Abstract
Introduction
Few studies are available to appreciate the broad spectrum of dive-related injuries (DI), which are not limited to decompression illness (DCI) and fatalities. Studies supporting injury-management efficacy from early recognition to first-aid, final treatment and outcome are also lacking. This study aims at making an epidemiologic inventory of DI among French scuba divers.
Methods
This online, retrospective, cross-sectional survey analyzed self-reported symptoms, context of occurrence, initial response and outcome. The relationships between symptoms and diver characteristics were assessed and severity scores created from the reports.
Results
A total of 799 divers responded, of whose questionnaires 784 were sufficiently complete to be analyzed. Approximately one-third (35%) of respondents had never experienced a DI. DCI-like symptoms represent a small fraction of DIs, the most commonly reported being ear barotrauma. Self-reported symptom rates decreased with increasing age and male sex. The ranking dive leader was the primary care provider in 58% of reports and 32% of injured divers never sought help. Management decisions (first aid and/or hyperbaric oxygen treatment) were related to the severity score. Complete resolution was achieved in 84 (74%) of 114 DCI cases, whilst mild (n = 22, 19%) and severe (n = 8, 7%) residual symptoms were reported. One in 10 divers who did not seek treatment for symptoms believed to be related to DCI declared some residual symptoms.
Conclusion
Based on these results, diving injury rates may be higher than previously reported. However, the most frequent symptoms appear to be of only a modest nature.
Keywords: Diving incidents, Epidemiology, Barotrauma, Decompression illness, First aid, Hyperbaric oxygen therapy
Introduction
Although generally a safe sport, scuba diving is associated with a spectrum of injury severity. Data from the French Federation of Undersea Studies and Sports (FFESSM), the main diver training organization in France, indicate roughly proportional increases in numbers of French divers undergoing advanced training and the numbers of recorded injuries, from 170 in 1991 to 412 in 2013.[ 1] Reports on dive-related injuries (DI) have concentrated on acute and/or severe injuries, primarily decompression illness (DCI) and fatalities.[ 2 - 4] However, DI are not limited to DCI and fatalities but, rather, cover a much broader spectrum, with other injuries remaining largely unaccounted for.[ 5] Owing to a paucity of data regarding the risk and prevalence of DI among recreational divers,[ 5 - 7] it is difficult to provide an overview of the situation. This occurs because the reporting of recreational diving accidents is not mandatory unlike the protocols for military or scientific diving.[ 8 - 10] According to the few readily available reports on DI, the most common insults do not involve DCI. For example, mild ear barotrauma and sinus barotrauma were common amongst a sample of 709 divers.[ 11 , 12] These symptoms were experienced on more than one occasion by 369 (52%) and 245 (35%) divers, respectively. Only a small proportion (4%) of divers reported symptoms of DCI. More recently, 20 diving-related injuries of sufficient concern to be logged in the dive boat manifest were reported out of 97,144 dives, 11 being non DCI-related incidents, including ear and sinus barotraumas.[ 13]
Accurate data concerning incident management, from the recognition of a DI by divers to the implementation of a treatment, first aid and/or hyperbaric oxygen treatment (HBOT), are also lacking.[ 14] Indeed, even if DCI may be tracked through hyperbaric treatment records, less is known regarding how divers respond to a problem. A significant proportion of sports divers in Orkney either failed to identify DCI or underestimated the potential consequences if left untreated.[ 14] According to data from 183 injured recreational divers treated in Corsica between 1996 and 2000, 54% of cases involved a delay of more than one hour before the emergency medical services were activated.[ 15]
First aid and adjunctive therapies for DI are mainly supported by accumulated experience over decades or by clinical judgement,[ 16] ather than being evidence-based. For example, surface oxygen is widely employed in the treatment of DI, but its use is supported by animal experiments only,[ 17] with few human studies supporting its efficacy.[ 18 , 19] More importantly, it seems from those studies that administration of first-aid oxygen serves to reduce the number of recompressions required but cannot necessarily improve the odds of recovery.
Improving knowledge of the pattern, frequency, management and outcome of DI is of importance to provide better insights for prevention and treatment. The aim of this study was to create an epidemiologic inventory of recreational diving injuries and their consequences among individuals that dived in French territorial waters (metropolitan and overseas territories).
Methods
Experimental procedures, conducted in accordance with the Declaration of Helsinki, were approved by the local correspondent of the Western Brittany University for informatic database and individual liberties (European Directive 95/46/EC).[ 20] Participation was voluntary, and responses were confidential. No identifying information was collected.
A cross-sectional study of French recreational divers used a questionnaire (Google Form) to investigate:
Diver demographic data, including dive experience;
Self-reported symptoms and the context of the incident;
First aid, medical intervention and outcome.
This self-reported online survey was conducted from 21 November 2017 to 05 March 2018 inclusive. In order to obtain a representative sample of the diving population, diving organizations and their national representatives were identified and contacted by email. The questionnaire was further disseminated through social networks and diving forums to allow us to also contact unaffiliated divers.
The retrospective survey focused on participant diving exposures and diving-related injuries. It was designed to address the presence of clinical symptoms rather than the presence of a type of accident (e.g., 'ear barotrauma' or 'neurological DCS'). The development of questions was based on the current literature regarding dive-related epidemiology.[ 5 - 7 , 21] In total, 28 symptoms were investigated. When a symptom was reported, contextual parameters (optional questions), such as dive environment and profiles, were also recorded. Finally, first aid, medical intervention and outcomes were also investigated. All questions were written to be understandable regardless of any previous knowledge of diving physiology and/or diving medicine. A draft version was sent to 10 divers of different certification levels (instructors and medical staff included) and from three different regions of France, and some questions which could be misinterpreted or not understood (e.g., a complicated medical term) were modified. A second validation was made in ‘real’ conditions by sending a beta version through social networks and email (which was the final mode of dissemination). In this manner, 69 responses were obtained, of which 67 contained sufficient information to be analyzed. This led us to additional minor adjustments to ensure that the survey avoided ambiguity.
STATISTICAL ANALYSIS
Most responses were analyzed descriptively. The relationship between the presence/absence of symptoms and divers’ characteristics were calculated from all self-reported dive-related symptoms using Pearson's Chi-squared Test. Since all discrete data, except the number of dives, passed the Kolmogorov-Smirnov test, allowing us to assume a Gaussian distribution, comparison between variables was carried out with unpaired t-tests. We used Chi-square tests to compare the number of dives. Statistical analysis was conducted with Statistica© software (ver. 10, StatSoft France, 2011). A probability of P < 0.05 was considered statistically significant. However, in case of multiple comparisons, this P-value was divided by the number of independent tests. Indeed, when the influence of sex on the age of divers, dive experience and certification level was tested, a P-value of 0.016 was considered statistically significant, whereas a probability of P < 0.007 was considered statistically significant for the influence of sex, age, dive experience, certification level, time spent in physical activity, dive location and seasonal rhythm of diving.
Results
Because of the method used for the dissemination of the questionnaire, the number of divers who accessed the questionnaire is unknown. A total of 799 divers responded during the study period, of whose questionnaires 784 were analysable. The respondents were geographically widespread within France and included both inland and coastal areas. All the French territories were represented except for French Guiana.
DESCRIPTION OF THE RESPONDENTS
Characteristics are described in Table 1. The majority of divers were men (n = 586, 75%) while women (n = 198) represented 25% of the total sample. The sex distribution within the different age categories was significantly different (χ² = 35.25, df = 5, P < 0.001); in men, the most representative age group was 46–55 years old (25.3%), then 36–45 years old (20.3%) second, whilst in women the age groups were represented more evenly (26–35 years old, 6.3%; 36–45, 5.8%; 46–55, 6.9%). Most respondents were experienced scuba divers, the majority being certified instructors (55%) or with advanced level certifications (41%); 4% having only a basic certification. However, sex distribution among all certification levels was significantly different (χ² = 142.72, df = 5, P < 0.001); the higher the certification level, the lower the proportion of women.
Table 1. Respondent profiles (n = 784); missing values in the table refer to the missing data from the respondents; * − diving certification: Basic = EN 14153-1/ISO 24801-1 level 1 'supervised diver'; Autonomous = EN 14153-2/ ISO 24801-2 level 2 'autonomous diver'; Advanced and dive guide = EN 14153-3/ ISO 24801-3 level 3 'dive leader'; Instructor = EN 14413-1/ ISO 24802-1 level 1 scuba instructor or EN 14413-2/ ISO 24802-2 level 2 scuba instructor. For simplicity of presentation, categories were pooled for the following components: Age, physical activity, experience (years) and experience (number of dives) .
| Male | Female | Total | |||||||
| n | % | % of total | n | % | % of total | n | % | ||
| Age (years) | |||||||||
| 18–35 | 101 | 17.2 | 12.9 | 71 | 35.9 | 9.1 | 172 | 22.0 | |
| 36–45 | 159 | 27.1 | 20.3 | 46 | 23.2 | 5.8 | 205 | 26.1 | |
| 46–55 | 198 | 33.8 | 25.3 | 54 | 27.3 | 6.9 | 252 | 32.2 | |
| > 56 | 127 | 21.7 | 16.2 | 26 | 13.1 | 3.3 | 153 | 19.5 | |
| Missing | 1 | 0.2 | 0.1 | 1 | 0.5 | 0.1 | 2 | 0.2 | |
| Physical activity (h/week) | |||||||||
| < 2 hr | 348 | 59.4 | 44.4 | 136 | 68.7 | 17.3 | 484 | 61.8 | |
| > 2 hr | 238 | 40.6 | 30.4 | 62 | 31.3 | 7.9 | 300 | 38.2 | |
| Dive certification* | |||||||||
| Basic | 10 | 1.7 | 1.2 | 20 | 10.1 | 2.6 | 30 | 3.8 | |
| Autonomous | 65 | 11.1 | 8.3 | 47 | 23.7 | 6.0 | 112 | 14.3 | |
| Advanced | 97 | 16.6 | 12.4 | 46 | 23.2 | 5.9 | 143 | 18.3 | |
| Dive guide | 54 | 9.2 | 6.9 | 11 | 5.6 | 1.4 | 65 | 8.3 | |
| Instructor | 358 | 61.1 | 45.7 | 74 | 37.4 | 9.4 | 432 | 55.1 | |
| Missing | 2 | 0.3 | 0.2 | 0 | 0.0 | 0.0 | 2 | 0.2 | |
| Open vs closed-circuit | |||||||||
| Open-circuit | 506 | 86.4 | 64.5 | 189 | 95.5 | 24.1 | 695 | 88.6 | |
| Rebreather | 71 | 12.1 | 9.1 | 8 | 4.0 | 1.0 | 79 | 10.1 | |
| Missing | 9 | 1.5 | 1.2 | 1 | 0.5 | 0.1 | 10 | 1.3 | |
| Breathing gas | |||||||||
| Air | 458 | 78.2 | 58.4 | 173 | 87.4 | 22.1 | 631 | 80.5 | |
| Nitrox | 101 | 17.2 | 12.9 | 22 | 11.1 | 2.8 | 123 | 15.7 | |
| Trimix | 24 | 4.1 | 3.0 | 3 | 1.5 | 0.4 | 27 | 3.4 | |
| Missing | 3 | 0.5 | 0.4 | 0 | 0.0 | 0.0 | 3 | 0.4 | |
| Experience (years) | |||||||||
| < 6 months | 0 | 0 | 0 | 4 | 2.0 | 0.5 | 4 | 0.5 | |
| 1 to 5 | 104 | 17.7 | 13.3 | 57 | 28.8 | 7.3 | 161 | 20.6 | |
| 5 to 10 | 112 | 19.1 | 14.3 | 33 | 16.7 | 4.2 | 145 | 18.5 | |
| 10 to 20 | 151 | 25.8 | 19.2 | 65 | 32.8 | 8.3 | 216 | 27.5 | |
| > 20 | 218 | 37.2 | 27.8 | 38 | 19.2 | 4.9 | 256 | 32.7 | |
| Missing | 1 | 0.2 | 0.1 | 1 | 0.5 | 0.1 | 2 | 0.2 | |
| Experience (number of dives) | |||||||||
| < 50 | 35 | 5.9 | 4.5 | 34 | 17.2 | 4.3 | 69 | 8.8 | |
| 51 to 300 | 157 | 26.8 | 20.0 | 79 | 39.9 | 10.1 | 236 | 30.1 | |
| 301 to 1,000 | 160 | 27.4 | 20.4 | 45 | 22.7 | 5.7 | 205 | 26.1 | |
| 1,001 to 3,000 | 108 | 18.4 | 13.8 | 17 | 8.6 | 2.2 | 125 | 16.0 | |
| > 3,000 | 34 | 5.8 | 4.3 | 8 | 4.0 | 1.1 | 42 | 5.4 | |
| Missing | 92 | 15.7 | 11.7 | 15 | 7.6 | 1.9 | 107 | 13.6 | |
Eighteen training organizations were represented with the vast majority of divers belonging to three, namely FFESSM (n = 664, 85%), Professional Association of Diving Instructors (n = 135, 17%), and Scuba Schools International (n = 43, 5 %). Most divers declared more than one affiliation, while others (n = 21, 3%), although trained and certified according to the ISO 24801/24802 standards were unaffiliated.
A total of 683,171 dives were reported over a period ranging from less than six months to over 30 years (median 400 per diver, interquartile range (IQR) 150−1,000 dives). Dive experience in years of practice was significantly lower in females than males (χ² = 45.58, df = 7, P < 0.001). The number of dives undertaken per year ranged from five to 230 (median 40, IQR 19–95).
SELF-REPORTED SYMPTOMS AND CONTEXT OF OCCURRENCE
Self-reported diving-related symptoms covered a 43-year span (from 1974 to 2017) and are summarised in Table 2. A total of 513 respondents (65%) reported at least one symptom, whilst 274 (35%) had not experienced any symptoms since the beginning of their diving career. The maximum number of symptoms reported by a diver was 23; however, the median was 1 (IQR 0–2) injury per diver. The primary symptom was related to the ears (ear pain in 44.8% at least once). After context analysis of self-reported symptoms through the optional questions, it appeared that the most common injuries incurred by divers were barotrauma (n = 320, 63% of the injured divers) followed by DCI (n = 146, 28% of injured divers). In 47 cases (9% of injured divers) a formal diagnosis could not be made.
Table 2. Self-reported symptoms after a dive; although some respondents may have declared several episodes, percentage calculations are made on the first episode .
| Male | Female | Total | ||||||
| (n = 586) | (n = 198) | (n = 784) | ||||||
| n | % | % of total | n | % | % of total | n | % | |
| No symptom reported | 222 | 37.9 | 28.3 | 49 | 24.7 | 6.3 | 271 | 34.6 |
| Self-reported symptoms | 364 | 62.1 | 46.4 | 149 | 75.3 | 19.0 | 513 | 65.4 |
| Ear pain | 240 | 40.9 | 30.6 | 111 | 56.0 | 14.2 | 351 | 44.8 |
| Sinus pain | 144 | 24.6 | 18.4 | 60 | 30.3 | 7.6 | 204 | 26.0 |
| Toothache | 58 | 9.9 | 7.4 | 26 | 13.1 | 3.3 | 84 | 10.7 |
| Loss of hearing or ringing in ears | 50 | 8.5 | 6.4 | 19 | 9.6 | 2.4 | 69 | 8.8 |
| Headache | 28 | 4.8 | 3.6 | 25 | 12.6 | 3.2 | 53 | 6.8 |
| Dizziness | 37 | 6.3 | 4.7 | 11 | 5.6 | 1.4 | 48 | 6.1 |
| Tingling | 36 | 6.1 | 4.6 | 11 | 5.6 | 1.4 | 47 | 6.0 |
| Joint pain | 37 | 6.3 | 4.7 | 9 | 4.6 | 1.1 | 46 | 5.8 |
| Unusual fatigue | 30 | 5.1 | 3.8 | 13 | 6.6 | 1.7 | 43 | 5.5 |
| Loss of strength | 29 | 5.0 | 3.7 | 14 | 7.1 | 1.8 | 43 | 5.5 |
| Muscle pain | 33 | 5.6 | 4.3 | 8 | 4.0 | 1.0 | 42 | 5.3 |
| Shortness of breath | 27 | 4.6 | 3.4 | 14 | 7.1 | 1.8 | 41 | 5.2 |
| Numbness | 29 | 4.9 | 3.7 | 9 | 4.6 | 1.1 | 38 | 4.8 |
| Stomach pain | 23 | 3.9 | 2.9 | 12 | 6.1 | 1.5 | 35 | 4.4 |
| Chest pain | 23 | 3.9 | 2.9 | 10 | 5.0 | 1.3 | 33 | 4.2 |
| Decreased/absent sensation | 25 | 4.3 | 3.2 | 7 | 3.6 | 0.9 | 32 | 4.1 |
| Breathing disorders | 19 | 3.2 | 2.4 | 12 | 6.1 | 1.5 | 31 | 3.9 |
| Nausea/vomiting | 19 | 3.2 | 2.4 | 10 | 5.0 | 1.3 | 29 | 3.7 |
| Thoracic oppression | 16 | 2.7 | 2.0 | 13 | 6.6 | 1.6 | 29 | 3.7 |
| Visual disturbances | 18 | 3.1 | 2.3 | 10 | 5.0 | 1.3 | 28 | 3.6 |
| Itchy skin | 21 | 3.6 | 2.7 | 7 | 3.6 | 0.9 | 28 | 3.6 |
| Coughing up blood | 16 | 2.7 | 2.0 | 8 | 4.0 | 1.0 | 24 | 3.0 |
| Balance disorders | 17 | 2.9 | 2.2 | 5 | 2.5 | 0.6 | 22 | 2.8 |
| Eye pain | 9 | 1.5 | 1.2 | 8 | 4.0 | 1.0 | 17 | 2.2 |
| Back pain | 11 | 1.9 | 1.4 | 6 | 3.0 | 0.8 | 17 | 2.2 |
| Confusion/unusual behaviour | 7 | 1.2 | 0.9 | 2 | 1.0 | 0.3 | 9 | 1.2 |
| Language disorders | 5 | 0.8 | 0.6 | 2 | 1.0 | 0.3 | 7 | 0.9 |
| Urinary disorders | 2 | 0.3 | 0.3 | 2 | 1.0 | 0.3 | 4 | 0.6 |
The proportion of women who declared no dive-related symptoms was significantly lower than in men (χ² = 11.29, df = 1, P < 0.001). A significant relationship between self-declared symptoms and age (χ² = 36.28, df = 5, P = 0.001) was also found; the older the diver the lower the ratio of respondents declaring a probable DI, based on symptoms. This ratio was independent of both dive experience (χ² = 11.78, df = 7, P = 0.108) and certification level (χ² = 6.03, df = 5, P = 0.303). The presence of symptoms after a dive and therefore, the probable occurrence of a dive injury, was independent of the time spent in physical activity (χ² = 3.04, df = 3, P = 0.385) or the dive location (χ² = 4.03, df = 4, P = 0.401). Finally, the relationship of symptoms to the seasonal rhythm of diving did not quite reach statistical significance (χ² = 9.38, df = 2, P = 0.009).
Injured respondents (n = 513) engaged in various types of diving (Table 3) depending on the purpose. Most DI were related to recreational diving (30% training and 59% exploration dives) while technical diving (rebreather, cave or deep trimix diving) accounted for 6%. No difference was observed between men and women in total dive time (45 ± 27 vs. 41 ± 18 minutes, paired t-test, P = 0.07, df = 511). However, male divers made significantly deeper dives than females (32 ± 17 vs. 25 ± 12 metres, paired t-test, P < 0.0001, df = 511). Most of the reported dives were decompression dives. It is noteworthy that 2% of the injured divers did not use any decompression tool, either because it was a no-decompression dive or because they completed the decompression required by following their dive buddy or instructor.
Table 3. Dive parameters for injured divers (n = 513). Missing values in the table refer to missing data from the respondents. (* P < 0.0001, men vs. women, paired t-test, df = 511) .
| Male | Female | Total | |||||||
| (n = 364) | (n = 149) | (n = 513) | |||||||
| n | % | % of total | n | % | % of total | n | % | ||
| Type of dive | |||||||||
| Single | 218 | 59.9 | 42.5 | 90 | 60.4 | 17.5 | 308 | 60.0 | |
| Interrupted | 2 | 0.5 | 0.4 | 0 | 0 | 0.0 | 2 | 0.4 | |
| Repetitive | 98 | 27.0 | 19.1 | 35 | 23.5 | 6.9 | 133 | 26.0 | |
| ≥ 3rd dive/day | 36 | 9.9 | 7.0 | 17 | 11.4 | 3.3 | 53 | 10.3 | |
| Missing | 10 | 2.7 | 1.9 | 7 | 4.7 | 1.4 | 17 | 3.3 | |
| Purpose | |||||||||
| Introductory | 4 | 1.1 | 0.8 | 3 | 2.0 | 0.6 | 7 | 1.4 | |
| Exploration | 210 | 57.7 | 40.1 | 91 | 61.1 | 18.6 | 301 | 58.7 | |
| Training | 112 | 30.8 | 21.8 | 40 | 26.8 | 8.4 | 152 | 29.6 | |
| Technical | 27 | 7.4 | 5.2 | 6 | 4.0 | 1.2 | 33 | 6.4 | |
| Missing | 11 | 3.0 | 2.1 | 9 | 6.1 | 1.8 | 20 | 3.9 | |
| Decompression | |||||||||
| Dive computer | 320 | 87.9 | 62.4 | 135 | 90.6 | 26.3 | 455 | 88.7 | |
| Dive table | 26 | 7.2 | 5.1 | 8 | 5.4 | 1.6 | 34 | 6.7 | |
| None | 8 | 2.2 | 1.6 | 3 | 2.0 | 0.5 | 11 | 2.1 | |
| Missing | 10 | 2.7 | 2.0 | 3 | 2.0 | 0.5 | 13 | 2.5 | |
| Diving depth (msw [mean ± SD])* | 32.1 ± 16.6 | 25.0 ± 11.6 | 30.2 ± 15.8 | ||||||
| Total dive time (min [mean ± SD]) | 45 ± 27 | 41 ± 18 | 44 ± 25 | ||||||
ANALYSIS OF DCI CASES
After contextual analysis, 114 datasets of DCI injuries (from the initial 799 questionnaires) were available for a complete analysis, including a severity score calculation,[ 22] first aid, HBOT and outcome.
First aid
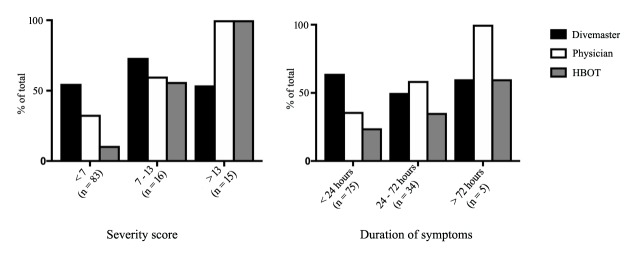
As described in Table 4, 70% of divers were symptomatic within 30 minutes. The ranking dive leader was the primary care provider in 58% of cases. Thereafter, 59% of these divers received care from a physician. In these cases, referral to the physician depended on the severity score (< 7: 47%; 7–13: 82%; > 13: 100%; χ² = 10.23, df = 2, P = 0.004). In only 10% of cases did divers seek help directly from a physician. The severity of the symptoms (χ² = 23.34, df = 2, P < 0.0001) as well as their duration (χ² = 9.97, df = 2, P = 0.007) were the primary triggers for seeking help directly from a physician, while severity had no influence on the activation of the ranking dive leader (χ² = 0.36, df = 2, P = 0.43) (Figure 1). Surprisingly, 32% of the injured divers did not activate an emergency response and none of these were treated. Again, low severity seemed to be the primary factor for not seeking help (severity score < 7: 36%; 7–13: 27%; > 13: 0%; χ² = 8.45, df = 2, P = 0.014).
Table 4. Diver responses to DCI-like symptoms according to onset, severity score and duration of symptoms (n = 114) (DM = Divemaster) .
| Onset | Severity score | Duration of symptoms | Men | Women | Total | |||||||
| (n = 73) | (n = 41) | (n = 114) | ||||||||||
| n | DM | Medic | n | DM | Medic | n | DM | Medic | HBO | |||
| In water | ||||||||||||
| <7 | ||||||||||||
| <24h | 7 | 4 | 0 | 8 | 0 | 3 | 15 | 7 | 3 | 0 | ||
| 24–72h | 6 | 5 | 1 | 4 | 1 | 3 | 10 | 6 | 4 | 2 | ||
| 7–13 | <24h | 3 | 1 | 1 | - | - | - | 3 | 1 | 1 | 1 | |
| >13 | <24h | 2 | 2 | 2 | 1 | 1 | 1 | 3 | 3 | 3 | 3 | |
| 24–72h | 1 | 1 | 1 | 2 | 1 | 2 | 3 | 2 | 3 | 3 | ||
| <5 min | ||||||||||||
| <7 | ||||||||||||
| <24h | 13 | 9 | 3 | 4 | 2 | 0 | 17 | 11 | 3 | 1 | ||
| 24–72h | 6 | 4 | 2 | 2 | 1 | 2 | 8 | 6 | 2 | 1 | ||
| >72h | 4 | 3 | 4 | 1 | 0 | 1 | 5 | 3 | 5 | 3 | ||
| 7–13 | <24h | 1 | 1 | 0 | - | - | - | 1 | 1 | 0 | 0 | |
| >13 | <24h | 1 | 1 | 1 | - | - | - | 1 | 1 | 1 | 1 | |
| 5–10 min | ||||||||||||
| <7 | ||||||||||||
| <24h | 2 | 1 | 0 | 1 | 0 | 0 | 3 | 1 | 0 | 0 | ||
| 24–72h | 1 | 0 | 1 | - | - | - | 1 | 0 | 1 | 1 | ||
| >13 | <24h | 1 | 1 | 1 | - | - | - | 1 | 1 | 1 | 1 | |
| 11–30 min | ||||||||||||
| <7 | <24h | 2 | 2 | 0 | 2 | 2 | 0 | 4 | 4 | 0 | 0 | |
| 24–72h | 1 | 1 | 0 | 1 | 1 | 1 | 2 | 2 | 1 | 0 | ||
| 7–13 | <24h | - | - | - | 2 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 24–72h | 1 | 1 | 1 | - | - | - | 1 | 1 | 1 | 1 | ||
| 31–60 min | ||||||||||||
| <7 | <24h | 3 | 3 | 0 | 1 | 1 | 0 | 4 | 4 | 0 | 0 | |
| 24–72h | 1 | 0 | 1 | - | - | - | 1 | 0 | 1 | 1 | ||
| 7–13 | <24h | 2 | 2 | 2 | - | - | - | 2 | 2 | 2 | 2 | |
| >13 | ||||||||||||
| <24h | 1 | 1 | 1 | - | - | - | 1 | 1 | 1 | 1 | ||
| 24–72h | 1 | 0 | 1 | - | - | - | 1 | 0 | 1 | 1 | ||
| 1–3 h | ||||||||||||
| <7 | ||||||||||||
| <24h | 2 | 1 | 1 | 4 | 0 | 2 | 6 | 1 | 3 | 0 | ||
| 24–72h | 1 | 0 | 1 | 3 | 1 | 2 | 4 | 1 | 3 | 1 | ||
| 7–13 | <24h | 3 | 2 | 1 | 2 | 2 | 2 | 5 | 4 | 3 | 2 | |
| >13 | <24h | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 2 | |
| 3– >24 h | <7 | |||||||||||
| <24h | 2 | 0 | 1 | - | - | - | 2 | 0 | 1 | 0 | ||
| 24–72h | 1 | 0 | 1 | - | - | - | 1 | 0 | 1 | 0 | ||
| 7–13 | <24h | - | - | - | 1 | 0 | 0 | 1 | 0 | 0 | 0 | |
| >13 | ||||||||||||
| <24h | 2 | 0 | 2 | - | - | - | 2 | 0 | 2 | 2 | ||
| 24–72h | 1 | 0 | 1 | 1 | 0 | 1 | 2 | 0 | 2 | 2 | ||
Figure 1.
Activating triggers among injured divers (n = 114) for seeking help and determining hyperbaric oxygen treatment (HBOT)
Amongst the 66 divers who informed the ranking dive leader of symptoms, 86% received oxygen at a minimal rate of 15 L∙min-1 and fluids were given in 65%. Despite it being a recommended procedure in France, unlike most other places, only 29% of injured divers recalled receiving oral acetylsalicylic acid.
Treatment and outcome for DCI cases
The decision to administer HBOT was made according to the severity score (< 7 32%; ≥ 7 100%; χ² = 25.66, df = 2, P < 0.0001), not based on the presence of continuing symptoms (< 24 hours 64%; ≥ 24 hours 60%; χ² = 0.10, df = 2, P = 0.949). However, the chosen protocol was not related to severity and included short 284 kPa treatment tables (14%; US Navy Treatment Table 5 or Comex 18C), long 284 kPa tables (64%; USN TT6 or Comex 18L) and a 405 kPa table (Comex 30). Complete resolution was reported by 84 (74%) divers, mild residual symptoms such as mild paresthesia, weakness, residual pain or some impairment of daily activities by 22 (19%). Eight (7%) divers self-declared severe residual symptoms, such as difficulty walking, paralysis, uncompensated vertigo or speech disorders. The final outcome was related to the initial severity score (χ² = 58.58, df = 4, P < 0.0001) and also to symptom duration (χ² = 27.28, df = 4, P < 0.0001), which did not appear to be a treatment choice criterion. Three out 31 divers who did not seek help reported having some residual symptoms.
Discussion
The characteristics of the general French diving population have been previously estimated by two French marketing studies, one conducted on behalf of the French diving organizations[ 23] and one conducted by the French government.[ 24] According to those studies, the average diver is a man aged 38 ± 10 (mean +/- SD) years (median 37, IQR 32–47), with a low certification level and for whom scuba diving is an occasional activity (8 ± 6 dives per year; median 12.5, IQR 5–16), despite an activity span of 7.1 ± 4.4 years (median 6.5, IQR 5.5–11.5). Women account for 32% of the total population and 25% of dive leaders and instructors. As far as sex, age and occupational categories are concerned, our sample is consistent with these general diving population characteristics. However, it differs markedly in its certification breakdown and diving activity, with high-level certification (82%) over-represented compared to the general diving population, as only one-third of the latter has a certification level higher than EN 14153-2/ ISO 24801-2 'autonomous diver'. This would also explain the reported greater diving activity. Therefore, these observations cannot evaluate the effect of relative inexperience on the occurrence of DI-related symptoms.
This is especially true for ear barotrauma, which is known to be associated with less experienced and intermediate divers.[ 25] Nonetheless, barotrauma accounted for the vast majority of the recorded DI in our study. It is likely that this is partly explained by the questionnaire design, which was meant to explore the whole diving career of respondents to mitigate this particular risk of bias. It could also be considered that the survey methods helped to reach those who dive more actively and so more frequently expose themselves to a possible DI. Therefore, the results give a fair picture of probable DI among more experienced French recreational divers.
Several factors, such as age, sex and lack of continuity of diving influenced the self-reporting of DI symptoms. For instance, women declare more DI symptoms than men, either because they are more willing to report a DI or owing to physiological differences, either genetic or hormonal. This relationship has been mostly studied in relation to DCI, with contradictory results. Although a lower risk has been reported in female professional divers owing to more conservative dive conditions,[ 26] other studies have reported an increased risk of DCI in women.[ 27] When it comes to the global risk of DI (not limited to DCI), to the best of our knowledge, only one study has assessed the influence of sex and several other factors.[ 5] Consistent with this previous survey, our data support the hypothesis that women could be more susceptible to DI than men. However, the possible reasons for this are unknown.
Age is a well-documented risk factor both for diving fatalities[ 28] and DCI.[ 27] However, our results indicate that when considering all types of DI, self-reporting of dive-related symptoms tended to decrease with increasing age. The absence of a relationship with diving experience or certification level suggests that age is paramount in this relationship. No definitive explanation is possible for such a counter-intuitive relationship, but this may be related to either a selection effect or, since it is a self-reported survey, a psychological difference in the perception of symptom severity. Indeed, divers who experience repeated symptoms, even minor, or comorbidities ('healthy diver' effect) might not continue to dive. As a result, the proportion of divers who never experienced injury increases with age. Alternatively, older divers might not declare symptoms considered as ‘normal’ or not sufficiently important to note. In the latter case, the question arises as to whether a diver’s training should include teaching on the potential impact of ‘minor’ injuries on long-term health issues.[ 29]
Although physical fitness and exercise are known to exert a protective effect for DCI,[ 30] this was not supported in this survey. One explanation could be that the beneficial effect of physical fitness may only be related to DCI but not to other DI, mainly barotrauma. Less than a third of divers who reported DCI-like symptoms reported neurological signs, a proportion less than in previous studies.[ 31 , 32] This discrepancy probably relates to a reporting bias, respondents only reporting what they remember retrospectively rather than being tested formally. Alternatively, this difference might also come from the absence of the less severe cases of DCI in these previous studies, as suggested by the number of divers in our survey who declared DCI-related symptoms but did not seek care from a physician.
After context analysis, the most common self-reported injuries were barotraumas (n = 320, 62% of injured divers), consistent with previous data.[ 5] This poses questions regarding prevention and overall knowledge of this particular issue. Barotrauma, except for pulmonary[ 33] and inner ear barotrauma,[ 34] are largely ignored by the scientific community. For instance, a recent review could only identify 44 relevant papers that constituted primary literature related to otology and scuba diving.[ 35]
Reduction of sequelae after DCI is based on early recognition of symptoms and signs, the initiation on site of first aid and swift evacuation to a hyperbaric chamber. Nonetheless, several studies have demonstrated that on-site first aid was often inadequate, with only 17 to 59% of injured divers receiving oxygen or fluids at some stage prior to recompression.[ 18 , 31 , 36] This survey is consistent with these observations. Permanent complete relief or improvement was reported in 59% of all treated cases, which is consistent with previous reports (65%[ 19] and 57%[ 18]). This raises questions about appropriate education on accident management, a concept commonly misunderstood and which is different from treatment.[ 12] Since the majority of the injured divers (70%) were symptomatic within 30 minutes of surfacing, consistent with the existing literature,[ 37] it also raises the question of how divers react to diving incidents. Injury severity did not appear to be a factor in reporting events to dive leaders, but it was a factor in medical referrals. Indeed, there is a high proportion of divers who fail to identify DCI owing to many factors (non-specific presentation, hope that symptoms will settle spontaneously, denial, underestimation of the potential consequences of untreated DCI,[ 31] unwillingness of fellow divers to acknowledge the evidence[ 15] and poor education on the diversity of symptomatology of DCI). These behaviours potentially may explain the large proportion of injured divers (32%, including those with DCI-like symptoms) who never sought help. Therefore, more emphasis should be given in divers' training to the varied, atypical symptomatology and unpredictable evolution of DCI, making pre-hospital diagnosis difficult. This is paramount since one out of 10 divers with DCI symptoms, who never sought treatment, reported some residual symptoms.
In France, transfer to a referral centre is required by law, and is under the responsibility of the CROSS (Search and Rescue Regional Centre).[ 38] It can be seen from this survey that the ranking dive leader often acts as a filter for referral to medical care. This indicates a need for better education of dive centres, instructors, boat skippers and deck hands in diving incident management. Fortunately, all but a few of the divers who did not receive oxygen or were not referred for medical assessment had complete resolution.
The decision to use HBOT seemed to be based solely on the severity score of the presenting symptoms and signs but this needs to be interpreted with caution since it is based only on patient self-reporting and not on the medical records. Since the time beyond which hyperbaric treatment is not effective has yet to be determined, this is of importance for triage by telemedicine where consultation with a diving medical officer who is not present at the accident site is organized by telephone or some other means.[ 39]
LIMITATIONS
Firstly, like all surveys, our results depend on self-reported data. Self-reported surveys introduce recall bias and there is a chance of over- or under-reporting of the frequency and/or severity of symptoms. This could be intentional or owing to missed or incorrectly assessed symptoms. Secondly, owing to the nature of the distribution of this survey, the response rate is unknown, resulting in a non-responder bias. Thirdly, the ability to generalize the findings to the general French diving population is limited because of the high responder rate amongst highly qualified and experienced divers.
Conclusions
This online survey provides insights into diving injuries amongst experienced French recreational divers, based on retrospective self-reporting of symptoms on an electronic questionnaire. The most frequently reported symptoms suggest the mild nature of most injuries, with ear barotrauma seeming to be the most frequent. The survey provided evidence of the influence of female sex, younger age and lack of continuity of diving as potential risk factors for injury. The data question divers’ knowledge about dive-related risks and showed the need for better information and education for recreational divers.
Table 5. Final outcome and applied treatment among DCI cases (n = 114); mild residual symptoms are mild paresthesia, weakness, residual pain or some impairment of daily activities. Severe residual symptoms are difficulty walking, paralysis, uncompensated vertigo, or speech disorders; 14 divers (13 with a severity score < 7, 1 between 7–13) had a spontaneous recovery with full resolution without any treatment, although they activated the emergency response system .
| Severity score | After first HBOT | Final outcome | |||||
| Complete resolution | Mild residual | Severe residual | Complete resolution | Mild residual | Severe residual | ||
| Received first-aid and HBOT | |||||||
| <7 (n = 9) | 8 | 1 | 0 | 8 | 1 | 0 | |
| 7-13 (n = 8) | 2 | 4 | 2 | 4 | 2 | 2 | |
| >13 (n = 16) | 2 | 6 | 8 | 1 | 9 | 6 | |
| (n = 16) | 12 | 11 | 10 | 13 | 12 | 8 | |
| Received first-aid | |||||||
| <7 (n = 31) | - | - | - | 25 | 6 | 0 | |
| 7-13 (n = 2) | - | - | - | 1 | 1 | 0 | |
| Not seeking help | |||||||
| <7 (n = 30) | - | - | - | 29 | 1 | 0 | |
| 7-13 (n = 4) | - | - | - | 2 | 2 | 0 | |
| Total | 84 (74%) | 22 (19%) | 8 (7%) | ||||
Footnotes
Acknowledgements
We wish to thank the diving organizations’ national representatives who spread the questionnaire through their networks.
Conflict of interest and funding: nil
Contributor Information
David Monnot, EA4324 ORPHY, Institut Brestois Santé Agro Matière, Université de Bretagne Occidentale, Brest, France.
Thierry Michot, EA3149 LABERS, Institut Brestois des Sciences de l’Homme et de la Société, Université de Bretagne Occidentale, Brest.
Emmanuel Dugrenot, EA4324 ORPHY, Institut Brestois Santé Agro Matière, Université de Bretagne Occidentale, Brest, France.
François Guerrero, EA4324 ORPHY, Institut Brestois Santé Agro Matière, Université de Bretagne Occidentale, Brest, France.
Pierre Lafère, EA4324 ORPHY, Institut Brestois Santé Agro Matière, Université de Bretagne Occidentale, Brest, France.
References
- Henckes A. Enquête nationale accidents de plongée autonome sportive, bilan 2013 [Internet] FFESSM; 2014. [cited 2018 July 13] Available from: http://medical.ffessm.fr/wp-content/uploads/Bilan-ADP-2013.pdf. [Google Scholar]
- Denoble PJ, Pollock NW, Vaithiyanathan P, Caruso JL, Dovenbarger JA, Vann RD, et al. Scuba injury death rate among insured DAN members . Diving Hyperb Med. 2008;38:182–8. [PubMed] [Google Scholar]
- Van Hulst RA. Analysis of ten year diving casualties 1979–1989, diving medical centre. The Netherlands . Undersea Biomed Res. 1990;17:144. [Google Scholar]
- Vinkel J, Bak P, Hyldegaard O. Danish diving-related fatalities 1999–2012. Diving Hyperb Med. 2016;46:142–9. [PubMed] [Google Scholar]
- Ranapurwala SI, Bird N, Vaithiyanathan P, Denoble PJ. Scuba diving injuries among Divers Alert Network members 2010-2011. Diving Hyperb Med. 2014;44:79–85. [PubMed] [Google Scholar]
- Hyun GS, Jee YS, Park JM, Cho NH, Cha JY. Injury survey in scuba divers of British Sub-Aqua Club: A retrospective study. J Exerc Rehabil. 2015;11:331–6. doi: 10.12965/jer.150252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevett AJ, Forbes R, Rae CK, Sheehan C, Ross J, Watt SJ, Stephenson R. Diving accidents in sports divers in Orkney waters. Scott Med J. 2001;46:176–7. doi: 10.1177/003693300104600608. [DOI] [PubMed] [Google Scholar]
- Arness MK. Scuba decompression illness and diving fatalities in an overseas military community . Aviat Space Environ Med. 1997;68:325–3. [PubMed] [Google Scholar]
- Dardeau MR, Pollock NW, McDonald CM, Lang MA. The incidence of decompression illness in 10 years of scientific diving . Diving Hyperb Med. 2012;42:195–200. [PubMed] [Google Scholar]
- Gempp E, Louge P, Blatteau JE, Hugon M. Descriptive epidemiology of 153 diving injuries with rebreathers among French military divers from 1979 to 2009 . Mil Med. 2011;176:446–50. doi: 10.7205/milmed-d-10-00420. [DOI] [PubMed] [Google Scholar]
- Taylor DM, O’Toole KS, Ryan CM. Experienced scuba divers in Australia and the United States suffer considerable injury and morbidity . Wilderness Environ Med. 2003;14:83–8. doi: 10.1580/1080-6032(2003)014[0083:esdiaa]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Taher A. Diving accident management, with special emphasis on the situation in the Red Sea . Wien Med Wochenschr. 1999;151:134–7. [PubMed] [Google Scholar]
- Hubbard M, Davis FM, Malcolm K, Mitchell SJ. Decompression illness and other injuries in a recreational dive charter operation . Diving Hyperb Med. 2018;48:218–23. doi: 10.28920/dhm48.4.218-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevett AJ, Forbes RF, Rae CK, Sheehan C. Reducing delays in treatment − how sports divers in Orkney respond to accidents. 2002. Available from: http://archive.rubicon-foundation.org/7262 [cited 2018 July 13].
- Grandjean B. Peut-on améliorer le délai de traitement hospitalier des accidents de plongée sous-marine autonome de loisir?. Table ronde de médecine de plongée de l’Océan Indien. October 10-11, 2001; Mauritius. [Google Scholar]
- Moon RE. Adjunctive therapy for decompression illness: a review and update . Diving Hyperb Med. 2009;39:81–7. [PubMed] [Google Scholar]
- Lillo RS, Parker EC. Evaluation of oxygen and pressure in treatment of decompression sickness in guinea pigs . Undersea Hyperb Med. 1998;25:51–7. [PubMed] [Google Scholar]
- Lippmann J. First aid oxygen administration for divers . SPUMS J. 2003;33:192–8. [Google Scholar]
- Longphre JM, Denoble PJ, Moon RE, Vann RD, Freiberger JJ. First aid normobaric oxygen for the treatment of recreational diving injuries . Undersea Hyperb Med. 2007;34:43–9. [PubMed] [Google Scholar]
- European Parliament . Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation). Off J Eur Union; 2016; 59: 89- 131. [Google Scholar]
- Ozyigit T, Egi SM, Denoble P, Balestra C, Aydin S, Vann R, Marroni A. Decompression illness medically reported by hyperbaric treatment facilities: cluster analysis of 1929 cases . Aviat Space Environ Med. 2010;81:3–7. doi: 10.3357/asem.2495.2010. [DOI] [PubMed] [Google Scholar]
- Boussuges A, Thirion X, Blanc P, Molenat F, Sainty JM. Neurologic decompression illness: a gravity score . Undersea Hyperb Med. 1996;23:151–5. [PubMed] [Google Scholar]
- Chauveau M. Etude socio-économique relative à la plongée subaquatique de loisir en 2004–2005 Section Permanente du Comité Consultatif de l’Enseignement de la Plongée Subaquatique; 2005. Available from: https://ffessm.fr/ckfinder/userfiles/files/Etude_Eco_plongee.pdf [cited 2018 July 13]. [Google Scholar]
- Muller L. La pratique sportive en France, reflet du milieu social . Insee. 2006 (Fre). [Google Scholar]
- Jansen S, Meyer MF, Boor M, Volland R, Pracht ED, Klünter ED, et al. Repetitive freshwater diving: risk factors and prevalence of barotrauma . Undersea Hyperb Med. 2017;44:407–14. [PubMed] [Google Scholar]
- Irgens Å, Troland K, Grønning M. Female professional divers. Similarities and differences between male and female professional divers . Int Marit Health. 2017;68:60–7. doi: 10.5603/IMH.2017.0010. [DOI] [PubMed] [Google Scholar]
- Cialoni D, Pieri M, Balestra C, Marroni A. Dive risk factors, gas bubble formation, and decompression illness in recreational SCUBA diving: Analysis of DAN Europe DSL Data Base . Front Psychol. 2017; 8: 1587. 10.3389/fpsyg.2017.01587. [cited 2018 Jul 11] Available from: http://journal.frontiersin.org/article/10.3389/fpsyg.2017.01587/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denoble PJ, Pollock NW, Vaithiyanathan P, Caruso JL, Dovenbarger JA, Vann RD. Scuba injury death rate among insured DAN members . Diving Hyperb Med. 2008;38:182–8. [PubMed] [Google Scholar]
- Hemelryck W, Germonpré P, Papadopoulou V, Rozloznik M, Balestra C. Long term effects of recreational SCUBA diving on higher cognitive function: cognitive functions in SCUBA divers . Scand J Med Sci Sports. 2014;24:928–34. doi: 10.1111/sms.12100. [DOI] [PubMed] [Google Scholar]
- Carturan D, Boussuges A, Vanuxem P, Bar-Hen A, Burnet H, Gardette B. Ascent rate, age, maximal oxygen uptake, adiposity, and circulating venous bubbles after diving . J Appl Physiol. 2002;93:1349–56. doi: 10.1152/japplphysiol.00723.1999. [DOI] [PubMed] [Google Scholar]
- Bessereau J, Genotelle N, Brun PM, Aboab J, Antona M, Chenaitia H, et al. Decompression sickness in urban divers in France . Int Marit Health. 2012;63:170–3. [PubMed] [Google Scholar]
- Hart AJ, White SA, Conboy PJ, Bodiwala G, Quinton D. Open water scuba diving accidents at Leicester: five years’ experience . J Accid Emerg Med. 1999;16:198–200. doi: 10.1136/emj.16.3.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafère P, Germonpré P, Balestra C. Pulmonary barotrauma in divers during emergency free ascent training: review of 124 cases . Aviat Space Environ Med. 2009;80:371–5. doi: 10.1001/jamaoto.2017.2617. [DOI] [PubMed] [Google Scholar]
- Lechner M, Sutton L, Fishman JM, Kaylie DM, Moon RE, Masterson L, et al. Otorhinolaryngology and diving - Part 1: Otorhinolaryngological hazards related to compressed gas scuba diving: A review . JAMA Otolaryngol Head Neck Surg. 2018;144:252–8. doi: 10.1001/jamaoto.2017.2617. [DOI] [PubMed] [Google Scholar]
- Livingstone DM, Smith KA, Lange B. Scuba diving and otology: a systematic review with recommendations on diagnosis, treatment and post-operative care . Diving Hyperb Med. 2017;47:97–109. doi: 10.28920/dhm47.2.97-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinnick MA. Recognition of scuba diving accidents and the importance of oxygen first aid . J Emerg Nurs. 1994;20:105–10. [PubMed] [Google Scholar]
- Hadanny A, Fishlev G, Bechor Y, Bergan J, Friedman M, Maliar A, et al. Delayed recompression for decompression sickness: retrospective analysis . PLoS ONE. 2015;10(4):e0124919. doi: 10.1371/journal.pone.0124919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulange M, Hugon M, Blatteau JE. Prise en charge préhospitalière des accidents de plongée: de l’alerte à l’admission . In: Broussolle B, Méliet JL, Coulange M, editors. Physiol Médecine Plong. Paris: Ellipses; 2006; 417- 24. p. [Google Scholar]
- Mitchell SJ, Bennett MH, Bryson P, Butler FK, Doolette DJ, Holm JR, et al. Consensus guideline: Pre-hospital management of decompression illness: expert review of key principles and controversies . Diving Hyperb Med. 2018;48:45–55. doi: 10.28920/dhm48.1.10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]