Abstract
Ventral thigh surface electromyography may be used to assess for periodic limb movements during sleep (PLMS) in a limb with an above-the-knee amputation. Presence of PLMS in the proximal portion of an amputated lower extremity supports theories of spinal and supraspinal mechanisms in PLMS generation, and demonstrates that intact distal motor efferent pathways and distal sensory afferent pathways are not absolutely necessary for the generation of periodic limb movements.
Citation:
Chada A, Hoque R. Periodic limb movements during sleep noted on ventral thigh surface electromyography in an above-the-knee amputated stump. J Clin Sleep Med. 2019;15(8):1183–1184.
Keywords: amputated limb, periodic limb movements during sleep
INTRODUCTION
The patient is a 57-year-old white man, with past medical history of hypertension, hypercholesterolemia, and diabetes mellitus, who at age 50 years was involved in a motorcycle accident that required above-the-knee amputation of the right lower extremity At age 51 years the patient received a diagnosis of obstructive sleep apnea, and has been on continuous positive airway pressure (CPAP) therapy of 11 cm of water pressure ever since. He presented to Emory Sleep Center clinic with worsening daytime sleepiness, following a 50-lb weight gain since the start of CPAP. His current CPAP device does not provide the residual apnea-hypopnea index at applied pressure; as such, an in-laboratory CPAP titration polysomnography was ordered to determine his current CPAP pressure requirement. He denied an urge to move his lower extremities while sitting still or sleeping; and denied lower extremity kicking during sleep.
IMAGE ANALYSIS
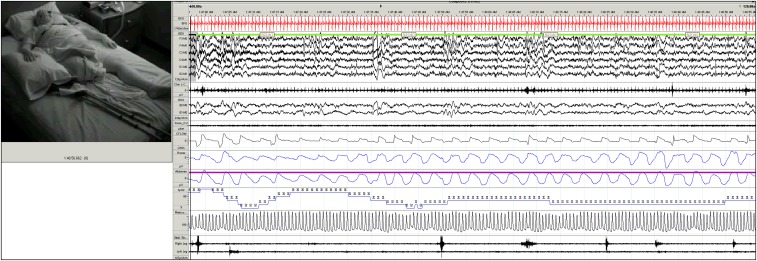
In-laboratory CPAP titration showed a periodic limb movement (PLM) index of 37.9 events per hour, with PLMs noted in both legs, but while in the supine sleep position PLMs were predominantly in his right lower extremity residual limb, with right lower extremity surface electromyography electrodes placed on the ventral right thigh surface (Figure 1). No clear evidence of right hip flexion was noted on review of infrared video. Optimal CPAP pressure was found to be 13 cm of water, with a respiratory disturbance index at optimal pressure of 1.5 events per hour of sleep.
Figure 1. Periodic limb movements during sleep (PLMS) noted from right lower extremity above-the-knee amputation residual limb, with right lower extremity surface electromyography electrodes placed on the ventral right thigh surface.
DISCUSSION
Periodic limb movements during sleep (PLMS) are involuntary, repetitive, stereotypic, short-lasting segmental movements of the lower extremities consisting of dorsiflexion of the big toe with fanning of the small toes, accompanied by flexion at the ankles, knees, and occasionally the hip, resembling the Babinski response flexion withdrawal reflex.1
The pathophysiology of PLMS is not yet completely understood, and there are major controversies regarding the localization of the neural structures involved in their pathophysiology. Implicated flexion reflex arc localizations in PLMS generation and modulation include a supraspinal (ie, suppression of supraspinal descending inhibitory pathways on the pyramidal tract) and spinal (ie, abnormal afferent inputs, and/or abnormal sensorimotor integration at the spinal interneuron level) mechanisms are implicated in PLMS generation and modulation.2 PLMS have been reported in patients with spinal cord injuries, even in cases of complete spinal transection, further supporting a supraspinal mechanism.3 It appears that the spinal generators are modulated and integrated in a complex circuit, involving supratentorial structures. Even though the pathophysiology of PLMS is still an open issue, there is growing evidence that PLMS are not a simple motor phenomenon, and may have a complex and dynamic interaction with cortical circuits and arousals.
The flexion reflex arc involves several synaptic links including flexion reflex afferents such as nociceptors and mechanoreceptors, which synapse on excitatory interneurons. These excitatory interneurons activate ipsilateral flexor motor neurons as well as the inhibitory interneurons, thereby diminishing ipsilateral extensor motor neurons. All of these excitatory and inhibitory neurons are under the influence of supraspinal inhibitory upper motor neuron influence.
The presence of PLMS in the proximal portion of an amputated lower extremity supports theories of spinal and supraspinal mechanisms in PLMS generation; and demonstrates that intact distal motor efferent pathways and distal sensory afferent pathways are not absolutely necessary for generation of PLM. Our case demonstrates the utility of ventral thigh surface electromyography in a limb with an above-the-knee amputation to assess for PLMs. A limitation of our case is that it is not possible to establish whether PLMS were present prior to the traumatic lower extremity injury; thus, we cannot necessarily determine whether PLMS appeared after the injury. Also, objective PLMS assessment was not performed after initiation of positive airway pressure therapy; therefore, postpositive airway pressure therapy change in PLM index was not assessed.
DISCLOSURE STATEMENT
The authors report no conflicts of interest. Patient has signed informed consent.
REFERENCES
- 1.American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine;2014. [Google Scholar]
- 2.Bara-Jimenez W, Aksu M, Graham S, Sato S, Hallett M. Periodic limb movements in sleep: state-dependent excitability of the spinal flexor reflex. Neurology. 2000;54(8):1609–1616. doi: 10.1212/wnl.54.8.1609. [DOI] [PubMed] [Google Scholar]
- 3.Ferri R, Proserpio P, Rundo F, et al. Neurophysiological correlates of sleep leg movements in acute spinal cord injury. Clin Neurophysiol. 2015;126(2):333–338. doi: 10.1016/j.clinph.2014.05.016. [DOI] [PubMed] [Google Scholar]