Abstract
The anterior or volar compartment of the forearm contains eight muscles: five belong to the superficial group (pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis and flexor carpi ulnaris), and three to the deep group (flexor digitorum profundus, flexor pollicis longus and pronator quadratus). Knowledge of the topographic anatomy is essential for correct performance of ultrasound (US) examinations and correct interpretation of the images provided.
Keywords: Forearm, Ultrasound, Sonoanatomy, Anterior compartment, Flexor muscles
Introduction
A profound knowledge of sonoanatomy is important for diagnostic purposes, as in cases of muscle atrophy or muscle disease, but also for treatment procedures such as nerve blocking and local botulinum toxin application. Given the tight relation between muscles and other structures like nerves and tendons, sonoanatomy plays an important role in the assessment of compression syndromes. Thus, a good sonoanatomy basis can improve ultrasound accuracy in the diagnosis and treatment of several conditions. There are 19 muscles in the forearm. Eleven are classified as extensor muscles and eight belong to the flexor group [1]. These muscles are arranged as a flexor compartment, anteriorly, and an extensor compartment, posteriorly [1]. The anterior compartment muscles are arranged in superficial and deep groups [2]. The muscles in the superficial flexor compartment are the pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis and flexor carpi ulnaris [1, 2]. The muscles in the deep flexor compartment are the flexor digitorum profundus, flexor pollicis longus and pronator quadratus [1, 2]. The anterior compartment muscles are separated from the dorsal muscles by the radioulnar interosseous membrane [3]. In the volar forearm, the ulnar nerve innervates the flexor carpi ulnaris and the flexor digitorum, profundus and the median nerve innervates all the other forearm flexor muscles [4].
Superficial muscles
The five muscles belonging to the superficial compartment arise from the medial epicondyle of the humerus. The intermuscular septa and the antebrachial fascia also provide partial origins, and some muscles have additional bony origins [1]. Proceeding from the lateral to the medial direction, there are the pronator teres (PT), flexor carpi radialis (FCR), palmaris longus (PL), flexor carpi ulnaris (FCU) and the flexor digitorum superficialis (FDS) (Figs. 1, 2). PT has both a humeral and an ulnar head. The humeral origin is larger and more superficial. It arises from the common flexor tendon, the intermuscular septum between it and FCR, and the antebrachial fascia [2]. The ulnar head arises from the medial side of the coronoid process of the ulna, distal to the attachment of flexor digitorum superficialis. The PT muscle passes obliquely across the forearm and ends in the middle of the lateral surface of the radius. The insertion is overlaid by the brachioradialis muscle [1]. The median nerve enters the anterior compartment, passing between the superficial and deep heads of the PT muscle [5]. The lacertus fibrosus, PT and FDS are key structures that can cause compression neuropathy of the median nerve at the elbow or proximal forearm [4]. Proximally, the medial border of the PT is related to the lateral aspect of flexor carpi radialis. The PT is anterior to the flexor digitorum superficialis [2]. The FCR arises from the common flexor tendon, from the antebrachial fascia and from adjacent intermuscular septa [2] (Fig. 3). In the mid-forearm, the FCR becomes a long tendon that accounts for about half of the muscle's length [1]. It passes within a synovial sheath, through a lateral canal in the wrist in a compartment formed by a split in the flexor retinaculum [1, 2], and ends in the palmar surface of the base of the second metacarpal (there is frequently an additional slip to the third metacarpal) [1]. Distal attachments lie beneath the oblique head of the adductor pollicis [2]. In the lower part of the forearm, the radial artery lies between the tendon of the FRC and the tendon of the brachioradialis [2]. The posterior ulnar recurrent artery passes deep into the PT to enter the deep surface of the FCR [2]. The FDS is the largest of the superficial flexors, and arises as a humero-ulnar and a radial head. The humero-ulnar origin arises from the common flexor tendon, the anterior band of the ulnar collateral ligament, the adjacent intermuscular septa and from the medial border of the coronoid process, proximal to the ulnar origin of the PT [1, 2]. The radial head is a thin layer arising from the upper two-thirds of the anterior border of the radius, between the radial tuberosity and the insertion of the PT [1, 2]. The muscle forms two planes—the tendons of its superficial plane pass to the middle and ring fingers, and the deep lamina ends in tendons for digits I and V [1, 2]. The FDS runs deep into the PT and FCR. The median nerve and ulnar artery descend between the heads of the FDS, and the nerve continues between the FDS and FDP muscles [2, 4]. The normal PL also originates from the common flexor tendon, with a proximal muscle belly and long distal tendon that inserts into the palmar fascia [1, 2]. The PL muscle can originate from the lacertus fibrosus, FDS, FCR or the FCU, and may insert into the antebrachial fascia, thenar eminence or flexor carpi ulnaris, or into the carpal bones [6]. It becomes tendinous in the mid-forearm and its tendon passes above the flexor retinaculum [2]. As the tendon crosses the retinaculum, it broadens out to become a flat sheet that constitutes the chief part of the palmar aponeurosis [1, 2]. The FCU has a humeral and an ulnar head and forms the bulk of the soft tissue cover of the medial aspect of the ulna [1, 2]. The smaller humeral head arises from the common flexor tendon [1], and the ulnar head origin arises from the medial border of the olecranon, the proximal two-thirds of the posterior border of the ulna and from the intermuscular septum between it and the FDS [1, 2]. The FCU tendon inserts on the pisiform bone. By means of two ligaments, it also reaches the hamulus of the hamate and the base of the fifth metacarpal [1]. The ulnar nerve and posterior ulnar recurrent artery pass under the tendinous arch, between the two heads of the FCU [2]. Ulnar vessels and nerve lie lateral to its tendon in the distal forearm [2].
Fig. 1.
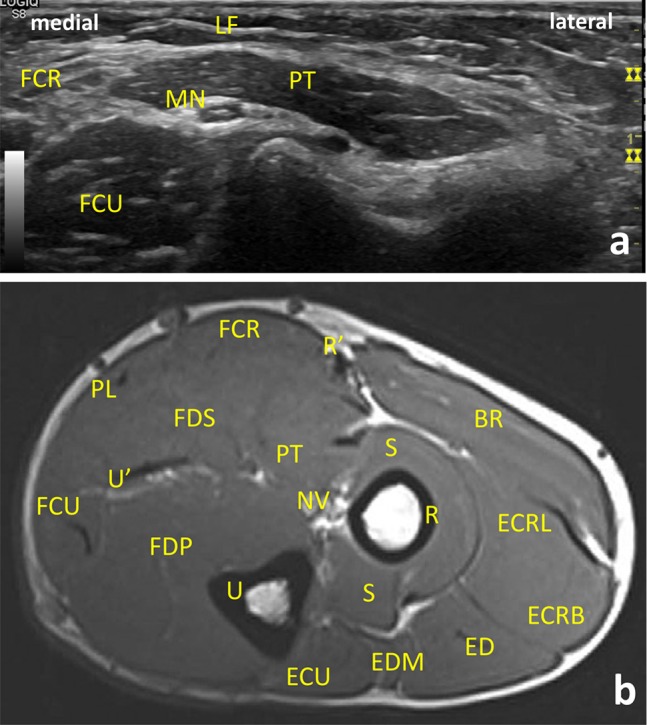
Ultrasound (US) (a) and magnetic resonance imaging (MRI) transversal/axial images of the proximal flexor compartment of the forearm (b). LF lacertus fibrosus, PT pronator teres, FCR flexor carpi radialis, FCU flexor carpi ulnaris, MN median nerve, FDS flexor digitorum superficialis, PL palmaris longus, FDP flexor digitorum profundus, S supinator, BR brachioradialis muscle, ECRL extensor carpi radialis longus, ECRB extensor carpi radialis brevis, ED extensor digitorum, EDM extensor digitorum minimi, ECU extensor carpi ulnaris, R radius, U ulna, NV neurovascular bundle with median nerve, brachial artery, and vein; R’ superior radial nerve, artery, and vein; U’ ulnar nerve, artery, and vein. MRI reprinted from Magnetic Resonance Imaging Clinics of North America, Vol. 19, Vogelius E, Hanna W, Robbin M. Magnetic Resonance Imaging of the Long Bones of the Upper Extremity, pages 567–579. Copyright (2019), with permission from Elsevier
Fig. 2.
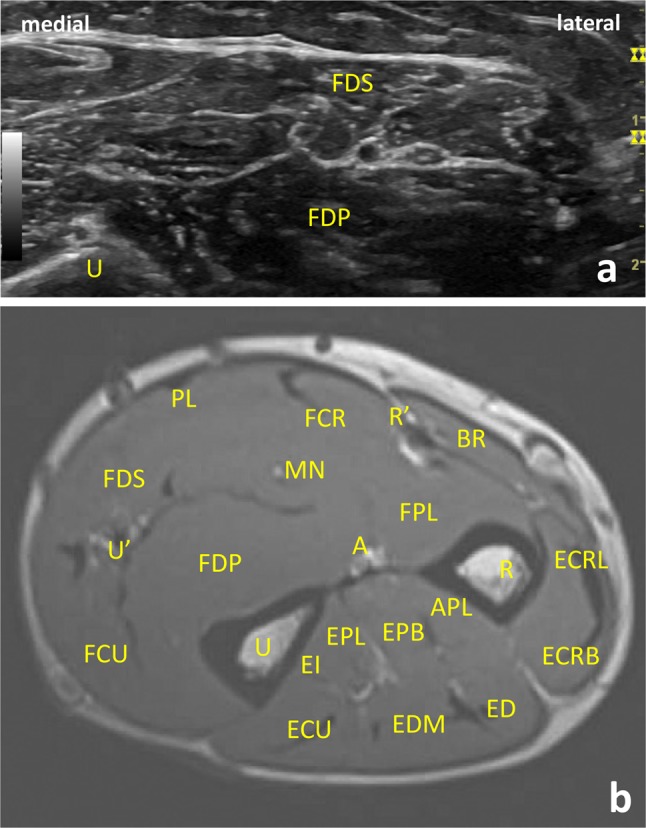
Ultrasound (US) (a) and magnetic resonance imaging (MRI) (b) transversal/axial images of anatomy of the mid-forearm at the level of the deep extensor origins. Flexor digitorum superficialis is the largest of the superficial flexors, and arises by a humero-ulnar and a radial head. Flexor digitorum profundus arises deep to the superficial flexors from the posterior border of the ulna and extends distally almost to pronator quadratus. FDS flexor digitorum superficialis, FPD flexor digitorum profundus, FCR flexor carpis radialis, FCU flexor carpi ulnaris, FDS flexor digitorum superficialis, PL palmaris longus, FDP flexor digitorum profundus, BR brachioradialis muscle, ECRL extensor carpi radialis longus, ECRB extensor carpi radialis brevis, ED extensor digitorum, EDM extensor digitorum minimi, ECU extensor carpi ulnaris, EI extensor indicis, EPL extensor pollicis longus, EPB extensor pollicis brevis, APL abductor pollicis longus, R radius, U ulna, U’ ulnar nerve, artery, and vein; R’ superior radial nerve, artery, and vein; A anterior interosseous nerve, MN median nerve. MRI reprinted from Magnetic Resonance Imaging Clinics of North America, Vol. 19, Vogelius E, Hanna W, Robbin M. Magnetic Resonance Imaging of the Long Bones of the Upper Extremity, pages 567–579. Copyright (2019), with permission from Elsevier
Fig. 3.
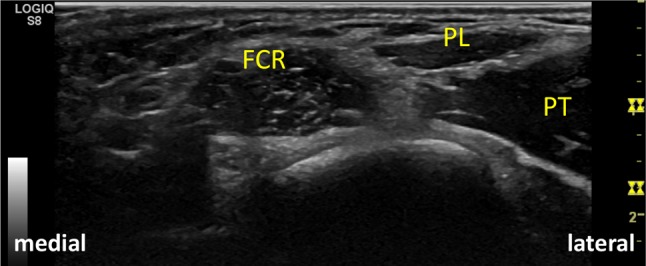
Flexor carpi radialis arises from the common flexor tendon, from the antebrachial fascia and from adjacent intermuscular septa. FCR flexor carpi radialis, PL palmaris longus, PT pronator teres
Accessory muscles or variant conditions of superficial muscles
In rare cases, the FCR may be absent. The flexor carpi radialis brevis (FCRB) is an anomalous muscle of the wrist that commonly originates from the volar radial surface of the distal radius, distal to the flexor pollicis longs and proximal to the insertion of the pronator quadratus. It runs superficial to the pronator quadratus outside of the carpal tunnel [6]. The insertion is typically in the second or third metacarpal base [7]. Its usual passage past the wrist is beside the FCR tendon, through its osteo-fibrous tunnel in the groove of the trapezium [7]. The FCRB may travel distally in the same sheath as the flexor carpi radialis [6]. In 13% of cases, PL is absent on one or both sides [1, 2]. An anomalous PL with three heads or as three distinct muscles has been described [6]. An accessory tendon may also exist at the ulnar aspect of the main tendon distally [6].
Deep muscles
In order from the radial to the ulnar side of the forearm, the muscles of the deep flexor compartment are the flexor digitorum profundus (FDP), flexor pollicis longus (FPL) and pronator quadratus (PQ) (Fig. 4). The FDP begins deep to the superficial flexors from the posterior border of the ulna [1, 2] and extends distally almost to the pronator quadratus [2]. The muscle ends in four tendons that terminate on the bases of the distal phalanges of digits II–V [1, 2]. In the forearm, the median nerve runs on the anterior surface of the FDP’s lateral aspect [2]. In the proximal third of the forearm, the median nerve runs off the anterior interosseous nerve (AIN) [4]. It is the nerve most frequently involved in compartment syndrome of the forearm [4]. FPL arises from the anterior surface of the radius and from the adjacent interosseous membrane [1]. It frequently arises by a variable slip from the lateral, or more infrequently, medial border of the coronoid process [2]. Its tendon passes between the two sesamoids of the metacarpophalangeal joint of digit I and inserts on the base of the distal phalanx of the thumb [1] The FPL runs lateral to the FDP and can sometimes be connected to the FDS or FDP, or to the PT [2]. The AIN and vessels descend on the interosseous membrane between the FPL and FDP [2].
Fig. 4.
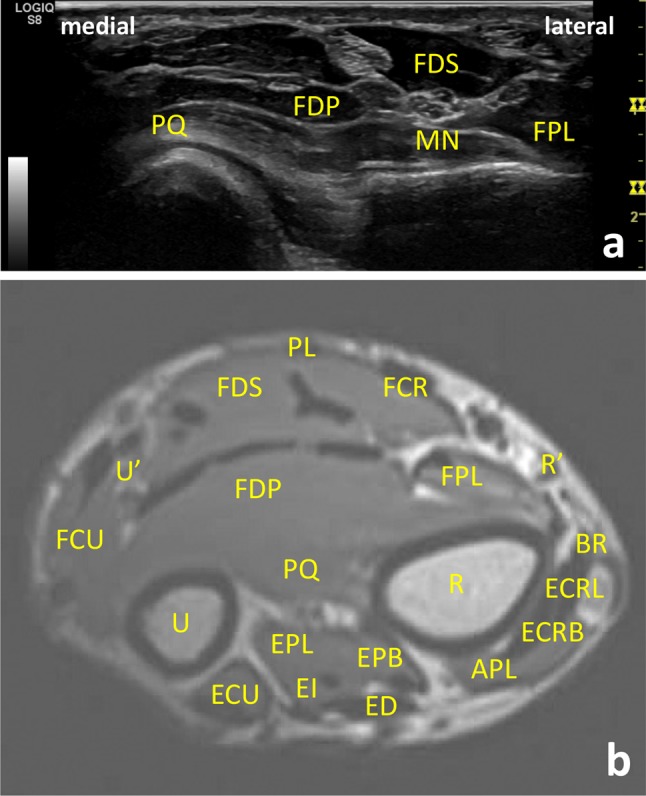
Ultrasound (US) (a) and magnetic resonance imaging (MRI) (b) transversal/axial images of anatomy of the distal forearm at the level of the proximal radial metaphysis. FDP flexor digitorum profundus, FPL flexor pollicis longus, PQ pronator quadratus, FSD flexor digitorum superficialis, FPL flexor pollicis longus, FDS flexor digitorum superficialis, FCR flexor carpis radialis, FCU flexor carpi ulnaris, PL palmaris longus, BR brachioradialis muscle, ECRL extensor carpi radialis longus, ECRB extensor carpi radialis brevis, ED extensor digitorum, ECU extensor carpi ulnaris, EI extensor indicis, EPL extensor pollicis longus, EPB extensor pollicis brevis, APL abductor pollicis longus, R radius, U ulna, U’ ulnar nerve, artery, and vein, R’ superior radial nerve, artery, and vein, MN median nerve. MRI reprinted from Magnetic Resonance Imaging Clinics of North America, Vol. 19, Vogelius E, Hanna W, Robbin M. Magnetic Resonance Imaging of the Long Bones of the Upper Extremity, pages 567–579. Copyright (2019), with permission from Elsevier
The PQ muscle is a flat, quadrilateral muscle located just above the wrist and deep to the FDP and FPL [1]. It arises from the anterior surface of the ulna, the medial part of this surface and an aponeurosis that covers the medial third of the muscle [2]. It extends across the front of the distal parts of the radius and ulna (Fig. 5) [2].
Fig. 5.
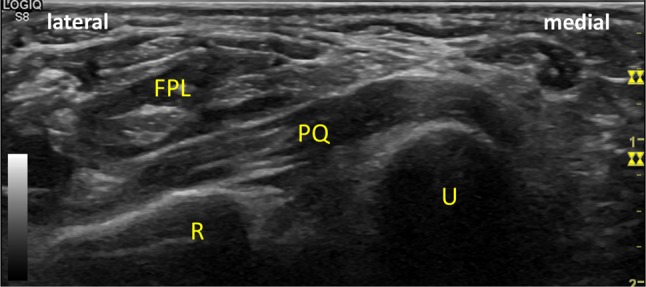
Pronator quadratus extends across the front of the distal parts of the radius and ulna. FPL flexor pollicis longus, PQ pronator quadratus, R radius, U ulna
Although they are not included in the structures of the anterior forearm already mentioned, some features of the lateral aspect of the forearm are described next, due to their clinical relevance to posterior interosseous nerve (PIN) compression syndrome. At the radial aspect of the forearm, the extensor carpi radialis brevis (ECRB) and longus and the brachioradialis form the so-called mobile wad [5]. The supinator is the deepest of the lateral muscles (Fig. 6) [5]. It has two heads, between which the posterior interosseous nerve, motor branch of the radial nerve passes to reach the posterior elbow [5]. At the level of the humeroradial joint, the radial nerve divides into the superficial radial sensory nerve and posterior interosseous nerve (PIN) [4]. After branching from the main radial nerve at the elbow, the PIN passes beneath the fascia of the supinator muscle (arcade of Frohse) [4] (Fig. 7). The areas of anatomic compression include fibrous bands volar to the radiocapitellar joint, ECRB fibrous bands, radial recurrent vessels, the arcade of Frohse (most common), and the distal fibrous border of the supinator [8, 9].
Fig. 6.
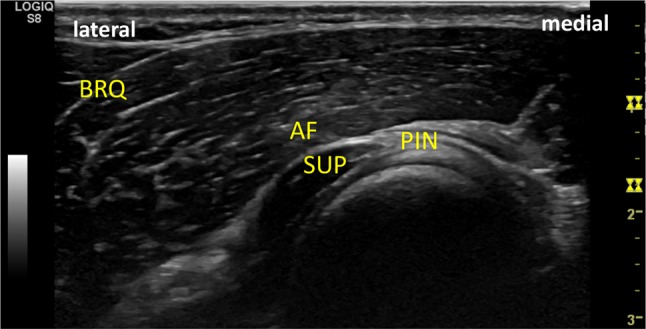
At the radial aspect of the forearm, the extensor carpi radialis brevis and longus and the brachioradialis form the so-called mobile wad. The supinator is the deepest of the lateral muscles. BRQ brachioradialis, SUP supinator
Fig. 7.
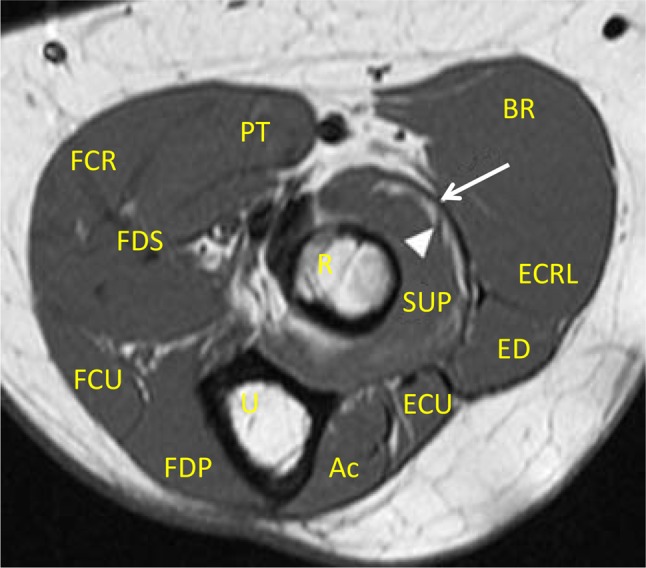
Magnetic resonance imaging (MRI) axial image of anatomy of the proximal forearm. After branching from the main radial nerve at the elbow, the posterior interosseous nerve (PIN) passes beneath the fascia of the supinator muscle (arcade of Frohse). Arrow: arcade of Frohse, arrowhead: PIN, SUP supinator, R radius, U ulna, BR brachioradialis muscle, ECRL extensor carpi radialis longus, ED extensor digitorum, Ac Anconeus muscle, ECU extensor carpi ulnaris, PT pronator teres, FCR flexor carpis radialis, FDS flexor digitorum superficialis, FDP flexor digitorum profundus, FCU flexor carpi ulnaris. MRI—Courtesy Dr. Michael Stadnick, in Stadnick M. Posterior Interosseous Nerve Syndrome. MRI Web Clinic, 2005. Retrieved from https://radsource.us/posterior-interosseous-nerve-syndrome/
Accessory muscles or variant conditions of deep muscles
The interosseous attachment of FPL, or even the whole muscle, may be absent [2]. The “Gantzer muscle” refers to an accessory slip of the flexor pollicis longus [5, 6]. It arises from the medial epicondyle in most cases—with a dual origin from the epicondyle and the coronoid process in 15% of the cases [5]—and inserts on the deep flexors of the digits [5, 6]. In rare cases, the “Gantzer muscle” can insert as three parts into the flexor pollicis longus, flexor digitorum superficialis, and flexor digitorum profundus [6]. The Palmaris profundus (PP) is an anomalous muscle of the forearm, and has been called the musculus comitans nervi median because of its close relation with the median nerve [6]. The PP runs through the carpal tunnel, adjacent to the median nerve, and terminates in the palmar aponeurosis distally [6]. Possible origins include the radial diaphysis, ulnar diaphysis, flexor digitorum superficialis fascia, PL, flexor pollicis longus, or the medial epicondyle. Insertional variations can include the third metacarpal or the radial carpal bones [6].
Conclusions
Ultrasound has become an indispensable tool for the study of the musculoskeletal system. It can provide images of muscles, tendons, ligaments, joints, and soft tissues throughout the body. Because it is a safe, relatively quick and noninvasive method, it is a useful diagnostic instrument in rheumatology and other areas. A thorough knowledge of the compartmental anatomy of the forearm and any possible anatomical variants is essential for performing ultrasound examinations correctly, making diagnosis and being able to treat patients satisfactorily.
Compliance with ethical standards
Conflict of interest
The authors have no conflict of interest.
Human and animal rights statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lannotti J, Parker R. Netter collection of medical illustrations: part I the upper limb. 2. Amsterdam: Elsevier; 2013. pp. 109–148. [Google Scholar]
- 2.Standing S (2016) Elbow and forearm. In: Gray's anatomy, 41th edn. Elsiever, Amsterdam, pp 837–861
- 3.Precerutti M, Garioni E, Ferrozzi G. Dorsal forearm muscles: US anatomy pictorial essay. J Ultrasound. 2010;13:66–69. doi: 10.1016/j.jus.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reavey P, Rafijah G (2017) Anatomy and examination of the hand, wrist, forearm, and elbow. In: Principles of hand surgery and therapy, 3rd edn. Elsevier, Amsterdam, pp e1–e25
- 5.Bianchi S, Martinoli C. ultrasound of the musculoskeletal system. New York: Springer; 2007. Forearm; pp. 409–423. [Google Scholar]
- 6.Andring N, Kennedy S, Lannuzzi N. Anomalous forearm muscles and their clinical relevance. J Hand Surg Am. 2018;43(5):455–463. doi: 10.1016/j.jhsa.2018.02.028. [DOI] [PubMed] [Google Scholar]
- 7.Trowbridge S, Vidakovic H, Hammer N, Kieser DC. A case of anomalous flexor carpi radialis brevis muscle and its clinical significance. Int J Anat Var. 2017;4:91–93. [Google Scholar]
- 8.S. Brent Brotzman, Steven R. Novotny (2018) Nerve compression syndromes. In: Clinical orthopaedic rehabilitation: a team approach, 4th edn. Elsevier, Amsterdam, pp 32–41.e1
- 9.Smith M, Carlisle J, Gerlach D, Wright R (2018) Elbow injuries. In: Netter's sports medicine, 2nd edn. Elsevier, Amsterdam, pp 382–390.e1


