Abstract
Background: Carpal tunnel release (CTR) can be performed with a variety of anesthesia techniques. General anesthesia is associated with higher risk profile and increased resource utilization, suggesting it should not be routinely used for CTR. The purpose of this study was to examine the patient factors associated with surgeons’ requests for general anesthesia for CTR and the frequency of routine use of general anesthesia by Veterans Health Administration (VHA) surgeons and facilities. Methods: National VHA data for fiscal years 2015 and 2017 were used to identify patients receiving CTR. Mixed-effects logistic regression was used to evaluate patient, procedure, and surgeon factors associated with requests by the surgeon for general anesthesia versus other anesthesia techniques. Results: In all, 18 145 patients underwent CTR performed by 780 surgeons in 113 VHA facilities. Overall, there were 2218 (12.2%) requests for general anesthesia. Although some patient (eg, older age, obesity), procedure (eg, open vs endoscopic), and surgeon (eg, higher volume) factors were associated with lower odds of requests for general anesthesia, there was substantial facility- and surgeon-level variability. The percentage of patients with general anesthesia requested ranged from 0% to 100% across surgeons. Three facilities and 28 surgeons who performed at least 5 CTRs requested general anesthesia for more than 75% of patients. Conclusions: Where CTR is performed and by whom appear to influence requests for general anesthesia more than patient factors in this study. Avoidance of routine use of general anesthesia for CTR should be considered in future clinical practice guidelines and quality measures.
Keywords: anesthesia, carpal tunnel release, health services research, quality measurement, practice variation
Introduction
Each year in the United States, carpal tunnel syndrome affects 16 million people and costs the health care system more than US $2 billion.1,2 In addition to nonoperative treatments provided in diverse health care settings, hand surgeons in the United States annually complete more than 500 000 carpal tunnel releases (CTRs) to treat this disabling syndrome.3,4 Carpal tunnel release can be successfully performed with a variety of anesthesia techniques, including local anesthesia (with or without sedation), regional or peripheral nerve block (with or without sedation), and general anesthesia. Ideally, the choice of anesthesia technique should optimize benefits, minimize risk, and control costs.
Relevant to this balance, several studies have found general anesthesia for CTR and other outpatient hand surgeries to be associated with higher resource utilization5-9 and risk of postoperative complications.6,10,11 A prospective comparative study of anesthetic techniques on clinical outcomes and costs of outpatient hand surgery found intravenous regional anesthesia to be associated with less postoperative nausea and earlier discharge compared with general anesthesia.6 Patients receiving general anesthesia were significantly more likely to require opioid analgesics after surgery (85%), compared with intravenous regional anesthesia (51%) or brachial nerve block (43%).6 Intravenous regional anesthesia was also associated with 30% lower nursing cost and 84% lower anesthesia drug cost compared with general anesthesia.6 A recent analysis of American College of Surgeons National Surgical Quality Improvement Program hand surgery data found general anesthesia to be associated with 59% higher odds of postoperative complications (odds ratio [OR] = 1.59 [1.19-2.13])—with even higher odds for patients over 65 years old (OR = 3.26 [1.69-6.28]).12 Risk of a serious complication was 1.2% for patients undergoing general anesthesia, more than twice as high as other anesthetic techniques.12 However, the overall risk of complications is low for CTR, and certain patient or context factors may justify general anesthesia in some cases.
Adapting concepts from the American Society of Anesthesiologists (ASA) Task Force on Pre-anesthesia Evaluation13 and the Agency for Healthcare Research and Quality (AHRQ),14 routine selection of an anesthesia technique can be defined as choosing the same technique in almost all cases, independent of patient characteristics or preferences. In the absence of a standard threshold, in this study we define routine selection as choice of the same technique in at least 75% of cases. Routine selection stands in contrast to per-protocol selection in which an anesthesia technique is systematically chosen based on a variety of patient and context characteristics. The third strategy is ad hoc or elective selection in which anesthetic technique is chosen at the discretion of the care team, perhaps based on the patient’s history, physical findings, or preference, but not chosen routinely or based on a protocol.
The higher risk of complications and higher perioperative resource use associated with general anesthesia suggest it should not routinely be the first-line option for CTR, but may be justified for specific patients (per-protocol or ad hoc selection). Although overall rates of general anesthesia use have been reported in samples of CTR patients, these overall rates may mask surgeon- and facility-level variability. For example, 13% of CTRs from the 2006 National Survey of Ambulatory Surgery received general anesthesia, but the distribution of general anesthesia rates between facilities was not described.5 Therefore, it is currently unknown to what extent general anesthesia is routinely used for CTR. If the consensus emerges that routine use of general anesthesia for CTR should be avoided, then it is important to know the extent, distribution, and drivers of the practice to inform clinical practice guideline and quality measure development, as well as efforts to design and test improvement strategies.
The goal of this study was to understand patterns and drivers of general anesthesia for CTR. We examined patient factors associated with surgeons’ requests for general anesthesia at the time of scheduling CTR, as well as the concentration of such requests from specific surgeons in specific facilities in the Veterans Health Administration (VHA). The VHA is the largest integrated health care system in the United States, in which approximately 10 000 CTRs are performed annually. We hypothesized that requests for general anesthesia for CTR would be strongly clustered in a subset of surgeons and facilities and would only be weakly linked to patient characteristics. Furthermore, we hypothesized that evidence of routine use of general anesthesia for CTR would be concentrated in a minority of surgeons and facilities.
Materials and Methods
Data from fiscal years 2015 and 2017 were extracted from the VHA Corporate Data Warehouse (CDW) Procedure Table and Surgery Table and used to identify the first CTR for each patient in the sample. The CDW Procedure Table captures surgeries that occur in nonoperating room locations (eg, procedure rooms) as well as some operating room cases. The CDW Surgery Table only captures surgeries that occur in operating rooms. Open and endoscopic CTRs were identified with the Current Procedural Terminology codes 64721 and 29848, respectively. Patients who were nonenrollees of VHA or who had another concurrent surgery that might have influenced the requested anesthesia were excluded.
The primary outcome variable was the anesthesia technique requested by the surgeon when the procedure was scheduled. Data on which anesthesia technique was actually used (vs requested) for each procedure do not exist in a usable form in national VHA data. Requested anesthesia was operationalized as a binary variable (general anesthesia vs local, nerve block, monitored anesthesia care [MAC], “choice,” and unrecorded). “Choice” is a designation made by the surgeon to allow the anesthesiologist to choose the anesthesia technique. For CTRs in which the requested anesthesia type was “choice” or unrecorded, we included only those which occurred outside of operating room locations and that we assumed to have been performed without general anesthesia. The CTRs with missing or “choice” requested anesthesia type that were performed in operating rooms were excluded because they may or may not have involved general anesthesia.
Patient-level predictor variables included age, sex, race/ethnicity, marital status, percent service connected (an indicator of VHA health care coverage), and comorbidities included in the Elixhauser Comorbidity Index,15 plus obstructive sleep apnea. The CTRs were classified as open versus endoscopic, and unilateral versus bilateral. Surgeon-level volume of CTR in the observation period was also included as a predictor. Mixed-effects logistic regression was used to evaluate the extent to which patient, procedure, and surgeon factors predicted surgeon request for general anesthesia versus other anesthesia techniques when the procedure was scheduled, accounting for clustering within surgeon and facilities.
Results
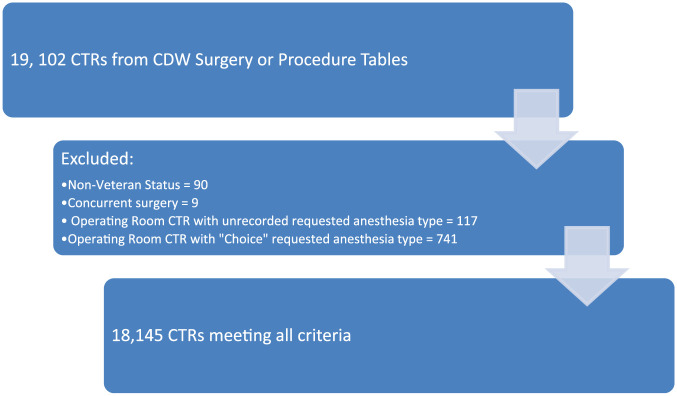
Of the 19 021 CTRs identified during the observation period, 18 145 CTRs performed by 780 surgeons in 113 VHA facilities met inclusion criteria (Figure 1). Characteristics of patients in the cohort are presented in Table 1. Typical of the overall VHA population, the sample had a mean age of 61.3 years and was predominantly men and Caucasian (89.5% and 75.7%, respectively). Of the procedures in the sample, 1188 (6.5%) were performed endoscopically and 551 (3.0%) were bilateral. The distribution of anesthesia types that were requested by surgeons at the time the procedure was scheduled is presented in Table 2. The MAC was requested most often (36.5%) and nerve blocks least often (11.0%). The requested anesthesia type was not recorded or listed as “choice” for 5001 nonoperating room CTRs, assumed to not have involved general anesthesia (27.6%).
Figure 1.
Application of cohort eligibility criteria.
Note. CTR = carpal tunnel release; CDW = Corporate Data Warehouse.
Table 1.
Characteristics of 18 145 Veterans Health Administration Patients Receiving CTR in Fiscal Years 2015 and 2017.
| Patient and Procedure Characteristics | Summary Statistics |
|---|---|
| Mean (SD) age | 61.3 (13.2) |
| Male | 89.5% |
| Non-Hispanic White | 75.7% |
| African American | 12.2% |
| Hispanic White or other minority | 6.9% |
| Married | 58.3% |
| Service connected | 63.6% |
| Congestive heart failure | 2.7% |
| Valvular disease | 1.9% |
| Pulmonary circulation disorders | 2.7% |
| Peripheral vascular disorders | 3.8% |
| Hypertension, uncomplicated | 43.6% |
| Hypertension, complicated | 3.6% |
| Paralysis | 0.6% |
| Other neurological disorders | 3.7% |
| Chronic pulmonary disease | 11.5% |
| Diabetes, uncomplicated | 13.6% |
| Diabetes, complicated | 11.5% |
| Hypothyroidism | 6.5% |
| Renal failure | 4.5% |
| Liver disease | 3.3% |
| Peptic ulcer disease | 0.2% |
| AIDS/HIV | 0.1% |
| Lymphoma | 0.3% |
| Metastatic cancer | 0.2% |
| Solid tumor without metastasis | 3.8% |
| Rheumatoid arthritis | 2.0% |
| Coagulopathy | 1.2% |
| Obesity | 21.9% |
| Weight loss | 1.1% |
| Fluid and electrolyte disorders | 3.1% |
| Blood loss anemia | 0.2% |
| Deficiency anemia | 5.7% |
| Alcohol use disorder | 6.2% |
| Drug use disorder | 3.9% |
| Psychoses | 7.4% |
| Depression | 17.7% |
| Obstructive sleep apnea | 17.4% |
| Endoscopic CTR | 6.5% |
| Bilateral CTR | 3.0% |
Note. CTR = carpal tunnel release.
Table 2.
Requested Anesthesia for Carpal Tunnel Release at the Time of Scheduling.
| Requested anesthesia type | No. | Percent |
|---|---|---|
| General anesthesia | 2218 | 12.2 |
| Local anesthesia | 2300 | 12.7 |
| Monitored anesthesia care | 6627 | 36.5 |
| Regional or peripheral nerve block | 1999 | 11.0 |
| Nonoperating room unknowna | 5001 | 27.6 |
Carpal tunnel releases with requested anesthesia listed as “choice” or unrecorded AND Location Type other than Operating Room.
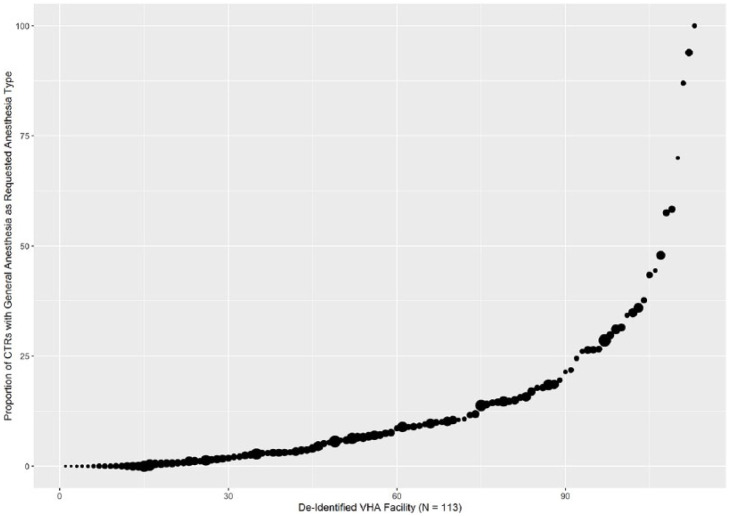
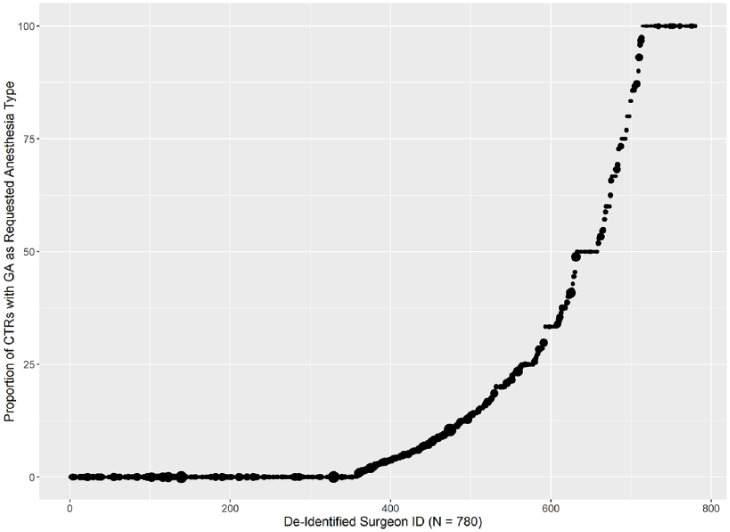
Overall, there were 2218 (12.2%) requests for general anesthesia with substantial facility- and surgeon-level variability (Figures 2 and 3). Among the 113 facilities, the median percentage of patients with general anesthesia requested was 7.1%, with a range of 0% to 100%. Three facilities requested general anesthesia for more than 75% of their CTR patients (86.7%, 93.9%, and 100%, respectively), representing 197 of 211 CTRs performed at these facilities, suggesting routine selection (Figure 2). Among the 780 surgeons performing CTR, the median percentage of patients for whom general anesthesia was requested was 3.3%, with a range of 0% to 100% (Figure 3). Among 299 surgeons who performed fewer than 5 CTRs, general anesthesia was requested for 25% of cases (155 of 619). Twenty-eight surgeons (4%) who performed at least 5 CTRs, and 63 (8.1%) who performed fewer than 5 CTRs, requested general anesthesia for more than 75% of their patients, suggesting routine selection.
Figure 2.
Variation in VHA facilities in surgeons’ requests for general anesthesia for CTR.
Note. VHA = Veterans Health Administration; CTR = carpal tunnel release.
Figure 3.
Variation in VHA surgeons’ requests for general anesthesia (GA) for CTR.
Note. VHA = Veterans Health Administration; CTR = carpal tunnel release.
After accounting for clustering within surgeon and facility, mixed-effects logistic regression (Table 3) revealed that older age and having a diagnosis of congestive heart failure, or obesity was associated with lower odds of having general anesthesia requested by the surgeon. Having a diagnosis of uncomplicated hypertension or liver disease was associated with higher odds of general anesthesia being requested. No other patient factors included in the model were significantly associated with general anesthesia being requested. Bilateral CTRs and those performed endoscopically were associated with higher odds of general anesthesia being requested. Surgeons with higher volume of CTR cases were significantly less likely to request general anesthesia. The intraclass correlation coefficient (ICC) of a mixed-effects regression model is a measure of how much outcome variance exists at different levels (ie, patient, surgeon, facility). The ICCs were 0.36 for the facility level and 0.32 for the surgeon level. This signifies that approximately 68% of the overall variance is due to facility and surgeon factors rather than the patient and procedure characteristics included in the model.
Table 3.
Mixed-Effects Logistic Regression Examining Association Between Patient, Procedure, and Surgeon Characteristics and Surgeons’ Requests for General Anesthesia for CTR.
| Coefficient | SE | Z | P value | |
|---|---|---|---|---|
| Intercept | −0.763 | 0.247 | −3.085 | .002*** |
| Age | −0.015 | 0.002 | −6.489 | .000*** |
| Female | 0.029 | 0.084 | 0.348 | .728 |
| Hispanic White or other minority (ref.: AA) | −0.198 | 0.117 | −1.684 | .092 |
| Non-Hispanic White (ref.: AA) | −0.142 | 0.079 | −1.796 | .073 |
| Single or never married (ref.: married) | −0.088 | 0.082 | −1.071 | .284 |
| Separated/divorced/widow (ref.: married) | −0.052 | 0.060 | −0.878 | .380 |
| Not service connected | 0.009 | 0.056 | 0.161 | .872 |
| Congestive heart failure | −0.515 | 0.216 | −2.385 | .071* |
| Valvular disease | −0.213 | 0.219 | −0.973 | .331 |
| Pulmonary circulation disorders | −0.049 | 0.150 | −0.329 | .741 |
| Hypertension, uncomplicated | 0.150 | 0.059 | 2.539 | .001** |
| Hypertension, complicated | −0.186 | 0.183 | −1.016 | .310 |
| Paralysis | 0.499 | 0.310 | 1.611 | .107 |
| Other neurological disorders | 0.188 | 0.134 | 1.399 | .162 |
| Chronic pulmonary disease | −0.069 | 0.085 | −0.806 | .420 |
| Diabetes, uncomplicated | 0.083 | 0.079 | 1.040 | .299 |
| Diabetes, complicated | 0.041 | 0.091 | 0.454 | .650 |
| Hypothyroidism | −0.068 | 0.110 | −0.617 | .537 |
| Renal failure | −0.179 | 0.147 | −1.220 | .223 |
| Liver disease | 0.324 | 0.129 | 2.513 | .012* |
| Peptic ulcer disease | 0.337 | 0.549 | 0.590 | .555 |
| AIDS/HIV | −0.418 | 0.563 | −0.742 | .458 |
| Lymphoma | 0.004 | 0.511 | 0.008 | .993 |
| Metastatic cancer | 0.133 | 0.521 | 0.255 | .789 |
| Solid tumor without metastasis | 0.094 | 0.143 | 0.660 | .509 |
| Rheumatoid arthritis | −0.090 | 0.180 | −0.501 | .617 |
| Coagulopathy | −0.321 | 0.261 | −1.230 | .219 |
| Obesity | −0.184 | 0.068 | −2.726 | .006** |
| Weight loss | −0.104 | 0.268 | −0.389 | .697 |
| Fluid and electrolyte disorders | 0.176 | 0.150 | 1.175 | .240 |
| Blood loss anemia | 0.574 | 0.499 | 1.149 | .251 |
| Deficiency anemia | −0.201 | 0.1121 | −1.659 | .097 |
| Alcohol use disorder | 0.140 | 0.109 | 1.281 | .199 |
| Drug use disorder | −0.205 | 0.138 | −1.486 | .137 |
| Psychoses | 0.077 | 0.097 | 0.790 | .429 |
| Obstructive sleep apnea | −0.132 | 0.073 | −1.793 | .073 |
| Endoscopic CTR (ref.: open) | 0.675 | 0.184 | 3.658 | .003** |
| Bilateral CTR (ref.: unilateral) | 0.858 | 0.152 | 5.658 | .000*** |
| Surgeon annual CTR volume | −0.015 | 0.002 | −6.02 | .000*** |
Note. Station-level ICC = 0.356; surgeon-level ICC = 0.316. Z = Z statistic; CTR = carpal tunnel release; AA = African American; ICC = intraclass correlation coefficient.
P < .05. **P < .01. ***P < .001.
Discussion
Evidence indicates that general anesthesia for hand surgery is associated with higher complication rates5-9 and resource use6,10,11 than other anesthesia options. This suggests it should not be routinely used for CTR, although it might be justified for specific patients. In this study, as hypothesized, we found that requests for general anesthesia for CTR are strongly clustered in a subset of surgeons and facilities and only partially driven by patient characteristics. We found a number of VHA facilities and surgeons that requested general anesthesia for more than 75% of their CTR patients, indicative of routine selection. Across the national sample, certain patient factors (eg, obesity or congestive heart failure) and procedure factors (open CTR vs endoscopic; unilateral vs bilateral) were associated with odds of having general anesthesia requested, suggesting at least some per-protocol or ad hoc selection of anesthesia technique is occurring.
The ASA Task Force on Pre-anesthesia Evaluation suggests that the anesthesia plan should be driven by patient-level evaluations of risk (procedural and anesthetic) along with patient preference.16 However, we found that the specific surgeon and facility where CTR is performed appears to influence the use of general anesthesia more than patient and procedure factors included in this study. Our data indicate that substantial surgeon-level variability exists with lower volume surgeons more likely to request general anesthesia. The typical arc of quality improvement and implementation science suggests the importance of properly diagnosing a gap in quality before designing a strategy to address it.17 It could be that surgeons who infrequently perform CTR are less confident to perform CTR outside the operating room or are unfamiliar with less sedating techniques. Or perhaps the patterns we observed at some locations were driven by the preferences of anesthesiologists or standard operating procedures for a wide variety of procedures, not the result of the specific preferences of hand surgeons. Future qualitative studies among surgeons and anesthesiologists should clarify the contextual factors and decision processes related to choices of anesthesia technique.18 Only then will enough information be available to design and test strategies to improve practice.
It will be especially important to better understand drivers of routine rather than targeted general anesthesia for CTR. For example, we noted that uncomplicated hypertension was associated with higher chances of a request for general anesthesia. Further evaluation of this counterintuitive result may explore how uncomplicated hypertension is evaluated preoperatively by facilities or surgeons with high rates of general anesthesia for CTR. Although this study focused on one specific hand surgery, it is possible that the overall pattern of results applies to other minor hand surgeries, such as trigger finger release or De Quervain release, where several anesthesia options also exist.
This study has several limitations, most prominently the lack of data on which anesthesia techniques were used versus requested, as well as the outcomes associated with anesthetic type. This is a current limitation of VHA national data that might have affected the results presented here. Relatedly, 27.6% of the cases had unrecorded or ambiguous (“choice”) requests of anesthesia technique. For these CTRs, we included only those that were performed outside the operating room to assume they were unlikely to have involved general anesthesia. Also, the patient characteristics and context of VHA are unique. It is important to repeat similar analyses in other health care contexts to understand whether use of general anesthesia is surgeon- and facility-driven in the private sector.
Although no established threshold exists to define routine selection of anesthesia technique, our results suggest that a small number of VHA surgeons and facilities request general anesthesia for more than 75% of CTRs. These data will be useful in future discussions regarding whether avoidance of routine use of general anesthesia should be included in the next version of clinical practice guidelines or quality measures, as well as what threshold should be used as an indicator for routine selection.
Footnotes
Authors’ Note: Erika D. Sears is also affilaited with Ann Arbor Veterans Affairs Medical Center, MI, USA.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Statement of Informed Consent: This study of existing health care data was conducted under a waiver of informed consent.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by grants from the VA HSR&D Service (I01-HAX002314-01A1; RCS14-232; CDA 13-279). The views expressed do not reflect those of the US Department of Veterans Affairs (VA) or other institutions.
ORCID iDs: Alex HS Harris  https://orcid.org/0000-0001-7267-3077
https://orcid.org/0000-0001-7267-3077
Robin N Kamal  https://orcid.org/0000-0002-3011-6712
https://orcid.org/0000-0002-3011-6712
References
- 1. Stapleton MJ. Occupation and carpal tunnel syndrome. ANZ J Surg. 2006;76(6):494-496. [DOI] [PubMed] [Google Scholar]
- 2. Dale AM, Harris-Adamson C, Rempel D, et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39(5):495-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fajardo M, Kim S, Szabo R. Incidence of carpal tunnel release: trends and implications within the United States ambulatory care setting. J Hand Surg Am. 2012;37:1599-1605. [DOI] [PubMed] [Google Scholar]
- 5. Nguyen C, Milstein A, Hernandez-Boussard T, Curtin CM. The effect of moving carpal tunnel releases out of hospitals on reducing United States health care charges. J Hand Surg Am. 2015;40(8):1657-1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chan VW, Peng PW, Kaszas Z, et al. A comparative study of general anesthesia, intravenous regional anesthesia, and axillary block for outpatient hand surgery: clinical outcome and cost analysis. Anesth Analg. 2001;93(5):1181-1184. [DOI] [PubMed] [Google Scholar]
- 7. Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y). 2007;2(4):173-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davison PG, Cobb T, Lalonde DH. The patient’s perspective on carpal tunnel surgery related to the type of anesthesia: a prospective cohort study. Hand (N Y). 2013;8(1):47-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Foster BD, Sivasundaram L, Heckmann N, et al. Surgical approach and anesthetic modality for carpal tunnel release: a nationwide database study with health care cost implications. Hand (N Y). 2017;12(2):162-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nelson R, Higgins A, Conrad J, Bell M, Lalonde D. The wide-awake approach to Dupuytren’s disease: fasciectomy under local anesthetic with epinephrine. Hand (N Y). 2010;5(2):117-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hadzic A, Arliss J, Kerimoglu B, et al. A comparison of infraclavicular nerve block versus general anesthesia for hand and wrist day-case surgeries. Anesthesiology. 2004;101(1):127-132. [DOI] [PubMed] [Google Scholar]
- 12. Hustedt JW, Chung A, Bohl DD, Olmschied N, Edwards SG. Comparison of postoperative complications associated with anesthetic choice for surgery of the hand. J Hand Surg Am. 2017;42(1):1-8.e5. [DOI] [PubMed] [Google Scholar]
- 13. American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Practice advisory for preanesthesia evaluation: a report by the American Society of Anesthesiologists Task Force on Preanesthesia evaluation. Anesthesiology. 2002;96:485-496. [DOI] [PubMed] [Google Scholar]
- 14. Balk E, Earley A, Hadar N, Shah N, Trikalinos TA. Benefits and harms of routine preoperative testing: comparative effectiveness. Review No. 130. Published 2014. Rockville, MD: Agency for Healthcare Research and Quality, US. [PubMed] [Google Scholar]
- 15. Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser comorbidity index. Med Care. 2017(7);55:698-705. [DOI] [PubMed] [Google Scholar]
- 16. American Society of Anesthesiologists Task Force on Preanesthesia Evaluation, Apfelbaum JL, Connis RT, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116(3):522-538. [DOI] [PubMed] [Google Scholar]
- 17. Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. 2015;3:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Flierler WJ, Nubling M, Kasper J, Heidegger T. Implementation of shared decision making in anaesthesia and its influence on patient satisfaction. Anaesthesia. 2013;68(7):713-722. [DOI] [PubMed] [Google Scholar]