Abstract
Background
Alcoholic liver disease (ALD) is the leading cause of liver transplantation (LT). The magnitude and risk factors of post-LT alcohol relapse are not well described. We conducted a meta-analysis to evaluate alcohol relapse rate and its predictors after LT.
Methods
Searches of MEDLINE and SCOPUS identified eligible published studies of alcohol relapse after LT published up to 31 March 2018. Alcohol relapse was defined as any alcohol consumption post-LT, and heavy alcohol relapse was defined as a relapse of alcohol consumption that was associated with a significant harm. Data for the proportion of alcohol relapse was pooled using a meta-analysis for pooling proportion. An odds ratio (OR) of the predictor of alcohol relapse was extracted and pooled using meta-analysis for the pooling risk factor. Data were analyzed using a random effect model if heterogeneity was presented; otherwise, a fixed effect model was applied. The study was registered at PROSPERO (CRD42017052659).
Results
Ninety-two studies with over 8000 cases were recruited for pooling proportion of alcohol relapse. The alcohol relapse rate and heavy alcohol relapse rate after LT during the mean follow-up time of 48.4 ± 24.7 months were 22% (95% confidence interval (CI): 19–25%) and 14% (95%CI: 12–16%). Psychiatric comorbidities (odds ratio (OR) 3.46, 95%CI: 1.87–6.39), pre-transplant abstinence of less than 6 months (OR 2.76, 95%CI: 2.10–3.61), unmarried status (OR 1.84, 95%CI: 1.39–2.43), and smoking (OR 1.72, 95%CI: 1.21–2.46) were associated with alcohol relapse after LT. However, we noticed publication bias of unpublished negative studies and high heterogeneity of results.
Conclusions
Post-transplant alcohol relapse occurred in about one-fifth of patients who underwent alcohol-related LT. Psychiatric comorbidities represented the strongest predictor of alcohol relapse. Psychiatric comorbidities monitoring and pre-LT alcohol abstinence for at least 6 months may decrease alcohol relapse after LT.
Keywords: Liver transplantation, Alcohol, Relapse, Recidivism, Psychiatric comorbidity
Background
Chronic and excessive alcohol consumption is a major cause of death around the world. Regular alcohol consumption can lead to steatosis, steatohepatitis, liver cirrhosis, and hepatocellular carcinoma [1–3]. Liver transplantation (LT) is an extended treatment for end-stage liver diseases; alcoholic liver cirrhosis is the second most frequent cause for LT in the United States and in Europe [4]. Previous studies demonstrated that LT in ALD patients offers an equal survival rate as that in other causes of end-stage liver disease [5]. Furthermore, LT for severe alcoholic hepatitis has a favorable outcome and better survival than medical therapy, but non-surgical therapy remains the standard of care for patients with severe alcoholic hepatitis [6, 7].
The issues of recidivism and disease recurrence remain a concern in LT for alcoholic liver disease. Alcohol relapse negatively impacts outcomes including graft rejection and graft loss from poor medical compliance, post-transplant malignancy, cardiovascular diseases, alcoholic cirrhosis, and decreased long-term survival [8–11]. An abstinence period of at least 6 months before LT is a mandatory selection criterion in most liver transplant centers, but the benefit of such pre-transplant 6 month abstinence remains unclear [8, 12, 13]. Furthermore, there are subsequent reports indicating that an abstinence period of 6 months is not a significant predictive factor for recidivism [14–16]. Careful evaluation of patients with alcoholic liver disease prior to liver transplantation can identify patients with a high risk of alcohol relapse. Modifying the negative factors before LT can prevent alcohol relapse and improve post-transplant survival.
Most of these studies on alcohol recidivism after LT were done in single centers and were reported as descriptive data [16–24]. A previously published meta-analysis study of alcohol relapse after liver transplantation by Dew et al. in 2008 only included published reports on this topic up to 2004 [25]. Several predictive factors have been reported in the last decade [8, 14, 15, 25, 26]. Thus, we performed a systematic review and meta-analysis from the published literature with the following objectives: First, to pool prevalence of alcohol relapse after LT; second, to explore factors associated with alcohol relapse and pool their magnitude of effects in alcoholic liver disease patients with LT.
Methods
This meta-analysis was conducted by following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines, and the review protocol was registered at PROSPERO (CRD42017052659).
Search strategy
Two investigators (L.C. and A.S.) independently conducted a search of databases via MEDLINE and SCOPUS via PubMed and Scopus search engines to identify relevant studies published up to 31 March 2018. The search terms were constructed by domains of patients, intervention/exposure, and outcome. The search strategy is outlined in Table 1. The investigators supplemented the manual reviews of article reference lists to identify studies that had not been included from the initial database search and also performed manual reviews of the relevant studies.
Table 1.
Search terms and search strategy
| Domain | Search term | Search strategy |
|---|---|---|
| P-Patient | - “Alcoholic hepatitis” | #1 |
| - “Alcoholic liver disease” | #2 | |
| - “Alcoholic cirrhosis” | #3 | |
| - “Liver transplantation” | #4 | |
| - “Hepatic transplantation” | #5 | |
| All P | #6 | #1 OR #2 OR #3 AND #4 OR #5 |
| E-Exposure (I-intervention/C-comparator) | - Gender | #7 |
| - Sex | #8 | |
| #9 | #7 OR #8 | |
| - Age | #10 | |
| - “Marital status” | #11 | |
| - Divorced | #12 | |
| #13 | #11 OR #12 | |
| - “Socioeconomic status” | #14 | |
| - Income | #15 | |
| - Education | #16 | |
| #17 | #14 OR #15 OR #16 | |
| - “Alcohol dependence” | #18 | |
| - Depression | #19 | |
| - “Drug use” | #20 | |
| - “Substance use” | #21 | |
| - “Substance abuse” | #22 | |
| - substance | #23 | |
| #24 | #20 OR #21 OR #22 OR #23 | |
| - Family history of alcohol | #25 | |
| - Alcohol abstinence | #26 | |
| - Alcohol cessation | #27 | |
| - Alcohol quit | #28 | |
| - Alcohol stop | #29 | |
| - Alcohol sobriety | #30 | |
| #31 | #26 OR #27 OR #28 OR #29 OR #30 | |
| - Rehabilitation | #32 | |
| - High Risk Alcoholism Relapse | #33 | |
| - HRAR | #34 | |
| #35 | #33 OR #34 | |
| All E | #36 | #9 OR #10 OR #13 OR #17 OR #18 OR #19 OR #24 OR #25 OR #31 OR #32 OR #35 |
| O-Outcome | - Alcohol relapse | #37 |
| - Alcohol recurrence | #38 | |
| - Recidivism | #39 | |
| All O | #40 | #37 OR #38 OR #39 |
| Overall | #6 AND #36 AND #40 |
Study selection
Two investigators (L.C. and A.S.) determined the eligibility of each article for inclusion by screening for relevance on titles and abstracts in parallel. If an eligibility of the study was indeterminable from abstracts, then the full articles were retrieved. The kappa statistic was used to estimate the agreement between the two reviewers [27]. Discordant decisions between the two investigators were advanced to full-text review and resolved by consensus with the third investigator (A.T.).
Inclusion criteria
Studies were eligible if they met all of the following criteria
The study was an observational design including cohort, cross-sectional, or case-control study published as an original article.
The work studied adult patients aged over 18 years with alcoholic liver disease who underwent any type of LT.
Reporting any of the following outcomes: alcohol relapse or alcohol recurrence.
The study assessed association between alcohol relapse and any risk factor including seven domains as follows: demographic data, psychiatric conditions, socioeconomic status, family support, alcohol abstinence, rehabilitation program, and high-risk alcohol relapse (HRAR) scale [28].
Exclusion criteria
Studies were excluded if they met one of the below criteria:
Non-English articles that cannot be translated.
Studies with multi-organ transplantation.
Insufficient data for extraction.
Outcome of interest
The outcome of interest was alcohol relapse and heavy alcohol relapse in patients who underwent LT for alcoholic liver disease. We selected papers on the occurrence of alcohol relapse based on the original authors’ definition of alcohol relapse and heavy relapse and used several methods of relapse assessment such as self-reporting and collateral reporting except for biochemical testing and indirect measures. In general, alcohol relapse was defined as any alcohol consumption post-transplantation, and heavy alcohol relapse was defined as a relapse of alcohol consumption associated with significant medical or social harm [29].
Data extraction
Data obtained from each study was independently extracted by two reviewers (L.C. and A.S.) using a standardized extraction form. Study design, details of the publication, the number of subjects, and baseline characteristics of study populations were extracted including patients with alcohol relapse and predictive factors of alcohol relapse after LT.
Quality and risk of bias assessment
All selected studies were independently reviewed by two investigators (L.C. and A.S.). Disagreements between the two reviewers were resolved by consensus with the third investigator (A.T.). Quality was assessed using a Newcastle-Ottawa Scale for eligible studies including selection, exposure, and comparability of studies on the basis of the design or analysis and assessment of the outcomes (Table 2).
Table 2.
Newcastle-Ottawa quality assessment scale of each included studies
| Author | Year | S1 | S2 | S3 | S4 | C | O1 | O2 | O3 |
|---|---|---|---|---|---|---|---|---|---|
| Starzl TE [30] | 1988 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Bird GLA [12] | 1990 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Kumar S [31] | 1990 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Doffoel M[32] | 1992 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Knechtle SJ [33] | 1992 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Lucey MR [34] | 1992 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Berlakovich GA [35] | 1994 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Howard L [36] | 1994 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Osorio RW [37] | 1994 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Gerhardt TC [38] | 1996 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Tringali RA [39] | 1996 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Tripp LE [40] | 1996 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Zibari GB [41] | 1996 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Anand AC [42] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Coffman KL [43] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Everson G [44] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ||
| Foster PF [24] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Lucey MR [45] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Reeck UH [46] | 1997 | ✹ | ✹ | ✹ | ✹ | ||||
| Shakil AO [47] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Stefanini GF [48] | 1997 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| DiMartini A [49] | 1998 | ✹ | ✹ | ✹ | ✹ | ||||
| Fabrega E [50] | 1998 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Heinemann A [51] | 1998 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Tang H [52] | 1998 | ✹ | ✹ | ✹ | ✹✹ | ✹ | |||
| Conjeevaram HS [53] | 1999 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Gledhill J [54] | 1999 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Newton SE [55] | 1999 | ✹ | ✹ | ✹ | ✹ | ||||
| Pageaux GP [18] | 1999 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Romano DR [56] | 1999 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Abosh D [57] | 2000 | ✹ | ✹ | ✹ | ✹ | ||||
| Berlakovich GA [58] | 2000 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Burra P [59] | 2000 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| DiMartini A [60] | 2000 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Jain A [61] | 2000 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Pereira SP [62] | 2000 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Platz KP [21] | 2000 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Bellamy CO [63] | 2001 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| DiMartini A [64] | 2001 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Gish RG [65] | 2001 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Karman JF [66] | 2001 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Mackie J [15] | 2001 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Tome S [67] | 2002 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Berlakovich GA [68] | 2004 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Jauhar S [14] | 2004 | ✹ | ✹ | ✹ | ✹✹ | ✹ | |||
| Miguet M [69] | 2004 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Björnsson E [20] | 2005 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Cuadrado A [10] | 2005 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| DiMartini A [70] | 2006 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Hwang S [71] | 2006 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Kelly M [72] | 2006 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| De Gottardi A [29] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Dumortier J [73] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Newton SE [74] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Nickels M [75] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Pfitzmann R [8] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Vieira A [76] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Wells JT [77] | 2007 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Gedaly R [23] | 2008 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Immordino G [17] | 2009 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Tandon P [26] | 2009 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Biselli M [78] | 2010 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Chen GH [79] | 2010 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| DiMartini A [80] | 2010 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Karim Z [81] | 2010 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Hartl J [82] | 2011 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Mathurin P [7] | 2011 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Schmeding M [9] | 2011 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Staufer K [83] | 2011 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Faure S [84] | 2012 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Addolorato G [85] | 2013 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Deruytter E [86] | 2013 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Kawaguchi Y [87] | 2013 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Park YH [19] | 2013 | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ||
| Rice JP [88] | 2013 | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ||
| Rodrigue JR [89] | 2013 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Egawa H [16] | 2014 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Grąt M [90] | 2014 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ||
| Piano S [91] | 2014 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | |
| Dumortier J [92] | 2015 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Hasanin M [93] | 2015 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Satapathy SK [94] | 2015 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ||
| Zhou M [28] | 2015 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Askgaard G [95] | 2016 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Hajifathalian K [96] | 2016 | ✹ | ✹ | ✹ | ✹ | ✹ | |||
| Im GY [97] | 2016 | ✹ | ✹ | ✹ | ✹✹ | ✹ | |||
| Kollmann D [98] | 2016 | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ | ✹ |
| Lee BP [99] | 2017 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | |
| Onishi Y [100] | 2017 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
| Wigg AJ [101] | 2017 | ✹ | ✹ | ✹ | ✹ | ✹✹ | ✹ | ✹ | ✹ |
Statistical analysis
The rate of alcohol relapse after LT was estimated along with its 95% confidence interval (CI) for each study. The rate was then pooled across studies using a meta-analysis for pooling proportion [102]. The random effect model was applied if there was heterogeneity between studies; otherwise, a fixed-effect model was applied. An odds ratio (OR) along with 95% CI of risk factor associated with alcohol relapse after LT was estimated for each study. Heterogeneity was assessed using the Cochrane Q test and the I2 statistic. Heterogeneity was present when the Q test was significant (p < 0.1) or I2 ≥ 25%. The sources of heterogeneity were then explored using a meta-regression if the data of the co-variables were available. Subgroup analysis by age, region of study, definition of alcohol relapse, and follow-up time was then performed accordingly. Publication bias was assessed by Egger’s test and a funnel plot. If there was asymmetry suggested from either a funnel plot or Egger’s test, then a contour-enhanced funnel plot was used to explore whether the asymmetry was due to publication bias or heterogeneity. All analyses were performed using STATA software version 14.1. P-values < 0.05 and < 0.10 were considered statistically significant for a two-sided test and one-sided test, respectively.
Results
Search result
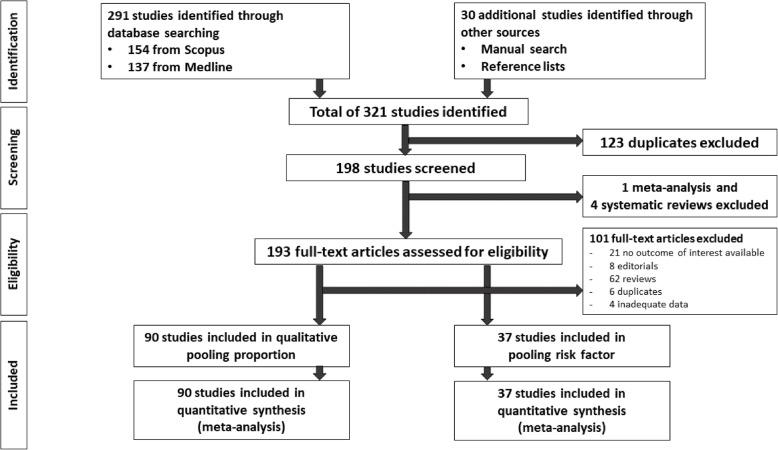
A total of 291 studies were identified from PubMed and Scopus databases plus 30 additional studies from the reference lists (Fig. 1). The title and abstracts were reviewed for 321 studies; 123 duplicated studies, 1 meta-analysis, and 4 systematic reviews were removed [25, 103–106]. The remaining 193 studies were reviewed in full text excluding 101 studies. Of the remaining studies, 90 reported the proportion of alcohol relapse, and 37 studies assessed risk factors of alcohol relapse. The kappa index between the two reviewers (L.C. and A.S.) was 0.96 for data extraction, which indicated very good inter-observer agreement.
Fig. 1.
Protocol flow chart
Study characteristics
Of the 90 studies reporting alcohol relapse, 86 were cohort studies (72 retrospective and 14 prospective cohorts), 2 were cross-sectional studies, and 2 were case-control studies (Table 3). Data for the 86 cohort studies were used for pooling in the incidence of alcohol relapse. Of these, 45 cohorts (40 retrospective and 5 prospective cohorts) were pooled for the proportion of heavy alcohol relapse; 37 studies (43.0%) were from North America, 40 studies (46.5%) were from Europe, 8 studies (9.3%) were from Asia-Pacific, and 1 study (0.1%) was from Brazil.
Table 3.
Main characteristics of the studies included in the meta-analysis
| Author | Year | Type of study | Region of study | Mean age (years) | Number of population | Number of any relapse | Number of heavy relapse | Follow-up time (months) |
|---|---|---|---|---|---|---|---|---|
| Starzl TE [30] | 1988 | Retrospective Cohort | US-Canada | - | 35 | 2 | - | 24 |
| Bird GL [12] | 1990 | Retrospective Cohort | Europe | - | 18 | 4 | - | - |
| Kumar S [31] | 1990 | Retrospective Cohort | US-Canada | 48.2 | 52 | 6 | 2 | 25 |
| Doffoel M [32] | 1992 | Retrospective Cohort | Europe | - | 57 | 19 | - | - |
| Knechtle SJ [33] | 1992 | Case-control | US-Canada | 51 | 32 | 4 | - | - |
| Lucey MR [34] | 1992 | Retrospective Cohort | US-Canada | 44 | 45 | 5 | 2 | 15 |
| Berlakovich GA[35] | 1994 | Retrospective Cohort | Europe | 47.6 | 44 | 14 | 7 | 33 |
| Howard L [36] | 1994 | Retrospective Cohort | Europe | 50 | 20 | 19 | 16 | 34 |
| Osorio RW [37] | 1994 | Prospective Cohort | US-Canada | 47 | 37 | 7 | 3 | 21 |
| Gerhardt TC [38] | 1996 | Retrospective Cohort | US-Canada | 49 | 41 | 20 | 2 | 47 |
| Tringali RA [39] | 1996 | Retrospective Cohort | US-Canada | 47.4 | 58 | 12 | 10 | 28 |
| Tripp LE [40] | 1996 | Retrospective Cohort | US-Canada | 49 | 68 | 9 | 5 | - |
| Zibari GB [41] | 1996 | Retrospective Cohort | US-Canada | 47 | 29 | 2 | - | - |
| Anand AC [42] | 1997 | Retrospective Cohort | Europe | 47.5 | 39 | 5 | - | 25 |
| Coffman KL [43] | 1997 | Prospective Cohort | US-Canada | - | 91 | 18 | - | - |
| Everson G [44] | 1997 | Retrospective Cohort | US-Canada | 53 | 62 | 11 | 6 | 12 |
| Foster PF [24] | 1997 | Retrospective Cohort | US-Canada | 48.6 | 63 | 13 | - | 49.3 |
| Lucey MR [45] | 1997 | Retrospective Cohort | US-Canada | 46 | 50 | 17 | - | 63 |
| Reeck UH [46] | 1997 | Retrospective Cohort | Europe | - | 52 | 6 | - | - |
| Shakil AO [47] | 1997 | Retrospective Cohort | US-Canada | 41 | 8 | 3 | - | - |
| Stefanini GF [48] | 1997 | Retrospective Cohort | Europe | 47 | 11 | 3 | 1 | 48 |
| DiMartini A [49] | 1998 | Retrospective Cohort | US-Canada | 49.5 | 63 | 15 | - | - |
| Fabrega E [50] | 1998 | Retrospective Cohort | Europe | 49 | 44 | 8 | - | 37.8 |
| Heinemann A [51] | 1998 | Retrospective Cohort | Europe | 45.6 | 13 | 4 | - | - |
| Tang H [52] | 1998 | Retrospective Cohort | Europe | 48 | 56 | 28 | 9 | 24 |
| Conjeevaram HS [53] | 1999 | Retrospective Cohort | US-Canada | 47 | 68 | 8 | 8 | - |
| Gledhill J [54] | 1999 | Retrospective Cohort | Europe | 48 | 31 | 7 | - | 13.5 |
| Newton SE [55] | 1999 | Retrospective Cohort | US-Canada | 47 | 122 | 33 | - | 62 |
| Pageaux GP [18] | 1999 | Retrospective Cohort | Europe | 48.8 | 47 | 15 | 5 | 42.1 |
| Romano DR [56] | 1999 | Case-control | Europe | 47.6 | 152 | 7 | - | - |
| Abosh D [57] | 2000 | Retrospective Cohort | US-Canada | 50 | 10 | 5 | 5 | 10 |
| Berlakovich GA [58] | 2000 | Retrospective Cohort | Europe | - | 118 | 15 | - | 53.7 |
| Burra P [59] | 2000 | Prospective Cohort | Asia Pacific | 48 | 34 | 11 | 4 | 40.1 |
| DiMartini A [60] | 2000 | Retrospective Cohort | Europe | 50 | 72 | 4 | 1 | - |
| Jain A [61] | 2000 | Retrospective Cohort | US-Canada | 50.8 | 185 | 37 | 1 | 94 |
| Pereira SP [62] | 2000 | Retrospective Cohort | Europe | 51 | 56 | 28 | 15 | 30 |
| Platz KP [21] | 2000 | Retrospective Cohort | Europe | - | 117 | 30 | - | - |
| Bellamy CO [63] | 2001 | Retrospective Cohort | US-Canada | 53 | 123 | 13 | - | 84 |
| DiMartini A [64] | 2001 | Prospective Cohort | US-Canada | - | 36 | 8 | - | - |
| Gish RG [65] | 2001 | Prospective Cohort | US-Canada | 47 | 61 | 12 | - | 82.8 |
| Karman JF [66] | 2001 | Retrospective Cohort | US-Canada | 49 | 19 | 4 | - | 36 |
| Mackie J [15] | 2001 | Retrospective Cohort | Europe | 51 | 46 | 21 | 3 | 25 |
| Tome S [67] | 2002 | Prospective Cohort | Europe | 51 | 68 | 7 | 2 | 38 |
| Berlakovich GA [68] | 2004 | Case-control | Europe | 51.5 | 44 | 3 | - | 43.5 |
| Jauhar S [14] | 2004 | Retrospective Cohort | US-Canada | 51 | 11 | 17 | 15 | 44.1 |
| Miguet M [69] | 2004 | Prospective Cohort | Europe | 48.7 | 51 | 13 | 9 | 35.7 |
| Björnsson E [20] | 2005 | Retrospective Cohort | Europe | 53 | 93 | 32 | 7 | 31 |
| Cuadrado A [10] | 2005 | Retrospective Cohort | Europe | 48.9 | 54 | 14 | 14 | 99.2 |
| DiMartini A [70] | 2006 | Prospective Cohort | US-Canada | 49.7 | 167 | 70 | 43 | - |
| Hwang S [71] | 2006 | Retrospective Cohort | US-Canada | 50 | 15 | 3 | - | 41 |
| Kelly M [72] | 2006 | Retrospective Cohort | Asia Pacific | 50.1 | 90 | 28 | 18 | 67 |
| De Gottardi A [29] | 2007 | Retrospective Cohort | Europe | 51.3 | 387 | 46 | 46 | 61.2 |
| Dumortier J [73] | 2007 | Retrospective Cohort | Europe | 50 | 305 | 37 | 37 | 63 |
| Newton SE [74] | 2007 | Cross sectional | US-Canada | - | 18 | 4 | - | - |
| Nickels M [75] | 2007 | Retrospective Cohort | US-Canada | 48.8 | 27 | 8 | - | 23.4 |
| Pfitzmann R [8] | 2007 | Retrospective Cohort | Europe | 51.2 | 290 | 56 | 23 | 89 |
| Vieira A [76] | 2007 | Retrospective Cohort | Other(Brazil) | 47 | 17 | 2 | - | 29.6 |
| Wells JT [77] | 2007 | Retrospective Cohort | Europe | 50.3 | 148 | 24 | 20 | 90.5 |
| Gedaly R [23] | 2008 | Retrospective Cohort | US-Canada | 52 | 142 | 27 | - | 41.2 |
| Immordino G [17] | 2009 | Retrospective Cohort | US-Canada | 53.2 | 110 | 13 | - | - |
| Tandon P [26] | 2009 | Retrospective Cohort | US-Canada | 52 | 171 | 41 | 22 | 64.8 |
| Biselli M [78] | 2010 | Retrospective Cohort | Europe | 48 | 49 | 13 | 3 | 58 |
| Chen GH [79] | 2010 | Retrospective Cohort | Asia Pacific | 52.8 | 16 | 1 | - | 32.4 |
| DiMartini A [80] | 2010 | Prospective Cohort | US-Canada | 52 | 208 | 95 | - | - |
| Karim Z [81] | 2010 | Retrospective Cohort | US-Canada | 50.5 | 80 | 8 | 8 | - |
| Hartl J [82] | 2011 | Retrospective Cohort | Europe | 52.5 | 109 | 17 | - | 31 |
| Mathurin P [7] | 2011 | Prospective Cohort | Europe | 47.4 | 26 | 3 | 2 | 20 |
| Schmeding M [9] | 2011 | Retrospective Cohort | Europe | 48.9 | 271 | 73 | 73 | - |
| Staufer K [83] | 2011 | Prospective Cohort | Europe | 53.5 | 141 | 28 | - | - |
| Faure S [84] | 2012 | Retrospective Cohort | Europe | 51 | 206 | 90 | 50 | 81.7 |
| Addolorato G [85] | 2013 | Retrospective Cohort | Europe | 49.4 | 92 | 22 | - | - |
| Deruytter E [86] | 2013 | Retrospective Cohort | Europe | 56 | 108 | 31 | 17 | 55 |
| Kawaguchi Y [87] | 2013 | Retrospective Cohort | Asia Pacific | 52 | 13 | 1 | - | 38 |
| Park YH [19] | 2013 | Retrospective Cohort | Asia Pacific | 52 | 18 | 3 | 2 | 57 |
| Rice JP [88] | 2013 | Retrospective Cohort | US-Canada | 49.3 | 300 | 48 | 16 | 82 |
| Rodrigue JR [107] | 2013 | Retrospective Cohort | US-Canada | 55 | 118 | 40 | 12 | 55 |
| Egawa H [16] | 2014 | Retrospective Cohort | Asia Pacific | 35 | 140 | 32 | 21 | 44 |
| Grąt M [90] | 2014 | Retrospective Cohort | Europe | 46 | 66 | 22 | - | 88.8 |
| Piano S [91] | 2014 | Prospective Cohort | Europe | 60 | 23 | 5 | - | - |
| Dumortier J [92] | 2015 | Retrospective Cohort | Europe | 47.2 | 712 | 128 | 128 | 63 |
| Hasanin M [93] | 2015 | Cross-sectional | US-Canada | - | 45 | 8 | - | - |
| Satapathy SK [94] | 2015 | Retrospective Cohort | US-Canada | 54 | 148 | 16 | 16 | 112.8 |
| Zhou M [28] | 2015 | Retrospective Cohort | US-Canada | 54.2 | 35 | 6 | - | - |
| Askgaard G [95] | 2016 | Retrospective Cohort | Europe | 54 | 156 | 35 | 35 | - |
| Hajifathalian K [96] | 2016 | Prospective Cohort | Europe | 56 | 19 | 4 | - | 40.8 |
| Im GY [97] | 2016 | Retrospective Cohort | US-Canada | 41 | 9 | 2 | 1 | 24.5 |
| Kollmann D [98] | 2016 | Retrospective Cohort | Europe | - | 382 | 16 | - | 73 |
| Lee BP [99] | 2017 | Retrospective Cohort | US-Canada | 51.4 | 31 | 11 | 7 | 19.2 |
| Onishi Y [100] | 2017 | Retrospective Cohort | Asia Pacific | 46 | 7 | 1 | - | 60 |
| Wigg AJ [101] | 2017 | Retrospective Cohort | Asia Pacific | 50 | 87 | 18 | 14 | 52 |
The incidence of alcohol relapse
The characteristics of the studies and the data on alcohol relapse rates are detailed in Table 3. A total of 86 cohort studies with 8061 patients reported incidences of alcohol relapse at any time after LT. The mean age of patients ranged from 35 to 60 years, and the mean follow-up time was 10 to 112 months. The alcohol relapse rate varied across studies with a range of 4 to 95% with an I2 of 90.7%. A random effect model was applied and yielded the pooled alcohol relapse rate of 22% (95% CI: 19–25%) during the mean follow-up time of 48.4 ± 24.7 months. The rate of heavy alcohol relapse varied markedly across studies with an I2 of 85% and pooled rate of 14% (95%CI: 12–16%).
Pooled risk factors of alcohol relapse
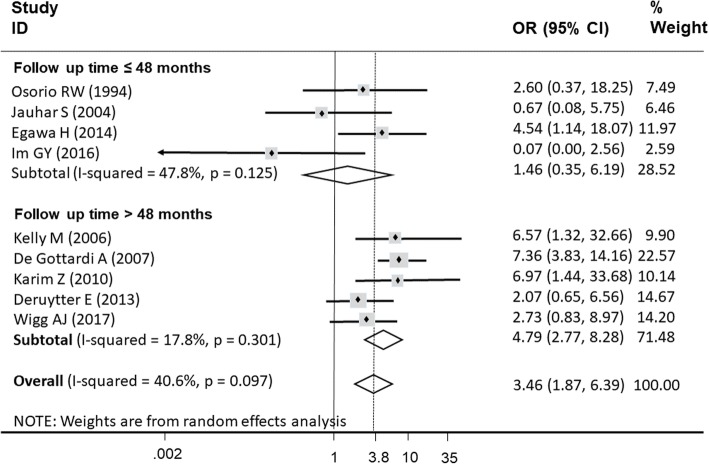
The effects of all of the risk factors on alcohol relapse after LT that were classified by demographic, risk behavior, social, and comorbidity factors; these were pooled in 37 cohort studies (Table 4). The results of pooling these effects are summarized in Table 5. The results showed that psychiatric comorbidities, pre-transplant abstinence less than 6 months, being unmarried, and smoking were significantly associated with alcohol relapse after LT with corresponding pooled ORs of 3.46 (95% CI: 1.87–6.39), 2.76 (95%CI: 2.10–3.61), 1.84 (95%CI: 1.39–2.43), and 1.72 (95%CI: 1.21–2.46), respectively. In addition, the I2 ranged from 0 to 40.6%, with the highest I2 in psychiatric comorbidities.
Table 4.
Summary of the included studies reported risk factors in the meta-analysis
| Author | Year | Demographic factors | Risk behavior factors | Social factors | Comorbidity |
|---|---|---|---|---|---|
| Kumar S [31] | 1990 | - | - | Abstinence < 6months | - |
| Osorio RW [37] | 1994 |
Male Unmarried Unemployed |
Substance use |
Abstinence < 6months Rehabilitation |
Psychiatric disease |
| Gerhardt TC [38] | 1996 | - | - | Abstinence < 6months | - |
| Tringali RA [39] | 1996 | - | - | Abstinence < 6months | - |
| Foster PF [24] | 1997 | Family history of alcohol use | Substance use |
Abstinence < 6months Rehabilitation |
- |
| Lucey MR [45] | 1997 | Male | - | Abstinence < 6months | - |
| Shakil AO [47] | 1997 | Male | - | - | - |
| Tang H [52] | 1998 | Male | - | - | - |
| Conjeevaram HS [53] | 1999 | Male | - | - | - |
| Newton SE [55] | 1999 | - | Substance use | - | - |
| Pageaux GP [18] | 1999 |
Male Unmarried Unemployed |
- | Abstinence < 6months | - |
| Burra P [59] | 2000 |
Unmarried Family history of alcohol use |
Substance use Alcohol dependence |
Rehabilitation | - |
| Jain A [61] | 2000 | - | - |
Abstinence < 6months Rehabilitation |
- |
| Mackie J [15] | 2001 |
Male Unmarried Lack of social support Low SES Family history of alcohol use |
Smoking | Abstinence < 6months | - |
| Jauhar S [14] | 2004 |
Male Unmarried Unemployed |
Substance use |
Abstinence < 6months Rehabilitation |
Psychiatric disease |
| Björnsson E [20] | 2005 | - | - | Rehabilitation | - |
| Cuadrado A [10] | 2005 | Male | - | - | |
| Hwang S [71] | 2006 | - | - | Abstinence < 6months | - |
| Kelly M [72] | 2006 |
Unmarried Lack of social support Unemployed |
Substance use | Abstinence < 6months |
Psychiatric disease Depression |
| De Gottardi A [29] | 2007 |
Age < 50 years Male Unmarried Low SES Unemployed |
High HRAR | Abstinence < 6months | Psychiatric disease |
| Nickels M [75] | 2007 |
Age < 50 years Male |
Alcohol dependence | - | Depression |
| Pfitzmann R [8] | 2007 |
Age < 50 years Male Unmarried |
- | Abstinence < 6months | - |
| Karim Z [81] | 2010 |
Age < 50 years Male Unmarried Low SES Unemployed |
Smoking Substance use |
Abstinence < 6months Rehabilitation |
Psychiatric disease |
| Hartl J [82] | 2011 | - | Smoking |
Abstinence < 6months Rehabilitation |
- |
| Addolorato G [85] | 2013 | - | - | Rehabilitation | - |
| Deruytter E [86] | 2013 |
Age < 50 years Male Unmarried Unemployed Family history of alcohol use |
Smoking Alcohol dependence |
- | Psychiatric disease |
| Kawaguchi Y [87] | 2013 | Male | High HRAR | - | - |
| Park YH [19] | 2013 | Male | - | Abstinence < 6months | - |
| Rice JP [88] | 2013 | Male | - | - | - |
| Rodrigue JR [89] | 2013 | Lack of social support | Smoking |
Abstinence < 6months Rehabilitation |
- |
| Egawa H [16] | 2014 |
Male Unmarried Lack of social support Unemployed |
Smoking High HRAR |
Abstinence < 6months | Psychiatric disease |
| Zhou M [28] | 2015 | - | High HRAR | - | - |
| Askgaard G [95] | 2016 |
Male Unmarried Unemployed Family history of alcohol use |
Smoking Alcohol dependence |
Abstinence < 6 months | Depression |
| Im GY [97] | 2016 |
Male Unmarried Family history of alcohol use |
Smoking | - | Psychiatric disease |
| Lee BP [99] | 2017 | Male | - | - | - |
| Onishi Y [100] | 2017 |
Age < 50 years Male |
- | - | - |
| Wigg AJ [101] | 2017 |
Male Unmarried Lack of social support Unemployed Family history of alcohol use |
Smoking Substance use |
Rehabilitation | Psychiatric disease |
Table 5.
Pooled risk factors of alcohol relapse
| Factors | N | OR | 95%CI | Pooling method | I2 | Egger test (P-value) |
|---|---|---|---|---|---|---|
| Demographic factors | ||||||
| Age < 50 years | 6 | 1.16 | 0.43 - 3.15 | Random effect | 75.2 | 0.55 |
| Sex (male) | 23 | 0.89 | 0.69 - 1.11 | Fixed effect | 21.7 | 0.43 |
| Unmarried | 14 | 1.84 | 1.39 - 2.43 | Fixed effect | 14.6 | 0.57 |
| Lack of social support | 5 | 1.78 | 0.72 - 4.38 | Random effect | 49.5 | 0.18 |
| Low SES | 3 | 0.99 | 0.15 - 6.50 | Random effect | 86.3 | 0.28 |
| Unemployed | 10 | 1.33 | 0.93 - 1.89 | Fixed effect | 7.7 | 0.74 |
| Family history of alcohol use | 7 | 1.49 | 0.94 - 2.36 | Fixed effect | 23.0 | 0.50 |
| Risk behavior factors | ||||||
| Smoking | 9 | 1.72 | 1.21 - 2.46 | Fixed effect | 0 | 0.69 |
| Substance use | 8 | 1.06 | 0.48 - 2.34 | Random effect | 58.5 | 0.71 |
| Alcohol dependence | 4 | 1.22 | 0.43 - 3.40 | Random effect | 61.8 | 0.15 |
| High HRAR | 4 | 2.93 | 0.30 - 28.64 | Random effect | 79.6 | 0.18 |
| Social factors | ||||||
| Abstinence < 6 months | 20 | 2.76 | 2.10 - 3.61 | Fixed effect | 18.1 | 0.02 |
| Rehabilitation program | 11 | 1.10 | 0.59 - 2.04 | Random effect | 67 | 0.71 |
| Comorbidity | ||||||
| Psychiatric disease | 9 | 3.46 | 1.87 - 6.39 | Random effect | 40.6 | 0.02 |
| Depression | 3 | 2.13 | 0.49 - 9.25 | Random effect | 54.4 | 0.60 |
N Number, OR Odds ratio, CI Confidence interval, I2 I2statistics, SES Socioeconomic status, HRAR High-risk alcohol relapse scale
Subgroup analysis
Subgroup analysis by age (≤ 50 years or > 50 years), regions of studies (Europe, North America, Asia Pacific and Brazil), definition of alcohol relapse (only report or report combining with biochemical testing), and follow-up time (≤ 4 years or > 4 years) was performed to explore the potential cause of heterogeneity of pooled rates of alcohol relapse and heavy alcohol relapse. Likewise, the subgroup analysis was performed with psychiatric comorbidities to identify the factor associated with alcohol relapse with the highest risk and heterogeneity. Subgroup analyses showed no significant difference in all analyses of alcohol relapse and heavy alcohol relapse rates except for one analysis of psychiatric comorbidities. Patients with psychiatric comorbidities who had longer follow-up time (> 4 years) had an increased risk of alcohol relapse versus those with a shorter follow-up time (≤ 4 years) (Fig. 2).
Fig. 2.
Subgroup analysis of duration of follow-up time in psychiatric comorbidity factor
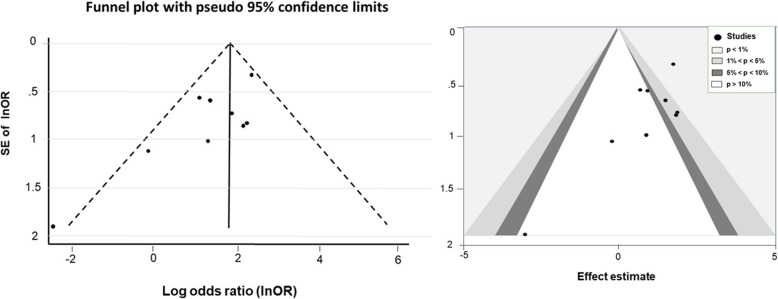
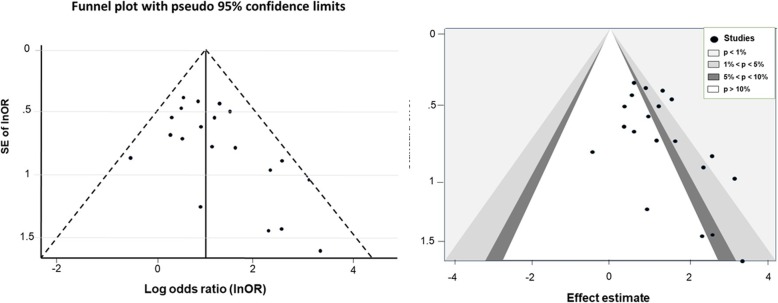
Publication bias
The Egger test showed no evidence of publication bias among the studies, and the shape of the funnel plots was symmetrical in all analyses except for psychiatric comorbidities (Fig. 3) and abstinence less than 6 months (Fig. 4). The studies that reported less than 6 months of abstinence were both non-significant and significant leading to a contour-enhanced funnel plot; thus, asymmetry may not be due to either publication bias or heterogeneity. The studies with negative effect of psychiatric co-morbidities and abstinence less than 6 months were not reported.
Fig. 3.
Funnel plot and contour-enhanced funnel plot for psychiatric comorbidities
Fig. 4.
Funnel plot and contour-enhanced funnel plot for less than 6 months of pre-transplant abstinence
Discussion
Alcohol relapse after LT remains an ethical issue in LT for alcoholic liver disease due to its harmful and negative impacts on liver grafts. One meta-analysis and four systemic reviews of alcoholic liver disease in LT patient were published earlier [25, 103–106]. The well-designed meta-analysis of rate and risk factors of alcohol relapse by Dew et al. in 2008 included 54 studies published between 1983 and 2005 [25]. A systematic review by Rustard et al. in 2015 selected only articles of the risk factors of alcohol relapse [103]. A systematic review by McCallum et al. in 2006 included only studies that were associated with psychosocial criteria [106]. Bravata et al. performed a systematic review of alcohol relapse and evaluated only the association between employment aspect and alcohol relapse [105]. One systematic review focused on neither alcohol relapse rate nor risk factor [104]. Our study is a systematic review and meta-analysis of all published studies up to 2018, which aimed to estimate post-LT alcohol relapse rate and its predictive factors. To date, the current study is the most extensive meta-analysis of alcohol relapse in LT patients.
Our study demonstrated that any alcohol relapse and heavy alcohol relapse rates were as high as 22 and 14% during the mean follow-up time of 48.4 ± 24.7 months, respectively. The literature on alcohol relapse post-transplantation has reported a wide range of alcohol relapse rates, which might be due to different definitions of alcohol relapse. Dew et al. reported that the average rate for alcohol relapse after LT was 5.6 cases per 100 patients per year for any alcohol relapse and 2.5 cases per 100 patients per year for heavy alcohol relapse [25]. The authors suggested that a significant proportion of patients who returned to any alcohol drinking then became heavy drinkers, which led to a significant harm to LT recipients [25].
In our study, the most significant risk factors of relapse were psychiatric comorbidities followed by pre-transplant alcohol abstinence less than 6 months, being unmarried, and smoking. Four of the nine studies reported that psychiatric conditions had a link with alcohol relapse [16, 29, 72, 81]. The finding was consistent with the previous meta-analysis [25]. The study identified 3 of the 12 psychosocial variables associated with any alcohol relapse: < 6 months abstinence prior to transplant, poor social support, and a family history of alcohol abuse or dependence [25]. We found that 9 of the 20 studies revealed that alcohol abstinence less than 6 months was associated with alcohol relapse [8, 18, 29, 37, 81, 82, 95, 107, 108]. Our study confirms the validity of using the 6-month rule of alcohol abstinence as a criterion for pre-transplant selection in patients with ALD; this is consistent with the previous meta-analysis study [25].
A systematic review of large prospective studies focusing on risk factors for alcohol relapse following LT has also suggested that a shorter length of pre-transplant sobriety was a significant predictor of alcohol relapse [103]. However, the 6-month rule cannot be applied in LT for patients with severe acute alcoholic hepatitis whose condition is not allowed to wait until 6 months. LT in this group of patients remains a controversial issue in many transplant centers. The current data do not suggest that LT in patients with severe alcoholic hepatitis leads to more alcohol relapse [109]. Therefore, 6 months of alcohol abstinence may not reliably predict post-LT alcohol relapse. Other risk factors were psychiatric comorbidities, a high score on the HRAR scale, and a diagnosis of alcohol dependence [103]. Scoring systems to predict alcohol relapse after LT such as HRAR and the ARRA were proposed for use, but they have never been validated by well-designed studies.
In this study, psychiatric co-morbidities and pre-transplant abstinence less than 6 months were strong predictive factors of alcohol relapse with some publication bias against negative studies. Psychiatric comorbidities were the strongest risk factor in this study but with high heterogeneity. Interestingly, subsequent subgroup analysis showed that longer follow-up times led to an increased impact of psychiatric comorbidities on any alcohol relapse. The psychiatric comorbidities defined in enrolled studies included all psychiatric conditions that could cause impaired daily functioning, i.e. anxiety, schizophrenia, and personality disorders. In this study, we analyzed three cohort studies that reported depression separately because depression is a known risk factor associated with alcoholic drinking. We found that depression was not a significant factor in alcohol relapse (OR = 3; 95%CI 0.49–9.25).
Clinical practice has changed considerably since the first studies that recruited in 1988. The differences in the definition of alcohol relapse and heavy relapse as well as a lack of objective means of documenting alcohol use in these studies are limitations. Furthermore, heavy alcohol relapse was defined only in some studies (Table 2). Including unpublished studies may solve this problem. The absence of negative studies of psychiatric co-morbidities and abstinence less than 6 months likely caused publication bias. However, this attempt cannot guarantee a reasonably low heterogeneity after including unpublished studies.
Conclusions
We demonstrated the pooled rates of any alcohol relapse and heavy alcohol relapse post-LT. Furthermore, we identified predictive factors of alcohol relapse after LT to be used during the selection process of LT candidates. With respect to the prevention of alcohol relapse post-LT, alcohol abstinence of at least 6 months, appropriate screening and care of psychiatric co-morbidities, and smoking cessation should be incorporated in pre-transplant selection and management periods. Careful selection of LT candidates and modifying pre-transplant risk factors of alcohol relapse has the potential to reduce alcohol relapse after LT.
Acknowledgments
We would like to thank the statistical team of Section for Clinical Epidemiology and Biostatistics, Faculty of Medicine, Ramathibodi Hospital for statistical analysis assistance.
Abbreviations
- ALD
Alcoholic liver disease
- CI
Confidence interval
- HRAR
High-Risk Alcohol Relapse
- LT
Liver transplantation
- OR
Odds ratio
Authors’ contributions
LC participated in the design of the study, interpreted the data and wrote the manuscript. NY performed in the design of the study, interpreted the data and reviewed the manuscript. AT participated in the design of the study, statistical analysis, interpretation of the data and reviewed of the manuscript. AS participated in the design of the study, interpreted the data and wrote and edited the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by the Gastroenterological Association of Thailand that does not have its role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lancharat Chuncharunee, Email: Lancharat@gmail.com.
Noriyo Yamashiki, Email: nyamashiki-gi@umin.ac.jp.
Ammarin Thakkinstian, Email: Ammarin.tha@mahidol.ac.th.
Abhasnee Sobhonslidsuk, Phone: +66 2-201-1304, Email: abhasnee.sob@mahidol.ac.th.
References
- 1.Singal AK, Chaha KS, Rasheed K, Anand BS. Liver transplantation in alcoholic liver disease current status and controversies. World J Gastroenterol. 2013;19:5953–5963. doi: 10.3748/wjg.v19.i36.5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Testino G, Burra P, Bonino F, Piani F, Sumberaz A, Peressutti R, et al. Acute alcoholic hepatitis, end stage alcoholic liver disease and liver transplantation: an Italian position statement. World J Gastroenterol. 2014;20:14642–14651. doi: 10.3748/wjg.v20.i40.14642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Testino G, Leone S, Borro P. Alcohol and hepatocellular carcinoma: a review and a point of view. World J Gastroenterol. 2014;20:15943–15954. doi: 10.3748/wjg.v20.i43.15943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallegos-Orozco JF, Charlton MR. Alcoholic Liver Disease and Liver Transplantation. Clin Liver Dis. 2016;20:521–534. doi: 10.1016/j.cld.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Neuberger J, Tang H. Relapse after transplantation: European studies. Liver Transpl Surg. 1997;3:275–279. doi: 10.1002/lt.500030313. [DOI] [PubMed] [Google Scholar]
- 6.Burra P, Senzolo M, Adam R, Delvart V, Karam V, Germani G, et al. Liver transplantation for alcoholic liver disease in Europe: a study from the ELTR (European Liver Transplant Registry) Am J Transplant. 2010;10:138–148. doi: 10.1111/j.1600-6143.2009.02869.x. [DOI] [PubMed] [Google Scholar]
- 7.Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, Durand F, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365:1790–1800. doi: 10.1056/NEJMoa1105703. [DOI] [PubMed] [Google Scholar]
- 8.Pfitzmann R, Schwenzer J, Rayes N, Seehofer D, Neuhaus R, Nussler NC. Long-term survival and predictors of relapse after orthotopic liver transplantation for alcoholic liver disease. Liver Transpl. 2007;13:197–205. doi: 10.1002/lt.20934. [DOI] [PubMed] [Google Scholar]
- 9.Schmeding M, Heidenhain C, Neuhaus R, Neuhaus P, Neumann UP. Liver transplantation for alcohol-related cirrhosis: a single centre long-term clinical and histological follow-up. Dig Dis Sci. 2011;56:236–243. doi: 10.1007/s10620-010-1281-7. [DOI] [PubMed] [Google Scholar]
- 10.Cuadrado Antonio, Fábrega Emilio, Casafont Fernando, Pons-Romero Fernando. Alcohol recidivism impairs long-term patient survival after orthotopic liver transplantation for alcoholic liver disease. Liver Transplantation. 2005;11(4):420–426. doi: 10.1002/lt.20386. [DOI] [PubMed] [Google Scholar]
- 11.Kawaguchi Y, Sugawara Y, Akamatsu N, Kaneko J, Tanaka T, Tamura S, et al. Perceptions of post-transplant recidivism in liver transplantation for alcoholic liver disease. World J Hepatol. 2014;6:812–817. doi: 10.4254/wjh.v6.i11.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bird GL, O'Grady JG, Harvey FA, Calne RY, Williams R. Liver transplantation in patients with alcoholic cirrhosis: selection criteria and rates of survival and relapse. BMJ. 1990;301:15–17. doi: 10.1136/bmj.301.6742.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shawcross DL, O'Grady JG. The 6-month abstinence rule in liver transplantation. Lancet. 2010;376:216–217. doi: 10.1016/S0140-6736(10)60487-4. [DOI] [PubMed] [Google Scholar]
- 14.Jauhar S, Talwalkar JA, Schneekloth T, Jowsey S, Wiesner RH, Menon KV. Analysis of factors that predict alcohol relapse following liver transplantation. Liver Transpl. 2004;10:408–411. doi: 10.1002/lt.20086. [DOI] [PubMed] [Google Scholar]
- 15.Mackie J, Groves K, Hoyle A, Garcia C, Garcia R, Gunson B, et al. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transpl. 2001;7:418–427. doi: 10.1053/jlts.2001.23789. [DOI] [PubMed] [Google Scholar]
- 16.Egawa H, Nishimura K, Teramukai S, Yamamoto M, Umeshita K, Furukawa H, et al. Risk factors for alcohol relapse after liver transplantation for alcoholic cirrhosis in Japan. Liver Transpl. 2014;20:298–310. doi: 10.1002/lt.23797. [DOI] [PubMed] [Google Scholar]
- 17.Immordino G, Gelli M, Ferrante R, Ferrari C, Piaggio F, Ghinolfi D, et al. Alcohol abstinence and orthotopic liver transplantation in alcoholic liver cirrhosis. Transplant Proc. 2009;41:1253–1255. doi: 10.1016/j.transproceed.2009.03.092. [DOI] [PubMed] [Google Scholar]
- 18.Pageaux GP, Michel J, Coste V, Perney P, Possoz P, Perrigault PF, et al. Alcoholic cirrhosis is a good indication for liver transplantation, even for cases of recidivism. Gut. 1999;45:421–426. doi: 10.1136/gut.45.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park YH, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Living donor liver transplantation for patients with alcoholic liver disease. Korean J Hepatobiliary Pancreat Surg. 2013;17:14–20. doi: 10.14701/kjhbps.2013.17.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bjornsson E, Olsson J, Rydell A, Fredriksson K, Eriksson C, Sjoberg C, et al. Long-term follow-up of patients with alcoholic liver disease after liver transplantation in Sweden: impact of structured management on recidivism. Scand J Gastroenterol. 2005;40:206–216. doi: 10.1080/00365520410009591. [DOI] [PubMed] [Google Scholar]
- 21.Platz KP, Mueller AR, Spree E, Schumacher G, Nussler NC, Rayes N, et al. Liver transplantation for alcoholic cirrhosis. Transpl Int. 2000;13(Suppl 1):S127–S130. doi: 10.1111/j.1432-2277.2000.tb02000.x. [DOI] [PubMed] [Google Scholar]
- 22.Egawa H, Ueda Y, Kawagishi N, Yagi T, Kimura H, Ichida T. Significance of pretransplant abstinence on harmful alcohol relapse after liver transplantation for alcoholic cirrhosis in Japan. Hepatol Res. 2014;44:E428–E436. doi: 10.1111/hepr.12334. [DOI] [PubMed] [Google Scholar]
- 23.Gedaly R, McHugh PP, Johnston TD, Jeon H, Koch A, Clifford TM, et al. Predictors of relapse to alcohol and illicit drugs after liver transplantation for alcoholic liver disease. Transplantation. 2008;86:1090–1095. doi: 10.1097/TP.0b013e3181872710. [DOI] [PubMed] [Google Scholar]
- 24.Foster PF, Fabrega F, Karademir S, Sankary HN, Mital D, Williams JW. Prediction of abstinence from ethanol in alcoholic recipients following liver transplantation. Hepatology. 1997;25:1469–1477. doi: 10.1002/hep.510250627. [DOI] [PubMed] [Google Scholar]
- 25.Dew MA, DiMartini AF, Steel J, De Vito DA, Myaskovsky L, Unruh M, et al. Meta-analysis of risk for relapse to substance use after transplantation of the liver or other solid organs. Liver Transpl. 2008;14:159–172. doi: 10.1002/lt.21278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tandon P, Goodman KJ, Ma MM, Wong WW, Mason AL, Meeberg G, et al. A shorter duration of pre-transplant abstinence predicts problem drinking after liver transplantation. Am J Gastroenterol. 2009;104:1700–1706. doi: 10.1038/ajg.2009.226. [DOI] [PubMed] [Google Scholar]
- 27.Duvoux C, Villamil F, Renner EL, Grazi GL, Firpi RJ, Pageaux G, et al. Sustained virological response to antiviral therapy in a randomized trial of cyclosporine versus tacrolimus in liver transplant patients with recurrent hepatitis C infection. Ann Transplant. 2015;20:25–35. doi: 10.12659/AOT.892032. [DOI] [PubMed] [Google Scholar]
- 28.Zhou M, Wagner LM, Diflo T, Naegle M. Implementation of the High-Risk Alcoholism Relapse Scale in a Liver Transplant Clinic. Gastroenterol Nurs. 2015;38:447–454. doi: 10.1097/SGA.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 29.De Gottardi A, Spahr L, Gelez P, Morard I, Mentha G, Guillaud O, et al. A simple score for predicting alcohol relapse after liver transplantation: results from 387 patients over 15 years. Arch Intern Med. 2007;167:1183–1188. doi: 10.1001/archinte.167.11.1183. [DOI] [PubMed] [Google Scholar]
- 30.Starzl TE, Van Thiel D, Tzakis AG, Iwatsuki S, Todo S, Marsh JW, et al. Orthotopic liver transplantation for alcoholic cirrhosis. JAMA. 1988;260:2542–2544. doi: 10.1001/jama.1988.03410170090040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar S, Stauber RE, Gavaler JS, Basista MH, Dindzans VJ, Schade RR, et al. Orthotopic liver transplantation for alcoholic liver disease. Hepatology. 1990;11:159–164. doi: 10.1002/hep.1840110202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doffoel M. Can the risk of recurrent alcohol abuse after liver transplantation for alcoholic cirrhosis be predicted? Gastroenterol Clin Biol. 2004;28:843–844. doi: 10.1016/S0399-8320(04)95145-7. [DOI] [PubMed] [Google Scholar]
- 33.Knechtle SJ, Fleming MF, Barry KL, Steen D, Pirsch JD, Hafez GR, et al. Liver transplantation for alcoholic liver disease. Surgery. 1992;112:694–701. [PubMed] [Google Scholar]
- 34.Lucey MR, Beresford TP. Alcoholic liver disease: to transplant or not to transplant? Alcohol Alcohol. 1992;27:103–108. [PubMed] [Google Scholar]
- 35.Berlakovich GA, Steininger R, Herbst F, Barlan M, Mittlbock M, Muhlbacher F. Efficacy of liver transplantation for alcoholic cirrhosis with respect to recidivism and compliance. Transplantation. 1994;58:560–565. doi: 10.1097/00007890-199409150-00006. [DOI] [PubMed] [Google Scholar]
- 36.Howard L, Fahy T. Liver transplantation for alcoholic liver disease. Br J Psychiatry. 1997;171:497–500. doi: 10.1192/bjp.171.6.497. [DOI] [PubMed] [Google Scholar]
- 37.Osorio RW, Ascher NL, Avery M, Bacchetti P, Roberts JP, Lake JR. Predicting recidivism after orthotopic liver transplantation for alcoholic liver disease. Hepatology. 1994;20:105–110. doi: 10.1016/0270-9139(94)90141-4. [DOI] [PubMed] [Google Scholar]
- 38.Gerhardt TC, Goldstein RM, Urschel HC, Tripp LE, Levy MF, Husberg BS, et al. Alcohol use following liver transplantation for alcoholic cirrhosis. Transplantation. 1996;62:1060–1063. doi: 10.1097/00007890-199610270-00005. [DOI] [PubMed] [Google Scholar]
- 39.Tringali RA, Trzepacz PT, DiMartini A, Dew MA. Assessment and follow-up of alcohol-dependent liver transplantation patients. A clinical cohort. Gen Hosp Psychiatry. 1996;18:70s–77s. doi: 10.1016/S0163-8343(96)00083-7. [DOI] [PubMed] [Google Scholar]
- 40.Tripp LE, Clemons JR, Goldstein RR, McCarthy Stewart L. Drinking patterns in liver transplant recipients. Psychosomatics. 1996;37:249–253. doi: 10.1016/S0033-3182(96)71563-3. [DOI] [PubMed] [Google Scholar]
- 41.Zibari GB, Edwin D, Wall L, Diehl A, Fair J, Burdick J, et al. Liver transplantation for alcoholic liver disease. Clin Transplant. 1996;10:676–679. [PubMed] [Google Scholar]
- 42.Anand AC, Ferraz-Neto BH, Nightingale P, Mirza DF, White AC, McMaster P, et al. Liver transplantation for alcoholic liver disease: evaluation of a selection protocol. Hepatology. 1997;25:1478–1484. doi: 10.1002/hep.510250628. [DOI] [PubMed] [Google Scholar]
- 43.Coffman KL, Hoffman A, Sher L, Rojter S, Vierling J, Makowka L. Treatment of the postoperative alcoholic liver transplant recipient with other addictions. Liver Transpl Surg. 1997;3:322–327. doi: 10.1002/lt.500030320. [DOI] [PubMed] [Google Scholar]
- 44.Everson G, Bharadhwaj G, House R, Talamantes M, Bilir B, Shrestha R, et al. Long-term follow-up of patients with alcoholic liver disease who underwent hepatic transplantation. Liver Transpl Surg. 1997;3:263–274. doi: 10.1002/lt.500030312. [DOI] [PubMed] [Google Scholar]
- 45.Lucey MR, Carr K, Beresford TP, Fisher LR, Shieck V, Brown KA, et al. Alcohol use after liver transplantation in alcoholics: a clinical cohort follow-up study. Hepatology. 1997;25:1223–1227. doi: 10.1002/hep.510250526. [DOI] [PubMed] [Google Scholar]
- 46.Reeck UH, Egerer G, Otto G, Hoffmann W, Arnold JC. Theilmann L et al: [Rehabilitation of patients with alcoholic liver cirrhosis after orthotopic liver transplantation: a 7-year follow-up] Rehabilitation (Stuttg) 1997;36:116–120. [PubMed] [Google Scholar]
- 47.Shakil AO, Pinna A, Demetris J, Lee RG, Fung JJ, Rakela J. Survival and quality of life after liver transplantation for acute alcoholic hepatitis. Liver Transpl Surg. 1997;3:240–244. [PubMed] [Google Scholar]
- 48.Stefanini GF, Biselli M, Grazi GL, Iovine E, Moscatello MR, Marsigli L, et al. Orthotopic liver transplantation for alcoholic liver disease: rates of survival, complications and relapse. Hepatogastroenterology. 1997;44:1356–1359. [PubMed] [Google Scholar]
- 49.DiMartini A, Jain A, Irish W, Fitzgerald MG, Fung J. Outcome of liver transplantation in critically ill patients with alcoholic cirrhosis: survival according to medical variables and sobriety. Transplantation. 1998;66:298–302. doi: 10.1097/00007890-199808150-00004. [DOI] [PubMed] [Google Scholar]
- 50.Fabrega E, Crespo J, Casafont F. De las Heras G, de la Pena J, Pons-Romero F: Alcoholic recidivism after liver transplantation for alcoholic cirrhosis. J Clin Gastroenterol. 1998;26:204–206. doi: 10.1097/00004836-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 51.Heinemann A, Sterneck M, Kuhlencordt R, Rogiers X, Schulz KH, Queen B, et al. Carbohydrate-deficient transferrin: diagnostic efficiency among patients with end-stage liver disease before and after liver transplantation. Alcohol Clin Exp Res. 1998;22:1806–1812. doi: 10.1097/00000374-199811000-00028. [DOI] [PubMed] [Google Scholar]
- 52.Tang H, Boulton R, Gunson B, Hubscher S, Neuberger J. Patterns of alcohol consumption after liver transplantation. Gut. 1998;43:140–145. doi: 10.1136/gut.43.1.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Conjeevaram HS, Hart J, Lissoos TW, Schiano TD, Dasgupta K, Befeler AS, et al. Rapidly progressive liver injury and fatal alcoholic hepatitis occurring after liver transplantation in alcoholic patients. Transplantation. 1999;67:1562–1568. doi: 10.1097/00007890-199906270-00010. [DOI] [PubMed] [Google Scholar]
- 54.Gledhill J, Burroughs A, Rolles K, Davidson B, Blizard B, Lloyd G. Psychiatric and social outcome following liver transplantation for alcoholic liver disease: a controlled study. J Psychosom Res. 1999;46:359–368. doi: 10.1016/S0022-3999(98)00123-8. [DOI] [PubMed] [Google Scholar]
- 55.Newton SE. Recidivism and return to work posttransplant. Recipients with substance abuse histories. J Subst Abuse Treat. 1999;17:103–108. doi: 10.1016/S0740-5472(98)00059-2. [DOI] [PubMed] [Google Scholar]
- 56.Romano DR, Jimenez C, Rodriguez F, Loinaz C, Colina F, Urena MA, et al. Orthotopic liver transplantation in alcoholic liver cirrhosis. Transplant Proc. 1999;31:2491–2493. doi: 10.1016/S0041-1345(99)00432-7. [DOI] [PubMed] [Google Scholar]
- 57.Abosh D, Rosser B, Kaita K, Bazylewski R, Minuk G. Outcomes following liver transplantation for patients with alcohol- versus nonalcohol-induced liver disease. Can J Gastroenterol. 2000;14:851–855. doi: 10.1155/2000/867514. [DOI] [PubMed] [Google Scholar]
- 58.Berlakovich GA, Langer F, Freundorfer E, Windhager T, Rockenschaub S, Sporn E, et al. General compliance after liver transplantation for alcoholic cirrhosis. Transpl Int. 2000;13:129–135. doi: 10.1007/s001470050298. [DOI] [PubMed] [Google Scholar]
- 59.Burra P, Mioni D, Cillo U, Fagiuoli S, Senzolo M, Naccarato R, et al. Long-term medical and psycho-social evaluation of patients undergoing orthotopic liver transplantation for alcoholic liver disease. Transpl Int. 2000;13(Suppl 1):S174–S178. doi: 10.1111/j.1432-2277.2000.tb02014.x. [DOI] [PubMed] [Google Scholar]
- 60.DiMartini A, Magill J, Fitzgerald MG, Jain A, Irish W, Khera G, et al. Use of a high-risk alcohol relapse scale in evaluating liver transplant candidates. Alcohol Clin Exp Res. 2000;24:1198–1201. doi: 10.1111/j.1530-0277.2000.tb02083.x. [DOI] [PubMed] [Google Scholar]
- 61.Jain A, DiMartini A, Kashyap R, Youk A, Rohal S, Fung J. Long-term follow-up after liver transplantation for alcoholic liver disease under tacrolimus. Transplantation. 2000;70:1335–1342. doi: 10.1097/00007890-200011150-00012. [DOI] [PubMed] [Google Scholar]
- 62.Pereira SP, Howard LM, Muiesan P, Rela M, Heaton N, Williams R. Quality of life after liver transplantation for alcoholic liver disease. Liver Transpl. 2000;6:762–768. doi: 10.1053/jlts.2000.19030. [DOI] [PubMed] [Google Scholar]
- 63.Bellamy CO, DiMartini AM, Ruppert K, Jain A, Dodson F, Torbenson M, et al. Liver transplantation for alcoholic cirrhosis: long term follow-up and impact of disease recurrence. Transplantation. 2001;72:619–626. doi: 10.1097/00007890-200108270-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.DiMartini A, Day N, Dew MA, Lane T, Fitzgerald MG, Magill J, et al. Alcohol use following liver transplantation: a comparison of follow-up methods. Psychosomatics. 2001;42:55–62. doi: 10.1176/appi.psy.42.1.55. [DOI] [PubMed] [Google Scholar]
- 65.Gish RG, Lee A, Brooks L, Leung J, Lau JY, Moore DH., 2nd Long-term follow-up of patients diagnosed with alcohol dependence or alcohol abuse who were evaluated for liver transplantation. Liver Transpl. 2001;7:581–587. doi: 10.1053/jlts.2001.25455. [DOI] [PubMed] [Google Scholar]
- 66.Karman JF, Sileri P, Kamuda D, Cicalese L, Rastellini C, Wiley TE, et al. Risk factors for failure to meet listing requirements in liver transplant candidates with alcoholic cirrhosis. Transplantation. 2001;71:1210–1213. doi: 10.1097/00007890-200105150-00005. [DOI] [PubMed] [Google Scholar]
- 67.Tome S, Martinez-Rey C, Gonzalez-Quintela A, Gude F, Brage A, Otero E, et al. Influence of superimposed alcoholic hepatitis on the outcome of liver transplantation for end-stage alcoholic liver disease. J Hepatol. 2002;36:793–798. doi: 10.1016/S0168-8278(02)00047-8. [DOI] [PubMed] [Google Scholar]
- 68.Berlakovich GA, Soliman T, Freundorfer E, Windhager T, Bodingbauer M, Wamser P, et al. Pretransplant screening of sobriety with carbohydrate-deficient transferrin in patients suffering from alcoholic cirrhosis. Transpl Int. 2004;17:617–621. doi: 10.1111/j.1432-2277.2004.tb00395.x. [DOI] [PubMed] [Google Scholar]
- 69.Miguet M, Monnet E, Vanlemmens C, Gache P, Messner M, Hruskovsky S, et al. Predictive factors of alcohol relapse after orthotopic liver transplantation for alcoholic liver disease. Gastroenterol Clin Biol. 2004;28:845–851. doi: 10.1016/S0399-8320(04)95146-9. [DOI] [PubMed] [Google Scholar]
- 70.DiMartini A, Day N, Dew MA, Javed L, Fitzgerald MG, Jain A, et al. Alcohol consumption patterns and predictors of use following liver transplantation for alcoholic liver disease. Liver Transpl. 2006;12:813–820. doi: 10.1002/lt.20688. [DOI] [PubMed] [Google Scholar]
- 71.Hwang S, Lee SG, Kim KK, Kim KH, Ahn CS, Moon DB, et al. Efficacy of 6-month pretransplant abstinence for patients with alcoholic liver disease undergoing living donor liver transplantation. Transplant Proc. 2006;38:2937–2940. doi: 10.1016/j.transproceed.2006.08.139. [DOI] [PubMed] [Google Scholar]
- 72.Kelly M, Chick J, Gribble R, Gleeson M, Holton M, Winstanley J, et al. Predictors of relapse to harmful alcohol after orthotopic liver transplantation. Alcohol Alcohol. 2006;41:278–283. doi: 10.1093/alcalc/agh257. [DOI] [PubMed] [Google Scholar]
- 73.Dumortier J, Guillaud O, Adham M, Boucaud C, Delafosse B, Bouffard Y, et al. Negative impact of de novo malignancies rather than alcohol relapse on survival after liver transplantation for alcoholic cirrhosis: a retrospective analysis of 305 patients in a single center. Am J Gastroenterol. 2007;102:1032–1041. doi: 10.1111/j.1572-0241.2007.01079.x. [DOI] [PubMed] [Google Scholar]
- 74.Newton SE. Alcohol relapse and its relationship to the lived experience of adult liver transplant recipients. Gastroenterol Nurs. 2007;30:37–42. doi: 10.1097/00001610-200701000-00004. [DOI] [PubMed] [Google Scholar]
- 75.Nickels M, Jain A, Sharma R, Orloff M, Tsoulfas G, Kashyap R, et al. Polysubstance abuse in liver transplant patients and its impact on survival outcome. Exp Clin Transplant. 2007;5:680–685. [PubMed] [Google Scholar]
- 76.Vieira A, Rolim EG, Capua A, Jr, Szutan LA. Relapse of alcohol consumption in liver transplant candidates. Risk factor analysis. Arq Gastroenterol. 2007;44:205–209. doi: 10.1590/S0004-28032007000300005. [DOI] [PubMed] [Google Scholar]
- 77.Wells JT, Said A, Agni R, Tome S, Hughes S, Dureja P, et al. The impact of acute alcoholic hepatitis in the explanted recipient liver on outcome after liver transplantation. Liver Transpl. 2007;13:1728–1735. doi: 10.1002/lt.21298. [DOI] [PubMed] [Google Scholar]
- 78.Biselli M, Gramenzi A, Del Gaudio M, Ravaioli M, Vitale G, Gitto S, et al. Long term follow-up and outcome of liver transplantation for alcoholic liver disease: a single center case-control study. J Clin Gastroenterol. 2010;44:52–57. doi: 10.1097/MCG.0b013e3181a390a8. [DOI] [PubMed] [Google Scholar]
- 79.Chen GH, Yang Y, Lu MQ, Cai CJ, Zhang Q, Zhang YC, et al. Liver transplantation for end-stage alcoholic liver disease: a single-center experience from mainland China. Alcohol. 2010;44:217–221. doi: 10.1016/j.alcohol.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 80.DiMartini A, Dew MA, Day N, Fitzgerald MG, Jones BL, deVera ME, et al. Trajectories of alcohol consumption following liver transplantation. Am J Transplant. 2010;10:2305–2312. doi: 10.1111/j.1600-6143.2010.03232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Karim Z, Intaraprasong P, Scudamore CH, Erb SR, Soos JG, Cheung E, et al. Predictors of relapse to significant alcohol drinking after liver transplantation. Can J Gastroenterol. 2010;24:245–250. doi: 10.1155/2010/596246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hartl J, Scherer MN, Loss M, Schnitzbauer A, Farkas S, Baier L, et al. Strong predictors for alcohol recidivism after liver transplantation: non-acceptance of the alcohol problem and abstinence of <3 months. Scand J Gastroenterol. 2011;46:1257–1266. doi: 10.3109/00365521.2011.603160. [DOI] [PubMed] [Google Scholar]
- 83.Staufer K, Andresen H, Vettorazzi E, Tobias N, Nashan B, Sterneck M. Urinary ethyl glucuronide as a novel screening tool in patients pre- and post-liver transplantation improves detection of alcohol consumption. Hepatology. 2011;54:1640–1649. doi: 10.1002/hep.24596. [DOI] [PubMed] [Google Scholar]
- 84.Faure S, Herrero A, Jung B, Duny Y, Daures JP, Mura T, et al. Excessive alcohol consumption after liver transplantation impacts on long-term survival, whatever the primary indication. J Hepatol. 2012;57:306–312. doi: 10.1016/j.jhep.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 85.Addolorato G, Mirijello A, Leggio L, Ferrulli A, D'Angelo C, Vassallo G, et al. Liver transplantation in alcoholic patients: impact of an alcohol addiction unit within a liver transplant center. Alcohol Clin Exp Res. 2013;37:1601–1608. doi: 10.1111/acer.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Deruytter E, Van Steenkiste C, Trepo E, Geerts A, Van Vlierberghe H, Berrevoet F, et al. Liver transplantation for alcoholic liver disease: a retrospective analysis of recidivism, survival and risk factors predisposing to alcohol relapse. Acta Gastroenterol Belg. 2013;76:282–290. [PubMed] [Google Scholar]
- 87.Kawaguchi Y, Sugawara Y, Yamashiki N, Kaneko J, Tamura S, Aoki T, et al. Role of 6-month abstinence rule in living donor liver transplantation for patients with alcoholic liver disease. Hepatol Res. 2013;43:1169–1174. doi: 10.1111/hepr.12065. [DOI] [PubMed] [Google Scholar]
- 88.Rice JP, Eickhoff J, Agni R, Ghufran A, Brahmbhatt R, Lucey MR. Abusive drinking after liver transplantation is associated with allograft loss and advanced allograft fibrosis. Liver Transpl. 2013;19:1377–1386. doi: 10.1002/lt.23762. [DOI] [PubMed] [Google Scholar]
- 89.Rodrigue JR, Hanto DW, Curry MP. Substance abuse treatment and its association with relapse to alcohol use after liver transplantation. Liver Transplantation. 2013;19:1387–1395. doi: 10.1002/lt.23747. [DOI] [PubMed] [Google Scholar]
- 90.Grat M, Lewandowski Z, Grat K, Wronka KM, Krasnodebski M, Barski K, et al. Negative outcomes after liver transplantation in patients with alcoholic liver disease beyond the fifth post-transplant year. Clin Transplant. 2014;28:1112–1120. doi: 10.1111/ctr.12427. [DOI] [PubMed] [Google Scholar]
- 91.Piano S, Marchioro L, Gola E, Rosi S, Morando F, Cavallin M, et al. Assessment of alcohol consumption in liver transplant candidates and recipients: the best combination of the tools available. Liver Transpl. 2014;20:815–822. doi: 10.1002/lt.23881. [DOI] [PubMed] [Google Scholar]
- 92.Dumortier J, Dharancy S, Cannesson A, Lassailly G, Rolland B, Pruvot FR, et al. Recurrent alcoholic cirrhosis in severe alcoholic relapse after liver transplantation: a frequent and serious complication. Am J Gastroenterol. 2015;110:1160–1166. doi: 10.1038/ajg.2015.204. [DOI] [PubMed] [Google Scholar]
- 93.Hasanin M, Dubay DA, McGuire BM, Schiano T, Singal AK. Liver transplantation for alcoholic hepatitis: A survey of liver transplant centers. Liver Transpl. 2015;21:1449–1452. doi: 10.1002/lt.24208. [DOI] [PubMed] [Google Scholar]
- 94.Satapathy SK, Eason JD, Nair S, Dryn O, Sylvestre PB, Kocak M, et al. Recidivism in Liver Transplant Recipients With Alcoholic Liver Disease: Analysis of Demographic, Psychosocial, and Histology Features. Exp Clin Transplant. 2015;13:430–440. [PubMed] [Google Scholar]
- 95.Askgaard G, Tolstrup JS, Gerds TA, Hamberg O, Zierau L, Kjaer MS. Predictors of heavy drinking after liver transplantation for alcoholic liver disease in Denmark (1990-2013): a nationwide study with competing risks analyses. Scand J Gastroenterol. 2016;51:225–235. doi: 10.3109/00365521.2015.1067903. [DOI] [PubMed] [Google Scholar]
- 96.Hajifathalian K, Humberson A, Hanouneh MA, Barnes DS, Arora Z, Zein NN, et al. Ohio solid organ transplantation consortium criteria for liver transplantation in patients with alcoholic liver disease. World J Hepatol. 2016;8:1149–1154. doi: 10.4254/wjh.v8.i27.1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Im GY, Kim-Schluger L, Shenoy A, Schubert E, Goel A, Friedman SL, et al. Early Liver Transplantation for Severe Alcoholic Hepatitis in the United States--A Single-Center Experience. Am J Transplant. 2016;16:841–849. doi: 10.1111/ajt.13586. [DOI] [PubMed] [Google Scholar]
- 98.Kollmann D, Rasoul-Rockenschaub S, Steiner I, Freundorfer E, Gyori GP, Silberhumer G, et al. Good outcome after liver transplantation for ALD without a 6 months abstinence rule prior to transplantation including post-transplant CDT monitoring for alcohol relapse assessment - a retrospective study. Transpl Int. 2016;29:559–567. doi: 10.1111/tri.12756. [DOI] [PubMed] [Google Scholar]
- 99.Lee BP, Chen PH, Haugen C, Hernaez R, Gurakar A, Philosophe B, et al. Three-year Results of a Pilot Program in Early Liver Transplantation for Severe Alcoholic Hepatitis. Ann Surg. 2017;265:20–29. doi: 10.1097/SLA.0000000000001831. [DOI] [PubMed] [Google Scholar]
- 100.Onishi Y, Kimura H, Hori T, Kishi S, Kamei H, Kurata N, et al. Risk of alcohol use relapse after liver transplantation for alcoholic liver disease. World J Gastroenterol. 2017;23:869–875. doi: 10.3748/wjg.v23.i5.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wigg AJ, Mangira D, Chen JW, Woodman RW. Outcomes and predictors of harmful relapse following liver transplantation for alcoholic liver disease in an Australian population. Intern Med J. 2017;47:656–663. doi: 10.1111/imj.13431. [DOI] [PubMed] [Google Scholar]
- 102.Anothaisintawee T, Rattanasiri S, Ingsathit A, Attia J, Thakkinstian A. Prevalence of chronic kidney disease: a systematic review and meta-analysis. Clin Nephrol. 2009;71:244–254. doi: 10.5414/CNP71244. [DOI] [PubMed] [Google Scholar]
- 103.Rustad JK, Stern TA, Prabhakar M, Musselman D. Risk factors for alcohol relapse following orthotopic liver transplantation: a systematic review. Psychosomatics. 2015;56:21–35. doi: 10.1016/j.psym.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 104.Singal AK, Kodali S, Vucovich LA, Darley-Usmar V, Schiano TD. Diagnosis and Treatment of Alcoholic Hepatitis: A Systematic Review. Alcohol Clin Exp Res. 2016;40:1390–1402. doi: 10.1111/acer.13108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bravata DM, Olkin I, Barnato AE, Keeffe EB, Owens DK. Employment and alcohol use after liver transplantation for alcoholic and nonalcoholic liver disease: a systematic review. Liver Transpl. 2001;7:191–203. doi: 10.1053/jlts.2001.22326. [DOI] [PubMed] [Google Scholar]
- 106.McCallum S, Masterton G. Liver transplantation for alcoholic liver disease: a systematic review of psychosocial selection criteria. Alcohol Alcohol. 2006;41:358–363. doi: 10.1093/alcalc/agl033. [DOI] [PubMed] [Google Scholar]
- 107.Rodrigue JR, Hanto DW, Curry MP. Substance abuse treatment and its association with relapse to alcohol use after liver transplantation. Liver Transpl. 2013;19:1387–1395. doi: 10.1002/lt.23747. [DOI] [PubMed] [Google Scholar]
- 108.Im GY, Cameron AM, Lucey MR. Liver transplantation for alcoholic hepatitis. J Hepatol. 2019;70:328–334. doi: 10.1016/j.jhep.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 109.Lim J, Curry MP, Sundaram V. Risk factors and outcomes associated with alcohol relapse after liver transplantation. World J Hepatol. 2017;9:771–780. doi: 10.4254/wjh.v9.i17.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.