Abstract
This examination of 237 African American and Hispanic mothers of young children explored the longitudinal linkages between romantic partner relationship quality and maternal depressive symptoms among low-income ethnic minority populations. Most studies to date have largely focused on majority non-Hispanic White populations, as well as married partner dyads, and very few have utilized longitudinal designs. At three time points, participants completed a series of questionnaires including the Dyadic Adjustment Scale (DAS) for partner relationship quality, and the Center for Epidemiologic Studies Depression (CESD-R) scale for maternal depressive symptoms during home visit interviews. Both concurrent and prospective correlations were significant and negative, indicating a higher level of relationship quality was associated with fewer depressive symptoms. After adjusting for potential confounders, partner relationship quality was prospectively associated maternal depressive symptoms but not vice versa. This pattern did not differ by maternal ethnicity. The findings of this study support and contribute to the limited research conducted to date to uncover patterns and influences of associations between romantic partner relationship quality and depressive symptoms in representative samples of ethnic minority populations.
Keywords: African American, Depression, Hispanic, Mother, Relationship Quality
Partner Relationship Quality and Maternal Depressive Symptom Associations among Low- Income African American and Hispanic Mothers of Preschool-Aged Children
Transitions to various life stages, including long-term relationships, marriage, and/or parenthood, can result in critical periods in which there may be an increased risk for interpersonal relationship challenges or negative health outcomes (Fagan, 2009). In general, healthy relationships, especially those that are romantic in nature, can promote greater life satisfaction and are characterized by more effective communication, conflict resolution, and problem-solving (Dush & Amato, 2005; Papp, Goeke-Morey, & Cummings, 2007). However, research indicates that couples experiencing distress in their relationships often provide and receive reduced support from their partners as well as have increased negative interactions or engage in overt acts of hostility (Parker, Tambling, & Campbell, 2012). Poor relationships can also manifest in or be influenced by mental health issues (e.g., anxiety, depression) and/or physical health problems (Graham, & Liu, 2006; Parker, Tambling, & Campbell, 2012; Røsand, Slinning, Eberhard-Gran, Røysamb, & Tambs, 2012).
Much of the previous empirical literature related to relationships and their effects on individuals and their partners have largely focused on examining non-Hispanic White, married partner dyads, generally demonstrating consistent benefits derived from such unions (Marcussen, 2005; Simon, 2002). Married couples tend to be more educated, earn higher combined incomes, and report superior relationship and mental health outcomes, often due to increased personal, social, and socioeconomic resources at their disposal (Marcussen, 2005). However, in recent decades, numerous sociodemographic changes have altered the composition of romantic partnerships, including declining marriage rates, increasing average age at first marriage, increasing divorce and cohabitation rates, and evolving opportunities for same sex marriages/partnerships (Cherlin, 2010; Lee & Payne, 2010).
Shifts in the makeup of romantic partnerships may result in unique interpersonal and psychosocial outcomes among diverse populations that are worth examination. Notably, exploring differences based on relationship status may be important because ethnic minorities are less likely to be married than non-Hispanic Whites (Vespa, Lewis, & Kreider, 2013). In addition to potentially not enjoying some of the above-mentioned benefits of marital unions, those not married may also experience less psychological protections than do married couples. For instance, some studies have shown that non-married, cohabiting couples report less happiness and higher levels of depressive symptoms than do married individuals (Brown, Abe-Kim, & Barrio, 2003; Marcussen, 2005; Klausli & Owen, 2011). Therefore, assessing similarities and differences within ethnic minority dyads can be useful in comparing to the predominant literature in the field as it relates to the influence of relationships and their health effects on individuals, their partners, and/or families.
Associations between Partner Relationship Quality and Depressive Symptoms
When considering individual and family quality of life outcomes, depression is a condition that can have a profound impact on individual health, work/economic productivity and success, interpersonal relationships and social networks, parenting behaviors, and child well- being (Ensminger, Hanson, Riley, & Juon, 2003; Hammen & Brennan, 2003; Petterson & Albers, 2001). Depression is a leading cause of disability worldwide, affecting roughly 350 million people (World Health Organization, 2012). In the United States, findings from the 2009– 2010 National Health and Nutrition Examination Survey (NHANES) indicated that 25.7% of the population aged 18 years and older (representing nearly 40 million U.S. adults) reported having depressive symptoms in the past 2 weeks (Wittayanukorn, Qian, & Hansen, 2014). More specifically, the first study to investigate national trends of maternal depression in the U.S. found that one in ten mothers from a sample of 8,916 ethnically diverse women suffered from past-year depression (Ertel, Rich-Edwards, & Koenen, 2011).
Depression is increasingly recognized as a significant source of burden for many individuals, especially when long-lasting and of moderate to severe intensity. Depression also has the potential of having a substantially negative impact on health-related quality of life for those affected by it (Coulehan, Schulberg, Block, Madonia, & Rodriguez, 1997). Individuals battling depression may exhibit negative affect, go about their daily lives with less energy, or interpret neutral situations more negatively than most people. These negative behaviors may, in turn, provoke reciprocal negative responses from people interacting with these individuals (Trevino, Wooten, & Scott, 2007).
Longitudinal Associations between Relationship Quality and Depressive Symptoms
For decades, researchers have explored the association between relationship quality and partner depressive symptoms through longitudinal examinations (Beach, Katz, Kim, & Brody, 2003; Beach & O’Leary, 1993; Davila, Karney, Hall, & Bradbury, 2003). Evidence has suggested that poor relationship quality predicts symptoms of depression in partners over time (Beach & O’Leary, 1993; Fincham, Beach, Harold, & Osborne, 1997). Choi and Marks (2008) used three waves of data from a nationally representative sample of older married adults to examine all possible bidirectional associations among marital conflict, depressive symtoms, and functional impairment. Consistent with prior studies, Choi and Marks (2008) found that marital conflict had a direct effect on partners’ increase in both depressive symptoms and physical health limitations. The effects, however, were not consistent across time lags.
In a similar study, relationship satisfaction and depressive symptoms were assessed longitudinally in a sample of 260 couples (Gustavson et al., 2012). Gustavson et al. (2012) began collecting data from couples when their child was 18-months-old and continued to interview the couple over a 16-year period at seven different timepoints. However, their examination of relationship quality and depressive symtoms focused only on data from waves six and seven that were collected two years apart. Findings from the study extended prior literature because of their examination of the dyadic view of the relationship as well as each partners’ individual view of their relationship. Gustavson et al. (2012) found that individual depressive symptoms that over time manifested behaviorally, for example, withdrawal and criticism, impacted both partners’ assessment of relationship quality.
Aside from studying the association between relationship quality and symptoms of depression in partners in general, researchers have specifically examined symtoms in women partners (Assh & Byers, 1996; Horwitz, Briggs-Gowan, Storfer-Isser, & Carter, 2007). One longitudinal study assessed maternal depression in over 3,694 women three to five days after giving birth, when the child was six months old, five years, and 14 years of age (Mamun et al., 2009). Researchers were interested in understanding the bidirectional effects that exist between marital quality and symptoms of depression. Results of the study indicated that negative changes, such as shifting from reporting no depressive symtoms to feeling depressed and from a good relationship to a not so good relationship, significantly impacted womens’ relationship quality and mental health. Mamun et al. (2009) concluded that over the 14-year follow-up, poor relationship quality led to depression and depression consistently led to poor relationship quality. Findings from these longitudinal examinations are consistent with the marital discord model, which indicates that facets of the marital relationship, including distressed interactions between couples, can play powerful roles in the development and maintenance of depressive symptomatology (Beach & Cassidy, 1991).
Studying the association between relationship quality and partner depressive symptoms longitudinally provides important implications for interventions that could positively influence relational processes. However, samples in each of the longitudinal studies mentioned above included mostly non-Hispanic White participants that are not representative of an ethnically diverse U.S. population. In addition, these samples were predominantly upper middle class, focused on dyads with college educations. A key limitation of prior longitudinal studies has been researchers’ inability to generalize their findings to ethnic minority populations that includes consideration of the unique stressors that characterize their lived experiences. For example, in a large, nationally representative sample of women, researchers found that relations between depressive symptoms, relationship status, and demographic variables differed between Black and White women (Jones-Webb & Snowden, 1993). Lower SES can place individuals at risk for experiencing more challenging functioning in partner relationships, which can activate or exacerbate depressive symptoms (Papp, 2010). This may be due, in part, to intensified daily challenges along with limited resources or ability to cope with difficulties (McLeod & Kessler, 1990; Santiago, Wadsworth, & Stump, 2011). Economic hardships can generate negative feelings, including anger, frustration, anxiety, and depression, which may be inappropriately expressed in interactions with those close to the person (Parke et al., 2004).
To confirm whether the patterns of association and factors influencing the associations are similar across ethnic groups, additional opportunities are needed to examine the experiences of non-White populations, particularly those of the two largest ethnic minority groups in the U.S., African Americans and Hispanics (Cummings et al., 2005; Whisman, 2001). Furthermore, more research is needed that includes women from lower SES groups given the unique stresors that affect this population. Therefore, this analysis sought to expand the current literature base by exploring associations between relationship quality and depressive symptoms among economically disadvantaged members of these two groups.
Specifically, this study sought to examine the concurrent and prospective associations between the quality of parental romantic partner relationships and depressive symptoms reported among low-income, African-American and Hispanic mothers of preschool children. Based on previous findings, the working hypothesis for this study was that lower quality parental romantic partner relationships will be prospectively associated with higher levels of depressive symptoms among these mothers. Furthermore, we hypothesized that depressive symptoms would be prospectively associated with pooer partner relationship quality. This examination will contribute to the paucity of research conducted to date to uncover patterns and influences of associations between romantic partner relationship quality and maternal depressive symptoms in these populations.
Method
The study presented here represents a secondary analysis of data drawn from a larger longitudinal study assessing self-regulation, executive functioning, and school readiness among low-income, ethnic minority children and their families residing in a large urban area in the southwestern United States (author reference). The sample for the parent study was limited to African Americans and Hispanics due to the disparities in school readiness experienced in these groups.
Families were recruited using numerous strategies such as outreach and distribution of study-related information to agencies and organizations serving low-income populations (e.g., WIC clinics, Head Start programs, day care centers, churches, community recreational centers). Project staff also directly recruited study participants from venues such as community fairs, grocery stores, or parks, or through word-of-mouth. All recruitment information was available in English and Spanish (a single flyer/postcard with a different language on each side), and the message on the study phone line was recorded in English and Spanish. In addition, half of the study’s recruitment team was bilingual. Study procedures were reviewed and approved by the institutional review boards of [author institution] and [author institution]. Consent forms were available in both English and Spanish and were reviewed with the participant at the time of the enrollment home visit.
A total of 407 children and their families (approximately 45% and 55%, African- American and Hispanic, respectively) were enrolled into the parent study. At the time of enrollment, target children were 2½ years old (Time 1), and follow-up data collection visits were held one year later (Time 2), when the target child entered formal schooling (Time 3), and one year later (Time 4).
Starting at Time 2, partnership relationship quality data were collected for all primary caregivers living with a spouse or partner. Of the 407 enrolled families, 366 (90%) were seen at Time 2 and of those, 237 mothers had a cohabiting partner or spouse. Demographic characteristics of this selected sample appear in Table 1. Compared to the overall sample in the parent study, individuals included in the analytic sample did not differ in terms of income, education, or age. However, those included in the sub-sample were significantly more likely to be married (80% vs. 56%) and Hispanic (70% vs. 48%). Half of the mothers in the selected sample were between the ages of 20–29, and maternal age did not differ significantly between African American and Hispanic mothers. African American mothers were less likely to be married over the entire study period (41%) compared to Hispanic mothers (78%). Approximately two-thirds of the mothers had a minimum of a high school diploma/GED, and over half of the sample (60%) had household incomes less than 100% of the federal poverty level. More than 85% of Hispanic mothers were foreign-born (the vast majority being from Mexico), with two- thirds speaking predominantly Spanish and approximately 28% bilingual.
Table 1.
Characteristics of sample (N = 237)
| Total Sample (n = 237) | African American (n = 71) | Hispanic (n = 166) | χ2 | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Age | 2.40 | |||
| <20 years | 7 (3.0) | 1 (1.4) | 6 (3.6) | |
| 20–29 | 119 (50.4) | 40 (57.1) | 79 (47.6) | |
| 30–39 | 97 (41.1) | 25 (35.7) | 72 (43.4) | |
| 40+ | 13 (5.5) | 4 (5.7) | 9 (5.4) | |
| Average Family Income | 42.23*** | |||
| <50% federal poverty level | 31 (13.2) | 22 (31.9) | 9 (5.4) | |
| 50–99% federal poverty level | 110 (46.8) | 23 (33.3) | 87 (52.4) | |
| 100–149% federal poverty level | 60 (25.5) | 8 (11.6) | 52 (31.3) | |
| 150–200% federal poverty level | 34 (12.2) | 16 (23.2) | 18 (10.8) | |
| Educational Attainment | 31.95*** | |||
| Less than high school | 83 (35.0) | 9 (12.7) | 74 (44.6) | |
| High school diploma/GED | 84 (35.4) | 25 (35.2) | 50 (35.5) | |
| More than high school | 70 (29.5) | 37 (52.1) | 33 (19.9) | |
| Relationship Status | 30.39*** | |||
| Married | 159 (67.1) | 29 (40.8) | 130 (78.3) | |
| Not married, but cohabitating | 34 (14.3) | 27 (38.0) | 7 (4.2) | |
| Marital status changed | 44 (18.6) | 15 (21.1) | 29 (17.5) | |
| Nativity/Born in the U.S. (Hispanics only) | ||||
| Yes | -- | -- | 24 (14.5) | |
| No | -- | -- | 142 (85.5) | |
| Language Proficiency (Hispanics only) | ||||
| English-dominant | -- | -- | 6 (3.6) | |
| Spanish-dominant | -- | -- | 110 (66.3) | |
| Bilingual | -- | -- | 46 (27.7) | |
Note. Balance of cases is missing.
p < .001
Procedures
As stated above, home visits were completed when the study child was 2½ years old (Time 1), 3½ years old (Time 2), when the child entered formal schooling (Time 3), and one year later (Time 4). Each visit was completed by a team of two home visitors with one home visitor conducting the parent interview while the other home visitor conducted assessments with the child. For Hispanic families, both home visitors were fully bilingual. All measures not available in Spanish were forwarded translated by one bilingual team member and then back-translated by two different bilingual team members, one of which was a native speaker. Differences were resolved by consensus. In addition, measures already available in Spanish were reviewed by bilingual team members to ensure that the language used was consistent with local idiomatic Spanish. The results utilized in the present analysis were collected during Times 2–4, when dyadic adjustment data were collected.
Measures
Partner relationship quality.
The Dyadic Adjustment Scale (DAS), one of the most widely used multidimensional measures of relationship quality in the behavioral and social sciences literature, was used to assess the quality and functioning of the primary caregiver’s partner relationships at each time point from Time 2 onwards (Graham & Liu, 2006; Spanier, 1976). This 32-item instrument specifically measures individuals’ perceptions of their relationship adjustment in the areas of: 1) troublesome dyadic differences; 2) interpersonal tensions and personal anxiety; 3) dyadic satisfaction; 4) dyadic cohesion; and 5) consensus on matters of importance to dyadic functioning (Spanier, 1976). The DAS is summed to yield a total score ranging from 0 to 151, with higher scores reflecting greater relationship satisfaction. Only the total score was used in the present analysis. Evidence from a reliability generalization meta- analysis by Graham, Liu, and Jeziorski (2006) indicated that the variability in DAS score reliability across studies is not explained by demographic characteristics such as gender, ethnicity, marital status, or sexual orientation. Therefore, total DAS scores are likely to be generalizable across diverse samples and population subgroups when examining relationship quality issues. In the present investigation, the internal reliability of the DAS ranged from .90 to .94 across the three waves, and internal reliability did not differ by ethnicity.
Of these 237 mothers, 153 (64.6%) had three data points of DAS data, 36 (15.2%) had two data points, and 48 (20.3%) had only one data point. Mothers with more dyadic adjustment data did not differ from those with less in terms of maternal education, but those mothers who provided more dyadic adjustment data came from households with significantly higher household incomes, F (2, 232) = 3.55, p < .05. Finally, Hispanic mothers were more likely to complete DAS assessments compared with African American mothers, χ2 (2) = 37.53, p < .001.
Maternal depressive symptoms.
Maternal depressive symptoms were assessed using a revised version of the Center for Epidemiologic Studies Depression (CESD-R) scale (Eaton, Smith, Ybarra, Muntaner & Tien, 2004). Total CESD-R scale scores range from 0 to 60, with higher scores reflecting more depressive symptomatology and scores of 16 or higher indicating significant depressive symptoms. Internal reliability of the CESD across waves ranged from .92 to .95 and did not differ by ethnicity.
Of these 237 mothers, 193 (81.4%) completed the depressive symptoms measure at each of the three time points, while 25 (10.5%) had two time points of depressive symptoms data, and 19 (8.0%) only had one time point of data. Those mothers with more depressive symptoms data did not differ from those with less in terms of household income and maternal education. However, Hispanic mothers were more likely to complete more CESD assessments compared with African American mothers, χ2 (2) = 10.98, p < .01.
Covariates.
Covariates included maternal age, family income, education, ethnicity, and partner relationships status. Family income at each of the four time points was used to calculate family income-to-needs ratio based on federal poverty levels for that year and family size, and the ratios were averaged to estimate average family income-to-needs ratio across the entire study period. Partner status at each time point was used to create covariates to control for whether the relationship was marital and whether the woman experienced a change in partner across the three time points.
Results
Intercorrelations between maternal depressive symptoms, partner relationship quality, and sociodemographic variables as well as descriptive statistics are displayed in Table 2. Both concurrent and prospective correlations between the CESD and DAS were in the expected direction, with higher levels of depressive symptoms associated with lower dyadic adjustment.
Table 2.
Intercorrelations and descriptive statistics for study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1 | CESD T2 | 1.00 | |||||||
| 2 | CESD T3 | .458** | 1.00 | ||||||
| 3 | CESD T4 | .360** | .659** | 1.00 | |||||
| 4 | DAS T2 | −.328** | −.244** | −.231** | 1.00 | ||||
| 5 | DAS T3 | −.160* | −.382** | −.377** | .471** | 1.00 | |||
| 6 | DAS T4 | −.220** | −.169* | −.393** | .526** | .592** | 1.00 | ||
| 7 | Family income | −.087 | −.122 | −.144* | .076 | .000 | −.045 | 1.00 | |
| 8 | Partner status | −.159* | −.024 | −.078 | .156* | .092 | .096 | .271** | 1.00 |
|
Descriptive Statistics | |||||||||
| Full Sample | |||||||||
| Mean | 5.45 | 5.62 | 5.96 | 120.18 | 121.01 | 121.63 | .97 | ||
| Standard deviation | 9.38 | 11.14 | 11.42 | 18.43 | 18.61 | 18.01 | .53 | ||
| African Americans | |||||||||
| Mean | 7.68 | 5.57 | 6.3 | 119.52 | 126.12 | 123.93 | .94 | ||
| Standard deviation | 12.51 | 12.7 | 11.47 | 19.77 | 14.04 | 14.78 | .72 | ||
| Hispanics | |||||||||
| Mean (SD) | 4.5 | 5.63 | 5.82 | 120.45 | 119.74 | 121.02 | .99 | ||
| Standard deviation | 7.5 | 10.55 | 11.45 | 17.9 | 19.42 | 18.78 | .42 | ||
| t | 2.00* | −.04 | .27 | −.35 | 1.83+ | .86 | −.43 | ||
Note. CESD = Center for Epidemiologic Studies Depression scale; DAS = Dyadic Adjustment Scale. Partner status = 1 if married at Time 1. Correlations for partner status are Spearman Rank coefficients.
p < .10;
p < .05;
p < .01.
African American women displayed significantly higher depressive symptoms at Time 2 but not at Times 3 and 4 relative to Hispanic women. Dyadic adjustment did not differ significantly by ethnicity. Depressive symptoms were slightly lower among married women at Time 2, but there were no differences in depressive symptoms by marital status at Time 3 or Time 4.
Longitudinal Associations Between Maternal Depressive Symptoms and Dyadic Adjustment
MPlus (1998) was used to fit a crossed lag-panel model in which the CESD and DAS at each time point were regressed on the associated values from the prior time point. The model was adjusted for household income, marital status, and changes in partner. Results of the lag- panel analysis are displayed in the Figure. Model fit indices indicated a good model fit, χ2 (14) = 33.55, p < .01; RMSEA = .077; CFI = .944; SRMR = .05. Concurrent assessments of depressive symptoms and dyadic adjustment were significantly and negatively correlated at each time point. Likewise, the autoregressive paths for both outcomes were significant and positive. Higher depressive symptoms predicted higher depressive symptoms as the subsequent time point, and higher relationship quality predicted higher relationship quality at the subsequent time point.
Figure.
Lag-panel analysis of the transactional relation between dyadic adjusting and depressive symptoms over time.
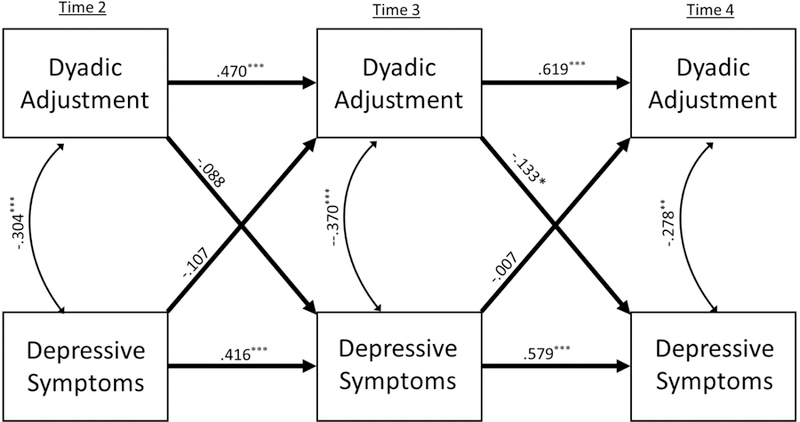
Note: Coefficients are standardized. Model adjusted for household income, marital status, and change in partner. Model fit: χ2 (14) = 33.55, p < .01; RMSEA = .077; CFI = .944; SRMR = .050. Adding 2nd degree lags (W2->W4) did not significantly improve model fit.
In terms of the cross-lagged paths, there was a significant and negative association between the DAS at Time 3 and the CESD at Time 4, in that a higher level of partner relationship quality at Time 3 was associated with fewer depressive symptoms at Time 4. The cross-lagged path from Time 2 DAS to Time 3 CESD was not significant. However, the indirect effect of Time 2 DAS on Time 4 CESD was significant via effects on Time 3 DAS, standardized coefficient for the indirect effect = −.097, se(B) = .037, t = −2.62, p < .01. Notably, none of the cross-lagged paths from the CESD to the DAS were significant, suggesting that partner relationship problems did not increase subsequent depressive symptoms.
To examine the possibility of ethnic differences, we fit a multiple group lagged-panel model. Any coefficients that appeared to differ were tested in a pairwise fashion, in which the pair of coefficients was fixed to be equal across groups, and the change in the chi-square model fit was examined. If the change in model fit was significant, this would suggest that the two coefficients differed significantly across groups. However, none of the pairwise comparisons was significant, suggesting that the lag-panel model did not differ significantly by maternal ethnicity.
Discussion
This analysis focused on longitudinal associations between parental partner romantic relationship quality and depressive symptoms reported among low-income African American and Hispanic mothers of young children. The study’s working hypothesis was that lower quality relationships would be prospectively associated with higher levels of depressive symptoms among these mothers. Likewise, we hypothesized that depressive symptoms would exacerbate relationship issues. Our findings supported our first hypothesis, that higher partner relationship distress was associated with higher subsequent levels of maternal depressive symptoms. These findings are consistent with other findings in the literature for non-Hispanic White dyads that supports both concurrent associations between partner relation distress and depressive symptoms (Cummings et al., 2005; Papp, Goeke-Morey, & Cummings, 2007b; Parker et al., 2012; Proulx et al., 2007; Røsand et al., 2012) as well as reports that partner relationship quality prospectively predicts increased depressive symptoms (Beach & O’Leary, 1993; Choi & Marks, 2008; Fincham et al., 1997).
Our second hypothesis, however, was not supported in that partner distress was not prospectively associated with increased depressive symptoms. The marital discord model (Beach & O’Leary, 1993) proposes that bidirectional relations between partner distress and psychological well-being are to be expected. However, findings in the literature regarding this bidirectional relation have been mixed. Fincham et al. (1997) found that depressive symptoms predicted compromised marital relationships for men but not women. In contrast, Choi and Marks (2008) found bidirectional relations between depressive symptoms and partnership quality for both men and women in a large, predominantly White U.S. sample. Similar bidirectional relations have been reported in a Norwegian sample of couples (Gustavson et al., 2012; Mamun et al., 2009). As far as we know, ours is the only study examining these relations in a low- income, ethnic minority sample. More research is needed using ethnically and economically diverse samples to clarify whether these effects are unidirectional (e.g., relationship distress prospectively associated with increased psychological distress) or bidirectional (relationship distress and psychological distress mutually exacerbate one another).
Bivariate analyses indicated that higher levels of depressive syptoms of African American women early in the study but not thereafter. Likewise, there were no differences in partner relationship satisfaction between African American and Hispanic women. In this sample, approximately 41% of African Americans reported being married across the course of the study compared with 78% of Hispanic women. Likewise, differences in psychological well-being associated with marital status were minimal in this sample. As previously discussed, empirical evidence consistently points to numerous financial and health benefits derived from marital unions (Marcussen, 2005; Simon, 2002). Additionally, while a more limited number of studies focused on unmarried romantic relationships has provided mixed findings. The studies, including ones that examine stable cohabitating parents (e.g., Klausli & Owen, 2009) indicate non-marital relationships enjoy less psychological benefits than do those of married couples. For instance, some studies have shown that cohabiting couples report less happiness and higher levels of depression than do married individuals (Brown et al., 2003; Marcussen, 2005). Others have indicated similar levels, with both groups having better outcomes than single individuals (Ross, 1995).
In contrast, our findings did not find consistent differences in psychological well-being between women in our sample who were married versus those who were not married but co- habitating. As stated previously, the majority of this research is based in White, middle-class samples of couples, whereas our study is focused on low-income ethnic minority women and their partners. Future research is needed to determine if our findings are replicated with other samples of low-income ethnic minority dyads as well as with more economically diverse ethnic minority dyads. It may be that within a low-income setting, the social support provided by having a residential partner is more important than whether the relationship is marital or not.
There are a few limitations to the present study that should be kept in mind when interpreting the results. Families included were predominantly low-income, thus limiting generalizability to more economically diverse populations. Furthermore, partner data were only collected from participants who had a co-resident partner. As such, these data do not represent the full range of partner relationships in which low-income ethnic minority woman participate. Another limitation of the study is that data on depressive symptoms were obtained via self- report, with no clinical diagnoses backing up the measure of depressive symptoms or the findings related to maternal depressive symptoms. In addition, measures of depressive symptoms and relationship quality were both obtained from the woman, which may have artificially inflated the association between the two due to same-source bias. Finally, among the Hispanic individuals participating in the study, over 95% were from Mexico, which limits generalizability for populations from other Spanish-speaking countries.
Results from the current study support the need for an emphasis on the role partner relationship quality for depressive symptoms among mothers of young children, including in low-income, ethnic minority populations. This is especially important because the prevalence of depression is particularly high in low-income, socially disadvantaged women of color, including mothers with small children and those of childbearing/childrearing age, with estimates as high as 25% (Cummings et al., 2005; Mendes et al., 2012; Weissman & Olfson, 1995). The exacerbated inequalities that these women face due to poverty can increase their vulnerability to depression. These experiences may include racism or discrimination, acculturation challenges, linguistic barriers, cultural norms that stigmatize discussing or seeking professional help, socioeconomic pressures, lack of health insurance, limited access to health care services, and/or perceptions of unsupportive attitudes from providers when care is actually sought (Brown, Abe-Kim, & Barrio, 2003; Ertel, Rich-Edwards, & Koenen, 2011; Lazear, Pires, Isaacs, Chaulk, & Huang, 2008).
Previous studies have found that negative effects from exposure to either poor maternal psychological states or parental relationship distress and challenges can occur very early in a child’s life and cause disturbances in attachment, expressive language development, and emotional self-regulation among children. Additionally, because most child caregivers are women, developing ways to intervene or mitigate negative effects will be important to improving the quality of life of both the primary caregivers and the care, attention, and emotional support conveyed to their children to thwart later negative outcomes and problem behaviors.
Contributor Information
Alicia L. Thomas, University of Texas School of Public Health
Margaret Tresch Owen, University of Texas at Dallas.
References
- Assh SD, & Byers ES (1996). Understanding the Co-Occurrence of Marital Distress and Depression in Women. Journal of Social and Personal Relationships, 13, 537–552. doi: 10.1177/0265407596134004 [DOI] [Google Scholar]
- Beach SR, & Cassidy JF (1991). The marital discord model of depression. Comprehensive Mental Health Care, 1, 119–136. [Google Scholar]
- Beach SRH, Katz J, Kim S, & Brody GH (2003). Prospective effects of marital satisfaction on depressive symptoms in established marriages: A dyadic model. Journal of Social and Personal Relationships, 20, 355–371. doi: 10.1177/0265407503020003005 [DOI] [Google Scholar]
- Beach SRH, & O’Leary KD (1993). Marital discord and dysphoria: For whom does the marital relationship predict depressive symptomatology? Journal of Social and Personal Relationships, 10, 405–420. doi: 10.1177/0265407593103007 [DOI] [Google Scholar]
- Brown C, Abe-Kim JS, & Barrio C (2003). Depression in ethnically diverse women: Implications for treatment in primary care settings. Professional Psychology: Research and Practice, 34, 10–19. 10.1037/0735-7028.34.1.10 [DOI] [Google Scholar]
- Cherlin A (2010). Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and the Family, 72, 403–419. 10.1111/j.1741-3737.2010.00710.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi H, & Marks NF (2008). Marital conflict, depressive symptoms, and functional impairment. Journal of Marriage and Family, 70, 377–390. 10.1111/j.1741-3737.2008.00488.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulehan JL, Schulberg HC, Block MR, Madonia MJ, & Rodriguez E (1997). Treating depressed primary care patients improves their physical, mental, and social functioning. Archives of Internal Medicine, 157, 1113–1120. 10.1001/archinte.1997.00440310079008 [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, & Davies PT (2005). Towards a family process model of maternal and paternal depressive symptoms: exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 46, 479–489. 10.1111/j.1469-7610.2004.00368.x [DOI] [PubMed] [Google Scholar]
- Davila J, Karney BR, Hall TW, & Bradbury TN (2003). Depressive symptoms and marital satisfaction: within-subject associations and the moderating effects of gender and neuroticism. Journal of Family Psychology, 17, 557–570. doi: 10.1037/0893-3200.17.4.557 [DOI] [PubMed] [Google Scholar]
- Dehle C, & Weiss RL (1998). Sex differences in prospective associations between marital quality and depressed mood. Journal of Marriage and Family, 60, 1002–1011. 10.2307/353641 [DOI] [Google Scholar]
- Dush CMK (2005). Consequences of relationship status and quality for subjective well- being. Journal of Social and Personal Relationships, 22, 607–627. 10.1177/0265407505056438 [DOI] [Google Scholar]
- Eaton WW, Smith C, Ybarra M, Muntaner C, & Tien A (2004). Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESDR). In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcome assessment. Instruments for adults (Third, pp. 363–378). Mahwah, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Ensminger ME, Hanson SG, Riley AW, & Juon H-S (2003). Maternal psychological distress: Adult sons’ and daughters’ mental health and educational attainment. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1108–1115. 10.1097/01.CHI.0000070261.24125.F8 [DOI] [PubMed] [Google Scholar]
- Ertel KA, Rich-Edwards JW, & Koenen KC (2011). Maternal depression in the United States: Nationally representative rates and risks. Journal of Women’s Health (2002), 20, 1609–1617. 10.1089/jwh.2010.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan J (2009). Relationship quality and changes in depressive symptoms among urban, married African Americans, Hispanics, and Whites. Family Relations, 58, 259–274. 10.1111/j.1741-3729.2009.00551.x [DOI] [Google Scholar]
- Fincham FD, Beach SRH, Harold GT, & Osborne LN (1997). Marital satisfaction and depression: different causal relationships for men and women? Psychological Science, 8, 351–356. doi: 10.1111/j.1467-9280.1997.tb00424.x [DOI] [Google Scholar]
- Graham JM, Liu YJ, & Jeziorski JL (2006). The Dyadic Adjustment Scale : A reliability generalization meta-analysis. Journal of Marriage and Family, 68, 701–717. 10.1111/j.1741-3737.2006.00284.x [DOI] [Google Scholar]
- Gustavson K, Røysamb E, Soest T. v., Helland MJ, Karevold E, & Mathiesen KS (2012). Reciprocal longitudinal associations between depressive symptoms and romantic partners’ synchronized view of relationship quality. Journal of Social and Personal Relationships, 29, 776–794. doi: 10.1177/0265407512448264 [DOI] [Google Scholar]
- Hammen C, & Brennan PA (2003). Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry, 60, 253–258. 10.1001/archpsyc.60.3.253 [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Briggs-Gowan MJ, Storfer-Isser A, & Carter AS (2007). Prevalence, correlates, and persistence of maternal depression. Journal of Women’s Health, 16, 678–691. doi: 10.1089/jwh.2006.0185 [DOI] [PubMed] [Google Scholar]
- Jones-Webb RJ, & Snowden LR (1993). Symptoms of depression among blacks and whites. American Journal of Public Health, 83, 240–244. 10.2105/AJPH.83.2.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klausli J, & Owen MT (2009). Maternal cohabitation and characteristics of the home environment across the child’s first two years. Journal of Family Psychology, 23, 103–106. doi: 10.1037/a0014588 [DOI] [PubMed] [Google Scholar]
- Lazear KJ, Pires SA, Isaacs MR, Chaulk P, & Huang L (2008). Depression among low-income women of color: Qualitative findings from cross-cultural focus groups. Journal of Immigrant and Minority Health / Center for Minority Public Health, 10, 127–133. 10.1007/s10903-007-9062-x [DOI] [PubMed] [Google Scholar]
- Leach LS, Butterworth P, Olesen SC, & Mackinnon A (2013). Relationship quality and levels of depression and anxiety in a large population-based survey. Social Psychiatry and Psychiatric Epidemiology, 48, 417–425. 10.1007/s00127-012-0559-9 [DOI] [PubMed] [Google Scholar]
- Lee GR, & Payne KK (2010). Changing marriage patterns since 1970: What’s going on, and why? Journal of Comparative Family Studies, 41, 537–556. doi: https://www.jstor.org/stable/41604567 [Google Scholar]
- Marcussen K (2005). Explaining differences in mental health between married and cohabiting individuals. Social Psychology Quarterly, 68, 239–257. 10.1177/019027250506800304 [DOI] [Google Scholar]
- Mamun AA, Clavarino AM, Najman JM, Williams GM, O’Callaghan MJ, & Bor W (2009). Maternal depression and the quality of marital relationship: A 14-year prospective study. Journal of Women’s Health, 18, 2023–2031. doi: 10.1089/jwh.2008.1050 [DOI] [PubMed] [Google Scholar]
- McLeod JD, & Kessler RC (1990). Socioeconomic status differences in vulnerability to undesirable life events. Journal of Health and Social Behavior, 31, 162–172. 10.2307/2137170 [DOI] [PubMed] [Google Scholar]
- Mendes AV, Loureiro SR, Crippa JA, de Meneses Gaya C, García-Esteve L, & Martín- Santos R (2012). Mothers with depression, school-age children with depression? A systematic review. Perspectives in Psychiatric Care, 48, 138–48. 10.1111/j.1744-6163.2011.00318.x [DOI] [PubMed] [Google Scholar]
- Muthen LL, & Muthen BO (1998). MPlus: The comprehensive modeling program for applied researchers. User’s guide Los Angeles: Muthen and Muthen. [Google Scholar]
- Olin GV, & Fenell DL (1989). The relationship between depression and marital adjustment in a general population. Family Therapy, 16, 11–20. [Google Scholar]
- Papp LM (2010). The course and quality of intimate relationships among psychologically distressed mothers. The American Journal of Orthopsychiatry, 80, 71–79. 10.1111/j.1939-0025.2010.01008.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papp LM, Goeke-Morey MC, & Cummings EM (2007a). Linkages between spouses’ psychological distress and marital conflict in the home. Journal of Family Psychology, 21, 533–537. https://doi.org/10.1037/0893-3200.21.3.533 [DOI] [PubMed] [Google Scholar]
- Papp LM, Goeke-Morey MC, & Cummings EM (2007b). Linkages between spouses’ psychological distress and marital conflict in the home. Journal of Family Psychology, 21, 533–537. [DOI] [PubMed] [Google Scholar]
- Parke RD, Coltrane S, Duffy S, Buriel R, Dennis J, Powers J, … Widaman KF (2004). Economic stress, parenting, and child adjustment in Mexican American and European American families, 75, 1632–1656. DOI: 10.1111/j.1467-8624.2004.00807.x [DOI] [PubMed] [Google Scholar]
- Parker ML, Tambling RB, & Campbell K (2012). Dyadic adjustment and depressive symptoms: The mediating role of attachment. The Family Journal, 21, 28–34. 10.1177/1066480712456674 [DOI] [Google Scholar]
- Petterson SM, & Albers AB (2001). Effects of poverty and maternal depression on early child development. Child Development, 72, 1794–1813. 10.1111/1467-8624.00379 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. 10.3102/10769986031004437 [DOI] [Google Scholar]
- Proulx CM, Helms HM, & Buehler C (2007). Marital quality and personal well-being: a meta-analysis. Journal of Marriage and Family, 69, 576–593. doi: 10.1111/j.1741-3737.2007.00393.x [DOI] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, & McGinn MM (2014). Marital quality and health: A meta-analytic review. Psychological Bulletin, 140, 140–187. 10.1037/a0031859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røsand G-MB, Slinning K, Eberhard-Gran M, Røysamb E, & Tambs K (2012). The buffering effect of relationship satisfaction on emotional distress in couples. BMC Public Health, 12, 66 10.1186/1471-2458-12-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE (1995). Reconceptualizing marital status as a continuum of social attachment. Journal Of Marriage And The Family, 57, 129–140. doi: 10.2307/353822 [DOI] [Google Scholar]
- Santiago CD, Wadsworth ME, & Stump J (2011). Socioeconomic status, neighborhood disadvantage, and poverty-related stress: Prospective effects on psychological syndromes among diverse low-income families. Journal of Economic Psychology, 32, 218–230. 10.1016/j.joep.2009.10.008 [DOI] [Google Scholar]
- Simon RW (2002). Revisiting the relationships among gender, marital status, and mental health. AJS; American Journal of Sociology, 107, 1065–1096. 10.1086/339225 [DOI] [PubMed] [Google Scholar]
- Spanier GB (1976). Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family, 38, 15–28. 10.2307/350547 [DOI] [Google Scholar]
- Trevino YA, Wooten HR, & Scott RE (2007). A correlational study between depression and marital adjustment in Hispanic couples. The Family Journal, 15, 46–52. 10.1177/1066480706294033 [DOI] [Google Scholar]
- Vespa BJ, Lewis JM, Kreider RM, & Vespa Jonathan; Lewis JM; Kreider RM (2013). America’s families and living arrangements : 2012 population characteristics U.S. Census Bureau, 1–34. Retrieved from http://www.census.gov/prod/2013pubs/p20-570.pdf
- Weissman M, & Olfson M (1995). Depression in women: Implications for health care research. Science, 269, 799–801. doi: 10.1126/science.7638596 [DOI] [PubMed] [Google Scholar]
- Whisman MA (2001). The association between depression and marital dissatisfaction. In Marital and family processes in depression: A scientific foundation for clinical practice (pp. 3–24). Washington, DC: American Psychological Association; 10.1037/10350-001 [DOI] [Google Scholar]
- Wittayanukorn S, Qian J, & Hansen RA (2014). Prevalence of depressive symptoms and predictors of treatment among U.S. adults from 2005 to 2010. General Hospital Psychiatry 36, 330–336. 10.1016/j.genhosppsych.2013.12.009 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2012). Depression Retrieved from http://www.who.int/mediacentre/factsheets/fs369/en/


