Abstract
Purpose
To evaluate the association of epilation before surgery on the surgical outcome in trachomatous trichiasis (TT) patients.
Methods
As a secondary data analysis, 1452 patients enrolled in the STAR trial were categorized according to preoperative epilation status. The main outcome was recurrent trichiasis after surgery. We used multivariable analysis, time-to-event analysis, and Cox proportional hazards model.
Results
Those who epilated prior to surgery tended to be older and female, with worse entropion at baseline. The proportion with postoperative trichiasis was 7.7%, 8.8% in those who epilated versus 5.3% in those who did not (P = 0.03). Adjusting for age and sex, the risk of postoperative TT with epilation was 1.71 (P value = 0.02). Although entropion may be in the biological pathway from epilation to postoperative TT, we adjusted for entropion, and the risk of postoperative TT with epilation was 1.41 (P = 0.14).
Conclusions
The study suggests that preoperative epilation may increase the risk of postoperative trichiasis. Further research is needed to confirm the finding.
Translational Relevance
Patients with TT often self-treat, epilating their inturned eyelashes. The World Health Organization recommends surgery to treat TT, but when patients refuse the procedure or mild trichiasis is present, epilation is often recommended. There is some evidence that repetitive or improper epilation can be harmful to the lid and hair follicles. If there is damage to the lid margin, any subsequent surgery could have deleterious outcomes.
Keywords: trichiasis, trachoma, epilation, postoperative trichiasis
Introduction
Trachoma, the leading infectious cause of blindness worldwide,1 is the result of repeated infection with ocular strains of Chlamydia trachomatis.2 The infections produce inflammation of the conjunctiva,2 and with repeated episodes, scarring develops1,3 that leads to entropion and trichiasis.4,5 The eyelashes turn toward the eye and rub the cornea, leading to opacification and visual loss.1,6
The World Health Organization (WHO) defines trachomatous trichiasis (TT) as at least one eyelash touching the globe or evidence of recent epilation of inturned eyelashes.7 Persons with trichiasis report considerable pain,8 so they will epilate the trichiatic lashes, and have to do so repeatedly. The procedure is commonly performed by the patient,6 a helper, or a health care professional.5 Rajak et al.5 reported 76.8% of TT patients in Ethiopia were epilating, with frequencies between once a week to once a month.
WHO recommends surgery for all TT patients, even if only one eyelash touches the eye. Surgery is effective in reducing pain and photophobia.2,9,10 However, recurrence of trichiasis after surgery can be as high as 50% after 2 years of follow-up.11 For this reason, WHO has recommended epilation for those who refuse surgery,12 and some countries' programs offer epilation to those who have just a few lashes that do not touch the cornea.4,5
This recommendation prompted a review of the safety of epilation for persons with trichiasis. Epilation—depilation or plucking—involves the removal of the hair shaft and the bulb.13 The phase of growth of the eyelashes can influence the need and frequency of epilation; if the eyelash is plucked during the inactive phase of growth, activity and regrowth are induced.14,15 A study in mice on the effect of plucking hairs during different phases of the follicular cycle showed that plucking induced mitotic activity, even with incomplete epilation,14 and plucking during the anagen period reduced the development period in the growing hair13,14 and can cause follicles to be damaged.16 Researchers observed an increment in the thickness of the epidermis16 where the club hair or inactive hair, was plucked.14 With repetitive plucking, the epidermis became less responsive, possibly due to a decrease in the number of stimulus-responsive cells.16 In human follicles, plucking alters the mesenchymal sheath of the hair, and the microtrauma produces edema, hyperemia, inflammation, and hemorrhages.17 Also, repetitive epilation may permanently harm the matrix,13,16 the portion of the hair that grows actively18 and contains the follicular stem cells.19 This damage to the matrix is in part explained by the removal of the stimulus-responsive cells.16
In addition to epilation itself, the actual practice involves the use of a variety of tools and invasive methods, such as using hand- or machine-made forceps, burning the eyelash with hot coals, cutting or pulling the eyelash with fingers,5 or using sticky tree resin to pluck the lash, as observed in the Amazon region. Epilation to treat minor trichiasis was associated with worse outcomes in a trial of epilation versus surgery.4
In general, common adverse effects described as associated with epilation and the epilation methods are as follows: discomfort, pain, irritation, scarring and burns of the skin, folliculitis and pseudofolliculitis (especially in androgenized areas),20 and postinflammatory hyperpigmentation of the lid.13,18 Poor technique or poor quality of forceps can cause incomplete epilation and broken lashes5 that could produce more damage.6
While epilation is generally perceived as a relatively harmless practice, the above findings suggest that there may be damage to the lid margin with repeated epilation that could worsen the inflammation and the entropion already caused by trachomatous scarring. Moreover, preoperative epilation could negatively affect the outcome of surgery for trichiasis, although there are no data on this.
The purpose of the study was to evaluate the effect of epilation before surgery on the surgical outcome in patients with TT.
Methods
We conducted secondary analyses using data from a randomized clinical trial of antibiotic use following trichiasis surgery, the Surgery for Trichiasis, Antibiotics to Prevent Trichiasis (STAR) Trial, which enrolled patients in Wolayta Soddo zone of southern Ethiopia in 2002. The design and outcomes of this study have been reported previously.3,8,9,21–23 In short, we found that epilation prior to surgery did not differ between the two randomization arms and that use of a single dose of azithromycin post surgery significantly reduced trichiasis recurrence.3 For this study, we used all the participants enrolled at baseline (n = 1452).
To be eligible, participants had to have upper lid trichiasis in at least one eye, have had no previous trichiasis surgery, and be age 18 years or older. At baseline, trained TT surgeons did the screening for trichiasis using a torchlight with patient's eyes in primary gaze. We evaluated the presence of eyelashes in contact with the eye, number of eyelashes touching the globe and the cornea, location of trichiatic eyelashes, age, gender, and the severity of entropion. Evidence of epilation was based on patient self-report and on the visualization of eyelash bases, short lash stubs, or broken lashes. Entropion was categorized as mild, moderate, or severe as follows: mild: all lash bases visible in the region with trichiasis; moderate: one or more lash bases inturned, but some still visible; severe: bases not visible.
Follow-up evaluations for postoperative trichiasis were conducted at 2 weeks and 2, 6, and 12 months after the trichiasis surgery. The definition of postoperative trichiasis was at least one eyelash touching the globe or new evidence of epilation. Study eyes were removed from further follow-up if postoperative trichiasis was found.
The Johns Hopkins Medical Institutions Institutional Review Board (JHMI-IRB) and the Ethiopian Science and Technology National Ethical Clearance Committee approved the study. Written informed consent was obtained from all participants.
Data Analysis
Data were analyzed using statistical software (Stata 15; StataCorp LLC, College Station, TX). Patients were categorized into two groups, depending on whether there was evidence of epilation at baseline or not. The data on epilation status were combined across both treatment arms and the results adjusted by azithromycin use. Demographic and baseline characteristics were analyzed by presence or absence of epilation at baseline and were tested for differences using Pearson χ2. Those characteristics found to be different by epilation group were entered into the multivariable models, with the exception of the variable “duration of trichiasis,” as only one case of postoperative TT was found in the group with duration of less than 2 years. We then performed time-to-event analysis, using a Kaplan-Meier curve to compare the time of recurrence by epilation status. To adjust for potential confounders and to determine any mediating factors, we used Cox proportional hazards model to estimate the hazard ratio, P value, and 95% confidence interval (CI) for each factor related to postoperative trichiasis.
Results
The analysis included data from all participants enrolled at baseline in the STAR trial (n = 1452). The majority of participants, 77.2%, were female (n = 1121), 75.4% were over 40 years of age (n = 10940), and 985 (68%) were classified as epilating before surgery. The vast majority (1322, or 91%) suffered from trichiasis for more than 2 years, with only 8% having trichiasis for less than 2 years. Of the 1452, 810 participants (56%) had mild entropion, 417 (29%) had moderate, and 225 (16%) severe. Lid closure defect was found in five participants.
Table 1 summarizes preoperative differences between the group of people who were epilating and the group not epilating. The group who were epilating tended to be older (P = 0.02) and female (P < 0.002). Almost all those epilating had had trichiasis for more than 2 years, with only 6% (n = 61) of epilators having trichiasis for less than 2 years (P = 0.02). Those epilating had a more severe grade of entropion (P ≤ 0.002). Epilation status did not differ by the original trial randomization arm (P = 0.57).
Table 1.
Baseline Characteristics of STAR Trial Participants by Epilation Status
| Epilate |
Do Not Epilate |
P Value |
|||
|
N |
% |
n |
% |
||
| Age | 0.024 | ||||
| Age <40 years | 224 | 22.74 | 134 | 28.69 | |
| ≥40 and ≤60 years | 492 | 49.95 | 228 | 48.82 | |
| >60 years | 269 | 27.31 | 105 | 22.48 | |
| Gender | <0.002 | ||||
| Male | 192 | 19.49 | 139 | 29.76 | |
| Female | 793 | 80.51 | 328 | 70.24 | |
| Entropion | <0.002 | ||||
| Mild | 458 | 46.50 | 352 | 75.37 | |
| Moderate | 352 | 35.74 | 65 | 13.92 | |
| Severe | 175 | 17.77 | 50 | 10.71 | |
| Trichiasis duration | <0.02 | ||||
| <1 year | 8 | 0.81 | 22 | 4.67 | |
| ≥1 and <2 years | 53 | 5.38 | 43 | 9.13 | |
| ≥2 years | 924 | 93.81 | 398 | 84.50 | |
| Don't know/missing | 0 | 8 | 1.70 | ||
| Number of lashes touching the globe | |||||
| None | 309 | 31.37 | 0 | 0 | a |
| 1–5 | 292 | 29.64 | 230 | 49.25 | |
| 6–9 | 150 | 15.23 | 89 | 19.06 | |
| More than 10 | 234 | 23.76 | 148 | 31.69 | |
| Number of lashes touching the cornea | |||||
| None | 364 | 36.95 | 58 | 12.42 | a |
| 1–5 | 423 | 42.94 | 258 | 55.25 | |
| 6–9 | 83 | 8.43 | 46 | 9.85 | |
| >10 | 115 | 11.68 | 105 | 22.48 | |
| Treatment | 0.57 | ||||
| Tetracycline | 333 | 33.81 | 151 | 32.33 | |
| Azithromycin | 652 | 66.19 | 316 | 67.67 | |
Since epilation can result in no/fewer lashes touching the globe, the numbers in the two groups are not comparable.
We report the number of eyelashes touching the globe and the cornea by epilation status, but since epilation can result in no/fewer lashes touching the globe, the numbers are not really comparable. Of note, 309 (32%) of the participants in the epilation group had no lashes touching the globe, and 364 (37%) had no lashes touching the cornea.
A total of 107 participants (8%) had postoperative TT after surgery by 1 year of follow-up, most within the first 6 months of surgery. The majority of participants who had trichiasis after surgery were in the group of participants with a positive history of epilation, as shown in Table 2.
Table 2.
Recurrence of Trichiasis After Surgery by Epilation Status
| Time to Follow-Up |
|||||
| 2 Weeks |
2 Months |
6 Months |
12 Months |
Total |
|
| Total N (population at risk) | 1452 | 1444 | 1398 | 1339 | |
| Epilation group | |||||
| N (population at risk) | 985 | 981 | 947 | 903 | |
| n (recurrence) | 1 | 21 | 38 | 23 | 83 |
| Recurrence % | 0.1 | 2.14 | 4.01 | 2.54 | 8.79 |
| Lost at end of interval | 3 | 13 | 4 | ||
| Nonepilation group | |||||
| N (population at risk) | 467 | 463 | 451 | 434 | |
| n (recurrence) | 2 | 8 | 9 | 5 | 24 |
| Recurrence % | 0.43 | 1.73 | 1.99 | 1.15 | 5.3 |
| Lost at end of interval | 2 | 4 | 8 | ||
Bold-italic formatting indicates the total recurrence across all months.
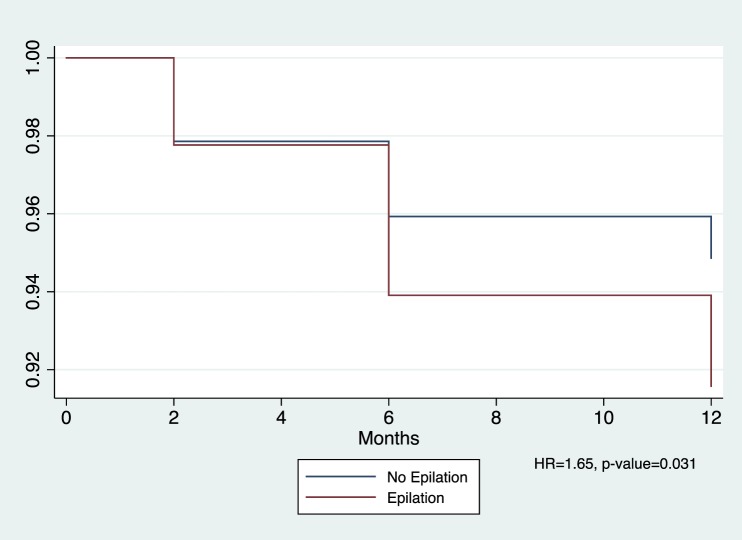
The Figure shows the differences in time to recurrence between the epilation and nonepilation groups after 12 months of follow-up. The unadjusted risk of recurrence of TT after surgery was 65% greater in the group epilating before surgery compared with the group not epilating (P = 0.031).
Figure.
Kaplan-Meier analysis of TT recurrence after surgery.
In addition to epilation, severity of entropion and duration of trichiasis were also related to postoperative TT (Table 3). Of note, there was only one case of postoperative TT in the group with duration of TT at baseline that was less than 2 years, and that case was in the epilation group. This variable was therefore not included in the final models. We constructed two Cox proportional hazards models to estimate the hazard ratio for postoperative TT according to epilation status, under two conditions (Table 4). First, adjusting for age and sex, the risk of postoperative TT with epilation was 1.71 (P = 0.02). Second, we also have adjusted for entropion, which may either be in the biological pathway from epilation to postoperative TT or be simply a confounder. Adjusting for entropion, the risk of postoperative TT with epilation was 1.41, P = 0.14.
Table 3.
Factors Associated With Recurrence of Trichiasis by 1 Year After Surgery
| HR |
P Value |
95% CI |
|
| Age | 1.12 | 0.417 | 0.85, 1.46 |
| Gender | 0.72 | 0.118 | 0.47, 1.08 |
| Epilation status | 1.65 | 0.031 | 1.05, 2.59 |
| Grade of entropion | 1.7 | <0.0002 | 1.35, 2.15 |
HR, hazard ratio.
Table 4.
Cox Regression Models of Risk of Recurrence With Epilation
| HR |
SE |
z |
P > |z| |
95% CI |
||
| Model 1 | ||||||
| Gender | 0.67 | 0.14 | −1.8 | 0.07 | 0.44 | 1.03 |
| Age | 1.07 | 0.14 | 0.51 | 0.6 | 0.82 | 1.4 |
| Epilation status | 1.71 | 0.39 | 2.29 | 0.02 | 1.08 | 2.7 |
| Model 2 | ||||||
| Gender | 0.61 | 0.13 | −2.22 | 0.02 | 0.4 | 0.94 |
| Age | 1.03 | 0.14 | 0.24 | 0.81 | 0.78 | 1.35 |
| Epilation status | 1.41 | 0.33 | 1.45 | 0.14 | 0.88 | 2.25 |
| Grade of entropion | 1.68 | 0.21 | 4.25 | <0.0002 | 1.32 | 2.14 |
Discussion
Understanding the factors that increase the risk of unfavorable outcomes after surgery is important because high recurrence rates after surgery can affect trachoma programs,12 undermining patient trust in the program and challenging the planning process due to the increase in numbers of postoperative TT. Some factors associated with recurrent TT following surgery are the severity of trichiasis prior to surgery,22 degree of entropion prior to surgery,5 surgeon skills,22 and previous trichiasis surgery.3 Because of the current practice of recommending epilation in programs, we undertook secondary data analyses to explore the effect of epilation before surgery on the surgical outcome in patients with TT.
Epilation was common in this series of patients with TT, with 68% having evidence of epilation prior to surgery. This is a common finding, especially in patients with severe trichiasis.5 In our study, we found that epilators tended to have more severe entropion (18%) compared to the nonepilators (11%), and this was also described by Rajak et al.5
We found a statistically significant association between epilation before surgery and higher rate of postoperative trichiasis. These findings are supported by data from a trial comparing epilation and surgery, where surgery was ultimately offered to those in the epilation arm.4 Those who had epilation followed by surgery had worse outcomes compared to the group who had surgery alone. There are limitations with that comparison, notably that the surgery group could have been epilating prior to surgery as well and that the epilation-to-surgery group had more severe disease at baseline.4 In our study, the association was no longer significant once we adjusted for severity of entropion, suggesting that entropion could be a confounder or a mediator (that is, epilation causes a worsening of entropion as the mechanism by which it leads to postoperative trichiasis).
To truly test this hypothesis, we would need data over time on epilation and entropion severity in order to perform mediation analyses. Such data were not available and indeed would be difficult to obtain because epilation itself is an indication for surgery and simply following TT cases over time without intervention is not ethical.
Since all but one case of postoperative TT occurred in the group with a duration of trichiasis of more than 2 years, we were unable to evaluate the potential effect of duration of time epilating on our outcome. Misclassification may also be a potential problem. It is possible for example, that a subject may have epilated, then stopped epilation and reported not epilating; with no evidence of newly growing lashes, the case would be classified as “nonepilator.” To the extent this group had worse outcomes as our data suggest, the misclassification would drive the results toward the null.
Eyelash follicles are similar to scalp hair follicles, with a shorter growth cycle that makes them shorter than scalp hair.24 Follicles are located anterior to the tarsal plate, in a deeper position with wider bulbs in the upper eyelid compared with the lower eyelid.15 In the lid, the epidermis is very thin, with a high density of melanocytes in the basal layer, and the hypodermis is absent.24,25 Epilation can be associated with erythema, edema, folliculitis, pseudofolliculitis, postinflammatory hyperpigmentation, and depigmentation,13,18 although the majority of these signs are of short duration.26 In mouse models, whose hair follicles are similar to that of humans,25 epilation induces inflammatory changes, hair keratinocyte apoptosis, and eventually hair regeneration.27 Hair follicles can suffer permanent damage, as observed with continuous eyebrow plucking, in association with infections from skin trauma.28,29
In addition to the well-described inflammatory changes with scarring in trachoma,30 which lead to entropion, it is possible that epilation adds to the inflammatory burden that leads to worse entropion. If this is the case, then our finding and that of others that epilators have worse entropion may be due to a causal effect of epilation on entropion. Since more severe entropion leads to a greater likelihood of postoperative recurrent trichiasis, our adjustment for entropion in examining the relationship of epilation and postoperative recurrence would be inappropriate; we would be adjusting for the mechanism by which epilation might produce recurrent trichiasis. Thus, the first model, where no adjustment is made for entropion, would be the correct model to assess the risk of recurrent trichiasis with epilation.
On the other hand, if epilation has no effect on entropion, and persons with worse entropion are simply more likely to choose to epilate, then entropion is truly a confounding factor in our understanding of the relationship between epilation and postsurgical recurrence. In this case, the second model is appropriate, which suggests an increased risk of recurrence with epilation, but one reduced to 1.41 and no longer statistically significant. There is cross-sectional evidence that epilation may decrease the risk of corneal opacity, although it is not possible to rule out the bias that persons with corneal opacity simply stopped epilating, not that epilating was protective.5,23
With our study design, we are unable to determine which of the two scenarios—epilation adding to the development of severe entropion (mediation) versus epilation not contributing to entropion (confounding)—is the more likely one. Ideally, a study would randomize persons with mild entropion and mild TT to epilation or no epilation and follow inflammatory changes and progression of entropion in both groups; clearly, such a study would be unethical as once someone develops TT, that person is at risk for vision loss and must be counseled for trichiasis management, including surgery.
Our study has the limitation that self-report of epilation, even though we also required physical evidence, may lead to misclassification. There is imperfect concordance between physical examination and patient self-report of epilation. We also note the study was carried out in Ethiopia, and the findings may not be generalizable to areas where epilation frequency or practices differ.
However, we investigated this issue out of concern that epilation has been recommended as an optional treatment for patients with minor TT.4,5,12 More research is needed to confirm our exploratory findings or provide more evidence that suggests epilation does not increase the risk of worse entropion or of surgical recurrence. Clearly, however, where surgery has been refused or no surgery is available, preventing lashes from touching the globe is important to reduce the risk of vision loss, and epilation is often the only viable alternative.
Acknowledgments
Disclosure: S.L. Talero, None; B. Muñoz, None; S.K. West, None
References
- 1.World Health Organization. Global WHO Alliance for the Elimination of Blinding Trachoma by 2020, progress report on elimination of trachoma, 2013. Wkly Epidemiol Rec. 2014;89:421–428. [PubMed] [Google Scholar]
- 2.Taylor HR, Burton MJ, Haddad D, West S, Trachoma. Wright H. Lancet. 2014;384:2142–2152. doi: 10.1016/S0140-6736(13)62182-0. . 201413; [DOI] [PubMed] [Google Scholar]
- 3.West SK, West ES, Alemayehu W, et al. Single-dose azithromycin prevents trichiasis recurrence following surgery: randomized trial in Ethiopia. Arch Ophthal. 2006;124:309–314. doi: 10.1001/archopht.124.3.309. [DOI] [PubMed] [Google Scholar]
- 4.Habtamu E, Rajak SN, Tadesse Z, et al. Epilation for minor trachomatous trichiasis: four-year results of a randomised controlled trial. PLoS Negl Trop Dis. 2015;9:e0003558. doi: 10.1371/journal.pntd.0003558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajak SN, Habtamu E, Weiss HA, et al. Epilation for trachomatous trichiasis and the risk of corneal opacification. Ophthalmology. 2012;119:84–119. doi: 10.1016/j.ophtha.2011.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alemayehu W, Melese M, Bejiga A, Worku A, Kebede W, Fantaye D. Surgery for trichiasis by ophthalmologists versus integrated eye care workers: a randomized trial. Ophthalmology. 2004;111:578–584. doi: 10.1016/j.ophtha.2003.06.030. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Trachoma Simplified Grading Card 1987 . SAFE documents. http://www.who.int/blindness/causes/trachoma_documents/en/ Accessed January 13, 2018.
- 8.Wolle MA, Cassard SD, Gower EW, et al. Impact of trichiasis surgery on physical functioning in Ethiopian patients: STAR trial. Am J Ophthalmol. 2011;151:850–857. doi: 10.1016/j.ajo.2010.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woreta TA, Munoz BE, Gower EW, Alemayehu W, West SK. Effect of trichiasis surgery on visual acuity outcomes in Ethiopia. Arch Ophthalmol. 2009;127:1505–1510. doi: 10.1001/archophthalmol.2009.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta KM, Harding JC, Othman MS, Merbs SL, Gower EW. Why do patients refuse trichiasis surgery? Lessons and an education initiative from Mtwara Region, Tanzania. PLoS Negl Trop Dis. 2018;12:e0006464. doi: 10.1371/journal.pntd.0006464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.West ES, Mkocha H, Munoz B, et al. Risk factors for postsurgical trichiasis recurrence in a trachoma-endemic area. Invest Ophthalmol Vis Sci. 2005;46:447–453. doi: 10.1167/iovs.04-0600. [DOI] [PubMed] [Google Scholar]
- 12.Courtright P, Gower EW, Kello AB, Solomon AW. World Health Organization Alliance for Global Elimination of Trachoma by 2020: Second Global Scientific Meeting on Trachomatous Trichiasis. Geneva: World Health Organization; 2016. [Google Scholar]
- 13.Shenenberger DW, Utecht LM. Removal of unwanted facial hair. Am Fam Physician. 2002;66:1907–1911. [PubMed] [Google Scholar]
- 14.Johnson E, Ebling FJ. The effect of plucking hairs during different phases of the follicular cycle. J Embryol Exp Morphol. 1964;12:465–474. [PubMed] [Google Scholar]
- 15.Elder MJ. Anatomy and physiology of eyelash follicles: relevance to lash ablation procedures. Ophthalmic Plast Reconstr Surg. 1997;13:21–25. doi: 10.1097/00002341-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Potten CS, Hamilton E. The effect of repeated plucking on mouse skin cell kinetics. J Invest Dermatol. 1974;62:560–562. doi: 10.1111/1523-1747.ep12679330. [DOI] [PubMed] [Google Scholar]
- 17.Bassukas ID, Hornstein OP. Effects of plucking on the anatomy of the anagen hair bulb. Arch Dermatol Res. 1989;281:188–192. doi: 10.1007/BF00456391. [DOI] [PubMed] [Google Scholar]
- 18.Wanitphakdeedecha R, Alster TS. Physical means of treating unwanted hair. Dermatol Ther. 2008;21:392–401. doi: 10.1111/j.1529-8019.2008.00220.x. [DOI] [PubMed] [Google Scholar]
- 19.Olsen EA. Methods of hair removal. J Am Acad Dermatol. 1999;40:143–155. doi: 10.1016/s0190-9622(99)70181-7. [DOI] [PubMed] [Google Scholar]
- 20.Azziz R. The evaluation and management of hirsutism. Obstet Gynecol 101:995–1007. doi: 10.1016/s0029-7844(02)02725-4. . 20031; [DOI] [PubMed] [Google Scholar]
- 21.West S, Alemayehu W, Munoz B, Gower EW. Azithromycin prevents recurrence of severe trichiasis following trichiasis surgery: STAR trial. Ophthalmic Epidemiol. 2007;14:273–277. doi: 10.1080/09286580701410323. [DOI] [PubMed] [Google Scholar]
- 22.Gower EW, Merbs SL, Munoz BE, et al. Rates and risk factors for unfavorable outcomes 6 weeks after trichiasis surgery. Invest Ophthalmol Vis Sci. 2011;52:2704–2711. doi: 10.1167/iovs.10-5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West ES, Munoz B, Imeru A, Alemayehu W, Melese M, West SK. The association between epilation and corneal opacity among eyes with trachomatous trichiasis. Br J Ophthalmol. 2006;90:171–174. doi: 10.1136/bjo.2005.075390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thibaut S, De Becker E, Caisey L, et al. Human eyelash characterization. Br J Dermatol. 2010;162:304–310. doi: 10.1111/j.1365-2133.2009.09487.x. [DOI] [PubMed] [Google Scholar]
- 25.Paus R, Burgoa I, Platt CI, Griffiths T, Poblet E, Izeta A. Biology of the eyelash hair follicle: an enigma in plain sight. Br J Dermatol. 2016;174:741–752. doi: 10.1111/bjd.14217. [DOI] [PubMed] [Google Scholar]
- 26.Litak J, Krunic AL, Antonijevic S, Pouryazdanparast P, Gerami P. Eyebrow epilation by threading: an increasingly popular procedure with some less-popular outcomes—a comprehensive review. Dermatol Surg. 2011;37:1051–1054. doi: 10.1111/j.1524-4725.2011.02016.x. [DOI] [PubMed] [Google Scholar]
- 27.Li H, Fan L, Zhu S, et al. Epilation induces hair and skin pigmentation through an EDN3/EDNRB-dependent regenerative response of melanocyte stem cells. Sci Rep. 2017;7:7272. doi: 10.1038/s41598-017-07683-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tomc CM, Malouf PJ. Eyebrow restoration: the approach, considerations, and technique in follicular unit transplantation. J Cosmet Dermatol. 2015;14:310–314. doi: 10.1111/jocd.12170. [DOI] [PubMed] [Google Scholar]
- 29.Insler MS, Zatzkis S. Periorbital cellulitis after eyebrow tweezing. Am J Ophthalmol. 1986;102:534–536. doi: 10.1016/0002-9394(86)90089-9. [DOI] [PubMed] [Google Scholar]
- 30.Hu VH, Macleod D, Massae P, et al. Non-chlamydial bacterial infection and progression of conjunctival scarring in trachoma. Invest Ophthalmol Vis Sci. 2018;59:2339–2344. doi: 10.1167/iovs.17-23381. [DOI] [PMC free article] [PubMed] [Google Scholar]