Abstract
We report a case of a 66-year-old woman who presented with acute shoulder pain. Initial radiographs revealed a sclerotic intraosseous lesion in the greater tuberosity with associated cortical erosions and subacromial calcification. The diagnosis of intraosseous calcific tendinitis was confirmed with additional magnetic resonance imaging and nuclear medicine imaging. Within 3 months of conservative measures, the patient's symptoms improved but the radiographic appearance had become more aggressive with a wider zone of transition. After 1 year, the imaging findings continued to change, with the development of subcortical cysts. Correct diagnosis of this uncommon manifestation of tendinitis requires knowledge of how its appearance changes with time.
Keywords: Calcific tendinitis, Intraosseous migration
Introduction
Calcific tendinitis is a common self-limiting cause of musculoskeletal pain caused by intratendinous deposits of calcium, primarily in the form of hydroxyapatite [1]. Unusual imaging manifestations of this condition can be challenging to diagnose. One such manifestation is cortical erosion at the greater tuberosity [2], [3]. Rarer still, intratendinous calcifications can penetrate and focally accumulate within adjacent bone, resulting in a mass-like sclerotic lesion [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15]. This intraosseous form of calcific tendinitis of the shoulder is important to recognize because it can mimic infection and neoplasm.
Uncertainty about the change with time in the radiographic appearance of this rare entity contributes to the diagnostic challenge, particularly in patients only imaged months after the acute onset of symptoms. The aim of this case report is 2-fold:
-
1.
to correlate the imaging findings of intraosseous calcific tendinitis of the shoulder using multiple modalities: radiographs, magnetic resonance imaging (MRI), and nuclear medicine;
-
2.
to characterize the interval changes of its radiographic appearance at the acute presentation, after 3 months, and after 1 year.
Case report
A 66-year-old female presented to the emergency department with acute worsening of chronic pain to the left shoulder. She had not experienced an acute injury and could not explain the cause of her worsening symptoms. Examination revealed limited active and passive range of motion due to pain, symptoms worsened primarily with abduction.
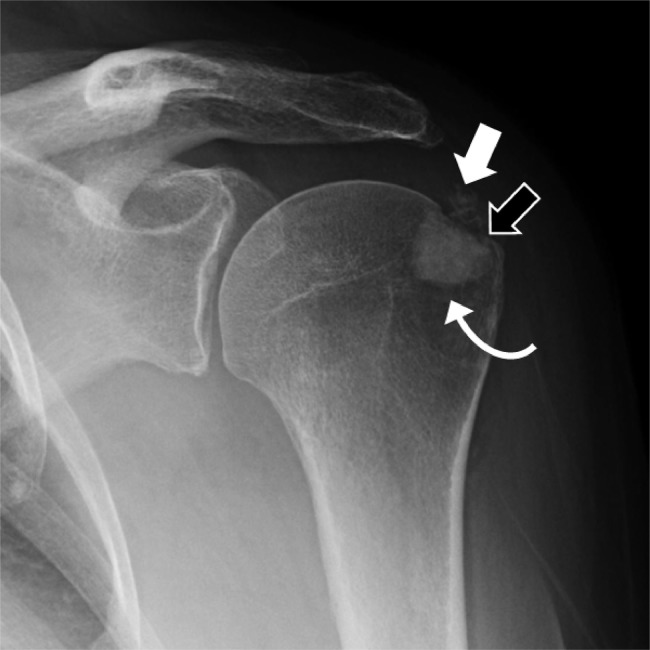
The initial X-ray imaging revealed irregular calcification along the distal rotator cuff, consistent with calcific tendinitis (Fig. 1). In addition, the radiographs showed a 1.6-cm region of sclerosis at the greater tuberosity, associated with cortical erosion. It was well circumscribed with a narrow zone of transition. The differential diagnosis was broad including intraosseous calcific tendinitis, bone island, osteoid osteoma, infection, and osteoblastic metastases, most commonly from breast, prostate, and lung cancer [4], [8].
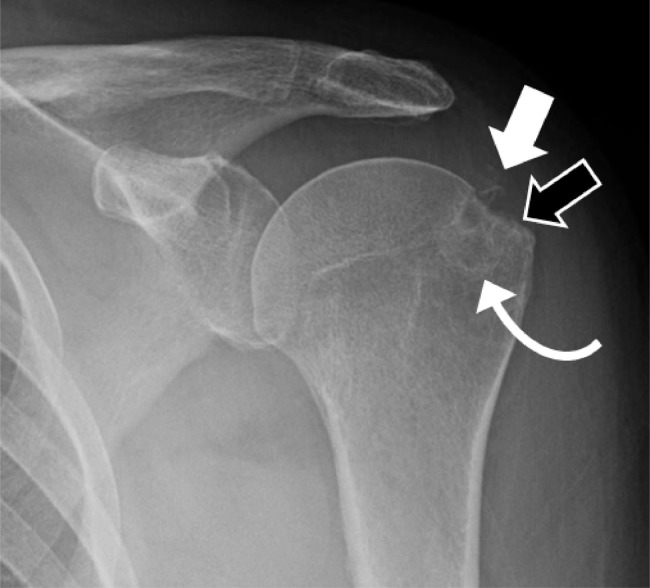
Fig. 1.
A 66-year-old female presents with acute-on-chronic left shoulder pain and no history of trauma. Radiographs at the time of acute presentation show amorphous calcifications in the subacromial space (white arrow), cortical erosion (black arrow), with an underlying ovoid sclerotic lesion in the greater tuberosity (curved arrow).
The patient was treated with Toradol 30-mg intramuscular injection (IM), with good effect and was discharged with a prescription for PO naproxen. Following the initial radiographs (Fig. 1), an MRI (Fig. 2) and bone scan (Fig. 3) were ordered to further characterize the lesion. Both tests were performed within 10 days of the radiographs.
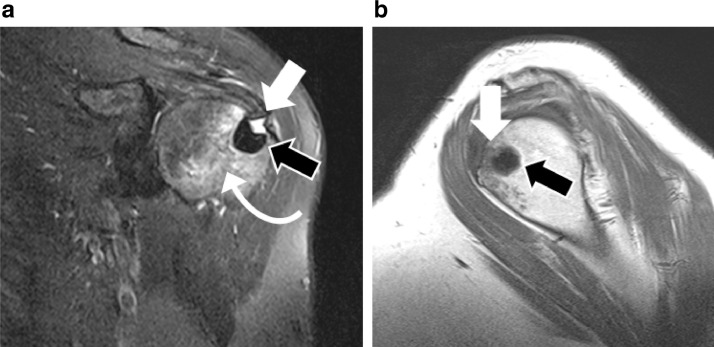
Fig. 2.
MRI acquired 1 week after acute presentation. Coronal fat-suppressed T2-weighted sequence (a) shows low signal intensity of the ovoid lesion in the greater tuberosity in keeping with sclerosis (black arrow). This is a superficial focus of fluid signal (white arrow) traversing the region of cortical erosions, which were evident on the prior radiographs (black arrow in Fig. 1). Ill-defined hyperintensity consistent with marrow edema (curved arrow) surrounds the lesion. Sagittal T1-weighted sequence (b) shows the low signal intensity sclerotic lesion (black arrow), with focal superficial intermediate signal (white arrow).
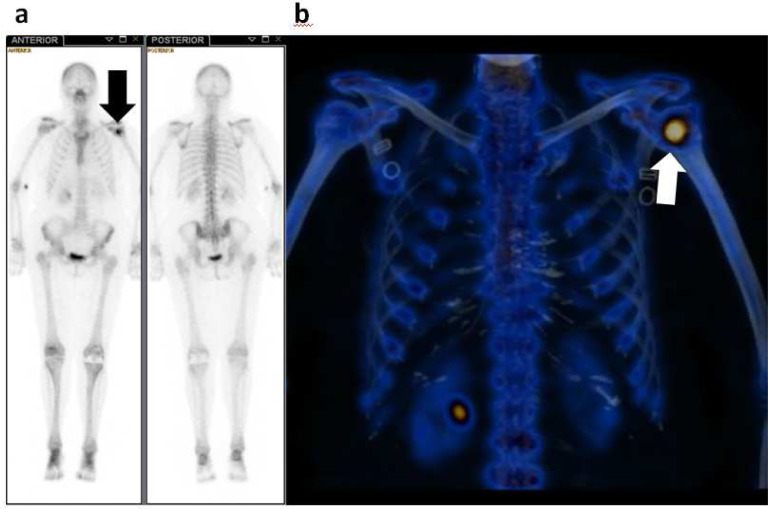
Fig. 3.
Tc-99m whole-body bone scan (a) acquired 1 week after acute presentation shows focal activity apart from the left proximal humerus (black arrow), with no further abnormal activity throughout the body. The 3D reformations of fused SPECT-CT images (b) localize this intense activity to the left greater tuberosity (white arrow).
The MRI images demonstrated the ovoid subcortical lesion in the greater tuberosity to have signal intensity on both T1- and T2-weighted sequences consistent with sclerosis (Fig. 2, black arrow). There was mild marrow edema signal surrounding the lesion. The supraspinatus tendon was thickened, demonstrating acute tendinitis, with subtle multifocal intrinsic low signal corresponding to the calcification better seen on radiographs (Fig. 1, white arrow). Tendinous involvement helps distinguish from other diagnostic considerations causing sclerotic lesions such as bone islands. There was no associated soft tissue mass or intramuscular signal abnormality, thereby excluding a soft tissue malignancy. The only extraosseous signal abnormality on the MRI was a focal rim of T1-hypointense and T2-hyperintense signal, matching that of complex fluid, penetrating the cortical surface into the footplate of the supraspinatus tendon. Osteomyelitis is a consideration for any tract of fluid signal in bone breaching the cortical surface [11], which was why clinical history was critically important to exclude infection in this case. The location of the focal fluid signal, bridging the thickened supraspinatus tendon and the lesion in the greater tuberosity, likely demonstrated the active process of calcification migrating into bone.
Tc-99m whole-body scintigraphy and fused Single-photon emission computed tomography (SPECT-CT) was performed within several days of the MRI. Figure 3a and b shows the intense activity at the left greater tuberosity. One of the entities on our differential diagnosis from the initial radiograph, a bone island, could be reasonably excluded, because bone islands are not typically metabolically active [7]. The scan also confirmed this was a solitary lesion, making metastatic disease less likely, particularly in the absence of a known primary malignancy.
The combined findings of clinical history, physical examination, and imaging were pathognomonic for the intraosseous migration of calcific tendinitis. The patient was treated with conservative measures including anti-inflammatories, intra-articular steroid injections, and physiotherapy. One month later, complete range of motion was restored with the patient experiencing minimal discomfort.
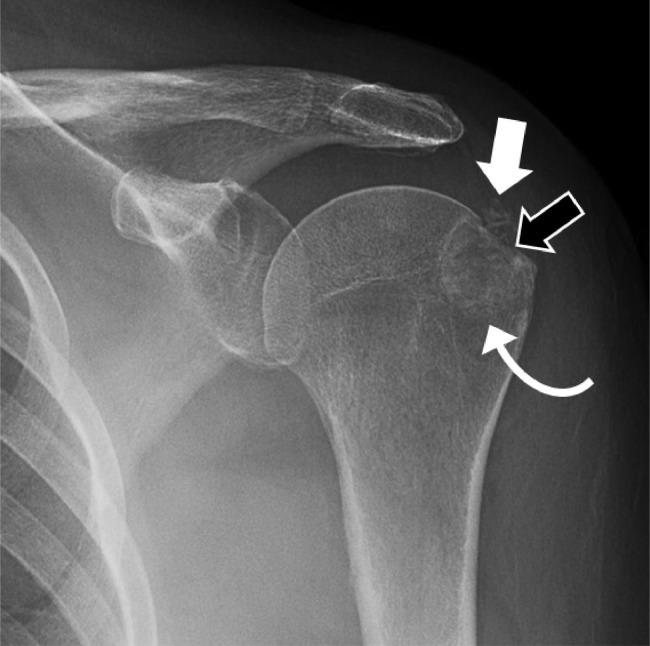
Radiographs 3 months after the initial presentation (Fig. 4) showed significant changes in the appearance of the intraosseous lesion in the greater tuberosity (curved arrow). The lesion was no longer purely sclerotic, now mixed sclerotic-lytic, with a zone of transition (ie, the interface between the lesion and normal-appearing bone) that is wide and ill-defined [8]. The calcifications in the subacromial space (white arrow) and the cortical erosion (black arrow) persisted unchanged.
Fig. 4.
Follow-up radiographs performed 3-months after initial presentation show the greater tuberosity lesion now has mixed sclerotic-lytic density (curved arrow). Its overall size is unchanged but its zone of transition (the interface between the lesion and normal-appearing bone) is wide and more ill-defined. The calcifications in the subacromial space (white arrow) and the cortical erosion (black arrow) persist, unchanged.
The patient was clinically asymptomatic 1 year after the original presentation. Radiographs (Fig. 5) showed the lesion had continued to change appearance. The interosseous component at the greater tuberosity (curved arrow) had become more subtle and was no longer the most prominent radiographic feature. The cortical erosion (black arrow) and the subacromial calcifications (white arrow) continued to persist, having only slightly decreased compared with the prior radiographs. The intraosseous appearance was that of multiple subcortical cysts with well demarcated sclerotic borders, unlikely at this stage to be mistaken for malignancy or infection.
Fig. 5.
Follow-up radiographs approximately 1 year (15 months) after initial presentation. The greater tuberosity lesion (curved arrow) can now be characterized by multifocal subcortical lucent cysts with sclerotic borders. The calcifications in the subacromial space (white arrow) have decreased, but only slightly with prior radiographs, and the cortical erosion (black arrow) persists.
Discussion
Calcific tendinitis of the rotator cuff, also referred to as calcifying/calcified/calcareous tendinosis or tendinopathy, is generally treated conservatively with physiotherapy and anti-inflammatory medication [1]. Radiographs that reveal calcifications in the subacromial space and the diagnosis can be easily made when these calcifications are an isolated finding.
The underlying cause of calcific tendinitis is still not fully understood. Current knowledge suggests that accumulation of calcification in the tendons occur in the following stages: precalcification, calcification, and postcalcific stages [15]. During the typically asymptomatic precalcification stage, tissues are altered such that cells are predisposed to create calcium deposits. The calcification stage consists of 2 parts. First, cells begin to secrete calcium hydroxyapatite and deposits are formed and a resting phase begins. The secretion is painless, and the resting phase can last for varying amounts of time. However, the next part of the calcification stage—the resorption of the calcium deposits, also termed the resorptive phase—is the painful component of calcific tendonitis. Once the deposits are removed they are replaced with tissue during the postcalcific stage, which is a painless process.
Osseous involvement of calcific tendinitis is uncommon. A 4-decade retrospective review of 2003 calcific tendonitis cases affecting various joints evaluated the spectrum of osseous involvement, from cortical erosions to intraosseous migration [2]. Of all these cases, only 50 met the criteria of osseous involvement, 11 of which were at the greater tuberosity. When osseous involvement was present, cortical erosions were the most prevalent manifestation. The pathogenesis of the cortical erosion is unclear, with inflammatory processes, altered vascularization, and mechanical effects of tendinous insertion likely contributing [6].
The most rare form of osseous involvement is the intraosseous migration of intratendinous calcification, as shown in this study [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15]. Intraosseous calcific tendinitis was first described in a paper entitled “Vanishing osteosclerotic lesion of the humeral head” [4]. The authors reported the “spontaneous disappearance of a dense round lesion from within the greater tuberosity of the humerus” when radiographed 3 months later. Rather than completely “vanishing” however, the authors described the lesion as being replaced by a purely “osteolytic focus of abnormality.” Our findings differed from these, with the 3-month appearance not entirely lytic, instead showing a mixed sclerotic-lytic appearance (curved arrow, Fig. 4).
Over the next 2 decades, intraosseous calcific tendinitis of the shoulder has been reported sporadically in the literature [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15]. Only one of these reported the radiographic appearance beyond the acute presentation; after a 4-month interval, the greater tuberosity showed “near complete resolution of the opacity, with only small residual calcification in the greater tuberosity and supraspinatus tendon” [2]. This interval appearance of a mixed sclerotic-lytic density also differs from the initial paper [4], and is concordant with our results (Fig. 4). If the diagnosis had not been previously established, or if no prior imaging was available for comparison, the radiographic appearance after a 3-month interval could create a greater diagnostic dilemma. The differential diagnosis would no longer include (benign) bone islands, which are typically purely sclerotic [7]. The heterogeneous density of the lesion is similar to chondroid matrix, and a wider zone of transition is a feature associated with more aggressive osseous lesions [8].
Radiographs, which are ideal for detection of intratendinous calcifications, should always be obtained prior to MRI or Tc-99m whole-body scintigraphy. The latter has been shown to be extremely sensitive in their retrospective review of osseous involvement with calcific tendinitis, positive in all 13 patients investigated [2].
To our knowledge, the radiographic appearance of intraosseous calcific tendinitis 1 year after the original presentation has not previously been reported. By this time, the patient was clinically asymptomatic. The lesion persisted but no longer had an aggressive appearance (Fig. 5). Follow-up radiographs for intraosseous calcific tendinitis may serve a purpose for treatment guidance, but only when complications are suspected [9]. More invasive treatment such as arthroscopic removal has provided conflicting results [14], [16]. Recent research has shown that the outcome of ultrasound-guided percutaneous irrigation is less favorable compared with purely tendinous or peritendinous disease [9].
In summary, interosseous migration of calcific tendinitis is a rare entity with the radiographic appearance of a sclerotic lesion adjacent to cortical erosions, which could be mistaken for malignancy or infection. Although the diagnosis can be made with radiographs, MRI and nuclear medicine can provide useful corroborating findings. For example, MRI can clearly show focal fluid signal bridging the thickened supraspinatus tendon and the lesion in the greater tuberosity, depicting the active process of calcification migrating into bone. This case also illustrates the changing nature of the radiographic appearance at 3-month and 1-year intervals. If prior imaging were unavailable, the diagnosis would be more difficult in the months after acute presentation. As the lesion becomes less sclerotic, its zone of transition increases, thereby it appears more aggressive. Awareness of such changes, particularly in patients who lack prior imaging of the acute phase, is important to avoid unnecessary treatment or investigations.
Declarations of interest
None.
Footnotes
Acknowledgments: The authors would like to thank Dr. Robert Hawkes for the MRI images and helpful discussions.
References
- 1.Kachewar S.G., Kulkarni D.S. Calcific tendinitis of the rotator cuff: a review. J Clin Diagn Res. 2013;7:1482–1485. doi: 10.7860/JCDR/2013/4473.3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flemming D.J, Murphey M.D., Shekitka K.M., Temple H.T., Jelinek J.J., Kransdorf M.J. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol. 2003;181:965–972. doi: 10.2214/ajr.181.4.1810965. [DOI] [PubMed] [Google Scholar]
- 3.Malghem J., Omoumi P., Lecouvet F., Vande Berg B. Intraosseous migration of tendinous calcifications: cortical erosions, subcortical migration and extensive intramedullary diffusion, a SIMS series. Skeletal Radiol. 2015;44:1403–1412. doi: 10.1007/s00256-015-2165-x. [DOI] [PubMed] [Google Scholar]
- 4.Chagnaud C., Gaubert J.Y., Champsaur P., Marciano S., Petit P., Moulin G. Vanishing osteosclerotic lesion of the humeral head. Skeletal Radiol. 1998;27:50–52. doi: 10.1007/s002560050337. [DOI] [PubMed] [Google Scholar]
- 5.Della Valle V., Bassi E.M., Calliada F. Migration of calcium deposits into subacromial-subdeltoid bursa and into humeral head as a rare complication of calcifying tendinitis: sonography and imaging. J Ultrasound. 2015;18:259–263. doi: 10.1007/s40477-015-0163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dürr H.R., Lienemann A., Silbernagl H., Nerlich A., Refior H.J. Acute calcific tendinitis of the pectoralis major insertion associated with cortical bone erosion. Eur Radiol. 1997;7:1215–1217. doi: 10.1007/s003300050277. [DOI] [PubMed] [Google Scholar]
- 7.Greenspan A. Bone island (enostosis): current concept—a review. Skeletal Radiol. 1995;24:111–115. doi: 10.1007/BF00198072. [DOI] [PubMed] [Google Scholar]
- 8.Helms C. 4th ed. Saunders; 2013. Fundamentals of skeletal radiology. [Google Scholar]
- 9.Klontzas M.E., Vassalou E.E., Karantanas A.H. Calcific tendinopathy of the shoulder with intraosseous extension: outcomes of ultrasound-guided percutaneous irrigation. Skeletal Radiol. 2017;46:201–208. doi: 10.1007/s00256-016-2538-9. [DOI] [PubMed] [Google Scholar]
- 10.Kraemer E.J., El-Khoury G.Y. Atypical calcific tendinitis with cortical erosions. Skeletal Radiol. 2000;29:690–696. doi: 10.1007/s002560000278. [DOI] [PubMed] [Google Scholar]
- 11.Lee Y.J., Sadigh S., Mankad K., Kapse N., Rajeswaran G. The imaging of osteomyelitis. Quant Imaging Med Surg. 2016;6:184–198. doi: 10.21037/qims.2016.04.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin S., Rapariz J.M. Intraosseous calcium migration in calcifying tendinitis: a rare cause of single sclerotic injury in the humeral head (2010: 2b) Eur Radiol. 2010;20:1284–1286. doi: 10.1007/s00330-009-1500-9. [DOI] [PubMed] [Google Scholar]
- 13.Serafini G, Sconfienza L.M., Lacelli F., Silvestri E., Aliprandi A., Sardanelli F. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle us-guided percutaneous treatment—nonrandomized controlled trial. Radiology. 2009;252:157–164. doi: 10.1148/radiol.2521081816. [DOI] [PubMed] [Google Scholar]
- 14.Seyahi A., Demirhan M. Arthroscopic removal of intraosseous and intratendinous deposits in calcifying tendinitis of the rotator cuff. Arthroscopy. 2009;25:590–596. doi: 10.1016/j.arthro.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 15.Uhthoff H.K., Loehr J.W. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997;5:183–191. doi: 10.5435/00124635-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Porcellini G., Paladini P., Campi F., Pegreffi F. Osteolytic lesion of greater tuberosity in calcific tendinitis of the shoulder. J Shoulder Elbow Surg. 2009;18:210–215. doi: 10.1016/j.jse.2008.09.016. [DOI] [PubMed] [Google Scholar]