Abstract
Background
Given the slow uptake of PrEP among cisgender men who have sex with men (MSM) in high-income countries, efforts to roll-out PrEP in low- and middle-income countries (LMIC) should address barriers to PrEP use to facilitate its more rapid uptake. To inform PrEP programs in LMIC, we examined patterns of perceived barriers to PrEP use among HIV-negative MSM in Tijuana, Mexico.
Methods
From 03/2016-09/2017, 364 MSM completed interviewer-administered surveys assessing perceived barriers to PrEP use across 4 domains: PrEP attribute, individual, interpersonal, and structural. Latent class analysis was performed to identify distinct classes with respect to perceived barriers to PrEP use. Multinomial logistic regression was used to identify factors associated with class membership.
Results
We identified three classes characterized by (1) high levels of perceived barriers across domains (12%), (2) low levels of perceived barriers across domains (43%), and (3) perceived PrEP attribute barriers (i.e., side-effects and cost) (45%). Membership in the high level of perceived barriers class (vs. the low level of perceived barriers class) was positively associated with having a history of incarceration (AOR: 2.44; 95% CI: 1.04, 5.73) and negatively associated with more social support (AOR: 0.99; 95% CI: 0.98, 1.00). Membership in the perceived PrEP attribute barriers class was positively associated with having seen a healthcare provider in the past year (AOR: 2.78; 95% CI: 1.41, 5.45) and negatively associated with having any HIV-positive or status unknown partners (AOR: 0.56; 95% CI: 0.31, 1.01).
Conclusions
Since most participants were in either the low level of perceived barriers class or the perceived PrEP attribute barriers class, future PrEP uptake may be high among MSM in Tijuana. However, these findings suggest that achieving sufficient PrEP uptake and adherence among MSM in Tijuana may require a range of comprehensive HIV prevention interventions.
Introduction
Worldwide, cisgender men who have sex with men (MSM) are disproportionately impacted by HIV infection [1, 2]. Daily oral use of emtricitabine and tenofovir disoproxil fumarate (FTC/TDF) as pre-exposure prophylaxis (PrEP) effectively prevents HIV infection [3–6] and has the potential to curb HIV epidemics among MSM globally [7–10]. In 2014, the World Health Organization (WHO) released guidelines recommending PrEP for MSM at substantial risk of HIV infection [11]. Yet, to-date, PrEP implementation and uptake have been slow and mainly concentrated among MSM in high-income countries [12, 13].
International research among MSM has identified barriers to PrEP uptake across multiple domains characterized by PrEP attribute, individual, interpersonal, and structural barriers. PrEP attributes are the most commonly cited barriers to PrEP use among MSM, particularly concerns about PrEP’s cost, efficacy, and side-effects [14–20]. Individual barriers to PrEP use include low perceived risk of HIV infection [14, 21–23], concerns about daily adherence [17, 20, 23, 24], and the potential for increased risk of other sexually transmitted infections due to decreased condom use as a result of PrEP use [19, 20]. With respect to interpersonal barriers to PrEP use, prior work has documented concerns that sex partners may expect condomless anal intercourse (CAI) in the context of PrEP use [20], as well as fears that PrEP users may be perceived as sexually promiscuous [21, 25–27] or HIV-positive [18, 24, 28] if others see them taking PrEP. Finally, structural barriers that limit healthcare access can also significantly impact PrEP use. For instance, stigma towards sexual minorities often limits the willingness of MSM to discuss sexual health and HIV prevention with healthcare providers (HCPs) [25–27], which may inhibit their ability to access PrEP [29].
Although many of these barriers to PrEP use have been consistently identified among MSM across diverse settings, less is known about how patterns of perceived barriers may vary across subgroups within MSM populations. Latent class analysis (LCA) identifies unobserved classes or subgroups within populations based on the similarity of their responses across individual measures [30–32]. Although LCA has been used to identify subgroups of MSM with respect to patterns of sexual and substance use risk behaviors, barriers to HIV testing, and HIV risk reduction strategies [33–36], it has not been used to identify subgroups of MSM with respect to patterns of perceived barriers to PrEP use. Understanding the underlying patterns of perceived barriers to PrEP use across subgroups of MSM and whether these subgroups differ by socio-demographic, psychosocial, healthcare access, substance use, and sexual risk factors may help inform future interventions to support PrEP uptake among MSM.
Given that PrEP uptake has been slow among MSM in early adopter countries [13], it is imperative that efforts to bring PrEP to scale in low- and middle-income countries (LMIC), like Mexico, address barriers to PrEP use to support its rapid uptake among those at high risk of HIV acquisition. To inform these efforts, we conducted an exploratory LCA to identify distinct classes of MSM in Tijuana, Mexico with respect to perceived barriers to PrEP use and factors associated with class membership. As in other LMIC, the HIV epidemic in Mexico is concentrated among MSM [37], with HIV prevalence among MSM in Tijuana estimated to be 20% [38]. Several socio-structural factors unique to the Mexico-United States border region, including elevated levels of poverty, sex work, drug trafficking, and migration, contribute to the HIV risk environment among MSM in Tijuana [39, 40]. However, as seen in other LMIC [1, 2], HIV risk and access to HIV prevention services among MSM in Tijuana are also shaped by stigma toward sexual minorities [39–41]. As such, findings from this exploratory study may help inform strategies to ensure that comprehensive HIV prevention packages that include PrEP are accessible to MSM in Mexico and other similar LMIC.
Methods
Study population
Between March 2016 and September 2017, 397 participants who tested HIV-negative as part of a parent study, Proyecto Enlaces (“Project Links”), were recruited to participate in Proyecto Redes (“Project Networks”). The primary aim of Proyecto Enlaces was to compare the effectiveness of respondent-driven sampling (RDS) and venue-based sampling (VBS) to identify MSM and persons who identify as transgender women (TW) with previously undiagnosed HIV infection in Tijuana. VBS is a time-space sampling method [42] that was conducted at venues identified via formative research as those where MSM and persons who identify as TW meet sexual partners (e.g., bars, public spaces). RDS is a chain-referral sampling method [43] and was initiated by 32 seeds selected to be diverse with respect to HIV status, age, socio-economic status, sexual orientation, gender identity, and recruitment source (i.e., Tijuana’s government-funded HIV treatment clinic and VBS venues). An additional goal of Proyecto Enlaces and Proyecto Redes was to characterize the sexual networks of MSM and persons who identify as TW due to the high prevalence of HIV among both populations in Tijuana and their often-overlapping sexual networks [38, 44]. As such, both MSM and persons who identify as TW were recruited via RDS and VBS to participate in these studies.
Eligibility criteria for VBS participants included: no prior HIV diagnosis, cisgender male or transgender female, ≥18 years-old, and anal sex with a cisgender male or transgender female in the past 4 months. Eligible individuals were offered rapid HIV testing (Advanced Quality HIV 1/2 Test Kits, Intec Products, Inc., Xiamen, China) and those who tested HIV-negative were offered enrollment in Proyecto Redes. Eligibility criteria for RDS seeds included: cisgender male or transgender female, ≥18 years-old, Tijuana residence, anal sex with a cisgender male or transgender female in the past 4 months, and a social network including ≥15 MSM or persons who identify as TW living in Tijuana. Seeds were given three coupons to recruit MSM peers and peers who identify as TW from their social networks who were then given three coupons to recruit their peers in subsequent recruitment waves. Peer-recruit eligibility criteria were similar to those for seeds, but peer-recruits were not required to live in Tijuana and only had to report anal sex with a cisgender male or transgender female in the past year. Peer-recruits without a prior HIV diagnosis were offered HIV testing. To ensure comparability to VBS participants, peer-recruits who tested HIV-negative and reported anal sex with a cisgender male or transgender female in the past 4 months were offered enrollment in Proyecto Redes. Since the Proyecto Redes survey only included MSM-specific measures for perceived barriers to PrEP use (described below), the sample for the current study was restricted to 364 HIV-negative MSM (i.e., cisgender males who reported anal sex with other cisgender males in the past 4 months) participants.
Data collection
Participants completed an interviewer-administered survey assessing socio-demographics, substance use behaviors, psychosocial factors, healthcare access, and perceived barriers to PrEP use. Socio-demographic measures included: age, gender identity, education, employment status, duration of residence in Tijuana, and incarceration history. Frequency of illicit drug use and routes of administration (e.g., injecting) were assessed in the past month for marijuana, methamphetamine, cocaine, heroin, tranquilizers, inhalants, ecstasy, amyl nitrate, barbiturates, gamma-hydroxybutyrate, and ketamine. Alcohol use in the past year was measured using the Alcohol Use Disorders Identification Test (AUDIT), with hazardous alcohol consumption defined as a score ≥8 [45]. With respect to psychosocial factors, participants were asked about their perceived lifetime risk of getting HIV (very likely; likely; neither unlikely nor likely; unlikely; very unlikely). Social support was measured using the 8-item Modified Medical Outcome Study Social Support Survey, which assesses one’s level of social support (e.g., “If you needed it, how often is someone available to turn to for suggestions about how to deal with a personal problem?”) on a scale from 1 (“none of the time”) to 5 (“all of the time”) [46]. Social support scores were computed by averaging responses across items and transforming the resulting average to a score on a 100-point scale; higher scores indicate more social support. Outness about having sex with men was assessed by asking participants to describe their level of “outness” on a scale from 1 (“not out to anyone”) to 7 (“out to everyone”) [47]. Depression was measured using the 10-item Center for Epidemiologic Studies Depression Scale (CESD-10), with depression defined as a score ≥10 [48]. Healthcare access questions assessed whether participants had seen a HCP and been tested for HIV in the past year.
Participants were then given basic information about PrEP, including its effectiveness, the importance of daily adherence, and potential side-effects. To assess awareness and use of PrEP, participants were asked whether they had ever heard of PrEP and, if aware, whether they had ever taken PrEP. To assess willingness to use PrEP, participants were asked how willing they would be to take PrEP if available in Mexico for free and at a cost. Participants who were willing to pay for PrEP, were asked how much they would be willing to spend monthly in Mexican pesos (≤150; 151–350; 351–550; 551–750; 751–950; ≥951). Perceived barriers to PrEP use were assessed by asking participants to indicate their level of agreement with 12 statements about why someone would not want to use PrEP using 5-point Likert scale responses (strongly disagree; disagree; neither agree nor disagree; agree; strongly agree). The statements were developed to assess important barriers to PrEP use identified in previous research [15–17, 20, 23, 49] across four domains: (1) PrEP attributes (e.g., “PrEP costs too much), (2) individual (e.g., “I am at low risk for HV”), (3) interpersonal (e.g., “Partners will expect me to have CAI if I take PrEP), and (4) structural (e.g., “I will receive poor healthcare if HCPs know I have sex with men”).
Finally, participants completed a sexual network survey assessing socio-demographics, HIV status (HIV-negative; HIV-positive; unknown), and sexual and substance use behaviors with ≤20 anal or vaginal sexual partners in the past 4 months. We considered participants’ responses for partners they identified as cisgender male and transgender female (since the likelihood of sexual exposure to HIV is greater with these partners than that with cisgender female partners [37]) to classify participants with respect to whether they had any HIV-positive or status unknown partners, engaged in CAI, used alcohol or illicit drugs before or during sex, and engaged in any transactional sex (i.e., gave or received something of value in exchange for sex) in the past 4 months.
Participants received 450 Mexican pesos for completing the survey and those recruited via RDS received an additional 100 Mexican pesos for each of their peer-recruits that successfully enrolled in the study. All participants provided written informed consent and study procedures were approved by institutional review boards at the University of California, San Diego and Universidad Xochicalco in Tijuana.
Statistical analysis
We conducted an exploratory LCA to identify distinct classes of participants with respect to perceived barriers to PrEP use. LCA probabilistically assigns individuals with similar response patterns on a series of observed measures to distinct classes of an unobserved latent variable [30–32]. For our LCA, we dichotomized participants’ Likert-scale responses to the 12 items measuring perceived barriers to PrEP use (strongly disagree, disagree, or neither agree nor disagree vs. agree or strongly agree), fit a series of models using those binary indicators with one to five classes, and examined the distribution of the log-likelihood values for each model to determine whether a maximum likelihood (ML) solution could be identified [50]. Although we added Bayesian priors (1.0) to stabilize parameter estimation and fit these models using 100 random starting values to facilitate the identification of an ML solution [51], we were unable to identify an ML solution for models with more than two classes due to the sparseness of our data (212 possible response patterns).
To help facilitate the identification of an ML solution, we considered two different methods of reducing the amount of unknown information [50]. First, we considered all 12 indicators with Bayesian priors (1.0) and imposed parameter restrictions that constrained parameter estimates to be equivalent across classes for two indicators: “I am concerned about talking to HCPs about having sex with men” and “People might assume I am promiscuous.” These indicators were chosen because they were least prevalent within their respective domains and had similar item-response probabilities within classes to two other indicators (i.e., “I am concerned about talking to HCPs about having sex with men” was similar to “I will receive poor healthcare if HCPs know I have sex with men” and “People might assume I am promiscuous” was similar to “People might assume I am HIV+”) [51]. Second, we considered only 10 indicators, excluding “I am concerned about talking to HCPs about having sex with men” and “People might assume I am promiscuous.” Using the first method we were again unable to identify an ML solution for models with more than two classes. However, using the second method, we were able to identify models with one to three classes. Therefore, we proceeded with the models identified via the second method. Next, we examined bivariate residuals (BVRs) to determine whether the local independence assumption underlying LCA may be violated (S1 Table) and allowed for local dependence between pairs of indicators with statistically significant associations (i.e., BVR>3.84) [51, 52]. To select our final model, we considered fit statistics (Akaike’s information criteria [AIC], Bayesian information criteria [BIC], sample size-adjusted Bayesian information criteria [a-BIC]) and entropy as a measure of classification certainty. Lower AIC and BIC values and higher values of entropy were considered indicators of better model fit. In addition, we examined class separation (e.g., distinct patterns of item-response probabilities across latent classes), within-class homogeneity (e.g., similarity of item-response probability patterns within classes), and the meaningfulness of identified classes [50, 51].
We then examined whether class membership was associated with socio-demographic, substance use, psychosocial, healthcare access, and sexual risk factors using Vermunt’s bias-adjusted three-step approach [53]. First, we used the posterior probabilities of class membership estimated from our final model (selected in Step 1) to assign participants to one of three classes based on the proportional assignment method (Step 2). Next, we used multinomial logistic regression to examine the relationship between class membership and the factors of interest (Step 3) applying Vermunt’s ML method to correct for classification errors in Step 2 and a robust variance estimator [53, 54]. Based on previous research examining factors associated with barriers to PrEP use and willingness to use PrEP among MSM [15, 21, 26, 55], we created directed acyclic graphs (DAGs) [56] to illustrate potential relationships among the factors of interest and class membership. We then used these DAGs to identify confounders of the relationship between each factor of interest and class membership. Finally, we constructed individual models for each factor to account for the possibility that a confounder of the relationship between one factor and class membership could be a mediator of the relationship between another factor and class membership [57, 58]. Data management and descriptive analyses were conducted using SAS 9.4 [59] and the LCA was conducted using Latent GOLD 5.1 [51].
Results
Sample characteristics
Our sample (N = 364) had a mean age of 38.3 years (SD: 11.5), mostly identified as Hispanic (99%), and approximately half reported at least a high school education (42%) and having seen a HCP in the past year (51%) (Table 1). Despite low prior PrEP awareness (17%) and use (5%), 88% were willing to take PrEP if it was available for free. Of participants willing to pay for PrEP (60%), 30% reported that they would only be willing to pay for it if it cost ≤150 Mexican pesos (~8.0 US dollars).
Table 1. Socio-demographic, substance use, sexual risk, psychosocial, and healthcare access characteristics among MSM in Tijuana, Mexico (N = 364).
| n (%) | |
|---|---|
| Recruitment Method | |
| RDS | 187 (51.4) |
| VBS | 177 (48.6) |
| Socio-demographics | |
| Median age (years) | 39 (IQR: 28.5–46.5) |
| Age (years) | |
| 18–24 | 49 (13.5) |
| 25–29 | 53 (14.6) |
| 30–39 | 84 (23.1) |
| ≥40 | 178 (48.9) |
| Hispanic ethnicity | 360 (98.9) |
| Gay identifying | 128 (35.2) |
| ≥ High school education | 151 (41.5) |
| Employed | 220 (60.4) |
| Median duration of residence in Tijuana (years) | 9 (IQR: 3–21) |
| Incarceration history | 157 (43.1) |
| Psychosocial factors | |
| Social support, mean score | 56.3 (SD: 34.8) |
| Outness about having sex with men, mean score | 4.0 (SD: 2.5) |
| Depression (CESD-D ≥10) | 163 (44.8) |
| Substance use | |
| Illicit drug use (≤1 month)a | 189 (51.9) |
| Marijuana | 128 (35.2) |
| Methamphetamine | 159 (43.7) |
| Cocaine | 45 (12.4) |
| Heroin | 62 (17.0) |
| Tranquilizers | 52 (14.3) |
| Inhalants | 9 (2.5) |
| Ecstasy | 20 (5.5) |
| Amyl nitrite (poppers) | 26 (7.1) |
| Barbiturates | 15 (4.1) |
| GHB | 8 (2.2) |
| Ketamine | 5 (1.4) |
| Injection drug use | 63 (17.3) |
| Hazardous alcohol consumption (≤12 months) | 196 (53.9) |
| Sexual Risk Behaviors (past 4 months) | |
| Any HIV-positive/status unknown partners | 158 (43.4) |
| Any substance use before/during sex with partners | 266 (73.1) |
| Gave/received something of value to/from partners in exchange for sex |
157 (43.1) |
| Any CAI with partners | 251 (69.2) |
| Healthcare Access | |
| Received care from a HCP, past 12 months | 186 (51.1) |
| HIV testing (≤12 months) | 161 (44.2) |
| PrEP awareness | 62 (17.0) |
| PrEP use (n = 62) | 3 (4.8) |
| Willing to use PrEP if available for free | 319 (87.6) |
| Willing to use PrEP if available, but not for free | 217 (59.6) |
| If PrEP were available, but not for free, how much would be willing to pay per month (pesos) (n = 217):b |
|
| ≤150 | 64 (29.5) |
| 150–350 | 40 (18.4) |
| 351–550 | 46 (21.2) |
| 551–750 | 23 (10.6) |
| 751–950 | 11 (5.1) |
| 950+ | 33 (15.2) |
| Perceived risk of HIV (likely/very likely) | 179 (49.2) |
Abbreviations: CESD-D = center for epidemiologic studies depression scale; MSM = men who have sex with men; RDS = respondent-driven sampling; VBS = venue-based sampling; HCP = healthcare provider; CAI = condomless anal intercourse; PrEP = pre-exposure prophylaxis; SD = standard deviation; IQR = interquartile range.
a Excluding marijuana.
b 2016–2017 conversion rate: 1 US dollar = 18.74 Mexican pesos.
Perceived barriers to PrEP use
Perceived barriers to PrEP use in the PrEP attribute domain were most common: “PrEP costs too much” (50%) and “I am concerned about long-term side-effects” (41%) (Table 2). Followed by “I have limited access to healthcare services” (32%) in the structural domain, “Taking PrEP might tempt me to have CAI” (31%) in the individual domain, and “People might assume I am HIV+” (28%) in the interpersonal domain.
Table 2. Perceived barriers to PrEP use among MSM in Tijuana, Mexico (N = 364).
| Barriers | Proportion Agree/ Strongly Agree |
|---|---|
| Product Attributes Domain | |
| PrEP costs too much | 50.0 |
| I am concerned about long-term side effects | 40.6 |
| PrEP does not fully protect against HIV | 20.3 |
| Individual Domain | |
| I am at low risk for HIV/AIDS | 23.6 |
| I would have trouble taking PrEP daily | 26.9 |
| Taking PrEP might tempt me to have CAI | 31.0 |
| Interpersonal Domain | |
| Partners will expect me to have CAI if I take PrEP | 26.4 |
| People might assume I am HIV+ | 27.8 |
| People might assume I am promiscuous | 26.1 |
| Structural Domain | |
| I have limited access to healthcare services | 31.6 |
| I am concerned about talking to HCP about having sex with men | 15.1 |
| I will receive poor healthcare if HCP knows I have sex with men | 16.5 |
Abbreviations: CAI = condomless anal intercourse; HCP = healthcare provider; PrEP = pre-exposure prophylaxis
Latent classes of perceived barriers to PrEP use
Of the three identified models, the AIC and BIC values were lowest for the three-class model (Table 3), suggesting that it fit the data best. However, because BVRs from all three models indicated a violation of the local independence assumption (S1 Table), we re-fit the two- and three-class models with direct effects between indicators with BVRs >3.84 to account for the relationships between those indicators, which improved the AIC and BIC values for both models relative to those without direct effects. We then considered item-response probabilities from the two models with direct effects and found that the three-class model had better within class homogeneity and between class separation relative to the two-class model and also identified more meaningful classes than the two-class model (S2 Table). Thus, we selected the three-class model with direct effects as our final model.
Table 3. Fit statistics across LCA models with an ML solution.
| LCA Model | Log Likelihood | Likelihood Ratio Test |
AIC | a-BIC | Entropy | DF | X2 |
|---|---|---|---|---|---|---|---|
| 1-class | -2132.06 | 1308.31 | 4284.11 | 4291.36 | 1.00 | 354.00 | 105778.53 |
| 2-class | -1809.32 | 662.83 | 3660.63 | 3675.85 | 0.83 | 343.00 | 1405.15 |
| 3-class | -1756.60 | 557.41 | 3577.21 | 3600.40 | 0.77 | 332.00 | 1266.21 |
| 2-class DE | -1749.36 | 542.91 | 3558.71 | 3580.45 | 0.74 | 334.00 | 1287.97 |
| 3-class DE | -1735.44 | 515.07 | 3540.87 | 3566.23 | 0.74 | 329.00 | 1180.03 |
Abbreviations: AIC = Akaike’s information criteria; BIC = Bayesian information criteria; a-BIC = sample-size adjusted Bayesian information criteria; DE = direct effects; DF = degrees of freedom; LCA = latent class analysis; ML = maximum likelihood.
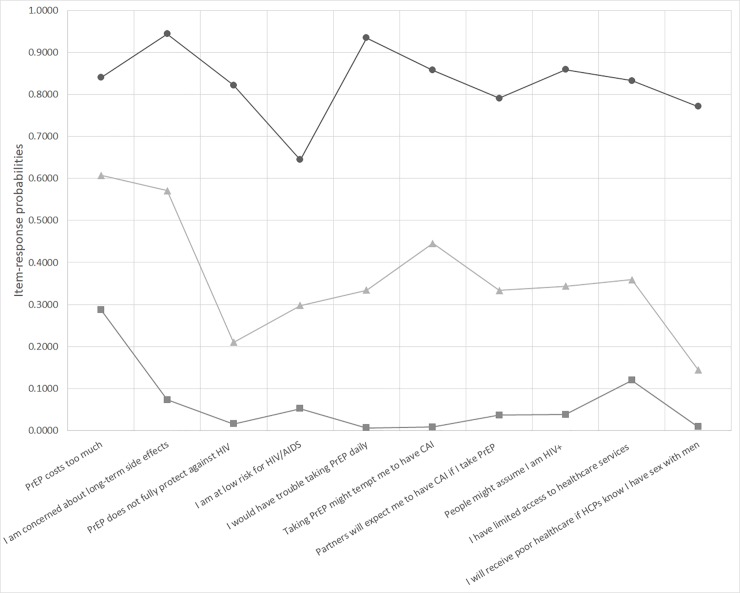
Based on the item-response probabilities for each of the perceived barriers (i.e., indicators) across classes identified by our final model (S2 Table; Fig 1), we labelled the classes (1) high level of perceived barriers (12%), (2) low level of perceived barriers (43%), and (3) perceived PrEP attribute barriers (45%). Participants in the “high level of perceived barriers” class had a high probability (0.64–0.94) of perceiving all of the measured barriers as barriers to PrEP use, while those in the “low level of perceived barriers” class had a low probability (0.007–0.288) of perceiving any of the measured barriers as barriers to PrEP use. Participants in the “perceived PrEP attribute barriers” class had a moderately high probability of perceiving cost (0.61) and side-effects (0.57) as barriers to PrEP use.
Fig 1. Item-response probabilities across classes of MSM in Tijuana, Mexico with varying patterns of perceived barriers to PrEP use as identified by Latent Class Analysis (N = 364).
Identified classes consist of MSM with high-levels of perceived barriers (circle; 12.0%), low-levels of perceived barriers (square; 43.0%), and those who perceived PrEP attribute barriers (triangle; 45.0%). Abbreviations: CAI = condomless anal intercourse; HCP = healthcare provider; MSM = men who have sex with men; PrEP = pre-exposure prophylaxis.
Factors associated with latent class membership
In multivariable analyses (Table 4), membership in the “high level of perceived barriers” class (vs. the “low level of perceived barriers” class) was negatively associated with greater social support (AOR: 0.99; 95% CI: 0.98–1.00) and positively associated with a history of incarceration (AOR: 2.44, 95% CI: 1.04–5.73). Membership in the “perceived PrEP attribute barriers” class, compared to the “low level of perceived barriers” class, was positively associated with receiving care from a HCP in the past year (AOR: 2.78; 95% CI: 1.41, 5.45) and negatively associated with having any HIV-positive or status unknown partners (AOR: 0.56; 95% CI: 0.31, 1.01).
Table 4. Socio-demographic, substance use, sexual risk, psychosocial, and healthcare access characteristics associated with membership in distinct classes with respect to perceived barriers to PrEP use among MSM in Tijuana, Mexico (N = 364).
| Perceived PrEP Attribute Barriers | High Level of Perceived Barriers | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | AOR | 95% CI | OR | 95% CI | AOR | 95% CI | |
| Socio-demographics | ||||||||
| Age (years) | 0.99 | (0.97, 1.01) | 0.99 | (0.97, 1.01)b | 1.01 | (0.99, 1.04) | 1.01 | (0.99, 1.04)b |
| ≥ High school education | 1.20 | (0.71, 2.03) | 1.15 | (0.67, 1.96)c | 0.41 | (0.17, 0.96) | 0.43 | (0.18, 1.02)c |
| Duration of residence in Tijuana (years) | 1.00 | (0.98, 1.02) | 1.00 | (0.98, 1.02)d | 0.98 | (0.95, 1.01) | 0.98 | (0.96, 1.01)d |
| Incarceration history | 0.95 | (0.55, 1.62) | 1.08 | (0.60, 1.95)e | 2.58 | (1.22, 5.47) | 2.44 | (1.04, 5.73)e |
| Employed | 1.28 | (0.74, 2.20) | 1.25 | (0.71, 2.19)f | 0.50 | (0.24, 1.03) | 0.68 | (0.30, 1.53)f |
| Psychosocial factors | ||||||||
| Social support | 1.00 | (0.99, 1.01) | 1.00 | (0.99, 1.01)g | 0.99 | (0.98, 1.00) | 0.99 | (0.98, 1.00)g |
| Outness about having sex with men | 0.95 | (0.86, 1.06) | 0.94 | (0.84, 1.05)h | 0.79 | (0.66, 0.93) | 0.84 | (0.69, 1.02)h |
| Depression (CESD-D ≥10) | 0.95 | (0.56, 1.62) | 0.94 | (0.54, 1.65)i | 1.77 | (0.86, 3.66) | 1.10 | (0.49, 2.45)i |
| Substance use | ||||||||
| Illicit drug use (≤1 month)a | 1.12 | (0.66, 1.88) | 1.09 | (0.58, 2.06)j | 2.42 | (1.13, 5.19) | 1.57 | (0.61, 4.01)j |
| Hazardous alcohol consumption (≤12 months) |
0.65 | (0.38, 1.10) | 0.62 | (0.35, 1.08)j | 0.75 | (0.37, 1.55) | 0.66 | (0.30, 1.43)j |
| Sexual Risk Behaviors (past 4 months) | ||||||||
| Any HIV-positive/status unknown partners | 0.58 | (0.34, 0.99) | 0.56 | (0.31, 1.01)k | 0.97 | (0.47, 1.99) | 0.91 | (0.40, 2.05)k |
| Any substance use before/during sex with partners |
0.75 | (0.42, 1.34) | 0.85 | (0.42, 1.74)k | 1.36 | (0.57, 1.67) | 0.76 | (0.20, 2.82)k |
| Gave/received something of value to/from partners in exchange for sex |
0.98 | (0.58, 1.67) | 0.95 | (0.53, 1.72)k | 3.02 | (1.41, 6.48) | 1.96 | (0.76, 5.04)k |
| Any CAI with partners | 0.86 | (0.49, 1.51) | 0.91 | (0.49, 1.66)l | 1.64 | (0.71, 3.81) | 1.87 | (0.54, 6.44)l |
| Healthcare Access | ||||||||
| Received care from a HCP (≤12 months) | 2.07 | (1.21, 3.53) | 2.78 | (1.41, 5.45)m | 0.72 | (0.34, 1.52) | 1.26 | (0.49, 3.23)m |
| HIV testing (≤12 months) | 1.67 | (0.99, 2.84) | 1.62 | (0.91, 2.89)m | 0.78 | (0.36, 1.68) | 1.14 | (0.48, 2.72)m |
| PrEP awareness | 1.05 | (0.54, 2.03) | 0.82 | (0.37, 1.81)n | 0.36 | (0.08, 1.57) | 0.44 | (0.03, 5.67)n |
| Perceived lifetime risk of HIV (likely/very likely) | 0.88 | (0.52, 1.48) | 0.98 | (0.52, 1.82)o | 1.10 | (0.54, 2.26) | 0.85 | (0.35, 2.03)o |
a Excluding marijuana.
b No identified confounders.
c Adjusted for age.
d Adjusted for variable in (c); additionally, adjusted for education.
e Adjusted for variables in (c) and (d); additionally, adjusted for duration of residence in Tijuana.
f Adjusted for variables in (c), (d), and (e); additionally, adjusted for incarceration history.
g Adjusted for variables in (c), (d), (e), and (f); additionally, adjusted for employment.
h Adjusted for variables in (c), (d), (e), (f), and (g); additionally, adjusted for social support.
i Adjusted for variables in (c), (d), (e), (f), (g), and (h); additionally, adjusted for outness.
j Adjusted for variables in (c), (d), (e), (f), (g), (h), and (i); additionally, adjusted for depression.
k Adjusted for variables in (c), (d), (e), (f), (g), (h), (i), and (j); additionally, adjusted for illicit drug use and hazardous alcohol consumption.
l Adjusted for variables in (c), (d), (e), (f), (g), (h), (i), (j), and (k); additionally, adjusted for HIV status of partners, substance use before/during sex with partners, and
exchange of something of value for sex with partners.
m Adjusted for variables in (c), (d), (e), (f), (g), (h), (i), (j), (k), and (l); additionally, adjusted for any CAI.
n Adjusted for variables in (c), (d), (e), (f), (g), (h), (i), (j), (k), (l), and (m); additionally, adjusted for receipt of care from a HCP and HIV testing.
o Adjusted for variables in (c), (d), (e), (f), (g), (h), (i), (j), (k), (l), (m), and (n); additionally, adjusted for PrEP awareness.
Abbreviations: CESD-D = center for epidemiologic studies depression scale; MSM = men who have sex with men; HCP = healthcare provider; CAI = condomless anal intercourse;
PrEP = pre-exposure prophylaxis.
Reference group = low level of perceived barriers.
Discussion
We assessed perceived barriers to PrEP use across four domains (PrEP attribute, individual, interpersonal, and structural) among HIV-negative MSM in Tijuana, Mexico. Using exploratory LCA, we identified three classes of participants with respect to patterns of perceived barriers to PrEP use. It is promising for future PrEP implementation that 43% of participants endorsed few barriers to PrEP use. However, 45% of participants perceived PrEP attributes, including cost and side-effects, as barriers to PrEP use, while 12% perceived multiple barriers to PrEP use. Although our LCA was exploratory, our findings provide important insight on how PrEP programs might be developed to best serve the needs of MSM in Tijuana. More specifically, our results suggest that a range of comprehensive HIV prevention packages may be needed to enhance PrEP uptake and adherence across subgroups of MSM in this setting.
Consistent with prior research among MSM in LMIC [16, 18, 55], PrEP attributes were commonly perceived barriers to PrEP use among participants in both the “perceived PrEP attribute barriers” and “high level of perceived barriers” classes. Although antiretroviral therapy (ART) is universally available in Mexico [60], it is currently unknown how PrEP will be incorporated into Mexico’s healthcare system. Branded FTC/TDF can cost up to 850 US dollars per month in high-income countries [61], while generic FTC/TDF, which is used as ART in some LMIC [61, 62], is estimated to cost 6.5 US dollars per month (~123 Mexican pesos). In our study, 30% of participants who reported that they would be willing to pay for PrEP said they would only do so if it cost ≤150 Mexican pesos (~8.0 US dollars) per month. Thus, making generic FTC/TDF available as PrEP in Mexico may enhance its acceptability to many MSM in Tijuana, while its integration into Mexico’s public healthcare system may fully address concerns related to cost within this vulnerable population. Although PrEP use has been associated with several mild, short-term side-effects [63], and non-progressive and reversible declines in renal function and bone density [64], it is generally considered safe and well tolerated [65]. Given that almost half (45%) of our sample was in the “perceived PrEP attribute barriers” class, raising potential PrEP users’ awareness of cost coverage options that may enhance its affordability and increasing their knowledge of the nature and duration of potential side-effects may significantly improve PrEP uptake among MSM in Tijuana.
It is promising that MSM with any HIV-positive or status unknown partners were less likely to be in the “perceived PrEP attribute barriers” class, indicating those who could benefit the most from PrEP may experience few barriers to PrEP uptake. Additionally, we found that having seen a HCP in the past year was associated with membership in this class. MSM already engaged in healthcare may perceive themselves to be healthy and thus at low risk for HIV infection. As such, they may feel the additional cost and potential side-effects of PrEP use are not worth the benefits. This finding suggests that achieving an increased level of PrEP coverage may be easily addressed in the context of provider-delivered PrEP education. However, the impact of such education on PrEP uptake may also depend on HCPs’ knowledge and perceptions of PrEP, which previous research suggests is linked to their willingness to prescribe PrEP [66, 67]. There is also evidence that heterosexism may decrease HCPs’ willingness to prescribe PrEP to MSM [68, 69], which could adversely affect PrEP provision to sexual minorities in Tijuana where they remain highly stigmatized. Thus, efforts to raise HCPs’ awareness of the benefits of PrEP and bolster their capacity to deliver culturally competent PrEP-related care to their sexual minority patients, including patient-centered, non-judgmental sexual risk assessment, may be critical to the success of provider-delivered PrEP education in Tijuana.
However, to achieve complete PrEP coverage among MSM in Tijuana, additional efforts may be needed to address the range of barriers to PrEP use endorsed by those in the “high level of perceived barriers” class within our sample. For example, a history of incarceration was associated with membership in this class. Persons with a history of incarceration often face elevated rates of unemployment, substance use, mental illness, and inadequate access to healthcare [70–72], which may limit PrEP uptake among this population. A peer navigation intervention initiated pre-release, which addressed social-environmental factors and incorporated individualized problem-solving techniques, was shown to effectively support viral suppression maintenance among HIV-positive men and TW released from jail [73]. Interventions which assess PrEP interest and eligibility during incarceration and provide peer navigation services post-release may support PrEP uptake and adherence and be particularly effective for MSM like those in the “high level of perceived barriers” class. However, lower levels of social support were also associated with being in this class. In Mexico, cultural norms of homophobia and machismo often inhibit MSM from being able to “come out” and positively experience their sexual identity [74]. This can cause psychological distress among MSM, resulting in withdrawal from social support networks (e.g., family and friends) [75, 76], which can impact their ability to access culturally competent healthcare [41, 74, 77]. As such, community-level programs which reduce negative social attitudes towards MSM in combination with counseling interventions to help MSM identify supportive social network members may be critical to PrEP use and adherence among MSM in Tijuana.
Our findings should be considered in the context of several limitations. First, our analysis was based on cross-sectional data, which limits our ability to make causal inferences. Second, participants were recruited using non-probability sampling methods, thus our findings may not be generalizable to all MSM in Tijuana or other settings. However, MSM experience significant levels of stigma and discrimination related to being sexual minorities, therefore using VBS and RDS may have increased our ability to access this hard-to-reach population. Third, this study is based on self-reported data, which may have been under-reported due to recall or social desirability bias. Participants may have also overstated their willingness to use PrEP given interviewers had just informed them of its potential benefits. However, interviewers were trained to encourage honest reporting of sensitive information. Fourth, we report on perceived barriers to PrEP use among MSM in Tijuana, which may differ from the actual barriers they may face once PrEP is implemented in Tijuana. Finally, because we were unable to identify ML solutions for models with more than three classes, our findings should be examined further in future research with a larger sample of MSM in the context of a confirmatory LCA.
Conclusion
Despite these limitations, our study is the first to examine perceived barriers to PrEP use among MSM in Tijuana. These findings, while exploratory, suggest that subgroups with respect to perceived barriers do exist among MSM in Tijuana and provide insight on the range of comprehensive HIV prevention packages that may be needed to achieve sufficient PrEP coverage within this vulnerable population.
Supporting information
(DOCX)
(DOCX)
(CSV)
(CSV)
Acknowledgments
The authors thank the study participants and staff without whom this study would not have been possible.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This work was supported by grants from the National Institute on Drug Abuse: K01DA040543 (HAP), R01DA037811 (TLP), and T32DA023356. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4(12):e339 Epub 2007/12/07. 10.1371/journal.pmed.0040339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367–77. Epub 2012/07/24. 10.1016/S0140-6736(12)60821-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. Epub 2010/11/26. 10.1056/NEJMoa1011205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. Epub 2012/07/13. 10.1056/NEJMoa1108524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. Epub 2012/07/13. 10.1056/NEJMoa1110711 . [DOI] [PubMed] [Google Scholar]
- 6.Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90. Epub 2013/06/19. 10.1016/S0140-6736(13)61127-7 . [DOI] [PubMed] [Google Scholar]
- 7.LeVasseur MT, Goldstein ND, Tabb LP, Olivieri-Mui BL, Welles SL. The Effect of PrEP on HIV Incidence Among Men Who Have Sex With Men in the Context of Condom Use, Treatment as Prevention, and Seroadaptive Practices. J Acquir Immune Defic Syndr. 2018;77(1):31–40. Epub 2017/09/30. 10.1097/QAI.0000000000001555 . [DOI] [PubMed] [Google Scholar]
- 8.Punyacharoensin N, Edmunds WJ, De Angelis D, Delpech V, Hart G, Elford J, et al. Effect of pre-exposure prophylaxis and combination HIV prevention for men who have sex with men in the UK: a mathematical modelling study. Lancet HIV. 2016;3(2):e94–e104. Epub 2016/02/06. 10.1016/S2352-3018(15)00056-9 . [DOI] [PubMed] [Google Scholar]
- 9.Gomez GB, Borquez A, Caceres CF, Segura ER, Grant RM, Garnett GP, et al. The potential impact of pre-exposure prophylaxis for HIV prevention among men who have sex with men and transwomen in Lima, Peru: a mathematical modelling study. PLoS Med. 2012;9(10):e1001323 Epub 2012/10/12. 10.1371/journal.pmed.1001323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jenness SM, Goodreau SM, Rosenberg E, Beylerian EN, Hoover KW, Smith DK, et al. Impact of the Centers for Disease Control's HIV Preexposure Prophylaxis Guidelines for Men Who Have Sex With Men in the United States. J Infect Dis. 2016;214(12):1800–7. Epub 2016/07/16. 10.1093/infdis/jiw223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. 2014. Available from: http://apps.who.int/iris/bitstream/handle/10665/128048/9789241507431_eng.pdf;jsessionid=8DD2748F02217FD1BE64637FC6FAB594?sequence=1. [PubMed]
- 12.Caceres CF, Borquez A, Klausner JD, Baggaley R, Beyrer C. Implementation of pre-exposure prophylaxis for human immunodeficiency virus infection: progress and emerging issues in research and policy. J Int AIDS Soc. 2016;19(7(Suppl 6)):21108 Epub 2016/10/21. 10.7448/IAS.19.7.21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoornenborg E, Krakower DS, Prins M, Mayer KH. Pre-exposure prophylaxis for MSM and transgender persons in early adopting countries. AIDS. 2017;31(16):2179–91. Epub 2017/10/11. 10.1097/QAD.0000000000001627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strauss BB, Greene GJ, Phillips G, 2nd, Bhatia R, Madkins K, Parsons JT, et al. Exploring Patterns of Awareness and Use of HIV Pre-Exposure Prophylaxis Among Young Men Who Have Sex with Men. AIDS Behav. 2017;21(5):1288–98. Epub 2016/07/13. 10.1007/s10461-016-1480-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men. Curr HIV Res. 2013;11(7):520–7. Epub 2014/01/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galea JT, Kinsler JJ, Salazar X, Lee SJ, Giron M, Sayles JN, et al. Acceptability of pre-exposure prophylaxis as an HIV prevention strategy: barriers and facilitators to pre-exposure prophylaxis uptake among at-risk Peruvian populations. Int J STD AIDS. 2011;22(5):256–62. Epub 2011/05/17. 10.1258/ijsa.2009.009255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brooks RA, Kaplan RL, Lieber E, Landovitz RJ, Lee SJ, Leibowitz AA. Motivators, concerns, and barriers to adoption of preexposure prophylaxis for HIV prevention among gay and bisexual men in HIV-serodiscordant male relationships. AIDS care. 2011;23(9):1136–45. Epub 2011/04/09. 10.1080/09540121.2011.554528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chakrapani V, Newman PA, Shunmugam M, Mengle S, Varghese J, Nelson R, et al. Acceptability of HIV Pre-Exposure Prophylaxis (PrEP) and Implementation Challenges Among Men Who Have Sex with Men in India: A Qualitative Investigation. AIDS Patient Care STDS. 2015;29(10):569–77. Epub 2015/09/09. 10.1089/apc.2015.0143 . [DOI] [PubMed] [Google Scholar]
- 19.Perez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP Uptake Among Racially/Ethnically Diverse Young Men Who Have Sex With Men: The P18 Study. AIDS Educ Prev. 2015;27(2):112–25. Epub 2015/04/29. 10.1521/aeap.2015.27.2.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDS. 2013;27(4):248–54. Epub 2013/04/10. 10.1089/apc.2012.0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen SE, Vittinghoff E, Bacon O, Doblecki-Lewis S, Postle BS, Feaster DJ, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP demonstration project. J Acquir Immune Defic Syndr. 2015;68(4):439–48. Epub 2014/12/17. 10.1097/QAI.0000000000000479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rendina HJ, Whitfield TH, Grov C, Starks TJ, Parsons JT. Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): Findings from a large cohort of gay and bisexual men in the U.S. Soc Sci Med. 2017;172:115–23. Epub 2016/11/22. 10.1016/j.socscimed.2016.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.King HL, Keller SB, Giancola MA, Rodriguez DA, Chau JJ, Young JA, et al. Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS Behav. 2014;18(9):1722–5. Epub 2014/07/16. 10.1007/s10461-014-0845-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kubicek K, Arauz-Cuadra C, Kipke MD. Attitudes and perceptions of biomedical HIV prevention methods: voices from young men who have sex with men. Arch Sex Behav. 2015;44(2):487–97. Epub 2015/01/31. 10.1007/s10508-014-0398-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oldenburg CE, Mitty JA, Biello KB, Closson EF, Safren SA, Mayer KH, et al. Differences in Attitudes About HIV Pre-Exposure Prophylaxis Use Among Stimulant Versus Alcohol Using Men Who Have Sex with Men. AIDS Behav. 2016;20(7):1451–60. Epub 2015/10/16. 10.1007/s10461-015-1226-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peng P, Su S, Fairley CK, Chu M, Jiang S, Zhuang X, et al. A Global Estimate of the Acceptability of Pre-exposure Prophylaxis for HIV Among Men Who have Sex with Men: A Systematic Review and Meta-analysis. AIDS Behav. 2018;22(4):1063–74. Epub 2017/02/09. 10.1007/s10461-017-1675-z . [DOI] [PubMed] [Google Scholar]
- 27.Pinto RM, Berringer KR, Melendez R, Mmeje O. Improving PrEP Implementation Through Multilevel Interventions: A Synthesis of the Literature. AIDS Behav. 2018. Epub 2018/06/07. 10.1007/s10461-018-2184-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Draper BL, Fowkes FJI, Oo ZM, Thein ZW, Aung PP, Veronese V, et al. Willingness to use HIV pre-exposure prophylaxis among gay men, other men who have sex with men and transgender women in Myanmar. J Int AIDS Soc. 2017;20(1):21885 Epub 2017/07/26. 10.7448/IAS.20.1.21885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petroll AE, Mosack KE. Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sex Transm Dis. 2011;38(1):63–7. Epub 2010/08/14. 10.1097/OLQ.0b013e3181ebd50f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goodman LA. The analysis of systems of qualitative variables when some of the variables are unobservable. Part IA modified latent structure approach. AJS. 1974;79(5):1179–259. [Google Scholar]
- 31.Goodman LA. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika. 1974;61(2):215–31. [Google Scholar]
- 32.Lazarsfeld PF, Henry NW. Latent structure analysis: Houghton Mifflin Co.; 1968. [Google Scholar]
- 33.Xu W, Zheng Y, Kaufman MR. Predictors of Recent HIV Testing Among Chinese Men Who Have Sex with Men: A Barrier Perspective. AIDS Patient Care STDS. 2018;32(10):408–17. Epub 2018/09/21. 10.1089/apc.2018.0061 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chan PA, Rose J, Maher J, Benben S, Pfeiffer K, Almonte A, et al. A Latent Class Analysis of Risk Factors for Acquiring HIV Among Men Who Have Sex with Men: Implications for Implementing Pre-Exposure Prophylaxis Programs. AIDS Patient Care STDS. 2015;29(11):597–605. Epub 2015/09/22. 10.1089/apc.2015.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCarty-Caplan D, Jantz I, Swartz J. MSM and drug use: A latent class analysis of drug use and related sexual risk behaviors. AIDS Behav. 2014;18(7):1339–51. Epub 2013/09/26. 10.1007/s10461-013-0622-x . [DOI] [PubMed] [Google Scholar]
- 36.Otis J, McFadyen A, Haig T, Blais M, Cox J, Brenner B, et al. Beyond Condoms: Risk Reduction Strategies Among Gay, Bisexual, and Other Men Who Have Sex With Men Receiving Rapid HIV Testing in Montreal, Canada. AIDS Behav. 2016;20(12):2812–26. Epub 2016/03/11. 10.1007/s10461-016-1344-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.UNAIDS. Countries: Mexico 2017. Available from: http://www.unaids.org/en/regionscountries/countries/mexico.
- 38.Pitpitan EV, Goodman-Meza D, Burgos JL, Abramovitz D, Chavarin CV, Torres K, et al. Prevalence and correlates of HIV among men who have sex with men in Tijuana, Mexico. J Int AIDS Soc. 2015;18:19304 Epub 2015/02/12. 10.7448/IAS.18.1.19304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Verduzco IL. Barriers to Sexual Expression and Safe Sex Among Mexican Gay Men: A Qualitative Approach. Am J Mens Health. 2016;10(4):270–84. Epub 2014/12/17. 10.1177/1557988314561490 . [DOI] [PubMed] [Google Scholar]
- 40.Strathdee SA, Magis-Rodriguez C, Mays VM, Jimenez R, Patterson TL. The emerging HIV epidemic on the Mexico-U.S. border: an international case study characterizing the role of epidemiology in surveillance and response. Ann Epidemiol. 2012;22(6):426–38. Epub 2012/05/26. 10.1016/j.annepidem.2012.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pines HA, Goodman-Meza D, Pitpitan EV, Torres K, Semple SJ, Patterson TL. HIV testing among men who have sex with men in Tijuana, Mexico: a cross-sectional study. BMJ open. 2016;6(2):e010388 Epub 2016/02/06. 10.1136/bmjopen-2015-010388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(1_suppl):39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heckathorn DD. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Soc Probl. 1997;44(2):174–99. 10.1525/sp.1997.44.2.03x0221m PubMed PMID: WOS:A1997XE13900003. [DOI] [Google Scholar]
- 44.Salas-Espinoza KJ, Menchaca-Diaz R, Patterson TL, Urada LA, Smith D, Strathdee SA, et al. HIV Prevalence and Risk Behaviors in Male to Female (MTF) Transgender Persons in Tijuana, Mexico. AIDS Behav. 2017;21(12):3271–8. Epub 2017/10/17. 10.1007/s10461-017-1931-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction. 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 46.Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–16. Epub 2012/07/24. 10.1016/j.jclinepi.2012.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease C, Prevention. HlV/STD risks in young men who have sex with men who do not disclose their sexual orientation—six U.S. cities, 1994–2000. MMWR Morb Mortal Wkly Rep. 2003;52(5):81–6. Epub 2003/02/18. . [PubMed] [Google Scholar]
- 48.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med. 1999;159(15):1701–4. Epub 1999/08/17. 10.1001/archinte.159.15.1701 . [DOI] [PubMed] [Google Scholar]
- 49.Wheelock A, Eisingerich AB, Ananworanich J, Gomez GB, Hallett TB, Dybul MR, et al. Are Thai MSM willing to take PrEP for HIV prevention? An analysis of attitudes, preferences and acceptance. PloS One. 2013;8(1):e54288 Epub 2013/01/24. 10.1371/journal.pone.0054288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences Hoboken, NJ: John Wiley & Sons; 2010. [Google Scholar]
- 51.Vermunt JK, Magidson J. Technical guide for Latent GOLD 5.1: Basic, advanced, and syntax Belmont, MA: Statistical Innovations Inc; 2016. [Google Scholar]
- 52.Hagenaars JA. Latent structure models with direct effects between indicators: local dependence models. Sociol Methods Res. 1988;16(3):379–405. [Google Scholar]
- 53.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Polit Anal. 2010;18(4):450–69. [Google Scholar]
- 54.Bakk Z, Oberski DL, Vermunt JK. Relating Latent Class Assignments to External Variables: Standard Errors for Correct Inference. Polit Anal. 2014;22(4). [Google Scholar]
- 55.Yi S, Tuot S, Mwai GW, Ngin C, Chhim K, Pal K, et al. Awareness and willingness to use HIV pre-exposure prophylaxis among men who have sex with men in low- and middle-income countries: a systematic review and meta-analysis. J Int AIDS Soc. 2017;20(1):21580 Epub 2017/07/12. 10.7448/IAS.20.1.21580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. Epub 1999/01/15. . [PubMed] [Google Scholar]
- 57.Bandoli G, Palmsten K, Chambers CD, Jelliffe-Pawlowski LL, Baer RJ, Thompson CA. Revisiting the Table 2 fallacy: A motivating example examining preeclampsia and preterm birth. Paediatr Perinat Epidemiol. 2018;32(4):390–7. Epub 2018/05/22. 10.1111/ppe.12474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177(4):292–8. Epub 2013/02/02. 10.1093/aje/kws412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.SAS Institute. SAS/STAT 9.4 ed. Cary, NC.
- 60.Bautista-Arredondo S, Colchero MA, Romero M, Conde-Glez CJ, Sosa-Rubi SG. Is the HIV epidemic stable among MSM in Mexico? HIV prevalence and risk behavior results from a nationally representative survey among men who have sex with men. PloS One. 2013;8(9):e72616 Epub 2013/09/17. 10.1371/journal.pone.0072616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.UNAIDS. Oral pre-exposure prophylaxis: putting a new choice in context.2015.
- 62.Hankins C, Macklin R, Warren M. Translating PrEP effectiveness into public health impact: key considerations for decision-makers on cost-effectiveness, price, regulatory issues, distributive justice and advocacy for access. J Int AIDS Soc. 2015;18(4 Suppl 3):19973 Epub 2015/07/23. 10.7448/IAS.18.4.19973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Glidden DV, Amico KR, Liu AY, Hosek SG, Anderson PL, Buchbinder SP, et al. Symptoms, Side Effects and Adherence in the iPrEx Open-Label Extension. Clin Infect Dis. 2016;62(9):1172–7. Epub 2016/01/23. 10.1093/cid/ciw022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mugwanya KK, Baeten JM. Safety of oral tenofovir disoproxil fumarate-based pre-exposure prophylaxis for HIV prevention. Expert Opin Drug Saf. 2016;15(2):265–73. Epub 2015/12/05. 10.1517/14740338.2016.1128412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kojima N, Klausner JD. Is Emtricitabine-Tenofovir Disoproxil Fumarate Pre-exposure Prophylaxis for the Prevention of Human Immunodeficiency Virus Infection Safer Than Aspirin? Open Forum Infect Dis. 2016;3(1):ofv221 Epub 2016/03/08. 10.1093/ofid/ofv221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Adams LM, Balderson BH. HIV providers' likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: a short report. AIDS care. 2016;28(9):1154–8. Epub 2016/02/27. 10.1080/09540121.2016.1153595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Castel AD, Feaster DJ, Tang W, Willis S, Jordan H, Villamizar K, et al. Understanding HIV Care Provider Attitudes Regarding Intentions to Prescribe PrEP. J Acquir Immune Defic Syndr. 2015;70(5):520–8. Epub 2015/08/08. 10.1097/QAI.0000000000000780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Calabrese SK, Earnshaw VA, Krakower DS, Underhill K, Vincent W, Magnus M, et al. A Closer Look at Racism and Heterosexism in Medical Students' Clinical Decision-Making Related to HIV Pre-Exposure Prophylaxis (PrEP): Implications for PrEP Education. AIDS Behav. 2018;22(4):1122–38. Epub 2017/11/21. 10.1007/s10461-017-1979-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Calabrese SK, Earnshaw VA, Underhill K, Krakower DS, Magnus M, Hansen NB, et al. Prevention paradox: Medical students are less inclined to prescribe HIV pre-exposure prophylaxis for patients in highest need. J Int AIDS Soc. 2018;21(6):e25147 Epub 2018/06/26. 10.1002/jia2.25147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bourey C, Stephenson R, Bautista-Arredondo S. Syndemic Vulnerability and Condomless Sex Among Incarcerated Men in Mexico City: A Latent Class Analysis. AIDS Behav. 2018;22(12):4019–33. 10.1007/s10461-018-2216-0 [DOI] [PubMed] [Google Scholar]
- 71.Khan MR, McGinnis KA, Grov C, Scheidell JD, Hawks L, Edelman EJ, et al. Past year and prior incarceration and HIV transmission risk among HIV-positive men who have sex with men in the US. AIDS care. 2019;31(3):349–56. 10.1080/09540121.2018.1499861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Albertie A, Bourey C, Stephenson R, Bautista-Arredondo S. Connectivity, prison environment and mental health among first-time male inmates in Mexico City. Glob Public Health. 2017;12(2):170–84. 10.1080/17441692.2015.1091023 [DOI] [PubMed] [Google Scholar]
- 73.Cunningham WE, Weiss RE, Nakazono T, Malek MA, Shoptaw SJ, Ettner SL, et al. Effectiveness of a Peer Navigation Intervention to Sustain Viral Suppression Among HIV-Positive Men and Transgender Women Released From Jail: The LINK LA Randomized Clinical Trial. JAMA Intern Med. 2018;178(4):542–53. Epub 2018/03/12. 10.1001/jamainternmed.2018.0150 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Diaz R. Latino gay men and HIV: Culture, sexuality, and risk behavior: Routledge; 1998. [Google Scholar]
- 75.Saleh LD, van den Berg JJ, Chambers CS, Operario D. Social support, psychological vulnerability, and HIV risk among African American men who have sex with men. Psychol Health. 2016;31(5):549–64. 10.1080/08870446.2015.1120301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wohl AR, Galvan FH, Myers HF, Garland W, George S, Witt M, et al. Social Support, Stress and Social Network Characteristics Among HIV-Positive Latino and African American Women and Men Who have Sex with Men. AIDS Behav. 2010;14(5):1149–58. 10.1007/s10461-010-9666-3 [DOI] [PubMed] [Google Scholar]
- 77.Santos GM, Beck J, Wilson PA, Hebert P, Makofane K, Pyun T, et al. Homophobia as a barrier to HIV prevention service access for young men who have sex with men. J Acquir Immune Defic Syndr. 2013;63(5):e167–70. Epub 2013/10/19. 10.1097/QAI.0b013e318294de80 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(CSV)
(CSV)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.