Abstract
A 6-day-old female presented to a pediatric cardiologist with tachypnea. A computed tomography angiogram of the chest showed partial anomalous pulmonary venous return, a pulmonary sequestration, and a horseshoe lung. Depicted here are radiographic findings which display this rare combination. This case demonstrates the need for the radiologist to consider additional abnormalities in the setting of anomalous pulmonary venous return.
Keywords: Congenital venolobar syndrome, Horseshoe lung, Pulmonary sequestration
Introduction
Congenital pulmonary venolobar syndrome is a type of partial anomalous pulmonary venous return in which the affected lung is hypoplastic and is drained by an anomalous vein into the systemic venous system [1]. Pulmonary sequestration is the aberrant formation of lung tissue that has no connection to the bronchial tree or pulmonary arteries. A horseshoe lung represents a band of pulmonary parenchyma extending between the right and left lungs [2].
Partial pulmonary venous has an incidence of approximately 1-3 in 100,000 live births with pulmonary sequestration manifesting in approximately 1 in 1000 of live births. Horseshoe lung is also uncommon with an unknown incidence. Presented here is a situation in which all 3 conditions manifest in concert [3].
Case report
A term female infant was born at full term and discharged a day following delivery. Pertinent medical history included an abnormal fetal magnetic resonance imaging, though the magnetic resonance imaging was performed at an outside facility and not available for review. An antenatal echocardiogram suggested a partial anomalous pulmonary venous return, moderate perimembranous ventricular septal defect, and possible major aortopulmonary collateral vessels. A routine well-child check-up shortly after discharge revealed that the patient had regained her birth weight and had been voiding and stooling normally.
At 6 days of life, the infant presented to cardiology clinic due to tachypnea. The tachypnea was initially only observed during feedings in the first few days of life, but it worsened and became apparent more regular. At the time of presentation to the cardiology clinic, there was no associated cyanosis or diaphoresis. There were intermittent suprasternal and subcostal retractions.
Upon presentation to the cardiology clinic, the patient's vital signs were 2.76 kg, height 49 cm, blood pressure 92/63 mm Hg, heart rate 158 bpm, and respiratory rate 100, which decreased to the 50s transiently during the visit. Oxygen saturation was 97%.
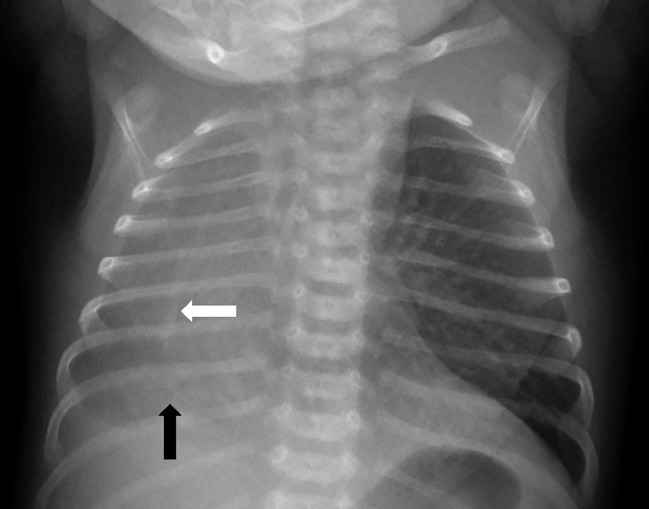
A chest radiograph was performed that showed a hypoplastic right lung with mediastinal shift to the right and pulmonary vascular congestion of the left lung (Fig. 1). No pleural effusion was seen.
Fig. 1.
Chest radiograph. There is right mediastinal shift with diffuse opacity throughout the right hemithorax (black arrow) and an abnormal vascular structure in the lower right lung (white arrow).
The patient was treated with furosemide and followed up 2 days later at which time her breathing had improved. She showed improved coordination with breast feeding and did not demonstrate any choking episodes.
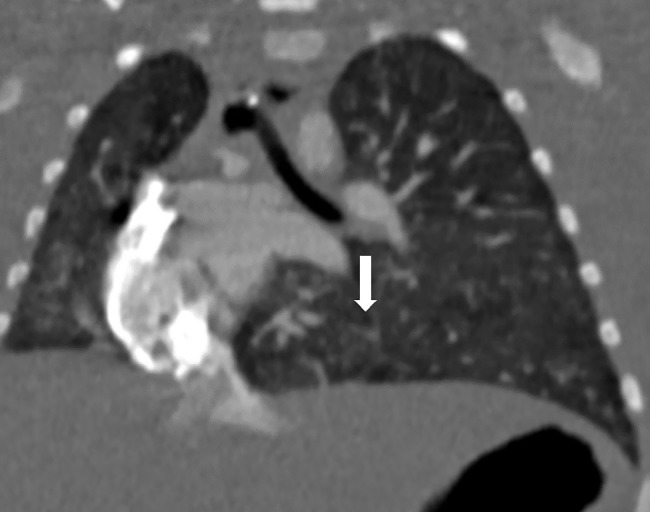
A cardiac computed tomography performed during the second week of life showed 2 anomalous veins draining into the inferior vena cava (Fig. 2). A well-defined pulmonary sequestration was apparent in the right lower lobe (Fig. 3). The pulmonary sequestration was fed by an arterial branch from the aorta (Fig. 2). Lung tissue was continuous across the inferior mediastinum in a horseshoe configuration (Fig. 4).
Fig. 2.
Three-dimensional reformat of the major vascular structures viewed from the posterior to highlight the right lung vascularity. The right lung is on the right. The normal pulmonary venous system is shown in purple. The aorta is red with a prominent aortic branch feeding the right lower lobe sequestration. The anomalous pulmonary veins are shown in blue. (Color version of figure is available online.)
Fig. 3.
Coronal reformat of a CT angiogram of the chest shows a pulmonary sequestration in the right lower lobe (black arrow). An anomalous draining pulmonary vein is indicated by the white arrow.
Fig. 4.
Coronal CT through the lower chest demonstrates continuous pulmonary tissue across the posterior mediastinum (white arrow).
The left lung exhibited normal venous drainage with 2 pulmonary veins connecting to the left atrium. There were 2 anomalous veins draining from the right lung to the intrahepatic inferior vena cava. The medial segment of the right lung was drained by a pulmonary vein connected to the left atrium. The majority of the hypoplastic right lung was drained via the abnormal (“scimitar”) veins. The isthmus of the horseshoe was drained into the left atrium through what appeared to be the left inferior pulmonary vein. The trachea was normal in caliber. There was an abnormal right bronchial branching pattern with an anomalous configuration of secondary bronchi as a result of the altered anatomy in the right lung. The left lung exhibited normal bronchial anatomy.
Discussion
Congenital pulmonary venolobar syndrome is a type of partial anomalous pulmonary venous return in which a hypoplastic lung is drained by an anomalous vein into the systemic venous system. Most commonly, the vein drains into the inferior vena cava as in the case presented here. This causes an acyanotic left to right shunt which is typically surgically corrected if symptomatic. The correction involves constructing an interatrial baffle to redirect the pulmonary venous return into the left atrium or reimplanting the anomalous vein into the left atrium.
Pulmonary sequestration is the aberrant formation of lung tissue which is not connected to the bronchial tree or pulmonary arteries. The condition predisposes the patient to hemoptysis or infections. These are the main reasons for surgical resection [4], [5].
Horseshoe lung occurs when a band of pulmonary parenchyma communicates between the right and left lungs with the formation of a single pleural cavity. This means if there were a pneumothorax, it would affect both lungs. Most cases of horseshoe lung published in the literature occur in the setting of additional pulmonary malformations such as either of the comorbid conditions in this patient. The combination of all 3 disorders is rarer.
These findings are important for the radiologist to recognize as each individual finding has its own inherent risks. When occurring together, the patient's prognosis, treatment, and surgical approach may be affected.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Konen E., Raviv-Zilka L., Cohen R.A., Epelman M., Bar-Ziv J., Hegesh J. Congenital pulmonary venolobar syndrome: spectrum of helical CT findings with emphasis on computerized reformatting. Radiographics. 2003;23(5):1175–1184. doi: 10.1148/rg.235035004. [DOI] [PubMed] [Google Scholar]
- 2.Frank J.L., Poole C.A., Rosas G. Horseshoe lung: clinical, pathologic, and radiologic features and a new plain film finding. AJR Am J Roentgenol. 1986;146(2):217–226. doi: 10.2214/ajr.146.2.217. [DOI] [PubMed] [Google Scholar]
- 3.Bhardwaj H., Bhardwaj B. A rare case of scimitar syndrome with horseshoe lung. Eur Respir Rev. 2014;23(131):153–154. doi: 10.1183/09059180.00005213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schramel F.M., Westermann C.J., Knaepen P.J., van den Bosch J.M. The scimitar syndrome: clinical spectrum and surgical treatment. Eur Respir J. 1995;8(2):196–201. doi: 10.1183/09031936.95.08020196. [DOI] [PubMed] [Google Scholar]
- 5.Vida V.L., Padalino M.A., Boccuzzo G., Tarja E., Berggren H., Carrel T. Scimitar syndrome: a European Congenital Heart Surgeons Association (ECHSA) multicentric study. Circulation. 2010;122(12):1159–1166. doi: 10.1161/CIRCULATIONAHA.109.926204. [DOI] [PubMed] [Google Scholar]