Abstract
Background:
Smoking trends among nurses are important to monitor as smoking negatively affects their health and decreases their likelihood of providing cessation interventions to patients.
Objectives:
To describe the changes in smoking trends in the participants in the Nurses’ Health Study (NHS) cohorts over 27-years.
Methods:
An analysis of biennial changes in smoking status and cigarette consumption within nine five-year birth cohorts (1920–24 to 1960–64) and age-specific mortality rates by smoking status were examined in 237,648 female registered nurses (RNs): NHS (ages 30–55 in 1976, followed through 2002), and NHS II (ages 25–42 in 1989, followed through 2003).
Results:
Current smokers constituted 33.2% of NHS in 1976 and 13.5% of NHS II in 1989. Smoking rates declined in all birth cohorts; 8.4% were smoking in 2002/2003. Seventy-nine percent of nurses who ever smoked had quit. The mean cigarettes per day declined over time but still exceeded half a pack per day (15.1 cigarettes) at the end of follow-up. The mortality rate among current smokers was higher than for former smokers and was about twice that of never smokers in all age categories; those who smoked were more likely to have comorbid conditions.
Discussion:
This study provides the first report of smoking trends among RNs in the NHS. The decline in smoking among female nurses mirrors the decline in smoking among women in the U.S over the past 25-years. Increased mortality and morbidity indicate the devastating cost of smoking to the profession and can provide support for the urgent need for further research to encourage continued smoking cessation efforts for nursing professionals.
Keywords: cigarette smoking, tobacco smoking, smoking cessation, nurse
The Nurses’ Health Study (NHS) (http://www.channing.harvard.edu/nhs/history) is the largest and longest running longitudinal study of health among women in the world. Data from these nurses have been used to inform healthcare providers, researchers, and policy makers about critical risk factors affecting women’s health. When the NHS was initiated in 1976, it was more than a decade after the first Surgeon General’s Report on smoking and health (based heavily upon information about men) (U.S. Department of Health, Education, & Welfare, 1964) and just before the 1980 publication of the first Surgeon General’s report focused on women and tobacco (U.S. Department of Health and Human Services [USDHHS], 1980). This was an era of targeted advertising promoting smoking among women (Amos & Haglund, 2000; Toll & Ling, 2005; USDHHS, 2001;). In the 1970’s, female registered nurses (RNs) smoked at a higher rate (38.9%) than women in the U.S. population (32.0%) and at a substantially higher rate than physicians (21%) (USDHHS, 1980).
Despite a drop in smoking in the 1990’s, smoking among RNs (18.3%) remained higher than the rate for physicians (3.3%) (Nelson et al. 1994). Smoking among RNs in the U. S. has continued to decline, although the 2001/2002 rate of 14.8% according to data from the Tobacco Use Supplement of the Current Population Survey (U.S. Census Bureau, 2000), remains markedly higher that that of physicians (1%) surveyed in 2005 (Association of Medical Colleges, 2007). When the NHS began, coverage of smoking and health in the nursing literature was limited (Malone, 2006; Sarna & Lillington, 2002). Even today, the inclusion of tobacco cessation in nursing education remains inadequate (Wewers, Kidd, Armbruster, & Sarna, 2004), nurses struggle with quitting (Bialous, Sarna, Wewers, Froelicher, & Danao, 2004), and smoking continues as an issue in the workplace (Sarna, Bialous, Wewers, Froelicher, & Danao, 2005).
Nurses in the NHS, 30 to 55 years of age in 1976, had a prevalence of smokers (33.2%) similar to that of the U.S. female population in 1974 (32.1%) (USDHHS, 2001). The myriad of negative health consequences of smoking, especially for women, include increased risk for cardiovascular disease, multiple cancers (including lung, cervical, kidney/bladder, esophageal, oral, laryngeal, pancreatic, stomach cancer and acute myeloid leukemia), peripheral vascular disease stroke, respiratory diseases (e.g. chronic obstructive pulmonary disease, pneumonia), reproductive effects (e.g. reduced fertility, early menopause, fetal death, pregnancy complications), hip fractures, and peptic ulcer disease, among many other diseases, result in twice the risk of death of continuing smokers as compared to never smokers (USDHHS, 2001; USDHHS, 2004). Knowledge of these health effects among women was based upon data provided, in part, by nurses who participated in the NHS.
For healthcare providers, smoking is not only a personal health issue but also a public health concern, as providers who smoke are less likely to intervene with patients who smoke (Braun et al. 2004; Sarna, Wewers, Brown, Lillington, & Brecht, 2001; Slater, McElwee, Fleming, & McKenna, 2006). For most nurses, encounters with smokers are a part of everyday nursing practice. In 2006, over one in five U.S. adults were current cigarette smokers (18.0% of women, 23.9% of men) (Centers for Disease Control and Prevention [CDC], 2007a) with little decline in prevalence over the past seven years. Some subgroups, such as women with college education, have lower rates (8.4% undergraduate, 5.8% graduate degrees). Smoking and efforts to quit smoking vary by state of residence (CDC, 2007b) with higher smoking rates in the south (i.e. Kentucky, West Virginia, Oklahoma, Mississippi) and lower rates in the west (i.e. Utah, California) and vary by demographic characteristics. In general, smoking is more prevalent in those with less education, those below the federal poverty level, and varies by race/ethnicity (American Indians/Alaska Natives, 32.4%, non-Hispanic blacks, 23.0%, non-Hispanic Whites, 21.9%, Hispanics, 15.2%, Asians, 10.4%) (CDC, 2007a). In 2006, among ever smokers, over half (50.2%) have quit smoking (CDC, 2007a). Smoking is higher among those with tobacco-related chronic illness (36.9%) as compared to those with other chronic disease (23.0%) (CDC, 2007a).
Since the recognition of smoking as a critical health care issue in the mid twentieth century, smoking among nurses has been examined by a number of investigators. In an international review of published studies of smoking trends among nurses and a critique of the quality of such epidemiologic research, Smith and Leggat (2007) reviewed 73 English-language studies. Approximately two-thirds were published in the last decade, and one-third focused on smoking among nurses in the U.S. In general, although varying widely, smoking prevalence among nurses is decreasing in most countries. They identified several problems in these studies, including inconsistencies in methods and definitions of smoking status, small sample size, poor response rates, and lack of long-term follow-up.
The examination of self-reports of smoking over a forty-year period among 91,651 participants in NHS in 1976, revealed that the percentage of smokers increased among birth cohorts, age at initiation was inversely related to quit attempts with fewer women who began smoking at a younger age able to quit smoking, and that the proportion of women who quit increased with age (Meyers, et al. 1987). Although a number of studies indicate that some nurses in the later part of the twentieth century began smoking as student nurses (Smith, 2007), others indicate that nurses who smoke, similar to most adult smokers, begin smoking in their youth, prior to entering the profession (Bialous et al. 2004; Jenkins & Ahijevich, 2001; Rowe & Macleod Clark, 2000, Rowe & Clark, 2000).
Smoking is now recognized as not just a bad “habit” or lifestyle choice but as tobacco dependence, a chronic condition requiring repeat intervention (Fiore et al. 2000; Steinberg, Schmelzer, Richardson, Foulds, 2008). Nurses who smoke, similar to the general population, also have struggled to quit smoking (Chalmers et al. 2001; Gritz et al. 1988; Rowe & Clark, 1999), but there are limited long-term prospective studies examining nurses’ quitting behaviors. When the NHS began, nicotine was not yet recognized as addictive (Center for Health Promotion and Education, 1988), and there was limited knowledge as to the most effective way to quit smoking. Based on the evidence of thousands of research studies, effective tobacco dependence treatments were identified (Fiore et al. 2000). Behavioral support including counseling and pharmacotherapy, used alone and in combination, can double or triple the odds of long-term successful quitting. The most common strategy used for quitting, “cold turkey”, results in fewer than 5% abstinence one year after cessation (Fiore et al. 2000).
Although the Current Population Survey (U.S. Census Bureau, 2000) provides valuable population-based estimates of current smoking levels among various occupational groups, including registered nurses and licensed practical/vocational nurses, prospective analysis of long-term changes in smoking behavior over time are not possible. Analysis of data from the NHS allows for such examination of changes in smoking status among a large group of nurses for over a quarter of a century. Using the NHS data-set, the purpose of this study is to describe 27-year trends (1976–2003) in smoking status (current, former, never) and smoking characteristics (age of smoking initiation, number of cigarettes per day (cpd), parental smoking) among nurses. Demographic characteristics (presence of comorbid conditions, including tobacco-related conditions, living alone, parity, educational degree, race/ethnicity, and state of residence) related to smoking status were examined by smoking status.
Methods
Study Population
The first NHS cohort began in 1976 with married, female RNs born in 1920–1946 (Belanger, Hennekens, Rosner, & Speizer, 1978). Seventy-one percent of RNs identified in the 11 most populous states responded after three mailings of a questionnaire. Responders were similar to non-responders (Barton et al., 1980). Current smokers represented 32.7%, 34.2%, and 34.5% of the respondents to the first, second, and third mailings. NHS II was launched in 1989 to recruit younger nurses, born in 1947–1964, with a single mailing to RNs from 14 most populous states (24% response rate). Questionnaires are mailed every two years to identify incident diseases and to collect health-related data. Response rates have remained high, averaging 90% in the NHS and 91% in NHS II. This analysis uses questionnaire data from 1976–2002 in the NHS and from 1989–2003 in NHS II. Women were excluded who lacked baseline information about smoking status (0.3%), leaving a study population of 237,648 (121,206 in the NHS and 116,442 in NHS II). Deaths were confirmed by next-of- kin, by the post-office, and by a search of the National Death Index for women who failed to respond to questionnaires (Rich-Edwards, Corsano, & Stampfer, 1994; Stampfer et al. 1984). During follow-up, there were a total of 15,192 confirmed deaths in NHS and 1,038 in NHS II, representing at least 98% of all deaths in the cohort.
Smoking Characteristics
In 1976, the NHS questionnaire asked participants if they currently or ever smoked cigarettes regularly, and if so, at what age regular smoking began. Current smokers wrote in their average number of cpd. As of 1982, cpd was reported by category (1–4, 5–14, 15–24, 25–34, 35–44, ≥45 cpd). The initial 1989 questionnaire in the NHS II collected similar baseline smoking information, though ever smokers were defined as having ever smoked 20 or more packs of cigarettes, and age at smoking initiation was inferred from reported cpd during earlier life periods: <15, 15–19, 20–24, 25–29, and 30–35 years. Continuous data for age at smoking initiation from the NHS were placed into these categories. In both the NHS and NHS II, current smoking and cpd were assessed in every questionnaire. However, cpd was not included on short versions of the questionnaire sent to participants who failed to respond after five mailings of the full version. Over follow-up, 12% of current smokers in the NHS and 7% in NHS II did not have an updated report of cpd. Missing cpd in current smokers was unrelated to previously reported quantity.
Participants were classified by smoking status at cohort initiation and reclassified in each biennial follow-up cycle. A standard algorithm used in analyses of NHS data was used to update smoking status if participants failed to respond. For those who had been a current smoker or a former smoker for less than ten years, smoking status was maintained for one follow-up cycle and assigned a missing status on the second consecutive missed questionnaire. For never smokers and former smokers who had quit ten or more years ago, smoking status was maintained when questionnaires were missed because less than 2% were observed to initiate smoking or have a relapse of smoking. The use of the algorithm reduced missing smoking status from 11% to 2.4% of the observations. The majority of these missing data (60%) were assigned to the never smoking category. Missing cpd data was not replaced.
Data on attempts at smoking cessation were not collected. As a crude proxy measure, the number of times a woman changed smoking status from current to former between consecutive biennial questionnaires was counted. Former smokers at study entry began with a count of one attempt.
Parental smoking during childhood was assessed in 1982 in the NHS and in 1999 in NHS II.
Comorbidity and demographic characteristics
The presence of a comorbid condition was determined from an affirmative response to questionnaire queries about diagnoses of major illnesses (cardiovascular disease (high blood pressure, myocardial infarction, angina pectoris, peripheral artery disease or claudication, coronary artery surgery, TIA, stroke), cancer (breast, cervical, uterine, ovarian, colon, rectum, lung, liver, melanoma, pancreas, bladder/kidney, esophageal, leukemia, laryngeal, oral, stomach), respiratory diseases (asthma, emphysema, chronic bronchitis, active TB), other (diabetes mellitus, systemic lupus erythematosis, multiple sclerosis, ALS, cataracts, macular degeneration, gastric or duodenal ulcer). The presence of a tobacco-related comorbidity was based on a subset of these illnesses (cardiovascular disease (as described above), cancer (cervical, lung, pancreas, bladder/kidney, esophageal, laryngeal, oral, stomach), respiratory (emphysema, chronic bronchitis) disease) as identified in the 2004 Surgeon General’s Report (USDHHS, 2004). Comorbidity was only determined for women in the NHS because prevalence was very low in the younger NHS II cohort.
Living arrangement (alone or with others) was assessed in 2000 in the NHS and in 2001 for NHS II. Parity was ascertained on every NHS II questionnaire and on NHS questionnaires through 1984. Highest educational degree was only assessed in NHS on the 1992 questionnaire. Race/ethnicity was self-reported as Caucasian, African American, Hispanic, Asian, and other; multiple categories were permitted. Though participants in the NHS and NHS II lived in selected states at cohort initiation, they resided throughout the U.S. by the end of follow-up. State of residence was grouped by residence into geographic areas (Northeast, Midwest, South, and West) according to the Current Population Survey (U.S. Census Bureau, 2000).
Statistical Analysis
Data were extracted from 14 biennial questionnaires (1976–2002) in NHS and from 8 biennial questionnaires (1989–2003) in NHS II. Age, smoking status and cpd were updated with each successive questionnaire. Mortality rates (deaths/100,000 person-years) were calculated by smoking status within 5-year age groups from 1976–2002 for women 50 to 79 years of age in NHS.
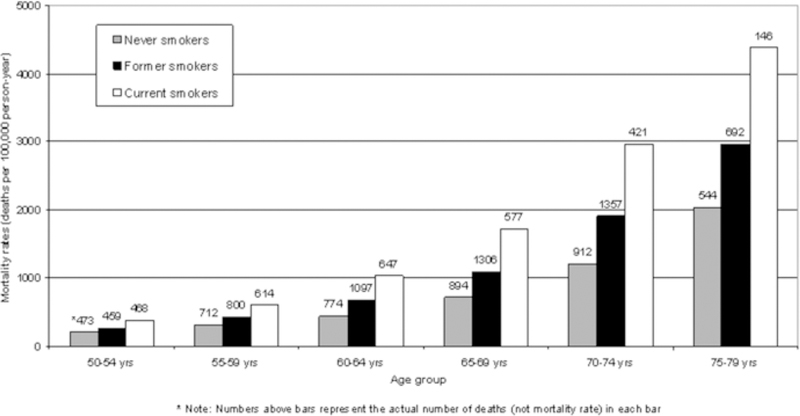
Prevalence of current and former smokers within the study population was calculated within nine 5-year birth cohorts (1920–24 through 1960–64) for each questionnaire year, combining the data from odd years in NHS II with those from even years in NHS as follows: 1988 and 1989, 1990 and 1991, etc, through 2002 and 2003. Because smoking is associated with an increased risk of death, smoking prevalence was anticipated to be misrepresented in the older birth cohorts. Therefore, the adjusted prevalence of current and former smokers was based on the observed probabilities of remaining a current smoker, remaining a former smoker, or changing smoking status from current to former or from former to current was calculated. (See footnote 1, Figure 2 and footnote 1, Figure 3).
FIGURE 2.

Adjusted prervalence of current smokers by calendar year for 5-yr birth cohorts (Nurses’ Health Study & Nurses’ Health Study II).
FIGURE 3.
Adjusted prevalence of former smokers among ever smokers, by calendar year, for 5-year birth cohorts (Nurses’ Health Study & Nurses’ Health Study II).
The mean number of cpd among current smokers was calculated within the same nine 5-year birth cohorts for each questionnaire year, using the median number within reported cpd categories.
Characteristics of the study population were determined at 2002/2003 or at time of death and were stratified by smoking status. Data were standardized to the age distribution of the study population to control for differences in age by smoking status; the chi-square statistic was used to test for significant differences. All p-values are two-tailed; values < 0.05 were considered to be statistically significant.
Results
When the NHS began in 1976, 33.2% of the nurse participants were current smokers and 23.3% were former smokers. In 1989 at the start of NHS II, current and former smokers represented 13.5% and 21.4%, respectively, of the cohort. At this time, smoking was still more prevalent in the older NHS nurses (19.6%). In the combined cohorts in 1988/1989, 16.5% were current smokers. At the end of follow-up in 2002/2003 when the women were 39 to 81 years of age, 8.4% were current smokers and 35.4% were former smokers.
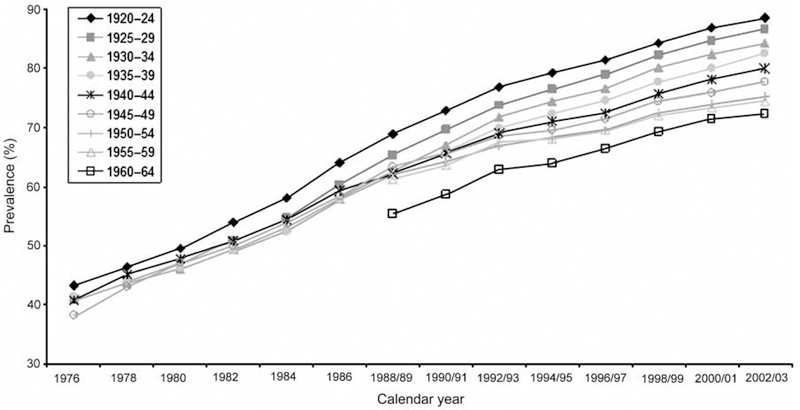
Differences in morbidity and mortality by smoking status
In all age groups, mortality rates were highest in current smokers and lowest in never smokers (Figure 1). Though mortality rose steeply with age, the increased risk with smoking was fairly stable across age groups. For example, in the youngest 50–54 year age group, mortality was 1.9 times higher in current smokers and 1.3 times higher in former smokers compared with never smokers, while among women 75–79 years of age, rates were 2.3 and 1.5 times higher, respectively.
FIGURE 1.
1976–2002 Age-specific mortality rates in never former and current smokers (Nurses’ Health Study & Nurses’ Health Study II).
* Note: Numbers above bars represent the actual number of deaths (not mortality rate) in each bar
Changes in smoking
The 27-year trends in adjusted prevalence of current smokers within 5-year birth cohorts, accounting for differential mortality by smoking status, are presented in Figure 2. Prevalence was highest in the 1930–34 birth cohort until 1992 when it was surpassed by the 1940–44 birth cohort. When the NHS II was added in 1989, these younger birth cohorts had lower prevalence of current smokers than the older NHS birth cohorts, but at the end of follow-up, current smokers contributed the lowest percentage in the oldest (1920–24) birth cohorts. The prevalence of current smokers appeared to drop sharply in the 1945–49 birth cohort with the addition of the NHS II women in 1989. Differences between the actual prevalence of current smokers and the adjusted ones in Figure 2 were minor except in late follow-up of the older birth cohorts when mortality rates were high. For example, in the 1920–24 birth cohort, the adjustment increased the prevalence of current smokers from 25.8% to 27.4% in 1980 and from 4.5% to 6.2% in 2002, whereas in the 1940–44 birth cohort, prevalence was more modestly increased from 28.1% to 29.2% and from 10.6% to 11.2%, respectively. There was little difference between the raw and adjusted prevalence in younger birth cohorts.
The 27-year trends in adjusted prevalence of former smokers by birth cohort within the population of ever smokers (45.9% of participants) are presented in Figure 3. The prevalence of former smokers increased in all birth cohorts as smokers continued to quit over time. At each point in follow-up, the highest prevalence was in the oldest, 1920–24, birth cohort and the lowest prevalence was in the youngest, 1960–64, birth cohort. At the end of follow-up in 2002/2003, the prevalence of former smokers increased in order of increasing age.
Changes in amount of cigarettes per day
The mean cpd among current smokers declined over time in all birth cohorts (Figure 4), but still exceeded a half pack per day. NHS birth cohorts reached a peak between 19.5 and 20.6 cpd in 1986, then decreased 4 to 5 cpd by 2002. From 1986 until 2002, the 1940–44 birth cohort had the highest cpd. When the younger NHS II women were added in 1989, they smoked fewer cigarettes but their consumption still dropped another 2 or 3 cpd by 2003. By the end of follow-up, cpd was lowest in the oldest (1920–24) and youngest (1960–64) birth cohorts (13.5 and 13.7 cpd, respectively) and highest in the 1940–44 and 1945–49 birth cohorts (16.1 cpd for both), with a mean of 15.3 among all participants.
FIGURE 4.

Mean cigarettes per day among current smokers, by calendar year, for 5-year birth cohorts: Nurses’ Health Study & Nurses’ Health Study II.
Demographic differences by smoking status
Characteristics of the study population at the end of follow-up for each participant (2002/2003 or time of death) are shown in Table 1. Seventy-nine percent of nurses who ever smoked had quit. Sixty-nine percent of the smokers never reported a non-smoking period. Eighty-six percent of former smokers had quit before initiation of the study and never reported another period of smoking. After adjusting for age differences by smoking status, current smokers were most likely to live alone and have grown up in a household where both parents smoked. Ever smokers were more likely to have comorbid conditions, including tobacco-related diseases compared with nurses who never smoked. Among the ever smokers, about 40% began to smoke at age 20 or later. When degree of educational attainment was assessed in NHS in 1992, smoking prevalence was 10% for those with a doctorate or master’s degree, 13% for those with a bachelor’s degree, and 16% for the women who did not attain a degree beyond RN.
Table 1.
Age and age-adjusted characteristics within smoking status as of 2002 (NHS), 2003 (NHS II), or time of death
| Smoking Status | ||||
|---|---|---|---|---|
| Never | Former | Current | p | |
| (n=126,015) | (n=82,441) | (n=21,410) | ||
| Mean age (y)a | 56.2 | 61.5 | 57.8 | <.001 |
| % | % | % | ||
| Age at smoking initiation | <.001 | |||
| < 15 y | 6.7 | 7.2 | ||
| 15–19 y | 54.0 | 51.8 | ||
| 20–24 y | 31.4 | 32.4 | ||
| ≥ 25 y | 7.9 | 8.6 | ||
| Change from current to former | <.001 | |||
| smoker | ||||
| Never | 68.6 | |||
| Once | 85.8 | 24.0 | ||
| Twice | 11.8 | 6.2 | ||
| Three or more times | 2.4 | 1.2 | ||
| Parental smoking during | <.001 | |||
| childhood | ||||
| Neither parent smoked | 39.2 | 28.3 | 24.2 | |
| Mother only smoked | 5.5 | 7.6 | 7.4 | |
| Father only smoked | 35.5 | 37.3 | 37.8 | |
| Both parents smoked | 19.8 | 26.8 | 30.6 | |
| Live alone | 10.1 | 11.8 | 16.4 | <.001 |
| Parous | 87.0 | 87.2 | 85.2 | <.001 |
| Comorbid diseaseb | 76.6 | 81.6 | 80.1 | <.001 |
| Tobacco-related comorbid | 42.9 | 50.8 | 54.8 | <.001 |
| diseasec | ||||
Note. All values are percents of the population within each smoking status.
Age comparisions included, never vs past, never vs current, and past vs current
Comorbid conditions included presence of: cardiovascular disease (high blood pressure, myocardial infarction, angina pectoris, peripheral artery disease or claudication, coronary artery surgery, TIA, stroke), cancer (breast, cervical, uterine, ovarian, colon, rectum, lung, liver, melanoma, pancreas, bladder/kidney, esophageal, leukemia, laryngeal, oral, stomach), respiratory diseases (asthma, emphysema, chronic bronchitis, active TB), other (diabetes mellitus, systemic lupus erythematosis, multiple sclerosis, ALS, cataracts, macular degeneration, gastric or duodenal ulcer), df = 2, chi square = 489.0, P < 0.001
Tobacco-related comorbid conditions included presence of: cardiovascular disease (as described above), cancer (cervical, lung, pancreas, bladder/kidney, esophageal, laryngeal, oral, stomach), respiratory (emphysema, chronic bronchitis) disease (U.S. Department of Health and Human Services, 2004).
Age-standardized smoking prevalence by race and by geographic region of residence in 2002/2003 or at time of death revealed significant differences in smoking patterns. Women in the NHS and NHS II cohorts were largely White-Non Hispanic (n = 210,265), and 9.5% of them were current smokers, compared with 8.0% in African Americans (n = 4,142), 3.5% in Asians (n = 2,963), 7.2% in Hispanic-White women (n = 1,420), and 8.8% in others (11,076). One percent (2,810) checked more than one race. Current smokers were most prevalent in the Northeast (10.2%), followed by the South (9.8%), Midwest (9.1%), and West (6.8%).
Discussion
This study provides the first prospective report of data about smoking trends among registered nurse participants in the Nurses’ Health Study (NHS and NHS II). These findings of declining smoking among these nurses mirrors the decline in smoking among women in the U.S. and provides a window into the changing social norms of smoking among women. Smoking in the NHS and NHS II cohorts declined substantially over the 27 years of follow-up. By 2002/2003, smoking prevalence was 8.4%, lower than the 2001/2002 national population-based rate of 14.8% among RNs (U.S. Census Bureau, 2000), but considerably higher than the 2005 1% smoking rate from a national sample of physicians (Association of Medical Colleges, 2007).
Sixty-nine percent of RNs who were smokers at the end of follow-up had never reported a non-smoking status on a biennial questionnaire, revealing the challenges of long term quitting for some nurses (Bialous et al., 2004) as for many smokers (Fiore et al. 2000). Although not unexpected because of the addictive nature of cigarettes, these data are sobering. Regardless of access to information about health risks, nurses may have lacked professional and institutional support for quitting (Sarna, Bialous, Barbeau, & McLellan, 2006).
Similar to the fifty-year findings of the British Doctor’s Health Study (Doll, Peto, Boreham, & Sutherland, 2004), these prospective data demonstrate that quitting smoking made a difference, with nurses who became former smokers having lower mortality rates. The increase in former smokers during the study followed the overall pattern in the country, partly as a reflection of increasing public awareness of harmful effects of tobacco use and policy changes increasing smoke-free environments (Fichtenberg & Glantz, 2002). The decline also may have been influenced by the 1993 Joint Commission’s mandate for smoke-free hospitals (Longo et al. 1996; Stillman, Hantula, & Swank, 1994). The increase in former smoking rates might reflect the increased mortality and morbidity among aging participants. Former smokers had the highest rates of comorbidity, but participants were not asked why they quit smoking.
The quantity of cigarettes consumed is an indication of addiction as well as increased risk for negative health outcomes (USDHHS, 2001). These data demonstrate a trend toward smoking fewer cpd after a peak in 1986. This is similar to a national trend in lighter smoking among women (USDHHS, 2001), with a mean of 15.3 cpd in 2004 (CDC, 2005a). Higher cpd’s in birth cohorts with higher prevalence of current smokers was observed. For example, the highest adjusted smoking prevalence (11.2%) and cpd (16.1) in 2002/2003 were among women born in 1940–44, while the oldest (1920–24) birth cohort had lower adjusted prevalence (6.2%) and the lowest cpd (13.5).
There are several limitations to this analysis. Although this is the largest prospective analysis of smoking patterns among nurses, unlike the British Doctor’s Study (Doll, Peto, Boreham, & Sutherland, 2004), the NHS was not originally intended to monitor smoking-related mortality. Despite the high response rate, the NHS cohorts were not selected as a nationally representative sample of nurses in the U.S. In particular, the observed smoking rates of the younger NHS II women may underestimate the rates in the general population of nurses in these age groups because the cohort is comprised of responders to a single questionnaire mailing, though smoking rates were similar in responders to the three mailings in NHS. Also, smokers may have been under-represented if they had a lower response rate to the biennial questionnaires, though less than three percent over follow-up was missing smoking status in our analyses. Smoking status was not biochemically validated and participants may have under-reported both smoking status and cpd. Due to the lack of data, the extent of exposure to secondhand smoke which might affect morbidity and mortality of both smokers and non-smokers is impossible to evaluate. Although the differential mortality by smoking status was corrected statistically, residual influence of higher mortality among smokers may have exaggerated declining smoking prevalence in the older birth cohorts. Due to lack of information, the assessment of the number of times women quit smoking before they successfully stopped is limited.
Additionally, due to lack of information on the NHS questionnaire, data on nursing specialty is not included. Other investigators have identified differences in smoking prevalence by nursing specialty group with higher smoking among psychiatric critical care and emergency room nurses (Storr, Trinkoff, & Hughes, 2000; Trinkoff & Storr, 1998). The information on changes in education is also not available. Higher education is linked with lower smoking rates (CDC, 2007a). The sample may include nurses who increased their level of education during the study period.
These data provide an insight into the devastating impact of smoking among nurses and among women during the past thirty years. In the NHS, 40% of participants reported beginning to smoke after age 20, a time when they might have been in nursing school. Even now, reports of high rates of smoking among nursing students (Patkar, Hill, Batra, Vergare, & Leone, 2003), four times higher than among medical students, indicate that smoking among future nurses needs further attention from nurse leaders.
Social norms about tobacco use in the US and other countries are changing (Koh, Joosens, & Connolly, 2007), but data in this study suggest a grim future for many nurses who continue to smoke at high rates internationally (CDC, 2005b; Mackay, Eriksen, & Shafey, 2006). These data can be used to support efforts to prevent the tobacco-related epidemic in other parts of the world where smoking trends in women are on the increase (Mackay, Eriksen, & Shafey, 2006). Smoking is also a critical public health concern because of the importance of nurses’ health, especially during a time of scarcity (Buerhaus, Donelan, Ulrich, Norman, & Dittus, 2006) and because nurses who smoke are less likely to effectively intervene with patients who smoke (Sarna, Wewers, Brown, Lillington, & Brecht, 2001; Slater, McElwee, Fleming, & McKenna, 2006). Actions and policies to support cessation services for current and future generations of nurses are needed.
Acknowledgements:
This project was supported by a grant from the Robert Wood Johnson Foundation #55769 (Sarna); funding from the National Cancer Institute 1 K07 CA 92696–02 (Mary E. Cooley). Nurses’ Health Study is supported by grants CA87979 and CA50385 from the National Institutes of Health. The authors thank Dr. Bernard A. Rosner, Professor of Biostatistics at Harvard School of Public Health and the chief statistician for the Nurses’ Health Study for valuable statistical consultation, and Dr. Marjorie Wells, Project Director, School of Nursing, University of California, for her assistance with this project.
References
- Amos A, & Haglund M (2000). From social taboo to “torch of freedom”: the marketing of cigarettes to women. Tobacco Control, 9, 3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of Medical Colleges. (2007). Physician behavior and practice patterns related to smoking cessation. A report prepared for the American Legacy Foundation; Retrieved July 1, 2007 from http://americanlegacy.org/Files/Physicians_Study_-Legacy_Report.pdf [Google Scholar]
- Barton J, Bain C, Hennekens CH, Rosner B, Belanger C, Roth A, et al. (1980). Characteristics of respondents and non-respondents to a mailed questionnaire. American Journal of Public Health, 70, 823–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belanger CF, Hennekens CH, Rosner B, & Speizer FE (1978). The nurses’ health study. American Journal of Nursing, 78, 1039–1040. [PubMed] [Google Scholar]
- Bialous SA, Sarna L, Wewers ME, Froelicher ES, & Danao L (2004). Nurses’ perspectives of smoking initiation, addiction, and cessation. Nursing Research 53, 387–395. [DOI] [PubMed] [Google Scholar]
- Braun BL, Fowles JB, Solberg LI, Kind EA, Lando H, & Pine D (2004). Smoking-related attitudes and clinical practices of medical personnel in Minnesota. American Journal of Preventive Medicine, 27, 316–322. [DOI] [PubMed] [Google Scholar]
- Buerhaus PI, Donelan K, Ulrich BT, Norman L, & Dittus R (2006). State of the registered nurse workforce in the United States. Nursing Economic$, 24, 6–12. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2005a). Cigarette Smoking Among Adults ---United States, 2004. Morbidity and Mortality Weekly Report, 54, 1121–1127. Retrieved Nov 11, 2005 from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5444a2.htm [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2005b). Tobacco use and cessation counseling---Global Health Professionals Survey pilot study, 10 countries, 2005. Morbidity and Mortality Weekly Report, 54, 505–509. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2007a). Cigarette smoking among adults---United States, 2006. Morbidity and Mortality Weekly Report, 56, 1157–1161. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2007b). State-specific prevalence of cigarette smoking among adults and quitting among persons aged 18–35 years---United States, 2006. Morbidity and Mortality Weekly Report, 56, 993–996. [PubMed] [Google Scholar]
- Center for Health Promotion and Education. (1988). The Health Consequences of Smoking: Nicotine Addiction: A Report of the Surgeon General. Office on Smoking and Health; Retrieved April 2, 2008 from http://profiles.nlm.nih.gov/NN/B/B/Z/G/_/nnbbzg.pdf [Google Scholar]
- Chalmers K, Bramadat IJ, Cantin B, Murnaghan D, Shuttleworth E, Scott-Findlay S, et al. (2001). A smoking reduction and cessation program with registered nurses: findings and implications for community health nursing. Journal of Community Health Nursing, 18(2), 115–134. [DOI] [PubMed] [Google Scholar]
- Doll R, Peto R, Boreham J, & Sutherland I (2004). Mortality in relation to smoking: 50 years’ observation on male British doctors. BMJ, 328, 1519–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichtenberg CM, & Glantz SA (2002). Effect of smoke-free workplaces on smoking behavior. systematic review. BMJ, 325, 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman S, Goldstein MG, Gritz ER, et al. (2000). Treating tobacco use and dependence Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service. [Google Scholar]
- Gritz ER, Marcus AC, Berman BA, Read LL, Kanim LE, & Reeder SJ (1988). Evaluation of a worksite self-help smoking cessation program for registered nurses. American Journal of Health Promotion, 3(2), 26–35. [DOI] [PubMed] [Google Scholar]
- Koh HK, Joossens LX, & Connolly GN (2007). Making smoking history worldwide. New England Journal of Medicine, 356, 1496–1498. [DOI] [PubMed] [Google Scholar]
- Longo DR, Brownson RC, Johnson JC Hewett JE, Kruse RL, Novotny TE, et al. (1996). Hospital smoking bans and employee behavior: results of a national survey. JAMA, 275, 1252–1257. [PubMed] [Google Scholar]
- Mackay J, Eriksen M, & Shafey O (2006). The Tobacco Atlas (Second Edition). Atlanta, Georgia: American Cancer Society, Myriad Editions Limited. [Google Scholar]
- Malone RE (2006). Nursing’s involvement in tobacco control: historical perspective and vision for the future. Nursing Research, 55 (4, Supplement 1), S51–S57. [DOI] [PubMed] [Google Scholar]
- Meyers AH, Rosner B, Abbey H, Willet W, Stampfer MJ, Bain C, et al. (1987). Smoking behavior among participants in the nurses’ health study. American Journal of Public Health, 77, 628–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson DE, Giovino GA, Emont SL, Brackbill R Cameron LL Peddicord J, et al. (1994). Trends in cigarette smoking among US physicians and nurses. JAMA, 271, 1273–1275. [PubMed] [Google Scholar]
- Patkar AA, Hill K, Batra V, Vergare MJ, & Leone FT (2003). A comparison of smoking habits among medical and nursing students. Chest, 124, 1415–1420. [DOI] [PubMed] [Google Scholar]
- Rich-Edwards JW, Corsano KA, & Stampfer MJ (1994). Test of the National Death Index and Equifax Nationwide Death Search. American Journal of Epidemiology, 140, 1016–1019. [DOI] [PubMed] [Google Scholar]
- Rowe K, & Clark JM (1999). Evaluating the effectiveness of a smoking cessation intervention designed for nurses. International Journal of Nursing Studies, 36, 301–311. [DOI] [PubMed] [Google Scholar]
- Rowe K, & Clark JM (2000). The incidence of smoking amongst nurses: A review of the literature. Journal of Advanced Nursing, 31, 1046–1053. [DOI] [PubMed] [Google Scholar]
- Rowe K, & Macleod Clark J (2000). Why nurses smoke: A review of the literature. International Journal of Nursing Studies, 37, 173–181. [DOI] [PubMed] [Google Scholar]
- Sarna L, Bialous S, Barbeau E, & McLellan D (2006). Strategies to implement tobacco control policy and advocacy initiatives. Critical Care Nursing Clinics of North America, 18, 113–122, xiii. [DOI] [PubMed] [Google Scholar]
- Sarna L, Bialous SA, Wewers ME, Froelicher ES, & Danao L (2005). Nurses, smoking, and the workplace. Research in Nursing and Health, 28, 79–90. [DOI] [PubMed] [Google Scholar]
- Sarna L, & Lillington L (2002). Tobacco: an emerging topic in nursing research. Nursing Research, 51, 245–253. [DOI] [PubMed] [Google Scholar]
- Sarna L, Wewers ME, Brown JK, Lillington L, & Brecht ML (2001). Barriers to tobacco cessation in clinical practice: report from a National Survey of Oncology Nurses. Nursing Outlook, 49(4), 166–172. [DOI] [PubMed] [Google Scholar]
- Slater P,MG, Fleming P, & McKenna H (2006). Nurses’ smoking behaviour related to cessation practice. Nursing Times, 102(19), 32–7. [PubMed] [Google Scholar]
- Smith DR (2007). A systematic review of tobacco smoking among nursing students. Nurse Education in Practice, 7, 293–302. [DOI] [PubMed] [Google Scholar]
- Smith DR, & Leggat PA (2007). An international review of tobacco smoking research in the nursing profession, 1976–2006. Journal of Research in Nursing, 12, 165–181. [Google Scholar]
- Stampfer M, Willet WC, Speizer FE, Dysert DC, Lipnick R, Rosner B, et al. (1984). Test of the National Death Index. American Journal of Epidemiology, 119, 837–839. [DOI] [PubMed] [Google Scholar]
- Steinberg MB, Schmeizer BA, Richardson DL, & Foulds J (2008). The case for treating tobacco dependence as a chronic disease. Annals of Internal Medicine, 148, 554–556. [DOI] [PubMed] [Google Scholar]
- Stillman FA, Hantula DA, & Swank R (1994). Creating a smoke-free hospital: attitudes and smoking behaviors of nurses and physicians. American Journal of Health Promotion, 9, 108–114. [DOI] [PubMed] [Google Scholar]
- Storr CL, Trinkoff AM, & Hughes P (2000). Similarities of substance abuse between medical and nursing specialties. Substance Use and Misuse, 35, 1443–1469. [DOI] [PubMed] [Google Scholar]
- Toll BA, & Ling PM (2005). The Virginia Slims identity crisis: an inside look at tobacco industry marketing to women. Tobacco Control, 14, 172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkoff AM, & Storr CL (1998). Substance use among nurses: differences between specialties. American Journal of Public Health, 88, 581–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (2000). The Current Population Survey: January 2001–2002: Tobacco Use Supplement. Retrieved May 5, 2004, from http://www.census.gov/prod/2002pubs/tp63rv.pdf
- U.S. Department of Health and Human Services. (1980). The Health Consequences of Smoking for Women: A Report of the Surgeon General. Retrieved April 4, 2006, from http://profiles.nlm.nih.gov/NN/B/B/R/T/_/nnbbrt.pdf
- U.S. Department of Health and Human Services. (2001). Women and smoking: A report of the Surgeon General Washington, DC: U.S. Department of Health and Human Services, Centers for Disease Prevention and Control, National Center for Chronic Disease Prevention and Promotion, Office on Smoking and Health. [Google Scholar]
- U.S. Department of Health and Human Services. (2004). The Health Consequences of Smoking: A Report of the Surgeon General. Washington, DC: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- U.S. Department of Health, Education, & Welfare. (1964). Smoking and Health: Report of the advisory committee to the Surgeon General of the Public Health Service. (Public Health Service Publication No. 1103). Washington, D.C: U.S. Public Health Service. Office of the Surgeon General. [Google Scholar]
- Wewers ME, Kidd K, Armbruster D, & Sarna L (2004). Tobacco dependence curricula in U.S. baccalaureate and graduate nursing education. Nursing Outlook, 52, 95–101. [DOI] [PubMed] [Google Scholar]


