Abstract
Objective:
To describe children’s diagnostic, social, and functional characteristics associated with use of core early intervention (EI) services.
Methods:
The sample included infants and toddlers (n=2,045) discharged from an urban EI program (2014–2016). Adjusted logit models estimated the marginal effects (95% CI) of receipt of any of the four core EI services, controlling for the child’s developmental condition type, race and ethnicity, primary language, sex, insurance type, age at referral, and the child’s functional performance at EI entry. Adjusted median regression estimated EI core service intensity controlling for child characteristics.
Results:
Median [IQR] per child EI service intensity was less than 3 hours per month (2.7. [2.1, 3.5]). Children whose primary language is English were 6% more likely to receive OT (ME=0.063 [0.010, 0.115]). Compared to infants, 1–2 year old children were less likely to receive PT and OT, but more likely to receive ST. Compared to infants, 1-year olds received more intensive ST (b=.42 [0.1, 0.7]) and 2-year olds received less intensive OT (b=−.70 [−1.3.1, −0.1]). Children’s functional performance at EI entry was significantly associated with receipt and intensity of EI services.
Conclusions:
Many EI-enrolled children received low intensity services, which was associated with primary language of the caregiver and child age and functional status. Results suggest the need for interventions to improve service delivery for vulnerable EI sub-groups.
Keywords: early intervention, therapy, functional performance, service use
Introduction
Part C of the Individuals with Disabilities Education Act authorizes states (with the incentive of financial support) to establish statewide early intervention (EI) systems for infants and toddlers with, or at risk for, developmental delays.1 There has been a growing demand for EI outcomes research to inform continuous system quality improvement.2 Until recently, child and family outcomes reporting has not been nationally mandated, resulting in limited opportunities for research on trends in EI service use and how EI service use links with child and family outcomes for quality improvement.
To this end, previous research using local and state-level administrative data suggests that compared to non-poor and white, non-Hispanic (WNH) children, minority, and low-income children are not only less likely to receive EI,3,4 but also receive lower therapy intensity.5,6 However, these studies have been limited to EI eligibility data (e.g., diagnosis). When measures of condition severity are also considered, children with less clinical need receive greater amounts of therapy.5 While there are numerous possible explanations for this finding, it suggests relying on diagnosis alone inadequately captures EI therapy need.
Nationally, states are now required to report to the Office of Special Education Programs on child functional outcomes at EI entry and exit. Therefore, child outcomes are becoming common data elements in electronic EI data capture systems.2 Most states use the Child Outcomes Summary (COS) to generate an estimate of a child’s functional performance in three domains: social-emotional, cognitive (acquiring and using knowledge and skills), and behavioral/adaptive (taking appropriate action to meet needs).7 As a baseline measure of function in these three areas, COS scores have potential to be markers for discipline-specific EI service need. To our knowledge, COS data have not yet been included in EI service use studies. In this era of increased EI accountability and fewer federal per child appropriations,8 it is critical to leverage COS data for estimating trends and correlates of EI service receipt and intensity.
The purpose of this study is to examine the relationship between developmental, social, and functional characteristics of children and their EI service use breadth and intensity.
Methods
Study Sample
The study sample was derived from electronic administrative data at a large EI program that actively serves approximately 1000 families annually. Sample EI-eligible and enrolled children were discharged between 10/1/2014 and 9/30/16 to coincide with the adoption of an expanded electronic data capture system by the EI program. The complete study sample included 2,045 EI-eligible children. Of those, 342 received a care plan but were discharged after being lost to follow up, leaving an analytic sample of 1,703. Of the 1,703 children who had at least one billable EI service, 1,681 received a core EI service. The remaining 22 children received non-core EI services only. Routine collection of COS was not mandatory at this program during the study period, therefore COS information was available for 65% (1,326/2,045) of children discharged during the study period and 70% (1,180/1,681) of children who received a core EI service.
Multi-site institutional review board approval was obtained for this study.
Measures
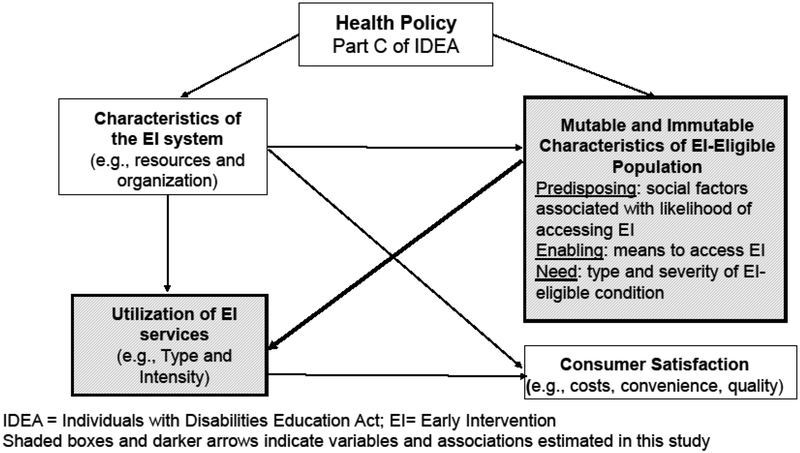
The choice of measures was informed by the Aday and Andersen conceptual model of health service access.9 This model posits that health service utilization and satisfaction are influenced, in part, by characteristics of the eligible population, including their predisposing characteristics, enabling characteristics and service need (Figure 1). For this study, we considered how EI service use is influenced by all three types of characteristics among the EI-eligible children sampled.
Figure 1.
Conceptual Framework for the Study of Early Intervention Utilization (Adapted from Aday and Andersen)
EI Service Use.
Total service use was described according to number of discipline-specific services received (1, 2, 3 or more), number of hours, and duration of services (in months). Service intensity was calculated as total hours divided by total duration of services (in months).
EI service use was also described by core discipline (i.e., physical therapy [PT], occupational therapy [OT], speech therapy [ST], and developmental intervention [DI]). DI is typically provided by someone trained in early childhood or special education, and focuses on global play skills and social behaviors. For each core discipline, we estimated 1) “any” discipline-specific service and 2) discipline-specific service intensity. “Any” discipline-specific service is contingent on receiving at least one billable service from that discipline. Discipline-specific service intensity was calculated by dividing total service hours in that discipline by EI enrollment length, allowing adjustment for varying lengths of EI enrollment.
Characteristics of EI-eligible children sampled.
Predisposing characteristics (Figure 1) are social factors that increase the likelihood of EI access. For this study, these factors included child’s race and ethnicity, age, sex (male or female), and language. Race and ethnicity were categorized as WNH; black, non-Hispanic (BNH); Hispanic; and other race, non-Hispanic (ONH; includes Asian, Pacific Islander and more than one race). Age at EI referral was grouped into under 12 months, 12–24 months, and greater than 24 months. Language spoken at home was categorized as English versus a language other than English.
Enabling characteristics are those factors that are associated with means to access EI, such as health insurance. For this study, health insurance type was grouped as private or public (includes Medicaid and CHP+). Although health insurance is not required for EI access, insurance type is a marker of income and access to developmental screening and surveillance.10
Service need is partially measured through EI eligibility by condition type (diagnosed medical or mental condition versus developmental delay). Children are automatically deemed EI-eligible if they have a diagnosed condition that typically results in developmental delay. These conditions are based upon federal legislation1 with specific diagnoses chosen by states.11 In Colorado, developmental delay is defined as performing at least 1 SD below the mean on a standardized developmental evaluation.
We also included measures of child function to indicate service need. Child functional characteristics were captured via the three EI entry COS score domains: 1) social emotional skills, 2) cognitive skills, and 3) adaptive/behavioral skills. COS is endorsed by the Office of Special Education Programs as a valid indicator of child’s function.12,13 EI teams use COS scores to develop a functional profile of the child that is monitored from EI entry to EI exit. These COS domains align with the activity dimension of the International Classification of Functioning, Disability, and Health (ICF-CY), an international rehabilitation service framework that guides the estimation of core EI service need.13–15 Each of the three COS scores is a consensus rating informed by provider clinical judgment, parent concerns, and developmental assessment results. COS uses a 7-point scale, from 1=very early skills (i.e., child does not use any immediate foundational skills related to this outcome) to 7=all skills expected (i.e., there are no concerns about the child’s function in this area).13 COS scores directly align with some core EI services and indirectly with others. For example, the social-emotional and cognitive scores directly align with developmental intervention whereas adaptive/behavioral function aligns with physical therapy (e.g., crawling to a toy), occupational therapy (e.g., feeding with a spoon), and speech therapy (e.g., communicating needs).13
Since the purpose of this study was to examine the relationship between developmental, social, and functional characteristics of children and service use breadth and intensity, we conducted analyses first on the whole sample, and secondly on the sub-group with complete COS information.
Analytic Approach
All analyses were conducted in STATA15.16 We first calculated descriptive statistics to describe study sample characteristics and EI service use. We calculated inter-quartile ranges to describe EI service use, due to skewed distribution of data on these variables. Of note, overall EI service use includes all EI services, whereas core EI service use outcomes are conditional on having received that service.
We fit adjusted logit models estimating the likelihood of receipt of any of the core EI services (i.e., PT, OT, ST, and DI). Given that odds ratios are not appropriate for non-rare outcomes (i.e., they overestimate the association), we present marginal effects and 95% confidence intervals for each child characteristic.17,18 Marginal effects, a common effect estimate in health services research, are interpreted as the predicted probability of the outcome occurring with respect to the reference group. Second, we fit adjusted median regression to estimate the association between child characteristics and EI core service intensity owing to skewness of EI service intensity data. For these models, we present the core EI service median intensity for each model parameter and its 95% confidence interval. Adjusted models included child characteristics listed above.
To determine the influence of baseline functional performance on receipt and intensity of EI service use, we fit the same multivariable logit and median regression models described above among the sub-sample of children with complete EI entry COS scores.
Results
Sample Characteristics
Of the 1,703 children who had at least one billable EI service, 1,681 received a core EI service. Over 50% of the sample was publicly insured. Nearly 42% of the sample was Hispanic and 10% was BNH. Over 75% of the sample was from a household where English was the primary language. A little over 30% of the sample was female. The large majority of sample children (89%) were deemed to be EI-eligible due to a developmental delay. Mean [SD] COS scores at entry were highest for social-emotional function (4.96 [1.7]) and lowest for cognitive skills (3.9 [1.6]). For reference, a COS score of 4 indicates “the child shows occasional age-appropriate functioning across settings and situations.”13 We found no differences in child characteristics for children with and without complete COS information (results not shown).
EI Service Use and Intensity
As shown in Table 2, ST was the most common core EI service and was accessed by 70% of children sampled. More than 80% of children sampled received multiple EI services concurrently. Median [IQR] per child total dosage (hours) of EI services was 12 [8.5, 17.4] and ranged from 6 [3, 10] for DI to 19 [12.1, 25] for ST. Median [IQR] per child intensity (hours/month) of EI services was 2.7 [2.1, 3.5] and ranged from 1 [1, 2] for DI to 4.2 [3.5, 4.5] for ST.
Table 2.
Service use characteristics of the sample of children who received at least one early intervention service (n=1,703)
| % (n) | |
|---|---|
| Type of EI Services Received | |
| Physical Therapy | 25.72 (438) |
| Occupational Therapy | 20.14 (343) |
| Speech and Language Pathology | 71.64 (1,220) |
| Developmental Intervention | 45.80 (780) |
| Number of EI Services Received | |
| One Service | 20.43 (348) |
| Two Services | 32.71 (557) |
| Three or more Services | 46.86 (798) |
| Median [IQR] | |
| Total Per Child Hours of EI Services, Conditional on Any Use | |
| All Services | 12.00 [8.50, 17.43] |
| Physical Therapy | 16.13 [9.00, 24.00] |
| Occupational Therapy | 12.00 [5.00, 22.33] |
| Speech and Language Pathology | 19.00 [12.13, 25.00] |
| Developmental Intervention | 6.00 [3.00, 10.00] |
| Total Per Child EI Service Intensity (hours/month), Conditional on Any Use | |
| All Services | 2.69 [2.07, 3.50] |
| Physical Therapy | 3.61 [2.00, 4.33] |
| Occupational Therapy | 3.00 [1.50, 4.28] |
| Speech and Language Pathology | 4.20 [3.50, 4.50] |
| Developmental Intervention | 1.00 [1.00, 2.00] |
| Total EI Service Use (Months) | 5.50 [3.50, 6.05] |
Receipt of Core EI Services by Characteristics of EI-Eligible Children and Service Need.
Receipt of Core EI Services by Predisposing Sample Characteristics
As compared to infants, 1–2 year-olds were 44% less likely (ME=−0.436 [−.402, −0.254]) to receive PT, 8% less likely to receive OT (ME=−0.084, [−.131, −0.036]), and 33% more likely to receive ST (ME=0.331, [0.276, 0.386]). Compared to infants, 2-year olds were 58% less likely (ME=−0.577 [−.630, −0.524]) to receive PT, 14% less likely to receive OT (ME=−0.141, [−.187, −0.095]), and 34% more likely to receive ST (ME=0.344, [0.287, 0.401]) (Table 3).
Table 3.
Adjusted marginal effects (ME) from logit models estimating receipt of a core early intervention service among a sample (n=2,045) of children enrolled in an urban early intervention program. Presented as ME [95% Confidence Intervals].
| Independent Variables | Marginal Effects of any PT | Marginal Effects of any OT | Marginal Effects of any ST | Marginal Effects of any DI |
|---|---|---|---|---|
| Condition Type | ||||
| Diagnosed Condition (DC) | −0.009 [−0.068, 0.051] | 0.070* [0.010, 0.131] | −0.005 [−0.079, 0.068] | 0.088* [0.012, 0.165] |
| Child’s Age | ||||
| Less than 12-Months | ref | ref | ref | ref |
| 12–24 Months | −0.436*** [−0.496, −0.376] | −0.084*** [−0.131, −0.036] | 0.331*** [0.276, 0.386] | −0.016 [−0.073, 0.041] |
| Greater than 24-Months | −0.577*** [−0.630, −0.524] | −0.141*** [−0.187, −0.095] | 0.344*** [0.287, 0.401] | −0.027 [−0.086, 0.032] |
| Race/Ethnicity | ||||
| White, non-Hispanic | ref | ref | ref | ref |
| Black, non-Hispanic | −0.022 [−0.090, 0.047] | −0.012 [−0.072, 0.048] | −0.039 [−0.116, 0.037] | 0.070 [−0.010, 0.151] |
| Hispanic | −0.026 [−0.079, 0.026] | −0.042 [−0.085, 0.001] | −0.042 [−0.099, 0.015] | 0.006 [−0.053, 0.064] |
| Other, non-Hispanic | −0.053 [−0.121, 0.014] | 0.096* [0.023, 0.169] | −0.021 [−0.103, 0.062] | −0.015 [−0.099, 0.070] |
| Primary Language, English | 0.001 [−0.048, 0.049] | 0.051* [0.011, 0.091] | 0.000 [−0.054, 0.054] | 0.012 [−0.044, 0.069] |
| Child’s sex, Female | 0.037 [−0.000, 0.074] | −0.024 [−0.056, 0.008] | −0.052* [−0.095, −0.010] | −0.030 [−0.073, 0.014] |
| Insurance Type, Medicaid and CHP+ | −0.027 [−0.073, 0.018] | −0.014 [−0.053, 0.025] | −0.002 [−0.053, 0.048] | −0.007 [−0.059, 0.045] |
| Number of Observations | 2,045 | 2,045 | 2,045 | 2,045 |
p<0.001,
p<0.01,
p<0.05
In the models including COS scores, Hispanic children were 6% less likely than their WNH peers to receive OT (ME=−0.057, [−0.114, 0.001]) which approached statistical significance (p=0.06) (Table 5).
Table 5.
Adjusted marginal effects [95% CI] from logit models estimating receipt of a core early intervention service among a sub-sample of children (n=1,326) with complete Child Outcomes Survey information at EI entry. Presented as ME [95% Confidence Intervals].
| Independent Variables | Marginal Effects of any PT | Marginal Effects of any OT | Marginal Effects of any ST | Marginal Effects of any DI |
|---|---|---|---|---|
| Condition Type | ||||
| Diagnosed Condition (DC) | 0.008 [−0.063, 0.080] | 0.057 [−0.021, 0.136] | 0.030 [−0.047, 0.107] | 0.081 [−0.020, 0.182] |
| Child’s Age | ||||
| Less than 12-Months | ref | ref | ref | ref |
| 12–24 Months | −0.328*** [−0.402, −0.254] | −0.076* [−0.138, −0.014] | 0.218*** [0.147, 0.290] | −0.046 [−0.120, 0.027] |
| Greater than 24-Months | −0.468*** [−0.540, −0.397] | −0.110*** [−0.175, −0.045] | 0.283*** [0.208, 0.358] | −0.020 [−0.101, 0.061] |
| Race/Ethnicity | ||||
| White, non-Hispanic | ref | ref | ref | ref |
| Black, non-Hispanic | 0.014 [−0.063, 0.092] | 0.012 [−0.068, 0.092] | 0.005 [−0.086, 0.095] | 0.138** [0.034, 0.243] |
| Hispanic | −0.057 [−0.114, 0.001] | −0.020 [−0.078, 0.038] | −0.012 [−0.080, 0.055] | −0.006 [−0.082, 0.069] |
| Other, non-Hispanic | −0.036 [−0.110, 0.039] | 0.108* [0.018, 0.199] | 0.023 [−0.065, 0.111] | −0.008 [−0.113, 0.097] |
| Primary Language, English | 0.026 [−0.032, 0.085] | 0.063* [0.010, 0.115] | −0.040 [−0.105, 0.025] | −0.006 [−0.080, 0.068] |
| Child’s sex, Female | 0.047* [0.005, 0.089] | −0.056** [−0.098, −0.014] | −0.041 [−0.090, 0.007] | −0.007 [−0.063, 0.048] |
| Insurance Type, Medicaid and CHP+ | −0.001 [−0.053, 0.050] | −0.029 [−0.081, 0.022] | −0.033 [−0.093, 0.028] | −0.017 [−0.084, 0.049] |
| Entry COSA | ||||
| Positive Social Emotional Skills | 0.006 [−0.011, 0.023] | −0.018* [−0.035, −0.001] | 0.021 [−0.000, 0.041] | −0.037** [−0.060, −0.015] |
| Acquiring and Using Knowledge and Skills | 0.049*** [0.032, 0.065] | 0.005 [−0.013, 0.023] | −0.066*** [−0.087, −0.046] | −0.008 [−0.030, 0.014] |
| Taking Appropriate Action to Meet Needs | −0.061*** [−0.075, −0.047] | −0.019** [−0.033, −0.004] | 0.028** [0.011, 0.044] | 0.006 [−0.014, 0.026] |
| Number of Observations | 1,326 | 1,326 | 1,326 | 1,326 |
p<0.001,
p<0.01,
p<0.05
Each COS sub-scale score is derived from provider clinical judgment, parent concerns, and developmental assessment results and measured on a 7-point scale, from 1=very early skills (i.e., child does not use any immediate foundational skills related to this outcome) to 7=all skills expected (i.e., there are no concerns about the child’s function in this area).
Children whose primary language was English (versus a language other than English) were 5% more likely to receive OT (ME=0.051, [0.011, 0.091]).
Receipt of Core EI Services by Enabling Sample Characteristics
We found no differences in core services receipt by health insurance type.
Receipt of Core EI Services by Service Need
Children with a diagnosis were 7% more likely to receive OT (ME=0.070, [0.010, 0.131]) and 9% more likely to receive DI (ME=0.088, [0.012, 0.165]) (Table 3). However, when functional performance at EI entry was included in the model, condition type was no longer statistically significantly associated with receipt of OT or DI (Table 5).
There were significant differences in receipt of EI core services for all three entry COS scores. A point-increase in cognitive COS score was associated with a 5% higher likelihood of receiving PT (ME=0.049 [0.032, 0.065]) and 7% lower likelihood of receiving ST (ME=−0.066, [−0.087, −0.046]). Children with higher entry behavioral/adaptive COS scores were less likely to receive PT (ME=−0.061, [−0.075, −0.047]), OT (ME=−0.019, [−0.033, −0.004]) and more likely to receive ST (ME=0.028, [0.011, 0.044]). Children with higher entry COS scores related to positive social relationships were less likely to receive OT (ME=−0.018, [−0.035, −0.001]) and DI (ME=−0.037, [−0.060, −0.015]) (Table 5).
Core EI Service Intensity by Characteristics of EI-Eligible Children and Service Need
Core EI Service Intensity by Predisposing Characteristics of Sampled Children.
Compared to children entering EI as infants, children entering as 2-year-olds received less intensive ST (b=−0.83 [−1.4, −0.3]), and those entering as 1- year-olds received more intensive ST (b=0.9 [0.3, 1.6]) and overall EI services (b=0.59 [0.03, 1.1]) and. Additionally, children entering EI as 2- year-olds received more intensive ST (b=0.65 [0.3, 0.9]) and overall EI services (b=0.24 [0.1, 0.4]) than those entering as infants (Table 4). BNH children received more intensive OT (b=0.76 [0.04, 1.5]) than their WNH counterparts.
Table 4.
Results of adjusted median regression models [95% CI] estimating per child intensity of all and core early intervention services among children enrolled in an urban early intervention program who received at least one core early intervention service (n=1,681).A Presented as beta coefficient [95% Confidence Intervals].
| Independent Variables | Total Intensity | PT Intensity | OT Intensity | ST Intensity | DI Intensity |
|---|---|---|---|---|---|
| Condition Type | |||||
| Diagnosed Condition (DC) | −0.037 [−0.341, 0.266] | −0.142 [−0.494, 0.211] | 0.029 [−0.435, 0.493] | −0.075 [−0.642, 0.492] | −0.121 [−0.453, 0.212] |
| Child’s Age | |||||
| Less than 12-Months | ref | ref | ref | ref | ref |
| 12–24 Months | 0.588* [0.033, 1.142] | −0.017 [−0.351, 0.318] | −0.307 [−0.727, 0.113] | 0.921** [0.279, 1.564] | 0.245 [−0.026, 0.516] |
| Greater than 24-Months | 0.241** [0.073, 0.409] | −0.450 [−1.085, 0.184] | −0.830** [−1.374, −0.286] | 0.652*** [0.339, 0.964] | 0.133 [−0.166, 0.432] |
| Race/Ethnicity | |||||
| White, non-Hispanic | ref | ref | ref | ref | ref |
| Black, non-Hispanic | −0.218 [−0.521, 0.084] | −0.358 [−1.026, 0.309] | 0.762* [0.036, 1.488] | 0.159 [−0.271, 0.590] | 0.091 [−0.250, 0.433] |
| Hispanic | 0.367 [−0.354, 1.087] | −0.187 [−0.633, 0.259] | −0.095 [−0.570, 0.381] | 0.574 [−0.420, 1.568] | −0.108 [−0.403, 0.188] |
| Other, non-Hispanic | 0.219 [−0.103, 0.541] | 0.185 [−0.492, 0.861] | −0.067 [−0.666, 0.531] | 0.137 [−0.247, 0.522] | −0.099 [−0.511, 0.314] |
| Primary Language, English | 0.152 [−0.647, 0.952] | −0.505* [−0.928, - 0.081] | −0.685** [−1.201, −0.169] | 0.334 [−0.814, 1.483] | −0.069 [−0.355, 0.216] |
| Child’s sex, Female | 0.310 [−0.298, 0.919] | 0.276 [−0.004, 0.556] | −0.050 [−0.431, 0.331] | 0.404 [−0.482, 1.289] | −0.272** [−0.469, - 0.075] |
| Insurance Type, Medicaid and CHP+ | 0.304 [−0.101, 0.710] | 0.078 [−0.328, 0.484] | 0.003 [−0.445, 0.451] | 0.248 [−0.337, 0.834] | 0.561*** [0.307, 0.816] |
| Number of Observations | 1,681 | 430 | 332 | 1,210 | 774 |
p<0.001,
p<0.01,
p<0.05
Core early intervention specific models include children who received that specific service. For example, the model estimating PT intensity includes all children who received any physical therapy.
Children whose primary language is English received less intensive PT (b=−0.51 [−0.9, −0.1]) and OT (b=−0.69 [−1.2, −0.2]) than their peers whose primary language was not English (Table 4). When functional performance was included in the models, child’s primary language was no longer significantly associated with PT or OT service use intensity (Table 6).
Table 6.
Results of adjusted median regression models [95% CI] estimating per child service use intensity overall and for core early interventions services among a sub-group of children with complete entry Child Outcomes Survey information who received at least one core EI service (n=1,180).
| Independent Variables | Total Intensity | PT Intensity | OT Intensity | ST Intensity | DI Intensity |
|---|---|---|---|---|---|
| Condition Type | |||||
| Diagnosed Condition (DC) | −0.109 [−0.439, 0.221] | 0.004 [−0.439, 0.447] | −0.185 [−0.740, 0.370] | −0.001 [−0.559, 0.558] | −0.284 [−0.634, 0.065] |
| Child’s Age | |||||
| ess than 12-Months | ref | ref | ref | ref | ref |
| 12–24 Months | 0.274* [0.050, 0.498] | 0.076 [−0.319, 0.471] | −0.318 [−0.802, 0.166] | 0.421* [0.098, 0.743] | 0.087 [−0.271, 0.444] |
| Greater than 24-Months | −0.016 [−0.681, 0.649] | −0.044 [−0.832, 0.743] | −0.702* [−1.347, - 0.057] | 0.166 [−0.710, 1.043] | 0.088 [−0.314, 0.489] |
| Race/Ethnicity | |||||
| White, non-Hispanic | ref | ref | ref | ref | ref |
| Black, non-Hispanic | −0.281 [−0.707, 0.145] | −0.403 [−1.146, 0.340] | 0.353 [−0.386, 1.092] | 0.108 [−0.444, 0.659] | −0.053 [−0.445, 0.339] |
| Hispanic | 0.654 [−0.409, 1.717] | 0.095 [−0.442, 0.632] | −0.180 [−0.742, 0.383] | 0.829 [−0.612, 2.270] | −0.158 [−0.498, 0.181] |
| Other, non-Hispanic | 0.405 [−0.038, 0.848] | 0.568 [−0.200, 1.337] | −0.127 [−0.821, 0.567] | 0.444 [−0.185, 1.073] | −0.142 [−0.657, 0.373] |
| Primary Language, English | 0.410 [−0.827, 1.646] | −0.381 [−0.942, 0.180] | −0.590 [−1.203, 0.023] | 0.724 [−1.023, 2.470] | −0.111 [−0.447, 0.226] |
| Child’s sex, Female | 0.532 [−0.453, 1.518] | 0.277 [−0.060, 0.613] | −0.207 [−0.641, 0.227] | 0.726 [−0.644, 2.095] | −0.316** [−0.529, −0.103] |
| Insurance Type, Medicaid and CHP+ | 0.419 [−0.211, 1.050] | −0.057 [−0.546, 0.432] | 0.060 [−0.467, 0.588] | 0.529 [−0.442, 1.500] | 0.541*** [0.241, 0.842] |
| Entry COSA | |||||
| Positive Social Emotional Skills | 0.206 [−0.247, 0.659] | −0.044 [−0.184, 0.097] | −0.153 [−0.327, 0.021] | 0.252 [−0.337, 0.841] | −0.248*** [−0.336, −0.161] |
| Acquiring and Using Knowledge and Skills | −0.331 [−0.972, 0.310] | 0.127 [−0.013, 0.266] | 0.226** [0.056, 0.395] | −0.509 [−1.368, 0.350] | 0.096* [0.013, 0.179] |
| Taking Appropriate Action to Meet Needs | 0.152 [−0.087, 0.391] | −0.128 [−0.264, 0.007] | −0.132 [−0.286, 0.022] | 0.257 [−0.028, 0.541] | 0.109* [0.023, 0.195] |
| Number of Observations | 1,180 | 317 | 248 | 912 | 549 |
p<0.001,
p<0.01,
p<0.05
Each COS sub-scale score is derived from provider clinical judgment, parent concerns, and developmental assessment results and measured on a 7-point scale, from 1=very early skills (i.e., child does not use any immediate foundational skills related to this outcome) to 7=all skills expected (i.e., there are no concerns about the child’s function in this area).
Core EI Service Intensity by Enabling Characteristics of Sampled Children.
Compared to their privately insured peers, publicly insured children received more intensive DI (b=0.56 [0.3, 0.8]).
Core EI Service Intensity by Service Need
Higher baseline social emotional scores were associated with lower DI intensity (b=−0.25 [−0.3, −0.2]), whereas higher baseline cognitive scores (b=0.10 [0.01, 0.2]) and adaptive/behavioral scores (b=0.11 [0.02, 0.2]) were associated with greater DI intensity (Table 6).
Discussion
A growing number of common data elements that are collected and reported annually across states affords for health services research in early intervention. This is one of the first studies to leverage data on social and functional characteristics of children discharged from a large, urban EI program to show that low rates of EI intensity and core EI service use were both associated with select predisposing factors, as well as service need as indicated by estimates of the child’s baseline functioning.
We found very low intensity of EI services overall; less than 1 hour per week (less than 2.7 hours per month, overall). These results are similar to our prior study whereby service use intensity was both low and variable.6 There are few national studies to which to compare our results, although a nationally representative sample of EI-enrolled children showed that about 1/3 received less than one hour per week, about 1/3 received 1–2 hours, and about 1/3 received 2 or more hours per week.19 Children in the current study appear to be receiving less intensive EI services than previously reported; perhaps a reflection of substantial decline in federal per child appropriations for EI since this cohort study was conducted over a decade ago.
Core service use intensity is consistent with previously reported therapy intensity among EI-enrolled and EI-eligible and Medicaid-enrolled children.5 Yet, previous studies were limited by smaller sample sizes and in the case of the Medicaid-enrolled children, inability to confirm EI participation. Thus, to our knowledge, this is the first study to examine patterns of core service use intensity within a large urban EI program. The service use intensity described in this study falls short of recommendations based on evidence-based models of pediatric therapy service breadth, intensity, and appropriateness.14,15 States are pressed to provide EI services to increasing numbers of EI-eligible children amid a context of declining federal per child EI appropriations,8 which may indirectly affect intensity when creating EI care plans. The choice of service delivery model (e.g. primary service provider model) may also influence service intensity.20,21,22 Future research should investigate and characterize cost-effective packages of EI service delivery in light of their impact on meaningful child and family outcomes.
Predisposing Characteristics
We found that children living in households where the primary language is not English were less likely to receive OT and Hispanic children were marginally less likely to receive PT. These findings are consistent with prior research involving a statewide cohort of children with developmental disabilities and delays, which found Hispanic children had significantly lower odds of receiving therapies after adjusting for a number of social and clinical characteristics.5 Similarly, language barriers to pediatric care have been described as limiting access to interpreter services, decreasing caregiver satisfaction with care,23,24 and increasing miscommunication about the child’s diagnosis or treatment plan.25 As EI endorses a family-centered care approach, providers must be equipped with culturally valid tools for engaging families of diverse backgrounds in care planning and outcomes monitoring.25,26,27 A few studies have applied best practice standards to culturally adapt assessments for use in EI and examine feasibility in light of limited organizational resources.26–29
Our study findings also confirm previous reports regarding the effects of predisposing factors such as race, ethnicity and age on EI service use.5,6 The finding that BNH children were more likely than their WNH peers to receive DI is surprising. This finding is consistent with one previous study that examined disparities in core EI service use.6 Implications of this finding are not immediately clear. It may be appropriate that BNH children are receiving DI to promote cognitive and social development, however, this finding is problematic if BNH children are receiving DI in lieu of indicated specialized therapies (e.g., PT). Future research should explore family preferences for EI core services in light of state EI service provision models to ensure efficient and equitable service delivery.
The American Academy of Pediatrics has developed an algorithm30 for early identification of developmental concerns and EI referral. Thus, pediatricians are instrumental in facilitating EI access and assisting families with advocating for appropriate EI service intensity.31,32 Moreover, our findings are consistent with previous literature31,32 suggesting EI access and intensity disparities among important EI sub-groups (e.g., infants and minority children). This suggests a potential opportunity for pediatricians to provide more intensive shared decision-making around EI access and anticipatory guidance around EI service intensity, particularly for families of children at greater risk for access barriers or low service use.
Characteristics of Need
Each of the three types of children’s baseline functional skills appeared to be potential indicators of service need as they contributed to differences in EI service use and intensity. This may help establish the clinical usefulness of COS by examining its connection to service type. Children with higher social-emotional scores were less likely to receive OT and DI and received less intensive DI. DI typically focuses on building children’s play skills and social interaction, and OTs often focus on improving self-regulation during social interactions, so it is plausible that these children have less need for DI and OT.
The finding that higher baseline behavioral/adaptive scores were associated with more intensive DI was unexpected, but highlights the breadth of DI interventions and of children receiving DI services (children receiving PT or OT are likely more homogenous groups). We also found children with higher baseline behavioral/adaptive scores were less likely to receive OT, but if they did, it was more intense. Children with higher behavioral/adaptive scores were also less likely to receive PT and more likely to receive ST. Adaptive and behavioral skills relate to a child’s capacity to perform practical tasks (e.g., feeding self with utensil, moving toward a desired toy, interacting with caregivers and peers). Children with these skills may be able to meet their needs through functional mobility and have less need for PT; instead, these children plausibly have difficulty using expressive language, suggesting higher need for ST, and complex self-care difficulties that warrant intensive OT.
Conversely, children with higher cognitive scores were more likely to receive PT, and less likely to receive ST. These children are plausibly referred to EI for motor delays, and therefore have greater need for PT and less for ST. Interestingly, children with higher cognitive scores receive more intensive DI. Again, this highlights the diversity of DI interventions and implies heterogeneity of children receiving DI services.
Study Limitations
Data were ascertained from one EI program, which could limit the generalizability of findings given the heterogeneity of EI programming. However, many EI programs routinely collect data elements used in this study, thus providing a common framework to employ in understanding service use patterns. We acknowledge that the study state has relatively generous eligibility criteria and therefore the study sample had relatively minor developmental delays. However, our data are consistent with a nationally representative sample of EI-enrolled children where the vast majority had a developmental delay (versus diagnosed condition) and the most common area of delay was language development. Further research should investigate the state policy levers influencing EI service delivery and interventions to improve EI service breadth and intensity.19 Additionally, we were missing data on COS information for about 30% of the sample. Although we found no differences by measured covariates for children with and without COS information, the possibility exists that the groups vary by unmeasured factors associated with EI access and service use.
In addition, COS scores are consensus ratings informed by parent and provider perceptions of the child’s functioning, which could result in variable score estimation. Multiple functional areas are covered in some COS domains, which could compromise face validity. Also, COS items specify how a functional task is performed, which may not differentiate it from an age-normed developmental score. Therefore, the required developmental assessment could be weighted heavily versus the optional family assessment, which is not completed by all families. As quality improvement initiatives continue to evolve, it will be important to determine best practices related to COS data collection and use to determine its convergent and divergent validity and clinical utility. For example, COS data that are based on measures of developmental status could be compared to those based on both developmental status and family assessment.14 COS is a relatively novel measurement and may not be the best determinant of service provision. While we recognize this as a limitation, we also consider its use an asset to this study as it is untested in the field and shows promising clinical utility for describing EI service need.
Conclusion
This study leveraged common data elements of children discharged from a large, urban EI program to identify salient characteristics that are associated with service use type and intensity. Overall, EI service use intensity was lower than previously reported national estimates. Results also suggest marked disparities in access to EI core services among Hispanic children and families whose primary language is not English. Core EI service access and intensity appear related to children’s social characteristics and functional skills, which provides new insight into the breadth and intensity of EI service needs for continuous quality improvement.
Table 1.
Characteristics of the study sample of children enrolled in an urban early intervention program by predisposing, enabling, and need characteristics (n=2,045)
| Percentages % (n) | |
|---|---|
| Predisposing Characteristics | |
| Child’s Age at EI entry | |
| Less than 12-Months | 25.97 (531) |
| 12–24 Months | 39.80 (814) |
| Greater than 24 Months | 34.23 (700) |
| Race/Ethnicity | |
| White, non-Hispanic | 40.73 (833) |
| Black, non-Hispanic | 10.07 (206) |
| Hispanic | 41.91 (857) |
| Other, non-Hispanic | 7.29 (149) |
| Primary Language, English | 75.79 (1,550) |
| Child’s sex, Female | 36.53 (747) |
| Enabling Characteristics | |
| Public Health Insurance (Medicaid and CHP+) | 55.60 (1,137) |
| Need Characteristics | |
| Condition Type | |
| Developmental Delay (DD) | 89.54 (1,831) |
| Diagnosed Condition (DC) | 10.46 (214) |
| Number of Delay Conditions | |
| One | 71.78 (1,267) |
| Two | 12.97 (229) |
| Three or more | 15.24 (269) |
| Mean (SD) | |
| Entry COSA | (n = 1,326) |
| Positive Social Relationships | 4.96 (1.74) |
| Acquiring and Using Knowledge and Skills | 3.91 (1.58) |
| Taking Appropriate Action to Meet Needs | 4.42 (1.74) |
Each COS sub-scale score is derived from provider clinical judgment, parent concerns, and developmental assessment results and measured on a 7-point scale, from 1=very early skills (i.e., child does not use any immediate foundational skills related to this outcome) to 7=all skills expected (i.e., there are no concerns about the child’s function in this area).
What’s New:
Early intervention (EI) service intensity is low. Access to most core EI services is related to children’s social characteristics and functional performance, and EI therapy service intensity is associated with children’s age and some functional performance measures.
Acknowledgments
BMM and MAK acknowledge funding from the National Institutes of Health (1R03HD084909–01A1) and the Comprehensive Opportunities in Rehabilitation Research Training program (K12 HD05593). These funding sources had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. We thank Briana Rigau for her feedback on earlier versions of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None
Contributor Information
Zachary S. Richardson, Department of Health Systems, Management & Policy, Colorado School of Public Health, 13001 E. 17th Place, MS B119, Aurora, CO 80045.
Mary A. Khetani, Department of Occupational Therapy, College of Applied Health Sciences, University of Illinois at Chicago (UIC), 1919 West Taylor Street, Room 316A, Chicago, IL 60612-7250.
Elizabeth Scully, Rocky Mountain Human Services Early Intervention Program, 9900 East Iliff Avenue, Denver, CO 80231.
Jodi Dooling-Litfin, Rocky Mountain Human Services Early Intervention Program, 9900 East Iliff Avenue, Denver, CO 80231.
Natalie Murphy, Colorado School of Public Health, 13001 E. 17th Place, MS B119, Aurora, CO 80045.
Beth M. McManus, Department of Health Systems, Management & Policy, Colorado School of Public Health, 13001 E. 17th Place, MS B119, Aurora, CO 80045, Phone: 617.529.8138, beth.mcmanus@ucdenver.edu.
References
- 1.PL 108–446. Individuals with Disabilities Education Act, Reauthorization 2004. http://www.copyright.gov/legislation/pl108-446.pdf. Accessed 8 August 2014.
- 2.Outcomes: Federal Requirements. Early Childhood Technical Assistance Center. http://ectacenter.org/eco/pages/fed_req.asp. Accessed February 21, 2018.
- 3.Feinberg E, Silverstein M, Donahue S, Bliss R. The impact of race on participation in Part C early intervention services. Journal of Developmental and Behavioral Pediatrics. 2012;32(4):284–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Twardzik E, Cotto-Negron C, MacDonald M. Factors related to early intervention Part C enrollment: A systematic review. Disability and Health Journal. 2017; 1–8. [DOI] [PubMed] [Google Scholar]
- 5.McManus BM, Rapport MJ, Richardson Z, Lindrooth RL. Differences by condition type in therapy utilization among Medicaid infants and toddlers with special health care needs in Colorado. Pediatric Physical Therapy. 2017. [Google Scholar]
- 6.Khetani M, Richardson Z, McManus BM. Social disparities in early intervention service use and provider-reported outcomes. Journal of Developmental and Behavioral Pediatrics. 2017;38:501–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Outcomes Measurement: Child Outcomes Summary (COS) Process. http://ectacenter.org/eco/pages/cos.asp#COSProcessModule. Accessed 14 March 2018.
- 8.Early Childhood Technical Assistance Center. Part C Infant and Toddler Program Federal Appropriations and National Child Count 1987–2015. http://ectacenter.org/~pdfs/growthcomppartc.pdf. Accessed 1 December 2017.
- 9.Aday LA, Andersen R. A framework for the study of access to medical care. Health Services Research. 1974;9(3):208. [PMC free article] [PubMed] [Google Scholar]
- 10.Hirai AH, Kogan MD, Kandasamy V, Reuland C, Bethell C. Prevalence and variation of developmental screening and surveillance in early childhood. JAMA Pediatrics. 2018. September 1;172(9):857–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Established Condition Database – Early Intervention Colorado. https://docs.google.com/spreadsheets/d/14ZfUsdLaMiv4ULd9oP-xkUVaPkKQQ7KI_yhrPOiFwqA/edit#gid=0. Accessed 22 October 2018
- 12.Barton L, Taylor C, Spiker D, & Hebbeler K (2016). Validity of the data from the Child Outcomes Summary Process: Findings from the ENHANCE Project. Menlo Park, CA: Center for IDEA Early Childhood Data Systems and Early Childhood Technical Assistance Center; http://ectacenter.org/~pdfs/calls/2016/ENHANCEbrief_03-02-16Final.pdf. Accessed 22 October 2018. [Google Scholar]
- 13.Definitions for Child Outcomes Summary (COS) Ratings. Early Childhood Technical Assistance Center. http://ectacenter.org/~pdfs/eco/definitions_outcome_ratings.pdf. Accessed 22 October 2018.
- 14.Bailes AF, Reder R, Burch C. Development of guidelines for determining frequency of therapy services in a pediatric medical setting. Pediatric Physical Therapy. 2008; 20:194–198 [DOI] [PubMed] [Google Scholar]
- 15.Gannotti M, Christy J, Heathcock J, Kolobe T. A Path Model for Evaluating Dosing Parameters for Children With Cerebral Palsy. Phys Ther. 2014; 94(3): 411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.StataCorp. STATA15, Copyright 1996–2017. College Station, TX: Stata-Corp LP. [Google Scholar]
- 17.Davies HT, Crombie IK, Tavakoli M. When can odds ratios mislead? British Medical Journal. 36(7136):989–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brzoska P Using average marginal effects over odds ratios as measures of effect size in epidemiology. Annals of Epidemiology. 2017; 27(8):525–526. [Google Scholar]
- 19.Hebbeler K, Spiker D, Bailey D, et al. Early intervention for infants and toddlers with disabilities and their families: participants, services, and outcomes. Final report of the National Early Intervention Longitudinal Study. 2007. http://www.seels.net/ or http://www.nlts2.org. Accessed December 1, 2017.
- 20.Bruder MB, Dunst CJ. Factors related to the scope of early intervention service coordinator practices. Infants Young Child. 2008;21(3):176–185. doi: 10.1097/01.IYC.0000324547.54693.18. [DOI] [Google Scholar]
- 21.Dunst CJ, Bruder MB. Early Intervention Service Coordination Models and Service Coordinator Practices. J Early Interv. 2006;28(3):155–165. doi: 10.1177/105381510602800301 [DOI] [Google Scholar]
- 22.Kingsley K, Mailloux Z. Evidence for the effectiveness of different service delivery models in early intervention services. American Journal of Occupational Therapy 2013;67:431–436. [DOI] [PubMed] [Google Scholar]
- 23.Agency for Health Care Research and Quality (2011). National healthcare disparities report. https://archive.ahrq.gov/research/findings/nhqrdr/nhdr11/index.html. Accessed 24 October 2018.
- 24.Data Resource Center for Child and Adolescent Health. National survey of children with special health care needs. 2010. http://www.childhealthdata.org/browse/survey. Accessed 24 Oct 2018.
- 25.Mosquera RA, Samuels C, Flores G. Family Language Barriers and Special-Needs Children. Pediatrics. 2016;138(4): e20160321. [DOI] [PubMed] [Google Scholar]
- 26.Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. Journal of Evaluation in Clinical Practice. 2001;17, 268–274. [DOI] [PubMed] [Google Scholar]
- 27.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24), 3186–3191. [DOI] [PubMed] [Google Scholar]
- 28.Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104. [DOI] [PubMed] [Google Scholar]
- 29.Arestad KE, MacPhee D, Lim CY, Khetani MA. Cultural adaptation of a pediatric functional assessment for rehabilitation outcomes research. BMC health services research. 2017. December;17(1):658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Council on Children with disabilities, Section on Developmental Behavioral pediatrics, Bright Futures Steering committee and Medical Home Initiatives for Children with Special Needs Project advisory Committee. Identifying infants and young children with developmental disorders in the medical home: An Algorithm for developmental Surveillance and Screening. Pediatrics 2006;118:405–420. [DOI] [PubMed] [Google Scholar]
- 31.Beckmann KA. “Mitigating adverse childhood experiences through investments in early childhood programs.” Academic pediatrics 17.7 (2017): S28–S29. [DOI] [PubMed] [Google Scholar]
- 32.Litt JS, Glymour MM, Hauser-Cram P, Hehir T, McCormick MC. Early Intervention Services Improve School-age Functional Outcome Among Neonatal Intensive Care Unit Graduates. Academic pediatrics. 2018. May 1;18(4):468–74. [DOI] [PubMed] [Google Scholar]