Abstract
Background:
In recent years, most U.S. states have passed autism mandates requiring private insurers to cover autism spectrum disorders (ASD). Little is known about the post-mandate changes in healthcare expenditures.
Method:
This study utilized 2006–2012 de-identified insurance claims data from the largest insurer in Pennsylvania (PA), where the mandate went into effect in 2009. Healthcare expenditures were defined as the amount the insurer paid for healthcare services and were adjusted to 2012 price level. A mixed model approach was used to analyze the expenditures.
Results:
A total of 9,471 children with ASD were included in the study. Although the pre-mandate total expenditures per child with ASD were similar, the post-mandate expenditures significantly increased for groups subject to the autism mandate (87% increase from $7,754 in 2008 to $14,486 in 2010) compared to the exempt groups (27% increase from $7,238 to $9,171). By insurance type, the change from 2008 to 2010 in ASD-related expenditures per child with ASD was $8,439 for fully insured large employer sponsored plans and $43 for the Children’s Health Insurance Program (CHIP), both subject to the PA mandate; and $2,631 for the self-insured, $980 for small-employers, and $−92 for individual plans, all of which are exempt from the mandate. These increases were due to outpatient services but not inpatient or drug costs.
Conclusions:
Healthcare expenditures increased significantly following the PA autism mandate. Nonexempt, large employer groups had the largest increase in spending. Some exempt, self-insured companies may have voluntarily covered ASD services, leading to a moderate increase.
Keywords: Autism Mandate, Healthcare Expenditures, Cost, Autism Spectrum Disorder, Private Insurance
1. Introduction
Autism spectrum disorders (ASD) affect 1 in every 59 children in the United States (Baio et al., 2018). Early treatment can greatly enhance patients’ functional independence and improve outcomes (Dawson & Burner, 2011; Rogers & Vismara, 2008; Warren et al., 2011). However, treating ASDs can be expensive, with the estimated annual healthcare expenditures per child being $5979-$22,772, and lifetime direct medical costs of $306,000 (Ganz, 2007; Liptak, Stuart, & Auinger, 2006; Wang & Leslie, 2010). Until recently, ASD services in the US had traditionally been covered by Medicaid and not private insurances (Kelly, 2015; Peele, Lave, & Kelleher, 2002). While Medicaid may provide autism coverage for children with ASD through Home and Community Based Services waiver programs under section 1915(c) of the Social Security Act (Merryman, Miller, Shockley, Eskow, & Chasson, 2015; Velott et al., 2015; Wang & Leslie, 2010), the waiver programs usually have a low quota resulting in many children with ASD being placed on a waitlist, unable to receive the ASD services they need (Eskow, Pineles, & Summers, 2011).
To improve access to autism care, more and more states have passed autism insurance mandates that require private insurers to provide autism coverage (Autism Speaks, 2018; Kelly, 2015). As of 2017, 46 states plus the District of Columbia have enacted an autism mandate (Autism Speaks, 2018). Under autism mandates, private insurers are required to provide coverage for the screening, diagnosis, and treatment of ASD. The treatment of ASD consists of behavioral health treatment, psychiatric care, psychological care and pharmacy care (Autism Speaks, 2018).
For those states with a mandate, all had the mandate after 2007 except for Indiana, and most states enacted the mandate after 2010 (Autism Speaks, 2018). The autism mandate is a new state insurance law, and studies on its actual impact are greatly needed. Only a few studies exist in the literature that use real-world post-mandate data to explore various mandate effects. Using Medicaid data, Stein et al. found that the autism mandate may decrease the number of families seeking Medicaid-funded services (Stein, Sorbero, Goswami, Schuster, & Leslie, 2012). Using survey data, Chatterji et al. discovered that autism mandates may have some effect on out-of-pocket costs (Chatterji, Decker, & Markowitz, 2015). Using interview data, Baller et al. reported increased access to autism services after the enactment of the autism mandate (Baller et al., 2015).
A major issue that is debated during the process of passing an autism mandate is its associated costs. There are many reports and published studies on the projected, rather than the actual, costs of implementing an autism mandate (Bouder, Spielman, & Mandell, 2009; Lambright, 2010, 2012; Pennsylvania Health Care Cost Containment Council, 2008). However, studies using actual post-mandate private insurance claims data to estimate the actual, rather than the projected costs are rare and have only recently been initiated. Using actual post-mandate insurance claims data in Kansas, a study showed that the actual costs increased substantially after the autism mandate (Barry et al., 2017). Based on a database from three private health insurers, research has shown that mandates increased spending in general, and the increase was higher for children with greater service needs and for states without an age cap (Barry et al., 2017; Candon et al., 2018; Kennedy-Hendricks et al., 2018). Given that the autism mandate is such an important insurance law regarding autism with far-reaching impact, more studies are needed to evaluate the actual effects. Our study used private insurance data from the largest private health insurer in Pennsylvania, Highmark Inc., and focused on the effect of increased expenditures resulting from the autism mandate.
When it comes to the cost implication of the autism mandate, it is important to know that the autism mandate does not apply to all privately insured plans in a given state. The cost implication is different between plans that are subject to the mandate and those that are exempt from the mandate. For example, it does not apply to self-insured (also called self-funded) plans, which provide insurance to employees through paying their medical bills with their own pooled funds and assuming the associated financial risks. Self-insured plans are exempt from state mandates because they are regulated by the federal Employee Retirement Income Security Act (ERISA) (Polzer & Butler, 1997). ERISA is a federal law that sets minimum standards which private companies must follow in designing their pension plans and insurance plans. About 60% of workers who are privately insured are self-insured (Kaiser Family Foundation [KFF], 2017). In addition to the exemption of self-insured groups in every state, small employers and individual plans are exempt from the autism mandate in a number of states (Autism Speaks, 2018). For example, in Pennsylvania, individual plans and small employer group insurance plans with no more than 50 employees are exempt from the autism mandate (Pennsylvania Department of Human Services [DHS], 2016). Those who are exempt from the mandate may not benefit in the same way as those who are subject to the mandate due to their exemption status. Using data from the National Survey of Children with Special Health Care Needs (NS-CSHCN), Chatterji et al. found no association between the autism mandate and better access to care in general, but some evidence of better access in states with a higher percentage of privately insured children who that are subject to the mandate (Chatterji et al., 2015).
Our data contain information on the type of insurance plans and their corresponding exemption status, offering a unique opportunity to explore how the autism mandate affects access to services and costs by insurance type. To the best of our knowledge, our study is the only one that differentiate large employer group insurance vs. small employer group insurance, thanks to the unique data information we have. The ability to differentiate between these two group insurance types provides a more accurate picture of the change in expenditures since the mandate affects each group differently. In addition, our data also contained insurance claims of PA Children’s Health Insurance Program (CHIP), for which Highmark administered its insurance claims data. The government-funded CHIP programs provide insurance to children up to age 19 in families who can’t afford private insurance but have an income too high to qualify for Medicaid. We included the CHIP data in our study, for our unique data can help provide valuable information of the mandate effect regarding this specific group which has not been studied in the literature.
In this study, we will focus on investigating the changes in healthcare expenditures, stratified by exemption status and insurance type. We hypothesize that post-mandate expenditures will rise substantially for the nonexempt groups, while the exempt groups may not see as much of an increase depending on whether they voluntarily provide ASD coverage.
2. Methods
De-identified insurance claims data from 2006–2012 for children with ASD were obtained from Highmark Inc., the largest private health insurer in PA. The PA autism mandate requires coverage for the diagnosis and treatment of ASD in children under 21 years of age who are in employer group insurance plans issued to large employers with at least 51 employees or insured by the CHIP. Examples of the treatment services covered include Applied Behavior Analysis (ABA) and prescription drugs among others. Since the PA mandate applies to both employers with at least 51 employees and to the CHIP, the nonexempt group in this study includes large employer insurance plans and the CHIP plan. Small employer group plans, individual plans and self-insured plans are exempt from the PA autism mandate, and are therefore included in the exempt group.
A child was considered to have ASD in a given year if he/she had at least two insurance claims with an ICD-9 diagnosis code of 299.xx in that year (Burke et al., 2014). To fully capture the yearly costs of autism care, a continuous enrollment of 12 months in a given year was required. Another inclusion criterion was that the child was under 21 years old in a given year, since the PA autism mandate is applicable only for children under 21 years old (DHS, 2016).
Healthcare expenditures were measured as the amount the insurance company paid. In this paper, expenditures and costs were used interchangeably as in Shimabukuro et al (Shimabukuro, Grosse, & Rice, 2008), for the term cost often refers to expenditures by both the general public and in the literature. The costs were adjusted to the 2012 price level using the medical care component of the Consumer Price Index. Total health care expenditures were defined as the amount the insurance company paid for drugs, and outpatient and inpatient care irrespective of the diagnosis code as defined in Shimabukuro et al (Shimabukuro et al., 2008). ASD-related costs were defined as healthcare expenditures from inpatient and outpatient care with a primary diagnosis code for ASD. For example, if a child with ASD was admitted for a sports injury with concussion as the primary diagnosis, the associated cost for that admission would not be included as an ASD-related cost, even if ASD diagnosis could be a secondary diagnosis.
Descriptive statistics for patient characteristics and expenditures were derived. County-level variables for the percentage of the white population and median income were used as a proxy for individual-level data. County level data were obtained from the Area Health Resource File (AHRF) available from the Health Resources and Services Administration (AHRF, 2014). Urban/rural status was also defined according to the county of residence.
A mixed effects model was used to estimate the effect of the autism mandate on total healthcare expenditures, with the variable county of residence as the random effect. We treated the county effect as random since 1) we were not particularly interested in estimating the fixed effect of a given county, and 2) there would be too many counties to estimate. Fixed effects variables included demographic variables such as age and gender. The mandate has a differential effect on exempt groups versus nonexempt groups. Therefore, we created a categorical mandate effect variable to capture the differential effect, which included three levels: “1: before mandate”, “2: post mandate and nonexempt”, and “3: post mandate but exempt”. Given the definition of the categorical mandate effect, estimates at two levels need to be obtained to assess the mandate effect: one for the post-mandate exempt groups and one for the post-mandate nonexempt groups, compared to the baseline pre-mandate period. The period from 2006–2009 was considered as the pre-mandate period, and all cases in 2006–2009 were considered “before mandate” for the mandate effect variable. The period from 2010–2012 was classified as the post-mandate period, and during those years nonexempt children in large group insurance plans and the CHIP were assigned “post mandate and nonexempt”, whereas children in small-employer-sponsored plans, individual plans or self-insured plans during those years were assigned “post mandate but exempt” for the mandate effect variable.
The unadjusted mean health expenditures were defined as the average total expenditures among all of the children with the same level of a given categorical variable. The adjusted means were derived as the average of model-predicted healthcare expenditures based on the original values of the covariates.
The Institutional Review Board (IRB) at the Penn State College of Medicine approved this study.
3. Results
A total of 9,471 unique children with ASD were included during the study period. Table 1 presents patient characteristics by year. The mean age increased by 1.3 years over the study period. Every year, about 80% of patients were males, consistent with the 4:1 male-to-female ratio for ASD prevalence rate (Whiteley, Todd, Carr, & Shattock, 2010). Note that the unit of study is person-year, so the same person could be included in multiple years of the study as long as he/she satisfied the inclusion criteria.
Table 1:
Patient characteristics by year
| Year | N | Mean age±sd | Male (%) | white population (%)±sd | Mean income±sd | urban (%) |
|---|---|---|---|---|---|---|
| 2006 | 1466 | 9.7±4.6 | 81.6 | 88.6±6.9 | $43704±6075 | 81.1 |
| 2007 | 1869 | 9.9±4.4 | 81.0 | 89.0±6.8 | $45886±6635 | 81.5 |
| 2008 | 2443 | 10.0±4.5 | 82.0 | 88.9±6.8 | $48250±6891 | 83.3 |
| 2009 | 2821 | 10.1±4.5 | 80.9 | 88.6±7.0 | $46792±6585 | 84.4 |
| 2010 | 3152 | 10.5±4.4 | 80.8 | 88.5±7.1 | $46919±6238 | 85.2 |
| 2011 | 4212 | 10.8±4.5 | 81.0 | 88.2±8.3 | $48530±7157 | 85.0 |
| 2012 | 4395 | 11.0±4.5 | 80.1 | 88.2±8.5 | $49830±7251 | 84.9 |
Table 2 shows average total expenditures and average ASD-related expenditures per child with ASD for non-exempt and exempt groups respectively, with the nonexempt groups further divided into large employer group plans and CHIP plan and the exempt groups divided into self-insured, small employer and individual plans. The three values separated by commas in a single cell in Table 2 are as follows: the first value is the number of children in the given group, the second value is the total expenditures per child with ASD, and the third value is the ASD-related costs per child with ASD. As indicated in table 2, the largest sample size in our study was from self-insured, followed by large employers and small employers. The sample sizes for individual plans and CHIP were relatively small, causing more cost variability across years among those two groups.
Table 2:
Total expenditures and ASD-related expenditures per child with ASD
| Non-exempt groups | Large employers | CHIP | Exempt groups | Self-insured | Individual plans | Small employers | |
|---|---|---|---|---|---|---|---|
| 2006 | 455, $6209, $642 |
439, $6206, $650 |
16, $6274, $430 |
1011, $6424, $722 |
739, $6402, $774 |
16, $4504, $230 |
256, $6607, $602 |
| 2007 | 616, $7424, $795 |
588, $7545, $807 |
28, $4894, $531 |
1253, $6945, $684 |
873, $6920, $721 |
17, $4306, $343 |
363, $7129, $612 |
| 2008 | 832, $7754, $767 |
783, $7857, $778 |
49, $6115, $597 |
1611, $7238, $695 |
1179, $6942, $727 |
21, $3342, $482 |
411, $8283, $612 |
| 2009 | 911, $8171, $2035 |
865, $8337, $2099 |
46, $5063, $836 |
1910, $7117, $1007 |
1408, $7276, $1040 |
35, $4866, $305 |
467, $6807, $960 |
| 2010 | 928, $14486, $8801 |
883, $15001, $9217 |
45, $4365, $640 |
2224, $9171, $2942 |
1729, $9573, $3358 |
41, $4970, $390 |
454, $8018, $1592 |
| 2011 | 1387, $12673, $6461 |
1322, $13029, $6740 |
65, $5441, $777 |
2825, $8790, $2986 |
2255, $8963, $3286 |
54, $9472, $506 |
516, $7966, $1932 |
| 2012 | 1500, $11665, $6289 |
1441, $11837, $6523 |
59, $7480, $576 |
2895, $9014, $2835 |
2383, $9471, $3110 |
53, $6050, $545 |
459, $6984, $1674 |
Among the nonexempt groups, the total expenditure per child with ASD increased slightly from $7,754 in 2008 to $8,171 in 2009 right after the mandate went into effect in July 2009, and increased sharply by more than $5000 to $14,486 in 2010, an increase of 87% in less than two years after the mandate. The healthcare expenditure per child with ASD in the nonexempt group then stayed high after 2010, being $12,673 in 2011 and $11,665 in 2012 respectively.
Among the exempt groups, the pre-mandate total costs in 2006–2008 were close to those of the nonexempt groups. However, the post-mandate total cost increased less for the exempt groups, rising from $7,238 in 2008 by 27% to $9,171 in 2010, resulting in more than $5000 cost difference between the exempt and non-exempt groups in 2010.
By type of insurance, Table 2 presents five specific insurance types. First, among those employment-based plans, the increase of the total healthcare expenditure from 2008 to 2010 was biggest in large employers (an increase of 87%), followed by self-insured (38%). Small employer groups had little increase in total healthcare expenditure from 2008 to 2010. For the year 2011–2012, the total costs remained much higher than pre-mandate period for large employer groups and self-insured, though slightly lower than 2010 due to lower average expenditures for newly treated children with less severe symptoms as explained in the discussion part. However, for small employers, the average expenditure in 2012 were still lower than those in the pre-mandate year 2008. Next, for CHIP and individual plans, there was no obvious pattern for cost change after the mandate, and their total costs fluctuate slightly and randomly during 2006–2012 due to their small sample sizes.
Regarding ASD-related costs as a percentage of total health care costs, they accounted for about one tenth of the total costs in 2006–2008 among nonexempt groups, and then rose to more than one third of the total costs in 2009. In the years 2010–2012, the ASD-related costs accounted for about half of the total costs for nonexempt groups. For the exempt groups, the pre-mandate ASD-related costs similarly accounted for about one tenth of the total costs in 2006–2008. However, the ASD-related costs among the exempt groups increased less after the mandate and counted for about one third of the total costs in 2010–2012.
By insurance type, the change from 2008 to 2010 in ASD-related expenditures per child with ASD was $8,439 for large employer sponsored plans, $43 for the Children’s Health Insurance Program (CHIP), both of which are subject to the PA mandate, and $2,631 for the self-insured, $980 for small-employers, and $−92 for individual plans, which are all exempt from the mandate.
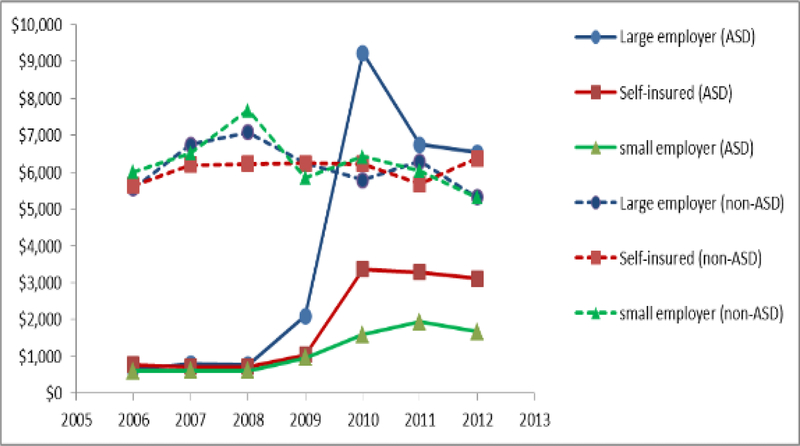
We in particular compared ASD costs vs. non-ASD costs among the three employment-based insurance plans as presented in Figure 1. The non-ASD costs (dashed lines) for large employers, small employers and the self-insured groups were similar and relatively constant throughout the years. In comparison, the ASD-related costs (solid lines) were similar across the three insurance types before the mandate, but varied greatly after the mandate, with the large employer groups having much higher ASD-related costs.
Figure 1:
ASD cost vs. non- ASD cost by employment-based insurance type
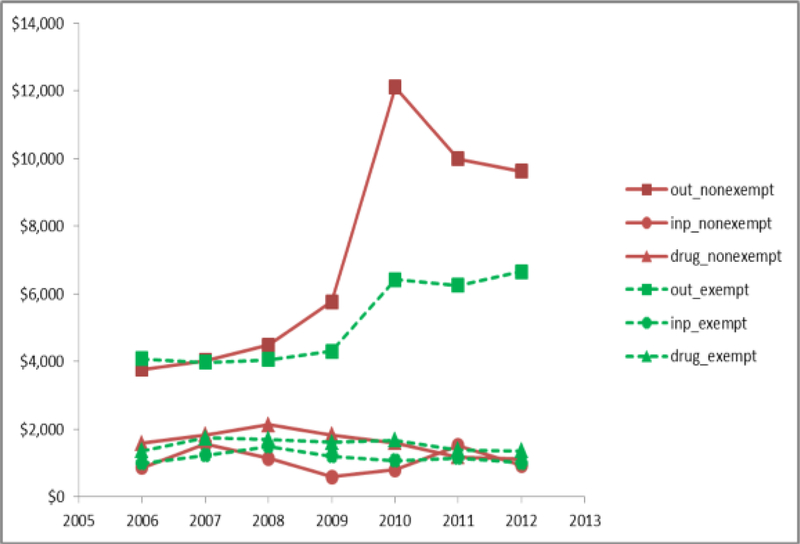
In Figure 2, total costs per child with ASD were divided into inpatient costs, outpatient costs and drug costs for nonexempt groups (solid lines) and exempt groups (dashed lines) respectively. For both groups, outpatient costs (the upper two lines in figure 2) were much higher than inpatient and drug costs (the lowest four lines in figure 2). Inpatient and drug costs were relatively stable over the study period, and were similar between exempt and nonexempt groups. However, the outpatient costs increased sharply after the autism mandate by $7612 for nonexempt groups and $2366 for exempt groups from 2008 to 2010.
Figure 2:
Outpatient, inpatient and drug costs for nonexempt and extempt groups
Table 3 lists the unadjusted and adjusted means of total expenditures at given levels of the categorical variables included in the mixed model. Regarding unadjusted raw means, the largest difference within the same variable was seen in “mandate”. For instance, the mean total expenditures per child with ASD in the pre-mandate period were $7,180, and were $12,718 in the post-mandate period for nonexempt groups, and $8,978 in the post-mandate period for exempt groups (P<0.0001). In the adjusted analysis, all previously significant variables in the unadjusted analysis remained significant, including gender (P=0.01), mandate (P<0.0001) and age (P<0.0001). Urban/rural status was not significant in either unadjusted analysis or adjusted analysis.
Table 3:
Mixed model estimation for total healthcare expenditures
| Unadjusted means | Adjusted means | |
|---|---|---|
| Age | P=0.0001 | P<0.0001 |
| <3 years | $5920 | $5778 |
| 3–5 years | $10067 | $9694 |
| 6–10 years | $8608 | $8001 |
| 11–14 years | $8460 | $7771 |
| 15–18 years | $9606 | $8931 |
| 18–20 years | $9301 | $8507 |
| Gender | P=0.02* | P=0.01* |
| female | $9718 | $9030 |
| male | $8732 | $8137 |
| Mandate | P<0.0001* | P<0.0001 * |
| Pre-mandate | $7180 | $6438 |
| Post-mandate nonexempt | $8978 | $8394 |
| Post-mandate exempt | $12718 | $12340 |
| Urban/Rural | P=0.97 | P=0.34 |
| urban | $8923 | $8212 |
| rural | $8904 | $8812 |
4. Discussion and Implications
The autism mandate has greatly increased healthcare expenditures for privately insured children with ASD in Pennsylvania. The pre-mandate total healthcare expenditures for a child with ASD in our study were $6,209 for the nonexempt groups and $6,424 for the exempt groups in 2006, similar to the estimated total expenditure of $6,185 (in 2012 price level) in 2003 using another private insurance database (Wang, Mandell, Lawer, Cidav, & Leslie, 2013). The post-mandate total expenditures in Pennsylvania soared for the non-exempt groups to $11665 in 2012 with ASD-related costs totaling $6289, which was much higher than the estimated $2,904 in autism-related treatment costs in 2012 under the Missouri autism mandate (Missouri Department of Insurance, Financial Institutions and Professional Registration [DIFP], 2013). Since the study methods were not adequately explained in that report, we could not determine whether or not it was partly because of their measurement methods that led to lower cost estimates compared to Pennsylvania post-mandate expenditures.
Many privately insured children with ASD in Pennsylvania are exempt from the state autism mandate, leading to considerable barriers when trying to access autism care. Compared to large group employers, small employers are often more vulnerable to the cost of health insurance and are sometimes exempt from various state-mandated health benefits (Jensen & Morrisey, 1999). The Pennsylvania autism mandate exempts small employers for cost concerns similar to the autism mandates in a number of other states such as Florida and Minnesota (Autism Speaks, 2018). Given that small businesses employ about half of the workforce (U.S. Small Business Administration, 2016), the exclusion of small employers from the autism mandate can hinder access to autism care for many children with ASD. As shown in this study, the ASD-related expenditures per child with ASD for those in small employer-sponsored insurance groups were only about one quarter of those in fully insured large employer-sponsored insurance groups after the mandate. Our unique dataset gives us the ability to differentiate small employers from large employers to shed light on the barriers faced by children when seeking ASD care in small employer-sponsored plans. Existing studies do not segregate small employers due to the lack of data required, but rather group them into nonexempt (eligible) groups since they are fully insured (Barry et al., 2017; Candon et al., 2018; Kennedy-Hendricks et al., 2018). In states where the autism mandate exempts small employers, children with small employer-sponsored plans are actually not eligible for autism services and probably have much lower ASD-related expenditures as demonstrated in our study. The inability to differentiate small employers may result in a lower estimate of the average post-mandate expenditure for the truly nonexempt insurance plans.
Among the exempt groups, the largest post-mandate cost increase was seen in the self-insured group. After the mandate went into effect, ASD-related expenditures for the self-insured rose from about $700 to approximately $3000. This large increase was due to some self-insured employers voluntarily providing ASD coverage (DIFP, 2013) in order to have competitive employee benefits. Although the autism mandate does not apply to self-insured employers, many of them acted instantly to offer ASD services, resulting in an immediate increase in expenditure following the mandate as shown in Figure 1. In this sense, the autism mandate indirectly impacted the self-insured, making them less than ideal candidates to serve as a study control group which should be free from the mandate effect. About 60% of the privately insured are in self-insured plans (KFF, 2017), which means there is still a large proportion of children with ASD that may not benefit from the autism mandate unless those self-insured employers voluntarily cover ASD.
A couple of years after the mandate, decreases in the average ASD-related costs and average total expenditures were seen in 2011–2012 when compared to 2010. These decreases may have been a result of newly diagnosis children having less severe ASD on average than those children diagnosed before the mandate due to improved access to diagnostic tools and awareness of the disease. This led to a greater proportion of children with less severe ASD in a given year, driving down the average costs per child. Using a sensitivity analysis, we followed a cohort of children who were diagnosed with ASD before the mandate in 2008 and who were in nonexempt groups. The average total expenditures for that subgroup from 2008 – 2012 were $7754, $9319, $17626, $18969, $17471 respectively, with no obvious decrease after 2010. In contrast, for the cohort of those newly diagnosed after 2010 and who were in nonexempt groups, the average expenditures were much lower totaling approximately $10,000 a year from 2010–2012.
Despite a substantial cost increase after the mandate, the ASD-related expenditure per child with ASD was far below the maximum allowable benefits for autism treatment specified in the autism mandate. The actual ASD-related expenditures per child for the nonexempt groups were $6,289 in 2012, only 17% of the maximum allowable cost of $36,000 under the PA autism mandate. In studies projecting the impact of the mandate on insurance premiums before the mandate was passed, the lower bound of the projected spending was often a much larger value than the actual $6,289 in 2012. For example, the lower bound of the projected spending was set at $10,000 by Bouder et al. in their cost projection (Bouder et al., 2009).
Based on our study, the post-mandate healthcare expenditure for children with ASD in private insurance was still much lower than those in Medicaid. Studies found that Medicaid expenditures per child with ASD were $28,682 in PA and $22,772 nationally in 2003 (Wang & Leslie, 2010; Wang et al., 2013), whereas the expenditures per child in nonexempt privately insured groups was much lower at $14,486 in 2010 (equivalent to $11,080 in 2003 dollars). This may suggest that children served by Medicaid tend to have more severe ASD requiring more intense treatment. Children need to have ASD symptoms that are severe enough to qualify for PA Medicaid program. Children with ASD who only have private insurance often tend to have less severe symptoms than children with ASD in Medicaid waiver programs. Note that many children with ASD in PA Medicaid waiver program also have private insurance, but the estimation of their private insurance cost would hardly be affected among those with both Medicaid and private insurance, since Medicaid is the “payer of last resort” and ASD treatment should be paid first by the private insurance.
In Pennsylvania, the autism mandate also applies to CHIP, and our data provided an opportunity to study this type of insurance coverage as well. Little change was seen in post-mandate expenditures for the nonexempt PA CHIP plan. A possible explanation for this is that children enrolled in the PA CHIP plan tend to have less severe ASD. In Pennsylvania, children may qualify for Medicaid if they meet the definition of disability by the Social Security Administration irrespective of their family income under the PA PH-95 Medicaid category (Kilgore, 2016). Children with more severe ASD are more likely to meet the definition and be eligible for PA Medicaid. Children who are potentially eligible for PA Medicaid due to their more severe ASD symptoms and who are also potentially eligible for CHIP due to their family income level would likely choose Medicaid over CHIP (they are not allowed to be insured by both), because of the probably lower out-of-pocket costs for families in Medicaid and its traditionally better ASD coverage. Therefore, those who enroll in PA CHIP generally would have less severe symptoms. In contrast to CHIP, privately insured children can be enrolled in PA Medicaid due to their ASD symptoms without losing their private insurance.
Although this study was based on the PA autism mandate, many of the conclusions can be generalized to other states. PA’s autism mandate is similar to most state autism mandates in many respects including the coverage of ABA treatment, the mandate’s applicability to large group insurers and exemption of the self-insured, the existence of yearly maximums etc. (Autism Speaks, 2018). Due to numerous similarities shared among state autism mandates, a similar pattern of a greater cost increase in the nonexempt groups when compared to the exempt groups can also be expected in other states. We also expect to see a similar pattern of significant increase in outpatient costs, but steady inpatient and drug cost in other states. However, the cost changes in small employer group plans and individual plans depend on whether a state autism mandate applies to those insurance plans.
Some limitations of this study are discussed as follows. First, insurance claims data do not contain clinical information on disease severity, limiting our ability to account for disease severity when estimating costs. Second, we used only data from one health insurer in one state. Admittedly variation among insurers can be seen even within the same state. Although many of our conclusions may be seen in other states, state mandates do have considerable variations in areas such as age limits and caps on ASD-related expenditures. The details of a state’s mandate as it relates to age, types of insurance, applicability of the mandate etc. need to be taken into account when interpreting the cost increase. Additional studies are needed to explore the differences among state mandates. Third, we do not have data on which self-insured plans voluntarily provided autism coverage. The value of the estimated average expenditure among the self-insured largely depends on the proportion of self-insured plans that voluntarily provided autism coverage. Despite these limitations, our study provides important information on the changes in post-mandate expenditures for children with autism in different insurance group plans.
The autism insurance mandate has tremendous impact on access to ASD care for children with ASD. As shown in this paper, children with ASD do not benefit from the mandate equally. Considerable barriers still exist when accessing ASD care due to certain exemptions from the mandate. Removing the barriers which continue to restrict access to ASD care warrants attention by policymakers to ensure all children receive the necessary ASD treatment. As seen in this paper, the autism mandate resulted in higher expenditures, which indicates that children with ASD are on average receiving more ASD treatment; however, further research is needed to assess the quality of this new care they receive and the resultant health benefits.
Highlights.
Healthcare expenditures for children with Autism Spectrum Disorders (ASD) greatly increased after the autism mandate
The post-mandate expenditure increase was much higher for groups that were subject to the autism mandate than exempt groups
The post-mandate expenditure increase was mainly due to outpatient services for ASD, rather than inpatient services or drug cost
The exempt self-insured plans experienced moderate increase in ASD-related expenditures after the autism mandate due to their voluntary coverage of ASD
Implications:
Healthcare providers treating children with ASD should be mindful of the state health insurance law regarding autism coverage. Even in states that have an autism mandate requiring private insurers to provide coverage for ASD, many children with private insurance may be exempt from the mandate and still face tremendous cost barriers when accessing ASD treatment.
Acknowledgements:
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number R01MH096711. The content is the solely responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare that they have no conflict of interest.
References:
- Health Resources & Services Administration. (2014). Area Health Resources Files. Retrieved from https://data.hrsa.gov/topics/health-workforce/ahrf
- Autism Speaks. (2018). Autism Insurance Reform. Retrieved from https://www.autismspeaks.org/advocacy/insurancereform
- Baio J, Wiggins L, Christensen D, Maenner M, Daniels J, Warren Z, & Kurzius-Spencer M (2018). Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ, 67, 1–23. doi: 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baller JB, Barry CL, Shea K, Walker MM, Ouellette R, & Mandell DS (2015). Assessing early implementation of state autism insurance mandates. Autism. doi: 10.1177/1362361315605972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendricks A, Candon MK, Xie M, & Mandell DS (2017). Effects Of State Insurance Mandates On Health Care Use And Spending For Autism Spectrum Disorder. Health Aff (Millwood), 36(10), 1754–1761. doi: 10.1377/hlthaff.2017.0515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouder JN, Spielman S, & Mandell DS (2009). Brief report: Quantifying the impact of autism coverage on private insurance premiums. J Autism Dev Disord, 39(6), 953–957. doi: 10.1007/s10803-009-0701-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JP, Jain A, Yang W, Kelly JP, Kaiser M, Becker L, … Newschaffer CJ. (2014). Does a claims diagnosis of autism mean a true case? Autism, 18(3), 321–330. [DOI] [PubMed] [Google Scholar]
- Candon MK, Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendricks A, Xie M, & Mandell DS (2018). The Differential Effects of Insurance Mandates on Health Care Spending for Children’s Autism Spectrum Disorder. Med Care, 56(3), 228–232. doi: 10.1097/MLR.0000000000000863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterji P, Decker SL, & Markowitz S (2015). The effects of mandated health insurance benefits for autism on out-of-pocket costs and access to treatment. J Policy Anal Manage, 34(2), 328–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, & Burner K (2011). Behavioral interventions in children and adolescents with autism spectrum disorder: a review of recent findings. Curr Opin Pediatr, 23(6), 616–620. doi: 10.1097/MOP.0b013e32834cf082 [DOI] [PubMed] [Google Scholar]
- Pennsylvania Department of Human Services. (2016). PA Autism Insurance Act. Retrieved from http://www.dhs.pa.gov/provider/paautisminsuranceact62
- Missouri Department of Insurance, Financial Institutions and Professional Registration. (2013). Annual Report to Missouri Legislature: Insurance Coverage for Autism Treatment & Applied Behavoir Analysis. Retrieved from http://insurance.mo.gov/consumers/autismFAQ/documents/2013AutismReport.pdf
- Eskow K, Pineles L, & Summers JA (2011). Exploring the Effect of Autism Waiver Services on Family Outcomes. Journal of Policy and Practice in Intellectual Disabilities, 8(1), 28–35. doi:DOI 10.1111/j.1741-1130.2011.00284.x [DOI] [Google Scholar]
- Ganz ML (2007). The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med, 161(4), 343–349. doi: 10.1001/archpedi.161.4.343 [DOI] [PubMed] [Google Scholar]
- Jensen GA, & Morrisey MA (1999). Small Group Reform and Insurance Provision by Small Firms, 1989—1995. Inquiry, 176–187. [PubMed] [Google Scholar]
- Kelly AM (2015). Caring for Patients with ASD and Their Caregivers: Federal and State Autism-Specific Insurance Reform. AMA J Ethics, 17(4), 328–341. doi: 10.1001/journalofethics.2015.17.4.hlaw1-1504 [DOI] [PubMed] [Google Scholar]
- Kennedy-Hendricks A, Epstein AJ, Mandell DS, Candon MK, Marcus SC, Xie M, & Barry CL (2018). Effects of State Autism Mandate Age Caps on Health Service Use and Spending Among Adolescents. J Am Acad Child Adolesc Psychiatry, 57(2), 125–131. doi: 10.1016/j.jaac.2017.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2017). 2017 Employer Health Benefits Survey. Retrieved from https://www.kff.org/report-section/ehbs-2017-section-10-plan-funding/
- Kilgore J (2016). An examination of Pennsylvania’s approach to Caring for Children with Special Healthcare Needs (CSHCN) and recommendations to improve access to needed services while controlling costs (Doctoral dissertation), University of Pittsburgh.
- Lambright. (2010). Actuarial Cost Estimate: Virginia House Bill No. 303 and Senate Bill No. 464 Retrieved from http://www.autismspeaks.org/sites/default/files/docs/gr/va.wyman_1.15.2010.pdf
- Lambright. (2012). Actuarial Cost Estimate: Nebraska Legislative Bill 1129. Retrieved from http://www.autismspeaks.org/images/advocacy/NE.Wyman.pdf
- Liptak GS, Stuart T, & Auinger P (2006). Health care utilization and expenditures for children with autism: data from U.S. national samples. J Autism Dev Disord, 36(7), 871–879. doi: 10.1007/s10803-006-0119-9 [DOI] [PubMed] [Google Scholar]
- Merryman MB, Miller NA, Shockley E, Eskow KG, & Chasson GS (2015). State adoption of Medicaid 1915(c) waivers for children and youth with Autism Spectrum Disorder. Disabil Health J, 8(3), 443–451. doi: 10.1016/j.dhjo.2015.03.003 [DOI] [PubMed] [Google Scholar]
- Peele PB, Lave JR, & Kelleher KJ (2002). Exclusions and limitations in children’s behavioral health care coverage. Psychiatr Serv, 53(5), 591–594. [DOI] [PubMed] [Google Scholar]
- Pennsylvania Health Care Cost Containment Council. (2008). Mandated Benefits Review by the Pennsylvania Health Care Cost Containment Council, 2008. Retrieved from http://www.phc4.org/reports/mandates/HB1150/docs/mandateHB1150report.pdf
- Polzer K, & Butler PA (1997). Employee health plan protections under ERISA. Employee Retirement Income Security Act. Health Aff (Millwood), 16(5), 93–102. [DOI] [PubMed] [Google Scholar]
- Rogers SJ, & Vismara LA (2008). Evidence-based comprehensive treatments for early autism. J Clin Child Adolesc Psychol, 37(1), 8–38. doi: 10.1080/15374410701817808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Small Business Administration. (2016). United States Small Business Profile. Retrieved from https://www.sba.gov/
- Shimabukuro TT, Grosse SD, & Rice C (2008). Medical expenditures for children with an autism spectrum disorder in a privately insured population. J Autism Dev Disord, 38(3), 546–552. doi: 10.1007/s10803-007-0424-y [DOI] [PubMed] [Google Scholar]
- Stein BD, Sorbero MJ, Goswami U, Schuster J, & Leslie DL (2012). Impact of a private health insurance mandate on public sector autism service use in Pennsylvania. J Am Acad Child Adolesc Psychiatry, 51(8), 771–779. doi: 10.1016/j.jaac.2012.06.006 [DOI] [PubMed] [Google Scholar]
- Velott DL, Agbese E, Mandell D, Stein BD, Dick AW, Yu H, & Leslie DL (2015). Medicaid 1915(c) Home- and Community-Based Services waivers for children with autism spectrum disorder. Autism. doi: 10.1177/1362361315590806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, & Leslie DL (2010). Health care expenditures for children with autism spectrum disorders in Medicaid. J Am Acad Child Adolesc Psychiatry, 49(11), 1165–1171. doi: 10.1016/j.jaac.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Mandell DS, Lawer L, Cidav Z, & Leslie DL (2013). Healthcare service use and costs for autism spectrum disorder: a comparison between medicaid and private insurance. J Autism Dev Disord, 43(5), 1057–1064. doi: 10.1007/s10803-012-1649-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren Z, McPheeters ML, Sathe N, Foss-Feig JH, Glasser A, & Veenstra-Vanderweele J (2011). A systematic review of early intensive intervention for autism spectrum disorders. Pediatrics, 127(5), e1303–1311. doi: 10.1542/peds.2011-0426 [DOI] [PubMed] [Google Scholar]
- Whiteley P, Todd L, Carr K, & Shattock P (2010). Gender Ratios in Autism, Asperger Syndrome and Autism Spectrum Disorder. Autism Insights, 2, 17–24. [Google Scholar]