Abstract
Functionalized gold nanoparticles (GNPs) with controlled geometrical and optical properties have been the subject of intense research and biomedical applications. This review summarizes recent data and topical problems in nanomedicine that are related to the use of variously sized, shaped, and structured GNPs. We focus on three topical fields in current nanomedicine: (1) use of GNP-based nanoplatforms for the targeted delivery of anticancer and antimicrobial drugs and of genes; (2) GNP-based cancer immunotherapy; and (3) combined chemo-, immuno-, and phototherapy. We present a summary of the available literature data and a short discussion of future work.
1. Introduction
In the past two decades, notable progress has been made in the development of robust and easy-to-use methods for the fabrication of gold nanoparticles (GNPs) with a great variety of sizes, shapes, and multicomponent structures. Alongside this progress, new advanced technologies have been designed to make multifunctional nanoparticles through their functionalization with various molecules ensuring required physicochemical and biological properties. As a result of these technological advances, functionalized GNPs have found numerous promising applications in current biomedicine. The long list of such applications includes, among others, optical bioimaging; biosensorics; chemo- and bioanalytics; targeted delivery of antigens, drugs, DNA, and siRNA; proteomics, and genomics. In fact, GNPs have found interesting applications in almost all branches of current biomedicine, such as diagnostics, treatment, prevention, and even hygiene. Numerous reviews and books [1–9] have considered in detail the published reports on the wet chemical synthesis and surface functionalization of GNPs and their use in biomedicine. Although GNPs have a long history of use [10], a new understanding of the physics behind their remarkable optical properties has been achieved by the development of the plasmonic concept, which relates the enormous near-field and far-field enhancement to collective excitations of free electrons in noble metals. By varying the GNP shape and structure, it is possible to tune the plasmonic resonance from visible to near-infrared (NIR) spectral band, thereby avoiding the shortcomings of many other optical probes. In addition to having unique optical properties, GNPs are low or not at all toxic and can be easily functionalized with biocompatible and stealth biomolecules.
The goal of this review is to provide a short discussion of the recent data on the application of GNPs as a convenient and promising platform in current nanomedicine. Because every year sees the publication of hundreds of papers, we restrict ourselves to three topics: the use of GNPs and gold-based composites (1) as drug carriers, (2) as nanoplatforms in cancer immunotherapy, and (3) in combined chemo- and immunotherapy. The last topic includes GNP-mediated phototherapy, discussed in several recent reviews [11–13]; therefore, we do not consider it here. As distinct from the previous reviews on the biomedical applications of GNPs, we consider a new and breakthrough direction in oncology that is related to the recent advances in cancer immunotherapy and is based on the use of the host immune system. Along with other nanoplatforms, functionalized GNPs have found pioneering applications in cancer immunotherapy. Thus, even a short consideration of this topic seems topical.
2. Gold nanoparticles as drug carriers
2.1. Targeted delivery of anticancer drugs
One of the most promising aspects of GNP use in medicine, currently under intense investigation, is targeted drug delivery [14,15]. The most popular objects for targeted delivery are antitumor preparations [16] and antibiotics [17].
The conventional administration of anticancer drugs leads to several serious drawbacks, including unwanted biodistribution of drugs in the patient’s body, accumulation of drugs in RES organs, poor solubility and stability in blood, limited half-time circulation, and lack of drug-specific binding to pathological sites [18]. Achieving desirable therapeutic effects involves repeated and frequent administration of large total doses, which leads to nonspecific toxicity and dose-dependent adverse side effects. The main benefit of GNP-based drug delivery systems (DDS) is that they can resolve most of the above problems in conventional anticancer therapeutics. GNP-based DDSs provide several significant advantages owing to the following intrinsic properties: (1) very high specific surface (scales like inverse power of size) and loading capacity of drug molecules; (2) efficient functionalization of GNPs through the addition of thiol-containing capping agents; efficient cellular uptake, which can be controlled by varying the particle size, shape, and charge and the chemical composition of the surface coating; and (3) increased selectivity in GNP-based vesicle uptake owing to the multivalent avidity caused by the comparable dimensions of GNP size and the adjacent receptor sites. With current functionalization technologies in hand, the GNP surface can be routinely coated at a ligand density of about 1,000,000 molecules per square micron. Compared to liposomal and polymeric DDS vesicles, the above number is 100- and 1000-fold higher. The optical/plasmonic properties of GNPs can be spectrally tuned to NIR through the variation of size/shape/structure, thus ensuring a penetration depth of up to 10 cm for admissible laser power densities. Furthermore, the unique plasmonic properties can be used for a controlled optically triggered release of the loaded drug at a specific site. Therefore, GNP-based systems have additional modalities for diagnostic/therapeutic treatment.
The major challenges in clinical applications of GNP-based DDSs are related to the biodistribution and long-term toxicity of metal particles through their unwanted accumulation in the patient’s body, slow clearance, and questionable biocompatibility. An additional drawback is the intrinsic toxicity of synthetic agents such as cetyltrimethylammonium bromide (CTAB), as used in gold nanorod fabrication. In many cases, problems can be resolved by replacing CTAB with nontoxic agents [14].
GNPs have been conjugated to a variety of antitumor substances (Table 1), including paclitaxel [19], methotrexate [20], daunorubicin [21], gemcitabine [22], 6-mercaptopurine [23], dodecylcysteine [24], sulfonamide [25], 5-fluorouracil [26], platinum complexes [27], kahalalide F [28], tamoxifen [29], herceptin [30], β-lapachon [31], doxorubicin [32], prospidin [33], camptothecin [34], docetaxel [35], curcumin [36], capecitabine [37], chloroquine [38], berberine hydrochloride [39], bortezomib [40], cetuximab [41], epigallocatechin-3-gallate [42], imatinib [43], epirubicin [44], metelimumab [45], indole-3-carbinol [46], mitoxantrone [47], bleomycin [48], and their combinations [37,49]. Conjugation has been done by simple physical adsorption of antitumor agents on GNPs or by using alkanethiol linkers. The effects of the resulting conjugates have been evaluated both in vitro (primarily), with tumor cell cultures, and in vivo, with mice bearing implanted tumors of various natures and localizations (Lewis lung carcinoma, pancreatic adenocarcinoma, etc.).
Table 1. Antitumor substances conjugated with GNPs.
| Drugs | Particles | Methods of functionalization | Auxiliary substances | Cell lines or animals |
|---|---|---|---|---|
| Paclitaxel | Gold nanospheres, 26 nm | Paclitaxel-SH | PEG-SH TNF |
MC-38; C57/BL6 mice implanted with B16/F10 melanoma cells |
| Methotrexate | Gold nanospheres, 13 nm | Physical adsorption | – | LL2, ML-1, MBT-2, TSGH 8301, TCC-SUP, J82, PC-3, HeLa |
| Daunorubicin | Gold nanospheres, 5 nm, 16 nm | Mercaptopropionic acid as a linker | – | K562/ADM |
| Gemcitabine | Gold nanospheres, 5 nm | Physical adsorption | Cetuximab | PANC-1, AsPC-1, MIA Paca2 |
| 6-Mercaptopurine | Gold nanospheres, 5 nm | Physical adsorption | – | K-562 |
| Dodecylcysteine | Gold nanospheres, 3-6 nm | Physical adsorption | – | EAC |
| 5-Fluorouracil | Gold nanospheres, 2 nm | Thiol ligand | – | MCF-7 |
| Pt(IV) pro drug | Gold nanospheres, 13 nm | Amide linkages | DNA | HeLa, U2OS, PC3 |
| Cisplatin | Gold nanospheres, 5 nm | PEG-SH as a linker | Folic acid, PEG-SH | OV-167, OVCAR-5, HUVEC, OSE |
| Oxaliplatin | Gold nanospheres, 30 nm | PEG-SH as a linker | PEG-SH | A549, HCT116, HCT15, HT29, RKO |
| Kahalalide F | Gold nanospheres, 20 nm, 40 nm | Physical adsorption | – | HeLa |
| Tamoxifen | Gold nanospheres, 25 nm | PEG-SH as a linker | PEG-SH | MDA-MB-231, MCF-7, HSC-3 |
| Herceptin | Gold nanorods | Mercaptoundecanoic acid as a linker | – | BT474, SKBR3, MCF-7 |
| β-Lapachon | Gold nanospheres, 25 nm | Physical adsorption | Cyclodextrin as a drug pocket, anti-EGFR, PEG-SH | MCF-7 |
| Doxorubicin | Gold nanospheres, 12 nm | Physical adsorption | Folate-modified PEG | KB |
| Prospidin | Gold nanospheres, 50 nm | Physical adsorption | – | HeLa |
| Docetaxel | Gold nanospheres, 2.5 nm | Bromododecanethiol | – | MCF-7, HCT15 |
| Curcumin | Gold nanospheres, 60 nm, 120 nm | Direct synthesis | Hyaluronic acid, Folate-modified PEG | HeLa, Caco-2 |
| Capecitabine | Gold nanospheres, 4 nm | Physical adsorption | – | Hepatocellular carcinoma biopsy |
| Chloroquine | Gold nanospheres, 7 nm | Mercaptoundecanoic acid as a linker | – | MCF-7 |
| Berberine hydrochloride | Gold nanospheres, 20-60 nm | Physical adsorption | Folic acid | Vero, HeLa |
| Bortezomib | Gold nanospheres, 35 nm | Physical adsorption | PEG-SH | S2-013, hTERT-HPNEs |
| Cetuximab | Gold nanospheres, 25 nm | PEG-SH as a linker | p-SCN-Bz-DOTA | A549 tumor xenograft mouse |
| Epigallocatechin-3-gallate | Gold nanospheres, 70-130 nm | Physical adsorption | – | B16F10 |
| Imatinib | Gold nanospheres, 100 nm | Layer-by-layer assembly with polyvinylpyrrolidone and polyethylene imine | – | B16F10 |
| Epirubicin | Gold nanospheres, 130 nm | Physical adsorption | Folic acid | MCF-7 |
| Metelimumab | Gold nanospheres, 50, 80, 100, 200, 400 nm; Gold nanorods; Gold nanostars; Gold nanocubes | Mercaptopropionic acid as a linker | Methotrexate, folic acid | MDA-MB-231 |
| Indole-3-carbinol | Gold nanospheres, 3 nm | Direct synthesis | – | EAC, DAL |
| Mitoxantrone | Gold nanorods | Thio-amino PEG | Folic acid | HeLa, C6, L929 |
| Bleomycin | Gold nanospheres, 13 nm | Dicarboxylic PEG as a linker | Doxorubicin | HeLa |
Delivery systems were made by using target molecules (e.g., cetuximab) along with the active substances to ensure better anchoring of the complex and its better penetration into the target cells [22]. The use of multimodal delivery systems has also been suggested; in these, GNPs are loaded with several drugs (both hydrophilic and hydrophobic) and with auxiliary substances (target molecules, photodynamic dyes, aptamers, cell-penetrating peptides, etc [50–53].). GNPs conjugated to rituximab and trastuzumab were used for computed tomography imaging of tumor cells [54]. GNPs proved useful as carriers of therapeutic peptides [55,56] and low-molecular-weight inhibitors [57]. Most researchers have pointed out increased effectiveness of GNP-conjugated antitumor preparations [58].
As noted in Wilhelm et al.’s excellent review [59], the delivery efficiency for inorganic nanoparticles is higher than that for organic nanoparticles. Furthermore, the delivery efficiency is dependent on the hydrodynamic diameter of particles. An optimal nanoparticle size for the delivery of drugs to tumors is about 60 nm. For this particular size, 6.4 × 1014 drug surface-loaded nanoparticles (equivalent to 45 mg/m2) are needed to elicit a therapeutic effect in humans.
2.2. Delivery of antibacterial drugs
The therapeutic efficiency of antibiotics is often low, for many reasons. First, oral administration achieves only partial drug adsorption, whereas up to 50% of the drug is excreted in urine. Second, antibiotic therapy often leads to gastrointestinal complications. Finally, the poor solubility of drugs in lipid membranes is also a serious limitation of antibiotic treatment. A promising way to overcome the limitations of the conventional oral administration of drugs is to load antibiotics with nanoparticles. After surface modification of nanoparticles with antibiotics, the antibiotics can be protected from degradation in the stomach. Furthermore, nanoparticle formulations increase the circulation half time and enhances the local drug concentration near microbial cells [60]. For example, Gu et al. [61] prepared a stable vancomycin–colloidal gold complex and showed its effectiveness toward various (including vancomycin-resistant) enteropathogenic strains of Escherichia coli, Enterococcus faecium, and Enterococcus faecalis. Similar results were presented by Rosemary et al. [62]: a complex formed between ciprofloxacin and gold nanoshells was highly active against E. coli. Selvaraj and Alagar [63] reported that the antileukemic drug 5-fluorouracil conjugated to colloidal gold had noticeable antibacterial and antifungal activities against Micrococcus luteus, Staphylococcus aureus, Pseudomonas aeruginosa, E. coli, Aspergillus fumigatus, and A. niger. Noteworthy is that in all those cases, the drug–GNP complexes were stable, which could be judged by their optical spectra.
By contrast, Saha et al. [64] (antibiotics: ampicillin, streptomycin, and kanamycin; bacteria: E. coli, M. luteus, and S. aureus) and Grace and Pandian [65] (aminoglycoside antibiotics: gentamicin, neomycin, and streptomycin; quinolone antibiotics: ciprofloxacin, gatifloxacin, and norfloxacin; bacteria: E. coli, M. luteus, S. aureus, and P. aeruginosa) failed to prepare stable complexes with GNPs. Nonetheless, those authors showed that depending on the antibiotic used, the activity of an antibiotic–colloidal gold mixture, as compared to that of the native drug, increases by 12 to 40%. From these data, they concluded that GNPs increased the antibiotics’ antibacterial action. However, the mechanisms responsible for the increase remained unclarified, which was noted by the authors themselves. In assays on solid and in liquid nutrient media, Burygin et al. [66] proved that free gentamicin and its mixture with GNPs do not significantly differ in antimicrobial activity. They proposed that a necessary condition for the increase in antibacterial activity is the preparation of stable conjugates of nanoparticles coated with antibiotic molecules. Specifically, Rai et al. [67] suggested the direct use of the antibiotic cefaclor in the synthesis of GNPs. Their conjugate was stable and was highly active against E. coli and S. aureus. As a result, they prepared a stable conjugate that had a high antibacterial activity against E. coli and S. aureus. Pradeepa et al.’s [68] conjugates between GNPs and the antibiotics levofloxacin, cefotaxime, ceftriaxone, and ciprofloxacin were effective against multidrug-resistant microorganisms such as E. coli, Klebsiella pneumoniae, and S. aureus.
GNPs have also been conjugated to a variety of antibiotics, including aminoglycosides [69], aminopenicillins [70], ansamycins [71], cephalosporins [72], fluoroquinolones [73], carbapenems [74], polymyxins [75], lincosamides [76], and other groups.
One of the currently most important public health problems is the emergence of pathogenic microbial strains with multiple antibiotic resistance. An active search is in progress for nonantibiotic antibacterial agents. One such agent is the antimicrobial peptides, and their delivery can take advantage of GNPs [77]. Specifically, a GNP-conjugated antimicrobial PEP peptide (CACWQVSRRRRG) inhibited in vitro the growth and development of S. aureus [78]. The antimicrobial peptide VG16KRKP (VARGWKRKCPLFGKGG) coupled to GNPs was highly potent against Salmonella typhi [79].
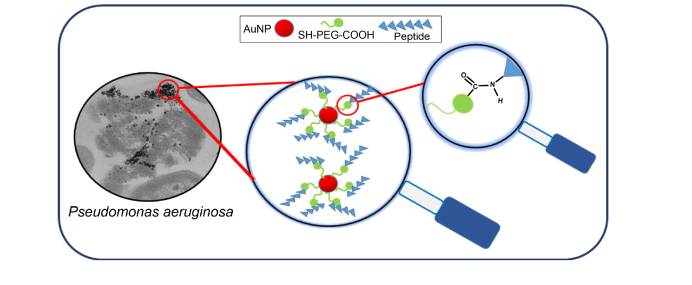
Casciaro [80] reported that covalent conjugation of a derivative of the frog skin antimicrobial peptide esculentin to GNPs via a poly(ethylene glycol) linker increased by about 15 times the activity of the free peptide against the motile and sessile forms of Pseudomonas aeruginosa without causing toxicity to human keratinocytes (Fig. 1).
Fig. 1.
Damage to P. aeruginosa by esculentin conjugated to GNPs via a PEG linker. Reproduced with permission from Ref [80].
GNPs conjugated to the antimicrobial peptide HPA3P (AKKVFKRLPKLFSKIWNWKHHHHHH) were used in vivo to treat mice infected with Brucella abortus [81]. The natural antimicrobial peptides Listeria adhesion protein (isolated from Listeria monocytogenes) and pediocin AcH (isolated from Pediococcus acidilactici) in complex with GNPs were highly active not only against L. monocytogenes cells but also against their biofilms [82]. GNPs coupled to the antimicrobial peptide indolicidin prevented biofilm formation by the pathogenic fungus Candida albicans [83]. Moreover, GNPs offer novel alternatives to combat antibiotic resistance in gram-negative bacteria through the inhibition of quorum sensing [84].
Zhao et al. [85] proposed a new strategy in designing antibacterial agents, using commercially available compounds—aminosubstituted pyrimidines. By themselves, they are completely inactive as antibiotics, but when conjugated to GNPs, they become active against gram-negative multidrug-resistant clinical isolates. Pyrimidine-coated GNPs exert their antibiotic effect through (1) the chemical binding of magnesium or calcium ions, thereby disrupting the bacterial cell membrane, with subsequent leakage of cytoplasmic contents, including nucleic acids, from the damaged cell membranes, and through (2) the interaction with DNA and inhibition of protein synthesis by internalization of GNPs. Unlike conventional antibiotics, GNP-conjugated amino-substituted pyrimidines do not cause resistance in bacteria and are harmless to human cells; therefore, they can be useful in clinical practice. For the same purpose, it was proposed to couple GNPs to amino sugars [86] and bisbiguanides [87].
2.3. Delivery of other substances and of genes
Whereas studies with other drugs conjugated to GNPs are rare, some of them deserve mention because of relevance to nanomedicine. Examples include nanoformulations for the treatment of HIV infection, diabetes, and other diseases. What is more, GNPs can be used in the rapidly growing field of gene therapy, which is based on the expression of required genes or on the suppression of unwanted ones. Nie et al. [88] demonstrated a high antioxidant activity of GNPs complexed with tocoferol and suggested potential applications for the complex. Bowman et al. [89] provided data to show that GNPs conjugated with the preparation TAK-779 were more active against HIV infection than was the unconjugated preparation; this gain in activity was at the cost of the high local TAK-779 concentration. Chiodo et al. [90] described the preparation and antiviral activity of carbohydrate-coated GNPs loaded with anti-HIV prodrugs. Joshi et al. [91] and Cho et al. [92] described the oral and intranasal administration of colloidal-gold-conjugated insulin to diabetic rats, showing significant decreases in blood sugar, which were comparable to those obtained by subcutaneous injection of insulin. Ehsan et al. [93] and Shilo et al. [94] reported the binding of insulin to GNPs and the efficacy of the complex when delivered subcutaneously for the treatment of diabetes mellitus. Finally, Chamberland et al. [95] reported a therapeutic effect of the antirheumatism drug etanercept conjugated to gold nanorods. Similar results are available from Huang et al. [96], who subcutaneously injected rats with galectin-1–nanogold, and from Gomes et al. [97], who conjugated GNPs to methotrexate. GNPs have also been coupled to a variety of other drugs such as octreotide [98], tocilizumab [99], gallic acid [100], lysozyme [101], therapeutic peptides [102], l-DOPA [103], tolbutamide [104], resveratrol [105], and macrophage membrane [106].
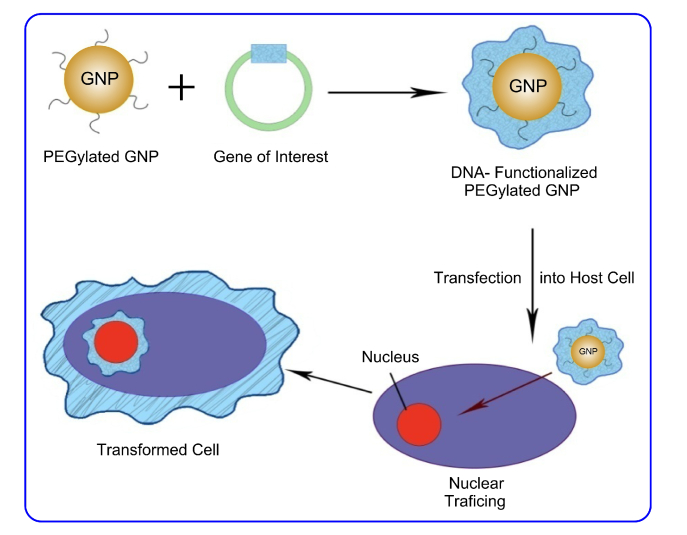
Finally, we should mention gene therapy—possibly an ideal strategy for the treatment of genetic and acquired diseases [107]. The term “gene therapy” describes a medical approach based on the therapeutic administration of gene constructs to cells [108]. The desired effect results either from expression of the introduced gene or from partial or complete suppression of the function of the damaged or overexpressed gene. There have also been recent attempts at correcting the structure and function of an improperly functioning (“bad”) gene. In such a case too, GNPs can be effective in the delivery of genetic material to the cytoplasm and the cell nucleus [109,110] (Fig. 2). In particular, GNPs are attractive vehicles for the target-specific delivery of gene-silencing moieties, alone or in combination with other drugs [111,112].
Fig. 2.
PEGylated GNPs for gene delivery. Adapted with permission from Ref [109].
Small interfering RNA (siRNA) is an effective means to regulate the expression of proteins—even “undruggable” ones, which are nearly impossible to target through traditional small-molecule therapeutics. Delivery to the cell and then to the cytosol is the primary requirement for the realization of the therapeutic potential of siRNA. Effective delivery of siRNA at the organismal and cellular levels, coupled with the low immunogenic response of GNPs, will facilitate the clinical translation of siRNA treatments for various gene-caused diseases, including cancer, macular degeneration, and other genetic diseases [113,114].
Morgan et al. [115] compared the loading, release and internalization efficiencies, and effectiveness of posttranscriptional gene silencing of hollow gold nanoshells, hollow gold nanocages, and gold nanorods with plasmons tuned to absorb NIR light at 800 nm. The hollow gold nanoshells could be loaded with up to three times more siRNA cargo, as compared to nanocages and nanorods, but nanorods were the most efficient in the release of attached siRNA strands when exposed to pulsed 800 nm laser excitation. In cellular treatments, all particles were efficiently internalized by HeLa cells, but the nanoshells and nanocages displayed the highest downregulation of protein expression at 72 h after treatment.
CRISPR/Cas genome editing techniques have many potential applications, including medicine [116]. There are many benefits of CRISPR/Cas9 systems that can be utilized in laboratory engineering in vitro. However, full realization of the potential of CRISPR/Cas9 approaches will require addressing many challenges. Regarding gene cargo delivery systems, this remains the greatest obstacle to the use of CRISPR/Cas9, and an all-purpose delivery method has yet to emerge [117]. Vehicles used to deliver the gene editing system cargo can be classified into three general groups: physical delivery, viral vectors, and nonviral vectors. Nonviral vector systems include systems such as lipid nanoparticles, cell-penetrating peptides, DNA “nanoclews,” and GNPs [118]. A recent study described a novel delivery vehicle called CRISPR–Gold, which is composed of GNPs conjugated to DNA plus cationic endosomal disruptive polymers. CRISPR–Gold can deliver the Cas9 ribonucleoprotein complex and donor DNA into a wide variety of cell types, including immune cells, muscle cell progenitors, human pluripotent stem cells, and human embryonic stem cells [119]. Mout et al. [120] demonstrated that, by engineering Cas9:sgRNA ribonucleoprotein and GNPs to associate with one another, a complex is created that can be efficiently delivered to cells and can cause a desired mutation at an approximate rate of 30%.
GNP-mediated laser optoporation is based on the plasmonic absorption of pulsed [121] or CW [122] laser light by GNPs after their adsorption on the cell surface or after their cellular uptake. The operating amplifier system emits 120 fs laser pulses at a repetition rate of 5 kHz. The maximum output power is 2.1 W at a fixed wavelength of 796 nm and is adjustable by an automated half wave plate and a polarizing beam splitter cube combination. The parameters used for an efficient and gentle cell manipulation were a radiant exposure of 100 mJ/cm2 [121].
The heating of GNPs leads to the nondamaging poration of the membranes and thus enables the diffusion of the target macromolecules into cell [123]. Being very simple in principle, CNP-mediated laser transfection nonetheless has serious drawbacks [124] because of potential cell damage from intense laser pulses and from random attachment of GNPs to the cell surface [125]. Pylaev et al. [126] suggested a new variant of laser transfection that used monolayers of gold nanostars immobilized on the chemically activated bottoms of microplates. Similar strategies using pulsed lasers and 2-D plasmonic nanolithographic structures have been reported in [127]. These modifications have been shown to be more effective than laser transfection with randomly distributed GNPs in cell cultures.
2.4. Use of drugs in GNP synthesis
Usually, drugs are conjugated to ready-made GNPs, which are synthesized chemically [10,128] and then functionalized with target molecules [129]. However, drugs can be used directly in the synthesis of GNPs as reducing agents. Such agents have included a number of hepatoprotecting, anticancer, antisclerotic, and antibiotic drugs.
The flavonoid silymarin, isolated from the fruit and seeds of milk thistle (Silybum marianum L. Gaertn.), is used widely as a hepatoprotector. Silymarin-coated GNPs with an average size of 20 nm were synthesized and functionalized by using silymarin as a reducing and stabilizing agent [130]. The authors observed a therapeutic effect of such GNPs on laboratory animals with liver injury and cirrhosis. The conjugate facilitated the degradation of the extracellular matrix and the inactivation of serous cells, with a strong enhancement of the regenerative ability of the liver. Silymarin-coated nanoparticles could be injected for up to 14 weeks without causing any side effects or any changes in the histological structure of the kidneys, heart, pancreas, or lungs. In addition, GNP-immobilized silymarin had an antitumor effect [131]. Similar results were obtained with GNP–luteolin, a conjugate prepared by the direct reduction of gold chloride with this flavonoid and proposed for use in tumor treatment [132]. GNPs conjugated to the plant flavonoid quercetin were successfully evaluated against leishmanial macrophage infections [133].
A new form of the diagnostic drug 5-aminolevulinic acid was prepared by using the drug for a one-step synthesis of a GNP conjugate [134]. Owing to the peculiarities of its metabolism in tumor cells, 5-aminolevulinic acid causes the accumulation of photoactive porphyrins in the epithelium, the tissues of neoplasms, and atherosclerotic plaques. As a result, this compound is used to visualize pathological tissues. For the same reason, 5-aminolevulinic acid is used in photodynamic therapy as a diagnostic and acting agent. It allows both effective identification of tumor zones (owing to the contrast of the red fluorescence of protoporphyrin IX with shortwave excitation light) and direct use of the photodynamic activity of protoporphyrin IX to destroy surface or cavity tumors. The resulting nanoconjugate was tested on animals and proved to be a highly sensitive means of theranostics, able to help in the early diagnosis and therapy of atherosclerosis.
Another antisclerotic (and antitumor) agent, epigallocatechin-3-gallate, was used to reduce HAuCl4 and prepare a GNP conjugate [135]. The resulting conjugate had low toxicity to healthy tissues and helped to prevent the development of stenosis in laboratory animals with cardiovascular diseases.
In the targeted delivery of anticancer agents, frequent use is made of folic acid to recognize tumor cells. This is due to the folate receptors’ being overexpressed on the surface of cancer cells. Folic acid was used for a one-step synthesis of GNPs [136]. The resultant 18-nm GNPs penetrated HeLa cells much better than did unconjugated particles of the same size. This penetration was largely inhibited by free folic acid in a competitive assay.
The antitumor drug indole-3-carbinol reduced chloroaurates to metal nanoparticles, acting as a reducer and stabilizer [46]. In vitro, the synthesized stable conjugate (particle diameter, 3 nm) showed pronounced cytotoxic, genotoxic and antitumor effects owing to the induction of apoptosis of cancer cells. A combination of two anticancer drugs, bleomycin and doxorubicin, was used to directly synthesize their GNP conjugates [48]. The therapeutic efficacy of the nanohybrid drug was strongly enhanced by active targeting to HeLa cells, with a significant decrease in the half-maximal effective drug concentration through the blocking of the HeLa cancer cell cycle. A GNP–alendronate conjugate prepared by the direct reduction of HAuCl4 was used as a dual chemo-photothermal agent for combined cancer treatment [137].
A terpene, nerolidol, was used for a one-step synthesis of GNPs [138]. The synthesized conjugates were examined for wound-healing activity in albino rats. Treatment with an ointment based on the GNP–nerolidol complex resulted in enhanced diabetic wound healing (within 14 days), as compared to the control group, in which wound healing took longer.
Vemuri et al. [139] reported on the synthesis and testing of various biosynthesized GNPs by using natural phytochemicals (curcumin, turmeric, quercetin, and paclitaxel). Their results demonstrated the anticancer potential of GNP conjugates in a combinatorial approach that could be the future of cancer nanomedicine.
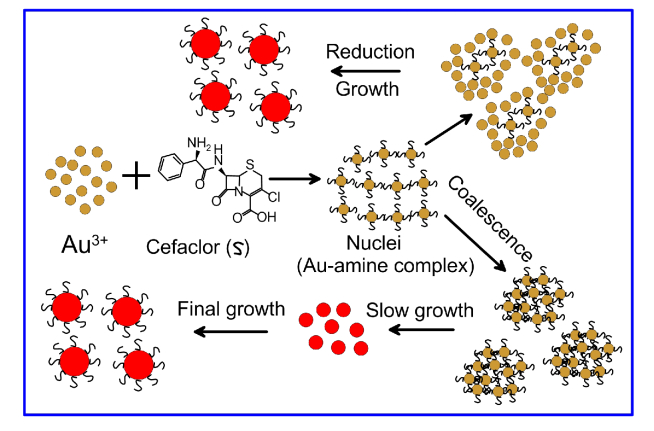
With the sharp increase in the spread of multidrug-resistant bacteria around the world, there is a huge demand for a new generation of antibiotics to combat them. The action of antibiotics can be enhanced by conjugating them to active substance delivery systems, including nanoparticles. To this end, several antibiotics have been used for the direct synthesis of GNP conjugates. Specifically, the cephalosporin cefaclor was used to make 20–50 nm nanoparticles [67]. The diameter of the particles depended mainly on the temperature of the reaction. Reduction was carried out at the expense of the primary amino group of the drug, leaving cefaclor’s β-lactam ring free for antimicrobial action (Fig. 3). Microbiological tests showed that GNP-conjugated cefaclor was more potent against gram-positive (S. aureus) and gram-negative (E. coli) bacteria, as compared to unconjugated cefaclor or to GNPs alone. The conjugate was very stable under adverse conditions (pH 3 and 10) and could be used many times without loss of activity.
Fig. 3.
Two possible mechanisms of the cefaclor-mediated synthesis of GNPs. Adapted from Ref [67].
The antibiotics ampicillin, streptomycin, and kanamycin were used together with sodium borohydride to reduce HAuCl4. The antibacterial activity of the resulting conjugates was higher than that of unconjugated antibiotics [64]. In another study, GNPs were coupled to ampicillin by the direct reduction of HAuCl4 with the antibiotic [140]. Remarkably, the newly prepared GNPs showed excellent activity against Streptococcus pyogenes (minimum inhibitory concentration, 0.14–1.09 μg/mL).
The aminoglycoside kanamycin was used for the one-step preparation of a GNP conjugate [141]. Bacteriological studies have shown a broad-spectrum, dose-dependent activity of the conjugate against both gram-positive and gram-negative bacteria, including those resistant to kanamycin. After 6 h of exposure of bacteria to kanamycin–GNPs, the conjugate was found to attach to and penetrate the cell wall, disrupting intracellular homeostasis. After 12 h of exposure, the cells were lysed owing to the leakage of the cellular components. In addition, as compared to free kanamycin, the minimum inhibitory concentration of kanamycin–20-nm GNPs against all tested bacterial strains decreased significantly.
Yet another antibiotic used in a one-step GNP synthesis was the tricyclic glycopeptide vancomycin [142]. The generated vancomycin–GNP conjugate maintained its antibiotic activity and inhibited the growth of bacterial pathogens (both gram-positive and gram-negative) and antibiotic-resistant strains. Furthermore, the minimum inhibitory concentration of the conjugate against the bacteria was lower than that of free vancomycin. The vancomycin–GNP conjugate was proposed for use in colorimetric and test-strip-based assays of S. aureus and Bacillus subtilis [143].
Amoxicillin, a semisynthetic penicillin, was used too for the one-pot synthesis of GNP conjugates [144,145]. The amoxicillin-coated nanoparticles were highly stable in vivo and were selective for the bacterial cell wall. They also were well excreted by the kidneys and were completely nontoxic to eukaryotic cells at bactericidal concentrations. In vitro, the conjugates were strongly antibacterial against antibiotic-sensitive and -resistant S. aureus strains, especially when combined with photothermolysis. The use of these nanoparticles to treat antibiotic-resistant infections is promising in view of their high stability and cytocompatibility.
The semisynthetic tetracycline doxycycline was able to reduce gold salts to GNPs [146]. The combined therapeutic agent restored the susceptibility of doxycycline and was active against major human pathogens.
The antifungal and antiprotozoal drugs amphotericin B, nystatin, and fluconazole were used in combination with sodium borohydride to restore HAuCl4 [147]. GNP conjugation made all three drugs more bioactive, with the most significant effects being on Acanthamoeba castellanii.
2.5. Future directions
The targeted delivery of drugs and the enhancement of their efficiency at small doses is a topical problem in the future development of personalized medicine, which is based on the individual features of a patient with respect to adverse side effects of a particular chemical drug. Besides oncological problems, nanomedicine can resolve such an important problem as multiple drug resistance. To overcome the current limitations of conventional chemotherapy, further work should aim to improve smart DDSs based on various nanoparticles, including GNPs. Despite the numerous publications, the number of clinically approved drug delivery nanosystems is still quite limited. Therefore, there is a critical need to further translate laboratory studies with animal models into clinical practice.
3. GNPs in cancer immunotherapy
3.1. A short review of recent data
Currently, immunotherapy is considered one of the most effective methods of treating neoplasms. All the developments and discoveries to date, up to the recent Nobel Prize, have increased interest in research in this vast area. The use of nanoparticles in the delivery of immunotherapeutic agents is being studied widely and is considered a promising area of research. Immunotherapeutic nanoparticles are becoming an effective cancer treatment option owing to their high specificity, efficacy, ability to be visualized, and therapeutic effect [148–156]. In addition to the targeted delivery of anticancer drugs, GNPs is a promising nanomaterial for cancer immunotherapy [157–159] for several reasons. Owing to their plasmonic properties, GNPs provide imaging and photothermal options, which can be combined with other therapeutics to monitor the development of immune response. Owing to their well-developed surface chemistry, GNPs are a convenient material for delivering various antigens and adjuvants that help the immune system to kill tumor cells through promoting or inducing cytotoxic T cell lymphocytes. In this way, GNPs are used to construct artificial antigen-presenting cells, which can be additionally functionalized with costimulating molecules and proteins of the MHS complex loaded with antigen peptides. Finally, GNPs themselves can serve as adjuvant nanoparticles interacting with dendritic cells and stimulating the production of cytokines.
One of the most popular variants is the use of GNPs conjugated to CpG oligodeoxynucleotides (CpG-ODNs). Native CpG-ODNs cannot penetrate the cytoplasm through the cell membrane and are easily damaged by the blood or cell cytoplasm nucleases. For their intracellular delivery, use has been made of ODN–GNP conjugates, which have demonstrated high efficacy in vitro [160–162]. When GNPs were complexed with CpG-ODNs, the best efficacy was shown by gold nanospheres with a diameter of 15–50 nm, as compared with nanorods, nanoshells, and nanostars [163].
Along with CpG-ODNs, cancer immunotherapy has been making use of GNPs coupled to TNF-α, αPDL1, TLR7 agonist, TGF-β inhibitor, specific antibodies and other tumor cell death factors and/or immunostimulants [19,164–168]. GNPs showed a significant tendency to interact with dendritic cells [169], with the subsequent secretion of immunostimulating cytokines (IL-1, IL-6, IL-12, and TNF-α) [7,170] and downregulation of immunosuppressive chemokines (TGF-β1 and IL-10) [171].
Nanovaccines are being designed that are based on GNPs, on the surface of which are presented tumor peptide antigens with a very high density. Each GNP can carry up to 1300 peptides. The proposed vaccine effectively delivers peptide antigens to dendritic cells, where they interact with major histocompatibility complex I (MHC I) and jumpstart antitumor immune response [172,173]. Lin et al. [172] reported that GNPs in complex with peptides derived from tumor-associated antigens are taken up effectively by dendritic cells. Moreover, dendritic cells take up GNPs with minimal toxicity and can process the vaccine peptides on the particles to stimulate cytotoxic T lymphocytes. A high peptide density on the GNP surface can stimulate cytotoxic T lymphocytes better than can free peptides. Thus, GNPs have great potential as carriers for various vaccine types. Nanovaccine designers have used various tumor antigens of a protein and a carbohydrate nature [174–180].
GNPs also have adjuvant effects [181]. Gold-based nanoparticles showed a 15-fold greater increase in the amount of secreted TNF-α, which suggests that nanoparticles alone, without an adjuvant, can be more effective at inducing host immune responses than free tumor-associated antigen [182].
A smart approach is to deliver antigens to the local lymph nodes, because the lymph node contains a high population of dendritic cells, macrophages, and immune cells responsible for producing humoral and cellular immunity [183,184]. Therefore, nanoparticles have been utilized for the delivery of antigens to the lymph node through lymphatic vessels in a size-dependent manner [185]. GNPs have been successfully utilized for cancer immunotherapy in various preclinical studies [186].
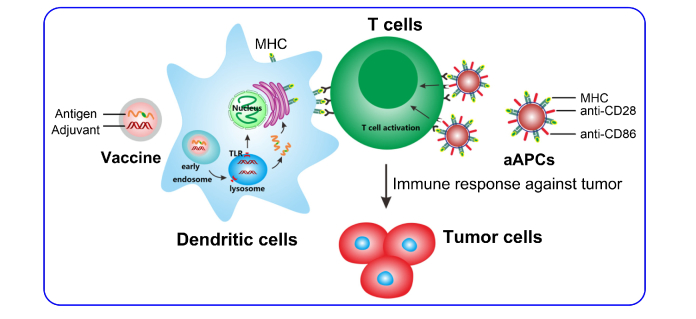
The use of activated dendritic cells has become a modern trend in cancer vaccinology [187], with variously sized, shaped, and structured GNPs being carriers for such therapeutic vaccines [188–190] (Fig. 4). In particular, studies with human dendritic cells showed the effect of GNPs on cellular uptake and internalization, maturation of dendritic cells, and the subsequent differentiation of T cells and their cytotoxicity [191]. GNPs coated with tumor antigens facilitated the maturation of dendritic cells and dendritic-cell-mediated lymphocyte proliferation [192]. Ultimately, successful vaccines based on dendritic cells and GNPs can cause phagocytosis, activation/maturation, migration, T-cell costimulation, and cytokine secretion, which is called GNP-induced dendritic cell tuning [193] or adjuvant action on dendritic cells [194].
Fig. 4.
Nanoparticle-based delivery system to activate dendritic cells or T cells for immunotherapy. Adapted with permission from Ref [190].
Cruz et al. [195] addressed dendritic cell uptake of and immune response activation by 13-nm GNPs conjugated to prostate cancer peptide antigens. GNPs functionalized with the peptides and with Fc fragments of IgG were shown to interact with the Fcg receptors of dendritic cells and were localized, upon uptake, in the cytoplasm in a diffuse way. Internalization of antigen-conjugated GNPs in the dendritic cells increased the immune response, whereas the use of the native antigen only enhanced lymphocyte proliferation. Such an approach, in the authors’ opinion, opens up the way to the design of an effective system for making antitumor and other vaccines.
Dreaden et al. [196] suggested the use of GNPs conjugated with macrolide antibiotics (azithromycin, clarithromycin, and tricyclic ketolide), which can accumulate in tumor-specific macrophages and induce their cytotoxicity, causing tumor cells to die. Thus, particle size and structure in these studies were not critical to macrophage uptake. Wang et al. [197] reported that BSA-coated gold nanorods showed high photothermal conversion efficiency and a good photothermal ablation effect toward tumor cells. The ablated tumor cells were cocultured with immature dendritic cells through a direct cell contacting model and a diffusion model to confirm the stimulatory effects of the cell–cell interaction and soluble factors released from ablated tumor cells. The photothermally ablated tumor cells induced immune-stimulatory responses in dendritic cells through both cell–cell interaction and soluble factors. With some inspiration from the data on GNP uptake by macrophages, Choi et al. [198] even put forward a new method for the photothermal therapy of tumors that employs a “Trojan horse” in the form of monocytes and macrophages laden with phagocytosed GNSs.
3.2. Future directions
Cancer immunotherapy has shown such unique benefits as the induction of specific antitumor immunity and long-term response of immunological memory. There are studies devoted to the effects of nanomaterials on the modulation of macrophages, T-lymphocytes, neutrophils, and dendrite cells. Additional studies are needed to selectively design nanomaterials that can recognize target immune cells and to design experiments aimed at evaluating nanomaterial efficiency with respect to immunotherapy. As innate immunity is a key factor in tumor growth, the great potential of immunotherapy can be related to the future development of nanomaterials for the specific modulation of innate immunity cells.
4. Combined chemo-, immuno-, and phototherapy
4.1. Multimodal nanotherapeutics
A modern trend in the use of nanoparticles in biomedical research is the combination of chemo-, immuno-, and phototherapy [199–201]. These methods combine the optical properties of GNPs, used for photothermolysis, with the properties of GNPs as a means of delivery of drugs, photodynamic dyes, immunomodulators, and other substances [202,203]. Compared to other nanoparticles, GNPs have several advantages for multimodal nanotherapeutics. First, they have remarkable plasmonic properties with finely controlled absorption and scattering of light within extraordinary broad spectral bands, including the first and second NIR transparency windows. Second, owing to the convenient functionalization technologies, GNPs provide a versatile and flexible platform for the fabrication of multimodal nanoparticles with desired theranostic abilities. Below we discuss recent examples of such a strategy.
You et al. [204] combined plasmonic photothermal therapy (PPTT) with chemotherapy by using a single multifunctional nanoconstruct that mediates simultaneous photothermal cell killing and drug release (photothermal chemotherapy). Such a hybrid nanostructure showed enhanced antitumor activity and reduced toxicity, as compared to chemotherapy alone. Doxorubicin was loaded to hollow gold nanospheres coated with PEG. Similar results were presented by Mendes et al. [205]—a synergistic interaction between heat and cytotoxic action of doxorubicin, with clear advantages over individual therapies. The resulting conjugate plus a NIR laser demonstrated greater antitumor activity than did free doxorubicin, GNPs, or liposomal doxorubicin. Strikingly, a single round of PPTT combined with a subtherapeutic dose of doxorubicin can elicit robust antitumor immune responses and can eliminate distant (untreated) as well as local tumors in >85% of animals with advanced metastatic cancer [206]. Bisker et al. [207] utilized gold nanospheres conjugated to rituximab, an anti-CD20 monoclonal antibody-based drug, for carrying and releasing the drug upon irradiation of specifically tailored femtosecond laser pulses.
Using a murine carcinoma model, Shao et al. [208] demonstrated higher therapeutic efficacy of GNP–TNF conjugates, as compared to that of laser treatment and GNP–TNF used singly and to that of laser treatment with TNF-free GNPs. Nam et al. [209] reported a new combination cancer therapy platform that consisted of relatively small (10 nm) pH-responsive spherical GNPs and conjugated doxorubicins. The conjugates accumulated in cancer cells through rapid phagocytic action and effective blockage of exocytosis by the increased aggregate size. They also effectively accumulated in tumors (up to 17 times, as compared with the control) because of the enhanced permeation and retention. The conjugates had a synergistic effect that was enhanced by nearly an order of magnitude at the cellular level. The synergistic effect was demonstrated as remarkable reductions in both the therapeutically effective drug dosage and the photothermal laser threshold. Effective suppression of tumor growth was also shown with an animal model.
Tao et al. [210] designed an immunomodulatory CpG-ODN–based platform conjugated with NIR-responsive gold nanorods and doxorubicin for cancer therapy. This engineered vehicle had significant antitumor efficacy both in vitro and in vivo. The authors developed a multifunctional platform by using a self-assembly strategy to incorporate materials with specific functions of chemotherapeutics, hyperthermia, and especially immunotherapy, which can collectively contribute to effective cancer treatment.
Plasmonic hollow gold nanoshells coated with PEGylated thermosensitive lipids were prepared as an efficient platform to ratiometrically co-deliver two drugs, bortezomib and gemcitabine, for combinational chemotherapy and PPTT of pancreatic cancer [211]. The nanoshells showed remotely controllable drug release when exposed to an NIR laser for site-specific delivery. The conjugates showed synergistic cytotoxicity and were better internalized by cancer cells.
Kim et al. [212] demonstrated the feasibility of biomedical application of GNPs coated with doxorubicin-loaded fucoidan in dual chemotherapy and PPTT of rabbit eye tumors in vitro and in vivo. The conjugates were highly toxic to the tumor cells and showed strong light absorption for a temperature increase in vitro. Upon administration, PPTT-assisted doxorubicin/fucoidan-loaded GNPs entailed the complete removal of the tumors without recurrence for 14 days after the treatment.
Functional chlorin gold nanorods were fabricated to treat breast cancer by phototherapy. The nanostructure was developed by synthesizing gold nanorods as the photothermal conversion material and by coating the PEGylated mesoporous SiO2 as the shell for entrapping the photosensitizer Ce6 and for linking the D-type cell-penetrating peptide [213]. When used in combinational PPTT and photodynamic therapy (PDT) therapy, the conjugates demonstrated strong cytotoxicity and apoptosis-inducing effects in breast cancer cells in vitro and robust treatment efficacy in breast cancer-bearing nude mice. The review by Tran et al. [214] provides an insight into current research on nanocarriers utilizing the synergistic effects of PPTT and PDT for anticancer therapy.
Cao et al. [215] designed a hyaluronic acid and ovalbumin-decorated GNP-based vaccine for photothermally controlled cytosolic antigen delivery by using NIR irradiation. Another goal was to induce antigen-specific CD8 + T-cell responses. Chemical binding of thiolated hyaluronic acid and ovalbumin to GNPs facilitated antigen uptake of dendritic cells via receptor-mediated endocytosis. GNPs exhibited enhanced NIR absorption and thermal energy translation. Cytosolic antigen delivery was then permitted through the photothermally controlled process of local heat-mediated endo/lysosome disruption by laser irradiation along with reactive oxygen species generation, which helps to augment proteasome activity and downstream MHC I antigen presentation. Consequently, the nanovaccine can effectively evoke a potent anticancer immune response in mice under laser irradiation.
In Zhou et al. [216], CTAB–coated gold nanorods were successively decorated with PEG and BSA and were loaded with the immunoadjuvant imiquimod (R837). Under NIR irradiation, the nanocomplexes effectively killed tumors and triggered strong immune responses in the treatment of metastatic melanoma in mice.
Chen et al. [217] described a cell-mediated strategy by transporting a photothermal reagent (gold nanorods) and a CpG adjuvant within macrophage vehicles. The nanocomposites exhibited immense macrophage uptake and a negligible cytotoxic effect in RAW264.7 cells. Nanocomposite-laden macrophages demonstrated an admirable photothermal response in vitro. Gold nanorods/CpG-laden macrophages significantly promoted tumor accumulation in vivo and dramatically enhanced the efficiency of photothermal cancer therapy.
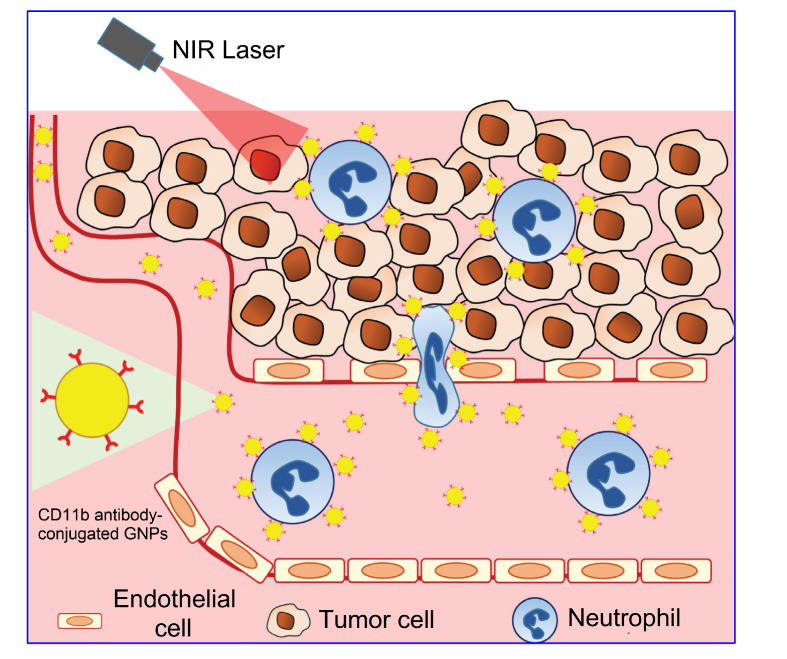
In Chu et al. [218], CD11b antibody-decorated GNPs were used to enhance the infiltration of neutrophils into tumor tissues (Fig. 5). The CD11b antibody was used as a biomarker for activated neutrophils. For enhancing the infiltration of neutrophils to tumor tissues, mice were preinjected with pyropheophorbide and illuminated at 660 nm. The researchers hypothesized that photosensitization-induced inflammation in tumor tissues might guide the gold nanoparticle-bound neutrophils to infiltrate the tumors. Indeed, the group of mice treated with antibody-decorated gold nanoparticles showed decreased tumor growth and prolonged survival, as compared to the group treated with PEGylated GNPs.
Fig. 5.
Neutrophil-mediated delivery of gold nanocarriers. Adapted with permission from Ref [159].
PTT efficacy can be increased by coupling GNPs to antibodies [219,220], photodynamic dyes [221], peptides [222], and siRNA [223].
The use of combined chemo- and phototherapy is not restricted to oncology. It also includes treatment of bacterial infections [144], in particular those caused by strains with multiple antibiotic resistance and by biofilms. Meeker et al. [224] demonstrated that polydopamine-coated gold nanocages can be used as a central core element around which different antibodies and antibiotics (daptomycin, ceftaroline, vancomycin, and gentamicin) can be incorporated to achieve the laser-assisted synergistic PPTT and antibiotic-mediated killing of both gram-positive and gram-negative pathogens—even in the intrinsically resistant environment of an established biofilm. In Chen et al. [225], a conjugate was easily fabricated by coupling a dual-functional adhesion peptide (P937) to gold nanorods. The peptide P937, designed by the phage display biopanning technology, had a specific binding affinity for bacteria. The conjugate exhibited an enhanced NIR-based photothermal conversion efficiency. Both E. coli and S. aureus were killed by the conjugate within 10 min under laser irradiation. Zhao et al. [226] designed a novel formulation containing 50–100-nm long gold nanorods decorated with two types of glycomimetic polymers to specifically block the bacterial LecA and LecB lectins, which are essential for bacterial biofilm development. This novel formulation most efficiently inhibits and kills P. aeruginosa through lectin blocking and the NIR-light-induced photothermal effect of gold nanorods, respectively.
4.2. Multifunctional gold-based composites in combined therapy
Combined therapy also uses multifunctional gold-based composites [227] that can be synthesized via three main routes [6]. First, a gold nanoparticle is covered with a nonmetallic shell, which is doped with diagnostic and therapeutic molecular agents. The shells of such nanocomposites can include magnetic particles, thus enabling a combination of plasmonic and magnetic properties. In the second route, the GNP surface is functionalized with a set of various molecules that ensure the targeting, diagnostic, and therapeutic modalities. Finally, the third route combines the above two approaches to make hybrid multifunctionalized nanocomposites.
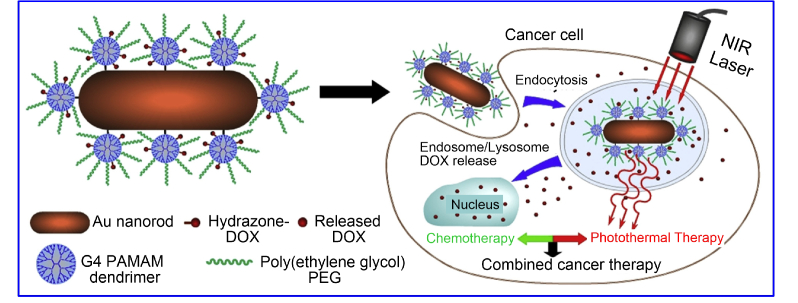
By conjugating doxorubicin to the dendrimer layer of gold nanorods, Li et al. [228] demonstrated synergistic photothermal and chemotherapy treatment of HeLa cells and colon carcinoma tumors in mice (Fig. 6). Polymeric biocompatible doxorubicin–GNP micelles were utilized for photothermal therapy in combination with chemotherapy in vivo [229,230]. Targeted drug delivery in conjunction with photothermal therapy was made possible with doxorubicin-encapsulated poly(lactide-co-glycolide) nanoparticles coated with a gold half-shell [231]. Chitosan-coated gold nanorods doped with cisplatin enhanced the drug’s antitumor effect when photothermal therapy was included as an additional option [232]. Huang and Liu [233] developed a new polymer self-assembly strategy for preparing octahedral, triangular, and multicore gold@poly(styrene-alt-maleic acid) nanoparticles. The gold–polymer particles with Pt drugs tethered to the polymer structure on the surface were used in combined chemo- and photothermal cancer therapy together with NIR-excited emission. Similar mesoporous silica-coated gold nanocomposites were made with gold nanorods as a plasmonic heater and doxorubicin as an antitumor drug for in vitro and in vivo dual photothermal and chemotherapy [234,235]. Interesting data emerged from Huang et al. [236], who embedded a magnetic core within a gold shell surrounded by the antibiotic vancomycin. The resultant composite structure was used for the magnetic separation of vancomycin-bound pathogenic bacteria, which was followed by their photothermal treatment.
Fig. 6.
Schematic illustration of GNRs conjugated to a pH-sensitive PEGylated PAMAM dendrimer for combined PPNT therapy and doxorubicin chemotherapy. Adapted with permission from Ref [228].
More complex nanocomposites have also been synthesized. Ma et al.’s [237] composite consisted of a magnetic core with a gold nanorod-doped silica shell and was found useful in combined photothermal therapy and chemotherapy of tumors, as coupled with magnetic resonance tomography and NIR-thermal imaging. In another example [238], a magnetic core was coated sequentially with layers of silica and gold and was stabilized with PEG-SH and functionalized with Erbitux therapeutic antibodies. The nanostructure was used in targeted cancer detection through both magnetic resonance imaging and localized synchronous therapy with Erbitux antibodies. In Cheng et al. [239], a polymeric capsule containing gold nanorods, quantum dots, and magnetic nanoparticles was coated with the anticancer agent paclitaxel. This combination made it possible to conduct chemotherapy and simultaneous photothermal therapy under the control of fluorescence microscopy and magnetic resonance tomography. Baek et al. [240] described gold nanorods that were coated successively with a mesoporous silica shell, doxorubicin, and a thermoresponsive polymer. By combining different modes of treatment (e.g., chemotherapy and hyperthermia) and the temperature and pH responsivity of the nanoparticles, it was possible (1) to enhance drug uptake, (2) to trigger drug release locally by using internal and external stimuli, and (3) to synergistically combine drug and temperature effects to induce cell death in a desired location. Furthermore, the attenuation of the X-ray signal achieved with the nanohybrids suggested their suitability for use as a contrast agent in computed tomography. Chen et al. [241] presented the synthesis and application of new graphene-based magnetic and plasmonic nanocomposites for magnetic-field-assisted drug delivery and chemo/photothermal synergistic therapy. The nanocomposites were prepared via conjugation of doxorubicin-loaded PEGylated Fe2O3/Au core/shell nanoparticles with reduced graphene oxide. Good efficacy was also achieved by concurrent attachment of paclitaxel and biotin to GNPs [242] and of doxorubicin and biotin to gold nanorods [243].
A gold nanostar-based multifunctional conjugate was developed for NIR imaging and combined photothermal, photodynamic, and chemical therapy of tumors [244]. The gold nanostars were functionalized with three ligands: a targeting peptide, doxorubicin, and indocyanine green. A combined chemo-photothermal therapy assay revealed that doxorubicin-loaded PEGylated mesoporous SiO2-coated gold nanostars have a higher therapeutic efficiency than individual therapies, demonstrating suitable synergistic effects [245]. Wang et al. [246] and Zhang et al. [247] developed mesoporous titania-based yolk–shell nanoparticles as a multifunctional therapeutic platform for SERS imaging and chemo- and photothermal treatment. Jiang et al. [248] proposed gold nanorods@mesoporous SiO2/rhodamine B isothiocyanate/doxorubicin composite nanoparticles for fluorescence-imaging-photocontrolled drug release and for photothermal therapy of cancer cells. Hu et al. [249] conducted SERS imaging, targeted drug delivery, and photothermal therapy with nanorattles made of nanocomposites loaded with the Raman reporter p-aminothiophenol and coated with hollow silica shells that were functionalized simultaneously with a cell-penetrating peptide and doxorubicin. Topete et al. [250] coated the surface of biodegradable poly(lactide-co-glycolide) nanoparticles containing encapsulated doxorubicin with a gold shell and functionalized it with indocyanine green- and folate-conjugated human serum albumin. This viruslike nanoplatform enabled fluorescence imaging in vivo, as well as simultaneous targeted chemotherapy and photothermal therapy. In vivo, it produced a high synergistic effect in experiments with mice implanted with breast cancer cells. Hao et al. [251] fabricated gold-nanoshelled docetaxel-loaded poly(lactide-co-glycolide) nanoparticles. A tumor-targeting peptide, angiopep-2, was introduced onto the nanoshell through the Au–S bond, and this permitted the authors to achieve drug delivery with an active targeting capability. This novel system afforded combined chemotherapy and thermal therapy of cancer, and it also showed a potential X-ray imaging ability. Yuan et al. [252] developed a combination of monoclonal antibodies, folic acid, and miR-122 (an RNA genetic drug)–loaded GNPs on graphene nanocomposites for drug delivery and for the photothermal therapy and imaging of tumor cells.
Marrache et al. [253] encapsulated zinc phthalocyanine (a long-wavelength absorbing photosensitizer) within a polymeric nanoparticle core made up of poly(D,L-lactic-co-glycolic acid)-b-poly(ethylene glycol). After coating the outside of the polymeric core with GNPs, the authors further modified the GNP surface with CpG-ODN. In vitro studies using 4T1 metastatic mouse breast carcinoma cells showed significant photocytotoxicity of the hybrid nanoparticles containing both zinc phthalocyanine and CpG-ODN after irradiation with a 660-nm laser light. This activity was remarkably better than either treatment alone.
An intriguing structure was proposed by Hembury et al. [254]. GNPs of ~7 nm diameter were placed inside hollow silica shells hosting GNCls (gold quantum dots) within their mesopores. The nanoclusters had a diameter of <2 nm and expressed magnetic and fluorescent properties. The gold–silica quantum rattles so produced had a total size of ~150 nm and were used for delivery, into tumor cells, of doxorubicin conjugated to their surface; photothermal therapy; and fluorescence, photoacoustic, and magnetic resonance imaging. Yi et al. [255] reported on a smart drug release nanosystem able to conduct photodynamic therapy, photothermal therapy and chemotherapy in a photocontrollable manner. Doxorubicin and 5, 10, 15, 20-tetrakis (1-methylpyridinium-4-yl) porphyrin (a photosensitizer) were physically intercalated into a DNA assembly immobilized on gold nanorods. The drugs were efficiently delivered to target cells and released under light irradiation, resulting in a synergism that combined phototherapy and chemotherapy for cancer treatment. Ramasamy et al. [256] described the construction of a programmed mesoporous silica-capped gold nanorod covered with nanoselenium overcoat (Se@Au@mSiO2@doxorubicin) nanoparticles as a multifunctional nanoplatform to incorporate materials with specific chemotherapeutic, chemoprevention, and photoablation/hyperthermia functions that collectively enhance anticancer efficacy in multidrug-resistant breast cancer.
In Xu et al. [257], the frequently overlooked, “weak” PPTT and PDT (no killing capability) were used to synergize chemotherapy against multidrug resistance without impairing normal tissues. An NIR-responsive nanosystem, gold-nanodot-decorated hollow carbon nanospheres coated with hyaluronic acid, was synthesized as a doxorubicin carrier with excellent photothermal and photodynamic properties.
Doxorubicin and GNPs loaded into thermosensitive liposomes served as a basis for nanoplatforms permitting cancer cells to be killed both through thermal treatment and through the effect of the encapsulated doxorubicin, which is released directly into tumor cells by NIR laser illumination [258].
4.3. Future directions
The surgical resection of tumors is a major therapeutic strategy, but it often leads to tumor recurrence. A possible improvement on this conventional approach is to combine it with nanomedical approaches such as nanoparticle-based chemotherapy and photodynamic and photothermal therapy, which can release tumor antigens inducing systemic anticancer immune responses. Thus, in combination with immunotherapy, nanoparticle-based therapy can prevent tumor recurrence and eliminate metastases. Several preclinical studies have already demonstrated successful application of nanomedicine in the combined immunotherapy of cancer, thus making clinical translation feasible.
An important note is in order here. In 2013, Setyawaty et al. [259] reported on a novel non-receptor-mediated mechanism by which titanium dioxide nanoparticles trigger intracellular signaling cascades via specific interaction with VE-cadherin, resulting in nanomaterial-induced endothelial cell leakiness (NanoEL). This finding was considered in a positive context in cancer nanomedicine, as the endothelium presents a formidable barrier to intravenously administered nanodrugs, which must leave the blood vessel at the tumor site. In particular, 10–30-nm GNPs are good candidates to induce NanoEL and, therefore, could be used in future to access immature tumors, which cannot accumulate nanodrugs owing to the enhanced permeability and retention (EPR) effect [260]. In addition to the nanoparticle size, the density of a nanoparticle material can also play a crucial role in NanoEL [261]. In contrast to the cited positive expectations, Peng et al. [262] recently demonstrated a possible negative role of NanoEL by using titanium dioxide, silica, and gold nanoparticles. The main finding is that NanoEL can induce intravasation of surviving cancer cells into the surrounding vasculature, thus accelerating cancer metastasis. Therefore, future work is needed to evaluate in detail the benefits and drawbacks of NanoEL.
5. Concluding remarks
Current progress in the chemical synthesis of GNPs has resulted in a great diversity of particles with controlled sizes, shapes, and internal structures. These are either available on the market or are laboratory made. The next step would be the rational design of theoretically predicted nanostructures with the required optical and physicochemical properties. An interesting approach is to use the functional components (drugs, peptides, etc.) as reducing agents to avoid the functionalization step.
In addition to the far-field plasmonic properties, the key feature of GNPs is the plasmonic enhancement of the local electromagnetic field. This phenomenon leads to an enormous enhancement of various weak physical effects such as SERS, CARS, and metal-enhanced fluorescence, which cannot be observed under ordinary excitation conditions. In particular, the detection sensitivity of the traditional lateral flow immunoassay can be greatly enhanced with SERS technologies [263]. Recent publications [264] have clearly demonstrated potential possibilities for sensitive detection and imaging on the single-particle level. There is no doubt that the current methods of chemical and biological sensing will benefit from the new plasmonic nanostructures with optimized local-field and far-field electromagnetic properties in combination with multifunctional theranostic capabilities.
A promising direction in the application of multifunctionalized GNPs in biomedicine is the targeted delivery of antitumor drugs and antibiotics for combined photothermal and chemical therapy. However, several important problems should be solved before PPTT can actually be used in oncological practice. First, the specificity of conjugate accumulation in tumors must be improved and the accumulation of conjugates in the reticuloendothelial system must be minimized. The efficient targeting of conjugates to tumors is also a critical step. As a result of a careful examination of active and passive tumor targeting, Huang et al. [265] showed that the active targeting of gold nanorods functionalized with several specific peptides does not improve the accumulation contrast, as compared to the passive EPR effect. This result clearly demonstrates that there is a pressing need to continue research on the targeted delivery of conjugates to tumors. According to published data, the geometrical (size, shape) and surface (coating, charge) properties can affect the efficacy of cellular uptake and, as a result, the delivery of desired compounds into cells and into tumors. In a pioneering study, Warren Chan’s team at Toronto University [266] described strongly size-dependent delivery of GNP–herceptin conjugates into cancer cells. Additional studies are required to elucidate the dependence of endocytosis solely on particle shape, with all other factors being equal [267].
Because of the strong scattering of light in tissues, the delivery of light to internal organs must be improved with fiber-optic methods. An interesting alternative could be nonplasmonic heating with combined gold–magnetite nanoparticles and an external magnetic field. Finally, for any type of therapy, one needs to control the dynamics of therapy success. For example, the real-time monitoring of circulating tumor cells and their phenotypic evolution after therapy can be used for treatment management. An instructive study has been published recently by Tsao et al. [268]. The authors reported successful application of SERS-based technology for the sensitive detection of drug-resistant clones of circulating cells for 10 patients with stage IV of melanoma.
An important issue is the development of controlled release of the payloads upon a change in physical–chemical conditions in the local area of the biotarget. In the case of passive stimuli such as action of specific enzymes or pH and redox potential changes, the payload delivery is triggered by the specific target environment. Laser light, ultrasound, magnetic field and other physical means can be used for the active delivery of therapeutic cargo to biotargets.
The cancer immunotherapy concept is based on the use of the host patient immune system for tumor treatment. The breakdown novelty and promising expectations of this approach have been confirmed by the 2018 Nobel Prize to J. P. Allison and T. Honjo for the discovery of “cancer therapy by inhibition of negative immune regulation.” Recent reports on successful clinical applications of cancer immunotherapy [269] have indicated the great potential of this strategy, especially when used in combination with conventional chemical and physical treatments, optimization of the treatment schedule, and reliable monitoring of immune response. At present, cancer immunotherapy is still in its infancy and further work is needed to move from the first successful clinical cases to approved technology. In particular, the interaction of the immune system cells with bare or functionalized GNPs is still poorly understood in detail and requires further study. Nevertheless, the accumulated experimental data show that the antigenic, adjuvant, and inflammation-causing properties can be considered important components of interactions between GNPs and immune system. From this point of view, the rational design of multifunctional nanoparticles, including those based on GNPs, can be critical to the future development of combinatorial cancer therapy, which utilizes the best advantages of photo-, chemo-, and immunotherapy.
To summarize, GNPs can be used in various fields of current nanomedicine, including drug delivery, immunotherapy, and phototherapy. This combined therapy seems the most promising approach, which has a synergistic effect on tumor growth and overall survival in preclinical tests. The important problems are the determination of optimal doses and the therapy design in clinical tests for early stages. Further work is needed to develop biocompatible and safe nanoparticles that are able to deliver a wide range of therapeutic agents with improved pharmacokinetics.
Acknowledgments
We thank Mr. D.N. Tychinin for his help in preparation of the manuscript.
Funding
Russian Science Foundation [18-14-00016 (N.K.) and 19-14-00077 (L.D.)].
Disclosures
The authors declare that there are no conflicts of interest related to this article.
References
- 1.Boisselier E., Astruc D., “Gold nanoparticles in nanomedicine: preparations, imaging, diagnostics, therapies and toxicity,” Chem. Soc. Rev. 38(6), 1759–1782 (2009). 10.1039/b806051g [DOI] [PubMed] [Google Scholar]
- 2.Dykman L., Khlebtsov N., “Gold nanoparticles in biomedical applications: recent advances and perspectives,” Chem. Soc. Rev. 41(6), 2256–2282 (2012). 10.1039/C1CS15166E [DOI] [PubMed] [Google Scholar]
- 3.Dreaden E. C., Alkilany A. M., Huang X., Murphy C. J., El-Sayed M. A., “The golden age: gold nanoparticles for biomedicine,” Chem. Soc. Rev. 41(7), 2740–2779 (2012). 10.1039/C1CS15237H [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao-Milán R., Liz-Marzán L. M., “Gold nanoparticle conjugates: recent advances toward clinical applications,” Expert Opin. Drug Deliv. 11(5), 741–752 (2014). 10.1517/17425247.2014.891582 [DOI] [PubMed] [Google Scholar]
- 5.Yang X., Yang M., Pang B., Vara M., Xia Y., “Gold nanomaterials at work in biomedicine,” Chem. Rev. 115(19), 10410–10488 (2015). 10.1021/acs.chemrev.5b00193 [DOI] [PubMed] [Google Scholar]
- 6.Dykman L. A., Khlebtsov N. G., “Multifunctional gold-based nanocomposites for theranostics,” Biomaterials 108, 13–34 (2016). 10.1016/j.biomaterials.2016.08.040 [DOI] [PubMed] [Google Scholar]
- 7.Dykman L. A., Khlebtsov N. G., “Immunological properties of gold nanoparticles,” Chem. Sci. (Camb.) 8(3), 1719–1735 (2017). 10.1039/C6SC03631G [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dykman L. A., Khlebtsov N. G., Gold Nanoparticles in Biomedical Applications (CRC Press, 2017). [DOI] [PubMed] [Google Scholar]
- 9.Sztandera K., Gorzkiewicz M., Klajnert-Maculewicz B., “Gold nanoparticles in cancer treatment,” Mol. Pharm. 16(1), 1–23 (2019). 10.1021/acs.molpharmaceut.8b00810 [DOI] [PubMed] [Google Scholar]
- 10.Dykman L. A., Khlebtsov N. G., “Methods for chemical synthesis of colloidal gold,” Russ. Chem. Rev. 88(3), 229–247 (2019). 10.1070/RCR4843 [DOI] [Google Scholar]
- 11.Yao C., Zhang L., Wang J., He Y., Xin J., Wang S., Xu H., Zhang Z., “Gold nanoparticle mediated phototherapy for cancer,” J. Nanomater. 2016, 1 (2016). 10.1155/2016/5497136 [DOI] [Google Scholar]
- 12.Norouzi H., Khoshgard K., Akbarzadeh F., “In vitro outlook of gold nanoparticles in photo-thermal therapy: a literature review,” Lasers Med. Sci. 33(4), 917–926 (2018). 10.1007/s10103-018-2467-z [DOI] [PubMed] [Google Scholar]
- 13.Vines J. B., Yoon J.-H., Ryu N.-E., Lim D.-J., Park H., “Gold nanoparticles for photothermal cancer therapy,” Front Chem. 7, 167 (2019). 10.3389/fchem.2019.00167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vigderman L., Zubarev E. R., “Therapeutic platforms based on gold nanoparticles and their covalent conjugates with drug molecules,” Adv. Drug Deliv. Rev. 65(5), 663–676 (2013). 10.1016/j.addr.2012.05.004 [DOI] [PubMed] [Google Scholar]
- 15.Connor D. M., Broome A. M., “Gold nanoparticles for the delivery of cancer therapeutics,” Adv. Cancer Res. 139, 163–184 (2018). 10.1016/bs.acr.2018.05.001 [DOI] [PubMed] [Google Scholar]
- 16.Llevot A., Astruc D., “Applications of vectorized gold nanoparticles to the diagnosis and therapy of cancer,” Chem. Soc. Rev. 41(1), 242–257 (2012). 10.1039/C1CS15080D [DOI] [PubMed] [Google Scholar]
- 17.Zhao Y., Jiang X., “Multiple strategies to activate gold nanoparticles as antibiotics,” Nanoscale 5(18), 8340–8350 (2013). 10.1039/c3nr01990j [DOI] [PubMed] [Google Scholar]
- 18.Elbayoumi T. A., “Nano drug-delivery systems in cancer therapy: gains, pitfalls and considerations in DMPK and PD,” Ther. Deliv. 1(2), 215–219 (2010). 10.4155/tde.10.31 [DOI] [PubMed] [Google Scholar]
- 19.Paciotti G. F., Myer L., Weinreich D., Goia D., Pavel N., McLaughlin R. E., Tamarkin L., “Colloidal gold: a novel nanoparticle vector for tumor directed drug delivery,” Drug Deliv. 11(3), 169–183 (2004). 10.1080/10717540490433895 [DOI] [PubMed] [Google Scholar]
- 20.Chen Y. H., Tsai C. Y., Huang P. Y., Chang M. Y., Cheng P. C., Chou C. H., Chen D. H., Wang C. R., Shiau A. L., Wu C. L., “Methotrexate conjugated to gold nanoparticles inhibits tumor growth in a syngeneic lung tumor model,” Mol. Pharm. 4(5), 713–722 (2007). 10.1021/mp060132k [DOI] [PubMed] [Google Scholar]
- 21.Li J., Wang X., Wang C., Chen B., Dai Y., Zhang R., Song M., Lv G., Fu D., “The enhancement effect of gold nanoparticles in drug delivery and as biomarkers of drug-resistant cancer cells,” ChemMedChem 2(3), 374–378 (2007). 10.1002/cmdc.200600264 [DOI] [PubMed] [Google Scholar]
- 22.Patra C. R., Bhattacharya R., Wang E., Katarya A., Lau J. S., Dutta S., Muders M., Wang S., Buhrow S. A., Safgren S. L., Yaszemski M. J., Reid J. M., Ames M. M., Mukherjee P., Mukhopadhyay D., “Targeted delivery of gemcitabine to pancreatic adenocarcinoma using cetuximab as a targeting agent,” Cancer Res. 68(6), 1970–1978 (2008). 10.1158/0008-5472.CAN-07-6102 [DOI] [PubMed] [Google Scholar]
- 23.Podsiadlo P., Sinani V. A., Bahng J. H., Kam N. W., Lee J., Kotov N. A., “Gold nanoparticles enhance the anti-leukemia action of a 6-mercaptopurine chemotherapeutic agent,” Langmuir 24(2), 568–574 (2008). 10.1021/la702782k [DOI] [PubMed] [Google Scholar]
- 24.Azzam E. M. S., Morsy S. M. I., “Enhancement of the antitumour activity for the synthesised dodecylcysteine surfactant using gold nanoparticles,” J. Surf. Deterg. 11(3), 195–199 (2008). 10.1007/s11743-008-1072-8 [DOI] [Google Scholar]
- 25.Stiti M., Cecchi A., Rami M., Abdaoui M., Barragan-Montero V., Scozzafava A., Guari Y., Winum J. Y., Supuran C. T., “Carbonic anhydrase inhibitor coated gold nanoparticles selectively inhibit the tumor-associated isoform IX over the cytosolic isozymes I and II,” J. Am. Chem. Soc. 130(48), 16130–16131 (2008). 10.1021/ja805558k [DOI] [PubMed] [Google Scholar]
- 26.Agasti S. S., Chompoosor A., You C. C., Ghosh P., Kim C. K., Rotello V. M., “Photoregulated release of caged anticancer drugs from gold nanoparticles,” J. Am. Chem. Soc. 131(16), 5728–5729 (2009). 10.1021/ja900591t [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dhar S., Daniel W. L., Giljohann D. A., Mirkin C. A., Lippard S. J., “Polyvalent oligonucleotide gold nanoparticle conjugates as delivery vehicles for platinum(IV) warheads,” J. Am. Chem. Soc. 131(41), 14652–14653 (2009). 10.1021/ja9071282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hosta L., Pla-Roca M., Arbiol J., López-Iglesias C., Samitier J., Cruz L. J., Kogan M. J., Albericio F., “Conjugation of Kahalalide F with gold nanoparticles to enhance in vitro antitumoral activity,” Bioconjug. Chem. 20(1), 138–146 (2009). 10.1021/bc800362j [DOI] [PubMed] [Google Scholar]
- 29.Dreaden E. C., Mwakwari S. C., Sodji Q. H., Oyelere A. K., El-Sayed M. A., “Tamoxifen-poly(ethylene glycol)-thiol gold nanoparticle conjugates: enhanced potency and selective delivery for breast cancer treatment,” Bioconjug. Chem. 20(12), 2247–2253 (2009). 10.1021/bc9002212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eghtedari M., Liopo A. V., Copland J. A., Oraevsky A. A., Motamedi M., “Engineering of hetero-functional gold nanorods for the in vivo molecular targeting of breast cancer cells,” Nano Lett. 9(1), 287–291 (2009). 10.1021/nl802915q [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park C., Youn H., Kim H., Noh T., Kook Y. H., Oh E. T., Park H. J., Kim C., “Cyclodextrin-covered gold nanoparticles for targeted delivery of an anti-cancer drug,” J. Mater. Chem. 19(16), 2310–2315 (2009). 10.1039/b816209c [DOI] [Google Scholar]
- 32.Wang F., Wang Y. C., Dou S., Xiong M. H., Sun T. M., Wang J., “Doxorubicin-tethered responsive gold nanoparticles facilitate intracellular drug delivery for overcoming multidrug resistance in cancer cells,” ACS Nano 5(5), 3679–3692 (2011). 10.1021/nn200007z [DOI] [PubMed] [Google Scholar]
- 33.Staroverov S. A., Gasina O. A., Kladiev A. A., Bogatyrev V. A., “The impact of complex prospidin–colloidal gold on tumor cells,” Russian Journal of Biotherapy 9(3), 22–23 (2010). [Google Scholar]
- 34.Xing Z., Liu Z., Zu Y., Fu Y., Zhao C., Zhao X., Meng R., Tan S., “Synthesis of camptothecin-loaded gold nanomaterials,” Appl. Surf. Sci. 256(12), 3917–3920 (2010). 10.1016/j.apsusc.2010.01.050 [DOI] [Google Scholar]
- 35.François A., Laroche A., Pinaud N., Salmon L., Ruiz J., Robert J., Astruc D., “Encapsulation of docetaxel into PEGylated gold nanoparticles for vectorization to cancer cells,” ChemMedChem 6(11), 2003–2008 (2011). 10.1002/cmdc.201100311 [DOI] [PubMed] [Google Scholar]
- 36.Manju S., Sreenivasan K., “Gold nanoparticles generated and stabilized by water soluble curcumin-polymer conjugate: blood compatibility evaluation and targeted drug delivery onto cancer cells,” J. Colloid Interface Sci. 368(1), 144–151 (2012). 10.1016/j.jcis.2011.11.024 [DOI] [PubMed] [Google Scholar]
- 37.Tomuleasa C., Soritau O., Orza A., Dudea M., Petrushev B., Mosteanu O., Susman S., Florea A., Pall E., Aldea M., Kacso G., Cristea V., Berindan-Neagoe I., Irimie A., “Gold nanoparticles conjugated with cisplatin/doxorubicin/capecitabine lower the chemoresistance of hepatocellular carcinoma-derived cancer cells,” J. Gastrointestin. Liver Dis. 21(2), 187–196 (2012). [PubMed] [Google Scholar]
- 38.Joshi P., Chakraborti S., Ramirez-Vick J. E., Ansari Z. A., Shanker V., Chakrabarti P., Singh S. P., “The anticancer activity of chloroquine-gold nanoparticles against MCF-7 breast cancer cells,” Colloids Surf. B Biointerfaces 95, 195–200 (2012). 10.1016/j.colsurfb.2012.02.039 [DOI] [PubMed] [Google Scholar]
- 39.Pandey S., Mewada A., Thakur M., Shah R., Oza G., Sharon M., “Biogenic gold nanoparticles as fotillas to fire berberine hydrochloride using folic acid as molecular road map,” Mater. Sci. Eng. C 33(7), 3716–3722 (2013). 10.1016/j.msec.2013.05.007 [DOI] [PubMed] [Google Scholar]
- 40.Coelho S. C., Rocha S., Juzenas P., Sampaio P., Almeida G. M., Silva F. S., Pereira M. C., Coelho M. A., “Gold nanoparticle delivery-enhanced proteasome inhibitor effect in adenocarcinoma cells,” Expert Opin. Drug Deliv. 10(10), 1345–1352 (2013). 10.1517/17425247.2013.827659 [DOI] [PubMed] [Google Scholar]
- 41.Kao H.-W., Lin Y.-Y., Chen C.-C., Chi K.-H., Tien D.-C., Hsia C.-C., Lin W.-J., Chen F.-D., Lin M.-H., Wang H.-E., “Biological characterization of cetuximab-conjugated gold nanoparticles in a tumor animal model,” Nanotechnology 25(29), 295102 (2014). 10.1088/0957-4484/25/29/295102 [DOI] [PubMed] [Google Scholar]
- 42.Chen C.-C., Hsieh D.-S., Huang K.-J., Chan Y.-L., Hong P.-D., Yeh M.-K., Wu C.-J., “Improving anticancer efficacy of (-)-epigallocatechin-3-gallate gold nanoparticles in murine B16F10 melanoma cells,” Drug Des. Devel. Ther. 8(8), 459–474 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Labala S., Mandapalli P. K., Kurumaddali A., Venuganti V. V. K., “Layer-by-layer polymer coated gold nanoparticles for topical delivery of imatinib mesylate to treat melanoma,” Mol. Pharm. 12(3), 878–888 (2015). 10.1021/mp5007163 [DOI] [PubMed] [Google Scholar]
- 44.Kumar C. S., Mahesh A., Antoniraj M. G., Vaidevi S., Ruckmani K., “Ultrafast synthesis of stabilized gold nanoparticles using aqueous fruit extract of Limonia acidissima L. and conjugated epirubicin: targeted drug delivery for treatment of breast cancer,” RSC Advances 6(32), 26874–26882 (2016). 10.1039/C6RA01482H [DOI] [Google Scholar]
- 45.Rizk N., Christoforou N., Lee S., “Optimization of anti-cancer drugs and a targeting molecule on multifunctional gold nanoparticles,” Nanotechnology 27(18), 185704 (2016). 10.1088/0957-4484/27/18/185704 [DOI] [PubMed] [Google Scholar]
- 46.Pradhan A., Bepari M., Maity P., Roy S. S., Roy S., Choudhury S. M., “Gold nanoparticles from indole-3-carbinol exhibit cytotoxic, genotoxic and antineoplastic effects through the induction of apoptosis,” RSC Advances 6(61), 56435–56449 (2016). 10.1039/C6RA05591E [DOI] [Google Scholar]
- 47.Nair R. V., Santhakumar H., Jayasree R. S., “Gold nanorods decorated with a cancer drug for multimodal imaging and therapy,” Faraday Discuss. 207, 423–435 (2018). 10.1039/C7FD00185A [DOI] [PubMed] [Google Scholar]
- 48.Farooq M. U., Novosad V., Rozhkova E. A., Wali H., Ali A., Fateh A. A., Neogi P. B., Neogi A., Wang Z., “Gold nanoparticles-enabled efficient dual delivery of anticancer therapeutics to HeLa cells,” Sci. Rep. 8(1), 2907 (2018). 10.1038/s41598-018-21331-y [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 49.Iram S., Zahera M., Khan S., Khan I., Syed A., Ansary A. A., Ameen F., Shair O. H. M., Khan M. S., “Gold nanoconjugates reinforce the potency of conjugated cisplatin and doxorubicin,” Colloids Surf. B Biointerfaces 160, 254–264 (2017). 10.1016/j.colsurfb.2017.09.017 [DOI] [PubMed] [Google Scholar]
- 50.Cheng Y., C Samia A., Meyers J. D., Panagopoulos I., Fei B., Burda C., “Highly efficient drug delivery with gold nanoparticle vectors for in vivo photodynamic therapy of cancer,” J. Am. Chem. Soc. 130(32), 10643–10647 (2008). 10.1021/ja801631c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morshed R. A., Muroski M. E., Dai Q., Wegscheid M. L., Auffinger B., Yu D., Han Y., Zhang L., Wu M., Cheng Y., Lesniak M. S., “Cell-penetrating peptide-modified gold nanoparticles for the delivery of doxorubicin to brain metastatic breast cancer,” Mol. Pharm. 13(6), 1843–1854 (2016). 10.1021/acs.molpharmaceut.6b00004 [DOI] [PubMed] [Google Scholar]
- 52.Ali M. R. K., Wu Y., Ghosh D., Do B. H., Chen K., Dawson M. R., Fang N., Sulchek T. A., El-Sayed M. A., “Nuclear membrane-targeted gold nanoparticles inhibit cancer cell migration and invasion,” ACS Nano 11(4), 3716–3726 (2017). 10.1021/acsnano.6b08345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Papaioannou L., Angelopoulou A., Hatziantoniou S., Papadimitriou M., Apostolou P., Papasotiriou I., Avgoustakis K., “Folic acid-functionalized gold nanorods for controlled paclitaxel delivery: in vitro evaluation and cell studies,” AAPS PharmSciTech 20(1), 13 (2018). 10.1208/s12249-018-1226-6 [DOI] [PubMed] [Google Scholar]
- 54.Moghiseh M., Lowe C., Lewis J. G., Kumar D., Butler A., Anderson N., Raja A., “Spectral photon-counting molecular imaging for quantification of monoclonal antibody-conjugated gold nanoparticles targeted to lymphoma and breast cancer: an in vitro study,” Contrast Media Mol. Imaging 2018, 2136840 (2018). 10.1155/2018/2136840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kumar A., Ma H., Zhang X., Huang K., Jin S., Liu J., Wei T., Cao W., Zou G., Liang X.-J., “Gold nanoparticles functionalized with therapeutic and targeted peptides for cancer treatment,” Biomaterials 33(4), 1180–1189 (2012). 10.1016/j.biomaterials.2011.10.058 [DOI] [PubMed] [Google Scholar]
- 56.Kalimuthu K., Lubin B.-C., Bazylevich A., Gellerman G., Shpilberg O., Luboshits G., Firer M. A., “Gold nanoparticles stabilize peptide-drug-conjugates for sustained targeted drug delivery to cancer cells,” J. Nanobiotechnology 16(1), 34 (2018). 10.1186/s12951-018-0362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saadat N., Liu F., Haynes B., Nangia-Makker P., Bao X., Li J., Polin L. A., Gupta S., Mao G., Shekhar M. P., “Nano-targeted delivery of RAD6/translesion synthesis inhibitor for triple negative breast cancer therapy,” Mol. Cancer Ther. 17(12), 2586–2597 (2018). 10.1158/1535-7163.MCT-18-0364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dreaden E. C., Mackey M. A., Huang X., Kang B., El-Sayed M. A., “Beating cancer in multiple ways using nanogold,” Chem. Soc. Rev. 40(7), 3391–3404 (2011). 10.1039/c0cs00180e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wilhelm S., Tavares A. J., Dai Q., Ohta S., Audet J., Dvorak H. F., Chan W. C., “Analysis of nanoparticle delivery to tumours,” Nat. Rev. Mater. 1(5), 16014 (2016). 10.1038/natrevmats.2016.14 [DOI] [Google Scholar]
- 60.Jijie R., Barras A., Teodorescu F., Boukherroub R., Szunerits S., “Advancements on the molecular design of nanoantibiotics: current level of development and future challenges,” Mol. Syst. Des. Eng. 2(4), 349–369 (2017). 10.1039/C7ME00048K [DOI] [Google Scholar]
- 61.Gu H., Ho P. L., Tong E., Wang L., Xu B., “Presenting vancomycin on nanoparticles to enhance antimicrobial activities,” Nano Lett. 3(9), 1261–1263 (2003). 10.1021/nl034396z [DOI] [Google Scholar]
- 62.Rosemary M. J., MacLaren I., Pradeep T., “Investigations of the antibacterial properties of ciprofloxacin@SiO2.,” Langmuir 22(24), 10125–10129 (2006). 10.1021/la061411h [DOI] [PubMed] [Google Scholar]
- 63.Selvaraj V., Alagar M., “Analytical detection and biological assay of antileukemic drug 5-fluorouracil using gold nanoparticles as probe,” Int. J. Pharm. 337(1-2), 275–281 (2007). 10.1016/j.ijpharm.2006.12.027 [DOI] [PubMed] [Google Scholar]
- 64.Saha B., Bhattacharya J., Mukherjee A., Ghosh A. K., Santra C. R., Dasgupta A. K., Karmakar P., “In vitro structural and functional evaluation of gold nanoparticles conjugated antibiotics,” Nanoscale Res. Lett. 2(12), 614–622 (2007). 10.1007/s11671-007-9104-2 [DOI] [Google Scholar]
- 65.Grace A. N., Pandian K., “Antibacterial efficacy of aminoglycosidic antibiotics protected gold nanoparticles – A brief study,” Colloids Surf. A Physicochem. Eng. Asp. 297(1–3), 63–70 (2007). 10.1016/j.colsurfa.2006.10.024 [DOI] [Google Scholar]
- 66.Burygin G. L., Khlebtsov B. N., Shantrokha A. N., Dykman L. A., Bogatyrev V. A., Khlebtsov N. G., “On the enhanced antibacterial activity of antibiotics mixed with gold nanoparticles,” Nanoscale Res. Lett. 4(8), 794–801 (2009). 10.1007/s11671-009-9316-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rai A., Prabhune A., Perry C. C., “Antibiotic mediated synthesis of gold nanoparticles with potent antimicrobial activity and their application in antimicrobial coatings,” J. Mater. Chem. 20(32), 6789–6798 (2010). 10.1039/c0jm00817f [DOI] [Google Scholar]
- 68.Pradeepa S. M., Vidya S. M., Mutalik S., Udaya Bhat K., Huilgol P., Avadhani K., “Preparation of gold nanoparticles by novel bacterial exopolysaccharide for antibiotic delivery,” Life Sci. 153, 171–179 (2016). 10.1016/j.lfs.2016.04.022 [DOI] [PubMed] [Google Scholar]
- 69.Rastogi L., Kora A. J., Arunachalam A., “Highly stable, protein capped gold nanoparticles as effective drug delivery vehicles for amino-glycosidic antibiotics,” Mater. Sci. Eng. C 32(6), 1571–1577 (2012). 10.1016/j.msec.2012.04.044 [DOI] [PubMed] [Google Scholar]
- 70.Kalita S., Kandimalla R., Sharma K. K., Kataki A. C., Deka M., Kotoky J., “Amoxicillin functionalized gold nanoparticles reverts MRSA resistance,” Mater. Sci. Eng. C 61, 720–727 (2016). 10.1016/j.msec.2015.12.078 [DOI] [PubMed] [Google Scholar]
- 71.Ali H. R., Ali M. R., Wu Y., Selim S. A., Abdelaal H. F., Nasr E. A., El-Sayed M. A., “Gold nanorods as drug delivery vehicles for rifampicin greatly improve the efficacy of combating Mycobacterium tuberculosis with good biocompatibility with the host cells,” Bioconjug. Chem. 27(10), 2486–2492 (2016). 10.1021/acs.bioconjchem.6b00430 [DOI] [PubMed] [Google Scholar]
- 72.Du L., Suo S., Zhang H., Jia H., Liu K. J., Zhang X. J., Liu Y., “The alternative strategy for designing covalent drugs through kinetic effects of pi-stacking on the self-assembled nanoparticles: a model study with antibiotics,” Nanotechnology 27(44), 445101 (2016). 10.1088/0957-4484/27/44/445101 [DOI] [PubMed] [Google Scholar]
- 73.Tom R. T., Suryanarayanan V., Reddy P. G., Baskaran S., Pradeep T., “Ciprofloxacin-protected gold nanoparticles,” Langmuir 20(5), 1909–1914 (2004). 10.1021/la0358567 [DOI] [PubMed] [Google Scholar]
- 74.Amini A., Kamali M., Amini B., Najafi A., “Enhanced antibacterial activity of imipenem-immobilized on surface of spherical and rod gold nanoparticles,” J. Phys. D 52(6), 065401 (2019). 10.1088/1361-6463/aaef4d [DOI] [Google Scholar]
- 75.Singh R., Patil S., Singh N., Gupta S., “Dual functionality nanobioconjugates targeting intracellular bacteria in cancer cells with enhanced antimicrobial activity,” Sci. Rep. 7(1), 5792 (2017). 10.1038/s41598-017-06014-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shittu K. O., Bankole M. T., Abdulkareem A. S., Abubakre O. K., Ubaka A. U., “Application of gold nanoparticles for improved drug efficiency,” Adv. Nat. Sci: Nanosci. Nanotechnol. 8(3), 035014 (2017). 10.1088/2043-6254/aa7716 [DOI] [Google Scholar]
- 77.Rajchakit U., Sarojini V., “Recent developments in antimicrobial peptide conjugated gold nanoparticles,” Bioconjug. Chem. 28(11), 2673–2686 (2017). 10.1021/acs.bioconjchem.7b00368 [DOI] [PubMed] [Google Scholar]
- 78.Peng L.-H., Huang Y.-F., Zhang C.-Z., Niu J., Chen Y., Chu Y., Jiang Z.-H., Gao J.-Q., Mao Z.-W., “Integration of antimicrobial peptides with gold nanoparticles as unique non-viral vectors for gene delivery to mesenchymal stem cells with antibacterial activity,” Biomaterials 103, 137–149 (2016). 10.1016/j.biomaterials.2016.06.057 [DOI] [PubMed] [Google Scholar]
- 79.Chowdhury R., Ilyas H., Ghosh A., Ali H., Ghorai A., Midya A., Jana N. R., Das S., Bhunia A., “Multivalent gold nanoparticle-peptide conjugates for targeting intracellular bacterial infections,” Nanoscale 9(37), 14074–14093 (2017). 10.1039/C7NR04062H [DOI] [PubMed] [Google Scholar]
- 80.Casciaro B., Moros M., Rivera-Fernández S., Bellelli A., de la Fuente J. M., Mangoni M. L., “Gold-nanoparticles coated with the antimicrobial peptide esculentin-1a(1-21)NH2 as a reliable strategy for antipseudomonal drugs,” Acta Biomater. 47, 170–181 (2017). 10.1016/j.actbio.2016.09.041 [DOI] [PubMed] [Google Scholar]
- 81.Arayan L. T., Kim H. B., Bernardo Reyes A. W., Xuan Huy N. T., Hong I. H., Lee K., Yeom J.-H., Park Y., Kim S., “The immunomodulatory effect of antimicrobial peptide HPA3P restricts Brucella abortus 544 infection in BALB/c mice,” Vet. Microbiol. 225, 17–24 (2018). 10.1016/j.vetmic.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 82.Singh A. K., Bai X., Amalaradjou M. A. R., Bhunia A. K., “Antilisterial and antibiofilm activities of Pediocin and LAP functionalized gold nanoparticles,” Front. Sustain. Food Syst. 2, 74 (2018). 10.3389/fsufs.2018.00074 [DOI] [Google Scholar]
- 83.de Alteriis E., Maselli V., Falanga A., Galdiero S., Di Lella F. M., Gesuele R., Guida M., Galdiero E., “Efficiency of gold nanoparticles coated with the antimicrobial peptide indolicidin against biofilm formation and development of Candida spp. clinical isolates,” Infect. Drug Resist. 11(11), 915–925 (2018). 10.2147/IDR.S164262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hayat S., Muzammil S., Shabana B., Aslam B., Siddique M. H., Saqalein M., Nisar M. A., “Quorum quenching: role of nanoparticles as signal jammers in Gram-negative bacteria,” Future Microbiol. 14(1), 61–72 (2019). 10.2217/fmb-2018-0257 [DOI] [PubMed] [Google Scholar]
- 85.Zhao Y., Tian Y., Cui Y., Liu W., Ma W., Jiang X., “Small molecule-capped gold nanoparticles as potent antibacterial agents that target Gram-negative bacteria,” J. Am. Chem. Soc. 132(35), 12349–12356 (2010). 10.1021/ja1028843 [DOI] [PubMed] [Google Scholar]
- 86.Yang X., Zhang L., Jiang X., “Aminosaccharide–gold nanoparticle assemblies as narrow-spectrum antibiotics against methicillin-resistant Staphylococcus aureus,” Nano Res. 11(12), 6237–6243 (2018). 10.1007/s12274-018-2143-4 [DOI] [Google Scholar]
- 87.Ahmed A., Khan A. K., Anwar A., Ali S. A., Shah M. R., “Biofilm inhibitory effect of chlorhexidine conjugated gold nanoparticles against Klebsiella pneumoniae,” Microb. Pathog. 98, 50–56 (2016). 10.1016/j.micpath.2016.06.016 [DOI] [PubMed] [Google Scholar]
- 88.Nie Z., Liu K. J., Zhong C. J., Wang L. F., Yang Y., Tian Q., Liu Y., “Enhanced radical scavenging activity by antioxidant-functionalized gold nanoparticles: a novel inspiration for development of new artificial antioxidants,” Free Radic. Biol. Med. 43(9), 1243–1254 (2007). 10.1016/j.freeradbiomed.2007.06.011 [DOI] [PubMed] [Google Scholar]
- 89.Bowman M. C., Ballard T. E., Ackerson C. J., Feldheim D. L., Margolis D. M., Melander C., “Inhibition of HIV fusion with multivalent gold nanoparticles,” J. Am. Chem. Soc. 130(22), 6896–6897 (2008). 10.1021/ja710321g [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chiodo F., Marradi M., Calvo J., Yuste E., Penadés S., “Glycosystems in nanotechnology: Gold glyconanoparticles as carrier for anti-HIV prodrugs,” Beilstein J. Org. Chem. 10, 1339–1346 (2014). 10.3762/bjoc.10.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Joshi H. M., Bhumkar D. R., Joshi K., Pokharkar V., Sastry M., “Gold nanoparticles as carriers for efficient transmucosal insulin delivery,” Langmuir 22(1), 300–305 (2006). 10.1021/la051982u [DOI] [PubMed] [Google Scholar]
- 92.Cho H.-J., Oh J., Choo M.-K., Ha J.-I., Park Y., Maeng H.-J., “Chondroitin sulfate-capped gold nanoparticles for the oral delivery of insulin,” Int. J. Biol. Macromol. 63, 15–20 (2014). 10.1016/j.ijbiomac.2013.10.026 [DOI] [PubMed] [Google Scholar]
- 93.Ehsan O., Qadir M. I., Malik S. A., Abbasi W. S., Ahmad B., “Efficacy of nanogold-insulin as a hypoglycemic agent,” J. Chem. Soc. Pak. 34(2), 365–370 (2012). [Google Scholar]
- 94.Shilo M., Berenstein P., Dreifuss T., Nash Y., Goldsmith G., Kazimirsky G., Motiei M., Frenkel D., Brodie C., Popovtzer R., “Insulin-coated gold nanoparticles as a new concept for personalized and adjustable glucose regulation,” Nanoscale 7(48), 20489–20496 (2015). 10.1039/C5NR04881H [DOI] [PubMed] [Google Scholar]
- 95.Chamberland D. L., Agarwal A., Kotov N., Brian Fowlkes J., Carson P. L., Wang X., “Photoacoustic tomography of joints aided by an Etanercept-conjugated gold nanoparticle contrast agent-an ex vivo preliminary rat study,” Nanotechnology 19(9), 095101 (2008). 10.1088/0957-4484/19/9/095101 [DOI] [PubMed] [Google Scholar]
- 96.Huang Y.-J., Shiau A.-L., Chen S.-Y., Chen Y.-L., Wang C.-R., Tsai C.-Y., Chang M.-Y., Li Y.-T., Leu C.-H., Wu C.-L., “Multivalent structure of galectin-1-nanogold complex serves as potential therapeutics for rheumatoid arthritis by enhancing receptor clustering,” Eur. Cell. Mater. 23, 170–181 (2012). 10.22203/eCM.v023a13 [DOI] [PubMed] [Google Scholar]
- 97.Gomes A., Datta P., Sengupta J., Biswas A., Gomes A., “Evaluation of anti-arthritic property of methotrexate conjugated gold nanoparticle on experimental animal models,” J. Nanopharm. Drug Deliv. 1(2), 206–211 (2013). 10.1166/jnd.2013.1015 [DOI] [Google Scholar]
- 98.Abdellatif A. A. H., Rasoul S. A. E., Osman S., “Gold nanoparticles decorated with octreotide for somatostatin receptors targeting,” J. Pharm. Sci. Res. 7(1), 14–20 (2015). [Google Scholar]
- 99.Lee H., Lee M.-Y., Bhang S. H., Kim B.-S., Kim Y. S., Ju J. H., Kim K. S., Hahn S. K., “Hyaluronate-gold nanoparticle/tocilizumab complex for the treatment of rheumatoid arthritis,” ACS Nano 8(5), 4790–4798 (2014). 10.1021/nn500685h [DOI] [PubMed] [Google Scholar]
- 100.Rattanata N., Klaynongsruang S., Leelayuwat C., Limpaiboon T., Lulitanond A., Boonsiri P., Chio-Srichan S., Soontaranon S., Rugmai S., Daduang J., “Gallic acid conjugated with gold nanoparticles: antibacterial activity and mechanism of action on foodborne pathogens,” Int. J. Nanomedicine 11(11), 3347–3356 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sonu V. K., Rajkumar I., Bhattacharjee K., Joshi S. R., Mitra S., “Interaction of caffeine and sulfadiazine with lysozyme adsorbed at colloidal metal nanoparticle interface: influence on drug transport ability and antibacterial activity,” J. Biomol. Struct. Dyn. 37(2), 321–335 (2019). 10.1080/07391102.2018.1426497 [DOI] [PubMed] [Google Scholar]
- 102.Gao N., Sun H., Dong K., Ren J., Qu X., “Gold-nanoparticle-based multifunctional amyloid-β inhibitor against Alzheimer’s disease,” Chemistry 21(2), 829–835 (2015). 10.1002/chem.201404562 [DOI] [PubMed] [Google Scholar]
- 103.Gonzalez-Carter D. A., Ong Z. Y., McGilvery C. M., Dunlop I. E., Dexter D. T., Porter A. E., “L-DOPA functionalized, multi-branched gold nanoparticles as brain-targeted nano-vehicles,” Nanomedicine (Lond.) 15(1), 1–11 (2019). 10.1016/j.nano.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 104.Imran M., Hameed A., Shafiullah R. M., Hafizur R. M., Ali I., Roome T., Shah M. R., “Fabrication of Xanthan stabilized green gold nanoparticles based tolbutamide delivery system for enhanced insulin secretion in mice pancreatic islets,” J. Macromol. Sci. A 55(11–12), 729–735 (2018). 10.1080/10601325.2018.1510290 [DOI] [Google Scholar]
- 105.Zhang D., Zhang J., Zeng J., Li Z., Zuo H., Huang C., Zhao X., “Nano-gold loaded with resveratrol enhance the anti-hepatoma effect of resveratrol in vitro and in vivo,” J. Biomed. Nanotechnol. 15(2), 288–300 (2019). 10.1166/jbn.2019.2682 [DOI] [PubMed] [Google Scholar]
- 106.Wang C., Wang Y., Zhang L., Miron R. J., Liang J., Shi M., Mo W., Zheng S., Zhao Y., Zhang Y., “Pretreated macrophage-membrane-coated gold nanocages for precise drug delivery for treatment of bacterial infections,” Adv. Mater. 30(46), e1804023 (2018). 10.1002/adma.201804023 [DOI] [PubMed] [Google Scholar]
- 107.Miller A. D., “Human gene therapy comes of age,” Nature 357(6378), 455–460 (1992). 10.1038/357455a0 [DOI] [PubMed] [Google Scholar]
- 108.Zelenin A. V., “Gene therapy: On the threshold of the third millennium,” Herald Russ. Acad. Sci. 71(3), 215–222 (2001). [Google Scholar]
- 109.Tiwari P. M., Vig K., Dennis V. A., Singh S. R., “Functionalized gold nanoparticles and their biomedical applications,” Nanomaterials (Basel) 1(1), 31–63 (2011). 10.3390/nano1010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zaimy M. A., Saffarzadeh N., Mohammadi A., Pourghadamyari H., Izadi P., Sarli A., Moghaddam L. K., Paschepari S. R., Azizi H., Torkamandi S., Tavakkoly-Bazzaz J., “New methods in the diagnosis of cancer and gene therapy of cancer based on nanoparticles,” Cancer Gene Ther. 24(6), 233–243 (2017). 10.1038/cgt.2017.16 [DOI] [PubMed] [Google Scholar]
- 111.Mendes R., Fernandes A. R., Baptista P. V., “Gold nanoparticle approach to the selective delivery of gene silencing in cancer—the case for combined delivery?” Genes (Basel) 8(3), 94 (2017). 10.3390/genes8030094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang S., Yan C., Zhang X., Shi D., Chi L., Luo G., Deng J., “Antimicrobial peptide modification enhances the gene delivery and bactericidal efficiency of gold nanoparticles for accelerating diabetic wound healing,” Biomater. Sci. 6(10), 2757–2772 (2018). 10.1039/C8BM00807H [DOI] [PubMed] [Google Scholar]
- 113.Barnaby S. N., Lee A., Mirkin C. A., “Probing the inherent stability of siRNA immobilized on nanoparticle constructs,” Proc. Natl. Acad. Sci. U.S.A. 111(27), 9739–9744 (2014). 10.1073/pnas.1409431111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Artiga A., Serrano-Sevilla I., De Matteis L., Mitchell S. G., de la Fuente J. M., “Current status and future perspectives of gold nanoparticle vectors for siRNA delivery,” J. Mater. Chem. B Mater. Biol. Med. 7(6), 876–896 (2019). 10.1039/C8TB02484G [DOI] [PubMed] [Google Scholar]
- 115.Morgan E., Wupperfeld D., Morales D., Reich N., “Shape matters: Gold nanoparticle shape impacts the biological activity of siRNA delivery,” Bioconjug. Chem. 30(3), 853–860 (2019). 10.1021/acs.bioconjchem.9b00004 [DOI] [PubMed] [Google Scholar]
- 116.Ledford H., “CRISPR: gene editing is just the beginning,” Nature 531(7593), 156–159 (2016). 10.1038/531156a [DOI] [PubMed] [Google Scholar]
- 117.Lino C. A., Harper J. C., Carney J. P., Timlin J. A., “Delivering CRISPR: a review of the challenges and approaches,” Drug Deliv. 25(1), 1234–1257 (2018). 10.1080/10717544.2018.1474964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Glass Z., Li Y., Xu Q., “Nanoparticles for CRISPR-Cas9 delivery,” Nat. Biomed. Eng. 1(11), 854–855 (2017). 10.1038/s41551-017-0158-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lee K., Conboy M., Park H. M., Jiang F., Kim H. J., Dewitt M. A., Mackley V. A., Chang K., Rao A., Skinner C., Shobha T., Mehdipour M., Liu H., Huang W. C., Lan F., Bray N. L., Li S., Corn J. E., Kataoka K., Doudna J. A., Conboy I., Murthy N., “Nanoparticle delivery of Cas9 ribonucleoprotein and donor DNA in vivo induces homology-directed DNA repair,” Nat. Biomed. Eng. 1(11), 889–901 (2017). 10.1038/s41551-017-0137-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mout R., Ray M., Yesilbag Tonga G., Lee Y. W., Tay T., Sasaki K., Rotello V. M., “Direct cytosolic delivery of CRISPR/Cas9-ribonucleoprotein for efficient gene editing,” ACS Nano 11(3), 2452–2458 (2017). 10.1021/acsnano.6b07600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Schomaker M., Killian D., Willenbrock S., Heinemann D., Kalies S., Ngezahayo A., Nolte I., Ripken T., Junghanß C., Meyer H., Murua Escobar H., Heisterkamp A., “Biophysical effects in off-resonant gold nanoparticle mediated (GNOME) laser transfection of cell lines, primary- and stem cells using fs laser pulses,” J. Biophotonics 8(8), 646–658 (2015). 10.1002/jbio.201400065 [DOI] [PubMed] [Google Scholar]
- 122.Xiong R., Raemdonck K., Peynshaert K., Lentacker I., De Cock I., Demeester J., De Smedt S. C., Skirtach A. G., Braeckmans K., “Comparison of gold nanoparticle mediated photoporation: vapor nanobubbles outperform direct heating for delivering macromolecules in live cells,” ACS Nano 8(6), 6288–6296 (2014). 10.1021/nn5017742 [DOI] [PubMed] [Google Scholar]
- 123.Nakatsuji H., Kawabata Galbraith K., Kurisu J., Imahori H., Murakami T., Kengaku M., “Surface chemistry for cytosolic gene delivery and photothermal transgene expression by gold nanorods,” Sci. Rep. 7(1), 4694 (2017). 10.1038/s41598-017-04912-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bibikova O., Singh P., Popov A., Akchurin G., Skaptsov A., Skovorodkin I., Khanadeev V., Mikhalevich D., Kinnunen M., Akchurin G., Bogatyrev V., Khlebtsov N., Vainio S. J., Meglinski I., Tuchin V., “Shape-dependent interaction of gold nanoparticles with cultured cells at laser exposure,” Laser Phys. Lett. 14(5), 055901 (2017). 10.1088/1612-202X/aa63ae [DOI] [Google Scholar]
- 125.Yao C., Rudnitzki F., Hüttmann G., Zhang Z., Rahmanzadeh R., “Important factors for cell-membrane permeabilization by gold nanoparticles activated by nanosecond-laser irradiation,” Int. J. Nanomedicine 12(12), 5659–5672 (2017). 10.2147/IJN.S140620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pylaev T., Vanzha E., Avdeeva E., Khlebtsov B., Khlebtsov N., “A novel cell transfection platform based on laser optoporation mediated by Au nanostar layers,” J. Biophotonics 12(1), e201800166 (2019). 10.1002/jbio.201800166 [DOI] [PubMed] [Google Scholar]
- 127.Lyu Z., Zhou F., Liu Q., Xue H., Yu Q., Chen H., “A universal platform for macromolecular deliveryinto cells using gold nanoparticle layers via the photoporation effect,” Adv. Funct. Mater. 26(32), 5787–5795 (2016). 10.1002/adfm.201602036 [DOI] [Google Scholar]
- 128.Hühn J., Carrillo-Carrion C., Soliman M. G., Pfeiffer C., Valdeperez D., Masood A., Chakraborty I., Zhu L., Gallego M., Yue Z., Carril M., Feliu N., Escudero A., Alkilany A. M., Pelaz B., del Pino P., Parak W. J., “Selected standard protocols for the synthesis, phase transfer, and characterization of inorganic colloidal nanoparticles,” Chem. Mater. 29(1), 399–461 (2017). 10.1021/acs.chemmater.6b04738 [DOI] [Google Scholar]
- 129.Sapsford K. E., Algar W. R., Berti L., Gemmill K. B., Casey B. J., Oh E., Stewart M. H., Medintz I. L., “Functionalizing nanoparticles with biological molecules: developing chemistries that facilitate nanotechnology,” Chem. Rev. 113(3), 1904–2074 (2013). 10.1021/cr300143v [DOI] [PubMed] [Google Scholar]
- 130.Kabir N., Ali H., Ateeq M., Bertino M. F., Shah M. R., Franzel L., “Silymarin coated gold nanoparticles ameliorates CCl4-induced hepatic injury and cirrhosis through down regulation of Hepatic stellate cells and attenuation of Kupffer cells,” RSC Advances 4(18), 9012–9020 (2014). 10.1039/C3RA46093B [DOI] [Google Scholar]
- 131.Rybin A. O., “Green synthesis of gold nanoparticles using silymarin, their effect on animal cell culture in vitro and in vivo,” Agrarian Scientific Journal (11), 37–40 (2017). (in Russian) [Google Scholar]
- 132.Gurunathan S., Kim J.-H., “Biocompatible gold nanoparticles ameliorate retinoic acid-induced cell death and induce differentiation in F9 teratocarcinoma stem cells,” Nanomaterials (Basel) 8(6), 396 (2018). 10.3390/nano8060396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Das S., Roy P., Mondal S., Bera T., Mukherjee A., “One pot synthesis of gold nanoparticles and application in chemotherapy of wild and resistant type visceral leishmaniasis,” Colloids Surf. B Biointerfaces 107, 27–34 (2013). 10.1016/j.colsurfb.2013.01.061 [DOI] [PubMed] [Google Scholar]
- 134.de Oliveira Gonçalves K., da Silva M. N., Sicchieri L. B., de Oliveira Silva F. R., de Matos R. A., Courrol L. C., “Aminolevulinic acid with gold nanoparticles: a novel theranostic agent for atherosclerosis,” Analyst (Lond.) 140(6), 1974–1980 (2015). 10.1039/C4AN02166E [DOI] [PubMed] [Google Scholar]
- 135.Khoobchandani M., Katti K., Maxwell A., Fay W. P., Katti K. V., “Laminin receptor-avid nanotherapeutic EGCg-AuNPs as a potential alternative therapeutic approach to prevent restenosis,” Int. J. Mol. Sci. 17(3), 316 (2016). 10.3390/ijms17030316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Li G., Li D., Zhang L., Zhai J., Wang E., “One-step synthesis of folic acid protected gold nanoparticles and their receptor-mediated intracellular uptake,” Chemistry 15(38), 9868–9873 (2009). 10.1002/chem.200900914 [DOI] [PubMed] [Google Scholar]
- 137.Plan Sangnier A., Aufaure R., Motte L., Wilhelm C., Guenin E., Lalatonne Y., “Hybrid Au@alendronate nanoparticles as dual chemo-photothermal agent for combined cancer treatment,” Beilstein J. Nanotechnol. 9, 2947–2952 (2018). 10.3762/bjnano.9.273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yu J., Wang X., Li Y., Huang X., Luo X., He X., “Synthesis of nerolidol functionalized gold nanoparticles for wound regeneration in people with diabetic foot ulcers in nursing care management,” Sci. Adv. Mater. 10(12), 1775–1781 (2018). 10.1166/sam.2018.3389 [DOI] [Google Scholar]
- 139.Vemuri S. K., Banala R. R., Mukherjee S., Uppula P., Subbaiah G, Gurava R.G.V, Malarvilli T., “Novel biosynthesized gold nanoparticles as anti-cancer agents against breast cancer: Synthesis, biological evaluation, molecular modelling studies,” Mater. Sci. Eng. C 99, 417–429 (2019). 10.1016/j.msec.2019.01.123 [DOI] [PubMed] [Google Scholar]
- 140.Hur Y. E., Kim S., Kim J.-H., Cha S.-H., Choi M.-J., Cho S., Park Y., “One-step functionalization of gold and silver nanoparticles by ampicillin,” Mater. Lett. 129, 185–190 (2014). 10.1016/j.matlet.2014.05.032 [DOI] [Google Scholar]
- 141.Payne J. N., Waghwani H. K., Connor M. G., Hamilton W., Tockstein S., Moolani H., Chavda F., Badwaik V., Lawrenz M. B., Dakshinamurthy R., “Novel synthesis of kanamycin conjugated gold nanoparticles with potent antibacterial activity,” Front. Microbiol. 7, 607 (2016). 10.3389/fmicb.2016.00607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lai H.-Z., Chen W.-Y., Wu C.-Y., Chen Y.-C., “Potent antibacterial nanoparticles for pathogenic bacteria,” ACS Appl. Mater. Interfaces 7(3), 2046–2054 (2015). 10.1021/am507919m [DOI] [PubMed] [Google Scholar]
- 143.You Q., Zhang X., Wu F.-G., Chen Y., “Colorimetric and test stripe-based assay of bacteria by using vancomycin-modified gold nanoparticles,” Sens. Actuators B Chem. 281, 408–414 (2019). 10.1016/j.snb.2018.10.103 [DOI] [Google Scholar]
- 144.Demurtas M., Perry C. C., “Facile one-pot synthesis of amoxicillin-coated gold nanoparticles and their antimicrobial activity,” Gold Bull. 47(1–2), 103–107 (2014). 10.1007/s13404-013-0129-2 [DOI] [Google Scholar]
- 145.Silvero C M. J., Rocca D. M., de la Villarmois E. A., Fournier K., Lanterna A. E., Pérez M. F., Becerra M. C., Scaiano J. C., “Selective photoinduced antibacterial activity of amoxicillin-coated gold nanoparticles: from one-step synthesis to in vivo cytocompatibility,” ACS Omega 3(1), 1220–1230 (2018). 10.1021/acsomega.7b01779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Haddada M. B., Jeannot K., Spadavecchia J., “Novel synthesis and characterization of doxycycline-loaded gold nanoparticles: the golden doxycycline for antibacterial applications,” Part. Part. Syst. Charact. 36(2), 1800395 (2019). 10.1002/ppsc.201800395 [DOI] [Google Scholar]
- 147.Anwar A., Siddiqui R., Raza Shah M., Ahmed Khan N., “Gold nanoparticles conjugation enhances antiacanthamoebic properties of nystatin, fluconazole and amphotericin B,” J. Microbiol. Biotechnol. 29(1), 171–177 (2019). 10.4014/jmb.1805.05028 [DOI] [PubMed] [Google Scholar]
- 148.Qiu H., Min Y., Rodgers Z., Zhang L., Wang A. Z., “Nanomedicine approaches to improve cancer immunotherapy,” Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 9(5), e1456 (2017). 10.1002/wnan.1456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Grimaldi A. M., Incoronato M., Salvatore M., Soricelli A., “Nanoparticle-based strategies for cancer immunotherapy and immunodiagnostics,” Nanomedicine (Lond.) 12(19), 2349–2365 (2017). 10.2217/nnm-2017-0208 [DOI] [PubMed] [Google Scholar]
- 150.Hu X., Wu T., Bao Y., Zhang Z., “Nanotechnology based therapeutic modality to boost anti-tumor immunity and collapse tumor defense,” J. Control. Release 256, 26–45 (2017). 10.1016/j.jconrel.2017.04.026 [DOI] [PubMed] [Google Scholar]
- 151.Surendran S. P., Moon M. J., Park R., Jeong Y. Y., “Bioactive nanoparticles for cancer immunotherapy,” Int. J. Mol. Sci. 19(12), 3877 (2018). 10.3390/ijms19123877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Evans E. R., Bugga P., Asthana V., Drezek R., “Metallic nanoparticles for cancer immunotherapy,” Mater Today (Kidlington) 21(6), 673–685 (2018). 10.1016/j.mattod.2017.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Yoon H. Y., Selvan S. T., Yang Y., Kim M. J., Yi D. K., Kwon I. C., Kim K., “Engineering nanoparticle strategies for effective cancer immunotherapy,” Biomaterials 178, 597–607 (2018). 10.1016/j.biomaterials.2018.03.036 [DOI] [PubMed] [Google Scholar]
- 154.Mahjub R., Jatana S., Lee S. E., Qin Z., Pauli G., Soleimani M., Madadi S., Li S.-D., “Recent advances in applying nanotechnologies for cancer immunotherapy,” J. Control. Release 288, 239–263 (2018). 10.1016/j.jconrel.2018.09.010 [DOI] [PubMed] [Google Scholar]
- 155.Jia J., Zhang Y., Xin Y., Jiang C., Yan B., Zhai S., “Interactions between nanoparticles and dendritic cells: from the perspective of cancer immunotherapy,” Front. Oncol. 8, 404 (2018). 10.3389/fonc.2018.00404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Englinger B., Pirker C., Heffeter P., Terenzi A., Kowol C. R., Keppler B. K., Berger W., “Metal drugs and the anticancer immune response,” Chem. Rev. 119(2), 1519–1624 (2019). 10.1021/acs.chemrev.8b00396 [DOI] [PubMed] [Google Scholar]
- 157.Luo L., Shu R., Wu A., “Nanomaterial-based cancer immunotherapy,” J. Mater. Chem. B Mater. Biol. Med. 5(28), 5517–5531 (2017). 10.1039/C7TB01137G [DOI] [Google Scholar]
- 158.Lopez-Campos F., Candini D., Carrasco E., Berenguer Francés M. A., “Nanoparticles applied to cancer immunoregulation,” Rep. Pract. Oncol. Radiother. 24(1), 47–55 (2019). 10.1016/j.rpor.2018.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Le Q.-V., Yang G., Wu Y., Jang H. W., Shokouhimehr M., Oh Y.-K., “Nanomaterials for modulating innate immune cells in cancer immunotherapy,” Asian J. Pharm. Sci. 14(1), 16–29 (2019). 10.1016/j.ajps.2018.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wei M., Chen N., Li J., Yin M., Liang L., He Y., Song H., Fan C., Huang Q., “Polyvalent immunostimulatory nanoagents with self-assembled CpG oligonucleotide-conjugated gold nanoparticles,” Angew. Chem. Int. Ed. Engl. 51(5), 1202–1206 (2012). 10.1002/anie.201105187 [DOI] [PubMed] [Google Scholar]
- 161.Lee I. H., Kwon H. K., An S., Kim D., Kim S., Yu M. K., Lee J. H., Lee T. S., Im S. H., Jon S., “Imageable antigen-presenting gold nanoparticle vaccines for effective cancer immunotherapy in vivo,” Angew. Chem. Int. Ed. Engl. 51(35), 8800–8805 (2012). 10.1002/anie.201203193 [DOI] [PubMed] [Google Scholar]
- 162.Lin A. Y., Almeida J. P., Bear A., Liu N., Luo L., Foster A. E., Drezek R. A., “Gold nanoparticle delivery of modified CpG stimulates macrophages and inhibits tumor growth for enhanced immunotherapy,” PLoS One 8(5), e63550 (2013). 10.1371/journal.pone.0063550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Dykman L. A., Staroverov S. A., Fomin A. S., Khanadeev V. A., Khlebtsov B. N., Bogatyrev V. A., “Gold nanoparticles as an adjuvant: Influence of size, shape, and technique of combination with CpG on antibody production,” Int. Immunopharmacol. 54, 163–168 (2018). 10.1016/j.intimp.2017.11.008 [DOI] [PubMed] [Google Scholar]
- 164.Visaria R. K., Griffin R. J., Williams B. W., Ebbini E. S., Paciotti G. F., Song C. W., Bischof J. C., “Enhancement of tumor thermal therapy using gold nanoparticle-assisted tumor necrosis factor-α delivery,” Mol. Cancer Ther. 5(4), 1014–1020 (2006). 10.1158/1535-7163.MCT-05-0381 [DOI] [PubMed] [Google Scholar]
- 165.Meir R., Shamalov K., Sadan T., Motiei M., Yaari G., Cohen C. J., Popovtzer R., “Fast image-guided stratification using anti-programmed death ligand 1 gold nanoparticles for cancer immunotherapy,” ACS Nano 11(11), 11127–11134 (2017). 10.1021/acsnano.7b05299 [DOI] [PubMed] [Google Scholar]
- 166.Sousa F., Castro P., Fonte P., Kennedy P. J., Neves-Petersen M. T., Sarmento B., “Nanoparticles for the delivery of therapeutic antibodies: Dogma or promising strategy?” Expert Opin. Drug Deliv. 14(10), 1163–1176 (2017). 10.1080/17425247.2017.1273345 [DOI] [PubMed] [Google Scholar]
- 167.Yang Y.-S. S., Moynihan K. D., Bekdemir A., Dichwalkar T. M., Noh M. M., Watson N., Melo M., Ingram J., Suh H., Ploegh H., Stellacci F. R., Irvine D. J., “Targeting small molecule drugs to T cells with antibody-directed cell-penetrating gold nanoparticles,” Biomater. Sci. 7(1), 113–124 (2018). 10.1039/C8BM01208C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mottas I., Bekdemir A., Cereghetti A., Spagnuolo L., Yang Y.-S. S., Müller M., Irvine D. J., Stellacci F., Bourquin C., “Amphiphilic nanoparticle delivery enhances the anticancer efficacy of a TLR7 ligand via local immune activation,” Biomaterials 190-191, 111–120 (2019). 10.1016/j.biomaterials.2018.10.031 [DOI] [PubMed] [Google Scholar]
- 169.Almeida J. P. M., Lin A. Y., Langsner R. J., Eckels P., Foster A. E., Drezek R. A., “In vivo immune cell distribution of gold nanoparticles in naïve and tumor bearing mice,” Small 10(4), 812–819 (2014). 10.1002/smll.201301998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Saha S., Xiong X., Chakraborty P. K., Shameer K., Arvizo R. R., Kudgus R. A., Dwivedi S. K. D., Hossen M. N., Gillies E. M., Robertson J. D., Dudley J. T., Urrutia R. A., Postier R. G., Bhattacharya R., Mukherjee P., “Gold nanoparticle reprograms pancreatic tumor microenvironment and inhibits tumor growth,” ACS Nano 10(12), 10636–10651 (2016). 10.1021/acsnano.6b02231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Tsai Y. S., Chen Y. H., Cheng P. C., Tsai H. T., Shiau A. L., Tzai T. S., Wu C. L., “TGF-β1 conjugated to gold nanoparticles results in protein conformational changes and attenuates the biological function,” Small 9(12), 2119–2128 (2013). 10.1002/smll.201202755 [DOI] [PubMed] [Google Scholar]
- 172.Lin A. Y., Lunsford J., Bear A. S., Young J. K., Eckels P., Luo L., Foster A. E., Drezek R. A., “High-density sub-100-nm peptide-gold nanoparticle complexes improve vaccine presentation by dendritic cells in vitro,” Nanoscale Res. Lett. 8(1), 72 (2013). 10.1186/1556-276X-8-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Almeida J. P. M., Lin A. Y., Figueroa E. R., Foster A. E., Drezek R. A., “In vivo gold nanoparticle delivery of peptide vaccine induces anti-tumor immune response in prophylactic and therapeutic tumor models,” Small 11(12), 1453–1459 (2015). 10.1002/smll.201402179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brinãs R. P., Sundgren A., Sahoo P., Morey S., Rittenhouse-Olson K., Wilding G. E., Deng W., Barchi J. J., Jr., “Design and synthesis of multifunctional gold nanoparticles bearing tumor-associated glycopeptide antigens as potential cancer vaccines,” Bioconjug. Chem. 23(8), 1513–1523 (2012). 10.1021/bc200606s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Parry A. L., Clemson N. A., Ellis J., Bernhard S. S. R., Davis B. G., Cameron N. R., “‘Multicopy multivalent’ glycopolymer-stabilized gold nanoparticles as potential synthetic cancer vaccines,” J. Am. Chem. Soc. 135(25), 9362–9365 (2013). 10.1021/ja4046857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Park Y. M., Lee S. J., Kim Y. S., Lee M. H., Cha G. S., Jung I. D., Kang T. H., Han H. D., “Nanoparticle-based vaccine delivery for cancer immunotherapy,” Immune Netw. 13(5), 177–183 (2013). 10.4110/in.2013.13.5.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Almeida J. P. M., Figueroa E. R., Drezek R. A., “Gold nanoparticle mediated cancer immunotherapy,” Nanomedicine (Lond.) 10(3), 503–514 (2014). 10.1016/j.nano.2013.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Biswas S., Medina S. H., Barchi J. J., Jr., “Synthesis and cell-selective antitumor properties of amino acid conjugated tumor-associated carbohydrate antigen-coated gold nanoparticles,” Carbohydr. Res. 405, 93–101 (2015). 10.1016/j.carres.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zhou Q., Zhang Y., Du J., Li Y., Zhou Y., Fu Q., Zhang J., Wang X., Zhan L., “Different-sized gold nanoparticle activator/antigen increases dendritic cells accumulation in liver-draining lymph nodes and Cd8+ T cell responses,” ACS Nano 10(2), 2678–2692 (2016). 10.1021/acsnano.5b07716 [DOI] [PubMed] [Google Scholar]
- 180.Ma X., Hui H., Jin Y., Dong D., Liang X., Yang X., Tan K., Dai Z., Cheng Z., Tian J., “Enhanced immunotherapy of SM5-1 in hepatocellular carcinoma by conjugating with gold nanoparticles and its in vivo bioluminescence tomographic evaluation,” Biomaterials 87, 46–56 (2016). 10.1016/j.biomaterials.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 181.Dykman L. A., Sumaroka M. V., Staroverov S. A., Zaĭtseva I. S., Bogatyrev V. A., “[Immunogenic properties of the colloidal gold],” Izv. Akad. Nauk Ser. Biol. 31(1), 86–91 (2004). [PubMed] [Google Scholar]
- 182.Ahn S., Lee I. H., Kang S., Kim D., Choi M., Saw P. E., Shin E. C., Jon S., “Gold nanoparticles displaying tumor-associated self-antigens as a potential vaccine for cancer immunotherapy,” Adv. Healthc. Mater. 3(8), 1194–1199 (2014). 10.1002/adhm.201300597 [DOI] [PubMed] [Google Scholar]
- 183.Tomić S., Ðokić J., Vasilijić S., Ogrinc N., Rudolf R., Pelicon P., Vučević D., Milosavljević P., Janković S., Anžel I., Rajković J., Rupnik M. S., Friedrich B., Colić M., “Size-dependent effects of gold nanoparticles uptake on maturation and antitumor functions of human dendritic cells in vitro,” PLoS One 9(5), e96584 (2014). 10.1371/journal.pone.0096584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kang S., Ahn S., Lee J., Kim J. Y., Choi M., Gujrati V., Kim H., Kim J., Shin E.-C., Jon S., “Effects of gold nanoparticle-based vaccine size on lymph node delivery and cytotoxic T-lymphocyte responses,” J. Control. Release 256, 56–67 (2017). 10.1016/j.jconrel.2017.04.024 [DOI] [PubMed] [Google Scholar]
- 185.Wu C., Chen H., Wu X., Cong X., Wang L., Wang Y., Yang Y., Li W., Sun T., “The influence of tumor-induced immune dysfunction on the immune cell distribution of gold nanoparticles in vivo,” Biomater. Sci. 5(8), 1531–1536 (2017). 10.1039/C7BM00335H [DOI] [PubMed] [Google Scholar]
- 186.Andersson H. A., Kim Y.-S., O’Neill B. E., Shi Z.-Z., Serda R. E., “HSP70 promoter-driven activation of gene expression for immunotherapy using gold nanorods and near infrared light,” Vaccines (Basel) 2(2), 216–227 (2014). 10.3390/vaccines2020216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Cohn L., Delamarre L., “Dendritic cell-targeted vaccines,” Front. Immunol. 5, 255 (2014). 10.3389/fimmu.2014.00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Vang K. B., Safina I., Darrigues E., Nedosekin D., Nima Z. A., Majeed W., Watanabe F., Kannarpady G., Kore R. A., Casciano D., Zharov V. P., Griffin R. J., Dings R. P. M., Biris A. S., “Modifying dendritic cell activation with plasmonic nano vectors,” Sci. Rep. 7(1), 5513 (2017). 10.1038/s41598-017-04459-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Liang R., Xie J., Li J., Wang K., Liu L., Gao Y., Hussain M., Shen G., Zhu J., Tao J., “Liposomes-coated gold nanocages with antigens and adjuvants targeted delivery to dendritic cells for enhancing antitumor immune response,” Biomaterials 149, 41–50 (2017). 10.1016/j.biomaterials.2017.09.029 [DOI] [PubMed] [Google Scholar]
- 190.Zang X., Zhao X., Hu H., Qiao M., Deng Y., Chen D., “Nanoparticles for tumor immunotherapy,” Eur. J. Pharm. Biopharm. 115, 243–256 (2017). 10.1016/j.ejpb.2017.03.013 [DOI] [PubMed] [Google Scholar]
- 191.Ahmad S., Zamry A. A., Tan H.-T. T., Wong K. K., Lim J., Mohamud R., “Targeting dendritic cells through gold nanoparticles: A review on the cellular uptake and subsequent immunological properties,” Mol. Immunol. 91, 123–133 (2017). 10.1016/j.molimm.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 192.Fogli S., Montis C., Paccosi S., Silvano A., Michelucci E., Berti D., Bosi A., Parenti A., Romagnoli P., “Inorganic nanoparticles as potential regulators of immune response in dendritic cells,” Nanomedicine (Lond.) 12(14), 1647–1660 (2017). 10.2217/nnm-2017-0061 [DOI] [PubMed] [Google Scholar]
- 193.Dings R. P. M., Cannon M., Vang K. B., “Design of gold nanoparticles in dendritic cell-based vaccines,” Part. Part. Syst. Charact. 35(9), 1800109 (2018). 10.1002/ppsc.201800109 [DOI] [Google Scholar]
- 194.Calderon-Gonzalez R., Terán-Navarro H., García I., Marradi M., Salcines-Cuevas D., Yañez-Diaz S., Solis-Angulo A., Frande-Cabanes E., Fariñas M. C., Garcia-Castaño A., Gomez-Roman J., Penades S., Rivera F., Freire J., Álvarez-Domínguez C., “Gold glyconanoparticles coupled to listeriolysin O 91-99 peptide serve as adjuvant therapy against melanoma,” Nanoscale 9(30), 10721–10732 (2017). 10.1039/C7NR02494K [DOI] [PubMed] [Google Scholar]
- 195.Cruz L. J., Rueda F., Cordobilla B., Simón L., Hosta L., Albericio F., Domingo J. C., “Targeting nanosystems to human DCs via Fc receptor as an effective strategy to deliver antigen for immunotherapy,” Mol. Pharm. 8(1), 104–116 (2011). 10.1021/mp100178k [DOI] [PubMed] [Google Scholar]
- 196.Dreaden E. C., Mwakwari S. C., Austin L. A., Kieffer M. J., Oyelere A. K., El-Sayed M. A., “Small molecule-gold nanorod conjugates selectively target and induce macrophage cytotoxicity towards breast cancer cells,” Small 8(18), 2819–2822 (2012). 10.1002/smll.201200333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wang X., Li J., Kawazoe N., Chen G., “Photothermal ablation of cancer cells by albumin-modified gold nanorods and activation of dendritic cells,” Materials (Basel) 12(1), 31 (2018). 10.3390/ma12010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Choi M. R., Stanton-Maxey K. J., Stanley J. K., Levin C. S., Bardhan R., Akin D., Badve S., Sturgis J., Robinson J. P., Bashir R., Halas N. J., Clare S. E., “A cellular Trojan Horse for delivery of therapeutic nanoparticles into tumors,” Nano Lett. 7(12), 3759–3765 (2007). 10.1021/nl072209h [DOI] [PubMed] [Google Scholar]
- 199.Spyratou E., Makropoulou M., Efstathopoulos E. P., Georgakilas A. G., Sihver L., “Recent advances in cancer therapy based on dual mode gold nanoparticles,” Cancers (Basel) 9(12), 173 (2017). 10.3390/cancers9120173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Tian Y., Guo R., Yang W., “Multifunctional nanotherapeutics for photothermal combination therapy of cancer,” Adv. Ther. 1(8), 1800049 (2018). 10.1002/adtp.201800049 [DOI] [Google Scholar]
- 201.Liu Y., Crawford B. M., Vo-Dinh T., “Gold nanoparticles-mediated photothermal therapy and immunotherapy,” Immunotherapy 10(13), 1175–1188 (2018). 10.2217/imt-2018-0029 [DOI] [PubMed] [Google Scholar]
- 202.Li Y., Li X., Zhou F., Doughty A., Hoover A. R., Nordquist R. E., Chen W. R., “Nanotechnology-based photoimmunological therapies for cancer,” Cancer Lett. 442, 429–438 (2019). 10.1016/j.canlet.2018.10.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Beik J., Khateri M., Khosravi Z., Kamrava S. K., Kooranifar S., Ghaznavi H., Shakeri-Zadeh A., “Gold nanoparticles in combinatorial cancer therapy strategies,” Coord. Chem. Rev. 387, 299–324 (2019). 10.1016/j.ccr.2019.02.025 [DOI] [Google Scholar]
- 204.You J., Zhang R., Zhang G., Zhong M., Liu Y., Van Pelt C. S., Liang D., Wei W., Sood A. K., Li C., “Photothermal-chemotherapy with doxorubicin-loaded hollow gold nanospheres: A platform for near-infrared light-trigged drug release,” J. Control. Release 158(2), 319–328 (2012). 10.1016/j.jconrel.2011.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Mendes R., Pedrosa P., Lima J. C., Fernandes A. R., Baptista P. V., “Photothermal enhancement of chemotherapy in breast cancer by visible irradiation of Gold Nanoparticles,” Sci. Rep. 7(1), 10872 (2017). 10.1038/s41598-017-11491-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Nam J., Son S., Ochyl L. J., Kuai R., Schwendeman A., Moon J. J., “Chemo-photothermal therapy combination elicits anti-tumor immunity against advanced metastatic cancer,” Nat. Commun. 9(1), 1074 (2018). 10.1038/s41467-018-03473-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Bisker G., Yeheskely-Hayon D., Minai L., Yelin D., “Controlled release of Rituximab from gold nanoparticles for phototherapy of malignant cells,” J. Control. Release 162(2), 303–309 (2012). 10.1016/j.jconrel.2012.06.030 [DOI] [PubMed] [Google Scholar]
- 208.Shao J., Griffin R. J., Galanzha E. I., Kim J. W., Koonce N., Webber J., Mustafa T., Biris A. S., Nedosekin D. A., Zharov V. P., “Photothermal nanodrugs: potential of TNF-gold nanospheres for cancer theranostics,” Sci. Rep. 3(1), 1293 (2013). 10.1038/srep01293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Nam J., La W.-G., Hwang S., Ha Y. S., Park N., Won N., Jung S., Bhang S. H., Ma Y.-J., Cho Y.-M., Jin M., Han J., Shin J.-Y., Wang E. K., Kim S. G., Cho S.-H., Yoo J., Kim B.-S., Kim S., “pH-responsive assembly of gold nanoparticles and “spatiotemporally concerted” drug release for synergistic cancer therapy,” ACS Nano 7(4), 3388–3402 (2013). 10.1021/nn400223a [DOI] [PubMed] [Google Scholar]
- 210.Tao Y., Ju E., Liu Z., Dong K., Ren J., Qu X., “Engineered, self-assembled near-infrared photothermal agents for combined tumor immunotherapy and chemo-photothermal therapy,” Biomaterials 35(24), 6646–6656 (2014). 10.1016/j.biomaterials.2014.04.073 [DOI] [PubMed] [Google Scholar]
- 211.Poudel B. K., Gupta B., Ramasamy T., Thapa R. K., Pathak S., Oh K. T., Jeong J. H., Choi H. G., Yong C. S., Kim J. O., “PEGylated thermosensitive lipid-coated hollow gold nanoshells for effective combinational chemo-photothermal therapy of pancreatic cancer,” Colloids Surf. B Biointerfaces 160, 73–83 (2017). 10.1016/j.colsurfb.2017.09.010 [DOI] [PubMed] [Google Scholar]
- 212.Kim H., Nguyen V. P., Manivasagan P., Jung M. J., Kim S. W., Oh J., Kang H. W., “Doxorubicin-fucoidan-gold nanoparticles composite for dual-chemo-photothermal treatment on eye tumors,” Oncotarget 8(69), 113719 (2017). 10.18632/oncotarget.23092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Liu L., Xie H. J., Mu L. M., Liu R., Su Z. B., Cui Y. N., Xie Y., Lu W. L., “Functional chlorin gold nanorods enable to treat breast cancer by photothermal/photodynamic therapy,” Int. J. Nanomedicine 13(13), 8119–8135 (2018). 10.2147/IJN.S186974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Tran T. H., Thapa R. K., Nguyen H. T., Pham T. T., Ramasamy T., Kim D. S., Yong C. S., Kim J. O., Choi H.-G., “Combined phototherapy in anti-cancer treatment: therapeutics design and perspectives,” J. Pharm. Investig. 46(6), 505–517 (2016). 10.1007/s40005-016-0272-x [DOI] [Google Scholar]
- 215.Cao F., Yan M., Liu Y., Liu L., Ma G., “Photothermally controlled MHC class I restricted CD8+ T-cell responses elicited by hyaluronic acid decorated gold nanoparticles as a vaccine for cancer immunotherapy,” Adv. Healthc. Mater. 7(10), e1701439 (2018). 10.1002/adhm.201701439 [DOI] [PubMed] [Google Scholar]
- 216.Zhou B., Song J., Wang M., Wang X., Wang J., Howard E. W., Zhou F., Qu J., Chen W. R., “BSA-bioinspired gold nanorods loaded with immunoadjuvant for the treatment of melanoma by combined photothermal therapy and immunotherapy,” Nanoscale 10(46), 21640–21647 (2018). 10.1039/C8NR05323E [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Chen J., Lin L., Yan N., Hu Y., Fang H., Guo Z., Sun P., Tian H., Chen X., “Macrophages loaded CpG and GNR-PEI for combination of tumor photothermal therapy and immunotherapy,” Sci. China Mater. 61(11), 1484–1494 (2018). 10.1007/s40843-018-9238-6 [DOI] [Google Scholar]
- 218.Chu D., Dong X., Zhao Q., Gu J., Wang Z., “Photosensitization priming of tumor microenvironments improves delivery of nanotherapeutics via neutrophil infiltration,” Adv. Mater. 29(27), 1701021 (2017). 10.1002/adma.201701021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Au L., Zheng D., Zhou F., Li Z. Y., Li X., Xia Y., “A quantitative study on the photothermal effect of immuno gold nanocages targeted to breast cancer cells,” ACS Nano 2(8), 1645–1652 (2008). 10.1021/nn800370j [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zhang M., Kim H. S., Jin T., Woo J., Piao Y. J., Moon W. K., “Near-infrared photothermal therapy using anti-EGFR-gold nanorod conjugates for triple negative breast cancer,” Oncotarget 8(49), 86566–86575 (2017). 10.18632/oncotarget.21243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Vijayaraghavan P., Liu C. H., Vankayala R., Chiang C. S., Hwang K. C., “Designing multi-branched gold nanoechinus for NIR light activated dual modal photodynamic and photothermal therapy in the second biological window,” Adv. Mater. 26(39), 6689–6695 (2014). 10.1002/adma.201400703 [DOI] [PubMed] [Google Scholar]
- 222.Barhoumi A., Wang W., Zurakowski D., Langer R. S., Kohane D. S., “Photothermally targeted thermosensitive polymer-masked nanoparticles,” Nano Lett. 14(7), 3697–3701 (2014). 10.1021/nl403733z [DOI] [PubMed] [Google Scholar]
- 223.Wang Z., Li S., Zhang M., Ma Y., Liu Y., Gao W., Zhang J., Gu Y., “Laser-triggered small interfering RNA releasing gold nanoshells against heat shock protein for sensitized photothermal therapy,” Adv. Sci. (Weinh.) 4(2), 1600327 (2016). 10.1002/advs.201600327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Meeker D. G., Wang T., Harrington W. N., Zharov V. P., Johnson S. A., Jenkins S. V., Oyibo S. E., Walker C. M., Mills W. B., Shirtliff M. E., Beenken K. E., Chen J., Smeltzer M. S., “Versatility of targeted antibiotic-loaded gold nanoconstructs for the treatment of biofilm-associated bacterial infections,” Int. J. Hyperthermia 34(2), 209–219 (2018). 10.1080/02656736.2017.1392047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Chen Q., Zhang L., Feng Y., Shi F., Wang Y., Wang P., Liu L., “Dual-functional peptide conjugated gold nanorods for the detection and photothermal ablation of pathogenic bacteria,” J. Mater. Chem. B Mater. Biol. Med. 6(46), 7643–7651 (2018). 10.1039/C8TB01835A [DOI] [PubMed] [Google Scholar]
- 226.Zhao Y., Guo Q., Dai X., Wei X., Yu Y., Chen X., Li C., Cao Z., Zhang X., “A biomimetic non-antibiotic approach to eradicate drug-resistant infections,” Adv. Mater. 31(7), e1806024 (2019). 10.1002/adma.201806024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Zhang M., Yilmaz T., Boztas A. O., Karakuzu O., Bang W. Y., Yegin Y., Luo Z., Lenox M., Cisneros-Zevallos L., Akbulut M., “A multifunctional nanoparticulate theranostic system with simultaneous chemotherapeutic, photothermal therapeutic, and MRI contrast capabilities,” RSC Advances 6(33), 27798–27806 (2016). 10.1039/C5RA27792B [DOI] [Google Scholar]
- 228.Li X., Takashima M., Yuba E., Harada A., Kono K., “PEGylated PAMAM dendrimer-doxorubicin conjugate-hybridized gold nanorod for combined photothermal-chemotherapy,” Biomaterials 35(24), 6576–6584 (2014). 10.1016/j.biomaterials.2014.04.043 [DOI] [PubMed] [Google Scholar]
- 229.Zhang Z., Wang J., Nie X., Wen T., Ji Y., Wu X., Zhao Y., Chen C., “Near infrared laser-induced targeted cancer therapy using thermoresponsive polymer encapsulated gold nanorods,” J. Am. Chem. Soc. 136(20), 7317–7326 (2014). 10.1021/ja412735p [DOI] [PubMed] [Google Scholar]
- 230.Deng H., Dai F., Ma G., Zhang X., “Theranostic gold nanomicelles made from biocompatible comb-like polymers for thermochemotherapy and multifunctional imaging with rapid clearance,” Adv. Mater. 27(24), 3645–3653 (2015). 10.1002/adma.201501420 [DOI] [PubMed] [Google Scholar]
- 231.Lee S.-M., Park H., Yoo K.-H., “Synergistic cancer therapeutic effects of locally delivered drug and heat using multifunctional nanoparticles,” Adv. Mater. 22(36), 4049–4053 (2010). 10.1002/adma.201001040 [DOI] [PubMed] [Google Scholar]
- 232.Chen R., Zheng X., Qian H., Wang X., Wang J., Jiang X., “Combined near-IR photothermal therapy and chemotherapy using gold-nanorod/chitosan hybrid nanospheres to enhance the antitumor effect,” Biomater. Sci. 1(3), 285–293 (2013). 10.1039/C2BM00138A [DOI] [PubMed] [Google Scholar]
- 233.Huang C.-C., Liu T.-M., “Controlled Au-polymer nanostructures for multiphoton imaging, prodrug delivery, and chemo-photothermal therapy platforms,” ACS Appl. Mater. Interfaces 7(45), 25259–25269 (2015). 10.1021/acsami.5b07110 [DOI] [PubMed] [Google Scholar]
- 234.Zhang Z., Wang L., Wang J., Jiang X., Li X., Hu Z., Ji Y., Wu X., Chen C., “Mesoporous silica-coated gold nanorods as a light-mediated multifunctional theranostic platform for cancer treatment,” Adv. Mater. 24(11), 1418–1423 (2012). 10.1002/adma.201104714 [DOI] [PubMed] [Google Scholar]
- 235.Li N., Cheng J., Zhang Y., Wang J., Huang G., Zhu J., He D., “A chemophotothermal and targeting multifunctional nanoprobe with a tumor-diagnosing ability,” Nano Res. 11(8), 4333–4347 (2018). 10.1007/s12274-018-2021-0 [DOI] [Google Scholar]
- 236.Huang W. C., Tsai P.-J., Chen Y.-C., “Multifunctional Fe3O4@Au nanoeggs as photothermal agents for selective killing of nosocomial and antibiotic-resistant bacteria,” Small 5(1), 51–56 (2009). 10.1002/smll.200801042 [DOI] [PubMed] [Google Scholar]
- 237.Ma M., Chen H., Chen Y., Wang X., Chen F., Cui X., Shi J., “Au capped magnetic core/mesoporous silica shell nanoparticles for combined photothermo-/chemo-therapy and multimodal imaging,” Biomaterials 33(3), 989–998 (2012). 10.1016/j.biomaterials.2011.10.017 [DOI] [PubMed] [Google Scholar]
- 238.Lee J., Yang J., Ko H., Oh S. J., Kang J., Son J.-H., Lee K., Lee S.-W., Yoon H.-G., Suh J.-S., Huh Y.-M., Haam S., “Multifunctional magnetic gold nanocomposites: human epithelial cancer detection via magnetic resonance imaging and localized synchronous therapy,” Adv. Funct. Mater. 18(2), 258–264 (2008). 10.1002/adfm.200700482 [DOI] [Google Scholar]
- 239.Cheng F.-Y., Su C.-H., Wu P.-C., Yeh C.-S., “Multifunctional polymeric nanoparticles for combined chemotherapeutic and near-infrared photothermal cancer therapy in vitro and in vivo,” Chem. Commun. (Camb.) 46(18), 3167–3169 (2010). 10.1039/b919172k [DOI] [PubMed] [Google Scholar]
- 240.Baek S., Singh R. K., Kim T.-H., Seo J.-W., Shin U. S., Chrzanowski W., Kim H.-W., “Triple hit with drug carriers: pH- and temperature-responsive theranostics for multimodal chemo- and photothermal-therapy and diagnostic applications,” ACS Appl. Mater. Interfaces 8(14), 8967–8979 (2016). 10.1021/acsami.6b00963 [DOI] [PubMed] [Google Scholar]
- 241.Chen H., Liu F., Lei Z., Ma L., Wang Z., “Fe2O3@Au core@shell nanoparticle–graphene nanocomposites as theranostic agents for bioimaging and chemo-photothermal synergistic therapy,” RSC Advances 5(103), 84980–84987 (2015). 10.1039/C5RA17143A [DOI] [Google Scholar]
- 242.Heo D. N., Yang D. H., Moon H.-J., Lee J. B., Bae M. S., Lee S. C., Lee W. J., Sun I.-C., Kwon I. K., “Gold nanoparticles surface-functionalized with paclitaxel drug and biotin receptor as theranostic agents for cancer therapy,” Biomaterials 33(3), 856–866 (2012). 10.1016/j.biomaterials.2011.09.064 [DOI] [PubMed] [Google Scholar]
- 243.Chen W.-H., Yang C.-X., Qiu W.-X., Luo G.-F., Jia H.-Z., Lei Q., Wang X.-Y., Liu G., Zhuo R.-X., Zhang X.-Z., “Multifunctional theranostic nanoplatform for cancer combined therapy based on gold nanorods,” Adv. Healthc. Mater. 4(15), 2247–2259 (2015). 10.1002/adhm.201500453 [DOI] [PubMed] [Google Scholar]
- 244.Chen H., Zhang X., Dai S., Ma Y., Cui S., Achilefu S., Gu Y., “Multifunctional gold nanostar conjugates for tumor imaging and combined photothermal and chemo-therapy,” Theranostics 3(9), 633–649 (2013). 10.7150/thno.6630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Su G., Miao D., Yu Y., Zhou M., Jiao P., Cao X., Yan B., Zhu H., “Mesoporous silica-coated gold nanostars with drug payload for combined chemo-photothermal cancer therapy,” J. Drug Target. 27(2), 201–210 (2019). 10.1080/1061186X.2018.1499746 [DOI] [PubMed] [Google Scholar]
- 246.Wang Y., Chen L., Liu P., “Biocompatible triplex Ag@SiO2@mTiO2 core-shell nanoparticles for simultaneous fluorescence-SERS bimodal imaging and drug delivery,” Chemistry 18(19), 5935–5943 (2012). 10.1002/chem.201103571 [DOI] [PubMed] [Google Scholar]
- 247.Zhang W., Wang Y., Sun X., Wang W., Chen L., “Mesoporous titania based yolk-shell nanoparticles as multifunctional theranostic platforms for SERS imaging and chemo-photothermal treatment,” Nanoscale 6(23), 14514–14522 (2014). 10.1039/C4NR04864D [DOI] [PubMed] [Google Scholar]
- 248.Jiang Z., Dong B., Chen B., Wang J., Xu L., Zhang S., Song H., “Multifunctional Au@mSiO2/rhodamine B isothiocyanate nanocomposites: cell imaging, photocontrolled drug release, and photothermal therapy for cancer cells,” Small 9(4), 604–612 (2013). 10.1002/smll.201201558 [DOI] [PubMed] [Google Scholar]
- 249.Hu F., Zhang Y., Chen G., Li C., Wang Q., “Double-walled Au nanocage/SiO2 nanorattles: integrating SERS imaging, drug delivery and photothermal therapy,” Small 11(8), 985–993 (2015). 10.1002/smll.201401360 [DOI] [PubMed] [Google Scholar]
- 250.Topete A., Alatorre-Meda M., Iglesias P., Villar-Alvarez E. M., Barbosa S., Costoya J. A., Taboada P., Mosquera V., “Fluorescent drug-loaded, polymeric-based, branched gold nanoshells for localized multimodal therapy and imaging of tumoral cells,” ACS Nano 8(3), 2725–2738 (2014). 10.1021/nn406425h [DOI] [PubMed] [Google Scholar]
- 251.Hao Y., Zhang B., Zheng C., Ji R., Ren X., Guo F., Sun S., Shi J., Zhang H., Zhang Z., Wang L., Zhang Y., “The tumor-targeting core-shell structured DTX-loaded PLGA@Au nanoparticles for chemo-photothermal therapy and X-ray imaging,” J. Control. Release 220(Pt A), 545–555 (2015). 10.1016/j.jconrel.2015.11.016 [DOI] [PubMed] [Google Scholar]
- 252.Yuan Y., Zhang Y., Liu B., Wu H., Kang Y., Li M., Zeng X., He N., Zhang G., “The effects of multifunctional MiR-122-loaded graphene-gold composites on drug-resistant liver cancer,” J. Nanobiotechnology 13(1), 12 (2015). 10.1186/s12951-015-0070-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Marrache S., Choi J. H., Tundup S., Zaver D., Harn D. A., Dhar S., “Immune stimulating photoactive hybrid nanoparticles for metastatic breast cancer,” Integr. Biol. 5(1), 215–223 (2013). 10.1039/c2ib20125a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Hembury M., Chiappini C., Bertazzo S., Kalber T. L., Drisko G. L., Ogunlade O., Walker-Samuel S., Krishna K. S., Jumeaux C., Beard P., Kumar C. S., Porter A. E., Lythgoe M. F., Boissière C., Sanchez C., Stevens M. M., “Gold-silica quantum rattles for multimodal imaging and therapy,” Proc. Natl. Acad. Sci. U.S.A. 112(7), 1959–1964 (2015). 10.1073/pnas.1419622112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Yi Y., Wang H., Wang X., Liu Q., Ye M., Tan W., “A smart, photocontrollable drug release nanosystem for multifunctional synergistic cancer therapy,” ACS Appl. Mater. Interfaces 9(7), 5847–5854 (2017). 10.1021/acsami.6b15414 [DOI] [PubMed] [Google Scholar]
- 256.Ramasamy T., Ruttala H. B., Sundaramoorthy P., Poudel B. K., Youn Y. S., Ku S. K., Choi H.-G., Yong C. S., Kim J. O., “Multimodal selenium nanoshell-capped Au@mSiO2 nanoplatform for NIR-responsive chemo-photothermal therapy against metastatic breast cancer,” NPG Asia Mater. 10(4), 197–216 (2018). 10.1038/s41427-018-0034-5 [DOI] [Google Scholar]
- 257.Xu L., Liu J., Xi J., Li Q., Chang B., Duan X., Wang G., Wang S., Wang Z., Wang L., “Synergized multimodal therapy for safe and effective reversal of cancer multidrug resistance based on low-level photothermal and photodynamic effects,” Small 14(31), e1800785 (2018). 10.1002/smll.201800785 [DOI] [PubMed] [Google Scholar]
- 258.Li Y., He D., Tu J., Wang R., Zu C., Chen Y., Yang W., Shi D., Webster T. J., Shen Y., “The comparative effect of wrapping solid gold nanoparticles and hollow gold nanoparticles with doxorubicin-loaded thermosensitive liposomes for cancer thermo-chemotherapy,” Nanoscale 10(18), 8628–8641 (2018). 10.1039/C7NR09083H [DOI] [PubMed] [Google Scholar]
- 259.Setyawati M. I., Tay C. Y., Chia S. L., Goh S. L., Fang W., Neo M. J., Chong H. C., Tan S. M., Loo S. C., Ng K. W., Xie J. P., Ong C. N., Tan N. S., Leong D. T., “Titanium dioxide nanomaterials cause endothelial cell leakiness by disrupting the homophilic interaction of VE-cadherin,” Nat. Commun. 4(1), 1673 (2013). 10.1038/ncomms2655 [DOI] [PubMed] [Google Scholar]
- 260.Setyawati M. I., Tay C. Y., Bay B. H., Leong D. T., “Gold nanoparticles induced endothelial leakiness depends on particle size and endothelial cell origin,” ACS Nano 11(5), 5020–5030 (2017). 10.1021/acsnano.7b01744 [DOI] [PubMed] [Google Scholar]
- 261.Tay C. Y., Setyawati M. I., Leong D. T., “Nanoparticle density: a critical biophysical regulator of endothelial permeability,” ACS Nano 11(3), 2764–2772 (2017). 10.1021/acsnano.6b07806 [DOI] [PubMed] [Google Scholar]
- 262.Peng F., Setyawati M. I., Tee J. K., Ding X., Wang J., Nga M. E., Ho H. K., Leong D. T., “Nanoparticles promote in vivo breast cancer cell intravasation and extravasation by inducing endothelial leakiness,” Nat. Nanotechnol. 14(3), 279–286 (2019). 10.1038/s41565-018-0356-z [DOI] [PubMed] [Google Scholar]
- 263.Khlebtsov B. N., Bratashov D. N., Byzova N. A., Dzantiev B. B., Khlebtsov N. G., “SERS-based lateral flow immunoassay of troponin I using gap-enhanced Raman tags,” Nano Res. 12(2), 413–420 (2019). 10.1007/s12274-018-2232-4 [DOI] [Google Scholar]
- 264.Lin K.-Q., Yi J., Zhong J.-H., Hu S., Liu B.-J., Liu J.-Y., Zong C., Lei Z.-C., Wang X., Aizpurua J., Esteban R., Ren B., “Plasmonic photoluminescence for recovering native chemical information from surface-enhanced Raman scattering,” Nat. Commun. 8(1), 14891 (2017). 10.1038/ncomms14891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Huang X., Peng X., Wang Y., Wang Y., Shin D. M., El-Sayed M. A., Nie S., “A reexamination of active and passive tumor targeting by using rod-shaped gold nanocrystals and covalently conjugated peptide ligands,” ACS Nano 4(10), 5887–5896 (2010). 10.1021/nn102055s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Jiang W., Kim B. Y. S., Rutka J. T., Chan W. C. W., “Nanoparticle-mediated cellular response is size-dependent,” Nat. Nanotechnol. 3(3), 145–150 (2008). 10.1038/nnano.2008.30 [DOI] [PubMed] [Google Scholar]
- 267.Dykman L. A., Khlebtsov N. G., “Uptake of engineered gold nanoparticles into mammalian cells,” Chem. Rev. 114(2), 1258–1288 (2014). 10.1021/cr300441a [DOI] [PubMed] [Google Scholar]
- 268.Tsao S. C.-H., Wang J., Wang Y., Behren A., Cebon J., Trau M., “Characterising the phenotypic evolution of circulating tumour cells during treatment,” Nat. Commun. 9(1), 1482 (2018). 10.1038/s41467-018-03725-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Melero I., Gaudernack G., Gerritsen W., Huber C., Parmiani G., Scholl S., Thatcher N., Wagstaff J., Zielinski C., Faulkner I., Mellstedt H., “Therapeutic vaccines for cancer: an overview of clinical trials,” Nat. Rev. Clin. Oncol. 11(9), 509–524 (2014). 10.1038/nrclinonc.2014.111 [DOI] [PubMed] [Google Scholar]