DJ, & Wu LT (2006). Psychiatric symptoms and substance use disorders in a nationally representative sample of American adolescents involved with foster care. Journal of Adolescent Health, 38(4), 351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, & DiClemente CC (1992). Stages of change in the modification of problem behaviors In Hersen M, Eisler RM, & Miller PM (Eds.), Progress in Behavior Modification (Vol. 28, pp. 183–218). Sycamore, IL: Sycamore Press. [PubMed] [Google Scholar]
- Proudfoot J, Clarke J, Birch M-R, Whitton AE, Parker G, Manicavasagar V, … Hadzi-Pavlovic D (2013). Impact of a mobile phone and web program on symptom and functional outcomes for people with mild-to-moderate depression, anxiety and stress: A randomised controlled trial. BMC psychiatry, 13(1), 312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. Retrieved from http://ezproxy.pire.org:2048/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=eoah&AN=17241312&site=ehost-live [Google Scholar]
- Ramo DE, Thrul J, Delucchi KL, Ling PM, Hall SM, & Prochaska JJ (2015). The Tobacco Status Project (TSP): Study protocol for a randomized controlled trial of a Facebook smoking cessation intervention for young adults. BMC public health, 15(1), 897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Resnicow K, & Page SE (2008). Embracing chaos and complexity: A quantum change for public health. American Journal of Public Health, 98(8), 1382–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice FP, & Dolgin KG (2008). The adolescent: Development, relationships, and culture (12th ed.). Boston, MA: Pearson. [Google Scholar]
- Richards D, & Richardson T (2012). Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clinical Psychology Review, 32(4), 329–342. [DOI] [PubMed] [Google Scholar]
- Rickwood DJ, Deane FP, & Wison CJ (2007). When and how do young people seek professional help for mental health problems? Medical Journal of Australia, 187, S35–S39. [DOI] [PubMed] [Google Scholar]
- Ringeisen H, Casanueva CE, Urato M, & Stambaugh LF (2009). Mental health service use during the transition to adulthood for adolescents reported to the child welfare system. Psychiatric Services, 60(8), 1084–1091. [DOI] [PubMed] [Google Scholar]
- Robinson SM, Sobell LC, Sobell MB, & Leo GI (2014). Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychology of Addictive Behaviors, 28(1), 154. [DOI] [PubMed] [Google Scholar]
- Rooke S, Thorsteinsson E, Karpin A, Copeland J, & Allsop D (2010). Computer-delivered interventions for alcohol and tobacco use: A meta-analysis. Addiction, 105(8), 1381–1390. doi: 10.1111/j.1360-0443.2010.02975.x. [DOI] [PubMed] [Google Scholar]
- Sarvet AL, Wall MM, Keyes KM, Cerdá M, Schulenber JE, O’Malley PM, … Hasin DS (2018). Recent rapid decrease in adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug & Alcohol Dependence, 186(1), 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall R, Okoniewski A, Tiase V, Low A, Rodriguez M, & Kaplan S (2013). Using text messaging to assess adolescents’ health information needs: An ecological momentary assessment. Journal of medical Internet research, 15(3), e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder J, Lemieux C, & Pogue R (2008). The collision of the Adoption and Safe Families Act and substance abuse: Research-based education and training priorities for child welfare professionals. Journal of Teaching in Social Work, 28(1–2), 227–246. [Google Scholar]
- Shin SH (2005). Need for and actual use of mental health service by adolescents in the child welfare system. Children and Youth Services Review, 27(10), 1071–1083. [Google Scholar]
- Shrier LA, Rhoads A, Burke P, Walls C, & Blood EA (2014). Real-time, contextual intervention using mobile technology to reduce marijuana use among youth: a pilot study. Addictive Behaviors, 39(1), 173–180. [DOI] [PubMed] [Google Scholar]
- Simms MD, Dubowitz H, & Szilagyi MA (2000). Health care needs of children in the foster care system. Pediatrics, 106(4), 909–918. [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press. [Google Scholar]
- Sobell LC, Brown J, Leo GI, & Sobell MB (1996). The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug and Alcohol Dependence, 42(1), 49–54. [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back: A technique for assessing self-reported alcohol consumption In Litten RZ & Allen JP (Eds.), Measuring alcohol consumption: Psychosocial and biochemical methods. (pp. 41–72). Totowa, NJ: Humana Press. [Google Scholar]
- SocioCultural Research Consultants LLC (2016). Dedoose, web application for managing, analyzing, and presenting qualitative and mixed method research data (Version 7.0.23). Los Angeles, CA: SocioCultural Research Consultants, LLC [Google Scholar]
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, … Myers M (2004). A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. The Journal of Pediatrics, 145(3), 396–402. [DOI] [PubMed] [Google Scholar]
- Stambaugh L, Ringeisen H, Casanueva C, Tueller S, Smith K, & Dolan M (2013). Adverse childhood experiences in NSCAW. (OPRE Report# 2013–26). Washington, DC: US Department of Health and Human Services. [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, & Del Boca FK (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Supplement(12), 70–75. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17–5044, NSDUH Series H-52). Rockville, MD: Author. [Google Scholar]
- Suffoletto B, Callaway C, Kristan J, Kraemer K, & Clark DB (2012). Text-Message-Based Drinking Assessments and Brief Interventions for Young Adults Discharged from the Emergency Department. Alcoholism: Clinical And Experimental Research, 36(3), 552–560. [DOI] [PubMed] [Google Scholar]
- Suffoletto B, Kristan J, Callaway C, Kim KH, Chung T, Monti PM, & Clark DB (2014). A text message alcohol intervention for young adult emergency department patients: a randomized clinical trial. Annals of Emergency Medicine, 64(6), 664–672.e664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto B, Kristan J, Chung T, Jeong K, Fabio A, Monti P, & Clark DB (2015). An interactive text message intervention to reduce binge drinking in young adults: A randomized controlled trial with 9-month outcomes. PLoS One, 10(11), e0142877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tevyaw TOL, & Monti PM (2004). Motivational enhancement and other brief interventions for adolescent substance abuse: Foundations, applications and evaluations. Addiction, 99(s2), 63–75. [DOI] [PubMed] [Google Scholar]
- Traube DE, James S, Zhang J, & Landsverk J (2012). A national study of risk and protective factors for substance use among youth in the child welfare system. Addictive Behaviors, 37(5), 641–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzilos Wernette GK, Plegue M, Kahler CW, Sen A, & Zlotnick C (2018). A pilot randomized controlled trial of a computer-delivered brief intervention for substance use and risky sex during pregnancy. Journal of Women’s Health, 27(1), 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2005). National Survey of Child and Adolescent Well-Being (NSCAW): CPS sample component wave 1 data analysis report. Retrieved from Washington, DC: [Google Scholar]
- U.S. Department of Health and Human Services. (2017). Child Maltreatment 2015. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Vasilaki EI, Hosier SG, & Cox WM (2006). The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism, 41(3), 328–335. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Ollie MT, McMillen JC, Scott L Jr, & Munson M (2007). Substance use and abuse among older youth in foster care. Addictive Behaviors, 32(9), 1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White CR, O’Brien K, White J, Pecora PJ, & Phillips CM (2008). Alcohol and drug use among alumni of foster care: Decreasing dependency through improvement of foster care experiences. Journal of Behavioral Health Services & Research, 35(4), 419–434. [DOI] [PubMed] [Google Scholar]
- Whittaker R, Dorey E, Bramley D, Bullen C, Denny S, Elley CR, … Rodgers A (2011). A theory-based video messaging mobile phone intervention for smoking cessation: randomized controlled trial. Journal of medical Internet research, 13(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittaker R, McRobbie H, Bullen C, Rodgers A, & Gu Y (2016). Mobile phone-based interventions for smoking cessation. Cochrane Database of Systematic Reviews(4). Retrieved from 10.1002/14651858.CD006611.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction, 97(9), 1183–1194. [DOI] [PubMed] [Google Scholar]
- Wray TB, Braciszewski JM, Zywiak WH, & Stout RL (2016). Examining the reliability of alcohol/drug use and HIV-risk behaviors using Timeline Follow-Back in a pilot sample. Journal of Substance Use, 21(3), 294–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L-T, & Ringwalt CL (2006). Use of alcohol treatment and mental health services among adolescents with alcohol use disorders. Psychiatric Services, 57(1), 84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]