This cohort study investigates the association between intensification of antihypertensive regimens at hospital discharge and clinical outcomes after discharge.
Key Points
Question
What is the association between the intensification of an antihypertensive regimen at hospital discharge and clinical outcomes of hospitalized older adults with hypertension?
Findings
In this national cohort study of 4056 propensity-matched older adults with hypertension who were hospitalized for noncardiac conditions, discharge with intensified antihypertensive regimens was associated with an increased risk of readmissions and serious adverse events within 30 days and was not associated with a reduction in cardiovascular events or blood pressure at 1 year.
Meaning
The findings suggest that intensification of antihypertensives at hospital discharge is associated with short-term harms without long-term benefits and should generally be avoided in older adults hospitalized for noncardiac conditions.
Abstract
Importance
Transient elevations of blood pressure (BP) are common in hospitalized older adults and frequently lead practitioners to prescribe more intensive antihypertensive regimens at hospital discharge than the patients were using before hospitalization.
Objective
To investigate the association between intensification of antihypertensive regimens at hospital discharge and clinical outcomes after discharge.
Design, Setting, and Participants
In this retrospective cohort study, patients 65 years and older with hypertension who were hospitalized in Veterans Health Administration national health system facilities from January 1, 2011, to December 31, 2013, for common noncardiac conditions were studied. Data analysis was performed from October 1, 2018, to March 10, 2019.
Exposures
Discharge with antihypertensive intensification, defined as receiving a prescription at hospital discharge for a new or higher-dose antihypertensive than was being used before hospitalization. Propensity scores were used to construct a matched-pairs cohort of patients who did and did not receive antihypertensive intensifications at hospital discharge.
Main Outcomes and Measures
The primary outcomes of hospital readmission, serious adverse events, and cardiovascular events were assessed by competing risk analysis. The secondary outcome was the change in systolic BP within 1 year of hospital discharge.
Results
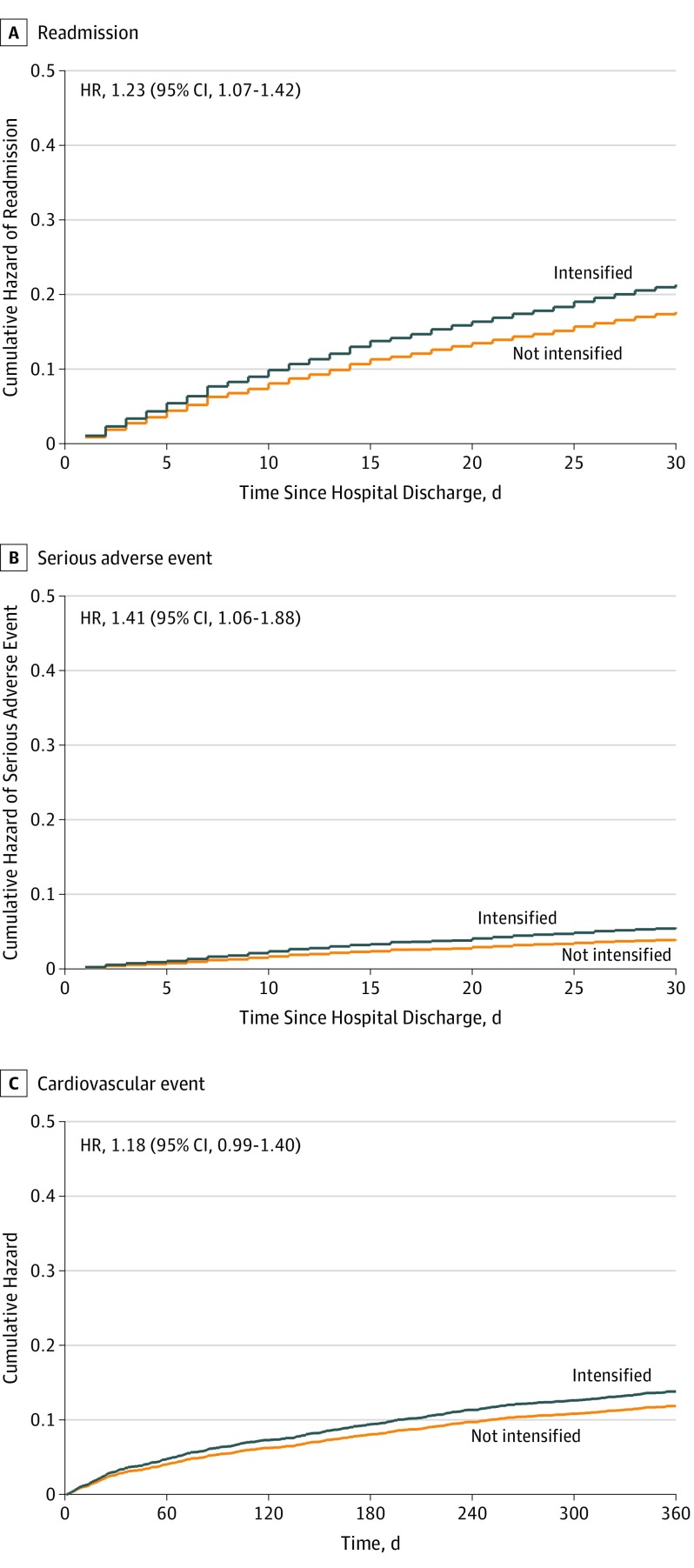
The propensity-matched cohort included 4056 hospitalized older adults with hypertension (mean [SD] age, 77 [8] years; 3961 men [97.7%]), equally split between those who did vs did not receive antihypertensive intensifications at hospital discharge. Groups were well matched on all baseline covariates (all standardized mean differences <0.1). Within 30 days, patients receiving intensifications had a higher risk of readmission (hazard ratio [HR], 1.23; 95% CI, 1.07-1.42; number needed to harm [NNH], 27; 95% CI, 16-76) and serious adverse events (HR, 1.41; 95% CI, 1.06-1.88; NNH, 63; 95% CI, 34-370). At 1 year, no differences were found in cardiovascular events (HR, 1.18; 95% CI, 0.99-1.40) or change in systolic BP among those who did vs did not receive intensifications (mean BP, 134.7 vs 134.4; difference-in-differences estimate, 0.6 mm Hg; 95% CI, −2.4 to 3.7 mm Hg).
Conclusions and Relevance
Among older adults hospitalized for noncardiac conditions, prescription of intensified antihypertensives at discharge was not associated with reduced cardiac events or improved BP control within 1 year but was associated with an increased risk of readmission and serious adverse events within 30 days.
Introduction
During hospitalization, older adults’ outpatient medication regimens are frequently changed.1,2 Medication changes may be related to the condition for which the patient was hospitalized (eg, cessation of antiplatelet therapy or initiation of proton pump inhibitor therapy in a patient hospitalized for gastrointestinal bleeding). However, changes may also be made to medications prescribed for chronic conditions that are not directly related to the reason for hospitalization.
A key exemplar of this is the treatment of high blood pressure (BP). Prior research3 suggests that inpatient practitioners commonly intensify patients’ outpatient antihypertensive regimens at hospital discharge, including patients with previously well-controlled outpatient BPs. This finding suggests that clinical practice may largely be driven by reflexive responses to elevated inpatient recordings being continued at discharge rather than planned adjustment of outpatient regimens.
The clinical outcomes of intensifying antihypertensive regimens at hospital discharge are not known, and there are 2 competing schools of thought. On the one hand, hospitalization may be an opportune time to set patients on the path toward better long-term BP control.4 On the other hand, discharging older adults home on intensified antihypertensive regimens may cause more harm than benefit.5,6 Short-term increases in BP during hospitalization likely have little long-term significance, yet these increases commonly precipitate treatment intensifications. For older adults with previously well-controlled outpatient BP, intensification of antihypertensive regimens in response to elevated inpatient BPs may lead to overtreatment when they return home. Even for patients with chronically elevated BP, failure to understand contextual factors and to achieve patient and primary care physician cooperation may often result in the manufacture of these medications being discontinued or lack of adherence after discharge. In either situation, adding medications has the potential to cause harm because medication confusion and medication errors are common after discharge. Moreover, in the posthospitalization period, older adults have a well-established increased susceptibility to both adverse drug events and hospital readmissions.7,8,9
Because intensification of antihypertensive regimens is common in hospitalized older adults and a subject of debate, understanding the actual benefits and harms of this practice is essential. To address this evidence gap, we conducted a retrospective cohort study of older adults with hypertension who were discharged from the national Veterans Health Administration health system after hospitalization for common noncardiac conditions at a Veterans Affairs (VA) hospital. We investigated the rates of hospital readmissions, medication-related severe adverse events, and cardiovascular events after discharge with intensified antihypertensive medication regimens compared with discharge without an intensified antihypertensive regimen.
Methods
We conducted a retrospective cohort study of older adults using national inpatient and outpatient VHA pharmacy and clinical data merged with VHA and Medicare claims data from January 1, 2009, to December 31, 2015. This research was approved by the institutional review boards of the San Francisco Veteran Affairs Medical Center and the University of California School of Medicine, San Francisco. Blanket informed consent was provided because administrative data were used. All data were deidentified.
Study Population
The study population has been described previously and consisted of older adults (≥65 years of age) with hypertension who were admitted to a VA hospital from January 1, 2011, to December 31, 2013, for pneumonia, urinary tract infection, or venous thromboembolism and discharged to the community setting.3 These conditions were chosen because they are among the most common medical discharge diagnoses for older adults and their management does not typically require the intensification of antihypertensive medications. Patients who were discharged with a secondary diagnosis of atrial fibrillation, acute coronary syndrome, or acute cerebrovascular event were excluded because these conditions might necessitate a change in antihypertensive treatment. Data analysis was performed from October 1, 2018, to March 10, 2019.
Exposure
We compared patients who were discharged from the hospital with intensified antihypertensive regimens with those discharged without intensified therapy. Intensifications were defined as newly prescribed antihypertensive medications that were not being used before hospitalization and medications present at admission for which a discharge prescription was filled for a dose increase of more than 20%. Intensifications were ascertained based on dispensing data from the VA inpatient and outpatient pharmacy using previously published methods that were validated in the study cohort through targeted medical record review.3 To ensure accurate classification of medication use, we excluded patients likely to receive medications outside the VA, including patients who received more than 20% of their outpatient care outside the VA, patients admitted from skilled nursing facilities, and patients who had been hospitalized in the 30 days preceding the index hospitalization.10
Study Outcomes
Three primary outcomes were chosen a priori to assess the benefits and harms of antihypertensive medications: all-cause hospital readmissions (to VA or non-VA facilities) within 30 days after index discharge, medication-related serious adverse events (SAEs) within 30 days, and cardiovascular events within 1 year. On the basis of prior hypertension trials, SAEs were defined as a composite of emergency department (ED) visits and hospitalizations for injurious falls, hypotension, syncope, electrolyte abnormalities, or acute kidney injury (eTable 1 in the Supplement).11,12,13 A timeframe of 30 days was chosen for SAEs because prior studies14,15,16 of antihypertensives indicate that SAEs may be most likely to occur shortly after initiation of medication use.
Cardiovascular events included a composite of ED visits and hospitalizations for acute myocardial infarction, unstable angina, stroke, heart failure, or hypertension (eTable 2 in the Supplement).11,12,13 A timeframe of 1 year was chosen for cardiovascular events because BP trials indicate that the timeframe to benefit from intensive BP control occurs within the first year of treatment.11,12,13 The SAEs and cardiovascular events were identified by primary discharge diagnoses through VA and Medicare claims.
Secondary outcomes included all-cause readmissions, SAEs, and all-cause mortality within 1 year as well as cardiovascular events and all-cause mortality within 30 days. In addition, we examined change in outpatient systolic BP (SBP) within 1 year of hospital discharge.
Statistical Analysis
We performed propensity score matching to control for differences between patients discharged with and without antihypertensive intensifications. First, a logistic regression model was developed to estimate the propensity of receiving the exposure (an antihypertensive intensification at hospital discharge). Covariates in the model were derived from covariates examined in prior trials, those included in a validated preventable hospital readmission prediction risk score,17 and according to clinical expertise. The full list of covariates appears in eTable 3 in the Supplement and includes the following: demographics, including race/ethnicity, obtained from VA administrative records; prehospitalization characteristics, including outpatient BP (measured as the median of the 3 most recent ambulatory recordings before hospitalization excluding the week before hospitalization); prior antihypertensive use patterns and health care use; index hospitalization characteristics and vital signs; hospital discharge laboratory values and medications; and comorbidities grouped using an aggregated version of the Centers for Medicare & Medicaid Services' condition categories.18 Missing data were imputed using the fully conditional specification method and 10 imputation sets. Estimates from each imputed data set were pooled into a single set of statistics using means for continuous variables and modes for categorical variables.
Second, 1:1 greedy nearest neighbor matching was performed using matching without replacement and a maximum caliper width of 0.2 times the pooled SD of the logit of the propensity scores for the cohort.19 Covariate balance between the intensified and control groups was assessed by visually inspecting cumulative probability distributions of the propensity scores between groups and by calculating standardized mean differences for which a difference of less than 0.10 was considered to indicate good balance.20
Third, survival analyses were conducted for all primary and secondary outcomes using Cox proportional hazards regression models for mortality and the Fine and Gray proportional subdistribution hazards models for all other outcomes to account for the competing risk of death.21 We report hazard ratios (HRs) and number needed to treat or number needed to harm (NNH) for each model.
Fourth, within propensity score–matched groups, the change in SBP after hospital discharge was estimated using a difference-in-differences approach. Linear regression analysis on 1000 bootstrap samples with replacement was used to estimate the change in SBP associated with discharge with an intensified antihypertensive after subtracting the background change among control patients.22
We conducted exploratory subgroup analyses specified a priori to determine the differential association of exposure with intensified antihypertensive medications by prehospitalization baseline SBP. We classified patients as having well-controlled or elevated prehospitalization baseline SBP based on their outpatient SBP before index hospitalization, using a threshold SBP of 140 mm Hg to define groups. We then repeated propensity score matching and analyses for each baseline BP group separately. In addition, because propensity score matching can only account for measured confounders, we calculated E-values for statistically significant primary outcomes to assess the robustness of observed associations to potential unmeasured confounding.23
In addition, because propensity score matching can only account for measured confounders, we calculated E-values for statistically significant primary outcomes to assess the robustness of observed associations to potential unmeasured confounding.23
We determined statistical significance by using 95% CIs and 2-tailed tests with P < .05. We used SAS statistical software, version 9.3 (SAS Institute Inc) and Stata, version 14.1 (StataCorp) for all analyses (eMethods in the Supplement).
Results
Patient Characteristics at Hospital Discharge
We identified 14 915 older adults (mean [SD] age, 77 [8] years; 3961 men [97.7%]) with hypertension who were discharged alive from VA medical centers after being treated for pneumonia, urinary tract infection, or venous thromboembolism (Table 1). Among the full cohort, 2074 patients (13.9%) were discharged with antihypertensive regimen intensifications. Patients discharged with intensifications had higher mean prehospitalization BPs; were more likely to be black, have elevated inpatient BPs, and have heart failure; and were less likely to have polypharmacy or cancer.
Table 1. Selected Cohort Characteristics Before and After Propensity Score Matchinga.
| Characteristic | Before Propensity Score Matching | SMD | After Propensity Score Matchingb | SMD | ||
|---|---|---|---|---|---|---|
| Intensified (n = 2074) | Not Intensified (n = 12 841) | Intensified (n = 2028) | Not Intensified (n = 2028) | |||
| Age, mean (SD), y | 76.8 (8.4) | 76.6 (8.6) | −0.02 | 76.8 (8.4) | 76.6 (8.7) | −0.02 |
| Male sex | 2022 (97.5) | 12 515 (97.5) | 0 | 1977 (97.5) | 1984 (97.8) | 0.02 |
| Race/ethnicity | ||||||
| White | 1450 (69.9) | 10036 (78.2) | 0.20 | 1428 (70.4) | 1432 (70.6) | 0.03 |
| Black | 507 (24.4) | 2192 (17.1) | 487 (24) | 482 (23.8) | ||
| Hispanic | 55 (2.7) | 222 (1.7) | 52 (2.6) | 45 (2.2) | ||
| Other | 62 (3.0) | 391 (3.0) | 61 (3.0) | 69 (3.4) | ||
| Preadmission clinical characteristics, mean (SD)c | ||||||
| BMI | 27.9 (6.7) | 27.6 (6.5) | −0.05 | 27.9 (6.7) | 28.1 (6.7) | 0.02 |
| Pulse, beats/mind | 73.6 (12.7) | 74.6 (12.5) | 0.08 | 73.6 (12.7) | 73.9 (12.5) | 0.02 |
| SBP, mm Hgd | 138.6 (19.1) | 132.3 (17.1) | −0.34 | 138.3 (18.9) | 137.9 (18.9) | −0.02 |
| Characteristics of index hospitalization | ||||||
| Length of stay, mean (SD), d | 6.8 (7.3) | 5.4 (6.7) | −0.2 | 6.7 (7.1) | 7.1 (11.6) | 0.04 |
| Inpatient SBPc | ||||||
| ≥3 Readings <90 mm Hg | 45 (2.2) | 419 (3.3) | 0.07 | 44 (2.2) | 42 (2.1) | 0.01 |
| ≥3 Readings ≥160 mm Hg | 719 (34.7) | 2041 (15.9) | 0.44 | 711 (35.1) | 760 (37.5) | −0.06 |
| ≥3 Readings ≥180 mm Hg | 349 (16.8) | 428 (3.3) | 0.46 | 311 (15.3) | 278 (13.7) | 0.06 |
| Discharge diagnosis | ||||||
| Pneumonia | 1045 (50.4) | 6681 (52) | 0.05 | 1027 (50.6) | 1019 (50.2) | 0.01 |
| Urinary tract infection | 790 (38.1) | 4849 (37.8) | 771 (38) | 773 (38.1) | ||
| Venous thromboembolism | 239 (11.5) | 1311 (10.2) | 230 (11.3) | 236 (11.6) | ||
| Laboratory values at discharge, mean (SD)c,e | ||||||
| Sodium level, mEq/L | 138.2 (3.5) | 138.1 (3.5) | −0.01 | 138.2 (3.5) | 138.2 (3.7) | 0.02 |
| Potassium level, mEq/L | 4.1 (0.5) | 4.1 (0.5) | −0.06 | 4.1 (0.5) | 4.1 (0.5) | |
| Estimated glomerular filtration rate, mL/min per 1.73 m2 | 66.3 (32.1) | 71.2 (31.8) | 0.16 | 66.5 (32.1) | 66.8 (32.2) | 0.01 |
| Health care use in year preceding hospitalization | ||||||
| Any Medicare use | 565 (27.2) | 3603 (28.1) | 0.02 | 557 (27.5) | 569 (28.1) | 0.01 |
| ≥3 ED visits | 392 (18.9) | 2555 (19.9) | 0.03 | 386 (19) | 383 (18.9) | 0.01 |
| >3 Hospitalizations | 571 (27.5) | 3651 (28.4) | 0.05 | 562 (27.7) | 552 (27.2) | 0.06 |
| Serious fall event | 94 (4.5) | 569 (4.4) | 0 | 93 (4.6) | 89 (4.4) | 0.01 |
| Admission antihypertensive use and adherencef | ||||||
| 0 Antihypertensives | 526 (25.4) | 3077 (24) | 0.19 | 501 (24.7) | 508 (25) | 0.05 |
| 1 Antihypertensive, PDC≤80% | 270 (13) | 1289 (10) | 261 (12.9) | 278 (13.7) | ||
| 1 Antihypertensive, PDC>80% | 282 (13.6) | 2255 (17.6) | 281 (13.9) | 294 (14.5) | ||
| 2 Antihypertensivess, PDC≤80% | 221 (10.7) | 1032 (8) | 215 (10.6) | 207 (10.2) | ||
| 2 Antihypertensive, PDC>80% | 327 (15.8) | 2378 (18.5) | 324 (16) | 302 (14.9) | ||
| ≥3 Antihypertensives, PDC≤80% | 138 (6.7) | 668 (5.2) | 136 (6.7) | 140 (6.9) | ||
| ≥3 Antihypertensives, PDC>80% | 310 (14.9) | 2142 (16.7) | 310 (15.3) | 299 (14.7) | ||
| Medication classes used at hospital admissiong | ||||||
| ≥8 Admission medications (polypharmacy) | 914 (44.1) | 6387 (49.7) | 0.11 | 910 (44.9) | 921 (45.4) | 0.01 |
| Angiotensin-converting enzyme inhibitors | 656 (31.6) | 4302 (33.5) | 0.04 | 650 (32.1) | 648 (32) | 0 |
| Angiotensin II inhibitors | 175 (8.4) | 1121 (8.7) | 0.01 | 174 (8.6) | 167 (8.2) | 0.01 |
| β-Blockers | 883 (42.6) | 5481 (42.7) | 0 | 873 (43) | 854 (42.1) | 0.02 |
| Calcium channel blockers | 587 (28.3) | 3759 (29.3) | 0.02 | 579 (28.6) | 584 (28.8) | 0.01 |
| Nonloop diuretics | 423 (20.4) | 2528 (19.7) | 0.02 | 416 (20.5) | 415 (20.5) | 0 |
| Other antihypertensives | 230 (11.1) | 1046 (8.1) | 0.10 | 224 (11) | 205 (10.1) | 0.03 |
| Anticoagulants | 96 (4.6) | 598 (4.7) | 0 | 93 (4.6) | 89 (4.4) | 0.01 |
| Platelet aggregation inhibitors | 201 (9.7) | 1206 (9.4) | 0.01 | 198 (9.8) | 198 (9.8) | 0 |
| Opioid analgesics | 467 (22.5) | 2915 (22.7) | 0 | 455 (22.4) | 472 (23.3) | 0.02 |
| Sedatives and hypnotics | 242 (11.7) | 1693 (13.2) | 0.05 | 239 (11.8) | 235 (11.6) | 0.01 |
| Insulin | 400 (19.3) | 2695 (21) | 0.04 | 394 (19.4) | 433 (21.4) | 0.05 |
| Selected comorbiditiesh | ||||||
| Heart failure | 715 (34.5) | 3272 (25.5) | 0.20 | 691 (34.1) | 729 (35.9) | 0.04 |
| Acute myocardial infarction | 116 (5.6) | 610 (4.8) | 0.04 | 112 (5.5) | 102 (5) | 0.02 |
| Coronary artery disease | 895 (43.2) | 5239 (40.8) | 0.05 | 880 (43.4) | 890 (43.9) | 0.01 |
| Valvular heart disease | 263 (12.7) | 1508 (11.7) | 0.03 | 262 (12.9) | 247 (12.2) | 0.02 |
| Arrhythmias | 666 (32.1) | 4225 (32.9) | 0.02 | 649 (32) | 632 (31.2) | 0.02 |
| Chronic obstructive pulmonary disease or asthma | 1021 (49.2) | 6695 (52.1) | 0.06 | 1006 (49.6) | 1028 (50.7) | 0.02 |
| Renal disorders | 1513 (73) | 8862 (69) | 0.09 | 1476 (72.8) | 1479 (72.9) | 0 |
| Diabetes | 1167 (56.3) | 6661 (51.9) | 0.09 | 1135 (56) | 1166 (57.5) | 0.03 |
| Hip fracture | 36 (1.7) | 276 (2.1) | 0.03 | 36 (1.8) | 42 (2.1) | 0.02 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); ED, emergency department; PDC, proportion of days covered; SBP, systolic blood pressure; SMD, standardized mean difference.
SI conversion factor: To convert sodium and potassium to millimoles per liter, multiply by 1.
Data are presented as number (percentage) of patients unless otherwise indicated. Selected covariates are presented; a full list of covariates included in propensity scoring are given in eTable 3 in the Supplement.
Patients who were discharged with intensified antihypertensive regimens were matched with patients who were discharged without antihypertensive intensifications based on 1:1 propensity score matching without replacement. Matching was performed using a caliper width of 0.2 times the pooled SD of the logit of the propensity scores for the cohort. Balance between the groups was assessed before and after matching by comparing SMDs for each variable for which a difference of less than 0.10 was considered to indicate adequate balance.
Missing data were as follows: income (n = 6), BMI (n = 960), outpatient blood pressure (n = 425), outpatient pulse (n = 534), inpatient blood pressure (n = 167), inpatient pulse (n = 174), hemoglobin (n = 1170), potassium (n = 586), sodium (n = 534), blood urea nitrogen (n = 839), carbon dioxide (n = 735), and platelets (n = 866).
Prehospitalization vital sign data were measured as the median of the 3 most recent ambulatory recordings before index hospitalization, collected in the year before hospitalization and excluding the week immediately preceding hospitalization.
Laboratory data collected from day of index hospitalization discharge or during index hospitalization up to 2 days before day of discharge.
Adherence calculated from electronic pharmacy dispensing data as the PDC for each admission antihypertensive regimen in the year before index hospital admission. A threshold of 80% is a commonly used criterion to determine clinically significant nonadherence. To account for patients taking multiple antihypertensives at hospital admission, a composite PDC was calculated as the mean of each antihypertensive PDC because individual antihypertensive PDCs were highly collinear within patients.
All medications classified using Veterans Affairs drug class coding. Combination medications were split into component parts. Topical, inhaled, otic, and optic medications were excluded.
Comorbidities include both secondary discharge diagnoses from index hospitalization and preadmission diagnoses from the year preceding index hospitalization.
Propensity score matching resulted in a cohort of 4056 patients equally split between those who received antihypertensive regimen intensifications and those who did not (eFigure 1 in the Supplement). Groups were well balanced on propensity score distribution and baseline characteristics (standardized mean differences for all covariates <0.1), including identical preadmission BP distributions (mean [SD] SBP, 138 [19] mm Hg) (Table 1 and eTable 3 in the Supplement).
Primary Outcomes
In the propensity score–matched cohort, patients discharged with antihypertensive regimen intensifications were more likely to be readmitted within 30 days of discharge than patients discharged without antihypertensive regimen intensifications (434 of 2028 [21.4%] vs 358 of 2028 [17.7%]; HR, 1.23; 95% CI, 1.07-1.42; NNH, 27; 95% CI, 16-76) (Figure, A and Table 2). Patients discharged with intensifications were also more likely to experience an ED visit or hospitalization for an SAE within 30 days of discharge (91 of 2028 [4.5%] vs 62 of 2028 [3.1%]; HR, 1.41; 95% CI, 1.06-1.88; NNH, 63; 95% CI, 34-370) (Figure, B and Table 2). Within 1 year of discharge, no significant difference was found in cardiovascular events between intensified and nonintensified groups (280 of 2028 [13.8%] vs 242 of 2028 [11.9%]; HR, 1.18; 95% CI, 0.99-1.40) (Figure, C and Table 2).
Figure. Cumulative Hazard Plots Comparing Outcomes With Exposure to Antihypertensive Regimen Intensifications at Hospital Discharge.
A, Patients were censored at 30 days after index hospitalization discharge. All-cause readmissions were identified through Veterans Affairs and Medicare claims. B, Patients were censored at 30 days after index hospitalization discharge. Serious adverse events were identified through Veterans and Medicare claims and defined as the first emergency department visit or hospitalization for injurious falls, syncope, hypotension, electrolyte abnormalities, or acute kidney injury. C, Patients were censored at 365 days after index hospitalization discharge. Cardiovascular events were identified through Veterans Affairs and Medicare claims and defined as the first emergency department visit or hospitalization for acute myocardial infarction, unstable angina, stroke, heart failure, or hypertension. HR indicates hazard ratio.
Table 2. Primary and Secondary Clinical Outcomes Associated With Receiving an Antihypertensive Intensification Regimen at Hospital Dischargea.
| Outcome | No. (%) of Patients | Hazard Ratio (95% CI) | NNH (95% CI)b | |
|---|---|---|---|---|
| Intensified Rgimen (n = 2028) | Not Intensified Regimen (n = 2028) | |||
| Primary outcomes | ||||
| Hospital readmission, 30 d | 434 (21.4) | 358 (17.7) | 1.23 (1.07-1.42) | 27 (16-76) |
| Serious adverse event, 30 d | 91 (4.5) | 62 (3.1) | 1.41 (1.06-1.88) | 63 (34-370) |
| Cardiovascular event, 365 d | 280 (13.8) | 242 (11.9) | 1.18 (0.99-1.40) | NA |
| Secondary 30-d outcomes | ||||
| Mortality | 84 (4.1) | 101 (5.0) | 0.84 (0.62-1.12) | NA |
| Cardiovascular event | 72 (3.6) | 44 (2.2) | 1.65 (1.13-2.40) | 72 (41-278) |
| Secondary 365-d outcomes | ||||
| Mortality | 477 (22.0) | 519 (25.6) | 0.91 (0.80-1.03) | NA |
| Readmission | 1210 (59.7) | 1161 (57.2) | 1.07 (0.99-1.16) | NA |
| Serious adverse event | 413 (20.4) | 376 (18.5) | 1.12 (0.97-1.28) | NA |
Abbreviations: NA, not applicable; NNH, number needed to harm.
Patients were censored at 30 or 365 days after index hospitalization discharge as indicated. Hazard ratios for mortality were generated from Cox proportional hazards regression models. For all other outcomes, subdistribution hazards were generated from competing risk regression models, accounting for the competing risk of death. Serious adverse events were defined as first emergency department visit or hospitalization for injurious fall, syncope, hypotension, electrolyte abnormalities, or acute kidney injury. Cardiovascular events were defined as first emergency department visit or hospitalization for acute myocardial infarction, unstable angina, stroke, heart failure, or hypertension.
The NNHs were only estimated when there was a statistically significant direction of treatment effect.
Secondary Clinical Outcomes
Secondary outcomes are given in Table 2. Patients discharged with intensification regimens were more likely to experience a cardiovascular event within 30 days of discharge (72 of 2028 [3.6%] vs 44 of 2028 [2.2%]; HR, 1.65; 95% CI, 1.13-2.40). No significant differences were found in mortality within 30 days (HR, 0.84; 95% CI, 0.62-1.12) or in any secondary outcome within 1 year.
Changes in SBP After Hospital Discharge
Among the 2323 patients in the propensity-matched cohort with an outpatient BP measurement recorded between 6 months and 18 months after discharge, the mean SBP among patients receiving intensifications decreased from 138.5 mm Hg (95% CI, 137.3-139.6 mm Hg) to 134.7 mm Hg (95% CI, 133.6-135.9 mm Hg), and the mean SBP among patients who did not receive intensifications decreased from 138.4 mm Hg (95% CI, 137.3-139.6 mm Hg) to 134.4 mm Hg (95% CI, 133.2-135.6 mm Hg). The mean (SD) time between baseline and postbaseline measures was 354 (52) days in the intensified group and 356 (51) days in the nonintensified group. The pre-post change was −3.8 (95% CI, −5.4 to −2.3) in the intensified group and −4.0 (95% CI, −5.6 to −2.4) in the not intensified group. No significant difference was found in the change in SBP between groups (differences-in-differences estimate, 0.2 mm Hg; 95% CI, –2.0 to 2.4 mm Hg).
Sensitivity Analyses
Prehospitalization Baseline BP Subgroups
Propensity score matching yielded a cohort of 2244 patients with previously well-controlled prehospitalization baseline SBP (<140 mm Hg) and a cohort of 1756 patients with elevated prehospitalization baseline SBP (≥140 mm Hg), each equally split between those who received intensifications and those who did not. Covariate balance between groups in each cohort was excellent except for differences in the regional distribution of patients (eTable 5, eTable 6, and eFigure 2 in the Supplement).
Among matched patients with well-controlled baseline SBP, the mean (SD) prehospitalization outpatient SBP was 125 (11) mm Hg for the intensified and not intensified groups. Those who received intensifications were more likely to be readmitted (HR, 1.34; 95% CI, 1.11-1.62) and to experience an SAE (HR, 1.65; 95% CI, 1.13-2.40) within 30 days and more likely to experience a cardiovascular event within 1 year (HR, 1.37; 95% CI, 1.08-1.75) (Table 3).
Table 3. Clinical Outcomes Associated With Receiving an Antihypertensive Intensification Regimen at Hospital Discharge in Subgroups With Controlled and Elevated Prehospitalization Baseline Blood Pressure Subgroupsa.
| Outcome | Well-Controlled Baseline Blood Pressure Group (SBP<140 mm Hg)b | Elevated Baseline Blood Pressure Group (SBP≥140 mm Hg)c | ||||||
|---|---|---|---|---|---|---|---|---|
| No. With Event | Hazard Ratio (95% CI) | NNH (95% CI)d | No. With Event | Hazard Ratio (95% CI) | NNH (95% CI)d | |||
| Intensified (n = 1122) | Not Intensified (n = 1122) | Intensified (n = 878) | Not Intensified (n = 878) | |||||
| Hospital readmission, 30 d | 252 | 193 | 1.34 (1.11-1.62) | 19 (12-51) | 178 | 161 | 1.12 (0.91-1.39) | NA |
| Serious adverse event, 30 d | 70 | 43 | 1.65 (1.13-2.40) | 41 (24-167) | 43 | 36 | 1.19 (0.77-1.86) | NA |
| Cardiovascular event, 365 d | 146 | 109 | 1.37 (1.08-1.75) | 30 (17-147) | 127 | 105 | 1.24 (0.95-1.60) | NA |
Abbreviations: NA, not applicable; NNH, number needed to harm; SBP, systolic blood pressure.
Patients were censored at 30 or 365 days after index hospitalization discharge as indicated. Subdistribution hazards were generated from competing risk regression models, accounting for the competing risk of death. Serious adverse events were defined as first emergency department visit or hospitalization for injurious fall, syncope, hypotension, electrolyte abnormalities, or acute kidney injury. Cardiovascular events were defined as first emergency department visit or hospitalization for acute myocardial infarction, unstable angina, stroke, heart failure, or hypertension.
Propensity score matching and survival analyses were performed separately for this subgroup of patients in whom well-controlled prehospitalization baseline SBP was defined to include all patients with an outpatient SBP less than 140 mm Hg before index hospitalization.
Propensity score matching and survival analyses were performed separately for this subgroup of patients in whom elevated prehospitalization baseline SBP was defined to include all patients with an outpatient SBP of 140 mm Hg or higher before index hospitalization.
The NNH was only estimated when there was a statistically significant direction of treatment effect.
Among matched patients with elevated baseline SBP, the mean (SD) prehospitalization outpatient BP was 154 (13) mm Hg for the intensified and nonintensified groups. No difference was found in the primary or secondary clinical outcomes among patients who were discharged with antihypertensive intensifications (Table 3 and eTable 7 in the Supplement). Receipt of an intensification was not associated with a significant difference in change in SBP for either subgroup (eTable 8 in the Supplement).
E-Value Analyses
An unmeasured confounder could fully account for the association of intensification with hospital readmissions if it were associated with the exposure and outcome by an HR of 1.58 (lower confidence limit, 1.27) and could fully account for the association of intensification with hospital readmissions if it was associated with the exposure and outcome by an HR of 2.17 (lower confidence limit, 1.31).
Discussion
In this national study of older adults with hypertension who were hospitalized for common noncardiac conditions, intensification of antihypertensive regimens at hospital discharge was associated with increased short-term risks of readmission and medication-related SAEs. Moreover, intensification of antihypertensive regimens at hospital discharge was not associated with longer-term improvements in BP control or a reduction in cardiovascular events. These results suggest that intensification of outpatient antihypertensive regimens during hospitalization for noncardiac conditions should generally be avoided in older adults.
To date, no clinical trials have evaluated the outcomes of intensifying antihypertensive regimens at hospital discharge. Thus, our findings provide important data to practitioners considering inpatient BP management decisions. Because more than half of patients in our study who received antihypertensive regimen intensifications at discharge had well-controlled outpatient BP before hospitalization, the observed increased rate of medication-related SAEs may partially be explained by BP overtreatment, which may be associated with postural or absolute hypotension, resulting in syncope, falls, or renal injury. Analyses stratifying patients by prehospitalization outpatient BP control demonstrated that patients with previously well-controlled BPs had increased risk of medication-related SAEs and readmissions, but these associations were not observed for patients with previously elevated BPs. Although these subgroup analyses were not definitive, they suggest that intensification of antihypertensive regimens at discharge should be discouraged for patients with previously controlled outpatient BP because there is little potential of additional cardiovascular benefit for patients already at goal.
Even in patients with previously elevated BPs, the timing of antihypertensive regimen intensification at hospital discharge may lead to unnecessary risk. Prior research16 indicates that the risk of antihypertensive-related SAEs may be particularly elevated in the first 30 days after initiation of medication use. This risk is likely to be compounded when antihypertensive regimens are intensified during hospitalization because patients who have increased rates of adverse drug events are often exposed to multiple other medication changes at hospital discharge and may be experiencing hospital-associated disability.24 Whereas the harms of antihypertensive intensification may be highest in the short term, outpatient clinical trials indicate the benefits of BP lowering at 6 to 12 months after initiation of BP-lowering therapy.11,12 Thus, the risk reduction in delaying adjustment of long-term BP medications until patients are seen in the outpatient setting is likely to outweigh the short delay in possible benefit.4,5
The findings suggest that intensification of antihypertensive regimens at hospital discharge was associated with an increased risk of all-cause hospital readmissions beyond the observed increased risk in SAEs. Intensification of antihypertensive regimens at discharge may contribute to polypharmacy and potentially medication confusion at discharge, which may be associated with increased risk of hospitalization for adverse drug events and reduced patient adherence to other medications that affect their short-term health. This finding may also be a result of unmeasured differences between intensified and nonintensified patients (eg, frailty,25 functional status,26 and social risk27), although it is unclear why patients receiving regimen intensifications might be more likely to have these risk factors. Furthermore, physicians who intensified antihypertensive regimens may deliver other types of care differently than physicians who did not intensify antihypertensive regimens and may be more likely to change to other medications, which could further contribute to medication confusion and risk of readmission. Thus, our finding of increased risk of readmission may reflect a broader phenomenon of overall medication regimen intensification at hospital discharge.
We found that intensification of antihypertensive regimens at hospital discharge was not associated with a reduction in cardiovascular events at 1 year in the full cohort or in the subgroup of patients with previously elevated BPs. This finding likely reflects a lack of persistence to antihypertensive intensifications after discharge because there was also no difference in SBP between intensified and nonintensified groups at 1 year. After discharge, outpatient practitioners may reverse antihypertensive changes made during hospitalization because of the occurrence of medication-related SAEs, observation of symptomatic hypotension, or knowledge of contextual factors about the patient’s care, such as preference for medication minimization, cost concerns, or prior medication intolerance. Furthermore, patients may discontinue intensification regimens on their own because of medication confusion, adverse effects, or the perception that medications received at hospital discharge need to only be taken in the short term. Exposure to intensified BP medications for short periods is unlikely to be associated with reduced cardiovascular risk but may contribute to polypharmacy and associated risks.
Our findings have implications for the management of chronic conditions at hospital discharge. Although clear communication remains paramount to minimizing the medication-related harms in the perihospitalization period, simply reconciling medications at discharge is not sufficient.28,29 Decisions to adjust chronic disease medications in the inpatient setting should incorporate considerations of patients’ likelihood of benefit and the interplay of the acute hospital condition with existing chronic conditions.30 In addition, practitioners should recognize that fluctuations in chronic disease markers during hospitalization (eg, BP or blood glucose recordings) may be transient and that decisions to adjust long-term regimens may often be able to be delayed until after hospitalization. To improve prescribing quality, efforts should target improving the accessibility of crucial outpatient disease information (eg, recent outpatient BPs and medication use) to inpatient practitioners making chronic disease management decisions at the point of care, possibly through the development of clinical decision support tools.31,32
Limitations
Our study has several limitations. First, to address the risk of confounding inherent to observational studies, we used propensity score matching that incorporated a large number of clinically relevant factors, including markers of BP control, comorbidities, prior health care and medication use patterns, and validated readmission prediction measures. Furthermore, the findings of our secondary analyses are mechanistically consistent with the primary outcome results. Nonetheless, our study may be subject to confounding by factors that were not able to be measured. Second, although our examination of adverse events was strengthened by examining VA and Medicare claims, this approach was limited to examining events that resulted in an ED visit or hospitalization and does not identify less serious adverse drug events for which patients sought ambulatory care or no care. Third, our examination of cardiovascular outcomes was limited to 1 year of follow-up; however, it is unlikely that there would be a differential change in longer-term cardiovascular events because there was no difference in BPs between groups at 1 year. Fourth, the subgroup analyses that examined outcomes stratified by preadmission BP control were exploratory and do not definitely prove differential effects of antihypertensive regimen intensification across levels of baseline BP. Fifth, our study took place in the VHA health system, which is the largest integrated health care system in the United States but serves a higher proportion of men and patients with multimorbidity than the general US population. As a result, our cohort was predominately male; thus, our findings may not be generalizable to female patients. Sixth, our study examined only older adults; thus, our findings are not generalizable to younger populations.
Conclusions
Among older adults hospitalized for noncardiac conditions, discharge with intensified antihypertensives was not associated with reduced cardiac events within 1 year but was associated with an increased risk of readmission and SAEs within 30 days. Shifting practice from intensifying antihypertensive regimens during hospitalization to communicating concerns about patients’ long-term BP control to outpatient practitioners for close follow-up may provide a safer treatment path for patients.
eMethods. Statistical Software Programs Used in Analyses
eTable 1. Serious Adverse Event Outcome Definitions
eTable 2. Cardiovascular Event Outcome Definitions
eTable 3. Complete Baseline Characteristics Before and After Propensity Score Matching
eTable 4. Components of Composite Outcomes Associated with Receiving Antihypertensive Intensifications at Hospital Discharge
eTable 5. Baseline Characteristics Before and After Propensity Score Matching, Well-Controlled Baseline BP Subgroup
eTable 6. Baseline Characteristics Before and After Propensity Score Matching, Elevated Baseline BP Subgroup
eTable 7. Secondary Clinical Outcomes Associated with Receiving Antihypertensive Intensifications at Hospital Discharge in Well-Controlled and Elevated Baseline Blood Pressure Subgroups
eTable 8. Changes in Systolic Blood Pressure Following Hospital Discharge in Well-Controlled and Elevated Baseline BP Subgroups
eFigure 1. Primary Cohort Propensity Score Balance Diagnostics
eFigure 2. Propensity Score Distribution Before and After Matching
References
- 1.Unroe KT, Pfeiffenberger T, Riegelhaupt S, Jastrzembski J, Lokhnygina Y, Colón-Emeric C. Inpatient medication reconciliation at admission and discharge: a retrospective cohort study of age and other risk factors for medication discrepancies. Am J Geriatr Pharmacother. 2010;8(2):115-126. doi: 10.1016/j.amjopharm.2010.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris CM, Sridharan A, Landis R, Howell E, Wright S. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150-153. doi: 10.1097/PTS.0b013e318286f87d [DOI] [PubMed] [Google Scholar]
- 3.Anderson TS, Wray CM, Jing B, et al. Intensification of older adults’ outpatient blood pressure treatment at hospital discharge: national retrospective cohort study. BMJ. 2018;362:k3503. doi: 10.1136/bmj.k3503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blecker S, Meisel T, Dickson VV, Shelley D, Horwitz LI. “We’re almost guests in their clinical care”: inpatient provider attitudes toward chronic disease management. J Hosp Med. 2017;12(3):162-167. doi: 10.12788/jhm.2699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steinman MA, Auerbach AD. Managing chronic disease in hospitalized patients. JAMA Intern Med. 2013;173(20):1857-1858. doi: 10.1001/jamainternmed.2013.9511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stall NM, Bell CM. Managing blood pressure medication at discharge. BMJ. 2018;362:k3789. doi: 10.1136/bmj.k3789 [DOI] [PubMed] [Google Scholar]
- 7.Beers MH, Dang J, Hasegawa J, Tamai IY. Influence of hospitalization on drug therapy in the elderly. J Am Geriatr Soc. 1989;37(8):679-683. doi: 10.1111/j.1532-5415.1989.tb02227.x [DOI] [PubMed] [Google Scholar]
- 8.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161-167. doi: 10.7326/0003-4819-138-3-200302040-00007 [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM. Post-hospital syndrome: an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. doi: 10.1056/NEJMp1212324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson TS, Xu E, Whitaker E, Steinman MA. A systematic review of methods for determining cross-sectional active medications using pharmacy databases. Pharmacoepidemiol Drug Saf. 2019;28(4):403-421. Epub ahead of print. doi: 10.1002/pds.4706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williamson JD, Supiano MA, Applegate WB, et al. ; SPRINT Research Group . Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315(24):2673-2682. doi: 10.1001/jama.2016.7050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beckett NS, Peters R, Fletcher AE, et al. ; HYVET Study Group . Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-1898. doi: 10.1056/NEJMoa0801369 [DOI] [PubMed] [Google Scholar]
- 13.Reboussin DM, Allen NB, Griswold ME, et al. Systematic Review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):2176-2198. doi: 10.1016/j.jacc.2017.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172(22):1739-1744. doi: 10.1001/2013.jamainternmed.469 [DOI] [PubMed] [Google Scholar]
- 15.Berry SD, Zhu Y, Choi H, Kiel DP, Zhang Y. Diuretic initiation and the acute risk of hip fracture. Osteoporos Int. 2013;24(2):689-695. doi: 10.1007/s00198-012-2053-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shimbo D, Barrett Bowling C, Levitan EB, et al. Short-term risk of serious fall injuries in older adults initiating and intensifying treatment with antihypertensive medication. Circ Cardiovasc Qual Outcomes. 2016;9(3):222-229. doi: 10.1161/CIRCOUTCOMES.115.002524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donzé J, Aujesky D, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Intern Med. 2013;173(8):632-638. doi: 10.1001/jamainternmed.2013.3023 [DOI] [PubMed] [Google Scholar]
- 18.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363. doi: 10.1001/jama.2012.216476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399-424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083-3107. doi: 10.1002/sim.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133(6):601-609. doi: 10.1161/CIRCULATIONAHA.115.017719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheung YB. A modified least-squares regression approach to the estimation of risk difference. Am J Epidemiol. 2007;166(11):1337-1344. doi: 10.1093/aje/kwm223 [DOI] [PubMed] [Google Scholar]
- 23.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 24.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. doi: 10.1001/jama.2011.1556 [DOI] [PubMed] [Google Scholar]
- 25.Belga S, Majumdar SR, Kahlon S, et al. Comparing three different measures of frailty in medical inpatients: multicenter prospective cohort study examining 30-day risk of readmission or death. J Hosp Med. 2016;11(8):556-562. doi: 10.1002/jhm.2607 [DOI] [PubMed] [Google Scholar]
- 26.Greysen SR, Stijacic Cenzer I, Auerbach AD, Covinsky KE. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern Med. 2015;175(4):559-565. doi: 10.1001/jamainternmed.2014.7756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269-282. doi: 10.1007/s11606-012-2235-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mansur N, Weiss A, Beloosesky Y. Relationship of in-hospital medication modifications of elderly patients to postdischarge medications, adherence, and mortality. Ann Pharmacother. 2008;42(6):783-789. doi: 10.1345/aph.1L070 [DOI] [PubMed] [Google Scholar]
- 29.Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):397-403. doi: 10.7326/0003-4819-158-5-201303051-00006 [DOI] [PubMed] [Google Scholar]
- 30.Tinetti ME, Green AR, Ouellet J, Rich MW, Boyd C. Caring for patients with multiple chronic conditions. Ann Intern Med. 2019;170(3):199-200. Epub ahead of print. doi: 10.7326/M18-3269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29-43. doi: 10.7326/0003-4819-157-1-201207030-00450 [DOI] [PubMed] [Google Scholar]
- 32.Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003;163(12):1409-1416. doi: 10.1001/archinte.163.12.1409 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Statistical Software Programs Used in Analyses
eTable 1. Serious Adverse Event Outcome Definitions
eTable 2. Cardiovascular Event Outcome Definitions
eTable 3. Complete Baseline Characteristics Before and After Propensity Score Matching
eTable 4. Components of Composite Outcomes Associated with Receiving Antihypertensive Intensifications at Hospital Discharge
eTable 5. Baseline Characteristics Before and After Propensity Score Matching, Well-Controlled Baseline BP Subgroup
eTable 6. Baseline Characteristics Before and After Propensity Score Matching, Elevated Baseline BP Subgroup
eTable 7. Secondary Clinical Outcomes Associated with Receiving Antihypertensive Intensifications at Hospital Discharge in Well-Controlled and Elevated Baseline Blood Pressure Subgroups
eTable 8. Changes in Systolic Blood Pressure Following Hospital Discharge in Well-Controlled and Elevated Baseline BP Subgroups
eFigure 1. Primary Cohort Propensity Score Balance Diagnostics
eFigure 2. Propensity Score Distribution Before and After Matching