Abstract
Objectives
This study aims to investigate the effects of Tai Chi (TC) exercises on muscle strength, pain, proprioception, and knee function in patients with partial anterior cruciate ligament (ACL) injuries.
Patients and methods
Between March 2017 and January 2018, a total of 58 patients with partial ACL injuries (30 male, 28 female; mean age 25.5±6.4; range, 18 to 36 years) were included in the study. The patients were randomly divided into two groups: TC group (n=29) and control group (n=29). For both groups, an activity modification approach was applied. The TC group participated in a 24-week TC exercise program, while no exercise or home-based program was administered to the control group. Isokinetic knee extension and flexion muscle strengths were evaluated at angular velocities of 60°/sec and 180°/sec. The visual analog scale (VAS), isokinetic system, Lysholm Knee Scale (LKS), and International Knee Documentation Committee 2000 (IKDC-2000) were used for the evaluation of pain, proprioception, and knee function, respectively.
Results
Significant changes were found in the TC group for the knee extensor muscle strength measured at an angular velocity of 60°/sec (p=0.012) and 180°/sec (p=0.011), VAS pain (p=0.005), and proprioception (measured with isokinetic device) (p<0.001). While knee extensor muscle strength, pain, proprioception, LKS, and IKDC-2000 scores improved in the TC group, improvements were recorded only for LKS and IKDC-2000 scores in the control group.
Conclusion
Based on these results, we conclude that TC exercises can yield positive outcomes on the knee extensor muscle strength, pain, proprioception and knee function in patients with partial ACL injuries. Hence, TC exercises can be used as a novel method by researchers and clinicians in the treatment of partial ACL injuries.
Keywords: Anterior cruciate ligament, conservative treatment, pain, proprioception, Tai Chi
Introduction
Accounting for about 10 to 28% of all anterior cruciate ligament (ACL) tears, partial tears of the ACL are quite common.[1,2] According to studies including patients with partial ACL injuries, less than 50% of patients return to their pre-injury level of activity.[1,2] In addition, several studies have demonstrated that patients trying to return to their active lifestyle commonly progress to total ligament rupture.[3] Therefore, it is of utmost importance to adopt individualized treatment plan which meets the needs of each patient. To provide appropriate treatment, it is fundamental to identify patients with a low and high risk of progression to total ligament defects.[4] In their study comparing the outcomes of surgically and non- surgically treated patients with partial ACL injuries, Dawson et al.[5] reported that these two groups could achieve similar and satisfactory levels of functionality. Some authors have shown that positive results can be achieved through conservative treatment approaches which are carefully and precisely planned to meet the needs of each individual patient and are associated with a minimal activity level decline, but no decline in stability.[3,6,7]
Preventing re-injury of ligaments as well as surrounding tissues, and maintaining stability, strength and functionality of the knee are amongst the main aims of conservative treatment.[6] This treatment approach remains as a beneficial option according to some studies.[7,8] Casteleyn and Handelberg[8] conducted a study in which cases from a general population less interested in sport activities with a mean of 8.5 years were treated conservatively for their ACL rupture. About 73% of these patients were categorized in Grade A or B according to the overall International Knee Documentation Committee-2000 (IKDC-2000) criteria. In another study, 100 acute ACL patients who underwent a rehabilitation program following arthroscopy were followed for 15 years.[7] According to the results of the study, an adequate activity level and satisfactory knee function could be achieved in most cases with ACL injury treated without reconstruction.
Originating from China, Tai Chi (TC) was initially developed as a military art of self-defense and was widely popular among the public for preserving good health.[9] It includes not only physical movements, but also elements to purify the mind such as setting the body upright, whilst letting the arms fall and aligning the feet.[9-11] Many studies investigating the effects of TC also included older adults in their sample.[9,10,12] A study concluded that muscle strength and gait ability improved in older adults as a result of TC.[9] Another study showed that iliopsoas, quadriceps femoris, hamstring, tibialis anterior, and other lower limb muscles improved in terms of strength following TC.[10] Other studies investigated the effects of TC on specific diseases. According to two studies, TC was found to be more effective than stretching exercises in cases of fibromyalgia[11] and knee osteoarthritis.[13] Based on these findings and relevant literature, the inclusion of TC exercises in the treatment programs have gained in importance.[14-16]
Considering the aforementioned studies, most have focused on older adults and the treatment of osteoarthritis. To date, no studies investigating the effects of TC on ACL injury have been published in the literature. In the present study, therefore, we aimed to investigate the effects of TC on the muscular strength, knee function, and proprioception of non-surgically treated patients with partial ACL injuries.
Patients and Methods
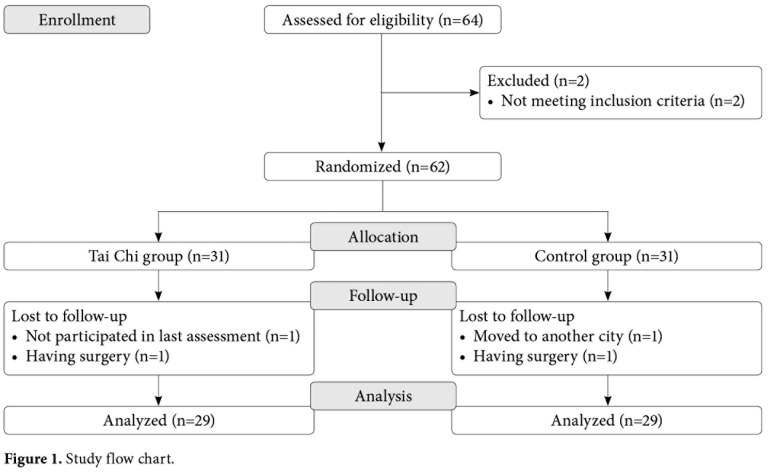
This single-blind, randomized-controlled trial was conducted at Ahi Evran University Faculty of Medicine, Departments of Orthopedics and Traumatology and Physical Medicine and Rehabilitation between March 2017 and January 2018. A total of 58 patients with partial ACL injuries (30 male, 28 female; mean age 25.5±6.4; range, 18 to 36 years) were included in the study. Clinical diagnosis was performed by a specialist physician based on the medical background, physical examination findings, and diagnostic images of the patients. Those with meniscus tears, meniscus injuries, chondral lesions, Grade IV injuries according to the Lachman test, ligament laxities or a generalized laxity, and/or a body mass index (BMI) above 30 kg/m2 were excluded from the study. Inclusion criteria were as follows: aged between 20 and 45 years, having a sedentary lifestyle or a low level of activity, requiring conservative treatment, and having a visual analog scale (VAS) score of <3. Although 64 patients were invited to participate in the study initially, two did not meet the inclusion criteria and excluded. The remaining 62 patients were randomly divided into two groups. However, two patients from each group did not attend to the final visit. Therefore, the study was completed with a total of 29 patients in each group. The study flow chart is shown in Figure 1.
Figure 1. Study flow chart.
The patients were randomly divided into two groups: TC group (n=29) and control group (n=29). Clinical trial was conducted on two groups as pretest-posttest assessment design. A written informed consent was obtained from each participant. The study protocol was approved by the Kırşehir Ahi Evran University, Faculty of Medicine Ethics Committee (2017-08/67). The study was conducted in accordance with the principles of the Declaration of Helsinki.
Interventions
All participants of the study were advised regarding the activity modification approach proposed by Paterno[17] for patients with partial ACL injuries.
Tai Chi group
The TC exercise program was planned in accordance with the Yang-Style with natural and extended postures, even and slow motions, steady and light movements, and flowing and curved lines of performance.[18] The sessions lasting 60 min were held three times each week for a total of 24 weeks by an experienced TC instructor with more than five years of experience. Each session consisted of 10 forms of Yang-Style; however, minor modifications were made to make the exercises suitable for patients with partial ACL injuries. These 10 modified postures either induced progressive amounts of stress onto postural stability or highlighted increasing magnitude of the rotation of the trunk over the arm, while decreasing the base of support in order that physical functionality could improve without excessive stress on the joints.[19] During the first session, mind-body exercise theory and procedures were explained by the instructor, and booklets on TC principles, techniques, and safety precautions were given to the participants.[16] Each session lasted for 60 min and consisted of 15 min of warm-up (i.e., stretching, mobility, and breathing techniques), 30 min of TC exercises, and 15 min of cool-down.
Control group
Except for the activity modification, no additional exercise therapy or home-based program was applied to the individuals in the control group. However, after the completion of the study, TC exercises were applied to those patients in the control group who were willing to perform the exercises.
Assessments
Socio-demographic characteristics, duration of symptoms, affected and dominant sides were recorded through the face-to-face interview method.
Knee function
To evaluate knee function, the Lysholm Knee Scale (LKS) was used. This scale is scored on a 0 to 100 range, where higher scores indicate better functionality.[1,20] The IKDC-2000 criteria were also used in the current study to evaluate knee function. Containing 18 items in three main domains of symptoms, sports, and daily activities, the LKS is a scale scored on a 0 to 100 range, where higher scores indicate better functionality and fewer symptoms.[21,22]
Pain
The VAS is a simple tool for the evaluation of pain. The patients were asked to mark their current pain on a 10-cm-long line. The line is scored from 0 to 10, with 0 indicating no pain, up to 10 which represents the worst pain they have ever experienced.[23]
Muscle strength
The isokinetic strength of the affected knee extensor and flexor muscles was assessed at the velocity of 60°/sec and 180°/sec using the Biodex System 4-Pro (Biodex Inc., Shirley, NY, USA). Prior to testing, a standard procedure was applied in terms of the equipment, data collection, and warm- up. The warm-up consisted of five min of active exercise with a stationary (exercise) bike. During the test, patients were asked to sit in a dynamometer with their pelvis, thighs and ankles stabilized with straps, thigh bolsters and ankle cuffs, and they were allowed to hold onto the handles of the bench. The lever arm was set individually, and the axis of rotation was adjusted to be in alignment with the knee axis. The range of motion was set between 90° for flexion and 0° for extension. Prior to testing, each patient was administered three repetitions to help them adapt to the test. Three min after the adaptation period, the muscle strength testing was performed.[24] After a three-min rest period, maximal knee extension–flexion concentric repetitions were performed with five at 60°/sec and 10 at 180°/sec, each with one-min rest intervals.[25] The patients were encouraged to apply maximum effort for each test. The results were recorded as the isokinetic peak torques for knee flexion and extension muscle strength. Proprioception Proprioception was measured using a Biodex System 4-Pro (Biodex Inc., Shirley, NY, USA). The patients were asked to sit on a chair in a position similar to the muscle strength assessment. The proximal malleoli of the ankle were attached to the dynamometer’s lever arm. At the level of the femur lateral epicondyle, the rotational axis of the dynamometer was aligned with the rotational axis of the knee.[26] While the dynamometer was tilted at 0° and orientated at 90° fixed, the seatback was 70 to 85° inclined and the seat orientation fixed at 90°. Proprioception of the affected knee was tested at a target angle of 30°, since this is the working angle of the knee during daily weight-bearing activities.[26] As active testing is more functional than passive testing, proprioception was tested in the active mode of the isokinetic system.[27] Prior to testing, the procedure was explained to each patient. Then, the patients were instructed about other details of the test, such as the sitting position, flexion and extension of knee, memorizing angle, rest periods, and when to press the stop button. For the data collection, the patients were instructed to extend their leg from the start position, until the arm of the dynamometer prevented any further movement (the target angle). The dynamometer kept the leg at the target angle for a period of 10 sec during which the patient memorized the position. Then, the patient flexed the knee back to the initial position before being asked to extend the leg and press the stop button, when they felt they achieved the target position. The tests were repeated three times and the average difference error of the three measurements between the target angle position and the subject’s perceived angle was recorded.[26,27] In the current study, the average of these three scores was used as the error score for each patient. The participants completed the tests with their eyes closed in a quiet laboratory setting.
Randomization and blinding
Based on their sex and age, the participants were divided into two groups using the matched randomization method as TC group and control group. The patients were assessed both at baseline and end of the study by a single researcher who was blind to the group allocation.
Sample size
Following the 24-week intervention for different knee pathologies, a clinically important difference (MCID) for IKDC-2000 was calculated as 8.8 points. Based on a standard deviation of 17, MCID of IKDC- 2000, using mixed design repeated measures analysis of variance (ANOVA) at 0.05 alpha level of significance, a statistical power of 80%, and a β level of 0.20, the minimum number of participants was calculated to be 29 per group.[28] Considering a potential drop-out rate of 10%, 64 patients were recruited to the study. Sample size was calculated using G*Power version 3.1.9.2 software (Heinrich-Heine-Universität Düsseldorf, Germany).[29]
Statistical analysis
Statistical analysis was performed using the IBM SPSS version 21.0 software (IBM Corp., Armonk, NY, USA). Descriptive statistics were expressed in mean ± standard deviation (SD) or number and frequency. The data were normally distributed according to the Shapiro-Wilk test. Therefore, parametric tests were used for the statistical analysis. For demographic comparisons of the two groups, the chi-square test was used for categorical variables and t-test for continuous variables. The changes in dependent variables pre- and post-intervention were analyzed using a mixed design repeated measures ANOVA to assess the overall group over time (i.e. before and after intervention) and within group (i.e. TC and control) interaction effects. To examine the difference between the baseline and follow-up values, pairwise comparisons were performed. The effect size (ES) was identified by calculating the difference between the baseline and follow-up values, divided by the standard deviation at baseline. A ES of 0.2, 0.5, and 0.8 was considered small, moderate, and large, respectively.[30] A p value of <0.05 was considered statistically significant.
Results
Baseline demographic and clinical data of the patients are shown in Table 1. There was no significant difference between the two groups in terms of age, sex, BMI, duration of symptoms, or their affected or dominant sides. Football (n=30, 58%), basketball (n=8, 15%), volleyball (n=6, 11%), tennis (n=5, 9%), judo (n=2, 3%), and wrestling (n=1, 1%) were reported as the main causes of injuries.
Table 1. Baseline demographic and clinical characteristics of patients.
| TC group (n=29) | Control group (n=29) | ||||||
| n | % | Mean±SD | n | % | Mean±SD | p | |
| Age (year) | 26.1±7.4 | 24.7±6.2 | 0,248 | ||||
| Body mass index (kg/m2) | 24.6±4.1 | 24.9±5.7 | 0,781 | ||||
| Gender | 0,121 | ||||||
| Female | 13 | 44,8 | 15 | 51,7 | |||
| Male | 16 | 55,2 | 14 | 48,3 | |||
| Dominant side | 0,683 | ||||||
| Right | 25 | 86,2 | 26 | 89,6 | |||
| Left | 4 | 13,8 | 3 | 10,4 | |||
| Affected side | 0,714 | ||||||
| Right | 20 | 68,9 | 22 | 75,8 | |||
| Left | 9 | 31,1 | 7 | 24,2 | |||
| Duration of symptoms (week) | 20.1±8.6 | 21.8±4.8 | 0,647 | ||||
| Education status (year) | 14.2±2.6 | 13.7±1.7 | 0,146 | ||||
| TC: Tai Chi; SD: Standard deviation. | |||||||
Although the overall group by interaction for ANOVA was found to be significant (p<0.05) for pain, proprioception, and muscle strength measured at angular velocity of 60°/sec and 180°/sec for knee flexors and extensors, it was not significant for LKS or IKDC-2000 scores (p>0.05). When the post- intervention differences between the two groups were examined, the TC group had more significant improvement in the knee extensor muscle strength, pain, and proprioception compared to the control group (p<0.05). However, there was no significant difference between the groups in terms of the flexor muscle strength, LKS, or IKDC-2000 scores (Table 2).
Table 2. Differences between groups in study outcome measures.
| Baseline | After treatment | ||||
| Variable | Mean±SD | 95% CI | Mean±SD | 95% CI | **p |
| Extension PT 60°/sec | 0,012 | ||||
| TC group | 165.6±15.6 | 154.2-177.4 | 187.8±18.9 | 179.1-196.7 | |
| Control group | 176.4±16.1 | 164.7-188.3 | 178.6±12.7 | 172.8-184.6 | |
| *p | 0,551 | 0,049 | |||
| Flexion PT 60°/sec | 0,061 | ||||
| TC group | 141.2±14.9 | 129.6-152.9 | 145.4±16.3 | 138.3-152.7 | |
| Control group | 136.9±9.8 | 123.4-150.2 | 138.2±11.2 | 128.0-149.1 | |
| *p | 0,316 | 0,104 | |||
| Extension PT 180°/sec | 0,011 | ||||
| TC group | 124.1±22.1 | 113.9-135.3 | 154.6±18.6 | 139.8-169.8 | |
| Control group | 127.8±19.4 | 117.6-138.3 | 130.9±16.7 | 118.1-143.4 | |
| *p | 0,427 | 0,021 | |||
| Flexion PT 180°/sec | 0,084 | ||||
| TC group | 105.6±18.6 | 97.6-113.8 | 113.6±19.1 | 101.1-125.6 | |
| Control group | 99.7±11.2 | 89.4-110.2 | 104.6±12.3 | 94.4-115.0 | |
| *p | 0,139 | 0,087 | |||
| Pain | 0,005 | ||||
| TC group | 4.5±1.5 | 4.2-4.9 | 2.1±0.8 | 1.7-2.5 | |
| Control group | 4.8±2.3 | 4.4-5.1 | 5.6±2.1 | 4.8-6.5 | |
| *p | 0,432 | 0,029 | |||
| Proprioception | <0.001 | ||||
| TC group | 4.0±1.4 | 3.6-4.5 | 2.1±0.8 | 1.8-2.5 | |
| Control group | 3.6±1.1 | 3.3-4.0 | 3.8±1.6 | 3.4-4.3 | |
| p1 | 0,571 | <0.001 | |||
| LKS | 0,147 | ||||
| TC group | 68.6±12.1 | 62.9-74.3 | 83.4±11.7 | 78.2-89.1 | |
| Control group | 72.5±13.6 | 66.1-78.9 | 84.6±12.4 | 79.4-90.2 | |
| *p | 0,091 | 0,325 | |||
| IKDC-2000 | 0,249 | ||||
| TC group | 62.7±14.2 | 58.3-66.8 | 85.4±17.1 | 79.1-91.5 | |
| Control group | 63.4±13.6 | 57.9-68.4 | 81.2±15.7 | 76.0-86.7 | |
| *p | 0,436 | 0,114 | |||
| SD: Standard deviation; CI: Confidence interval; PT: Peak torque; TC group: Tai Chi group; LKS: Lysholm Knee Scale; IKDC-2000: International Knee Documentation Committee-2000; * Independent sample t-test; ** Mixed design repeated measures ANOVA. | |||||
In both groups, significant changes were seen in some of the measurement scores following the intervention. While significant changes were observed in the extensor muscle strength, pain, proprioception, LKS, and IKDC-2000 scores in the TC group, there was a change only in LKS and IKDC-2000 scores in the control group. The ES obtained from all variables measured after the intervention was higher in the TC group (Table 3).
Table 3. Pairwise comparison of groups for muscle strengths, pain, proprioception, LKS and IKDC-2000 scores.
| Baseline | After treatment | ||||
| Variable | Mean±SD | Mean±SD | p | ES | 95% CI |
| Extension PT 60°/sec | |||||
| TC group | 165.6 ±15.6 | 187.8 ±18.9 | <0.001 | 1,4 | 1.0-1.7 |
| Control group | 176.4 ±16.1 | 178.6 ±12.7 | 0,094 | 0,4 | 0.1-0.7 |
| Flexion PT 60°/sec | |||||
| TC group | 141.2 ±14.9 | 145.4 ±16.3 | 0,081 | 0,3 | 0.1-0.4 |
| Control group | 136.9 ±9.8 | 138.2 ±11.2 | 0,148 | 0,2 | 0.2-0.3 |
| Extension PT 180°/sec | |||||
| TC group | 124.1 ±22.1 | 154.6 ±18.6 | <0.001 | 1,5 | 1.2-1.8 |
| Control group | 127.8 ±19.4 | 130.9 ±16.7 | 0,195 | 0,2 | 0.0-0.4 |
| Flexion PT 180°/sec | |||||
| TC group | 105.6 ±18.6 | 113.6 ±19.1 | 0,092 | 0,4 | 0.3-0.6 |
| Control group | 99.7 ±11.2 | 104.6 ±12.3 | 0,061 | 0,4 | 0.2-0.6 |
| Pain | |||||
| TC group | 4.5 ±1.5 | 2.1 ±0.8 | <0.001 | 1,6 | 1.0-2.2 |
| Control group | 4.8 ±2.3 | 5.6 ±2.1 | 0,115 | 0,3 | 0.1-0.4 |
| Proprioception | |||||
| TC group | 4.0 ±1.4 | 2.1 ±0.8 | <0.001 | 1,4 | 1.0-1.8 |
| Control group | 3.6 ±1.1 | 3.8 ±1.6 | 0,216 | 0,2 | 0.0-0.4 |
| LKS | |||||
| TC group | 68.6 ±12.1 | 83.4 ±11.7 | 0,001 | 1,2 | 0.7-1.7 |
| Control group | 72.5 ±13.6 | 84.6 ±12.4 | 0,018 | 0,9 | 0.6-1.2 |
| IKDC-2000 | |||||
| TC group | 62.7 ±14.2 | 85.4 ±17.1 | 0,001 | 1,6 | 1.1-2.0 |
| Control group | 63.4 ±13.6 | 81.2 ±15.7 | 0,001 | 1,3 | 0.9-1.7 |
| LKS: Lysholm Knee Scale; IKDC-2000: International Knee Documentation Committee-2000; SD: Standard deviation; ES: Effect size; CI: Confidence interval; PT: Peak torque; TC group: Tai Chi group. | |||||
Discussion
The most important finding of this single-blind, randomized-controlled study investigating the effectiveness of TC exercises on partial ACL injuries was that, compared to the control group, the patients in the TC group experienced improvements in the knee extensor muscle strength measured at angular velocity of 60°/sec and 180°/sec, pain, and proprioception scores. It was also found that knee functionality increased for participants of both groups. However, as the ES was found to be higher in the TC group, it can be concluded that the benefit of the intervention was greater for the TC group, compared to the control group.
According to Wu et al.,[12] the knee extensor muscle strength was better in individuals aged 55 years or above who performed TC exercises over a long period of time (minimum three years), compared to those who did not. In another study, TC exercises were found to increase the knee flexor and extensor muscle strength, compared the control group.[31] In contrast to these studies, Song et al.[32] conducted a study in which the knee muscle strengths were measured at an angular velocity of 60°/sec and 180°/sec in females with knee osteoarthritis. As a result of the study, the authors observed no significant difference in the knee muscle strength between the TC group and the control group in which only a self-help education program was applied. In another study investigating the effects of TC exercises on the muscle strength in older adults, Li et al.[33] found no significant changes in the knee flexion and extension muscle strength in both the TC and control groups at angular velocities of 30°/sec and 180°/sec. Although previous studies have shown that TC exercises have different effects on various diseases and age groups, a recent meta-analysis have suggested that, regardless of long-term or short-term effects of TC, these exercises can increase the knee muscle strength in older adults.[34] However, there is no study available in the literature investigating the effects of TC exercises on the knee extensor and flexor muscle strengths in patients with partial ACL injuries. In the current study, TC exercises were found to cause an increase in the knee extensor muscle strength; yet, they had no significant effect on the knee flexion strength. This can be attributed to many TC exercises being performed in the semi-squat position and to the fact that these exercises cause no overload on the knee, as they carry features of closed kinetic chain.[35]
In the present study, following the intervention program, pain severity was found to decrease in the TC group and increase in the control group. To the best of our knowledge, the efficacy of TC exercises has not been examined in partial ACL injuries. However, there are studies applying TC for some painful conditions, including fibromyalgia, osteoarthritis, rheumatoid arthritis, and cancer. In addition, there is a number of systematic reviews and meta-analyses demonstrating that TC exercises are particularly effective on pain management for patients with knee osteoarthritis.[36-38] In a meta-analysis by Lauche et al.,[36] the effects of TC exercises on knee osteoarthritis were investigated, and the TC exercises were shown to be an adjuvant treatment option in reducing pain in knee osteoarthritis. As in knee osteoarthritis, TC exercises also yielded positive effects on pain in cases of back pain and fibromyalgia.[14,15] Therefore, we can conclude that our study results are consistent with the published literature.
Knee proprioception, which plays an important role in the accuracy and efficiency of sport movements, commonly deteriorates with several sport injuries.[39] Wang et al.[40] examined the effects of 12 weeks of TC exercises on knee proprioception in individuals with knee using an electrogoniometer at angles of 30°, 45°, and 60°. At the end of Week 12, the authors reported statistically significant changes in the proprioception measured at 30° in the TC group, compared to the control group. In their randomized-controlled study, Chang et al.[41] investigated the effects of 24 weeks of TC exercises on older females and reported positive changes in their knee proprioception, compared to the control group. Based on these results, TC exercises are effective on knee proprioception in different age groups and for various diseases. However, no study examining the effectiveness of TC exercises in partial ACL injuries is available in the literature. In the current study, proprioception improved by approximately 48% in the TC group. In the control group, however, proprioception was impaired by 6%.
In the current study, knee function was evaluated using the LKS and IKDC-2000. There was no significant difference between the groups. However, there was an increase in the knee function with a higher range of effect in the TC group than in the control group, and a positive increase in knee function in the control group, as well. In a review by Pujol et al.,[42] the short- and mid-term natural course of partial ACL injury on the knee function was found to be satisfactory. In our study, both the TC and control groups showed similar results in terms of knee functionality, which is thought to be due to the natural course of partial ACL healing.
Nonetheless, this study has some limitations. First, we were only able to investigate the short-term effects of TC exercises, and long-term effects and follow-up results of these exercises still remain unknown. Second, the study mainly focused on physical complaints of patients with partial ACL injuries, whereas mind-body interventions such as TC are known to be associated with stress, anxiety, depression, and self-esteem.[43] Therefore, our study was limited in the absence of a parameter related to the psychological distress of the participants.
In conclusion, our study results suggest that TC exercises can be used as an alternative rehabilitation regimen for non-surgically treated patients with partial ACL injuries. Of note, there is no study in the literature investigating the effects of TC exercises on ACL injuries and, for the first time, the present study shows that TC can be a potential conservative treatment option for patients, as these exercises improve the knee function, proprioception, and knee extensor muscle strength at 60°/sec and 180°/sec with decreased pain severity. However, there is still a need for further studies in which TC exercises are compared with other non-operative ACL treatments, where long-term follow-up periods, different styles of TC, and different injuries and pathologies related to the knee joint are involved.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 2.Borbon CA, Mouzopoulos G, Siebold R. Why perform an ACL augmentation. Knee Surg Sports Traumatol Arthrosc. 2012;20:245–251. doi: 10.1007/s00167-011-1565-2. [DOI] [PubMed] [Google Scholar]
- 3.Tjoumakaris FP, Donegan DJ, Sekiya JK. Partial tears of the anterior cruciate ligament: diagnosis and treatment. Am J Orthop (Belle Mead NJ) 2011;40:92–97. [PubMed] [Google Scholar]
- 4.Temponi EF, de Carvalho Júnior LH, Sonnery-Cottet B, Chambat P. Partial tearing of the anterior cruciate ligament: diagnosis and treatment. Rev Bras Ortop. 2015;50:9–15. doi: 10.1016/j.rboe.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dawson AG, Hutchison JD, Sutherland AG. Is anterior cruciate reconstruction superior to conservative treatment. J Knee Surg. 2016;29:74–79. doi: 10.1055/s-0034-1396017. [DOI] [PubMed] [Google Scholar]
- 6.Delincé P, Ghafil D. Anterior cruciate ligament tears: conservative or surgical treatment. A critical review of the literature. Knee Surg Sports Traumatol Arthrosc. 2012;20:48–61. doi: 10.1007/s00167-011-1614-x. [DOI] [PubMed] [Google Scholar]
- 7.Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Fridén T, Roos H. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med. 2007;35:1135–1143. doi: 10.1177/0363546507299238. [DOI] [PubMed] [Google Scholar]
- 8.Casteleyn PP, Handelberg F. Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg [Br] 1996;78:446–451. [PubMed] [Google Scholar]
- 9.Jeon I, Han D, Park R, Kim B. The Effects of Tai Chi exercise program on the improvement of gait ability in the old women. Korean J Sport Sci. 2002;17:14–24. [Google Scholar]
- 10.Zhou M, Peng N, Dai Q, Li HW, Shi RG, Huang W. Effect of Tai Chi on muscle strength of the lower extremities in the elderly. Chin J Integr Med. 2016;22:861–866. doi: 10.1007/s11655-015-2104-7. [DOI] [PubMed] [Google Scholar]
- 11.Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, et al. A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363:743–754. doi: 10.1056/NEJMoa0912611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu G, Zhao F, Zhou X, Wei L. Improvement of isokinetic knee extensor strength and reduction of postural sway in the elderly from long-term Tai Chi exercise. Arch Phys Med Rehabil. 2002;83:1364–1369. doi: 10.1053/apmr.2002.34596. [DOI] [PubMed] [Google Scholar]
- 13.Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2009;61:1545–1553. doi: 10.1002/art.24832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Segura-Jiménez V, Romero-Zurita A, Carbonell-Baeza A, Aparicio VA, Ruiz JR, Delgado-Fernández M. Effectiveness of Tai-Chi for decreasing acute pain in fibromyalgia patients. Int J Sports Med. 2014;35:418–423. doi: 10.1055/s-0033-1353214. [DOI] [PubMed] [Google Scholar]
- 15.Hall AM, Maher CG, Lam P, Ferreira M, Latimer J. Tai chi exercise for treatment of pain and disability in people with persistent low back pain: a randomized controlled trial. Arthritis Care Res (Hoboken) 2011;63:1576–1583. doi: 10.1002/acr.20594. [DOI] [PubMed] [Google Scholar]
- 16.Lee AC, Harvey WF, Wong JB, Price LL, Han X, Chung M, et al. Effects of Tai Chi versus physical therapy on mindfulness in knee osteoarthritis. Mindfulness (N Y) 2017;8:1195–1205. doi: 10.1007/s12671-017-0692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paterno MV. Non-operative care of the patient with an ACL- deficient knee. Curr Rev Musculoskelet Med. 2017;10:322–327. doi: 10.1007/s12178-017-9431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164:493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 19.Wang C, Iversen MD, McAlindon T, Harvey WF, Wong JB, Fielding RA, et al. Assessing the comparative effectiveness of Tai Chi versus physical therapy for knee osteoarthritis: design and rationale for a randomized trial. BMC Complement Altern Med. 2014;14:333–333. doi: 10.1186/1472-6882-14-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Celik D, Coşkunsu D, Kiliçoğlu O. Translation and cultural adaptation of the Turkish Lysholm knee scale: ease of use, validity, and reliability. Clin Orthop Relat Res. 2013;471:2602–2610. doi: 10.1007/s11999-013-3046-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 22.Çelik D, Coşkunsu D, KiliÇoğlu Ö, Ergönül Ö, Irrgang JJ. Translation and cross-cultural adaptation of the international knee documentation committee subjective knee form into Turkish. J Orthop Sports Phys Ther. 2014;44:899–909. doi: 10.2519/jospt.2014.4865. [DOI] [PubMed] [Google Scholar]
- 23.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 24.Parcell AC, Sawyer RD, Tricoli VA, Chinevere TD. Minimum rest period for strength recovery during a common isokinetic testing protocol. Med Sci Sports Exerc. 2002;34:1018–1022. doi: 10.1097/00005768-200206000-00018. [DOI] [PubMed] [Google Scholar]
- 25.Rosene JM, Fogarty TD, Mahaffey BL. Isokinetic hamstrings: Quadriceps ratios in Intercollegiate Athletes. J Athl Train. 2001;36:378–383. [PMC free article] [PubMed] [Google Scholar]
- 26.Ghasemi GA, Zolaktaf V, Ibrahim K, Minasian V. Evaluation of joint position sense after ACL reconstruction with hamstring tendon auto graft. Am J Sport Med. 2013;1:52–55. [Google Scholar]
- 27.Ribeiro F, Oliveira J. Effect of physical exercise and age on knee joint position sense. Arch Gerontol Geriatr. 2010;51:64–67. doi: 10.1016/j.archger.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS- ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res (Hoboken) 2011;63:208–228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 30.de Vet HC, Terwee CB, Bouter LM. Current challenges in clinimetrics. J Clin Epidemiol. 2003;56:1137–1141. doi: 10.1016/j.jclinepi.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 31.Zhuang J, Huang L, Wu Y, Zhang Y. The effectiveness of a combined exercise intervention on physical fitness factors related to falls in community-dwelling older adults. Clin Interv Aging. 2014;9:131–140. doi: 10.2147/CIA.S56682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Song R, Roberts BL, Lee EO, Lam P, Bae SC. A randomized study of the effects of t’ai chi on muscle strength, bone mineral density, and fear of falling in women with osteoarthritis. J Altern Complement Med. 2010;16:227–233. doi: 10.1089/acm.2009.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li JX, Xu DQ, Hong Y. Changes in muscle strength, endurance, and reaction of the lower extremities with Tai Chi intervention. J Biomech. 2009;42:967–971. doi: 10.1016/j.jbiomech.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 34.Liu B, Liu ZH, Zhu HE, Mo JC, Cheng DH. Effects of tai chi on lower-limb myodynamia in the elderly people: a meta- analysis. J Tradit Chin Med. 2011;31:141–146. doi: 10.1016/s0254-6272(11)60029-0. [DOI] [PubMed] [Google Scholar]
- 35.Lan C, Lai JS, Chen SY, Wong MK. Tai Chi Chuan to improve muscular strength and endurance in elderly individuals: a pilot study. Arch Phys Med Rehabil. 2000;81:604–607. doi: 10.1016/s0003-9993(00)90042-x. [DOI] [PubMed] [Google Scholar]
- 36.Lauche R, Langhorst J, Dobos G, Cramer H. A systematic review and meta-analysis of Tai Chi for osteoarthritis of the knee. Complement Ther Med. 2013;21:396–406. doi: 10.1016/j.ctim.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 37.Yan JH, Gu WJ, Sun J, Zhang WX, Li BW, Pan L. Efficacy of Tai Chi on pain, stiffness and function in patients with osteoarthritis: a meta-analysis. e61672PLoS One. 2013;8 doi: 10.1371/journal.pone.0061672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Macfarlane GJ, Paudyal P, Doherty M, Ernst E, Lewith G, MacPherson H, et al. A systematic review of evidence for the effectiveness of practitioner-based complementary and alternative therapies in the management of rheumatic diseases: osteoarthritis. Rheumatology (Oxford) 2012;51:2224–2233. doi: 10.1093/rheumatology/kes200. [DOI] [PubMed] [Google Scholar]
- 39.Romero-Franco N, Montaño-Munuera JA, Fernández- Domínguez JC, Jiménez-Reyes P. Validity and reliability of a digital inclinometer to assess knee joint position sense in an open kinetic chain. J Sport Rehabil. 2017:1–22. doi: 10.1123/jsr.2017-0221. [DOI] [PubMed] [Google Scholar]
- 40.Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi for treating knee osteoarthritis: designing a long-term follow up randomized controlled trial. BMC Musculoskelet Disord. 2008;9:108–108. doi: 10.1186/1471-2474-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang S, Zhou J, Hong Y, Sun W, Cong Y, Qin M, et al. Effects of 24-week Tai Chi exercise on the knee and ankle proprioception of older women. Res Sports Med. 2016;24:84–93. doi: 10.1080/15438627.2015.1126281. [DOI] [PubMed] [Google Scholar]
- 42.Pujol N, Colombet P, Cucurulo T, Graveleau N, Hulet C, Panisset JC, et al. Natural history of partial anterior cruciate ligament tears: a systematic literature review. Orthop Traumatol Surg Res. 2012;98:160–164. doi: 10.1016/j.otsr.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 43.Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, Schmid CH. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. 2010;10:23–23. doi: 10.1186/1472-6882-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]