Abstract
Physical inactivity is highly prevalent in Latinos. Use of smartphone technology may improve physical activity (PA) among Latino adults. We sought to determine the efficacy of a multi-component intervention to promote PA among Latino adults. We conducted a 3-month, 2-arm randomized trial among Latino adults with one or more risk factors for cardiovascular disease (CVD). We adapted a scripted, counseling approach into text messages and combined this intervention with brief motivational interviewing delivered by telephone. We compared this intervention to a control group. Both groups received a handout on the benefits of PA. During the baseline visit, participants completed a validated medical history survey as well as an assessment of quality of life and exercise behaviors. The primary outcome was change at three months in mean steps per week. We enrolled 69 patients, 35 in the intervention arm and 34 in the control arm. The mean age of the cohort was 58.7 years (SD 6.82). At baseline, mean steps per week were 65,218.2 (SD 25420.8) for intervention participants compared to 71,581.26 (SD 26118.07) for control participants, P = 0.36. At 3 months, the change in mean steps per week was 31,184.6 (SD 26121.52) for participants randomized to the intervention compared to 15,370.9 (SD 22247.84) for those randomized to control, P = 0.045. Among Latino adults with one or more risk factors for CVD, there was an increase in mean steps per week among those randomized to an intervention, involving the use of smartphones, versus control.
Clinical trial registration
Keywords: Latino adults, Atherosclerotic risk factors, Text messaging, Exercise behaviors
1. Introduction
>59 million Latinos live in the U.S. and 8% of U.S. adults age 65 years or older are Latino (https://www.acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/Statistical-Profile-Older-Hispanic-Ameri.pdf, n.d.). Of Latino adults 18–74 years of age, 80% of men and 71% of women have one or more risk factors for cardiovascular disease (CVD) (Daviglus et al., 2012). Common risk factors for CVD among Latinos are diabetes type 2 and hyperlipidemia (Daviglus et al., 2012). Physical inactivity is an additional risk factor for CVD and highly prevalent among Latinos. The age-adjusted proportion of Latinos who met the federal PA guidelines for aerobic activity in 2017 was 45.4% for Latinos and 59.2% for non-Hispanic white adults (NCHS NHIS, 2017). Use of text messages to promote PA can be an efficient and efficacious approach (Buchholz et al., 2013; Fanning et al., 2012). The percent of U.S. Latino adults who utilize text messages is 83% compared to 68% of non-Hispanic whites (Pew Internet, 2010). Within the state of Kansas, the utilization of text messages among Latino adults is >90% (Collins et al., 2014). Thus, the delivery of a behavior change intervention using text messaging is a viable option for Latino adults residing in Wichita, KS.
We completed a randomized controlled trial using a telephone-based, scripted counseling approach (i.e., Patient-centered Assessment and Counseling for Exercise [PACE] program (Patrick et al., 1994)) to promote walking in persons with both peripheral artery disease (PAD) and diabetes mellitus (N = 145, 90% white) (Collins et al., 2011). Our results show that PACE was effective at improving participants' walking speed. As a scripted counseling approach, nearly 100% of the recommendations from PACE can be delivered as text messages. However, PACE has minimal content for low motivated patients. Motivational interviewing (MI) is an excellent counseling approach to address both of these areas (Resnicow et al., 2008). We sought to determine the efficacy of a scripted counseling intervention, translated into text messages and combined with MI delivered via brief phone calls and a handout, hereafter referred to as the intervention, versus a handout alone (control) to increase PA at three months in Latino adults with one or more CVD risk factors.
2. Methods
We conducted a one-year, NIH funded, randomized, investigator-blinded clinical trial in a cohort of Latino adults at risk for CVD. The study was conducted in Wichita, KS, where Latino adults comprise 13% of the population. All study activities were performed by research staff from our institution housed on the Wichita campus.
Trained staff performed prescreening activities on potential participants, which included assessment of ethnicity, language preference, either English or Spanish, presence of one or more CVD risk factors, and readiness for exercise. Staff also screened participants for peripheral artery disease (PAD), which is atherosclerosis of the abdominal aorta and/or arteries of the lower extremities sufficient to cause blockage of arterial flow to lower limbs; these blockages often limit a patient's ability to engage in walking as a form of PA. We screened for PAD using the ankle-brachial index (ABI) – ratio of the systolic pressure in the ankles to that in the arms. Participants who screened positive for PAD warranted follow up with their primary physician prior to engaging in our study.
2.1. Participants
The Human Subjects Committee at University of Kansas School of Medicine-Wichita approved the study protocol. Inclusion criteria were Latino adults, English or Spanish speaking, age 70 years or older, or age 50 years with at least one of the following: diabetes mellitus, hypertension, hyperlipidemia, and/or current or past smoker. Participants were required to have 24-hour access to a smartphone and text messaging. We excluded persons with the following: pregnancy, currently participating in another study, currently walking for exercise at least 3 days per week, prior major amputation (foot or lower leg) or critical leg ischemia (tissue loss, gangrene, or ulcers), use of supplemental oxygen, myocardial infarction within the preceding 3 months; the rationale for this is participant safety.
2.2. Participant recruitment
Recruitment approaches included flyers and advertisement in a local newspaper with a readership that was largely Latino. We provided local clinics and physicians with study flyers to distribute to patients. We provided up to $85 for study participation which included $10 for an initial in-person screen, $25 following randomization, and $50 upon completion of the trial.
2.3. Randomization and study interventions
After participants provided informed consent, they were randomized to one of two study groups in a 1:1 fashion: control or intervention. All participants received standard educational print material on risk factor modification for CVD. This material was provided in English and Spanish (Stevens et al., 2006).
In addition to the handout, participants in the intervention group received daily text messaging (7th grade reading level), five days per week. The content of the text messaging was the use of language to encourage PA, with a focus on walking, which is a form of PA that can commonly be completed in the community without the need for special equipment or access to a gym. Messages were tailored to a participant's stage of readiness to exercise as per their PACE score. We developed up to 21 messages per PACE score which were categorized as precontemplation (score of 1), contemplation (score in the range of two to four), or action (score in the range of five to eight). Messages were developed in English and, with the use of certified translators, translated into Spanish. Participants in the intervention group also received a phone call for 20 min or less in duration every two weeks for one month followed by a phone call every four weeks for two months. The brief phone calls were used to deliver MI. MI is a directive, client-centered counseling approach to elicit behavior change by assisting clients in exploring and resolving ambivalence (Miller and Rollnick, 1991). Prior randomized trials have demonstrated MI's clinical efficacy for PA and medication adherence for chronic diseases (Burke et al., 2003; Dunn et al., 2001; Ogedegbe et al., 2007). Evidence suggests that MI is best suited for persons who exhibit lower intrinsic motivation and readiness for behavior change (Butler et al., 1999). MI offers the advantage of targeting unique issues that limit behavior change. Within the philosophy behind MI (Miller and Rollnick, 2002), client resistance is often a behavior evoked by environmental conditions. Counselors engage with the client in exploring resistance or ambivalence rather than combatting it. In our study, we used MI to focus on three areas: Exploring and dealing with resistance to engage in PA, guiding and helping participants identify reasons, needs, and desires to increase PA, and choosing a goal, setting an action plan, and arranging follow up. A bachelor's level research assistant trained in MI provided the intervention. A two-day training workshop was provided by Dr. Kenneth Resnicow, an internationally recognized expert in MI. Follow up quality assessments involved direct observation of a subset of participants and it was conducted by a licensed social worker who was also trained by Dr. Resnicow and who worked with TCC to provide MI for a larger NIH funded clinical trial. (R01HL098909).
2.4. Measures
2.4.1. Ankle-brachial index
The ankle-brachial index (ABI) was used to define the presence or absence of PAD. During this assessment, a participant rested for 5 min and a 5 MHz hand-held Doppler with an attached stethoscope was used to measure systolic blood pressures in both brachial arteries and in both ankles (i.e., the dorsalis pedis and posterior tibial arteries) (Collins et al., 2003).
2.5. Medical history
We used the Lifestyle and Clinical Survey (LCS) to obtain sociodemographic (e.g., age) and comorbidity data. The PI and colleagues originally developed the LCS to obtain pertinent past medical history including smoking status and sociodemographic information (Collins et al., 2005).
2.5.1. Stage of readiness to engage in exercise
The Patient-Centered Assessment and Counseling for Exercise (PACE) score was used to identify a participant's stage of readiness for exercise. To obtain a PACE score, a participant chose one of eight graded statements that best described his/her current level of and interest in PA. This score determines the “Stage of Change” that they are in (Prochaska & DiClemente, 1983) (Prochaska and DiClemente, 1983). We assessed a participant's PACE score at baseline and 6 weeks to tailor the text messaging to their stage of readiness to engage in exercise.
2.6. Outcomes
2.6.1. Primary outcome: mean steps walked per week
We assessed PA based on mean steps per week. To capture steps per week, we distributed pedometers (Striiv Band) (https://www.striiv.com/, n.d.). that included a smartphone based application (App). With guidance by a research team member, participants downloaded the App on their phone up to 2 weeks prior to the randomization visit. The App was used to help participants monitor their weekly steps. Mean weekly steps were obtained at baseline and at 3 months.
2.6.2. Secondary outcomes
2.6.2.1. Quality of life
Medical Outcomes Short Form Survey (SF-36). Health related quality of life was measured using the Medical Outcomes Study-Short Form Survey (SF-36) (Ware et al., 2000). Each subscale is scored from 0 to 100; higher scores indicate a more positive quality of life.
2.7. Exercise behaviors
Exercise Behaviors Questionnaire. We administered the Stanford Patient Education Research Center Exercise Behavior Survey at baseline and again at 3 months. The exercise behaviors survey is a 6-item instrument that includes questions regarding the type of activity and the length of time during which the participant engaged in that activity during the past week (Lorig et al., n.d.). There is a category for stretching or strengthening exercises (e.g., weights, range of motion) and a category for aerobic exercise (e.g., walking, swimming) and each category is scored based on minutes per week of a participant's engagement in a given category. The test-retest reliability is 0.56 and 0.72 for stretching/strengthening and aerobic exercises, respectively.
2.8. Exit survey
In order to understand participants' perception of the study, each participant was provided a survey at the end. We designed a 15-item survey that included 7 questions with categorical responses (e.g., yes/no or options for how a participant learned about the study) and 8 questions with responses ranging from 1 (low) to 10 (high) which assessed a participant's perceptions of the study overall and components, as applicable, which motivated their use of PA.
2.9. Sample size
A sample size of 64 patients (32 in each group) would provide 80% power, using a 0.025 two-sided level of significance, to detect a mean difference at three months of 1009.8 steps walked in seven days between the intervention group and the control group, using a two-group t-test. It is assumed that the standard deviation of the change in steps walked was 1957, which was observed in Hu, 2015 (Hu et al., 2015). The primary comparison was change in mean steps per week comparing the intervention and control groups. The 0.025 level of significance accounts for the comparison. Assuming an attrition rate of 20%, the plan was to recruit 80 participants to ensure that there were 64 patients at 3 months. However, our attrition was much lower at 1.4%. Thus, with a sample of 69, we accomplished our goal at 3 months for both arms, which increased the power to 85%.
2.10. Randomization
The sequence for randomization generation was accomplished with a computer program. Each randomization allocation was placed in a sealed envelope by the study statistician. The envelope remained sealed until a participant was assigned to one of two groups. The envelope was opened by a full-time research assistant in the presence of the participant after the participant completed all assessments by a part-time research assistant who remained blinded to each participant's group assignment.
2.11. Statistical methods
The primary and secondary outcomes, 3-month change in steps walked per week performance were analyzed across control and intervention groups. Two sample, two-sided t-tests were used to compare changes in outcomes between baseline and three-month follow-up between intervention and control groups. For the exploratory analyses, which were determined post hoc based on comparisons between the intervention and control groups for the primary outcome, we used a generalized linear model to compare mean steps between study groups by level of education and the primary language spoken at home. A P value <0.05 considered statistically significant for all analyses. The analyses were performed using SAS statistical software version 9.4.
3. Results
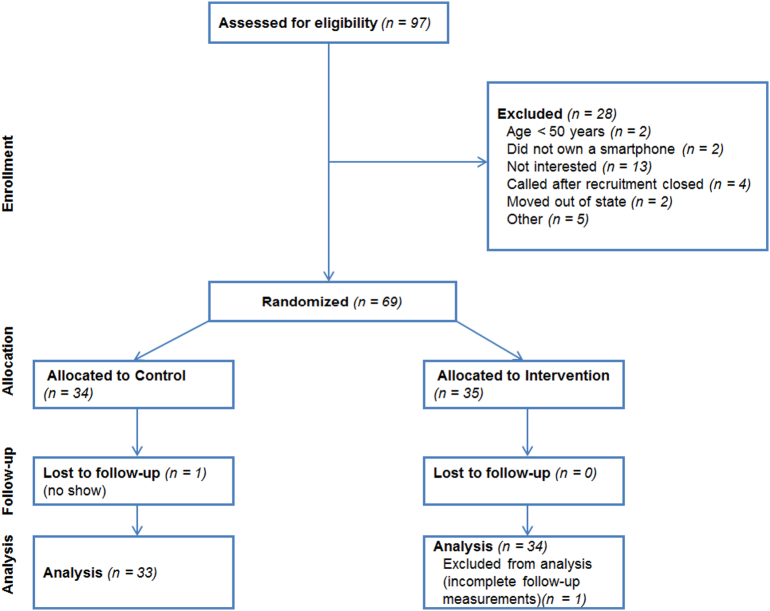
We randomized 69 Latino adults to one of two study protocols (35 to intervention, 34 to control). At 3 months, there were 34 participants in intervention and 34 in control. (Fig. 1).
Fig. 1.
Consort diagram.
Baseline characteristics of participants are shown in Table 1 and are reported for the overall cohort and by the originally assigned treatment group. For the overall cohort, the mean age was 58.7 years (SD 6.82). (Table 1) The prevalence of major CVD risk factors was hypertension 37.7%, diabetes mellitus 37.7%, and history of smoking at least 100 cigarettes during their lifetime 33.3%. Except for a slightly lower mean systolic blood pressure and a higher proportion of persons whose primary language was English, in the intervention versus control group, there were no differences between the three groups in baseline characteristics. At baseline, mean steps walked per week for the entire cohort was 68,353.6 (SD 25776.39) and, by group, mean steps walked per week were 65,218.2 (SD 25420.8) for the intervention and 71,581.26 (SD 26118.07) for control, P = 0.36. (SD).
Table 1.
Baseline characteristics of participants.
| Baseline measures | Overall | Intervention | Control | p-Valuea |
|---|---|---|---|---|
| N | 69 | 35 | 34 | |
| Age, mean (SD) | 58.7 (6.82) | 58.6 (6.40) | 58.73 (7.32) | 0.88 |
| Female (%) | 58 (85.5) | 30 (85.7) | 29 (85.3) | 0.97 |
| Education ≥ high school (%) | 58 (84.1) | 31 (88.6) | 27 (79.4) | 0.05 |
| Ethnicity | ||||
| Mexican/Mexican American/Chicano | 31 (44.9) | 16 (45.7) | 15 (44.1) | 0.86 |
| Other Spanish/Hispanic/Latino | 38 (55.1) | 19 (54.3) | 19 (55.9) | 1 |
| Language commonly spoken at home (%) | ||||
| English | 19 (27.5) | 14 (40.0) | 5 (14.7) | 0.038 |
| Spanish | 50 (72.5) | 21 (60.0) | 29 (85.3) | 0.26 |
| Income | 0.81 | |||
| Less than $5000 (%) | 2 (2.9) | 1 (2.9) | 1 (2.9) | |
| $5000–$30,000 (%) | 20 (29.0) | 9 (25.7) | 11 (32.4) | |
| $30,000–$50,000 (%) | 8 (11.6) | 4 (11.4) | 4 (11.8) | |
| $50,000–$100,000 (%) | 9 (13.0) | 6 (17.1) | 3 (8.8) | |
| >$100,000 (%) | 5 (7.3) | 4 (11.4) | 1 (2.9) | |
| Medical history | ||||
| Atrial fibrillation (%) | 5 (7.3) | 2 (5.71) | 3 (8.8) | 0.62 |
| High blood pressure or hypertension (%) | 26 (37.7) | 18 (51.4) | 8 (23.5) | 0.017 |
| High blood cholesterol (%) | 51 (73.9) | 24 (68.6) | 27 (79.4) | 0.31 |
| Congestive or chronic heart failure (%) | 1 (1.5) | – | 1 (2.9) | |
| Stroke (%) | 1 (1.5) | – | 1 (2.9) | |
| Mini stroke or TIA (%) | 1 (1.5) | 1 (2.9) | – | |
| Diabetes (%) | 26 (37.7) | 16 (45.7) | 10 (29.41) | 0.17 |
| Kidney, eye or circulation problems (%) | 1 (1.5) | 1 (2.9) | – | |
| Chronic bronchitis or emphysema (%) | 5 (7.3) | 2 (5.7) | 3 (8.8) | 0.62 |
| Asthma (%) | 5 (7.3) | 3 (8.6) | 2 (5.9) | 0.67 |
| Cancer (%) | 2 (2.9) | 1 (2.9) | 1 (2.9) | 0.98 |
| Ulcerative colitis or Crohn's disease (%) | 2 (2.9) | 2 (5.7) | – | |
| Kidney disease other than infection or a stone (%) | 1 (1.5) | 1 (2.9) | – | |
| Stomach or duodenal ulcer (%) | 5 (7.3) | 3 (8.6) | 2 (5.9) | 0.67 |
| Ulcerative colitis or Crohn's disease (%) | 2 (2.9) | 2 (5.7) | – | |
| Rheumatoid arthritis (%) | 13 (19.1) | 6 (17.1) | 7 (21.2) | 0.68 |
| Arthritis other than rheumatoid (%) | 7 (10.1) | 2 (5.7) | 5 (14.7) | 0.22 |
| Systemic lupus erythematosus (%) | 1 (1.5) | – | 1 (2.9) | |
| Osteoporosis (%) | 7 (10.1) | 5 (14.3) | 2 (5.9) | 0.25 |
| Current smoker (%) | 2 (2.9) | 2 (5.7) | – | 0.13 |
| Smoked at least 100 cigarettes during lifetime (%) | 23 (33.3) | 11 (31.4) | 12 (35.3) | 0.74 |
| 0–4 cigarettes per day (%) | 16 (69.6) | 6 (54.6) | 10 (83.3) | |
| 5–15 cigarettes per day (%) | 4 (17.4) | 3 (27.3) | 1 (8.3) | |
| One pack per day (%) | 3 (13.0) | 2 (18.2) | 1 (8.3) | |
| Drinking alcohol beverage (%) | 38 (55.1) | 21 (60.0) | 17 (50.0) | 0.41 |
| Weekly (%) | 3 (7.9) | 1 (4.8) | 2 (11.8) | |
| Occasionally (%) | 35 (92.1) | 20 (95.2) | 15 (88.2) | |
| Walking more than 10 mins without stopping | 0.80 | |||
| Rarely or never (%) | 33 (47.8) | 17 (48.6) | 16 (47.1) | |
| 1 time each week (%) | 17 (24.6) | 9 (25.7) | 8 (23.5) | |
| 2–3 times each week (%) | 19 (27.5) | 9 (25.7) | 10 (29.4) | |
| Activity level while working | 36 (52.2) | 18 (51.4) | 18 (52.9) | 0.13 |
| Light (%) | 11 (30.6) | 8 (44.4) | 3 (16.7) | |
| Moderate (%) | 23 (63.9) | 9 (50.0) | 14 (77.8) | |
| Strenuous (%) | 2 (5.6) | 1 (5.6) | 1 (5.6) | |
| Strenuous or very hard, mean (SD) | 0.44 | |||
| None (%) | 54 (78.3) | 27 (77.1) | 27 (79.4) | |
| 1 day per week (%) | 9 (13.0) | 4 (11.4) | 5(14.7) | |
| 2 days per week (%) | 4 (5.8) | 2 (5.7) | 2 (5.9) | |
| 3 days per week (%) | 2 (2.9) | 2 (5.7) | – | |
| Moderate exercise, mean (SD) | 0.40 | |||
| None (%) | 47 (68.1) | 23 (65.7) | 24 (70.6) | |
| 1 day per week (%) | 14 (20.3) | 7 (20.0) | 7 (20.6) | |
| 2 days per week (%) | 6 (8.7) | 3 (8.6) | 3 (8.8) | |
| 3 days per week (%) | 2 (2.9) | 2 (5.7) | – | |
| Light exercise, mean (SD) | 0.49 | |||
| None (%) | 64 (92.8) | 32 (91.4) | 32 (94.1) | |
| 1 day per week (%) | 4 (5.8) | 2 (5.7) | 2 (5.9) | |
| 2 days per week (%) | 1 (1.5) | 1 (2.9) | – | |
| ABI | ||||
| Estimate left ABI, mean (SD) | 1.13 (0.088) | 1.11 (0.083) | 1.15 (0.090) | 0.12 |
| Estimate right ABI, mean (SD) | 1.13 (0.084) | 1.12 (0.087) | 1.14 (0.081) | 0.48 |
p-Value indicates that the mean difference in baseline measures of participants between messaging and handout groups. Mann–Whitney U test was applied to variables with non-normal distribution.
For the primary outcome of change at three months in mean steps walked per week, the results were: 31184.6 (SD 26121.52) for the intervention group and 15,370.9 (SD 22247.84) for the control group, P = 0.045. (Table 2, Table 3) For each group, there was a statistically significant increase at three months for within group improvements in mean steps walked per week (intervention P < 0.0001 and control P ≤0.0001).
Table 2.
Study outcomes.
| Outcome measures, mean (SD) | Baseline | Three-months | Three-month changes | Within group p-valuea | Between groups p-valueb |
|---|---|---|---|---|---|
| Pace Scorec | |||||
| Intervention | 4.2 (1.3) | 6.71 (1.19) | 2.53 (1.31) | <0.0001 | |
| Control | – | – | – | ||
| Steps | |||||
| Intervention | 65,218.2 (25,420.80) | 97,240.4 (33,795.37) | 31,184.6 (26,121.52) | <0.0001 | 0.045⁎ |
| Control | 71,581.3 (26,118.07) | 87,640.6 (21,351.97) | 15,370.9 (22,247.84) | <0.0001 | – |
| Exercise Behavior | |||||
| Aero | |||||
| Intervention | 28.29 (37.06) | 232.06 (73.32) | 204.71 (81.15) | <0.0001 | 0.97 |
| Control | 29.56 (44.54) | 234.09 (75.28) | 204.09 (91.62) | <0.0001 | – |
| Strength | |||||
| Intervention | 15.86 (23.56) | 109.41 (70.99) | 93.53 (71.52) | <0.0001 | 0.37 |
| Control | 10.15 (13.17) | 116.82 (73.94) | 106.82 (74.03) | <0.0001 | – |
| SF-36d Scores | |||||
| Physical Functioning | |||||
| Intervention | 86.29 (14.77) | 95.59 (5.74) | 9.56 (13.16) | <0.0001 | 0.78 |
| Control | 85.00 (18.01) | 94.24 (8.11) | 8.79 (13.64) | 0.0003 | – |
| Role-physical | |||||
| Intervention | 20.71 (7.99) | 25.00 (0) | 4.41 (8.07) | 0.002 | 0.19 |
| Control | 22.43 (6.36) | 24.05 (3.87) | 1.70 (6.49) | 0.203 | – |
| Bodily pain | |||||
| Intervention | 76.71 (18.41) | 90.91 (11.42) | 14.41 (14.85) | <0.0001 | 0.58 |
| Control | 71.12 (19.77) | 89.48 (14.40) | 18.39 (16.04) | <0.0001 | – |
| General health | |||||
| Intervention | 66.26 (17.93) | 88.21 (10.97) | 22.41 (13.22) | <0.0001 | 0.29 |
| Control | 69.98 (14.43) | 89.03 (7.76) | 18.27 (12.84) | <0.0001 | – |
| Outcome measures, mean (SD) | Baseline | 3-Month | 3-Month Change | Within Group p-valuea | Between Groups p-valueb |
|---|---|---|---|---|---|
| Vitality | |||||
| Intervention | 65.54 (19.96) | 81.25 (12.81) | 16.54 (17.96) | <0.0001 | 0.32 |
| Control | 70.59 (12.91) | 83.46 (14.28) | 13.07 (12.40) | <0.0001 | – |
| Social functioning | |||||
| Intervention | 82.14 (21.28) | 98.90 (6.43) | 17.28 (21.32) | <0.0001 | 0.46 |
| Control | 87.13 (16.99) | 100.00 (0) | 13.26 (17.10) | <0.0001 | – |
| Role-emotional | |||||
| Intervention | 22.14 (6.69) | 25.00 (0) | 2.94 (6.77) | 0.031 | 0.82 |
| Control | 22.06 (6.11) | 24.75 (1.45) | 2.78 (5.77) | 0.016 | – |
| Mental health | |||||
| Intervention | 77.57 (15.27) | 87.39 (11.30) | 10.11 (14.61) | <0.0001 | 0.56 |
| Control | 80.69 (14.47) | 89.89 (11.93) | 9.79 (15.44) | 0.0008 | – |
Abbreviations: SF-36, The Short Form (36) Health Survey.
P-value indicates the significance of the three-month changes in outcomes by group. Wilcoxon signed-rank test was applied to variables with non-normal distribution.
P-value indicates the significance of the three-month changes in outcomes by group. Mann–Whitney U test was applied to variables with a non-normal distribution.
The PACE score was only calculated for the intervention group.
SF-36 is used to measure health-related quality of life. The SF-36 consists of eight scaled scores, physical functioning (10 items), role-physical (4 items), bodily pain (2 items), general health (5 items), vitality (5 items), social functioning (2 items), role-emotional (3 items) and mental health (5 items). Each scale is directly transformed into a 0–100 scale on the assumption that each question carries equal weight. The lower the score the more disability. The higher the score the less the disability.
Significant (p-value<0.05).
Table 3.
Study outcomes within subsets of participants.
| Outcome measures/participant characteristics, mean (SD) | Intervention |
Control |
Between groups p-valueb | ||
|---|---|---|---|---|---|
| Three-month changes | Within group p-valuea | Three-month changes | Within group p-valuea | ||
| Steps | |||||
| Education ≥ high school | 29,586.2 (25,682.70) | <0.0001 | 18,431.5 (18,948.30) | <0.0001 | 0.20 |
| Ethnicity (Mexican) | 37,144.1 (27,821.97) | <0.0001 | 13,468.2 (26,616.34) | 0.095 | 0.056 |
| Ethnicity (Other Hispanic) | 26,479.6 (24,411.76) | <0.0001 | 16,956.5 (18,504.93) | 0.0016 | 0.34 |
| Speaking English | 33,096.0 (26,182.89) | 0.0001 | 6019.2 (31,237.17) | 0.69 | 0.13 |
| Hypertension | 29,984.4 (24,549.92) | <0.0001 | 23,332.4 (17,291.5) | 0.016 | 0.68 |
| Diabetes | 26,401.6 (18,174.94) | <0.0001 | 13,731.8 (22,217.85) | 0.064 | 0.21 |
| Exercise Behavior | |||||
| Aero | |||||
| Education ≥ high school | 205.0 (84.70) | <0.0001 | 207.7 (76.33) | <0.0001 | 0.89 |
| Speaking English | 158.6 (65.97) | 0.0002 | 213.0 (88.36) | 0.06 | 0.23 |
| Hypertension | 190.0 (69.98) | <0.0001 | 196.9 (146.85) | 0.02 | 0.76 |
| Diabetes | 207.0 (81.61) | <0.0001 | 247.5 (101.55) | 0.002 | 0.33 |
| Strength | |||||
| Education ≥ high school | 87.0 (72.89) | <0.0001 | 105.6 (75.83) | <0.0001 | 0.48 |
| Speaking English | 84.6 (64.88) | 0.002 | 90.0 (82.16) | 0.13 | 0.89 |
| Hypertension | 90.8 (67.57) | 0.0002 | 125.6 (69.87) | 0.02 | 0.13 |
| Diabetes | 105.0 (68.50) | 0.0005 | 132.0 (65.12) | 0.004 | 0.20 |
| SF-36c Scores | |||||
| Physical Functioning | |||||
| Education ≥ high school | 10.0 (13.65) | <0.0001 | 6.9 (11.58) | 0.007 | 0.48 |
| Speaking English | 9.3 (15.30) | 0.07 | 12.0 (11.51) | 0.25 | 0.63 |
| Hypertension | 9.7 (10.21) | 0.0009 | 8.8 (12.75) | 0.09 | 0.87 |
| Diabetes | 8.3 (10.80) | 0.008 | 16.5 (16.67) | 0.02 | 0.26 |
| Role-physical | |||||
| Education ≥ high school | 4.2 (7.58) | 0.004 | 0.96 (6.30) | 0.75 | 0.08 |
| English speaking | 10.6 (16.26) | 0.08 | 25.4 (11.04) | 0.06 | 0.12 |
| Hypertension | 12.9 (15.59) | 0.003 | 16.8 (19.99) | 0.06 | 1.00 |
| Diabetes | 9.7 (16.74) | 0.04 | 23.3 (22.93) | 0.02 | 0.16 |
| General health | |||||
| Education ≥ high school | 22.3 (13.8) | <0.0001 | 16.7 (12.68) | <0.0001 | 0.15 |
| English speaking | 21.8 (14.58) | 0.0002 | 15.2 (14.55) | 0.13 | 0.74 |
| Hypertension | 23.6 (14.01) | <0.0001 | 18.3 (13.93) | 0.02 | 0.60 |
| Diabetes | 22.5 (10.95) | <0.0001 | 22.8 (13.53) | 0.002 | 1.00 |
| Vitality | |||||
| Education ≥ high school | 17.3 (18.49) | <0.0001 | 13.5 (11.51) | <0.0001 | 0.25 |
| English speaking | 21.3 (20.58) | 0.004 | 6.3 (7.65) | 0.25 | 0.21 |
| Hypertension | 20.6 (18.13) | 0.0003 | 19.3 (15.38) | 0.008 | 0.82 |
| Diabetes | 18.2 (15.30) | 0.0004 | 12.5 (9.32) | 0.004 | 0.28 |
| Social functioning | |||||
| Education ≥ high school | 17.5 (21.92) | <0.0001 | 12.5 (16.20) | 0.0005 | 0.44 |
| English speaking | 19.6 (27.17) | 0.016 | 17.5 (14.25) | 0.13 | 0.66 |
| Hypertension | 19.4 (22.37) | 0.002 | 17.2 (19.97) | 0.13 | 0.86 |
| Diabetes | 17.5 (22.06) | 0.008 | 21.3 (21.29) | 0.03 | 0.58 |
| Role-emotional | |||||
| Education ≥ high school | 2.8 (6.69) | 0.06 | 1.9 (4.89) | 0.13 | 0.84 |
| English speaking | 4.2 (8.49) | 0.25 | 6.7 (9.13) | 0.50 | 0.55 |
| Hypertension | 5.6 (8.57) | 0.03 | 4.2 (6.30) | 0.25 | 0.92 |
| English speaking | 10.9 (17.01) | 0.02 | 2.6 (10.10) | 0.63 | 0.40 |
| Hypertension | 10.7 (16.09) | 0.01 | 10.9 (21.01) | 0.25 | 0.68 |
| Diabetes | 9.6 (18.06) | 0.08 | 7.9 (13.42) | 0.12 | 0.76 |
Abbreviations: SF-36, The Short Form (36) Health Survey.
P-value indicates significance of three-month changes in outcomes. Wilcoxon signed-rank test was applied to variables with a non-normal distribution.
P-value indicates significance of three-month changes in outcomes. Mann–Whitney U test was applied to variables with a non-normal distribution.
SF-36 is used to measure health-related quality of life. The SF-36 consists of eight scaled scores, physical functioning (10 items), role-physical (4 items), bodily pain (2 items), general health (5 items), vitality (5 items), social functioning (2 items), role-emotional (3 items) and mental health (5 items). Each scale is directly transformed into a 0–100 scale on the assumption that each question carries equal weight. The lower the score the more disability. The higher the score the less the disability.
3.1. Exercise behaviors
At three months, there was no significant difference between groups in change in aerobic or strength training exercise behaviors. For both groups, there was a statistically significant within group increase in aerobic and strength training exercise behaviors. Specifically, for aerobic activity, there was an increase in the exercise behavior score of 204.71 (SD 81.15) for the intervention group and 204.09 (SD 91.62) for the control group, P < 0.0001 for each group. For strength training, there was increase of 93.53 (SD 71.52) for the intervention group and 106.82 (SD 74.03) for the control group, P < 0.0001 for each group.
3.2. Quality of life
For quality of life subscale scores, there were no significant differences between groups at three months in physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. For within group differences, there were statistically significant increases in each group for all subscales (P < 0.031) except for role-physical in which there was not a significant increase for the control group (P = 0.20).
3.3. Exploratory analyses
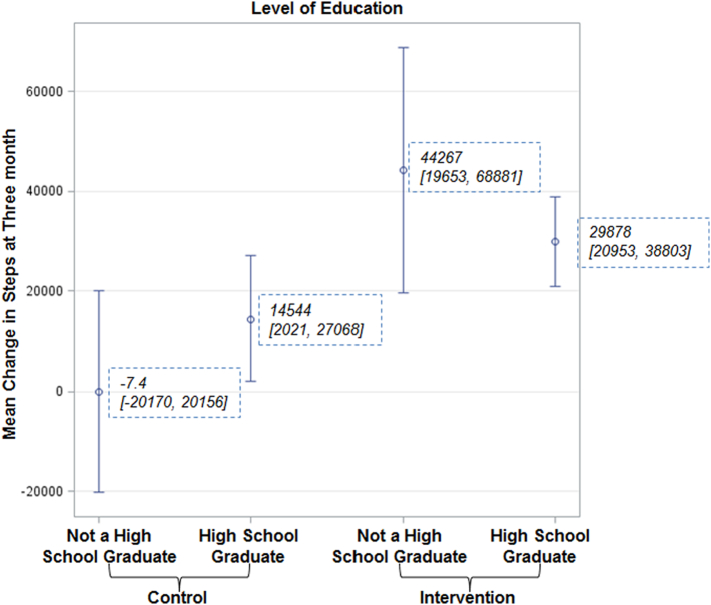
We found that participants randomized to the control group who did not graduate from high school walked fewer steps at three months compared to those at the same education level in the intervention group with a mean three-month change = 14,544.3, p-value = 0.024. (Fig. 2) Participants randomized to the intervention group had a significant increase in mean steps per week, regardless of level of education.
Fig. 2.
Error bars indicate 95% Cls.
a. There was a significant difference between participants randomized to the control group who did not graduate from high school versus persons in the intervention group with the same level of education (mean difference = 44,275, p-value = 0.035). Similarly, the difference in mean steps at three months was significantly different for participants randomized to the control group who did not graduate from high school compared to participants in the intervention group who graduated from high school (mean difference = 29,886, p-value = 0.042).
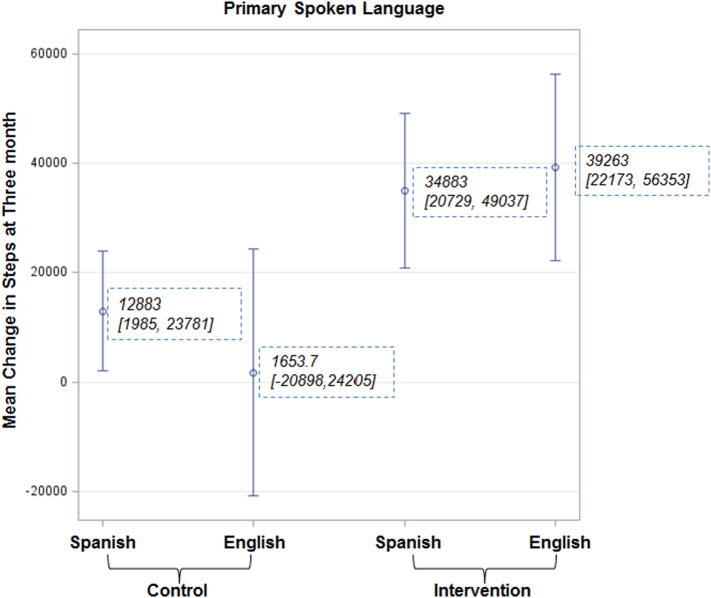
Independent of primary language spoken at home, the intervention group significantly increased their mean steps per week at three months. For the control group, only participants whose primary language was Spanish demonstrated a statistically significant increase in mean steps per week (12,883, p-value = 0.021) (Fig. 3).
Fig. 3.
Error bars indicate 95% Cls.
a. For participants whose spoken language was English, there was significant difference between those in the control group versus intervention in mean change in steps at three months (mean difference = 37,609, p-value = 0.048).
3.4. Exit survey
Sixty-seven of the 69 participants completed the exit survey. Results show half of participants (N = 34) learned about the study from their family members or friends. The vast majority (99%, N = 67) agreed that the study motivated them. On a scale of 1 to 10 with 10 indicating a high motivation effect, the wrist pedometer was considered highly motivating by all participants with a mean score of 9.62 (SD = 0.62) without a significant difference (P = 0.25) between groups, control (M = 9.71, SD = 0.58) and intervention (M = 9.53, SD = 0.66).
All 34 participants enrolled in intervention group agreed that both text messages and follow-up phone calls were highly motiviating. On a scale 1 to 10 with 10 indicating a high motivation effect, the mean score for text messages was 9.37 (SD = 0.85), which was significantly (p = 0.005) lower than the score for MI phone calls (M = 9.72 SD = 0.57).
3.5. Adverse events
There were no reported adverse events.
4. Discussion
Participants randomized to a multicomponent intervention, which included text messaging and MI, had a significant increase at three months in average weekly steps walked compared to control. There were no significant differences between groups at three months in quality of life or exercise behavior scores. Our findings add to the growing body of literature regarding the efficacy of interventions that include technology, such as text messaging, to promote PA. Below, we describe comparable studies involving the use of technology and/or MI to promote healthy behaviors, largely focusing on PA. We discuss similarities as well as distinctions.
Joseph et al. completed a systematic review of electronic and mobile health PA interventions for African American and Hispanic women. Among the 10 studies reported, four focused on Hispanic women; two of the four were large-scale randomized trials. Both studies found significant differences between the intervention and control arms for improving outcomes among Hispanic women. Distinct from our trial, the interventions for the two large-scaled trials were Internet-based. (Joseph et al., 2019). One of the two studies included objective measures for PA (Marcus et al., 2016). Among all 10 studies within the systematic review, there were significant between and within group differences in outcomes. Our trial adds to this body of work by focusing on Latino adults and use of text messaging.
In an additional systematic review of technology to promote PA, Buchholz et al. (2013) reported results on 10 studies conducted in seven countries (Buchholz et al., 2013). Similar to our study, six of the ten 10 studies were randomized controlled trials. Two of the 10 studies measured pedometers steps as the primary outcome. All 10 studies revealed a positive effect of the text messaging intervention with effect sizes all >0.20. Distinct from our work, none of the studies focused on Latino adults.
In 2014, Collins and colleagues published the findings from a survey assessment of use of text messaging (N = 82) a six-week pilot study (N = 11), pre/post design, involving Latino adults, both English and Spanish-speaking (Collins et al., 2014). The intervention was the use of text messaging to motivate PA. At the end of six weeks, participants had a significant improvement in minutes per week of aerobic activity. Our current study adds to this prior pilot by including a larger sample and use of a randomized controlled design with follow up at three months.
Aside from PA, one study reported the efficacy of text messaging to improve glycemic control in Latino adults with type 2 diabetes (Fortmann et al., 2017). One study also demonstrated the efficacy of culturally tailored intervention that included MI to improve glycemic control and self-management among Puerto Ricans with type 2 diabetes (Osborn et al., 2010). The interventions from both of these studies overlap with our work with the use of text messaging and MI. However, in our work, we combined both interventions which offer a more robust approach.
Given the association of PA with CVD as noted in the introduction, it is important to assess the potential benefits of technology to prevent CVD. Park et al. (2016) published that findings of a quantitative systematic review (Park et al., 2016). The authors reviewed 28 publications of studies, published in English, related to the use of mobile phone interventions including text messaging for cardiovascular health. Twenty two of the 28 publications reported significant improvement in behavioral and clinical outcomes. In 2018, Unal et al., conducted a systematic review to determine the efficacy of text messaging to improve secondary prevention in cardiovascular disease (Unal et al., 2018). Adding to the findings of Park et al., Unal et al. reported that text messaging may be beneficial for the secondary prevention of CVD but the current evidence does not address adverse effects, harms, or patient satisfaction.
In our study, there were no reported adverse events and, per the exit survey, intervention participants were satisfied with the text messaging intervention. Of note, they had a slighter higher preference for MI. This finding may reflect the desire for brief human contact as part of a text messaging intervention.
Limitations of the study include the use of a three-month trial. Thus, we do not know the sustainability of our findings. However, our findings provide excellent pilot data which can be used to inform a larger trial with more long-term follow up. Additionally, we did not include an attention control group. Thus, we did not account for the impact of increased attention on the benefits of the intervention. Based on the exit survey, participants in the intervention arm preferred MI and this was limited to four phone calls total. So the actual amount of increased attention to intervention participants was limited. Our exploratory analyses were post-hoc which may reduce the statistical significance of these findings. An additional limitation of the study is the Hawthorne effect which would bias our findings such that participants may have altered their behavior favorably given their participation in the study. However, both intervention and control participants were aware of our focus on improving PA but ultimately the intervention group had a greater increase in this outcome. If both groups had increased their PA, there would have been no difference between the groups which would have suggested a greater Hawthorne effect. Finally, we do not have validity data for the pedometer, Striiv Band, which may limit the validity of our primary outcome.
In conclusion, our results highlight the potential efficacy of text messaging combined with MI to increase PA among Latino adults. Future work should include more participants with longer follow up.
Acknowledgments
Acknowledgments
Special thanks to the graduate students working with Dr. David Akopian who provided technical support for the text messaging.
Sources of funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number 1R56AG047590-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of competing interest
None.
References
- Buchholz S.W., Wilbur J., Ingram D., Fogg L. Physical activity text messaging interventions in adults: a systematic review. Worldviews Evid.-Based Nurs. 2013;10(3):163–173. doi: 10.1111/wvn.12002. [DOI] [PubMed] [Google Scholar]
- Burke B.L., Arkowitz H., Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J. Consult. Clin. Psychol. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Butler C.C., Rollnick S., Cohen D., Russell I., Bachmann M., Stott N. Motivational consulting versus brief advice for smokers in general practice: a randomized trial. Br. J. Gen. Pract. 1999;49:611–616. [Google Scholar]
- Collins T., Petersen N., Suarez-Almazor M., Ashton C. The prevalence of peripheral arterial disease in a racially diverse population. Arch. Intern. Med. 2003;163:1469–1474. doi: 10.1001/archinte.163.12.1469. [DOI] [PubMed] [Google Scholar]
- Collins T., O'Malley K., Petersen N., Suarez-Almazor M. The lifestyle and clinical survey: a pilot study to validate a medical history questionnaire. Fed. Pract. 2005;22(5):25–46. [Google Scholar]
- Collins T.C., Lunos S., Carlson T., Henderson K., Lightbourne M., Nelson B. Effects of a home-based walking intervention on mobility and quality of life in people with diabetes and peripheral arterial disease: a randomized controlled trial. Diabetes Care. 2011;34(10):2174–2179. doi: 10.2337/dc10-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins T.C., Dong F., Ablah E., Parra-Medina D., Cupertino P., Rogers N. Text messaging to motivate exercise among Latino adults at risk for vascular disease: a pilot study, 2013. Prev. Chronic Dis. 2014;11:E192. doi: 10.5888/pcd11.140219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus M.L., Talavera G.A., Aviles-Santa M.L., Allison M., Cai J., Criqui M.H. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn C., Deroo L., Rivara F.P. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Fanning J., Mullen S.P., McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J. Med. Internet Res. 2012;14(6) doi: 10.2196/jmir.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortmann A.L., Gallo L.C., Garcia M.I., Taleb M., Euyoque J.A., Clark T. Dulce digital: an mHealth SMS-based intervention improves glycemic control in Hispanics with type 2 diabetes. Diabetes Care. 2017;40(10):1349–1355. doi: 10.2337/dc17-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://www.acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/Statistical-Profile-Older-Hispanic-Ameri.pdf
- https://www.striiv.com/
- Hu J., Wallace D.C., Amirehsani K.A., McCoy T.P., Coley S.L., Wiseman K.D. Improving physical activity in Hispanics with diabetes and their families. Public Health Nurs. 2015;32(6):625–633. doi: 10.1111/phn.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph R.P., Royse K.E., Benitez T.J. A systematic review of electronic and mobile health (e- and mHealth) physical activity interventions for African American and Hispanic women. J. Phys. Act. Health. 2019;16(3):230–239. doi: 10.1123/jpah.2018-0103. [DOI] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions. Standford Chronic Disease Self-management Study. Thousand Oaks, Calif: Sage Publications; vol. 1996: 24–5.
- Marcus B.H., Hartman S.J., Larsen B.A., Pekmezi D., Dunsiger S.I., Linke S. Pasos Hacia La Salud: a randomized controlled trial of an internet-delivered physical activity intervention for Latinas. Int. J. Behav. Nutr. Phys. Act. 2016;13:62. doi: 10.1186/s12966-016-0385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W., Rollnick S. Guilord Press; New York: 1991. Motivational Interviewing: Preparing People to Change Addictive Behavior. [Google Scholar]
- Miller W., Rollnick S. Second ed. The Guilford Press; New York: 2002. Motivational Interviewing: Preparing People for Change. [Google Scholar]
- NCHS NHIS . Sample Adult Core component. 2017. January–September. [Google Scholar]
- Ogedegbe G., Schoenthaler A., Richardson T., Lewis L., Belue R., Espinosa E. An RCT of the effect of motivational interviewing on medication adherence in hypertensive African Americans: rationale and design. Contemp. Clin. Trials. 2007;28(2):169–181. doi: 10.1016/j.cct.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Osborn C.Y., Amico K.R., Cruz N., O'Connell A.A., Perez-Escamilla R., Kalichman S.C. A brief culturally tailored intervention for Puerto Ricans with type 2 diabetes. Health Educ. Behav. 2010;37(6):849–862. doi: 10.1177/1090198110366004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park L.G., Beatty A., Stafford Z., Whooley M.A. Mobile phone interventions for the secondary prevention of cardiovascular disease. Prog. Cardiovasc. Dis. 2016;58(6):639–650. doi: 10.1016/j.pcad.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K., Sallis J., Long B., Calfas K., Wooten W., Heath G. A new tool for encouraging activity: project PACE. Physician Sportsmed. 1994;22(11):45–52. doi: 10.1080/00913847.1994.11947706. [DOI] [PubMed] [Google Scholar]
- Pew Internet. 2010. [Google Scholar]
- Prochaska J.O., DiClemente C.C. Stages and processes of self-change of smoking: toward an integrative model of change. J. Consult. Clin. Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Resnicow K., Davis R.E., Zhang G., Konkel J., Strecher V.J., Shaikh A.R. Tailoring a fruit and vegetable intervention on novel motivational constructs: results of a randomized study. Ann. Behav. Med. 2008;35(2):159–169. doi: 10.1007/s12160-008-9028-9. [DOI] [PubMed] [Google Scholar]
- Stevens L.M., Lymn C., Glass R.M. JAMA patient page. Peripheral arterial disease. JAMA. 2006;295(5):584. doi: 10.1001/jama.295.5.584. [DOI] [PubMed] [Google Scholar]
- Unal E., Giakoumidakis K., Khan E., Patelarou E. Mobile phone text messaging for improving secondary prevention in cardiovascular diseases: a systematic review. Heart Lung. 2018;47(4):351–359. doi: 10.1016/j.hrtlng.2018.05.009. [DOI] [PubMed] [Google Scholar]
- Ware J.E., Snow K.K., Kosinski M., Gandek B. Quality Metric Incorporated; Lincoln, RI: 2000. SF-36 Health Survey: Manual and Interpretation Guide. [Google Scholar]