Abstract
Purpose
To assess the effectiveness and safety of acupuncture for erectile dysfunction (ED).
Materials and Methods
We searched six major English and Chinese databases included randomized controlled trials (RCTs) testing acupuncture alone or in combination for ED. Dichotomous data were presented as risk ratio (RR) and continuous data were presented as mean difference (MD) both with 95% confidence interval (CI). The Revman (v.5.3) was used for data analyses. Quality of evidence across studies was assessed by the online GRADEpro tool.
Results
We identified 22 RCTs, fourteen of them involving psychogenic ED. Most of the included RCTs had high or unclear risk of bias. There was no difference between electro-acupuncture and sham acupuncture with electrical stimulation on the rate of satisfaction and self-assessment (RR, 1.50; 95% CI, 0.71–3.16; 1 trial). Acupuncture combined with tadalafil appeared to have better effect on increasing cure rate (RR, 1.31; 95% CI, 1.00–1.71; 2 trials), and International Index of Erectile Function-5 scores (MD, 5.38; 95% CI, 4.46–6.29; 2 trials). When acupuncture plus herbal medicine compared with herbal medicine alone, the combination therapy showed significant better improvement in erectile function (RR, 1.68; 95% CI, 1.31–2.15; 7 trials). Only two trials reported facial red and dizziness cases, and needle sticking and pruritus cases in acupuncture group.
Conclusions
Low quality evidence shows beneficial effect of acupuncture as adjunctive treatment for people mainly with psychogenic ED. Safety of acupuncture was insufficiently reported. The findings should be confirmed in large, rigorously designed and well-reported trials.
Keywords: Acupuncture, Erectile dysfunction, Meta-analysis, Randomized controlled trial, Systematic review
INTRODUCTION
Erectile dysfunction (ED), also called impotence, is defined as an inability to obtain or maintain a penile erection sufficient for satisfactory sexual intercourse [1]. ED is a common clinical condition, affecting men of all ages, particularly the elderly. ED affects around 52% in men aged 40 to 70 years, with more than 320 million men predicted to suffer from ED by 2025 years worldwide [2]. ED can result in considerable distress and lowered quality of life. As it is associated with a wide variety of underlying conditions such as diabetes and cardiovascular co-morbidities, treatment options depend upon the associated factors and diverse approaches in different settings [3]. Current treatment for ED included oral drugs, intrapenile therapies and penile prosthesis implantation, but with uncertain effect [4]. Alternative options such as non-pharmaceutical therapies are needed and expected.
Acupuncture, part of traditional Chinese medicine (TCM), is increasingly used for the treatment of ED. There are different ways for its use, including stimulation of acupoints with needling, heating (moxibustion), electrical current, or injecting drugs into acupoints [5]. TCM theory states that ED is usually caused by the decline of fire from the life gate (Ming men), sexual indulgence or frequent masturbation, and emotional disturbances. Thus, the principle of acupuncture treatment is to invigorate the kidney qi and nourish the heart and spleen. As such, and selecting acupoints from the Kidney Meridian of Foot-Shaoyin and the Ren Meridian and back-shu points is commonly used for treating ED, and moxibustion can be used as well during the treatment [6,7].
The potential mechanism of action by how acupuncture may have an effect on ED is unclear. However, there is some indication that acupuncture may stimulate nerve endings, and induce nerve impulses which then impact on levels of norepinephrine, acetylcholine, and their biological enzymes in the central nervous system [8]. Some clinical trials have been conducted to investigate the effect of acupuncture in the treatment of ED. A systematic review published in 2016 concluded with insufficient results about the effect of acupuncture when comparing with sham acupuncture and psychological therapy [9]. Another recent systematic review summarized evidence of acupuncture for ED [10]. However, this review searched literature mainly from Chinese databases, and its control groups were only Chinese herbal medicine. As a result, the interpretation of the findings may be limited. Our review aims to comprehensively review the current evidence of acupuncture for ED.
MATERIALS AND METHODS
1. Inclusion/exclusion criteria
We included both parallel, cross-over, randomized clinical trials, regardless of blinding and publication status. Types of participants included men who were diagnosed as ED by any recognized national or international criteria, regardless of psychogenic and organic origin of impotence. Interventions included as verum acupuncture (defined as needling stimulation of acupuncture points or trigger points by manual acupuncture with or without heating [moxibustion]), electro-stimulating, acupoint injection, acupressure and laser acupuncture [5,6]. Controls included no treatment, sham acupuncture, herbal medicine, or conventional medicine. Co-interventions were allowed as long as they were given equally to all randomized arms.
1) Primary outcomes
(1) Patient erectile function and partner satisfaction measured by International Index of Erectile Function-5 (IIEF-5) score and its components [11]; (2) The effect and quality of sexual intercourse presented as “cure”, or “markedly improved on erectile function” based on validated measurement tools or scales. “Cure” was defined as symptom disappearance with successful sexual activity and/or with IIEF-5 score ≥22 [11]. “Markedly improved on erectile function” referred to that all the three below items were met: the self-report disappearance of clinical symptoms, the erection angle of penis is more than 90 degrees in sexual activity, and the success rate of sexual intercourse is over 75%.
2) Secondary outcomes
(1) The quality of sexual activity measured by “satisfaction and self-assessment”, which defined as the self-reported satisfaction by patients or their partners. They reported that the symptoms disappeared, at same time, erectile function and sexual life returned to normal; (2) Angle of penile erection measured by self-assessment tools or scales; (3) Adverse events.
2. Search strategy
We searched for published studies in two English and four Chinese electronic databases from their inception to August 31st, 2018, including PubMed, the Cochrane Library, Sinomed Database, China National Knowledge Infrastructure, Wanfang Database, and China Science Technology Journal Database. The search terms included acupuncture-related terms (i.e., “acupuncture”, “electro-acupuncture”, “auricular therapy”, “warm needling”, “fire needling”, “shark hook needling”, “magnet needle”, “acupoint injection”, “point injection”, “moxibustion”, “acupressure”), combined with erectile dysfunction related terms (i.e., “erectile dysfunction [Mesh terms]”, “impotence”, “yang wei”). Search term strategies were adapted for each specific database.
3. Study selection and data extraction
Two authors (Lai BY and Jia LY) independently selected the trials included in the review according to the inclusion/exclusion criteria. Any disagreement was resolved by discussion. We performed data extraction using a self-developed data extraction form. If the necessary data were not available in the trial reports, further information was sought by contacting corresponding author.
4. Assessment of methodological quality
The risk of bias of the included trials was assessed independently according to the criteria from the Cochrane Handbook for Systematic Reviews of Interventions [12]. Criteria included adequacy of generation of the allocation sequence, allocation concealment, blinding (blinding of participants and personnel, blinding of outcome assessors), incomplete outcome data or not, whether selected reporting the results and other bias (e.g., imbalance of the baseline information). Risk of bias for each trial was assessed as low, high, or unclear. A trial was considered as having low risk of bias when all the items met the criteria; a trial was considered at high risk of bias when at least one of the items was not met; and a trial was considered unclear risk of bias where insufficient information was available to make the judgment. Any difference in the quality assessment of trials was resolved by discussion in order to reach consensus. Quality of evidence across studies for each important outcome was assessed using the online GRADE approach to support the recommendations using the online GRADEpro tool (https://gradepro.org/).
5. Data analysis
Meta-analysis was performed within comparisons of the same type of acupuncture versus the similar control. Dichotomous data were presented as risk ratio (RR) and continuous outcomes as mean difference (MD), both with 95% confidence intervals (CI). We used I-square value to detect statistical heterogeneity and to measure the percentage of the variability in effect sizes between studies that is due to heterogeneity rather than to sampling error. We used random effects model to combine the results in this review due to potential sources of clinical heterogeneity [12]. If the I2>75%, we did not pool the data and results from each individual trial were presented respectively. The statistical analysis was carried out using Revman 5.3 software. If a sufficient numbers of randomized trials were identified and data available, subgroup analysis would be performed according to the comparisons.
RESULTS
1. Study selection
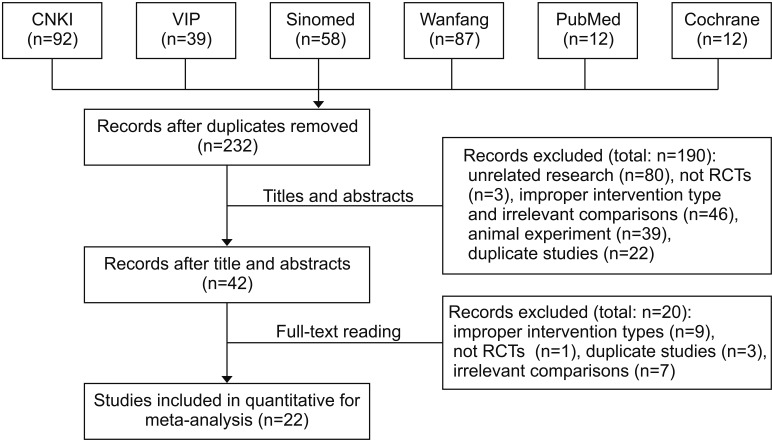
We identified 300 studies, of which 68 duplicates were removed. After screening the abstracts, 190 trials were excluded with reasons. Full-texts of the remaining 42 trials were retrieved and assessed for eligibility. A total of 22 randomized controlled trial (RCT) met the inclusion criteria. Fig. 1 illustrates a PRISMA flow diagram.
Fig. 1. Study selection flow diagram. CNKI: China National Knowledge Infrastructure, VIP: Chinese Science Journal Database, RCT: randomized controlled trial.
2. Description of studies
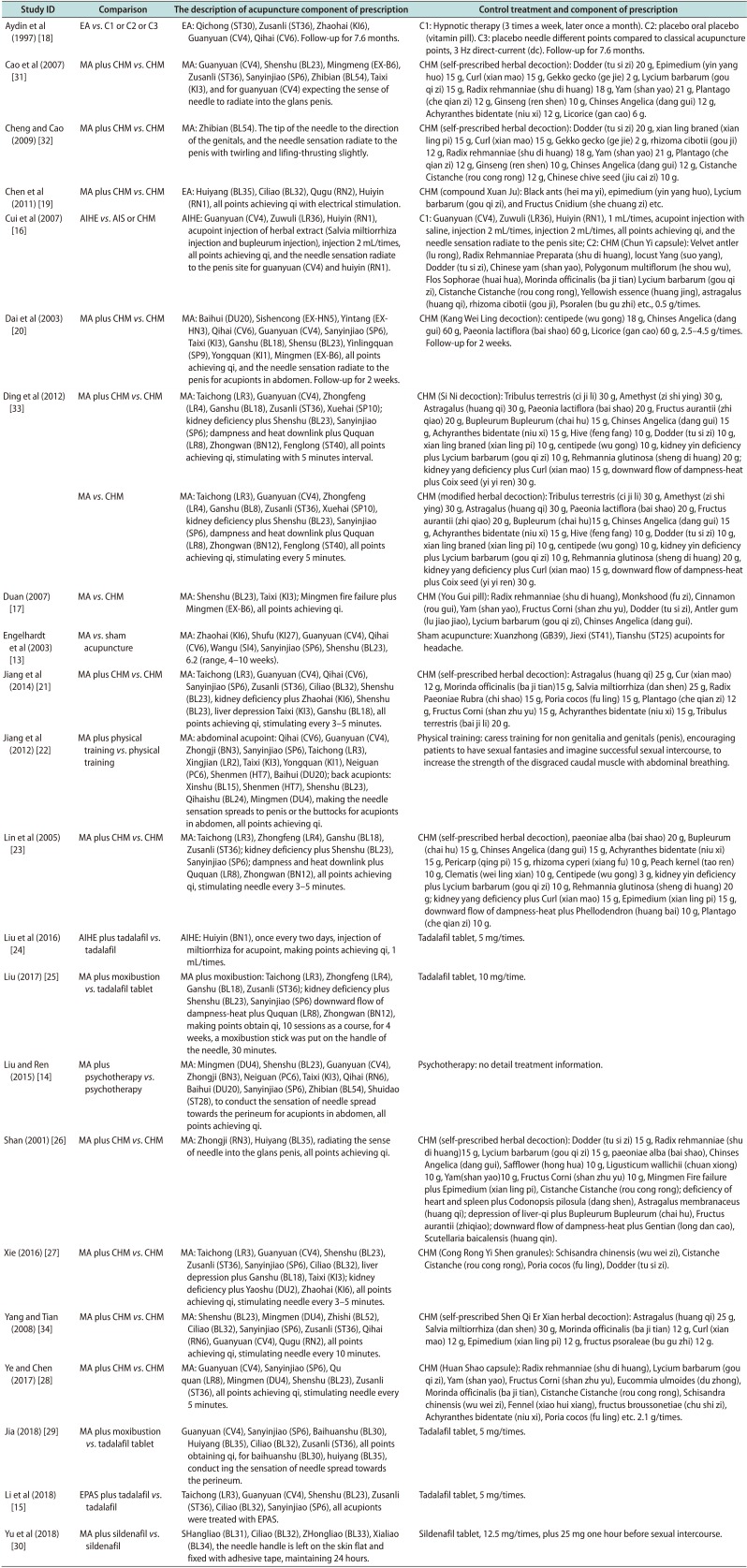
Twenty-two RCTs involving 1,751 participants were enrolled in this review. All of them were conducted in China, and 2 of them published in English. All trials had parallel comparisons, except one [13] that used a crossover design. The sample size varied from 21 to 176 participants, with an average of 35 patients per group. The participants were male adults aged from 20 to 69 years old. The interventions included manual acupuncture with or without moxibustion, electro-acupuncture, and acupuncture point injection. Type of controls included sham acupuncture, herbal medicine, Western medicine, psychological therapy, and hypnosis therapy. The types of ED of twenty-two trials included 2 trials [14,15] were involving ED participants with type-2 diabetes, two trials [16,17] were involving ED participants with psychogenic or arterial supply insufficiency, fourteen trials [13,18,19,20,21,22,23,24,25,26,27,28,29,30] were ED participants with psychogenic, and four trials [31,32,33,34] not reported ED information. The characteristics of included studies are shown in Table 1.
Table 1. Characteristics of 22 the included randomized trials.
| Study ID | Samplea | Age (y)b | Type of ED | Intervention | Control | Duration of treatment (wk)c | Outcome measure |
|---|---|---|---|---|---|---|---|
| Aydin et al (1997) [18] | T: 15, C1: 15, C2: 15, C3: 15 | T: 36.75±10.43, C1: 38.4±10.75, C2: 35.1±10.46, C3: 37.1±11.32 | Psychogenic | EA, 3 Hz direct-current (dc), 20 minutes, twice a week | C1: hypnotic therapy, (3 times a week, later once a month) | T: 6, C1: 6, C2: 6, C3: 6 | Satisfaction of selfassessment rate, adverse effects |
| C2: oral placebo (vitamin pills) | |||||||
| C3: sham acupuncture (non-acupuncture points) 3 Hz dc, 20 minutes, twice a week | |||||||
| Cao et al (2007) [31] | T: 36, C: 18 | T: 25–58, C: 26–59 | NR | MA plus control, 30 minutes, once daily | CHM (self-prescribed herbal decoction), twice daily | 8 | Markedly improved on erectile function rate |
| Cheng and Cao (2009) [32] | T: 32, C: 32 | T: 20–56, C: 21–54 | NR | MA plus control, 30 minutes, once daily | CHM (self-prescribed herbal decoction), twice daily | 4 | Markedly improved on erectile function rate |
| Chen et al (2011) [19] | T: 61, C: 62 | T: 27.62, C: 27.58 | Psychogenic | EA plus control, with density wave, 30 minutes, once daily | CHM (compound Xuan Ju), 3 capsules, 3 times daily | 4 | Satisfaction of selfassessment rate, IIEF-5 scores |
| Cui et al (2007) [16] | T: 50, C1: 50, C2: 50 | T: 20–69, C1: 20–69, C2: 20–69 | Psychogenic or arterial supply insufficiency | Salvia miltiorrhiza injection and bupleurum injection once every 2 days | C1: acupoint injection with saline, once every 2 days | 3 | Markedly improved on erectile function rate, IIEF-5 scores |
| C2: CHM (Chun Yi capsule), 0.5 g/times, 3 times daily | |||||||
| Dai et al (2003) [20] | T: 44, C: 41 | T: 35.75±3.17, C: 36.24±4.12 | Psychogenic | MA plus control, 30 minutes, once daily | CHM (Kang Wei Ling decoction), 2.5–4.5 g/times, twice daily | 4 | Markedly improved on erectile function rate |
| Ding et al (2012) [33] | T1: 88, C: 44 | T: 41.3±8.1, C: 39.1±6.7 | Psychogenic | MA plus control, 30 minutes, once daily | CHM (Si Ni decoction), 3 times daily | 4–8 | Markedly improved on erectile function rate, penile erection angle |
| T2: 44, C: 44 | T: 38.3±7.4, C: 39.1±6.7 | Psychogenic | MA, 30 minutes, once daily | CHM (modified herbal decoction), 3 times daily | 4–8 | Markedly improved on erectile function rate, penile erection angle | |
| Duan (2007) [17] | T: 30, C: 30 | T: 27–55, C: 29–52 | Psychogenic or arterial supply insufficiency | MA, 30 minutes, once daily | CHM (You Gui pill), one pill, twice daily | 4 | Markedly improved on erectile function rate |
| Engelhardt et al (2003) [13] | T: 10, C: 11 | T: 38.9, C: 38.9 | Psychogenic | MA, 20 minutes, once or twice weekly | Sham acupuncture against headache acupoint, 20 minutes, once or twice weekly | 6.2 (4–10) | Satisfaction of selfassessment rate, IIEF scores, adverse effects |
| Jiang et al (2014) [21] | T: 64, C: 64 | T: 21–64, C: 22–65 | Psychogenic | MA plus control, 30 minutes, once daily | CHM (self-prescribed herbal decoction), twice daily | 3–5 | Cure rate, IIEF scores |
| Jiang et al (2012) [22] | T: 51, C: 51 | T: 28.73±3.27, C: 27.67±4.12 | Psychogenic | MA plus control, 30 minutes, once daily | Physical training, 5–15 minutes each time, 12 times from 15 days | 4 | Satisfaction of selfassessment rate |
| Lin et al (2005) [23] | T: 64, C: 32 | T: 38.3±8.1, C: 39.1±6.7 | Psychogenic | MA plus control, 30 minutes, once daily | CHM (self-prescribed herbal decoction), twice daily | 4–8 | Markedly improved on erectile function rate, penile erection angle |
| Liu et al (2016) [24] | T: 32, C: 30 | T: 32, C: 30 | Psychogenic | AIHE plus control, injection 1 mL/time, once every 2 day | Tadalafil tablet, 5 mg/times, once daily | 12 | Cure rate, IIEF scores |
| Liu (2017) [25] | T: 31, C: 31 | T: 42.68±2.35, C: 42.56±2.45 | Psychogenic | MA with moxibustion plus control, MA: 30 minutes, once daily | Tadalafil tablet, 10 mg/times, 3 times daily | 4 | Cure rate, adverse effects |
| Liu and Ren (2015) [14] | T: 30, C: 30 | T: 47.4±6.01, C: 47.8±6.51 | ED with type-2 diabetes | MA plus control, 20 minutes, once daily | Psychotherapy and exercise | 8 | Cure rate, IIEF scores |
| Shan (2001) [26] | T: 60, C: 30 | T: 43.6, C: 43.6 | NR | MA plus control, 20 minutes, once daily | CHM (self-prescribed herbal decoction), twice daily | 12 | Markedly improved on erectile function rate |
| Xie (2016) [27] | T: 40, C: 40 | T: 42.8±8.35, C: 43.19±8.07 | Psychogenic | MA plus control, 30 minutes, once daily | CHM (Cong Rong Yi Shen granules), twice daily | 16 | Cure rate, IIEF scores, adverse effects |
| Yang and Tian (2008) [34] | T: 20, C: 20 | T: 40, C: 40 | NR | MA plus control, 30 minutes, once daily | CHM (self-prescribed Shen Qi Er Xian herbal decoction), twice daily | 4–8 | Satisfaction of selfassessment rate |
| Ye and Chen (2017) [28] | T: 20, C: 20 | T: 34.15±6.43, C: 36.25±5.25 | Psychogenic | MA plus control, 30 minutes, once daily | CHM (Huan Shao capsule), 2.1 g/times, 3 times daily | 4 | Cure rate, IIEF scores |
| Jia (2018) [29] | T: 20, C: 20 | T: 40.15±1.68, C: 40.86±1.91 | Psychogenic | MA with moxibustion plus control, 30 minutes, once daily | Tadalafil tablet, 5 mg/times, once daily | 3 | Cure rate, IIEF scores, adverse effects |
| Li et al (2018) [15] | T: 45, C: 45 | T: 45.26±4.17, C: 46.14±4.51 | ED with type-2 diabetes | EPAS plus control, 4 min/time for one acupoint, total 24 minutes, once daily | Tadalafil tablet, 5 mg/times, once daily | 4 | Cure rate, IIEF scores, adverse effects |
| Yu et al (2018) [30] | T: 20, C: 20 | T: 34.15±6.43, C: 36.25±5.25 | Psychogenic | MA plus control, 30 minutes, once daily | Sildenafil tablet, 12.5 mg/times, twice daily | 6 | Cure rate, IIEF scores |
“Cured” refers to patients who reported that their clinical symptoms disappeared, they had no problem with sexual activity, and/or with International Index of Erectile Function (IIEF-5) score was ≥22 [31]. ‘Markedly improved on erectile function’ refers to that all the three below items were met: the self-report disappearance of clinical symptoms, the erection angle of penis is more than 90 degrees in sexual activity, and the success rate of sexual intercourse is over 75%.
ED: erectile dysfunction, T: treatment group, C: control group, NR: not reported, EA: electro acupuncture, MA: manual acupuncture, AIHE: acupoint injection of herbal extract, EPAS: moderate—frequency electrical pulse acupoint stimulation, CHM: Chinese herbal medicine.
aValues are presented as number only. bValues are presented as mean±standard deviation, range, or mean only. cValues are presented as mean only, range only, or median (range).
3. Description of therapeutic regimen
A summary of acupuncture regimen is provided in Appendix, which contains a list of acupoints, treatment frequency and duration for each trial (Appendix). Participants of included trials accepted acupuncture one session daily for 30 minutes at most of the occasions. The principle of acupuncture treatment was to improve the erectile function and the most common used acupoints and involving meridian were Guan Yuan (CV4, the Ren Meridian, 15 trials), San Yin Jiao (SP6, the Splenic Meridian of Foot-taiyin, 15 trials), Shen Shu (BL23, the Bladder Meridian Foot-taiyang, 13 trials), Zu San Li (ST36, the Stomach Meridian of Foot-yangming, 12 trials), Ming Men (DU4, the Du Meridian of Foot-shaoyin, 8 trials), Tai Chong (LR3, the Liver Meridian of Foot-jueyin, 7 trials), Tai Xi (KI3, the Kidney Meridian of Foot-shaoyin, 7 trials) and Ci Liao (BL32, the Bladder Meridian Foot-taiyang, 5 trials).
4. Assessment of risk of bias
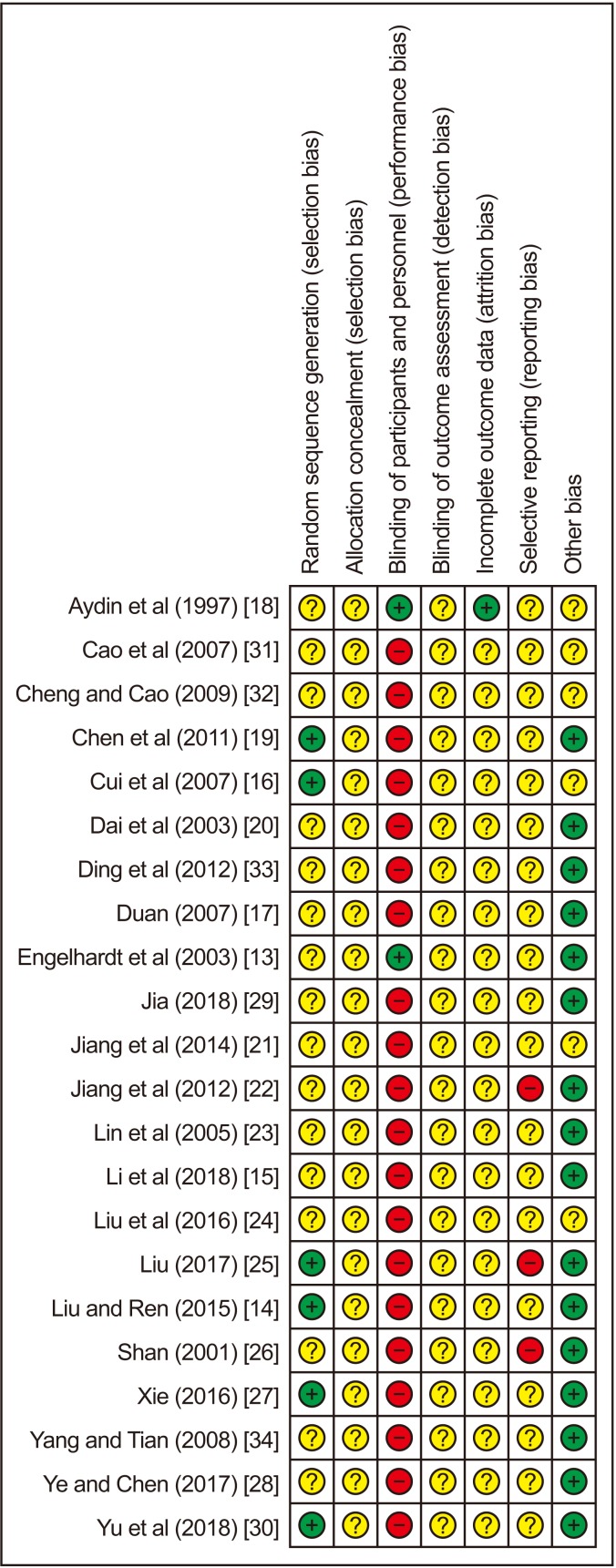
According to the pre-defined approach, 22 trials were found to be either unclear (n=19) or high risk of bias (n=3) due to insufficient or inadequate reporting of the information. Only 6 trials [14,16,19,25,27,30] described that random number table was used to generate the random allocation, thus assessed as having low risk of bias. However, none of the trials reported the allocation concealment. Due to special characteristics of acupuncture, it is difficult for blinding to practitioners, so only two trials [13,18] used sham acupuncture as control and were assessed as low risk of performance bias regarding to the potential adequate blinding method of participants. Risk of detective bias was assessed to be unclear since none of them reported the method of blinding to outcome assessors or statistician. One trial [18] reported number and reasons for drop-out participants, which was regarded low risk of attrition bias. The other 21 trials did not specify the drop-out, and were all evaluated as unclear risk of attrition bias. Twenty trials were assessed as having unclear risk of selective reporting bias due to the absence of protocol; the remaining three trials [22,25,26] were assessed as high risk of selective reporting bias since they all had obvious problems on primary outcome reporting. Other bias was assessed by comparability between groups on baseline data such as age and duration of ED. Only six trials [16,18,21,24,31,32] reported baseline data including age and duration of dysfunction. There is no statistical description of details, so the risk of bias was assessed as unclear. The methodological quality of all the included trials is shown in the Fig. 2.
Fig. 2. Risk of bias summary.
5. Effect estimates
Data analysis was conducted according to the type of comparisons. Table 2 illustrates the details of effect estimates of acupuncture for ED.
Table 2. Effect estimates of included 22 trials.
| Outcome and comparison | Study | Participant | Effect estimate (95% CI) REM | p-value | Study ID |
|---|---|---|---|---|---|
| Electronic acupuncture versus sham acupuncture with electrical stimulation | |||||
| Satisfaction of self-assessment rate | 1 | 60 | RR 1.50 (0.71–3.16) | - | Aydin et al (1997) [18] |
| Manual acupuncture versus sham acupuncture | |||||
| Satisfaction of self-assessment rate | 1 | 60 | RR 7.53 (1.13–50.00) | - | Engelhardt et al (2003) [13] |
| Acupuncture plus tadalafil tablet versus tadalafil tablet | |||||
| Cure rate | 2 | 152 | RR 1.31 (1.00–1.71), I2=0% | 0.48 | Liu et al (2016) [24], Li et al (2018) [15] |
| IIEF-5 score | 2 | 152 | MD 5.38 (4.46–6.29), I2=0% | 0.04 | Liu et al (2016) [24], Li et al (2018) [15] |
| Acupuncture plus sildenafil tablet versus sildenafil tablet | |||||
| Cure rate | 1 | 70 | RR 3.00 (0.65–13.86) | - | Yu et al (2018) [30] |
| IIEF-5 score | 1 | 70 | MD 3.23 (2.12–4.34) | - | Yu et al (2018) [30] |
| Manual acupuncture plus moxibustion versus tadalafil tablet | |||||
| Cure rate | 2 | 102 | RR 1.40 (0.74–2.66), I2=0% | 0.3 | Liu (2017) [25], Jia (2018) [29] |
| IIEF-5 score | 1 | 40 | MD 1.15 (1.37–0.93) | - | Jia (2018) [29] |
| Acupuncture versus herb medicine | |||||
| Markedly improved on erectile function rate | 2 | 148 | RR 1.40 (0.42–4.69), I2=46%, | 0.18 | Ding et al (2012) [33], Duan (2007) [17] |
| IIEF-5 score | 1 | 100 | MD 4.00 (3.66–4.34) | - | Cui et al (2007) [16] |
| Acupuncture point injection of herbal extracts versus oral herbal medicine | |||||
| IIEF-5 score | 1 | 100 | MD 4.0 (3.66–4.34) | - | Cui et al (2007) [16] |
| Markedly improved on erectile function rate | 1 | 100 | RR 1.94 (0.69–5.43) | - | Cui et al (2007) [16] |
| Acupuncture plus herbal medicine versus herbal medicine alone | |||||
| Cure rate | 2 | 168 | RR 1.36 (1.12–1.65), I2=0% | 0.77 | Jiang et al (2014) [21], Ye and Chen (2017) [28] |
| Markedly improved on erectile function rate | 7 | 601 | RR 1.68 (1.31–2.15), I2=0% | 0.90 | Cao et al (2007) [31], Cheng and Cao (2009) [32], Dai et al (2003) [20], Ding et al (2012) [33], Lin et al (2005) [23], Shan (2001) [26], Xie (2016) [27] |
| Satisfaction of self-assessment rate | 2 | 163 | RR 1.67 (0.64–4.36), I2=75% | 0.3 | Chen et al (2011) [19], Yang and Tian (2008) [34] |
| IIEF-5 score | 3 | 331 | No pooled data of trials for I2=95% | <0.05 | Chen et al (2011) [19], Jiang et al (2014) [21], Xie (2016) [27] |
| Erectile angle | 2 | 228 | MD 6.73° (4.10–9.36), I2=0% | 0.94 | Ding et al (2012) [33], Lin et al (2005) [23] |
| Manual acupuncture plus physical therapy versus physical therapy | |||||
| Cure rate | 1 | 102 | RR 1.56 (0.99–2.43) | - | Jiang et al (2012) [22] |
| IIEF-5 score | 1 | 60 | MD 2.90 (2.59–3.21) | - | Liu and Ren (2015) [14] |
CI: confidence interval, REM: random effect model, IIEF: International Index of Erectile Function, RR: risk ratio, MD: mean difference.
1) Acupuncture versus sham acupuncture
One trial [18] compared electro-acupuncture with sham acupuncture (needles inserted into non acupoints), the results showed no difference on the rates of satisfaction and self-assessment between groups (RR, 1.50; 95% CI, 0.71–3.16; 60 participants). Another crossover trial [13] compared manual acupuncture with sham acupuncture (needle insert into irreverent points) showed significant better effect on the rates of satisfaction and self-assessment (RR, 7.53; 95% CI, 1.13–50.00; 60 participants). No other results were reported from these two trials.
2) Acupuncture plus western medicine versus western medicine
Two trials [15,24] compared acupuncture plus tadalafil compared with tadalafil alone. The combination therapy showed better effect on increasing cure rate (RR, 1.31; 95% CI, 1.00–1.71; I2=0%; 2 trials; 152 participants) and IIEF-5 scores (MD, 5.38; 95% CI, 4.46–6.29; I2=0%; 2 trials; 152 participants). Another trial [30] compared acupuncture plus sildenafil compared with sildenafil alone, and the combination therapy showed better effect on increasing IIEF-5 scores (MD, 3.23; 95% CI, 2.12–4.34; 1 trial; 70 participants). There was no significant between-group difference in terms of cure rate (RR, 3.0; 95% CI, 0.65–13.86; 1 trial; 70 participants).
3) Manual acupuncture plus moxibustion versus tadalafil tablet
Two trials [25,29] compared acupuncture plus moxibustion compared with tadalafil alone. There was no significant difference between groups in cure rate (RR, 1.40; 95% CI, 0.74–2.66; 2 trials; I2=0%; 102 participants). No difference between groups was found from one trial [29] in IIEF-5 scores (MD, 1.15; 95% CI, 1.37–0.93; 40 participants).
4) Acupuncture versus herbal medicine
Two trials [17,33] compared acupuncture with herbal medicine and another trial [16] compared acupoint injection of herbal extracts with oral herbal medicine. There was no difference between acupuncture and herbal medicine in terms of markedly improved on erectile function rate (RR, 1.40; 95% CI, 0.42–4.69; I2=46%; 2 trials; 148 participants) [17,33]. However, the acupoint injection of herbal extracts significantly increased the IIEF-5 scores compared to oral herbal medicine (MD, 4.0; 95% CI, 3.66–4.34; 1 trial; 100 participants) [16].
5) Acupuncture plus herbal medicine versus herbal medicine alone
Acupuncture plus herbal medicine was tested in seven trials [20,23,26,27,31,32,33], which showed significant better effect on markedly improved rate on erectile function (as measured by the erection angle and success rate of sexual intercourse) than herbal medicine alone (RR, 1.68; 95% CI, 1.31–2.15; I2=0%; 7 trials; 601 participants).
By excluding three trials [26,31,32] for not reporting types information of ED, remaining four trials only involving ED patients with psychogenic also show that better effect on markedly improved rate on erectile function in combination therapy group (RR, 1.63; 95% CI, 1.21–2.19; I2=0%; 4 trials; 393 participants). The pooled results also showed significantly better effects of the combination therapy on cure rate (RR, 1.36; 95% CI, 1.12–1.65, I2=0%; 2 trials; 168 participants) [21,28] and rigidity (as measured by erectile angle) in sexual intercourse (MD, 6.73 degree; 95% CI, 4.10–9.36; I2=0%; 2 trials; 228 participants) [23,33]. However, no difference was found between groups in the rate of satisfaction and self-assessment (RR, 1.67; 95% CI, 0.64–4.36; I2=75%; 2 trials; 163 participants) [19,34]. Moreover, three trials [19,21,27] favored the combination therapy of acupuncture and herbal medicine in higher IIEF-5 scores (MD, 3.53) to herbal medicine alone, but the results could not be pooled due to high statistical heterogeneity (I2=97%).
6) Acupuncture plus psychological therapy versus psychological therapy
Two trials compared acupuncture plus psychological therapy with psychological therapy alone. One of them [22] found no difference between groups for cure rate (RR, 1.56; 95% CI, 0.99–2.43; 1 trial; 102 participants). Another trial [14] involving 60 ED participants with type-2 diabetes and found the combination therapy appeared to be better on higher IIEF-5 scores (MD, 2.90; 95% CI, 2.59–3.21; 1 trial; 60 participants).
6. Adverse events
Seven trials reported the outcome of adverse events and side effects [13,15,16,18,25,27,29]. One trial [16] reported five cases of dyspepsia, two cases of dizziness and one case of dry mouth from tadalafil in the control group; and one case having facial red and one case of dizziness in acupuncture group. Another one trial [29] reported three patients suffered from needle sticking and pruritus during treatment in acupuncture group; and there were two cases having dry mouth and headache from tadalafil in control group. No adverse effect or side effect was found in the remaining 5 trials.
7. Overall quality of evidence by GRADE
We graded the overall quality of available evidence using GRADE criteria. When combination of acupuncture compared to tadalafil, the quality of evidence for cure rate and IIEF-5 scores was low. In comparison of other interventions and outcome assessments, the quality of evidence was mainly low or very low due to high risk of bias, imprecision (small number of total events or small sample size), or indirectness (outcome measures). Detail of result is show in Table 3.
Table 3. Summary of main findings of RCTs on acupuncture for erectile dysfunction.
| Outcome | No. of participant (No. of RCT) | Quality of the evidence | Relative effect (95% CI) | Anticipated absolute effect | |
|---|---|---|---|---|---|
| Risk with control | Risk difference with intervention (95% CI) | ||||
| Electronic acupuncture versus sham acupuncture | |||||
| Satisfaction of self-assessment rate | 30 (1) | ⨁○○○acd | RR 1.50 (0.71–3.16) | 400 per 1,000 | 200 more per 1,000 (116 more to 864 more) |
| Manual acupuncture versus sham acupuncture | |||||
| Satisfaction of self-assessment rate | 30 (1) | ⨁○○○acd | RR 7.53 (1.13–50.00) | 91 per 1,000 | 594 more per 1,000 (12 more to 1,000 more) |
| Acupuncture plus tadalafil tablet versus tadalafil tablet | |||||
| Cure rate | 152 (2) | ⨁⨁○○ac | RR 1.31 (1.00–1.71) | 467 per 1,000 | 145 more per 1,000 (0 more to 331 more) |
| IIEF-5 score | 152 (2) | ⨁⨁○○ac | N/A | MD 5.38 higher (4.46 higher to 6.29 higher) | |
| Acupuncture versus herb medicine | |||||
| Markedly improved on erectile function rate | 204 (3) | ⨁○○○acd | RR 1.51 (0.96–2.38) | 194 per 1,000 | 99 more per 1,000 (8 fewer to 268 more) |
| IIEF-5 score | 100 (1) | ⨁⨁○○ac | N/A | MD 4 higher (3.66 higher to 4.34 higher) | |
| Acupuncture plus herb medicine versus herb medicine | |||||
| Cure rate | 168 (2) | ⨁⨁○○ac | RR 1.36 (1.12–1.65) | 607 per 1,000 | 219 more per 1,000 (73 more to 395 more) |
| Markedly improved on erectile function rate | 601 (7) | ⨁○○○acd | RR 1.68 (1.31–2.17 | 164 more per 1,000 (75 more to 281 more) | |
| Satisfaction of self-assessment rate | 163 (2) | ⨁○○○abc | RR 1.67 (0.64–4.36) | 463 per 1,000 | 310 more per 1,000 (167 fewer to 1,557 more) |
| IIEF-5 score | 331 (3) | ⨁⨁○○ab | N/A | MD 3.53 higher (0.65 higher to 6.4 higher) | |
| Erectile angle | 228 (2) | ⨁○○○acd | N/A | MD 6.73 higher (4.1 higher to 9.36 higher) | |
GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
RCT: randomized controlled trial, CI: confidence interval, IIEF: International Index of Erectile Function, RR: risk ratio, N/A: not applicable, MD: mean difference.
aRisk of bias: All the trials had high risk of performance bias for not blinding the participants. Methodological quality of these trials was graded as “high risk of bias,” due to the design of comparison (acupuncture therapy versus conventional medications) is difficult to blind personnel and participants. The trials also had unclear risk of performance bias for not reporting blinding the outcome assessor. bInconsistency; There is significantly statistical heterogeneity indicating by I2 value. cImprecision: For dichotomous outcomes, the total number of events is less than 300, for continuous outcomes, the total population size is less than 400 or pooled results included no effects. dIndirectness. For outcomes of satisfaction of self-assessment rate, markedly improved on erectile function rate, and erectile angle. This was not internationally applied outcome measures. ⊕: Very low quality of the evidence; ⊕⊕: Low quality of the evidence.
8. Additional analysis
We tried to do the subgroup analyses according to the types of ED participants, but failed, due to the insufficient number of trials and related information. We could not perform other meaningful sensitivity analysis either.
DISCUSSION
1. Summary of the main results
Twenty-three RCTs were included in this review. The majority of the included studies were having high or unclear risk of bias. Low quality evidence showed there was no difference between acupuncture alone and sham acupuncture, tadalafil, or herbal medicine on symptoms improvement for ED. Combination of acupuncture appeared to show beneficial effect of acupuncture as adjunctive treatment for ED participants with psychogenic or partly with type-2 diabetes, when compared with other conventional therapies (such as tadalafil, psychological therapy or herbal medicine). However, the level of evidence for all outcomes were assessed as “low” or “very low” due to high risk of bias, imprecision or indirectness among included trials. The findings need to be seen as inconclusive due to small sample size and poor methodological quality. Safety of acupuncture was insufficiently reported in the included trials.
2. Comparison with previous studies
There are two published reviews on this topic. One included 3 RCTs involving 183 participants with ED [9], which compared acupuncture with sham acupuncture and psychological therapy respectively. The included RCTs in this review failed to show a specific therapeutic effect of acupuncture, and had methodological flaws as concluded by the authors. And the other recent one only involved Chinese database and included 6 RCTs, control treatment were only involving Chinese herbal medicine and details of treatment information were not clearly specified [10]. In addition, the findings of both two reviews of included trials were not finally pooled due to statistical and clinical heterogeneity, which failed to show a specific therapeutic effect of acupuncture for ED. Compared to the previous two reviews, this update review covered a broader combination of studies, including acupuncture with moxibustion, the acupoint injection and different comparisons, and additional outcome assessments. We performed analyses based on different comparisons and found that although the strength of the evidence was weak, the findings showed there was a potential add-on effect of acupuncture for patients with ED. A total of 31.8% (7/22) of included trials had reported adverse information from acupuncture. This review provided latest evidence of acupuncture for ED.
There are also some limitations of this systematic review. Firstly, the findings are summarized from original included trials with the poor quality and small sample size, which contributed to reduced internal validity of the pooling result. Secondly, it should be point out that although some combination of acupuncture appeared to show beneficial effect of acupuncture as an adjunctive treatment for ED according to the symptom improvement assessed by IIEF-5 scores scale or self-assessment,our analysis was not able to reach a clear recommendation regarding the effect of acupuncture on ED because most studies showed no benefit of acupuncture alone and variable outcome measurements used among studies. It is difficult to draw a conclusion addressing the usage of acupuncture in ED without well-designed trials with a definitive outcome measurement.
3. Implications for practice
According to this review, the main acupuncture points used in the treatment of ED were Guan Yuan (CV4), San Yin Jiao (SP6), Shen Shu (BL23), Zu San Li (ST36), Ming Men (DU4), Tai Chong (LR3), Tai Xi (KI3), and Ci Liao (BL32). The stimulation of these acupionts aimed to achieve the needle sensation (de qi) during treatment. In addition, selecting acupionts of abdominal and lumbosacral regions (such as Guan Yuan [CV4], Ci Liao [BL32]) were expected to spread the sensation to the front of the penis or the perineum during the treatment period as well. TCM theory states that ED is usually caused by kidney yang or qi deficiency, the treating acupionts of Shen Shu (BL23), Zhao Hai (KI6) and San Yin Jiao (SP6) were prescribed accordingly [21,23,27,33]. ED may also be caused by other TCM pathophysiological factors such as “the damp-heat pouring downward”, the treating acupionts of Qu Quan (LR8), Zhong Wan (RN12), and Yin Ling Quan (SP9) were prescribed accordingly [23,29,33]. However, current clinical evidence is insufficient to support its clinical use. Considering potential therapeutic effects of acupuncture, practitioners may consider its use based clinical experience and preference of patients.
4. Implications for research
Considering the variety of acupuncture therapy for ED, future trials should develop optimal acupuncture regimens for ED through Delphi process and/or experts' consensus, validated measurements or tools, such as IIEF-5 scales, to support appropriate interpretation of the findings [11]. In addition, the rational of acupuncture regimen and control should be specified appropriately, and avoid using of comparisons with unclear evidence of effect. To analyze if acupuncture therapy was effective in what kind of ED, the type information of ED participants will be expected to specify clearly in future trials. Furthermore, long-term effect of acupuncture for ED remains unclear. We suggest a follow-up period should be considered in future trials for the assessment of quality of sexual intercourse or sexual life progression.
To improve the quality of trial design and transparent reporting, we strongly suggest future trials should be prospectively registered on international registry platforms, conducted according to “good clinical practice”, and reported according to the Consolidated Standards of Reporting Trials (CONSORT) and Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) statement [35].
CONCLUSIONS
Due to insufficient and weak evidence that was summarized, the potential effect of acupuncture as adjunctive treatment (such as compared with tadalafil, psychological therapy or herbal medicine) mainly on psychogenic ED participants is inconclusive and safety of acupuncture was insufficiently reported. Findings of this review should be confirmed in large, rigorously designed and well-reported trial with a definitive outcome measurement.
ACKNOWLEDGEMENTS
This work is supported by the fund from Beijing University of Chinese Medicine for the Project on Research and Development of Evidence-Based Medicine of Clinical Scientific Research Capacity and International Development in TCM (No.2016-ZXFZJJ-011; No.1000061020008). JP Liu was partially supported by the NCCIH grant (AT001293 with subaward no. 020468C).
Appendix
Components of intervention and control in 22 included trials
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceived of the study: Liu JP.
- Searched literature, identified studies: Yang XY, Li XL.
- Extracted data: Li XL, Jia LY, Lai BY.
- Assessed study quality, analyzed data: Jia LY, Lai BY.
- Conducted the design of the study and drafted the manuscript: Lai BY.
- Revised the manuscript: Cao HJ, Yang GY, Grant S, Wong E, Fei YT.
- Read and approved the final manuscript: all authors.
References
- 1.Jardin A, Wagner G, Khoury S, Giuliano F, Goldstein I, Padma-Nathan H, et al. Recommendations of the 1st International Consultation on Erectile Dysfunction, co-sponsored by the World Health Organization (WHO) Plymouth: Health Publications Ltd.; 2000. [Google Scholar]
- 2.McMahon CG. Erectile dysfunction. Intern Med J. 2014;44:18–26. doi: 10.1111/imj.12325. [DOI] [PubMed] [Google Scholar]
- 3.Kirby M. The circle of lifestyle and erectile dysfunction. Sex Med Rev. 2015;3:169–182. doi: 10.1002/smrj.52. [DOI] [PubMed] [Google Scholar]
- 4.Peak TC, Yafi FA, Sangkum P, Hellstrom WJ. Emerging drugs for the treatment of erectile dysfunction. Expert Opin Emerg Drugs. 2015;20:263–275. doi: 10.1517/14728214.2015.1021682. [DOI] [PubMed] [Google Scholar]
- 5.Tsai MY, Liu CT, Chang CC, Chen SY, Huang ST. Overview of the relevant literature on the possible role of acupuncture in treating male sexual dysfunction. Acupunct Med. 2014;32:406–410. doi: 10.1136/acupmed-2014-010592. [DOI] [PubMed] [Google Scholar]
- 6.Kho HG, Sweep CG, Chen X, Rabsztyn PR, Meuleman EJ. The use of acupuncture in the treatment of erectile dysfunction. Int J Impot Res. 1999;11:41–46. doi: 10.1038/sj.ijir.3900381. [DOI] [PubMed] [Google Scholar]
- 7.Shamloul R, Bella A. Complementary and alternative medicine (CAM) for sexual dysfunction. J Sex Med. 2014;11:1097–1098. doi: 10.1111/jsm.12516. [DOI] [PubMed] [Google Scholar]
- 8.Yin ZH, Ma ZG, Liu CZ. [Study on the mechanism of impotence treated with acupuncture] J Clin Acupunct Moxib. 2004;20:1–2. Chinese. [Google Scholar]
- 9.Cui X, Zhou J, Qin Z, Liu Z. Acupuncture for erectile dysfunction: a systematic review. Biomed Res Int. 2016;2016:2171923. doi: 10.1155/2016/2171923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang R, Qu Y, Wang T, Wan Y, Xu W. Meta-analysis of clinical effectiveness of the acupuncture treatment for erectile dysfunction. Chin J Hum Sex. 2018;27:82–85. [Google Scholar]
- 11.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [Internet] London: The Cochrane Collaboration; 2011. [cited 2018 Oct 6]. Available from: http://handbook-5-1.cochrane.org/ [Google Scholar]
- 13.Engelhardt PF, Daha LK, Zils T, Simak R, König K, Pflüger H. Acupuncture in the treatment of psychogenic erectile dysfunction: first results of a prospective randomized placebo-controlled study. Int J Impot Res. 2003;15:343–346. doi: 10.1038/sj.ijir.3901021. [DOI] [PubMed] [Google Scholar]
- 14.Liu ZX, Ren ZX. Clinical observation on acupuncture in treatment of erectile dysfunction with type 2 diabetes. Cap Food Med. 2015;22:66–67. [Google Scholar]
- 15.Li T, Tan Y, Xie ZP, Wang WR, Xie S. [Clinical efficacy observation on moderate-frequency electrical pulse acupoint stimulation combined with tadalafil in treatment of diabetic men with erectile dysfunction] Chin J Hum Sex. 2018;27:21–23. Chinese. [Google Scholar]
- 16.Cui Y, Feng Y, Chen L, Zhou Y, Yang X, He J, et al. [Randomized and controlled research of Chinese drug acupoint injection therapy for erectile dysfunction] Chin Acupunct Moxib. 2007;12:881–885. Chinese. [PubMed] [Google Scholar]
- 17.Duan XY. Clinical research of Zhen Yang acupuncture therapy in treating impotence [thesis] Changchun: Changchun University of Chinese Medicine; 2007. [Google Scholar]
- 18.Aydin S, Ercan M, Caşkurlu T, Taşçi AI, Karaman I, Odabaş O, et al. Acupuncture and hypnotic suggestions in the treatment of non-organic male sexual dysfunction. Scand J Urol Nephrol. 1997;31:271–274. doi: 10.3109/00365599709070347. [DOI] [PubMed] [Google Scholar]
- 19.Chen ZL, Wang GW, Pan PK. [61 cases of psychological erectile dysfunction treated by electro acupuncture combined with Traditional Chinese Herb Medicine] J Clin Acupunct Moxib. 2011;27:43–44. Chinese. [Google Scholar]
- 20.Dai EQ, Zhang HW, Liu ZQ. [44 cases of impotence treated with acupuncture combined with Traditional Chinese Medicine] Shaanxi J Tradit Chin Med. 2003;24:66–67. Chinese. [Google Scholar]
- 21.Jiang P, Dai N, Yu XH. Therapeutic observation of acupuncture combined with medication for erectile dysfunction. Shanghai J Acupunct Moxib. 2014;33:408–409. [Google Scholar]
- 22.Jiang XP, Liu XY, Li Q. Clinical observation on effect of acupuncture combined with psychological therapy. Chin Foreign Health Abstr. 2012;9:401–402. [Google Scholar]
- 23.Lin XL, Deng PH, Yuan JX. Clinical research on treatment of erectile dysfunction with integrative traditional Chinese medicine and acupuncture. Chin J Hum Sex. 2005;14:8–10. [Google Scholar]
- 24.Liu K, Zeng CH, Ding JY. [Effect of acupoint injection combined with small dose of tadalafil for functional erectile dysfunction] Modern Tradit Chin Med. 2016;36:50–51. Chinese. [Google Scholar]
- 25.Liu XJ. Eight liao points warming needle moxibustion in the treatment of impotence 31 cases. Guangming J Chin Med. 2017;32:2227–2229. [Google Scholar]
- 26.Shan YH. Analysis of curative effects of sexual impotence treated by elongated needle and Chinese herb. Shanghai J Acupunct Moxib. 2001;2:14–15. [Google Scholar]
- 27.Xie DB. Clinical efficacy observation on acupuncture combined with TCM medicine in treatment of male erectile dysfunction. J Hubei College Tradit Chin Med. 2016;18:29–31. [Google Scholar]
- 28.Ye P, Chen SY. [Observation effect of acupuncture combined with Huan Shao capsule for erectile dysfunction] J Pract Tradit Chin Med. 2017;33:21. Chinese. [Google Scholar]
- 29.Jia JB. Clinical observation on the clinical efficacy of acupuncture and moxibustion combined with drug therapy in the treatment of functional ED [thesis] Wulumuqi: Xinjiang Medical University; 2018. [Google Scholar]
- 30.Yu WX, Liu SM, Sun N, Yang LJ, Zhang YY. Clinical observation of press-needling combined with sildenafil in the treatment of erectile dysfunction. J Clin Acupunct Moxib. 2018;34:27–30. [Google Scholar]
- 31.Cao YH, Guo XJ, Cheng YZ. [Treatment of impotence with deficiency of kidney-yang by Chinese medicine and acupuncture] Tradit Chin Med Res. 2007;20:42–43. Chinese. [Google Scholar]
- 32.Cheng YZ, Cao YH. [Acupuncture at the point of zhibian (BL54) plus Traditional Chinese Herb Medicine in treating 32 cases of impotence due to deficiency of kidney yang] Tradit Chin Med Res. 2009;22:61–62. Chinese. [Google Scholar]
- 33.Ding SL, Zhang FG, Yuan ZJ, Li YF, Qin GZ. [Clinical observation on 88 cases of erectile dysfunction treated by acupuncture combined with medicine] Yunnan J Tradit Chin Med Materia Medica. 2012;33:50–51. Chinese. [Google Scholar]
- 34.Yang X, Tian BK. [20 cases of impotence treated with acupuncture combined with Traditional Chinese Herb Medicine] J Clin Acupunct Moxib. 2008;24:27–28. Chinese. [Google Scholar]
- 35.Laine C, Horton R, DeAngelis CD, Drazen JM, Frizelle FA, Godlee F, et al. Clinical trial registration: looking back and moving ahead. N Engl J Med. 2007;356:2734–2736. doi: 10.1056/NEJMe078110. [DOI] [PubMed] [Google Scholar]